Population health monitoring has become a priority for large healthcare organizations. Rising chronic conditions, unmanaged risk, fragmented records, and widening care gaps put pressure on clinical and operational teams. Many health systems still use retrospective dashboards that show what happened last quarter, rather than what is happening with their patient population today.
An AI population health management platform addresses these challenges by bringing together clinical, claims, behavioral, and social data into one system. This approach reveals hidden risk patterns and suggests timely actions. It helps teams identify which groups need proactive support, assigns the right pathways, and coordinates follow-up across departments. Instead of waiting for avoidable escalations, organizations can spot issues early, use resources wisely, and distribute them more effectively.
At Intellivon, we have spent over a decade creating healthcare platforms that combine interoperability, workflow improvement, and AI-driven insights. With our experience, in this blog, we will guide you through the key steps to develop a patient engagement portal that can support real clinical and operational needs.
Key Takeaways of the Population Health Management Market
The population health management market is expanding rapidly as health systems respond to rising risk and operational strain. Market value stands at USD 63.5 billion in 2025 and is projected to reach USD 150.83 billion by 2030, supported by an 18.89% CAGR. This acceleration reflects a shift from retrospective reporting to real-time intelligence that can guide preventive care, cost reduction, and scalable clinical coordination.
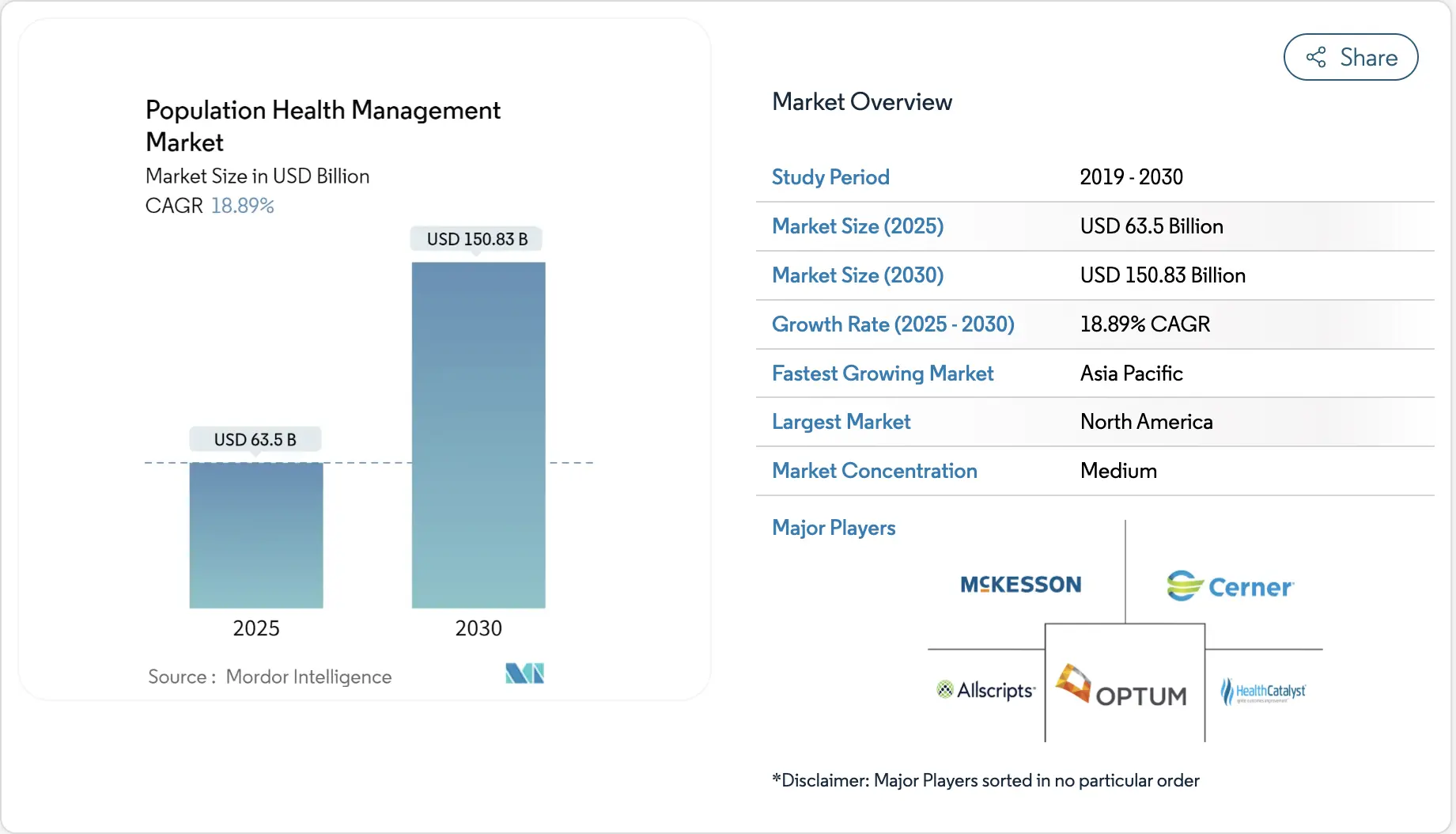
Key Growth Drivers
- Value-based payment models create demand for AI-driven risk prediction and care gap insights, with U.S. programs pushing faster adoption.
- Chronic disease growth requires earlier detection; AI-driven tools uncover undocumented conditions with 75% clinician acceptance.
- Converging data ecosystems enable unified EHR analytics, SDoH mapping, and personalized planning across large populations.
- Global regulatory initiatives strengthen interoperability and encourage cloud-native and AI-enabled infrastructure investments.
Adoption Statistics
- Predictive AI use in hospitals reached 71% in 2025, with large systems leading adoption.
- Multi-hospital networks show 81–86% penetration compared with 31–37% in independent hospitals.
- Epic-driven ecosystems report 90% adoption rates, influenced by native AI capabilities.
- Domain-specific AI climbed 7x year-over-year, especially in chronic care and quality management.
- Large hospitals achieved 90–96% deployment, while smaller organizations remained at 53–59%.
- Population health teams focused on workflow optimization and risk prediction, the two fastest-maturing categories.
AI-enabled population strategies deliver measurable clinical and financial outcomes. Health systems report improvements across cardiac and heart failure readmissions, prevention of avoidable hospitalizations, and meaningful reductions in overall care costs.
Programs at Geisinger and Kaiser show clear evidence that predictive models improve early detection and intervention. Revenue cycle teams also gain efficiency, with fewer errors in claims and earlier identification of overlooked conditions.
What Is an AI Population Health Management Platform?
An AI population health management platform unifies clinical, claims, behavioral, and social data to predict risk, guide interventions, and coordinate care across entire populations in real time.
An AI-enabled population health platform takes this further. It ingests data from EHRs, claims, remote monitoring, labs, and social determinants, then applies machine learning to stratify risk, detect emerging issues, and recommend targeted interventions. Instead of static reports, leaders get an operational system that supports prevention, early detection, and continuous improvement in how populations are managed.
By surfacing who is likely to deteriorate, what is driving that risk, and which action has the highest yield, the platform becomes a decision layer for both clinical and business strategy.
How It Works
This type of platform does not operate as a single algorithm. It functions as an end-to-end workflow that connects data, intelligence, and human action. The sequence matters because each stage builds trust and usability for clinical and operational teams.
Below is a simplified step-by-step view of how an AI population health platform typically works inside a large enterprise.
1. Aggregate Data from Fragmented Sources
The first step is to connect all relevant systems. This includes EHRs, claims platforms, lab systems, pharmacy data, remote monitoring feeds, and sometimes community datasets.
Data arrives in different formats and standards, so the platform must map, normalize, and timestamp each element. At this point, leaders decide which populations and contracts matter most, such as high-cost cohorts, value-based arrangements, or specific service lines.
2. Clean, Normalize, and Govern the Data
Once collected, data quality becomes the limiting factor. Missing values, inconsistent codes, and outdated records will weaken any model.
The platform applies validation rules, deduplication, and terminology mapping so that conditions, procedures, and medications follow a shared vocabulary. Governance policies define who can see what, how PHI is protected, and how audits will be conducted over time.
3. Build Longitudinal Patient and Population Views
After standardization, the platform creates longitudinal records. Each patient’s encounters, results, prescriptions, and social context are stitched into a single timeline.
On top of that, populations are defined by contract, geography, condition, or risk profile. This allows teams to shift between an individual view and a cohort view without losing context.
4. Generate Predictive and Prescriptive Insights
With a stable data foundation, machine learning models can operate reliably. They estimate readmission risk, likelihood of complications, cost trajectories, or gaps in care.
In addition to predicting outcomes, some models identify which factor contributes most to that risk. This helps teams understand whether medication adherence, access barriers, or clinical instability is driving the score. The platform then surfaces recommended actions that match the identified drivers.
5. Trigger Workflows and Assign Tasks to Teams
Insights only matter when they reach the right person at the right time. The platform routes alerts and task lists into existing tools, such as case management systems, EHR inboxes, or care coordination dashboards.
High-risk patients may be assigned to specialized teams, while moderate-risk groups receive automated outreach or telehealth follow-up. Clear routing rules prevent alert fatigue and keep each role focused on actions that match their scope.
6. Execute Interventions and Track Response
Care teams then carry out the interventions. This may involve scheduling earlier follow-up visits, arranging home health services, adjusting medication plans, or connecting patients with social support.
The platform tracks which interventions were performed and how quickly. Over time, it learns which combinations of actions lead to fewer admissions, better control of chronic conditions, and stronger patient engagement.
7. Learn, Refine, and Report Outcomes
The final step is continuous learning. The system measures outcomes across cohorts, comparing predicted risk with actual results.
Models are retrained with new data, thresholds are tuned, and workflows are adjusted. Leadership teams receive clear views of performance against contracts, quality targets, and financial goals, which inform strategy for the next planning cycle.
In practice, an AI population health management platform operates as a living system rather than a static tool. It connects data, analytics, and frontline workflows in a loop that constantly refines how populations are managed. When this loop is designed well, organizations see a steady shift from reactive care toward earlier, targeted, and more efficient interventions.
AI Population Health Management Platforms Reduce Unplanned Readmission Rates by 29%
AI-enabled population health platforms can significantly reduce preventable readmissions by combining unified data, predictive modeling, and workflow-ready care coordination. A Mayo Clinic-affiliated study documented a 29% relative reduction after implementing an AI-driven readmission tool.
AI population health platforms help resolve these breakdowns. They evaluate clinical and non-clinical indicators in real time to identify who is most likely to deteriorate after discharge. Care managers can then adjust workflows, escalate support, or schedule earlier follow-ups for those who need it. This shift from blanket protocols to precise intervention is what produces sustained reduction in readmission metrics.
A Mayo Clinic–affiliated academic medical center captured this effect clearly. After deploying an AI-driven readmission predictor inside daily discharge routines, unplanned 30-day readmissions dropped from 11.4% to 8.1%, representing a 29% relative reduction.
1. Why AI Outperforms Traditional Readmission Scoring
Conventional scoring systems rely on static inputs and rarely adapt to changes in a patient’s condition. They also fail to incorporate unstructured data like notes, social factors, or recent utilization patterns. This limits their ability to identify emerging signals of clinical decline.
AI models continuously learn from diverse data sources. They process vitals, labs, medications, comorbidities, trends over time, and behavioral indicators. Because predictions refresh throughout the admission, clinicians get a current view of risk rather than a fixed score assigned at admission.
This dynamic approach allows teams to intervene sooner. High-risk cases are no longer lost in the average. Instead, each patient receives a level of planning aligned with their likelihood of returning within 30 days.
2. How AI Platforms Support Scalable Care Coordination
Reducing readmissions is not only about prediction. It depends on how quickly operational teams can act on early warnings. AI platforms strengthen this coordination by routing alerts, prioritizing caseloads, and aligning tasks across nurses, discharge planners, and social workers.
Teams receive structured recommendations based on each patient’s risk drivers. This may include medication reconciliation, home health referral, transportation support, or early primary-care follow-up. When these actions are triggered consistently, the odds of a return trip drop.
Scalability is the key advantage. Instead of expanding staff, health systems use AI to focus attention where it creates the highest impact.
3. Real-World Evidence Shows Clear Financial and Clinical Gains
The Mayo Clinic–affiliated study is one of the clearest examples of enterprise-scale impact. By embedding the prediction model directly into clinician workflows, the organization improved outcomes without increasing workload.
The reduction from 11.4% to 8.1% was achieved through better prioritization and structured follow-up. This directly translates into stronger quality scores, reduced penalties, and improved operational efficiency across the system.
For enterprises pursuing value-based care, these gains offer a defensive and growth-oriented advantage. More accurate targeting means fewer preventable admissions and more predictable resource use.
AI-driven population health platforms strengthen early detection, streamline coordination, and improve discharge transitions. When implemented within daily workflows, they reduce unplanned readmissions at a scale that manual processes cannot match. The evidence shows that predictive capabilities paired with operational alignment deliver meaningful clinical and financial outcomes.
Key Features of an AI Population Health Management Platform
AI population health platforms rely on predictive models, unified data infrastructure, workflow automation, and interoperability to manage risk and coordinate care at scale.
Enterprise leaders evaluating population health systems often look for capabilities that go beyond dashboards. The value comes from how well the platform connects insight with action. The features below represent the core elements that support real operational scale.
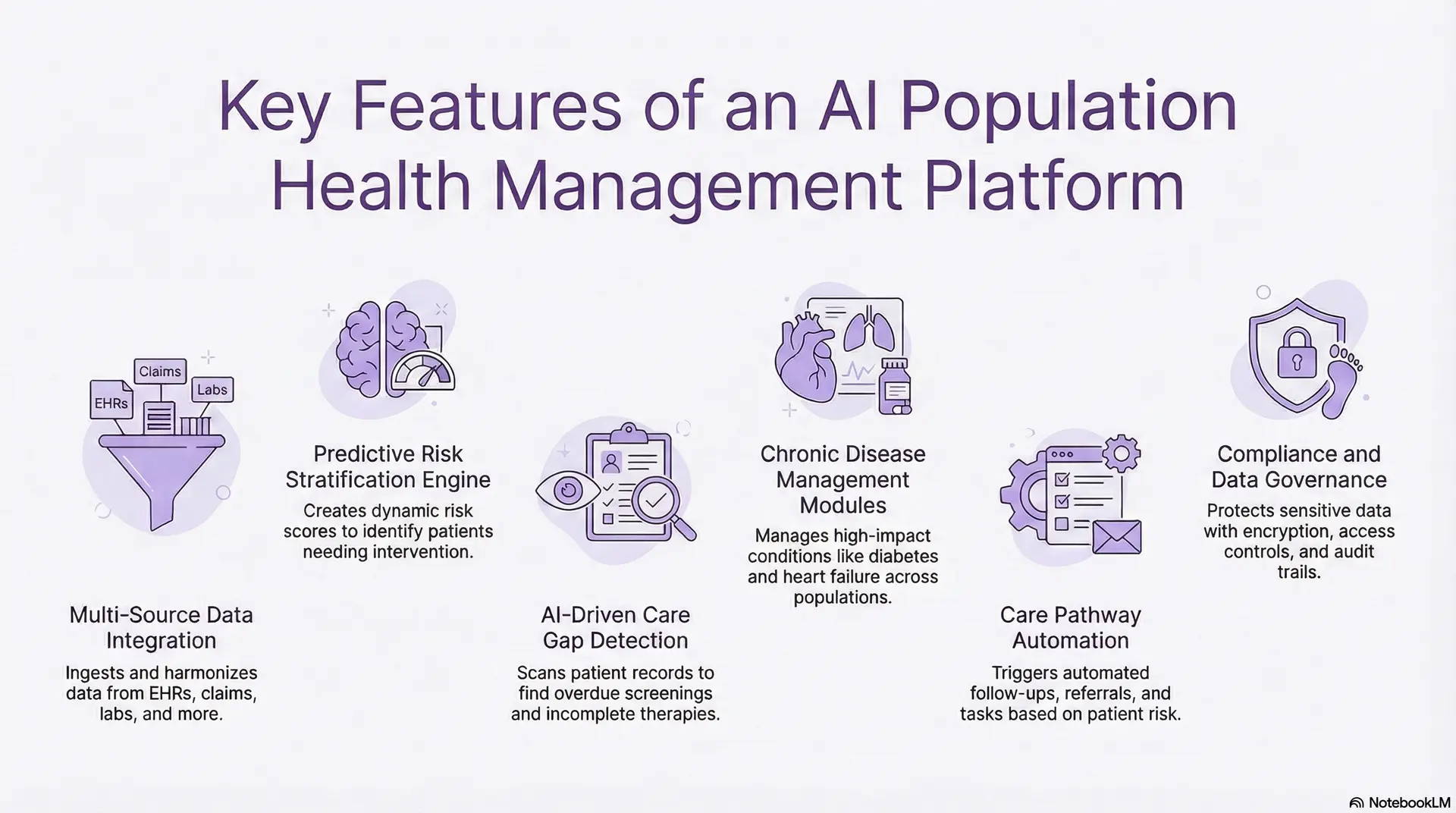
1. Predictive Risk Stratification Engine
A risk engine estimates who is likely to decline, return to the hospital, or experience complications. It evaluates vitals, labs, comorbidities, medication patterns, and social indicators to create a dynamic risk score that updates as new information appears.
Teams use these scores to set priorities for discharge planning, remote monitoring, and chronic disease management. When models highlight the specific drivers behind risk, clinical and operational teams gain a clearer path to intervention.
2. Chronic Disease Management Modules
These modules help teams manage diabetes, heart failure, COPD, and other high-impact conditions across large populations. They aggregate longitudinal trends, identify therapy gaps, and flag unexpected deterioration.
Decision support tools guide care teams with evidence-based recommendations. Leaders can track control rates and utilization patterns across cohorts, which helps inform strategy for value-based contracts.
3. Care Pathway Automation
Care pathways translate insights into repeatable actions. When a patient reaches a certain risk level, the system can schedule earlier follow-ups, trigger referral workflows, or route tasks to case managers.
Automated rules reduce manual triage and ensure consistency across teams. Over time, these pathways adapt as the system learns which interventions deliver the greatest improvement for each population segment.
4. AI-Driven Care Gap Detection
This feature scans medical records, claims history, and notes to uncover overdue screenings, missing diagnoses, and incomplete therapy plans. It interprets both structured and unstructured data, which allows it to surface gaps that traditional rules-based systems may overlook.
Care teams receive curated lists with context and recommended actions. Closing these gaps improves quality measures and reduces preventable utilization.
5. Social Determinants of Health (SDoH)
SDoH data provides insight into risks that clinical records fail to capture. Housing instability, transportation challenges, food insecurity, and caregiver support often influence outcomes more than medical factors alone.
An AI-driven SDoH layer helps teams understand which social variables are elevating risk and which interventions may help. This guides more holistic care planning, especially for populations with complex needs.
6. Cohort Builder
A cohort builder helps teams group patients by condition, risk level, utilization pattern, payer contract, or geography. Segmentation makes it easier to run targeted programs and measure their impact.
These tools allow clinical, operational, and financial teams to collaborate with a shared view of defined populations. Leaders can also simulate scenarios and compare outcomes across cohorts.
7. Multi-Source Data Integration
A population health platform is only as strong as its data foundation. It needs to ingest EHR data, claims records, lab results, imaging reports, and remote monitoring streams with minimal friction.
The integration layer maps codes, resolves duplicates, and harmonizes standards. This creates a consistent baseline for analytics, modeling, and reporting.
8. FHIR/HL7-Based Interoperability
Interoperability ensures that data flows smoothly between the platform and existing clinical systems. FHIR and HL7 standards make it easier to connect to EHRs, imaging systems, and external partners.
Reliable interoperability reduces friction during deployment and minimizes disruption to clinical operations. It also ensures long-term scalability as new systems are added.
9. Compliance and Data Governance
Enterprise deployments require strong compliance safeguards. Encryption, access controls, audit trails, and data minimization policies protect sensitive information and reduce regulatory risk.
Advanced governance frameworks like HIPAA, GDPR, and the EU AI Act outline how data is shared, who receives access, and how models are monitored for fairness and accuracy. This strengthens trust across the organization.
A mature population health platform brings together prediction, coordination, and accountability in one environment. When these features work in harmony, organizations can shift from reactive management to anticipatory, scalable, and financially sustainable care delivery.
How AI Works Inside a Population Health Management Platform
AI in population health systems analyzes multi-source data, predicts risk, identifies care gaps, and guides coordinated interventions across entire patient cohorts.
AI becomes valuable when it turns complex, fragmented information into clear signals that teams can act on. In population health, this requires models that recognize early deterioration, uncover hidden risks, and recommend interventions that match each patient’s needs. The goal is not only prediction but also operational clarity.
Below is a structured view of how AI functions inside an enterprise-grade population health management platform.
1. Predictive Models Identify
A. Readmission Risk Forecasting
Models examine vitals, labs, diagnoses, comorbidities, and utilization patterns to predict the likelihood of a patient returning within 7, 14, or 30 days. These predictions refresh throughout the care journey, which gives teams real-time visibility into changing risk.
Enterprises use these insights to prioritize discharge planning, allocate case management resources, and schedule timely follow-up visits.
B. Cost Prediction and Utilization Forecasts
Predictive models estimate future spending based on chronic disease severity, historical claims, medication adherence, and social factors. This helps financial teams anticipate high-cost cases and plan outreach programs.
It also supports value-based care arrangements, where cost predictability is essential for meeting contract targets.
C. Chronic Disease Progression Modeling
AI detects subtle clinical trends that often precede disease escalation. For example, small fluctuations in weight, blood pressure, or medication patterns may signal worsening heart failure or COPD.
These early warnings support proactive interventions that reduce hospitalizations and stabilize long-term outcomes.
D. Hospitalization Likelihood Predictions
By combining clinical indicators with SDoH factors, the platform predicts who is likely to require acute care. This helps organizations deploy remote monitoring, home-based support, or urgent follow-ups before a crisis emerges.
2. Interpreting Clinical Notes with NLP
A. Extracting Diagnoses and Missing Details
AI-powered NLP scans clinician notes, imaging reports, and care summaries to surface undocumented conditions or overlooked symptoms. This reduces coding errors and improves risk adjustment accuracy.
The platform then integrates these findings with structured data to create a more complete picture of each patient.
B. Detecting Care Gaps
NLP identifies screening requirements, overdue tests, medication issues, or recommended follow-ups hidden in documentation. These gaps are highlighted for care managers and routed to workflows that close them efficiently.
3. Computer Vision Identifies Imaging Trends
A. Pattern Recognition Across Large Populations
Computer vision models analyze radiology images over time to detect subtle patterns linked to disease progression. When combined with EHR data, these insights help stratify risk with greater precision.
This provides a population-level understanding of imaging trends that manual review cannot replicate.
4. Generative AI Supports Care Summaries
A. Producing Patient Summaries
Generative AI creates concise, clinically aligned summaries that help physicians and case managers understand a patient’s history quickly.
These summaries highlight risk drivers, key events, and recommended next steps, which reduces time spent reviewing complex records.
B. Drafting Outreach Messages
The platform can generate outreach templates tailored to patient-specific needs, such as chronic disease education, follow-up reminders, or medication instructions. Care teams review and finalize the messages before sending.
5. Reinforcement Learning Personalizes Pathways
A. Learning From Past Interventions
Reinforcement learning models study which interventions worked for similar patients. Over time, the platform refines care pathway recommendations, adjusting thresholds and escalation rules.
This continuous learning makes programs more effective as the population changes.
6. AI-Driven SDoH Mapping and Risk Attribution
A. Integrating Social Determinants of Health
AI evaluates community-level data such as housing stability, transportation access, food security, and caregiver support. These factors often influence outcomes more than clinical indicators alone.
The platform combines these insights with clinical risk to create a comprehensive view of vulnerability.
AI functions as the intelligence layer inside a population health platform. It forecasts risk, interprets complex records, identifies gaps, and guides teams toward timely interventions. When this intelligence is connected to workflows and governance, it becomes a practical system for improving outcomes across entire populations.
Enterprise Use Cases of AI Population Health Management
AI population health platforms help large healthcare organizations reduce utilization, improve chronic disease outcomes, control costs, and manage high-risk cohorts with precision at scale.
The use cases below reflect where AI creates a measurable impact.
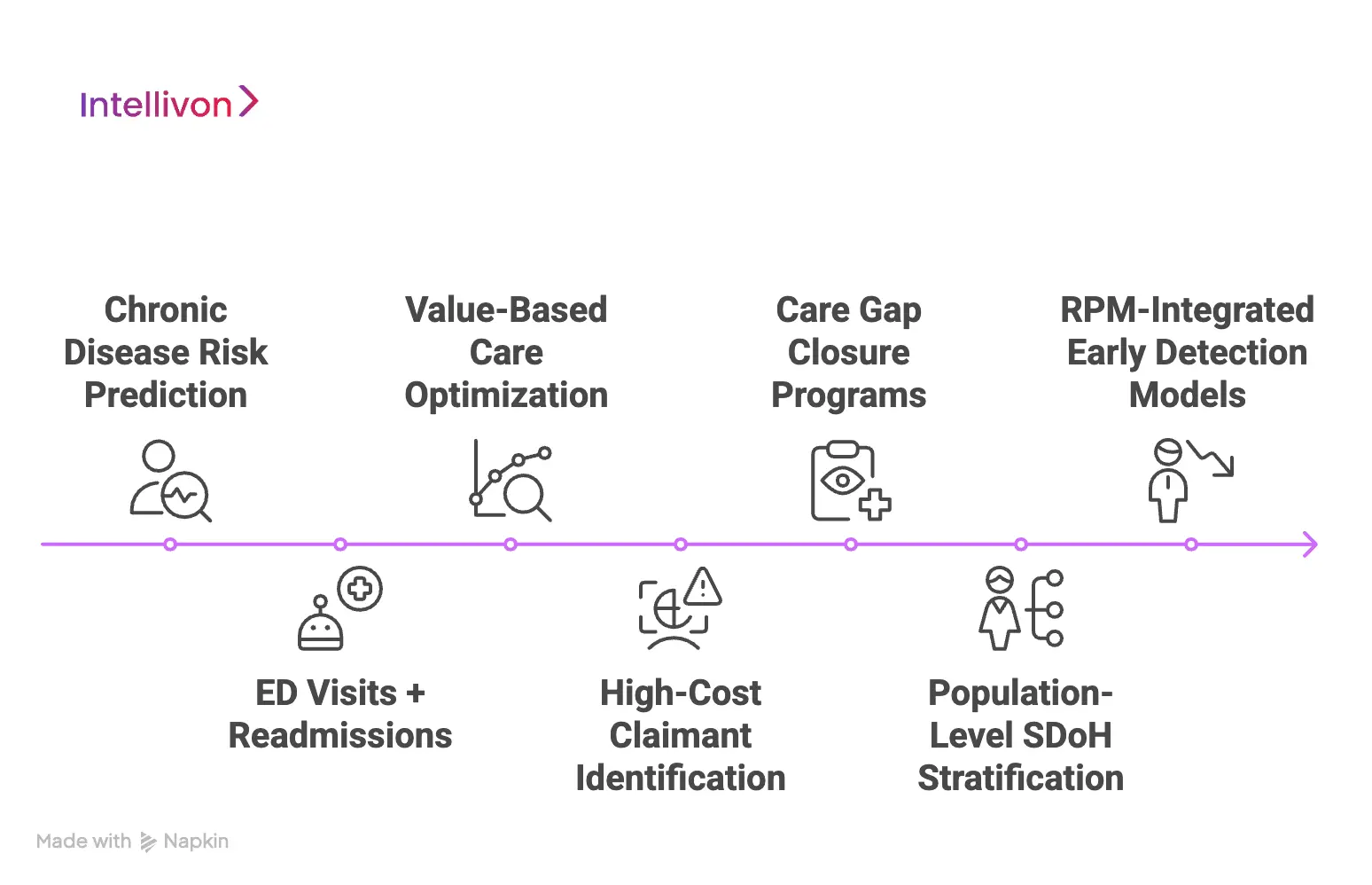
1. Chronic Disease Risk Prediction
AI models identify patients whose conditions are likely to worsen in the near term. For diabetes, COPD, and heart failure, small clinical shifts often predict significant deterioration.
The platform highlights these changes early, giving care teams the chance to adjust medications, escalate monitoring, or schedule timely visits. Enterprises benefit from fewer unplanned admissions, improved disease control, and higher performance on chronic-care quality metrics.
2. ED Visits + Readmissions
Emergency visits and readmissions often reflect gaps in follow-up care, medication adherence, or access barriers. AI pinpoints the individuals most at risk of returning to the hospital, which helps teams focus resources where they are most needed.
By combining risk forecasts with automated pathways, organizations reduce unscheduled utilization and free capacity for higher-acuity cases. This supports value-based contracts and lowers penalties tied to readmissions.
3. Value-Based Care Optimization
Population health platforms give leaders a clear view of cost trends across entire attributed populations. Predictive analytics estimate future spending and highlight members likely to exceed benchmarks.
ACOs use these insights to plan outreach, target chronic disease programs, and support care models that reduce avoidable costs. The result is stronger shared-savings performance and more stability across contract years.
4. High-Cost Claimant Identification
A small percentage of patients often drives a large share of total spending. AI can detect patterns that signal rising financial risk well before it appears in claims.
This helps organizations prepare proactive care plans, arrange specialty follow-ups, or expand support for social needs. Forecasting tools also help financial teams plan budgets and manage variation across service lines.
5. Care Gap Closure Programs
Manual chart review makes it difficult to close gaps for large populations. AI scans structured and unstructured records to identify overdue screenings, missing diagnoses, and preventive opportunities.
Teams receive prioritized lists that focus on the highest-impact actions. This improves compliance with HEDIS, Stars, and other quality programs that influence reimbursement and public ratings.
6. Population-Level SDoH Stratification
AI interprets social factors alongside clinical indicators to understand which groups face higher barriers to care. This includes transportation challenges, food insecurity, financial strain, and environmental risks.
These insights help leaders design community programs, assign case managers more effectively, and align resources with actual needs rather than assumptions.
7. RPM-Integrated Early Detection Models
Remote monitoring devices generate continuous streams of data, but without AI, it is difficult to interpret these signals at scale. AI models detect subtle shifts that indicate clinical decline, especially for heart failure, COPD, and hypertension.
When integrated into population health platforms, these signals trigger timely interventions that reduce acute utilization and stabilize chronic conditions.
These use cases illustrate that AI improves visibility, sharpens prioritization, and strengthens follow-through across large populations. When organizations combine these capabilities with coordinated workflows, they achieve better outcomes at lower operational cost.
Data Sources Required for AI-Driven Population Health Management
AI population health platforms require unified clinical, claims, lab, SDoH, RPM, and community datasets to model risk accurately and guide targeted interventions.
When these inputs converge, the platform moves beyond simple dashboards and becomes a reliable engine for prediction, coordination, and quality improvement.
1. EHR and EMR Clinical Data
Electronic health records anchor the platform. They capture diagnoses, vitals, labs, medications, procedures, and clinician assessments. These elements allow AI models to recognize disease progression, emerging complications, and therapy effectiveness.
Structured data offers consistency, while unstructured notes (processed through NLP) add nuance. Together, they form the clinical spine of population health intelligence.
2. Claims and Utilization Data
Claims provide a full view of care delivered inside and outside the enterprise. They reveal utilization patterns, chronic condition complexity, and cost drivers that may not appear in the EHR alone.
For value-based contracts, claims data is essential. It helps forecast financial risk, identify high-cost claimants, and understand where unnecessary utilization originates.
3. Lab, Pharmacy, and Radiology Data
These data streams strengthen the platform’s predictive accuracy. Lab values track trends that signal worsening conditions. Pharmacy data shows adherence, therapy changes, and drug interactions.
Imaging reports highlight structural or functional changes relevant to chronic disease prediction. By blending these inputs, the system identifies subtle shifts long before they manifest as acute episodes.
4. Social Determinants of Health (SDoH)
SDoH factors often explain variations in outcomes that clinical data alone cannot. Housing stability, access to food, transportation, caregiver support, and financial strain shape how people manage their health.
AI models use SDoH variables to refine predictions and guide interventions that address both medical and non-medical drivers of risk.
5. Wearable and Remote Patient Monitoring (RPM) Streams
RPM devices capture continuous data that traditional clinical systems miss. Heart rate, oxygen saturation, weight fluctuations, and activity levels highlight issues in real time.
When AI interprets these signals, teams gain early warning of deterioration—especially for heart failure, COPD, and hypertension—and can intervene before a hospitalization becomes likely.
6. Patient-Reported Outcomes (PROs)
PROs surface symptoms, functional challenges, and treatment experiences directly from patients. These insights are critical for understanding how individuals respond to therapy between visits.
AI integrates PROs to enhance personalization, detect unmet needs, and identify when additional support may prevent an escalation.
AI population health platforms perform best when they draw from a broad, interconnected data ecosystem. By unifying these sources, enterprises gain a clearer view of risk, a stronger foundation for prediction, and a more effective framework for improving outcomes across diverse populations.
How We Build AI Population Health Management Platforms
Intellivon follows a structured, eight-step framework to design, build, and deploy AI population health platforms that align with clinical workflows, contracts, and enterprise governance.
Building an AI population health platform is not only a technical exercise. It is a strategic decision that affects contracts, clinical operations, and long-term cost structure. Our approach focuses on aligning architecture, AI models, and workflows with the realities of large health systems and payers.
Below is the step-by-step framework we use when partnering with enterprise clients.
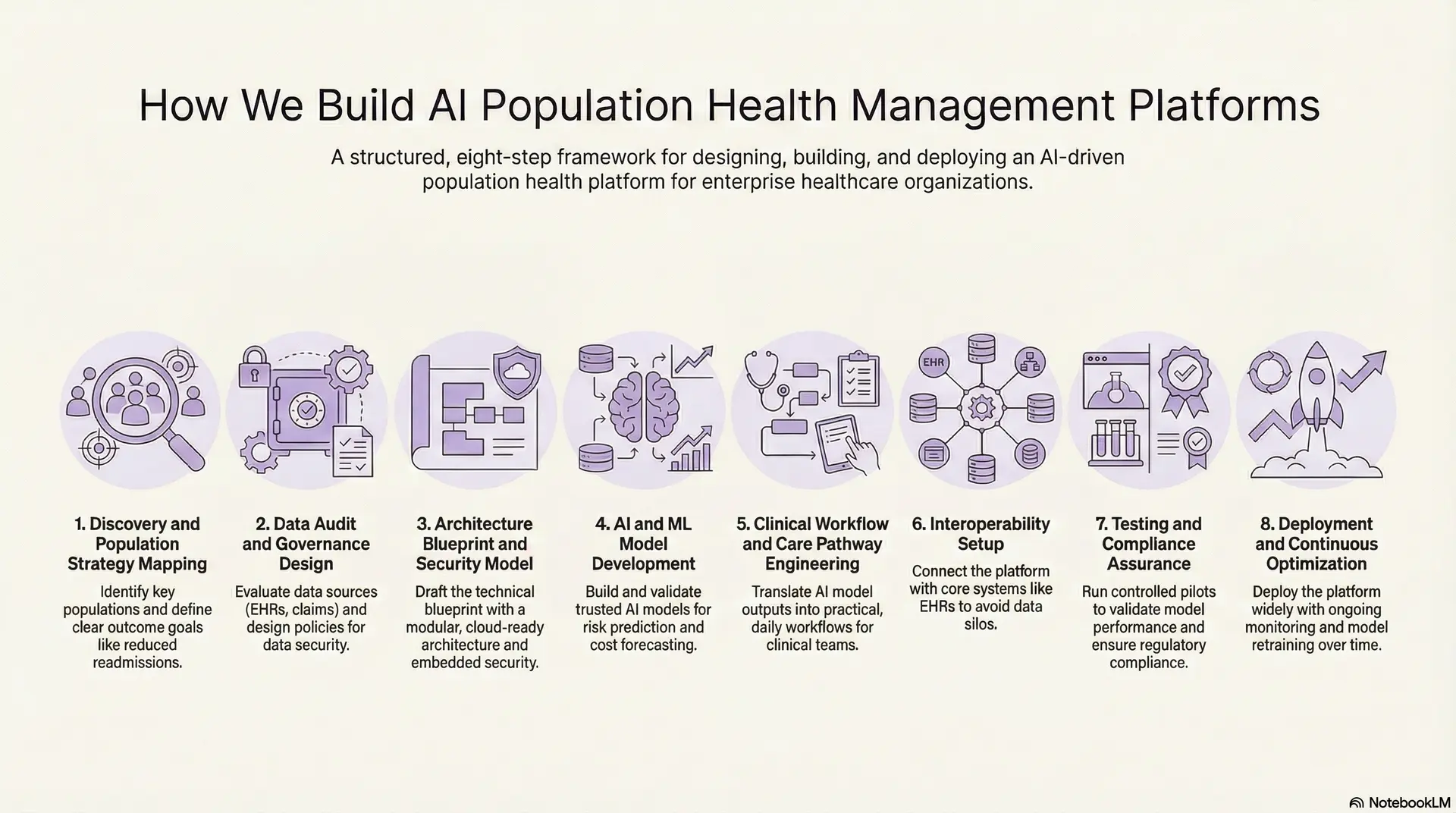
1. Discovery and Population Strategy Mapping
We begin by understanding which populations matter most for your organization. This includes value-based contracts, high-cost cohorts, chronic disease programs, and specific service lines that carry the most financial or clinical risk.
Together, we define clear outcome goals, such as reduced readmissions, lower ER utilization, or improved quality scores. These objectives guide every design decision that follows.
2. Data Audit and Governance Design
Next, we evaluate your data estate. We review EHR systems, claims platforms, lab and pharmacy feeds, RPM infrastructure, and existing analytics tools. The goal is to identify what is usable today, what needs cleaning, and where the gaps are.
In parallel, we design governance policies around PHI handling, access control, retention, and auditability. This ensures that the platform supports regulatory expectations from day one.
3. Architecture Blueprint and Security Model
With strategy and data clarified, we draft the technical blueprint. This covers data ingestion layers, storage choices, AI and analytics services, and user-facing applications. We typically recommend a modular, cloud-ready architecture that can grow with your organization.
Security is embedded at each layer. We define encryption standards, identity and access control patterns, logging, and incident response processes that align with HIPAA, GDPR, and regional regulations.
4. AI and ML Model Development
We then build and calibrate the core intelligence of the platform. This includes models for readmission risk, disease progression, cost prediction, and SDoH-informed vulnerability.
Our teams use historical data to train, validate, and stress test each model. We pay careful attention to bias, explainability, and stability over time, so clinical and business leaders can trust the outputs.
5. Clinical Workflow and Care Pathway Engineering
AI only delivers value when it fits daily practice. We work with clinicians, case managers, and operations teams to translate model outputs into concrete workflows and care pathways.
This may involve risk-based discharge protocols, tiered care management, telehealth outreach rules, or targeted community referrals. Every pathway is designed to be practical within existing staffing and systems.
6. Interoperability Setup
To avoid creating yet another silo, we connect the platform with your core systems. This includes FHIR and HL7 interfaces for EHRs, secure APIs for claims and lab systems, and streaming pipelines for RPM data.
Our aim is to make the platform feel native to your ecosystem. Users should not have to fight with multiple logins or duplicate data entry to benefit from the new capabilities.
7. Testing and Compliance Assurance
Before scaling, we run controlled pilots. We validate model performance in real workflows, measure impact on key metrics, and collect feedback from frontline users.
We also perform rigorous security, compliance, and reliability testing. This phase confirms that the platform can meet both regulatory requirements and internal risk standards.
8. Deployment and Continuous Optimization
Once validated, the platform moves into broad deployment. We establish monitoring for model performance, system uptime, and data quality, supported by a structured MLOps process.
Over time, we retrain models, refine thresholds, and adjust workflows as populations and contracts evolve. The platform becomes a living system that adapts with your enterprise, rather than a static project that ages quickly.
This framework ensures that AI population health platforms are built with strategy, governance, and clinical reality in mind. By moving carefully from discovery to continuous optimization, we help organizations adopt AI in a way that is sustainable, compliant, and directly tied to measurable outcomes.
Real Examples of Population Health Management Platforms
Leading population health platforms such as Epic Healthy Planet, Cerner HealtheIntent, Innovaccer, Arcadia, and AthenaPopulation Health demonstrate how AI, interoperability, and workflow automation drive improved outcomes at enterprise scale.
These examples help illustrate what strong execution looks like and how different vendors approach interoperability, predictive modeling, and large-scale coordination.
1. Epic Healthy Planet
Epic Healthy Planet is a population health suite embedded within the broader Epic ecosystem. It consolidates clinical data, claims feeds, quality metrics, and cohort definitions into one operational layer. Large systems use it to manage risk-based contracts, track gaps, and support care teams across ambulatory and inpatient settings.
The platform works by offering registries, risk stratification tools, and care management workflows that connect directly to the EHR. This eliminates the friction of switching systems and allows clinicians to take action from within their daily workspace.
Healthy Planet incorporates machine learning for risk prediction, care gap detection, and quality performance monitoring. AI enhances its ability to anticipate which patients need attention, helping organizations improve outcomes while supporting value-based agreements.
2. Cerner HealtheIntent
HealtheIntent operates as a cloud-based platform that aggregates data across disparate EHRs, claims systems, and community organizations. It focuses on building longitudinal records that travel with the patient and reflect events across multiple care environments.
Its architecture allows health systems to standardize data, define populations, and build analytics programs without depending on a single EHR vendor. Care teams use HealtheIntent for cohort creation, care plan management, and quality tracking across large networks.
AI capabilities appear in predictive models that estimate readmission risk, rising-cost members, and chronic disease progression. The platform also supports automated tasking, making it easier for care teams to respond to high-priority alerts.
3. Innovaccer Population Health Cloud
Innovaccer’s platform is built around a strong data transformation and unification layer. It ingests EHR, claims, lab, SDoH, and third-party feeds to create a master record that supports both analytics and operational workflows.
The platform functions as a flexible layer that care managers, analysts, and clinical leaders can adapt to contract-specific needs. It includes dashboards, referral tools, care pathways, and quality measure automation.
AI powers several features, such as identifying undocumented conditions, surfacing care gaps, predicting high-utilization members, and guiding intervention selection. Its AI also assists physicians with chart summaries and coding integrity, which improves the accuracy of risk scores across populations.
4. Arcadia Analytics
Arcadia focuses heavily on data engineering and value-based care performance. The platform integrates EHR, claims, and SDoH data into curated data models designed for high-scale analytics and ACO reporting.
Its workflows help teams deploy care management programs, monitor quality measures, and engage specific cohorts through targeted interventions. Arcadia is widely used by systems with complex payer contracts and large attributed populations.
AI supports forecasting of contract performance, detection of care gaps, attribution risk scoring, and identification of members likely to benefit from immediate outreach. This helps organizations direct resources more effectively.
5. AthenaPopulation Health
AthenaPopulation Health extends the capabilities of athenahealth’s network by linking clinical, claims, and operational data across practices and partner systems. It is often adopted by multi-site ambulatory networks and physician groups.
The platform assists with patient segmentation, referral coordination, care management, and monitoring performance across value-based arrangements. Its design emphasizes usability and minimal disruption to clinical workflows.
AI models in AthenaPopulation identify rising-risk patients, streamline quality reporting, and recommend actions to close gaps. These capabilities allow smaller and mid-size organizations to operate with insights typically seen in larger systems.
These platforms show how population health technology is evolving into a unified engine for data, prediction, and coordinated action. Each example demonstrates a different path to execution, but all share a common theme: AI strengthens the ability to manage risk, support clinicians, and improve outcomes across entire populations.
Conclusion
Population health has moved from a reporting exercise to a strategic advantage. Organizations that unify their data, deploy predictive intelligence, and activate coordinated workflows see clearer patterns, faster interventions, and stronger performance across value-based contracts. These platforms become part of the enterprise operating system, guiding decisions that shape quality, cost, and long-term sustainability.
AI amplifies this impact. It identifies risk earlier, highlights the drivers behind that risk, and supports teams with actionable steps. When combined with strong governance, interoperability, and workflow design, AI-driven platforms help large health systems operate with greater accuracy and efficiency.
The opportunity now is to build systems that adapt as populations evolve. With the right foundation, enterprises can improve outcomes, stabilize margins, and design care models that scale with future needs.
Build an AI Population Health Management Platform With Intellivon
At Intellivon, we help large healthcare organizations move beyond fragmented data and reactive care models. Our teams design population health platforms that unify clinical, claims, SDoH, RPM, and community data into a single decision layer. We engineer systems that surface risk early, guide coordinated interventions, and support value-based performance at scale.
Each platform is built with enterprise realities in mind. Your teams get a secure, compliant, and interoperable foundation that integrates seamlessly with EHRs, claims systems, lab networks, and remote monitoring infrastructure. AI models are trained on real-world patterns, validated with clinical stakeholders, and deployed through workflows that reduce burden and do not add to it.
Why Partner With Intellivon?
- Compliance-First Architecture: HIPAA, GDPR, and emerging AI governance frameworks built into every layer.
- Interoperability You Can Trust: Native support for FHIR, HL7, X12, DICOM, and secure API frameworks for multi-system integration.
- Healthcare-Tuned AI Models: Predictive engines for readmissions, chronic disease progression, cost forecasting, and SDoH risk mapping.
- Enterprise Reliability: High-availability infrastructure, MLOps pipelines, and continuous monitoring to ensure stability at scale.
- Deployment Without Disruption: We integrate into existing workflows and minimize operational downtime during rollout.
Population health success requires precision, coordination, and systems that adapt as your populations change. Intellivon brings the engineering, clinical insight, and enterprise experience to make that transformation real.
Ready to build your AI-enabled population health management platform? Let’s design a system that delivers measurable outcomes and future-ready care at scale.
FAQs
Q1. What is an AI population health management platform?
A1. It is a system that unifies clinical, claims, SDoH, and monitoring data to identify risk, guide interventions, and support large-scale care coordination. It helps organizations manage populations proactively instead of reactively.
Q2. How does AI improve population health outcomes for hospitals?
A2. AI predicts deterioration, flags care gaps, and recommends targeted actions. Hospitals use these insights to prevent avoidable admissions, improve chronic disease control, and strengthen value-based performance.
Q3. What data sources are required for population health analytics?
A3. EHR data, claims files, labs, pharmacy data, imaging reports, RPM devices, SDoH indicators, and patient-reported outcomes. Together, they create a full longitudinal view for accurate prediction.
Q4. How much does it cost to build an AI population health platform?
A4. Enterprise builds typically range from USD 140,000 to 291,000, depending on data complexity, integrations, predictive models, and workflow automation. Annual maintenance adds 15–25%.
Q5. How do you ensure compliance and data security in PHM platforms?
A5. By implementing PHI encryption, identity controls, access policies, audit logs, and continuous monitoring. Compliance follows HIPAA, GDPR, and emerging AI governance standards.