Clinicians spend nearly 50% of their workday on documentation, resulting in $226 billion annually in administrative costs across the healthcare sector. Overwhelming paperwork leads to clinician burnout, delayed diagnoses, and patient frustration. This is where AI clinical summarization steps in, not just as a tool for automation, but as a powerful ally for intelligent understanding, accuracy, and speed in clinical workflows.
AI clinical summarization refers to the use of AI to transform large volumes of unstructured healthcare data into clear, actionable, and legally sound summaries. According to a McKinsey report, AI-driven documentation tools can reduce the time physicians spend on administrative tasks by up to 45%, freeing nearly $1 trillion in global healthcare value. Yet, despite the value, many healthcare enterprises struggle with adoption. Common challenges include integrating AI into legacy systems, managing compliance, and ensuring the AI truly understands complex clinical contexts.
At Intellivon, we’ve worked directly with large healthcare enterprises to solve these exact challenges. Our AI experts build enterprise-grade clinical summarization systems that are compliant, context-aware, and customizable. In this blog, we’ll take you inside that process by showing how we develop robust AI clinical solutions from the ground up.
Healthcare Enterprises Are Rapidly Adopting AI in Clinical Summarization
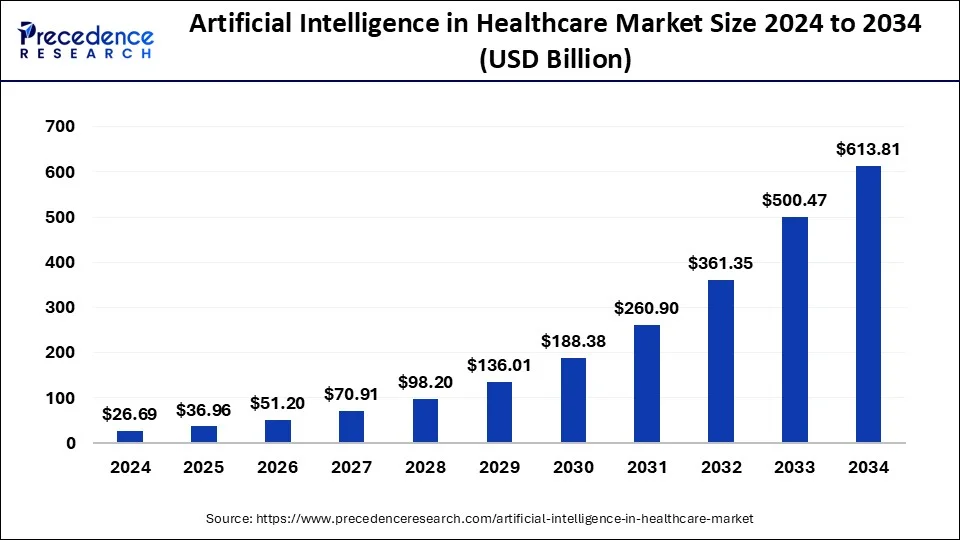
The global AI in healthcare market, valued at USD 26.69 billion in 2024, is expected to grow to USD 613.81 billion by 2034, with a CAGR of 36.83% from 2025 to 2034, according to Precedence Research reports. This significant growth is marked by the revolutionary role of AI in the clinical summarization space, which cuts through hectic manual loads, thereby reducing costs, human errors, and saving time to focus on critical work.
Key Drivers for AI Adoption:
-
- AI Healthcare Market Growth: Expected to reach USD 400-500 billion by 2032, driven by AI adoption in diagnostics, clinical documentation, drug discovery, and patient monitoring.
- AI in Clinical Trials: Projected to grow from USD 2 billion in 2024 to USD 5.1–19.5 billion by 2034, with a CAGR of 16% to 25%.
- North America Dominance: North America holds 49% of the AI healthcare market share in 2024, driven by advanced AI research, regulatory readiness, and infrastructure.
- ROI: Healthcare organizations realize $3.20 for every $1 invested in AI within 14 months.
- Reduction of administrative burdens (AI can reduce physician administrative time by up to 45%).
- Improving clinical efficiency and accuracy through AI-assisted summarization and decision support.
- The growing complexity of healthcare data requires scalable AI solutions.
- Increasing regulatory support and investment in AI technologies.
With AI adoption in healthcare continuing to compound, this is the perfect time to adopt it in clinical summarization for your healthcare enterprise.
Role of AI in Transforming Clinical Summaries for Enterprises
AI is a game-changer in how clinical information is understood, organized, and shared across enterprise healthcare systems. Traditional summarization relies heavily on manual data entry, which is time-consuming and error-prone. With AI, clinical summaries become faster, smarter, and far more reliable. Here is how:
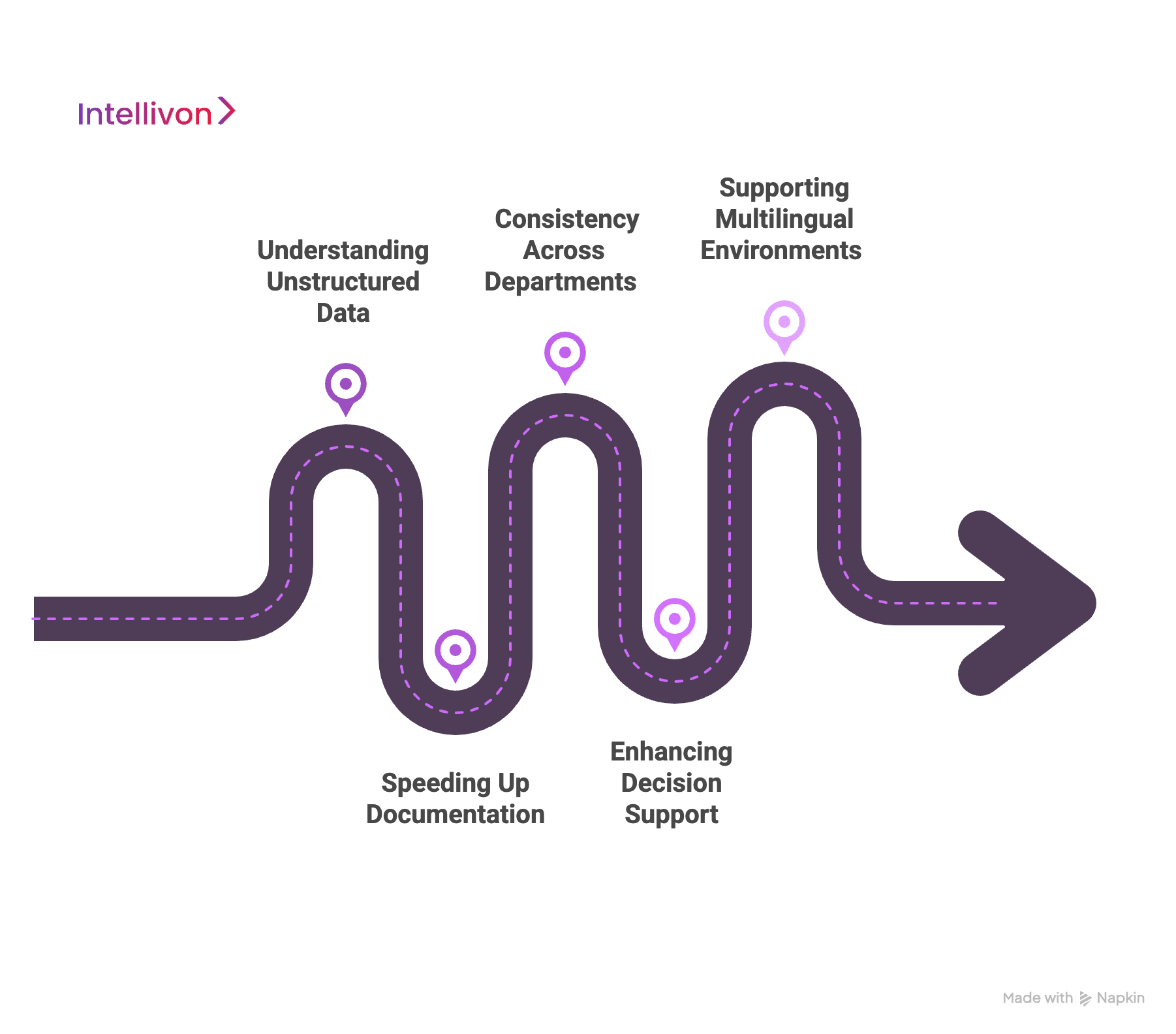
1. Understanding Unstructured Data
Most clinical data lives in messy formats, such as doctor notes, voice recordings, scanned lab results, or discharge instructions. AI can read and interpret this unstructured information using NLP. This means the system understands context, such as symptoms, diagnoses, and treatments.
For instance, if a physician types, “Patient has a history of hypertension and diabetes. Prescribed Metformin,” the AI can extract medical conditions and medications, then generate a summary that includes the patient’s chronic illnesses and current prescriptions.
2. Speeding Up Documentation
Healthcare professionals often spend hours summarizing patient visits. AI can reduce this to minutes or even seconds. The system auto-generates summaries from real-time data inputs, which doctors can quickly review and approve.
For example, during a telemedicine consultation, an AI-powered tool can listen to the conversation, identify clinical keywords, and prepare a summary draft before the session ends. This gives clinicians more time for care instead of paperwork.
3. Consistency Across Departments
In large hospitals, different departments often write summaries in different formats. This makes patient data hard to follow during transitions of care. AI introduces standardization, ensuring all summaries follow the same structure and terminology.
For instance, an AI engine can be trained to use standardized medical vocabularies like SNOMED CT or ICD-10, creating uniformity whether the summary comes from cardiology or orthopedics.
4. Enhancing Decision Support
AI identifies missing data, potential drug conflicts, or red flags in medical histories. This adds a layer of safety and intelligence to the process.
Imagine this: A patient is prescribed a medication that conflicts with an allergy listed in their records. The AI detects the issue and alerts the physician before the summary is finalized.
5. Supporting Multilingual Environments
In global or diverse healthcare settings, AI can translate and summarize patient records across multiple languages. This ensures clear communication between teams and with patients.
For example, AI can convert an English discharge note into a standard French summary for review in a central hospital system.
By transforming messy, unstructured data into usable, clear summaries, AI enables healthcare enterprises to improve accuracy, save time, and deliver better care at scale.
Real-World Enterprise Use Cases of AI in Healthcare Clinical Summarization
AI clinical summarization is being adopted across major healthcare systems to solve widespread issues. These real-world applications demonstrate how enterprise-level healthcare providers are using AI to streamline clinical workflows, improve charge capture, optimize care decisions, and increase operational efficiency. Let’s look at five key enterprise use cases and their examples:
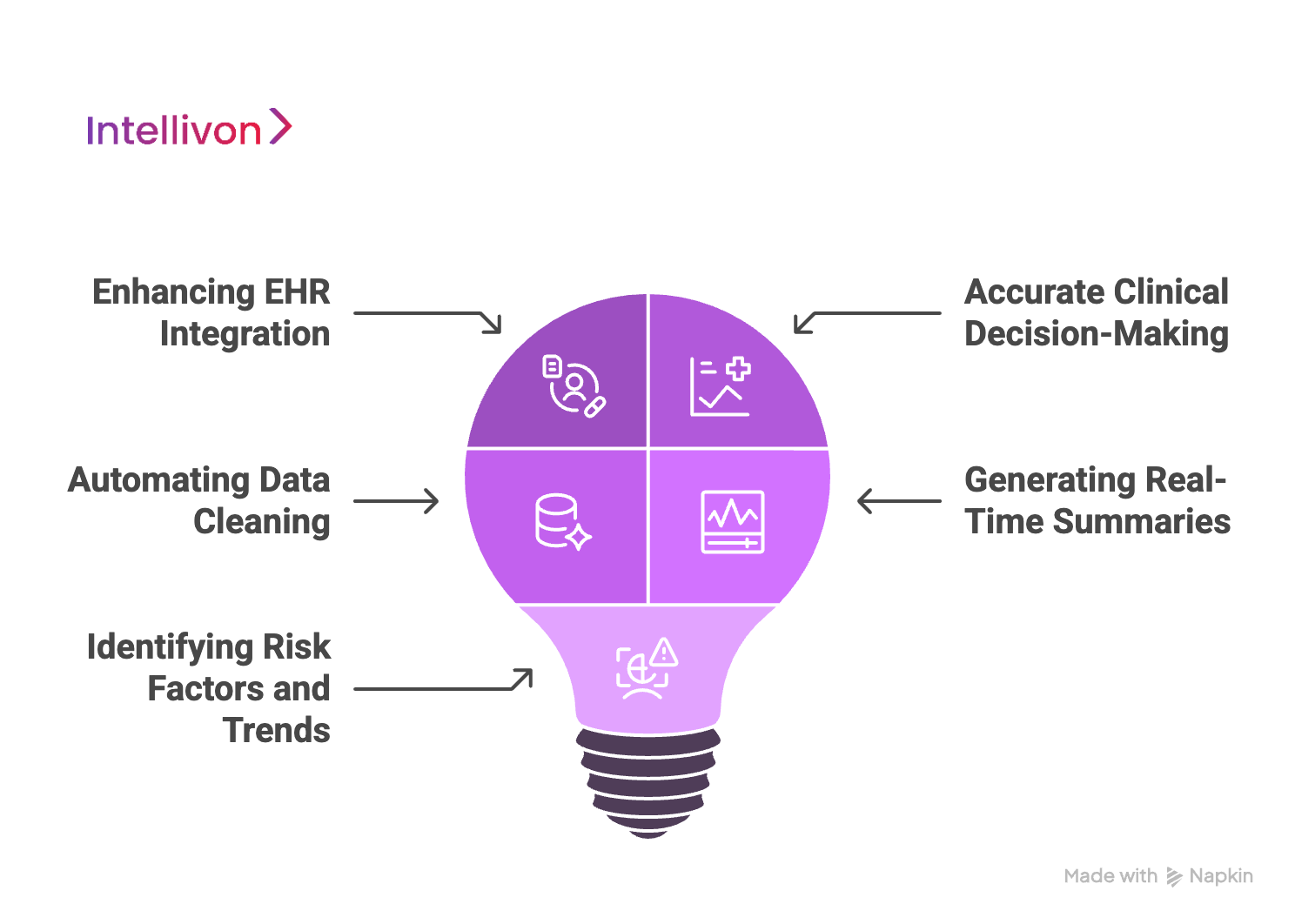
1. Enhancing EHR Integration
One of the most immediate benefits of AI in clinical summarization is improving how data flows into electronic health records (EHRs). By automating and standardizing summaries, AI ensures that essential details are captured in real time. This not only helps with diagnosis and care planning but also ensures accurate billing, an area where hospitals often lose revenue due to incomplete documentation.
Example: University of Rochester Medical Center (URMC)
URMC integrated AI-powered ultrasound tools with clinical summary automation. This move increased ultrasound charge capture by 116%, tripled the number of scans uploaded to the EHR, and improved diagnostic speed and accuracy. The AI system collected data from ultrasound devices, generated structured summaries instantly, and pushed them directly to the patient’s EHR, cutting manual input and errors.
2. Accurate Clinical Decision-Making
In high-stakes environments like emergency care or post-op recovery, nurses and clinicians must make quick, informed decisions. AI clinical summaries pull relevant patient data, such as vitals, history, and medication interactions, into a digestible format. This accelerates decision-making and reduces reliance on manual chart reviews.
Example: Valley Medical Center
Valley Medical Center used AI to implement medical necessity scoring aligned with Medicare standards. Nurses accessed AI-generated summaries that highlighted crucial details, helping them determine whether a patient needed admission or observation. As a result, case review rates jumped from 60% to 100%, enabling quicker escalations and improved documentation consistency.
3. Automating Data Cleaning
AI isn’t limited to summarizing what happened. It can also predict what might happen next. By automating data normalization and analysis, AI prepares data for predictive modeling that guides proactive interventions. These models require real-time, structured summaries to function effectively.
Example: Healthfirst
Healthfirst deployed AI to automate data cleaning, normalization, and real-time predictive modeling within clinical workflows. Using AI clinical summarization, they implemented 17 predictive models that supported fast decision-making. The AI flagged high-risk patients and summarized the risk in clear, actionable terms, helping clinicians intervene early and accurately.
4. Generating Real-Time Summaries
Surgical and critical care units rely heavily on real-time data. AI can digest ongoing inputs from monitoring equipment and turn it into coherent summaries, giving teams immediate insights into patient status and helping them adjust care on the go.
Example: University of Alabama at Birmingham (UAB) Medicine
UAB Medicine used AI in surgical environments for real-time monitoring during cardiac procedures. Personalized clinical summaries were created as surgeries progressed, helping anesthesiologists and surgeons make informed, split-second decisions. The AI synchronized and interpreted patient vitals continuously, offering live summaries that improved response time and patient outcomes.
5. Identifying Risk Factors and Trends
Large healthcare enterprises deal with thousands of patient records daily. AI clinical summaries help filter and surface patterns across populations, allowing providers to detect risks and trends early. This improves both individual care and population health strategies.
Example: Hackensack Meridian Health
Hackensack developed AI tools to generate clinical summaries that highlight emerging patterns in patient data. These summaries supported risk scoring and helped identify early warning signs for conditions like sepsis or cardiac events. With these insights, providers could act faster and more confidently, improving patient outcomes across departments.
By addressing a range of enterprise needs, from documentation speed to proactive care, AI clinical summarization is reshaping the way healthcare providers operate. These real-world examples show that AI is not just promising; it’s already delivering measurable results in complex healthcare environments.
Three-Tier Clinical AI Framework for Healthcare Enterprises
To build a scalable and reliable AI clinical summarization system, healthcare enterprises need more than just a good model. They need a well-structured framework that integrates data, understands clinical context, and supports enterprise-wide decisions. At Intellivon, we follow a three-tier framework designed specifically for complex, high-volume healthcare environments.
This architecture ensures your AI system is not only fast and intelligent but also secure, accurate, and compliant.
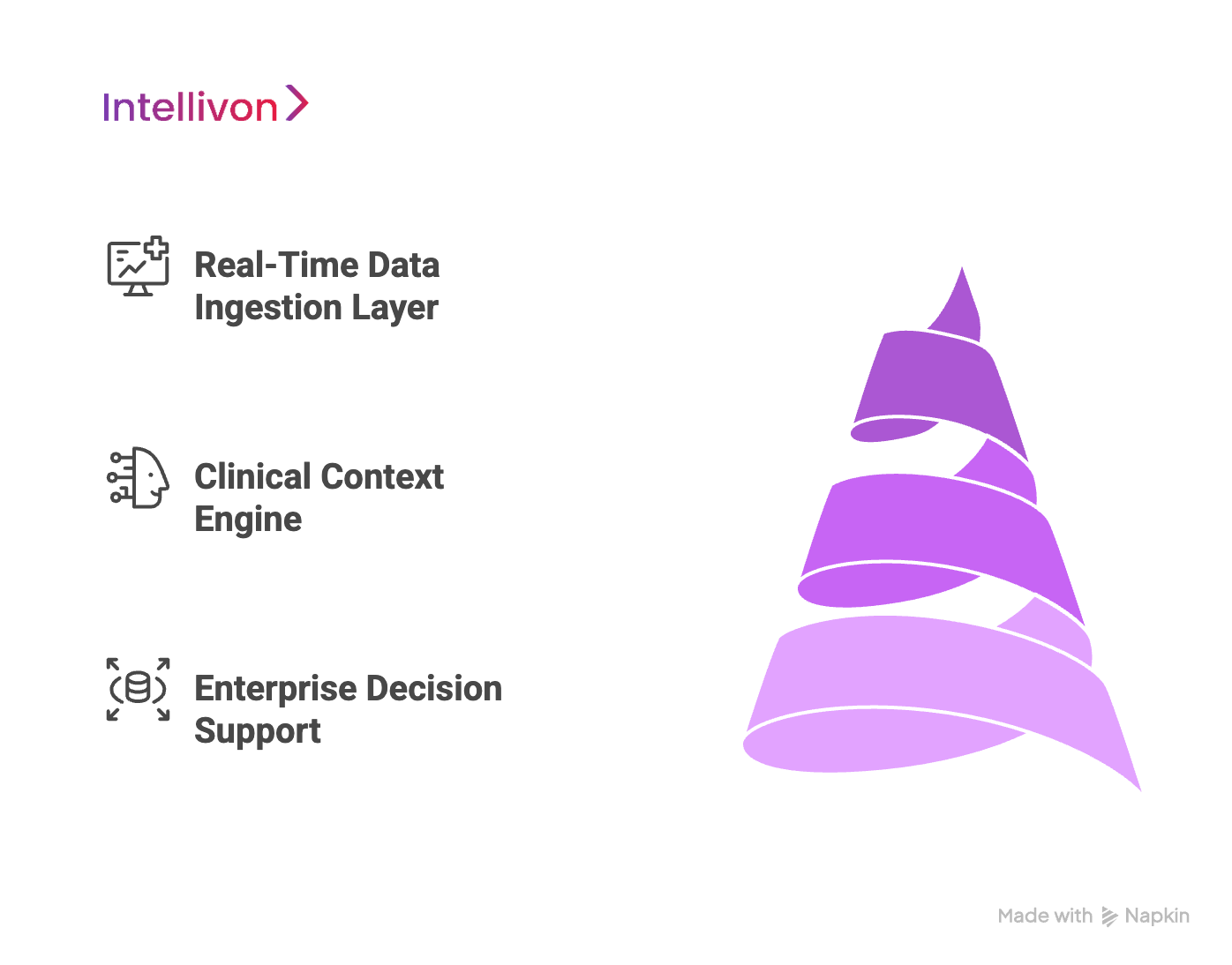
Tier 1: Real-Time Data Ingestion Layer
The foundation of any clinical AI system is its ability to collect and process data in real time. Hospitals generate information from multiple sources, like electronic medical records (EMRs), radiology (PACS), lab results, and even wearable devices. This tier manages how that data is captured, cleaned, and prepared for intelligent processing.
- Multi-Source Integration – AI must work across fragmented systems. This includes EMRs, imaging archives, lab databases, and IoT medical devices. A unified ingestion pipeline pulls structured and unstructured data into one secure environment. For example, a patient’s blood pressure reading from a smartwatch and imaging reports from PACS are processed together for a complete clinical view.
- Edge Computing for Latency-Sensitive Environments – Some environments, like surgical theaters or ICUs, require ultra-low latency. Here, edge computing allows AI systems to process data locally, reducing delay and ensuring summaries are generated on the spot.
- Data Validation and Quality Scoring- Not all clinical data is usable. Algorithms automatically flag missing, outdated, or inconsistent entries. A quality scoring system ensures that only high-integrity data moves forward for AI processing.
Tier 2: Clinical Context Engine
This is the brain of the AI clinical summarization system. It transforms raw data into meaningful insights by understanding the language, logic, and timelines of medicine.
- Medical Entity Recognition (NER) – AI identifies and classifies clinical terms, like symptoms, medications, and procedures, with benchmarked accuracy as high as 99.2% in some systems. This ensures the right terms make it into the summary. For instance, “HTN” is correctly tagged as “Hypertension,” avoiding ambiguity in physician notes.
- Specialty-Specific Language Models – Language in oncology differs vastly from cardiology. This tier uses domain-trained models to ensure that summarization is tailored to the department or specialty involved.
- Temporal Reasoning for Treatment Timelines – Understanding when things happened is crucial. AI uses temporal logic to construct timelines from multiple records, linking symptoms, test results, and interventions in the correct order.
Tier 3: Enterprise Decision Support
Once the AI understands the data and its context, it must support real-world decision-making. This final tier enables hospital-wide actions, reporting, and compliance based on the AI-generated summaries.
- Risk Stratification Algorithms – AI scores patients based on risk, helping prioritize care. These scores are embedded in the summaries so doctors can act immediately.For example, a summary might indicate that a patient has a high readmission risk based on their vitals and recent medication changes.
- Quality Metric Automation – Hospitals are measured against performance benchmarks. AI can automatically extract quality metrics from summaries, saving hours of manual reporting.
- Regulatory Compliance Validation – This layer ensures that all AI outputs are HIPAA-compliant, audit-ready, and aligned with standards like FHIR, HL7, or local regulatory bodies. Built-in checks prevent summaries from containing non-compliant data or privacy violations.
This three-tier clinical AI framework is what makes enterprise-grade clinical summarization possible. It ensures that the system is not only intelligent but also practical, ready to scale, adapt, and deliver value across every layer of the healthcare ecosystem.
How We Develop AI For Clinical Summaries for Healthcare Enterprises
At Intellivon, we follow a rigorous, enterprise-grade 9-step development framework tailored specifically for building AI clinical summarization systems in large-scale healthcare environments. Our framework ensures the final solution is accurate, secure, explainable, and most importantly, usable by every stakeholder involved in patient care.
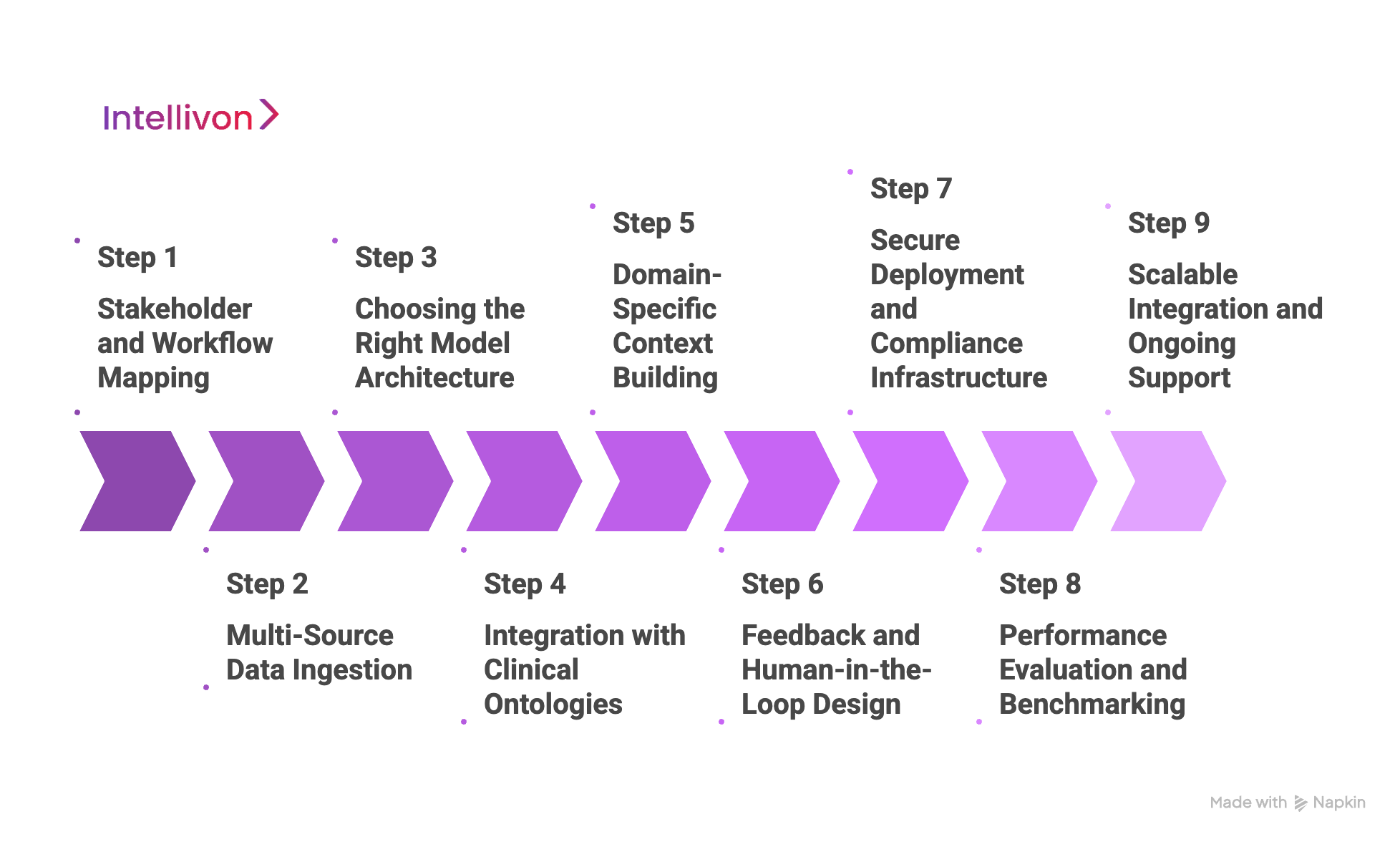
Step 1: Stakeholder and Workflow Mapping
Every successful AI deployment begins with deep stakeholder discovery. We first identify the primary users of the AI-generated clinical summaries, which often include physicians, nurses, billing coders, legal teams, and administrative staff. Each group has different needs and levels of technical comfort.
Once we understand the stakeholders, we map the specific points in the healthcare workflow where summarization will be implemented. This includes areas like patient intake, post-consultation notes, discharge summaries, care transitions, and even billing verification. The goal here is simple: make sure the AI is solving a real-world workflow pain point, and not just a theoretical problem.
Step 2: Multi-Source Data Ingestion
Once workflows are mapped, we build a robust data pipeline capable of ingesting structured and unstructured data from various clinical systems. This includes electronic health records (EHRs), HL7 or FHIR APIs, scanned documents, lab reports, and even voice notes from physicians.
During this process, we apply de-identification protocols to protect patient privacy and meet HIPAA standards. We also clean and standardize data across formats and languages. This is followed by building an annotated corpus of training data with clinician input, ensuring that the AI learns from real medical cases, not generic text.
Step 3: Choosing the Right Model Architecture
Contrary to popular belief, LLMs are not always the best solution for clinical summarization. In many enterprise settings, domain-specific models offer better accuracy, context awareness, and explainability.
At Intellivon, we often choose transformers like ClinicalBERT or GatorTron depending on the clinical domain. In other cases, we use prompt-engineered smaller models that are easier to fine-tune and deploy securely.
For knowledge-intensive tasks, we implement retrieval-augmented generation (RAG) and hybrid models to connect live databases and structured medical knowledge with the model’s predictions. This ensures summaries are fact-checked, relevant, and up to date.
Step 4: Integration with Clinical Ontologies
To produce medically accurate summaries, the AI needs to understand not just language, but clinical logic. This step involves integrating ontologies such as ICD-10, SNOMED CT, and UMLS into the AI pipeline. These resources provide standardized definitions for diseases, symptoms, and procedures.
Alongside these, we implement custom-built rule engines that detect and prevent hallucinations or contradictions in the generated summaries. For example, if a medication is suggested that conflicts with a listed allergy, the AI is trained to either omit it or flag it for review. This step makes the system safe, explainable, and audit-ready.
Step 5: Domain-Specific Context Building
Different medical specialties use different terminologies, formats, and reasoning processes. That’s why we build custom context engines for each clinical department, whether it’s cardiology, oncology, or emergency medicine. We also teach the model to understand temporal relationships in patient care, such as how symptoms progressed over time or how treatments evolved across visits.
This helps the AI reconstruct a logical and clinically meaningful timeline, which is critical for summaries that inform downstream decisions.
Step 6: Feedback and Human-in-the-Loop (HITL) Design
Clinical AI must remain dynamic. That’s why we build HITL systems that allow doctors, nurses, and reviewers to interact with, correct, or validate AI-generated summaries. These edits feed back into our training data, creating a continuous learning loop that improves the system over time.
To support this, we deploy intuitive review dashboards, where each summary is time-stamped, versioned, and traceable. This structure also ensures compliance with audit requirements and enhances user trust in the AI’s reliability.
Step 7: Secure Deployment and Compliance Infrastructure
Security and compliance are non-negotiable in healthcare AI. We deploy solutions using secure configurations, whether on-premises, in private cloud environments, or in hybrid infrastructures.
All APIs and data layers are encrypted, and our pipelines are designed to meet HIPAA, GDPR, and local regulatory guidelines. We use FHIR-compliant APIs to seamlessly integrate the AI solution into existing EHR systems like Epic or Cerner, without disrupting core clinical operations. Every step in the pipeline is auditable and version-controlled, providing peace of mind for both IT teams and compliance officers.
Step 8: Performance Evaluation and Benchmarking
After deployment, we rigorously track how the AI is performing, not just technically, but clinically. We evaluate metrics such as BLEU score, ROUGE-L, concept accuracy, and hallucination rate.
More importantly, we assess clinical outcomes, including time saved per note, physician satisfaction, reduction in documentation errors, and billing accuracy. This ensures the AI system is delivering real, measurable value at every level of the enterprise.
Step 9: Scalable Integration and Ongoing Support
The final step is to ensure the system is scalable, sustainable, and well-supported. Our architecture is modular, allowing clients to scale from one use case, like discharge summaries, to broader deployments like SOAP notes or full chart summarization.
We provide ongoing model tuning, compliance updates, user training, and analytics dashboards. Our support team works closely with IT and clinical leadership to ensure long-term success. This is a strategic transformation of how clinical documentation is handled across the organization.
This 9-step development process is what sets Intellivon apart. We build AI that works in real hospitals, with real data, solving real problems. From intake to integration, every layer of our system is designed to meet the demands of enterprise-scale healthcare environments.
How We Ensure HIPAA-Compliant Clinical Summaries for Enterprises
In healthcare, compliance is foundational. At Intellivon, we understand that every AI-generated clinical summary must meet strict legal, ethical, and operational standards. That’s why we bake compliance into every layer of our AI development and deployment process. From secure data handling to real-time audit trails, our approach is designed to help healthcare enterprises stay protected while innovating at scale.
Here’s how we ensure our AI clinical summarization systems meet and exceed HIPAA and related regulatory requirements.
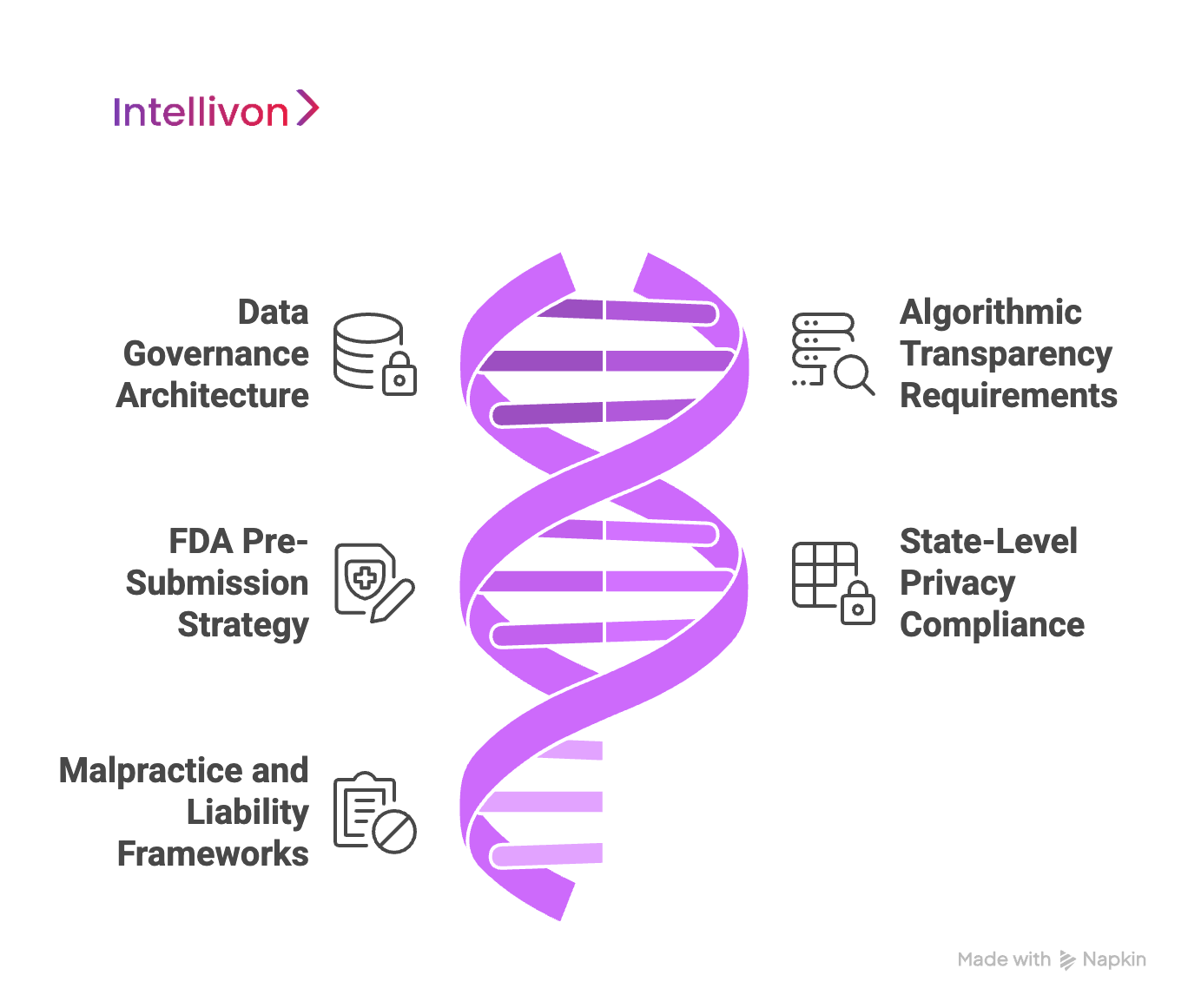
1. Data Governance Architecture
Strong governance begins with how we manage protected health information (PHI). We implement zero-trust security models, which means no device or user is trusted by default. Every request to access patient data is verified, logged, and restricted based on permission levels.
Picture this: A doctor logs into the system to view a clinical summary. Behind the scenes, the AI checks their credentials, limits their access to only what’s relevant, and records every interaction in an audit trail. This trail ensures that any future questions about clinical decisions can be answered quickly and clearly.
We also define data retention and purging protocols. This ensures patient data isn’t stored longer than necessary, reducing exposure risk. Think of it like this: once a clinical summary is no longer needed, it’s securely deleted or anonymized according to the organization’s data lifecycle policy.
2. Algorithmic Transparency Requirements
Healthcare enterprises can’t rely on AI that they can’t explain. That’s why every model we build includes explainability mechanisms. When the AI system makes a suggestion, it shows what data points led to that recommendation.
For instance, if a patient’s lab result indicates abnormal kidney function, the AI summary highlights this and connects it to the flagged condition. This transparency helps clinicians trust the system and improves documentation for medical reviews.
We also monitor the model for bias. Using real-world data from diverse patient populations, we assess whether the AI performs equally well across age, gender, and racial groups. All model updates are version-controlled, so we can track what changed, when it changed, and why.
3. FDA Pre-Submission Strategy
Some clinical summarization systems may cross into the category of regulated medical devices, especially when they assist in diagnosis or treatment planning. In such cases, we help our clients prepare for regulatory review.
Imagine your hospital wants to use an AI system that doesn’t just summarize but suggests care plans. We guide you through the FDA’s De Novo pathway or other relevant processes. This includes collecting real-world evidence, validating safety and effectiveness, and preparing pre-submission materials to ensure the solution can be cleared for use.
4. State-Level Privacy Compliance
HIPAA is the baseline, but many states have their own health privacy laws. These can affect how you manage consent, share data across state lines, or handle minors’ records.
For example, if your enterprise operates in California and Texas, the AI platform must account for both CPRA and Texas HB 300. We build consent management tools that let organizations handle these complexities at scale. That means patients can control who sees their data, how long it’s stored, and where it can be used, even across different jurisdictions.
5. Malpractice and Liability Frameworks
When AI becomes part of the care process, legal risk shifts. We work with providers to ensure every AI-generated summary is clear, verifiable, and legally sound. Documentation is designed to support legal reviews, malpractice insurance, and internal audits.
For instance, if a provider faces a legal claim, they can present the AI-generated summary, its source data, and clinician edits. all time-stamped and versioned. This helps demonstrate that proper clinical judgment was applied.
We also support provider training and certification. Before deployment, clinicians are trained to understand what the AI can and cannot do. This makes sure AI is used responsibly, reducing risk to both the organization and the patient.
Our Compliance-First Development Approach
Our commitment to compliance extends beyond mere compliance to encompass how we design, develop, deploy, and support AI systems.
From the start, Intellivon includes legal and compliance teams in the development loop. Built-in audit tools and automated compliance reporting make it easy to stay inspection-ready. We also offer real-time dashboards that track usage, performance, and risk metrics, so enterprises stay in control.
Overcoming Common Barriers in AI Adoption for Healthcare Enterprises
While the benefits of AI in clinical summarization are clear, many healthcare enterprises still face significant hurdles when adopting these technologies. These challenges go beyond the technical to involve compliance, culture, cost, and complexity.
At Intellivon, we’ve worked with large healthcare systems and understand these pain points firsthand. Here’s how we address the most pressing enterprise-specific barriers to AI adoption.
1. Privacy and Security Concerns
Healthcare organizations handle some of the most sensitive data imaginable. Any AI solution must meet the highest security standards, not just to protect patient information, but also to maintain trust.
Our Solution:
We take a compliance-first approach in all our AI deployments. From day one, our systems are designed to meet HIPAA, GDPR, and any applicable state-level health privacy laws. We use zero-trust architecture, meaning access to patient data is always verified and restricted based on user roles.
For example, if a nurse needs to view a clinical summary, the system only allows access to the relevant portion, no more, no less. Every interaction is logged in a tamper-proof audit trail, which is critical for legal and compliance reviews. We also support real-time alerts for unauthorized access attempts, adding another layer of protection.
2. Data Interoperability
Hospitals often operate with dozens of systems that don’t talk to each other, like EHRs, lab platforms, radiology systems, and custom apps. Making AI work across this fragmented data landscape is no small task.
Our Solution
We’ve built flexible ingestion pipelines that support both HL7 and FHIR standards, enabling seamless integration with major platforms like Epic, Cerner, and Allscripts. Our system can also handle PDFs, voice dictations, and data from wearable devices, harmonizing all of it into a consistent format.
Imagine a hospital that stores discharge notes in one system and vitals in another. Our AI engine pulls data from both and processes it securely, and generates a unified summary. This ensures clinicians get a complete view without toggling between platforms.
3. Adoption Resistance
Even the best AI tool won’t succeed if clinicians don’t use it. Resistance often comes from fear of workflow disruption, lack of trust in machine-generated outputs, or unfamiliarity with the tech itself.
Our Solution
We work closely with providers to build confidence in the system after it has been deployed. This includes training programs, onboarding sessions, and pilot testing within smaller departments before wider rollout.
For instance, in one large hospital network, we started with the emergency department, where documentation pressure was high. After seeing time savings and accuracy improvements, physicians in other departments began requesting access. This organic adoption, backed by real clinical results, helped build long-term trust.
4. Cost Considerations
AI investments can feel overwhelming, especially when enterprises don’t know where to start or how to measure ROI.
Our Solution
We design our deployments to be modular and phased. Instead of implementing a hospital-wide AI solution in one go, we start with a single high-impact use case, like discharge summaries or billing support.
This phased approach allows organizations to see results quickly, build internal buy-in, and allocate budgets gradually. We also provide performance dashboards that track ROI metrics, such as documentation time saved, error reduction, and billing accuracy, so leadership teams can justify continued investment.
Adopting AI doesn’t have to be a high-risk, high-cost transformation. With the right strategy and a partner who understands enterprise realities, healthcare systems can overcome these barriers and unlock the full value of clinical AI.
How We Ensure Integration with Existing EHRs and Hospital IT Stack
One of the most common questions we get from enterprise healthcare clients is, “Will your AI disrupt our existing systems?” The short answer is no. At Intellivon, we’ve built our AI clinical summarization platform to seamlessly integrate with your current hospital infrastructure, especially your EHR.
Whether you’re using Epic, Cerner, Meditech, or a custom-built system, our integration strategy is designed for minimum disruption and maximum interoperability.
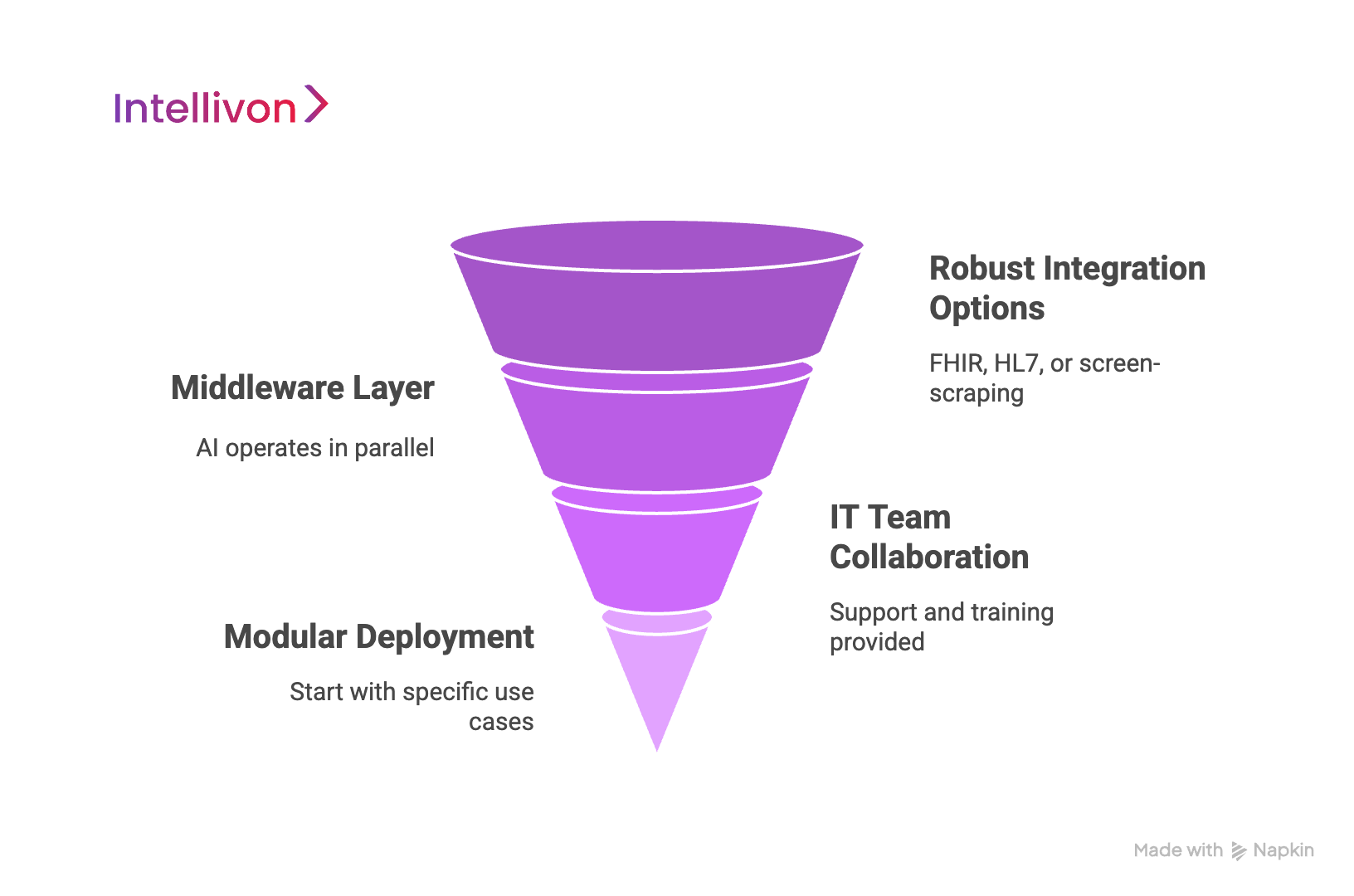
1. Robust Integration Options
Each hospital runs a different setup, which is why we never take a one-size-fits-all approach. For some organizations, FHIR or HL7-based APIs provide a clean path to connect with systems like Epic or Cerner. Where APIs are limited, we use secure HL7 bridges or screen-scraping tools as fallback options, always ensuring compliance and data integrity.
2. Middleware Layer
Rather than tampering with core EHR systems, Intellivon deploys a middleware layer, which is a secure bridge that connects our AI engine with your hospital’s systems. This means the AI operates in parallel, not in the middle of your workflow.
Imagine this: your clinical staff continues using the same EHR interface they’re familiar with. Behind the scenes, our middleware layer collects data, runs it through the AI model, and returns a completed summary, ready for review and validation. No interface changes required.
This is especially useful during patient intake or discharge, where time is critical and workflow consistency is essential.
3. IT Team Collaboration
We understand that every hospital IT team is under pressure to maintain uptime, security, and compliance. That’s why we work directly with your IT department during every stage, from initial assessment to final deployment.
We provide comprehensive documentation, sandbox environments, and support for testing integrations before going live. This gives your IT staff full control and visibility. We also offer on-site or virtual training, so your team can troubleshoot, optimize, and expand the system confidently.
4. Modular Deployment
One of Intellivon’s key strengths is modular deployment. Whether your hospital wants to start with discharge summaries, care transition notes, or specialty-specific documentation, we can deploy the AI engine for just that one use case. Over time, as trust and ROI grow, you can scale to cover broader documentation areas without rebuilding the system.
We ensure you get enterprise-grade AI that fits right into your system, not the other way around.
Future of AI in Healthcare Clinical Summarization for Enterprises
The journey of AI clinical summarization is only just beginning. What we see today is a fraction of what’s possible. As AI continues to evolve, large healthcare enterprises will unlock entirely new layers of efficiency, personalization, and precision in patient care and operations.
1. Moving from Reactive to Predictive
Today’s AI clinical summarization tools largely work with historical data. But the future lies in predictive summarization, where AI doesn’t just document what happened, but anticipates what’s likely to happen next.
Imagine a system that summarizes a patient’s current condition and adds, “Based on the lab trends and comorbidity profile, there is a 78% chance of readmission within 14 days unless XYZ interventions are made.” This level of foresight can help clinicians intervene earlier, prevent complications, and improve outcomes at scale.
2. Greater Personalization at Care Point
As AI becomes more context-aware, it will start tailoring summaries not just by specialty, but by individual clinician preferences. For example, a cardiologist may prefer brief summaries focused on test results, while a general physician may want a more narrative structure with social history. Future systems will learn these preferences and auto-adjust formats and language accordingly, making summaries more usable and intuitive.
This personalization can also extend to patient-facing summaries. Consider simplified versions of clinical notes that patients can easily understand, such as those generated automatically and shared through patient portals, which can help improve health literacy and engagement.
3. Ambient Documentation and Voice AI
Another frontier is ambient AI documentation, where the system listens in on doctor-patient conversations (with consent) and generates summaries in real time. This technology is already emerging and will become more refined, freeing clinicians from their screens and allowing them to focus entirely on the patient.
For enterprises, this means dramatic reductions in documentation time, fewer burnout cases, and more accurate notes, since they’re captured in the moment, not reconstructed later from memory.
4. Advanced Multimodal Summarization
Future AI systems will handle not just text, but multimodal data, such as X-rays, MRIs, ECGs, and even genomic data. They will be able to generate comprehensive summaries that integrate imaging findings, pathology reports, and genetic risk scores into a unified view.
Picture this: a single AI-generated summary that includes the CT scan interpretation, histopathology notes, and a personalized treatment recommendation, all aligned in one document. This level of integration can help care teams coordinate more effectively, especially in complex or multi-specialty cases.
5. Enterprise-Wide Learning
In the near future, AI summarization tools will learn not just from individual interactions but from entire enterprise ecosystems. They’ll detect patterns across departments, surface system-wide inefficiencies, and recommend process improvements automatically.
For example, if surgical teams across hospitals in a network consistently under-document a critical post-op observation, the system can flag it and suggest workflow improvements. This kind of enterprise-level intelligence transforms AI from a documentation assistant to a strategic enabler.
We’re already building toward this future. Our roadmap includes integrating voice AI, advanced personalization engines, and predictive analytics layers directly into our clinical summarization framework. We’re also working on explainable multimodal AI pipelines that help care teams make safer, faster decisions without sacrificing compliance or control.
The future is closer than you think, and it’s being built today.
Conclusion
Clinical summarization AI is about elevating the quality and consistency of care across the enterprise. When implemented thoughtfully, it turns fragmented medical data into clear, actionable insights that support faster decisions, better coordination, and improved patient outcomes.
But this transformation doesn’t happen by accident. It requires a framework built on technical precision, regulatory compliance, and deep clinical understanding. From secure integration with your existing EHR to specialty-specific model tuning and human-in-the-loop validation, every layer must work in harmony to deliver real, lasting value.
Ready to Transform Clinical Documentation with AI-Powered Summarization?
With over 11 years of enterprise AI expertise and 500+ successful deployments across the globe, Intellivon is your trusted partner in building scalable, compliant, and intelligent clinical summarization systems that go far beyond automation. From real-time note generation to seamless EHR integration, we help healthcare enterprises move from documentation chaos to clarity, speed, and accuracy.
What Sets Intellivon Apart?
- Medical-Grade Language Models: We develop and fine-tune clinical summarization engines using domain-specific LLMs integrated with FHIR, SNOMED CT, and ICD-10, ensuring high accuracy and clinical relevance.
- Workflow-Customized AI: Our solutions are trained on your organization’s specialties and documentation processes, delivering summaries that match your care standards and reduce rework.
- Compliance-First Architecture: Every deployment meets HIPAA, GDPR, and state-level privacy laws, with secure hybrid cloud infrastructure and built-in audit trails.
- Seamless EHR Integration: We support modular plug-and-play integrations with Epic, Cerner, Meditech, and other platforms, without disrupting existing operations.
- Human-Centric Improvement Loop: Clinician feedback is continuously incorporated into model training, ensuring ongoing accuracy, usability, and adoption at scale.
Our healthcare AI specialists will deliver:
- A deep dive review of your current documentation workflows and IT stack
- EHR integration planning tailored to your ecosystem
- A regulatory compliance and risk mitigation checklist
- A deployment roadmap aligned with ROI and clinical impact goals
Book your free strategy call with an Intellivon expert today and start building a secure, compliant, and scalable clinical summarization future.