Healthcare leaders face a hidden problem that hospitals and clinics don’t always choose the same treatments for similar patients. This can mean some people get care they don’t need, or miss out on what they do. At the same time, doctors and nurses can get confused by mixed messages, and older ways of working can’t keep up with all the new information available. Because of this, many hospitals are trying to find better ways to help their staff make the right choices.
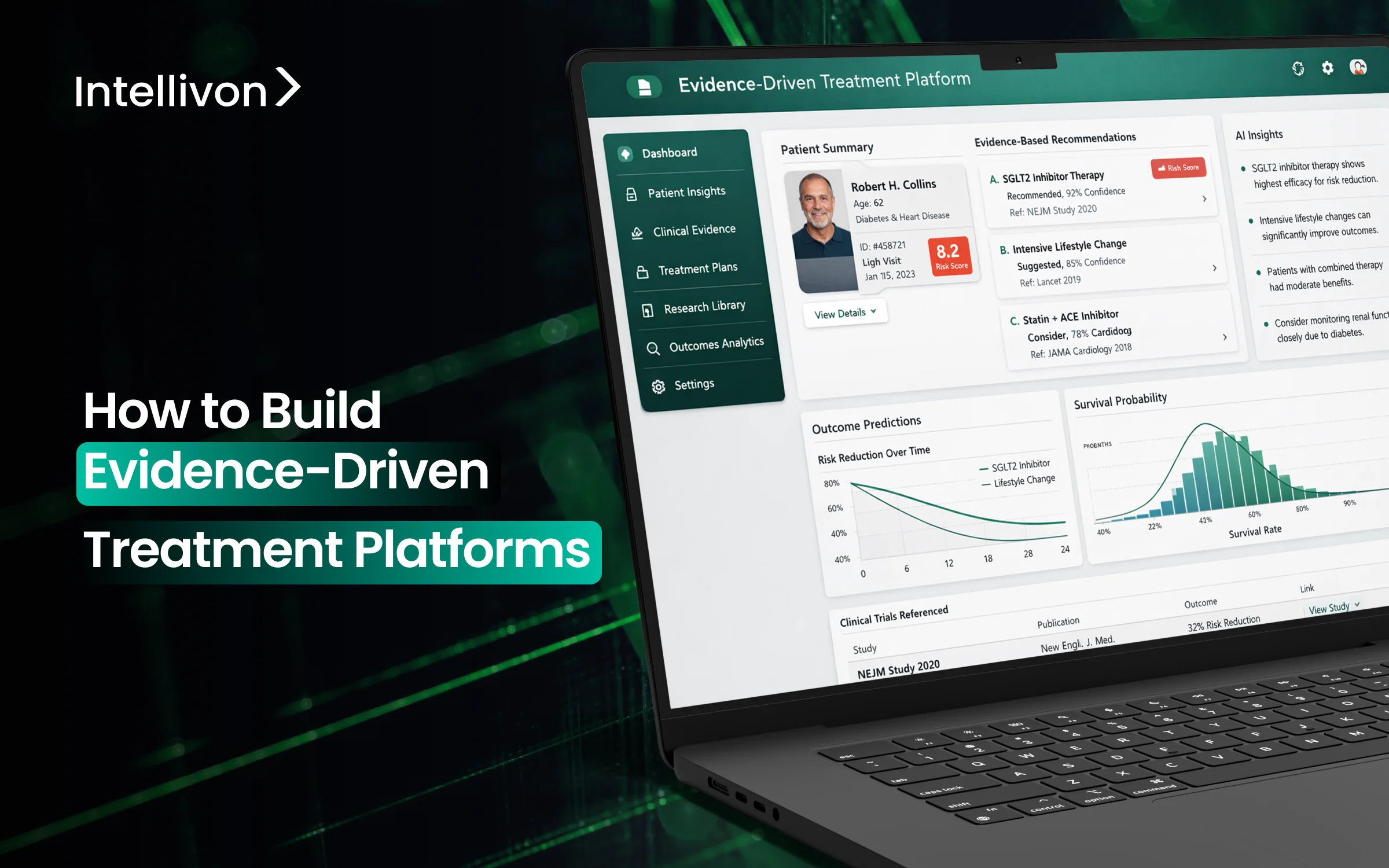
New evidence-based treatment platforms use the latest medical knowledge to give real-time advice for each patient. This helps doctors and nurses follow the best steps for care and decide what to do more quickly. At the same time, these hospitals can also see how care is given and find ways to make it better.
At Intellivon, we make these platforms from the ground up so hospitals see real improvements. We keep medical advice current, connect with hospital systems, use smart tools to help staff focus on what matters most, and track results. In this blog, we draw from this experience to show you how we build these platforms for healthcare enterprises.
Why Healthcare Systems Are Shifting Toward Evidence-Driven Care
Healthcare organizations are shifting to evidence-driven care to improve outcomes and control costs as fee-for-service models offer limited visibility into treatment effectiveness.
Evidence-driven treatment platforms turn real-world evidence and AI insights into patient-specific guidance by analyzing EHR data, claims, and patient inputs.
As a result, clinicians make more consistent decisions while leaders gain clearer visibility into care quality and financial performance. The global real-world evidence (RWE) solutions market is expected to grow from USD 52.4 billion in 2025 to USD 136.2 billion by 2035, reflecting a steady compound annual growth rate of 10.2% during the forecast period.
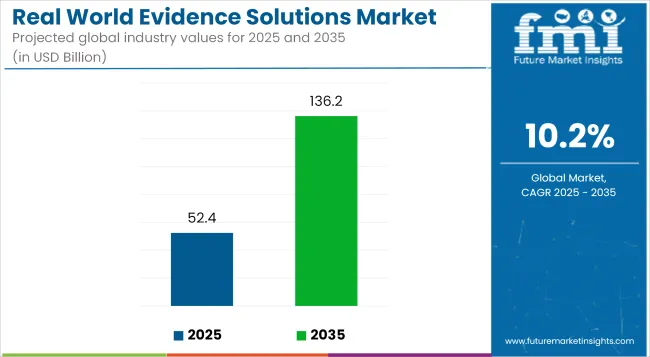
Key Growth Drivers:
- Rising chronic disease rates and aging populations are increasing demand for scalable, effective interventions beyond traditional clinical trials.
- Real-world evidence provides the practical effectiveness data needed to support more informed treatment decisions.
- Value-based care models now tie reimbursement directly to outcomes, which is accelerating platform adoption among payers and providers.
- Advances in AI and machine learning enable predictive modeling and patient stratification at scale.
Healthcare systems are adopting evidence-driven care to reduce variation, improve measurable outcomes, manage multi-system complexity, and support faster, data-backed clinical decisions.
1. Rising Clinical Variation Risk
Across many health systems, patients with similar conditions still receive different treatments. This variation increases the risk of avoidable complications and inconsistent outcomes.
In addition, it makes quality performance harder to predict and manage. Evidence-driven treatment platforms help standardize decisions using validated clinical guidance, so care teams follow more consistent pathways.
2. Quality and Outcome Accountability
Payment models are steadily moving toward outcome-based reimbursement. Therefore, providers must show clear proof that care decisions lead to measurable improvements. Manual audits and retrospective reviews no longer provide enough visibility.
Evidence-driven platforms give leaders real-time insight into guideline adherence, treatment patterns, and quality performance across the organization.
3. Multi-EHR and Multi-Site Complexity
Many enterprises operate across multiple EHR systems, facilities, and specialty groups. However, clinical guidance often remains fragmented across these environments.
This creates gaps in care consistency and reporting. Evidence-driven treatment platforms unify decision support across systems, which helps organizations maintain alignment even in complex, multi-site settings.
4. Demand for Real-Time Clinical Intelligence
Care teams work in fast-moving environments where delays can affect outcomes. Static protocols and delayed reports cannot support timely decisions.
Evidence-driven platforms deliver patient-specific insights at the point of care. As a result, clinicians can act faster while leaders maintain better visibility into how care is delivered.
As care delivery grows more complex, evidence-driven treatment platforms give organizations the clarity and control needed to improve outcomes and manage risk. Those who act early will be better positioned to deliver consistent, high-quality care at scale.
What Is an Evidence-Driven Treatment Platform?
An evidence-driven treatment platform uses clinical data, medical evidence, and intelligent rules to guide consistent, patient-specific care decisions in real time.
An evidence-driven treatment platform is a clinical decision system that turns trusted medical evidence into real-time treatment guidance. It brings together clinical guidelines, patient data, and analytics to help care teams choose the most appropriate next step. Instead of relying on manual interpretation or static protocols, clinicians receive patient-specific recommendations directly within their workflow.
As a result, treatment decisions become more consistent and easier to track. In addition, leaders gain visibility into how care is delivered, which supports better quality management and more informed operational planning.
Evidence-Driven Platform vs Traditional Clinical Decision Support
Many healthcare organizations already use clinical decision support tools. However, most traditional CDSS solutions were designed for basic alerts, not for continuous, enterprise-wide guidance.
As care environments became more data-driven, these tools started to show clear limitations. Evidence-driven treatment platforms take a broader and more connected approach, which helps organizations manage care quality more effectively.
| Area | Traditional Clinical Decision Support | Evidence-Driven Treatment Platform |
| Decision Logic | Static, rule-based alerts | Dynamic, evidence-informed guidance |
| Workflow Integration | Often interruptive and siloed | Embedded within clinical workflows |
| Evidence Updates | Manual and infrequent | Governed and continuously refreshed |
| Data Usage | Limited patient context | Deep, longitudinal patient view |
| Enterprise Visibility | Department-level insights | System-wide performance visibility |
| Scalability | Difficult across multiple sites | Built for multi-site consistency |
In short, traditional CDSS tools support isolated decisions, while evidence-driven treatment platforms enable coordinated, measurable care improvement across the enterprise.
Core Architecture of an Evidence-Driven Treatment Platform
The architecture of an evidence-driven treatment platform combines governed clinical knowledge, real-time data integration, intelligent decision logic, and embedded workflow support to enable consistent care.
A strong architecture is what separates pilot tools from enterprise-ready treatment platforms. Healthcare organizations need systems that deliver accurate guidance while fitting naturally into clinical workflows.
Therefore, each layer must work together to ensure reliability, traceability, and real-time responsiveness. When designed correctly, the platform supports both frontline clinicians and operational leaders without creating additional complexity.
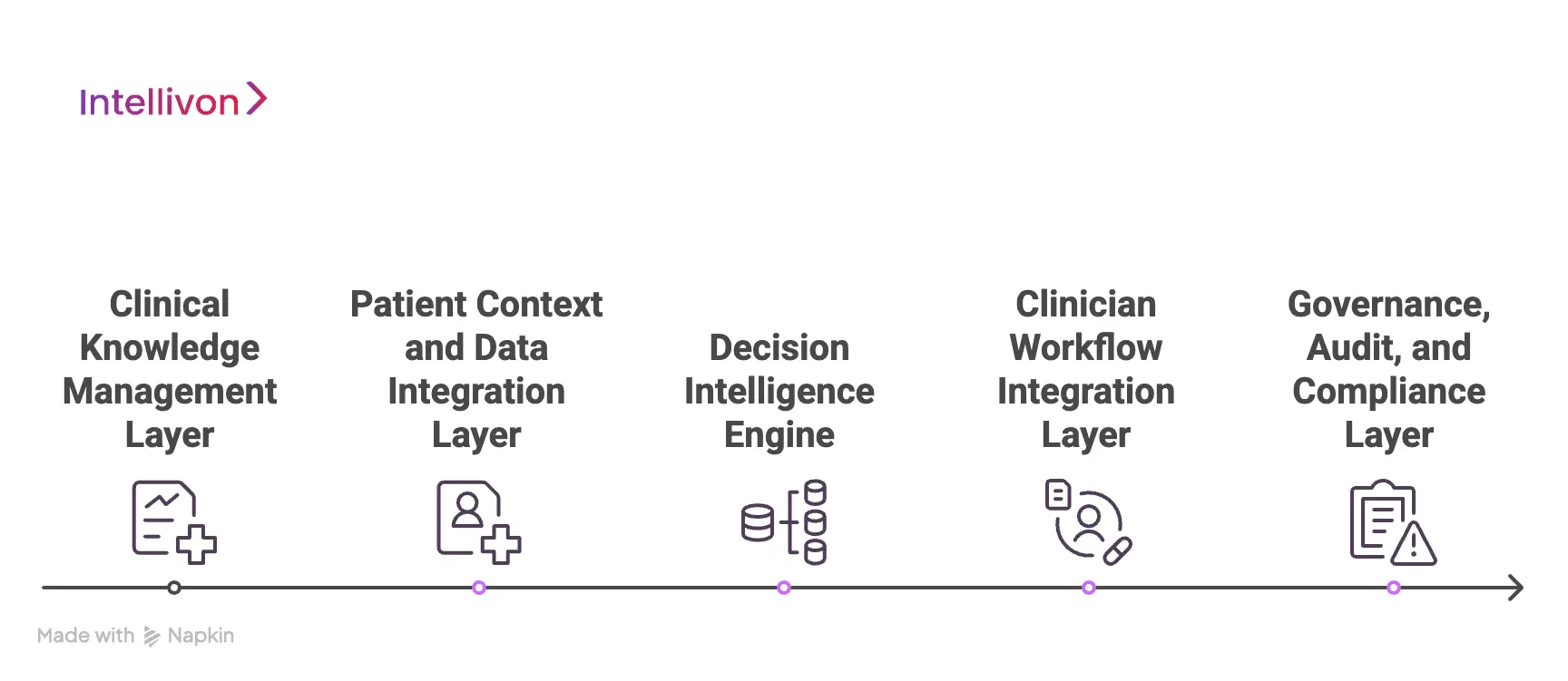
1. Clinical Knowledge Management Layer
This layer manages the clinical evidence that powers the platform. It ingests guidelines, research updates, and care pathways from trusted sources. In addition, governance workflows ensure that medical teams review and approve changes before release.
Version control keeps a clear history of updates. As a result, organizations maintain confidence that recommendations stay current and defensible.
2. Patient Context and Data Integration Layer
This layer connects the platform to real patient data. It pulls structured and unstructured inputs from EHR systems, claims platforms, and other clinical sources. Standards such as FHIR and HL7 help maintain interoperability.
In addition, the system builds a longitudinal patient view that updates in near real time. Therefore, treatment guidance reflects the latest clinical context.
3. Decision Intelligence Engine
The decision engine turns data and evidence into actionable guidance. It applies clinical rules, risk models, and pathway logic to evaluate each patient scenario.
In many environments, a hybrid approach combines deterministic rules with predictive analytics. As a result, clinicians receive recommendations that are both explainable and clinically relevant.
4. Clinician Workflow Integration Layer
Even the best logic fails if it disrupts care delivery. This layer embeds recommendations directly into existing workflows inside the EHR or care management tools. It also manages alert timing and prioritization to reduce fatigue.
In addition, mobile and point-of-care access ensures teams can act quickly. Therefore, adoption improves across departments.
5. Governance, Audit, and Compliance Layer
Enterprise environments require strong oversight. This layer provides full traceability of decisions, evidence versions, and user actions. Audit logs support regulatory reviews and internal quality programs.
Policy controls also ensure the platform aligns with privacy and compliance requirements. As a result, organizations can scale with confidence while maintaining proper clinical and regulatory control.
When these layers work together, the platform delivers reliable, real-time guidance that supports consistent care and stronger enterprise oversight.
Data Sources That Power Evidence-Driven Treatment Decisions
Evidence-driven treatment platforms rely on multiple data sources, including EHRs, claims, clinical guidelines, real-world evidence, and patient-generated data to support accurate decisions.
Strong treatment platforms depend on the quality and breadth of the data behind them. No single source provides a complete clinical picture. Therefore, organizations must combine multiple inputs to generate reliable, patient-specific guidance. When these sources work together, care teams gain a clearer and more actionable view of each patient.
1. Electronic Health Record (EHR) Data
EHR data forms the clinical foundation of most treatment platforms. It includes diagnoses, medications, lab results, vitals, and care history.
Because this data updates frequently, it helps ensure recommendations reflect the patient’s current condition. In addition, structured EHR integration supports real-time decision support within clinician workflows.
2. Claims and Utilization Data
Claims data adds important financial and utilization context. It highlights prior services, care patterns, and cost drivers that may not appear in the clinical record alone.
Therefore, organizations can identify unnecessary utilization and variation more effectively. This layer is especially valuable for population health and value-based care programs.
3. Clinical Guidelines and Medical Literature
Trusted medical guidelines provide the evidence backbone for treatment recommendations. Platforms ingest and normalize guidance from professional bodies and peer-reviewed research.
Governance workflows then validate and approve updates. As a result, clinicians can rely on recommendations that reflect current medical standards.
4. Real-World Evidence and Outcomes Data
Real-world evidence shows how treatments perform outside controlled trials. It includes registry data, longitudinal outcomes, and observational studies.
This information helps refine pathways based on actual patient response. In addition, it supports the continuous improvement of clinical decision logic.
5. Patient-Generated and Remote Monitoring Data
Data from home monitoring tools and patient-reported inputs add valuable context between visits. It can include symptom logs, glucose readings, blood pressure trends, or recovery feedback.
Therefore, care teams gain earlier visibility into patient status changes and potential risks.
6. Wearables and Digital Biomarkers
Wearables provide continuous streams of physiological data such as activity levels, heart rate, and sleep patterns. When integrated properly, these signals enhance risk detection and early intervention.
However, organizations must apply filtering and validation to ensure clinical relevance.
When unified and governed correctly, these data sources transform treatment platforms from static tools into continuously learning clinical guidance systems.
Role of AI and Predictive Analytics in Evidence-Driven Treatment
AI and predictive analytics enhance evidence-driven treatment platforms by identifying risk earlier, prioritizing patients, and delivering more precise, data-informed clinical guidance.
AI strengthens treatment platforms by turning large volumes of clinical data into timely, practical insight. However, value appears only when AI supports clinical judgment rather than replacing it.
Therefore, successful platforms combine predictive intelligence with governed medical evidence. This balanced approach improves decision quality while preserving clinician trust.
1. Risk Prediction and Early Intervention Models
Predictive models analyze historical and real-time data to identify patients who may deteriorate or require intervention. For example, risk scores can flag early signs of sepsis, readmission risk, or care gaps.
As a result, care teams can act sooner instead of reacting after complications appear. Early visibility also helps organizations reduce avoidable utilization and improve outcomes.
2. Hybrid Rules and AI Decision Frameworks
Pure AI models can lack transparency, while rule-only systems may miss subtle risk patterns. Therefore, many enterprises adopt a hybrid approach that combines deterministic clinical rules with machine learning models.
Rules provide clinical guardrails, while AI adds pattern recognition at scale. This structure helps organizations maintain both accuracy and explainability in treatment decisions.
3. Model Explainability and Clinical Trust
Clinicians are more likely to adopt AI when they understand why a recommendation appears. Therefore, platforms must present clear reasoning, supporting data points, and confidence levels.
Explainability tools translate complex model output into clinician-friendly language. As a result, trust improves, and override rates tend to decline over time.
4. Safety Guardrails for Clinical AI
AI in clinical settings requires strict oversight. Leading platforms implement governance controls such as model monitoring, bias checks, and performance thresholds. In addition, human review workflows remain in place for high-risk decisions.
These safeguards help organizations innovate responsibly while protecting patient safety and regulatory alignment.
5. Where Deterministic Rules Still Matter
Not every decision should rely on predictive models. Certain clinical scenarios, such as medication safety checks or protocol enforcement, require fixed rules.
Therefore, mature treatment platforms maintain strong rule engines alongside AI capabilities. This ensures consistent baseline safety while still enabling advanced, data-driven insight where it adds real value.
When applied with the right controls, AI and predictive analytics turn evidence-driven treatment platforms into proactive decision systems that improve outcomes while maintaining clinical trust and oversight.
Interoperability Requirements for Enterprise Deployment
Enterprise treatment platforms require strong interoperability across EHRs, HIEs, and clinical systems to deliver consistent, real-time guidance without disrupting workflows.
Interoperability determines whether an evidence-driven treatment platform can operate reliably across complex healthcare environments. Most enterprises manage multiple systems, data formats, and care settings.
Therefore, the platform must exchange data smoothly while preserving clinical context and accuracy. When interoperability is designed correctly, organizations avoid fragmentation and maintain consistent decision support across the network.
1. FHIR and HL7 Integration Strategy
Standards such as FHIR and HL7 form the backbone of modern healthcare data exchange. They allow treatment platforms to pull structured clinical data from EHR systems in near real time.
In addition, standards-based integration reduces custom interface work and speeds deployment. This approach also helps organizations future-proof their architecture as interoperability requirements evolve.
2. Multi-EHR Environment Support
Many health systems operate more than one EHR across hospitals and specialty groups. However, inconsistent data models can create gaps in decision support.
Enterprise platforms must normalize inputs from different systems into a unified patient view. As a result, clinicians receive consistent recommendations regardless of where care occurs.
3. Health Information Exchange Connectivity
Health Information Exchanges extend visibility beyond a single organization. By connecting to regional or national HIE networks, treatment platforms access external encounter history, medications, and care events.
Therefore, decision logic reflects a more complete patient picture. This is especially important for transitions of care and population health programs.
4. Data Normalization and Semantic Mapping
Raw clinical data often arrives in different formats and coding structures. Without normalization, decision logic may produce unreliable results.
Platforms must map data to common clinical vocabularies such as SNOMED, LOINC, and ICD. In addition, semantic alignment improves reporting accuracy and cross-site comparability.
5. API and Microservices Strategy
Modern enterprises prefer modular, API-driven architectures. A microservices approach allows treatment platforms to integrate with surrounding systems without tight coupling.
It also supports phased rollout and easier upgrades over time. Therefore, organizations gain flexibility while maintaining strong performance and scalability.
When interoperability is engineered from the start, treatment platforms deliver consistent guidance across systems, sites, and care settings without adding operational friction.
Step-by-Step Process to Build an Evidence-Driven Treatment Platform
Building an evidence-driven treatment platform requires clear clinical priorities, governed evidence workflows, deep EHR integration, clinician-first design, and continuous measurement to deliver ROI.
A treatment platform succeeds when it fits enterprise priorities and clinical reality at the same time. Therefore, the build approach must balance governance, integration, usability, and measurable outcomes.
Intellivon follows a delivery model that keeps clinical safety and enterprise ROI aligned from day one. Each step below shows what matters and why.
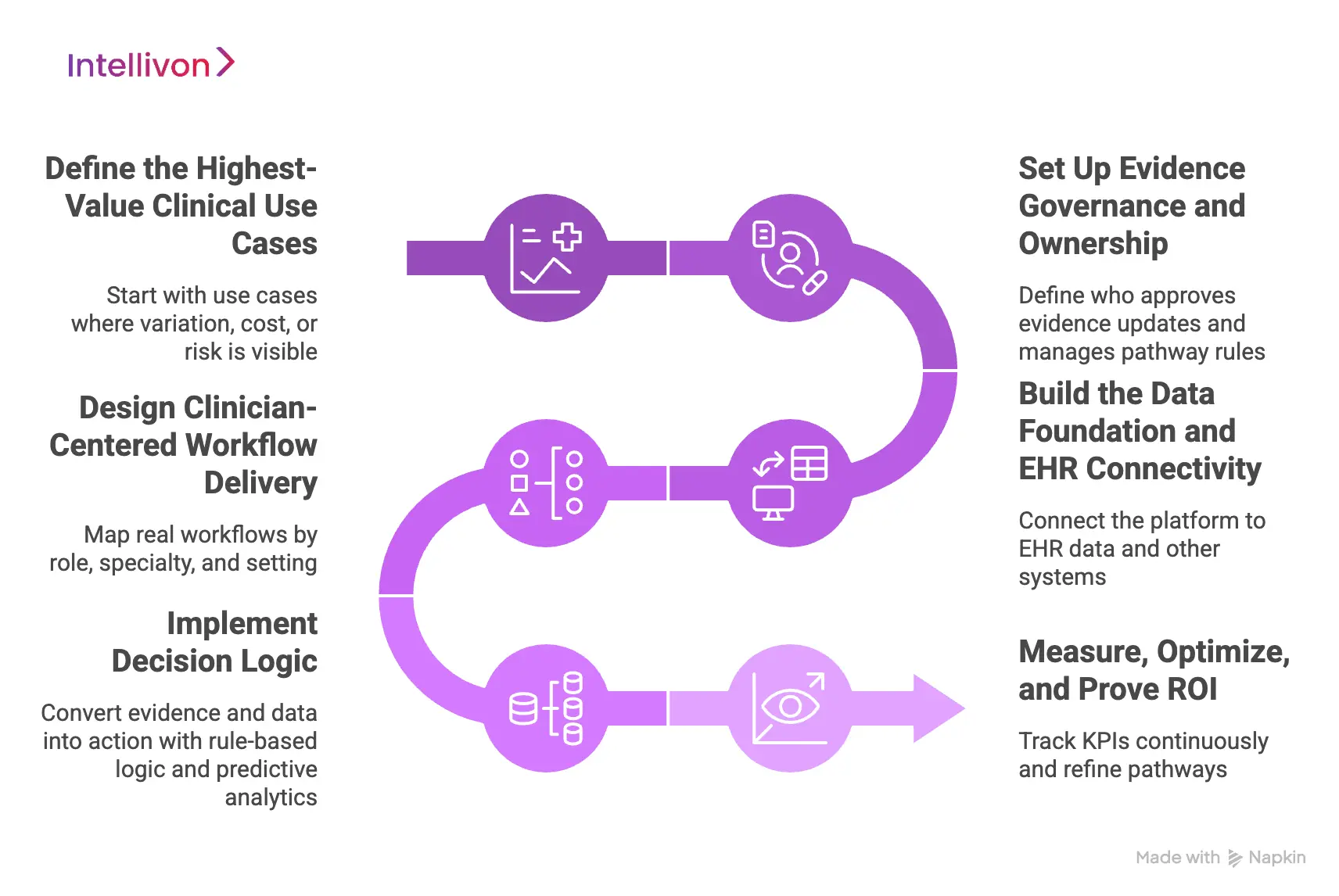
Step 1: Define the Highest-Value Clinical Use Cases
Start with use cases where variation, cost, or risk is already visible. Focus on pathways that affect outcomes and utilization. In addition, choose scenarios where decision support can change actions, not just inform them.
Common starting points include sepsis, heart failure, oncology protocols, and discharge planning. This prioritization sets the ROI baseline early.
Step 2: Set Up Evidence Governance and Ownership
Strong platforms need clinical ownership, not just IT sponsorship. Therefore, define who approves evidence updates, who manages pathway rules, and who signs off on changes.
Intellivon implements evidence workflows with review queues, version control, and release governance. This creates defensible guidance that stays current without operational chaos.
Step 3: Build the Data Foundation and EHR Connectivity
Next, connect the platform to the systems that hold patient truth. That includes EHR data, orders, labs, medications, and care plans. In addition, many enterprises add claims and utilization feeds to capture cost signals.
Intellivon designs standards-based integration using FHIR and HL7 where possible, then normalizes data for consistent decision logic across sites.
Step 4: Design Clinician-Centered Workflow Delivery
Guidance must appear where clinicians already work. Otherwise, adoption drops fast. Therefore, Intellivon maps real workflows by role, specialty, and setting before designing delivery.
The platform then supports context-aware recommendations, clear reasoning, and smart timing. This reduces alert fatigue and keeps decisions moving during busy clinical shifts.
Step 5: Implement Decision Logic
Then, convert evidence and data into action. Rule-based logic enforces safety and pathway consistency. Predictive analytics helps prioritize risk and identify patients who need attention earlier.
Intellivon builds hybrid decision engines with explainability and clinical guardrails. As a result, recommendations remain both useful and trusted.
Step 6: Measure, Optimize, and Prove ROI
ROI comes from measurable operational and clinical shifts, not from the platform launch itself. Therefore, define KPIs upfront and track them continuously. Intellivon embeds analytics to measure adherence, variation reduction, time-to-treatment, avoidable utilization, and cost impact.
In addition, feedback loops refine pathways, improve model performance, and strengthen adoption over time.
When built with governance, workflow fit, and measurable outcomes in mind, evidence-driven treatment platforms move from clinical support to enterprise performance infrastructure, with ROI you can prove.
Cost To Build An Evidence-Driven Treatment Platform
At Intellivon, evidence-driven treatment platforms are engineered as a regulated clinical decision infrastructure, not alert tools layered onto existing systems. The focus stays on building platforms that operate reliably across providers, care settings, and evolving regulatory requirements. Every design decision accounts for clinical governance, interoperability depth, and long-term risk exposure from the start.
When budget pressure exists, scope can be adjusted carefully. However, evidence integrity, workflow safety, auditability, and data controls are never compromised. Therefore, enterprises avoid costly rework after go-live. Predictability improves, and long-term ROI remains protected.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery and Clinical Alignment | Use case prioritization, pathway scoping, regulatory review, stakeholder workshops | $10,000 – $16,000 |
| Evidence and Knowledge Architecture | Guideline ingestion model, version control design, governance workflows | $12,000 – $20,000 |
| Platform Architecture and Data Design | Decision engine structure, data models, interoperability planning | $14,000 – $24,000 |
| Backend and Enterprise Integrations | EHRs, HIEs, claims systems, terminology services, APIs | $20,000 – $38,000 |
| Clinician Workflow and UI Design | Role-based interfaces, in-workflow guidance, usability optimization | $12,000 – $22,000 |
| Decision Intelligence and Risk Models | Rules engine, predictive models, explainability layers | $14,000 – $26,000 |
| Security, Privacy, and Compliance Controls | PHI protection, access controls, audit logging, policy enforcement | $11,000 – $20,000 |
| Testing and Clinical Validation | Functional testing, model validation, workflow verification | $8,000 – $14,000 |
| Deployment and Performance Readiness | Cloud or hybrid rollout, monitoring setup, performance tuning | $9,000 – $16,000 |
Total initial investment: $110,000 – $220,000
Ongoing maintenance and optimization: ~15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped treatment platform programs can face pressure when indirect cost drivers are overlooked. Planning early protects budgets, timelines, and clinical confidence.
- Integration complexity grows as additional EHRs and data feeds are connected
- Evidence governance requires ongoing clinical review and pathway updates
- Model monitoring and recalibration demand continuous oversight
- Infrastructure costs increase as data volume and analytics usage expand
- Change management includes clinician onboarding and workflow training
- Continuous compliance monitoring becomes essential as regulations evolve
Best Practices to Avoid Budget Overruns
Based on Intellivon’s experience delivering enterprise clinical intelligence platforms, these practices consistently lead to controlled costs and predictable outcomes.
- Start with clearly defined clinical use cases tied to measurable outcomes
- Embed evidence governance and auditability into the core architecture
- Use modular services that scale without major redesign
- Plan interoperability early to avoid expensive retrofitting later
- Maintain observability across clinical, operational, and model performance
- Design for regulatory evolution instead of one-time compliance
Request a tailored proposal from Intellivon’s healthcare AI experts to receive a delivery roadmap aligned with your clinical priorities, compliance exposure, and long-term enterprise strategy.
Evidence-Driven Treatment Platform Use Cases
Evidence-driven treatment platforms support high-impact clinical use cases such as sepsis detection, oncology pathways, chronic disease management, antimicrobial stewardship, and care gap closure.
Healthcare organizations see the most value when treatment platforms target areas with high variation, risk, or cost exposure.
Therefore, leading enterprises begin with focused clinical use cases that can demonstrate measurable improvement. Over time, these platforms expand across service lines as confidence grows.
1. Sepsis Early Detection and Intervention
Sepsis remains one of the most time-sensitive and costly conditions in acute care. However, early warning signs often appear subtly across labs, vitals, and clinical notes.
Evidence-driven platforms analyze these signals continuously and alert care teams when risk begins to rise.
Key impact areas include:
- Earlier identification of at-risk patients
- Faster antibiotic and protocol initiation
- Reduced ICU escalation and mortality risk
- Better compliance with sepsis bundles
As a result, organizations improve both clinical outcomes and quality metrics tied to sepsis management.
2. Oncology Pathway Management
Cancer care involves complex, rapidly evolving treatment protocols. Clinicians must balance guidelines, patient factors, and therapy sequencing. Evidence-driven platforms help standardize pathway selection while still allowing appropriate clinical judgment.
These platforms typically support:
- Guideline-aligned therapy recommendations
- Biomarker-driven treatment selection
- Regimen sequencing support
- Variation monitoring across oncology programs
Therefore, oncology leaders gain stronger control over both care quality and treatment costs.
3. Chronic Disease Optimization
Conditions such as diabetes, heart failure, and COPD require continuous management across care settings. However, gaps in monitoring and follow-up often lead to avoidable complications.
Evidence-driven treatment platforms help teams intervene earlier and manage risk more proactively.
Common capabilities include:
- Risk stratification for high-need patients
- Care gap identification and alerts
- Medication and monitoring reminders
- Population health dashboard visibility
In addition, organizations often see improvements in readmissions and long-term cost trends.
4. Antimicrobial Stewardship
Antibiotic overuse continues to create both clinical and financial risk. Evidence-driven platforms support stewardship teams by guiding appropriate selection, dosing, and duration based on patient context and guidelines.
Typical benefits include:
- Reduced unnecessary antibiotic exposure
- Better adherence to stewardship protocols
- Improved resistance monitoring
- Stronger audit and reporting support
This use case is especially valuable in large hospital networks managing high antibiotic volume.
5. Care Gap Closure in Value-Based Programs
Value-based contracts require consistent follow-through on preventive and chronic care measures. However, care gaps often remain hidden across fragmented systems. Evidence-driven platforms surface these gaps and prompt timely action.
Organizations commonly use them to:
- Identify missing screenings and preventive services
- Track quality measure performance in real time
- Prioritize outreach for high-risk populations
- Support payer reporting requirements
As a result, enterprises strengthen both quality scores and shared savings performance.
When deployed in the right clinical areas, evidence-driven treatment platforms quickly move from pilot tools to enterprise assets that improve outcomes, utilization, and financial performance.
Conclusion
Healthcare organizations can no longer rely on fragmented guidance and retrospective reviews to manage care quality. Evidence-driven treatment platforms bring clinical knowledge, patient data, and decision intelligence together at the point of care.
As a result, teams make faster, more consistent decisions while leaders gain clearer visibility into performance and risk.
However, the real value comes from how these platforms are designed and governed. Intellivon builds evidence-driven treatment platforms as enterprise-grade clinical infrastructure with deep interoperability, strong evidence controls, and measurable outcome tracking.
This approach helps organizations reduce variation, improve quality metrics, and unlock sustainable ROI. If you are planning your next step, Intellivon can help you move forward with clarity and confidence.
Build Evidence-Driven Treatment Platforms With Intellivon
At Intellivon, evidence-driven treatment platforms are built as a governed clinical decision infrastructure, not as decision support layered onto disconnected systems. Every architectural and delivery decision focuses on evidence integrity, workflow alignment, and real-time data reliability.
As enterprise healthcare environments become more complex, consistency becomes essential. Governance, performance, and audit visibility remain stable even as data volume, clinical pathways, and system integrations expand. Therefore, organizations maintain control over care quality while continuing to improve operational performance.
Why Partner With Intellivon?
- Enterprise-grade treatment platform architecture designed for regulated healthcare ecosystems
- Proven delivery across hospitals, multi-site health systems, and digital care environments
- Compliance by design approach with embedded evidence governance and audit readiness
- Secure modular infrastructure supporting cloud, hybrid, and on-prem deployments
- AI-enabled monitoring, risk prioritization, and performance intelligence with strong governance controls
Book a strategy call to explore how Intellivon can help you build and scale evidence-driven treatment platforms with confidence, control, and long-term enterprise value.
FAQs
Q1. What is an evidence-driven treatment platform in healthcare?
A1. An evidence-driven treatment platform is a clinical decision system that combines medical guidelines, patient data, and analytics to guide care in real time. It helps clinicians follow consistent, data-backed treatment pathways. As a result, organizations improve quality performance and reduce unwarranted variation.
Q2. How is an evidence-driven treatment platform different from traditional CDSS?
A2. Traditional CDSS tools usually provide basic alerts based on fixed rules. Evidence-driven treatment platforms go further by using real-time patient context, governed clinical evidence, and predictive insights. Therefore, they support more precise and enterprise-wide decision-making.
Q3. What data sources are required to power these treatment platforms?
A3. Most platforms rely on EHR data, claims information, clinical guidelines, and real-world outcomes data. In addition, many organizations include remote monitoring and wearable inputs. When unified correctly, these sources provide a complete patient view for better decisions.
Q4. How long does it take to implement an evidence-driven treatment platform?
A4. Timelines vary based on integration scope and clinical complexity. However, many enterprises see initial deployments within four to six months. Broader, multi-site rollouts typically follow in phased stages to ensure stability and adoption.
Q5. How do evidence-driven treatment platforms deliver measurable ROI?
A5. ROI comes from reduced clinical variation, earlier risk detection, and improved guideline adherence. In addition, organizations often see lower avoidable utilization and stronger quality scores. When governance and analytics are embedded from the start, financial impact becomes easier to track and sustain.