When hospitals get bigger and add new services and technology, it gets harder to keep track of patient care by hand. Old ways of working don’t work as well anymore. This can cause confusion, mistakes when handing off patients, and make it tough for teams to know how patients are doing. A special software designed specifically for care pathway management can help fix these problems by not only automating the entire workflow, but also integrating it with existing systems that the hospital already runs on.
Care pathway software helps everyone follow the same steps and see what’s happening with each patient right away. Instead of caregivers working separately, the whole care team can check on patients, see who is responsible for tasks, and make sure everyone follows the plan.
Building this kind of software needs to work with other hospital systems, have clear rules, and fit with how doctors and nurses work. At Intellivon, we build this software to be safe and reliable for big hospitals. In this blog, we’ll explain how we build from the ground up, what it can do, and how our software scales as your enterprise grows.
Why Healthcare Enterprises Need Structured Care Pathways Now
Hospitals and clinics use set care plans to make sure patients get the same good care every time. These plans help stop mistakes and make it easier to reach goals like better health at a lower cost. With more people getting sick and costs going up, this is more important than ever.
Care pathway software helps by putting smart tools, like AI and data analysis, all in one place. This means care teams can help patients get the right care for them, keep things running smoothly, and track how well treatments are working.
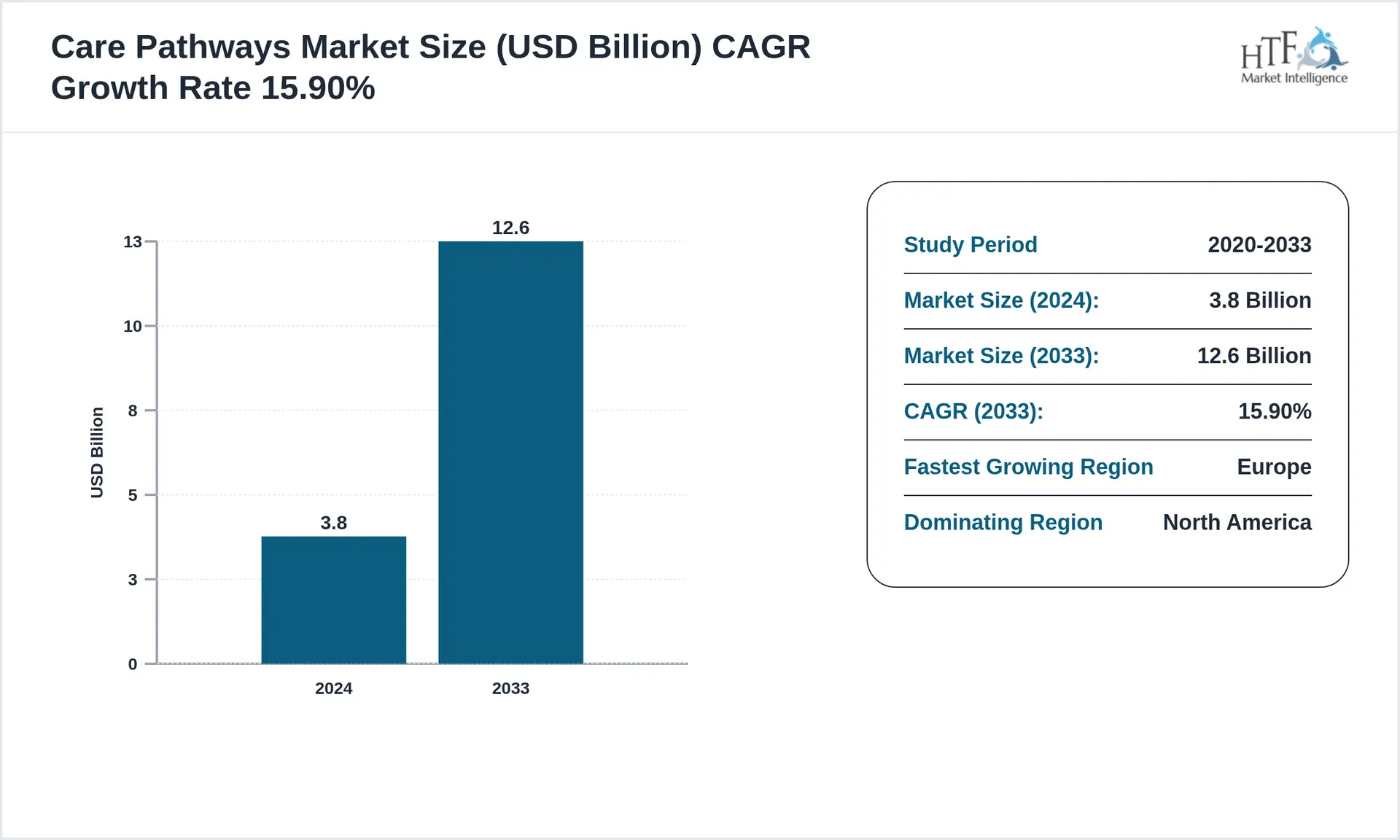
The care pathways market is growing quickly, with a projected CAGR of 15.9% and an expected value of 12.6 billion dollars by 2033. This growth is largely driven by the rising demand for standardized treatment approaches and better chronic disease management.
Key Growth Drivers:
- The shift to value-based care focuses on outcomes instead of service volume. Therefore, organizations need standardized pathways to support accountability and reimbursement.
- The rising burden of chronic disease demands coordinated, data-driven care management. As a result, health systems can reduce readmissions and use resources more efficiently.
- AI and predictive analytics support more personalized care plans. In addition, they help teams forecast risk and make faster, real-time decisions.
1. Growing Pressure to Deliver Consistent Care
Hospitals and clinics must deliver the same high standard of care across every department and location. However, as organizations expand, care delivery often becomes uneven. Small variations in clinical practice can lead to delays, errors, and unpredictable outcomes.
Structured care pathways help reduce this variation. They give care teams a clear, shared plan so patients receive reliable treatment every time.
2. Rising Chronic Disease and Care Complexity
More patients are living with long-term conditions such as diabetes, heart disease, and respiratory disorders. As a result, care journeys have become longer and more complex to manage.
Without a coordinated approach, follow-ups get missed, and patients fall through the gaps. Structured pathways bring these moving parts together. They help teams monitor progress, intervene earlier, and manage chronic populations more effectively.
3. Increasing Focus on Value-Based Care Outcomes
Healthcare payment models are shifting toward outcomes instead of service volume. Because of this change, organizations must prove that care is both effective and efficient.
Structured care pathways make performance easier to measure. They embed quality checkpoints into daily workflows and create clear visibility into patient progress.
This supports better reporting, stronger reimbursement alignment, and improved financial performance.
4. Limited Visibility Into Patient Progress
In many systems, teams still rely on manual tracking and disconnected tools to follow patient journeys. Consequently, leaders often lack real-time insight into where delays or risks are building.
Care pathway management software solves this by creating a unified view of each patient’s progress. With better visibility, teams can act faster, remove bottlenecks, and keep care on track.
5. Need for Smarter, Data-Driven Care Decisions
Healthcare leaders are under pressure to use data more effectively in clinical and operational decisions. Yet many organizations still struggle to turn raw data into practical action.
Modern pathway platforms bring AI and analytics into everyday workflows. This allows teams to identify risk earlier, personalize care plans, and make more confident decisions at scale.
Together, these pressures explain why structured care pathways are quickly becoming essential infrastructure for modern healthcare enterprises.
What Is A Care Pathway Management Software?
Care pathway management software is a digital platform that helps healthcare teams plan, guide, and track each step of a patient’s treatment journey. It brings clinical tasks, timelines, and responsibilities into one structured workflow so care stays consistent across departments and locations. Instead of relying on manual coordination, teams can see what should happen next and who owns each action.
The platform also monitors patient progress in real time and flags delays or missed steps early. As a result, organizations gain better control over care quality, operational efficiency, and outcomes. In large healthcare environments, this software acts as the control layer that keeps complex patient journeys organized and measurable.
Care Pathway Management Platforms Vs Basic Clinical Workflows
Many healthcare organizations still rely on basic clinical workflows to coordinate patient care. These approaches often use manual tracking, static checklists, or loosely connected systems. While this may work in smaller environments, it becomes difficult to manage at an enterprise scale.
As patient volumes grow and care journeys become more complex, gaps begin to appear. Teams spend more time chasing updates, and leadership loses clear visibility into patient progress. This is where care pathway management software creates a meaningful shift. It brings structure, real-time oversight, and coordinated execution into one unified platform.
Basic Workflows vs Care Pathway Management Platforms
| Area | Basic Clinical Workflows | Care Pathway Management Software |
| Care coordination | Often manual and team-dependent | Automated and centrally orchestrated |
| Visibility | Limited real-time insight | Continuous patient journey tracking |
| Standardization | Varies across departments | Consistent, protocol-driven care |
| Variance detection | Usually identified late | Flagged early through real-time monitoring |
| Scalability | Hard to sustain at enterprise scale | Designed for multi-site environments |
| Data usage | Reactive reporting | Proactive, data-driven guidance |
| Operational control | Fragmented across systems | Unified workflow governance |
In practice, the difference becomes clear as organizations scale. Basic workflows help teams manage tasks. However, care pathway platforms help leaders manage entire patient journeys with greater confidence.
Over time, this shift improves consistency, reduces operational friction, and strengthens outcome visibility across the enterprise.
Core Features of Enterprise Care Pathway Management Softwares
Modern care pathway management software brings structure and real-time control to complex care environments. These platforms help organizations keep patient journeys consistent, visible, and easier to manage at scale.
Below are the core capabilities that define enterprise-ready solutions.
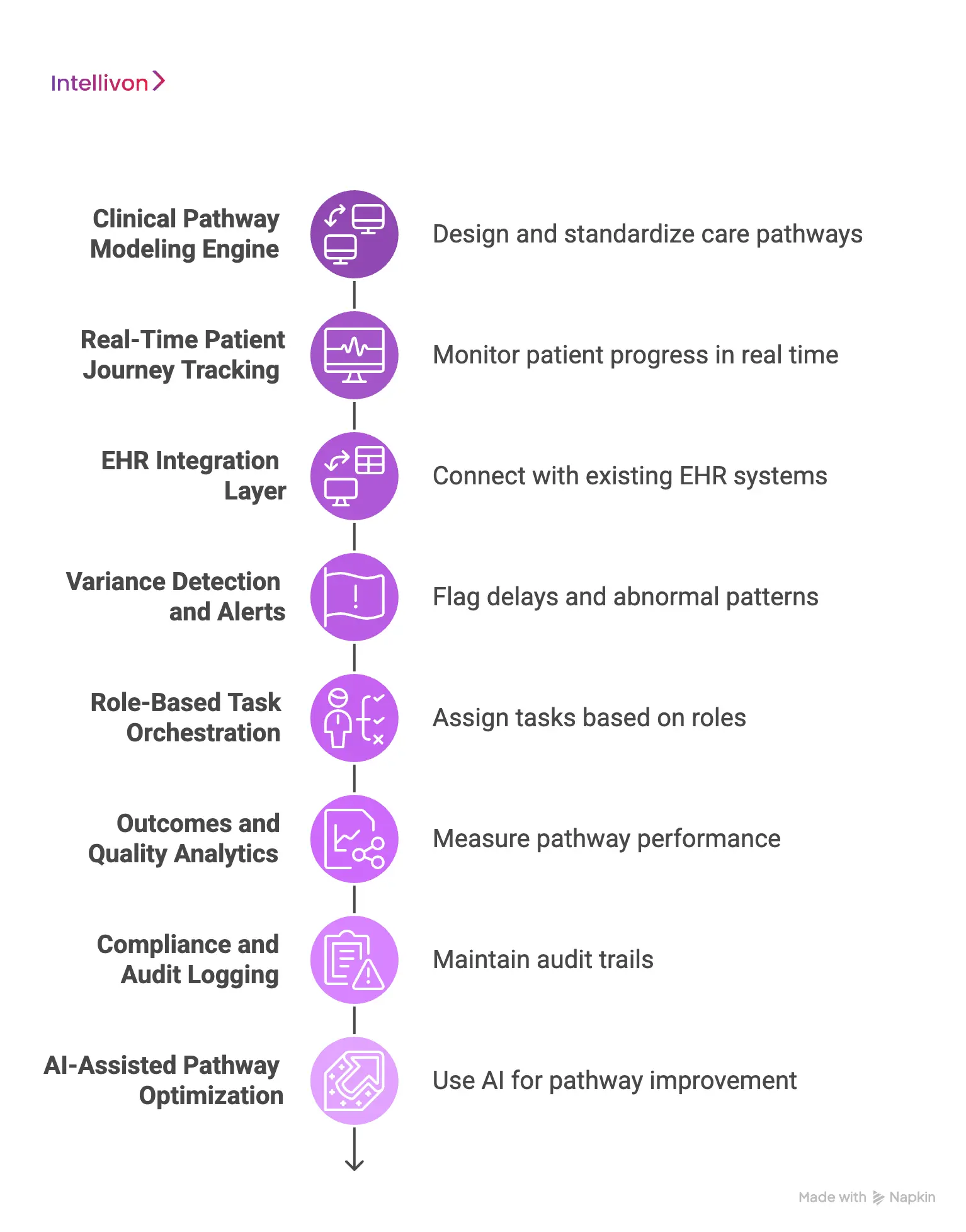
1. Clinical Pathway Modeling Engine
This engine allows organizations to design, standardize, and manage care pathways across conditions and service lines. Clinical leaders can update protocols centrally, which keeps care aligned with the latest guidelines.
It also supports version control, so teams know which pathway is active. As pathways evolve, changes can be rolled out without disrupting frontline workflows. This creates a reliable foundation for consistent care delivery.
2. Real-Time Patient Journey Tracking
The platform continuously tracks where each patient stands in the care process. Care teams can quickly see completed steps, pending tasks, and potential delays. Because updates happen in real time, teams respond faster to emerging risks.
Leaders also gain a clear operational view across departments and facilities. Over time, this visibility helps reduce bottlenecks and improve patient flow.
3. EHR Integration Layer
A strong integration layer connects the pathway platform with existing electronic health record (EHR) systems. This ensures patient data flows automatically between clinical workflows and the pathway engine.
As a result, teams avoid duplicate data entry and manual reconciliation. Real-time data exchange also keeps pathways accurate as patient status changes. Reliable integration is essential for trust at enterprise scale.
4. Variance Detection and Alerts
Care pathway platforms monitor patient progress against the expected clinical plan. When delays, missed steps, or abnormal patterns appear, the system flags them early.
These alerts allow care teams to intervene before small issues become larger problems. Variance tracking also helps quality teams understand where processes may need refinement. This improves both clinical consistency and operational control.
5. Role-Based Task Orchestration
The platform assigns tasks automatically based on clinical roles and responsibilities. Each team member sees exactly what action is required and when it is due.
This reduces confusion during handoffs and improves accountability across departments. As workflows scale, role-based orchestration keeps coordination structured and predictable. It also supports smoother collaboration across multidisciplinary teams.
6. Outcomes and Quality Analytics
Enterprise platforms include built-in analytics to measure pathway performance and patient outcomes. Leaders can track key metrics such as length of stay, readmissions, and protocol adherence.
These insights support both clinical improvement and operational planning. In addition, dashboards help organizations demonstrate performance under value-based care models. Over time, data visibility drives more informed decision-making.
7. Compliance and Audit Logging
Care pathway software maintains detailed audit trails of pathway actions and clinical decisions. This supports regulatory reporting and strengthens internal governance. Teams can quickly review who performed each step and when it occurred.
Consistent audit visibility reduces compliance risk in complex environments. It also builds confidence during external reviews and accreditation processes.
8. AI-Assisted Pathway Optimization
Advanced platforms use AI and predictive analytics to strengthen pathway performance. The system can identify risk patterns, suggest next-best actions, and highlight patients who may need attention sooner.
However, recommendations remain transparent and clinically reviewable. This keeps decision-making grounded in human oversight. When used responsibly, AI helps organizations move from reactive care to more proactive management.
Interoperability in Care Pathway Platforms: Why It Matters
Care pathway management software only works well when it connects smoothly with the systems clinicians already use. In most healthcare environments, patient data lives across EHRs, lab systems, imaging platforms, and specialty applications. When these systems do not communicate reliably, care coordination slows down, and trust in the workflow begins to drop.
Strong interoperability keeps the pathway aligned with real clinical activity. It allows data to move automatically between systems so teams always work from the latest patient information. For large healthcare organizations, this capability is essential for maintaining accuracy and operational control at scale.
1. Eliminates Manual Data Silos
Many hospitals still struggle with information spread across disconnected systems. As a result, care teams often spend time searching for updates or entering the same data multiple times. This creates delays and increases the risk of human error.
Interoperability removes these silos by allowing systems to share data automatically. Patient information flows into the pathway platform without manual effort. Over time, this reduces administrative burden and improves care team efficiency.
2. Keeps Patient Pathways Continuously Updated
Patient conditions can change quickly during treatment. However, static workflows often fail to reflect these updates in real time. When pathways fall out of sync, teams may act on outdated information.
With strong interoperability, the platform receives live clinical signals from connected systems. Pathways adjust automatically as new data arrives. This helps ensure that care decisions stay aligned with the patient’s current status.
3. Supports Multi-System Care Coordination
Enterprise health systems rarely operate on a single technology stack. Patients often move between hospitals, specialty clinics, and partner networks. Without reliable integration, coordination across these environments becomes difficult.
Interoperability allows the pathway platform to function across multiple systems and care settings. Teams gain a unified view of the patient journey even when care spans locations. This is especially important for large, distributed healthcare organizations.
4. Strengthens Trust in Clinical Workflows
Care teams rely on technology only when the information feels accurate and timely. If data appears delayed or incomplete, adoption quickly declines. Trust is therefore closely tied to integration quality.
When interoperability is implemented well, clinicians see consistent and reliable updates. The pathway becomes part of the everyday workflow rather than an extra system to check. Over time, this strengthens both adoption and operational confidence.
Strong interoperability ensures care pathway platforms remain accurate, trusted, and scalable as healthcare ecosystems grow more complex.
How We Build A Care Pathway Management Software
Building care pathway software requires more than screens and checklists. The platform must work inside real hospital environments. It must connect with existing systems, support clinical governance, and stay reliable as usage grows.
At Intellivon, we follow a structured build process so the platform stays practical, safe, and scalable.
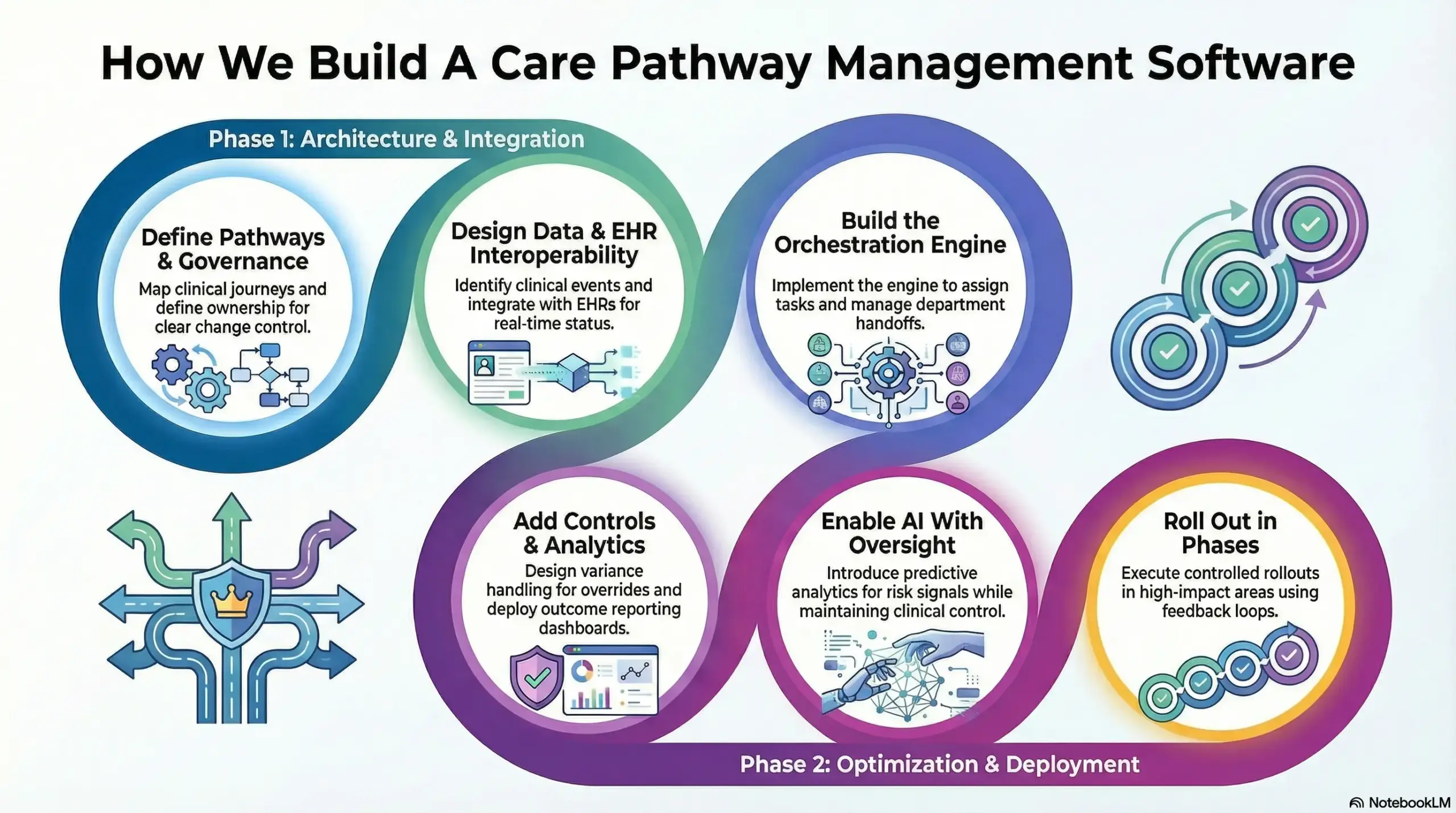
Step 1: Define the Care Pathways
We start by mapping the care journeys that matter most to your organization. This includes clinical steps, handoffs, exceptions, and escalation points. In addition, we define what success looks like, such as reduced delays or improved adherence.
This keeps the build aligned with real outcomes, not assumptions. It also helps teams stay focused during rollout.
Step 2: Build the Operational Governance Model
Every pathway needs ownership and clear change control. Therefore, we define who can create pathways, who can approve them, and how updates are released.
We also set rules for documentation, versioning, and review cycles. This keeps pathways consistent across facilities and service lines. It also improves audit readiness over time.
Step 3: Design the Data Model
Pathway platforms depend on clean, trusted data. We identify the clinical events that should trigger actions, such as orders, results, vital changes, or discharge milestones.
In addition, we define how patient context is captured and reused across workflows. This reduces duplication and improves accuracy. It also helps the platform support analytics later.
Step 4: Implement Interoperability With EHRs
We integrate the platform with EHR environments and supporting systems using standards such as FHIR and HL7 where appropriate. However, we also focus on real operational needs like event timing, data mapping, and write-back.
This ensures pathways reflect current patient status in real time. It also keeps care teams from working across disconnected tools. Integration quality is a key factor in adoption.
Step 5: Build the Orchestration Engine
Next, we implement the engine that assigns tasks, tracks completion, and manages handoffs. Tasks are routed based on role, department, and escalation logic.
As a result, teams know what to do and when to do it. This reduces confusion during busy shifts. It also improves accountability across complex care teams.
Step 6: Add Variance Controls
Healthcare workflows need flexibility, but they also need structure. We design variance handling so clinicians can override steps when needed while documenting the reason. In addition, we set alert thresholds to avoid noise and reduce alert fatigue.
This keeps clinical judgment intact while preserving pathway integrity. It also provides leadership with visibility into true process gaps.
Step 7: Deploy Analytics and Outcome Reporting
Once the pathway runs reliably, we add reporting that leaders can trust. This includes adherence tracking, bottleneck insights, and outcome metrics such as length of stay and readmissions.
In addition, we design dashboards for different user groups, from frontline managers to enterprise leadership. This helps teams improve performance continuously. It also supports value-based care reporting needs.
Step 8: Enable AI Support With Strong Oversight
Where it adds real value, we introduce predictive analytics for risk signals and pathway deviation forecasting. However, we keep outputs transparent and reviewable. Teams can see why a risk is flagged and decide the next step.
This keeps clinical control in the right hands. Over time, this improves proactive care management without introducing black-box decisions.
Step 9: Roll Out in Phases
We roll out pathways in controlled phases to protect operations and build trust. We start with high-impact areas, train users, and track real adoption.
In addition, we use feedback loops to refine pathways and improve usability. This approach supports stable scaling across sites and programs. It also helps the platform deliver measurable value faster.
This step-by-step approach helps Intellivon build care pathway platforms that teams can adopt quickly, and leaders can scale with confidence across enterprise healthcare environments.
Key Use Cases of Care Pathway Management Software
Healthcare organizations use care pathway management software to standardize treatment, improve coordination, and gain real-time visibility into patient progress. As care delivery expands across facilities and specialties, manual oversight becomes harder to sustain. Teams need a clearer structure to keep patients moving through the right steps at the right time.
The platform supports both clinical and operational scenarios across hospitals and health systems. It brings tasks, timelines, and patient signals into one coordinated flow. As a result, leaders gain better control over quality, efficiency, and outcomes.
Below are some of the most common enterprise use cases:
1. Post-Surgical Care Coordination
After surgery, patients must move through tightly timed recovery steps. However, manual tracking often leads to missed milestones, delayed mobilization, or discharge bottlenecks. These gaps can extend the length of stay and increase avoidable risk.
Care pathway software activates the appropriate recovery plan automatically and keeps every step visible. Tasks route to the right teams while progress updates in real time. When recovery slows or a milestone is missed, the system flags it early. This helps hospitals keep post-operative care consistent and on schedule.
How the Workflow Operates
Phase 1: Automatic Pathway Activation
When the patient moves to post-operative status, the platform triggers the correct recovery pathway based on procedure and clinical rules.
Phase 2: Coordinated Task Orchestration
The system assigns recovery tasks to nursing, physiotherapy, and care teams while tracking each milestone.
Phase 3: Real-Time Variance Monitoring
Delays, missed steps, or abnormal recovery signals generate alerts so teams can intervene early.
Phase 4: Discharge Readiness Evaluation
The platform evaluates recovery criteria and supports timely, evidence-based discharge decisions.
2. Chronic Disease Management Programs
Chronic conditions such as diabetes, heart failure, and COPD require consistent long-term oversight. However, care plans often become fragmented across visits and providers. Important follow-ups may slip without a structured system.
Care pathway platforms create a connected view of the patient’s long-term journey. They schedule follow-ups, track adherence, and surface early risk signals.
As a result, care managers can intervene sooner and keep patients on track. This supports stronger population health management and value-based care goals.
How the Workflow Operates
Phase 1: Program Enrollment and Pathway Activation
When a patient enters a chronic care program, the platform activates the condition-specific pathway.
Phase 2: Longitudinal Care Coordination
The system schedules follow-ups, labs, and medication checks within a unified care timeline.
Phase 3: Adherence and Risk Monitoring
Missed visits, abnormal readings, or medication gaps trigger alerts for care managers.
Phase 4: Proactive Care Intervention
Care teams conduct outreach, adjust treatment plans, and document outcomes across the population.
3. Emergency Department Throughput Optimization
Emergency departments operate under constant pressure to move patients quickly without compromising care quality. However, limited visibility into patient progression often creates bottlenecks. Delays in labs, imaging, or consults can quickly slow the entire department.
Care pathway platforms provide real-time tracking from triage through final disposition. Tasks route automatically, and delays surface early for review. Teams can act faster and keep patient flow steady. Over time, this improves throughput, reduces wait times, and supports better resource use.
How the Workflow Operates
Phase 1: Intelligent Triage Pathway Assignment
When the patient is registered and triaged, the platform assigns the appropriate emergency care pathway.
Phase 2: Automated Task Routing
Diagnostics, consults, and treatment tasks route automatically to the correct teams.
Phase 3: Throughput and Bottleneck Monitoring
The system tracks patient movement and flags delays in labs, imaging, or consult workflows.
Phase 4: Disposition Decision Support
The platform supports timely admission, transfer, or discharge decisions based on current status.
4. Oncology Treatment Pathway Management
Cancer care involves complex, multi-step protocols that span departments and timeframes. Without strong coordination, gaps and inconsistencies can appear across the treatment journey. This makes oversight difficult for both clinicians and leadership.
Care pathway software brings the entire oncology workflow into one structured view. It coordinates chemotherapy cycles, diagnostics, and follow-ups while tracking adherence. Care teams can quickly see where each patient stands. This improves protocol consistency and strengthens multidisciplinary coordination.
How the Workflow Operates
Phase 1: Protocol-Based Pathway Activation
When the oncologist selects an approved regimen, the platform activates the matching oncology pathway.
Phase 2: Treatment Milestone Coordination
Chemo sessions, labs, imaging, and supportive care tasks are scheduled and tracked centrally.
Phase 3: Safety and Variance Surveillance
Adverse events, missed milestones, or abnormal results trigger alerts for rapid review.
Phase 4: Outcomes and Protocol Tracking
The platform records adherence, treatment progress, and outcomes for continuous evaluation.
5. Value-Based Care and Quality Measure Tracking
Organizations operating under value-based contracts must closely monitor quality performance. However, manual tracking makes this difficult at enterprise scale. Leaders need clearer visibility into care compliance and outcomes.
Care pathway platforms embed quality checkpoints directly into clinical workflows. Compliance data is captured automatically, and care gaps surface early.
Leadership dashboards update continuously as performance changes. This helps organizations align care delivery with reimbursement and regulatory expectations.
How the Workflow Operates
Phase 1: Quality Measure Mapping
When patients enter a value-based program, the required quality metrics map directly to the pathway.
Phase 2: Embedded Care Guidance
Care teams receive prompts and task guidance at key clinical milestones.
Phase 3: Continuous Compliance Monitoring
The platform tracks adherence and flags gaps in real time.
Phase 4: Performance and Contract Reporting
Leadership dashboards update automatically to reflect performance against value-based targets.
As healthcare delivery grows more complex, these workflows show how care pathway management software brings structure, visibility, and control to enterprise care operations.
How AI Is Transforming Care Pathway Management
AI is changing how healthcare teams design, monitor, and improve care pathways. Earlier systems focused mainly on task tracking and standardization. However, modern platforms can now analyze patterns, surface risk earlier, and support more proactive care decisions.
For large healthcare organizations, the goal is not to replace clinical judgment. Instead, AI strengthens visibility and helps teams act sooner when patient risk begins to rise. When used carefully, it turns static pathways into adaptive care guidance that improves both clinical and operational performance.
1. Early Risk Detection Across Patient Journeys
AI models can scan large volumes of clinical and operational data in real time. This allows the platform to identify subtle risk signals that manual review may miss. For example, small changes in vitals, labs, or utilization patterns can indicate a potential complication.
When the system detects elevated risk, it flags the patient for review. Care teams can then intervene earlier instead of reacting late. Over time, this helps reduce avoidable deterioration and unplanned escalations.
2. Personalized Pathway Guidance
Traditional pathways apply the same steps to most patients. However, individuals often respond differently based on comorbidities, history, and current condition. AI helps tailor pathway recommendations using real patient context.
The platform can suggest next best actions or highlight patients who may need closer monitoring. Clinicians still make the final decision, but they do so with stronger decision support. This approach improves personalization without removing clinical control.
3. Predictive Length of Stay and Throughput Insights
Capacity pressure remains a constant concern for healthcare leaders. AI models can analyze historical and real-time data to forecast the length of stay and potential delays. This gives operations teams earlier visibility into flow risks.
With these insights, hospitals can adjust staffing, prioritize discharges, and manage beds more effectively. Over time, predictive visibility supports smoother throughput and better resource planning.
4 Intelligent Variance Pattern Analysis
Not every pathway deviation signals a problem. Some reflect appropriate clinical judgment. AI helps organizations distinguish between expected variation and true process gaps.
The platform reviews variance patterns across large patient populations. It can highlight where delays cluster or where protocols may need refinement. Quality teams gain clearer insight into what requires attention. This supports continuous pathway improvement at scale.
5. Human-Governed Clinical Decision Support
Enterprise healthcare environments require strong oversight of AI-driven recommendations. Therefore, modern pathway platforms keep outputs transparent and reviewable. Clinicians can see why a patient was flagged and what data influenced the signal.
This human-in-the-loop model preserves clinical authority while still delivering advanced analytics. It also builds trust among care teams and leadership. When governance remains strong, AI becomes a practical support layer rather than a black-box risk.
When implemented with proper oversight, AI helps care pathway management software move from passive tracking to proactive, data-informed care coordination at enterprise scale.
Conclusion
Care pathway management is quickly becoming essential for healthcare organizations that want to scale safely and perform consistently. As patient volumes rise and care models shift toward value, manual coordination can no longer keep pace. Structured pathway platforms bring the visibility, control, and discipline that modern health systems require.
However, success depends on more than deploying new software. Organizations need strong interoperability, clinical alignment, and governance built into the foundation. This is where the right partner makes a measurable difference.
Intellivon designs enterprise-grade AI solutions that turn care pathways into reliable, scalable infrastructure. If your organization is ready to strengthen care delivery and operational performance, now is the time to take the next step.
Develop Care Pathway Management Software With Intellivon
At Intellivon, care pathway management software is engineered as a governed clinical orchestration infrastructure, not as workflow layers added onto disconnected systems. Every architectural and delivery decision focuses on interoperability, clinical alignment, and operational reliability.
As enterprise healthcare environments expand, consistency becomes essential. Governance, performance, and real-time visibility remain stable even as patient volume, integrations, and care complexity grow across the organization.
Why Partner With Intellivon?
- Enterprise-grade care pathway architecture designed for regulated healthcare ecosystems
- Proven delivery across hospitals, multi-site health systems, and digital care platforms
- Compliance by design approach with built-in audit visibility and pathway governance
- Secure modular infrastructure supporting cloud, hybrid, and on-prem deployments
- AI-enabled monitoring, performance insights, and optimization with strong governance controls
Book a strategy call to explore how Intellivon can help you build and scale care pathway management software with confidence, control, and long-term enterprise value.
FAQs
Q1. What is care pathway management software used for?
A1. Care pathway management software helps healthcare teams plan, track, and standardize each step of a patient’s treatment journey. It brings tasks, timelines, and clinical signals into one structured workflow. As a result, organizations improve care consistency, coordination, and real-time visibility. It is especially useful in large health systems where manual oversight becomes difficult to sustain.
Q2. How does care pathway management improve patient outcomes?
A2. The platform keeps care teams aligned with evidence-based steps and flags delays early. Because of this, clinicians can intervene sooner when risks appear. It also reduces missed handoffs and process variation. Over time, these improvements support safer care delivery and more predictable outcomes.
Q3. Can care pathway software integrate with existing EHR systems?
A3. Yes, enterprise platforms are designed to integrate with major EHR environments. They typically use standards such as FHIR and HL7 to exchange data securely. This allows patient updates to flow automatically between systems. Strong integration ensures pathways stay accurate without adding manual work.
Q4. When should a healthcare organization implement care pathway management software?
A4. Organizations usually benefit most when care complexity begins to strain manual coordination. This often happens during multi-site expansion, value-based care adoption, or chronic disease program growth. Implementing the platform earlier helps prevent workflow fragmentation. It also creates a stronger foundation for scalable care delivery.
Q5. Does AI replace clinical decision-making in care pathways?
A5. No, AI is designed to support clinical teams, not replace them. It helps identify risk patterns, highlight delays, and suggest next steps based on data. However, clinicians remain in control of final decisions. With proper governance, AI strengthens care pathways while preserving clinical judgment.