Healthcare enterprises cannot afford to treat compliance as routine paperwork when a single healthcare compliance failure can cost millions of dollars. According to IBM reports, costs can go up to $10.93 million per incident, making compliance a crucial focus when using AI-powered platforms. Still, organizations rely on outdated, manual systems that cannot keep up with today’s complexity. AI healthcare compliance platforms emerge as a necessity during this time. These intelligent systems can turn inconsistent compliance processes into well-oiled automated systems that predict risks before they happen, adapt to regulatory changes in real-time, and integrate compliance into every layer.
With years of experience building AI healthcare compliance platforms for enterprises of every scale, we’re using our expertise to guide you through how we develop such platforms for your organization. In this blog, we’ll share how these platforms are designed to adapt as your enterprise grows, the steps behind their development, and show you why compliance is not a cost burden but a competitive advantage.
What is an AI Healthcare Compliance Platform?
An AI healthcare compliance platform is a system designed to help healthcare enterprises stay aligned with complex regulatory requirements, such as HIPAA, HITECH, CMS, FDA, and state-specific privacy mandates, all the while reducing the burden on human compliance teams.
This platform is like a real-time compliance control tower. Instead of relying on periodic audits and manual oversight, the platform continuously monitors data flows, user activity, billing practices, and clinical processes to ensure everything remains compliant. It turns compliance into a live operational function rather than a retrospective check.
How it Differs from Traditional Compliance Tools
Legacy compliance solutions were reporting engines. They generated logs, produced static reports, and helped teams prepare for audits, but they couldn’t prevent problems in real time. An AI compliance platform, in contrast, is proactive. It uses machine learning to flag suspicious activities (like unauthorized EHR access), detect billing anomalies before claims go out, and even predict where future compliance risks are likely to surface.
For executives, the key difference is impact:
- Traditional tools include more staff hours, higher audit prep costs, and reactive issue handling.
- AI platforms include reduced headcount strain, lower risk exposure, and always audit-ready operations.
Core Functions You Should Expect
For an enterprise to consider such a system “fit for purpose,” it must cover more than HIPAA checkboxes. At a minimum, the core capabilities include:
- HIPAA & HITECH compliance – Safeguarding protected health information (PHI) across all systems.
- CMS billing compliance – Automated checks against Medicare/Medicaid rules and coding accuracy.
- FDA-related compliance – Ensuring trial data integrity and adherence to clinical regulations.
- Enterprise-wide governance – Dashboards for executives that bring together privacy, billing, risk, and operational compliance in one view.
These are platforms that are built for healthcare enterprises to see financial risk exposure, understand system vulnerabilities, and keep operations aligned with regulators.
Why Enterprises Should Use AI Healthcare Compliance Platforms in 2025
Grand View Research projects that the AI healthcare sector will expand dramatically, rising from about USD 26.6 billion in 2024 to nearly USD 187.7 billion by 2030. This acceleration reflects the industry’s push to build more efficient care systems, address ongoing workforce shortages, and improve patient outcomes.
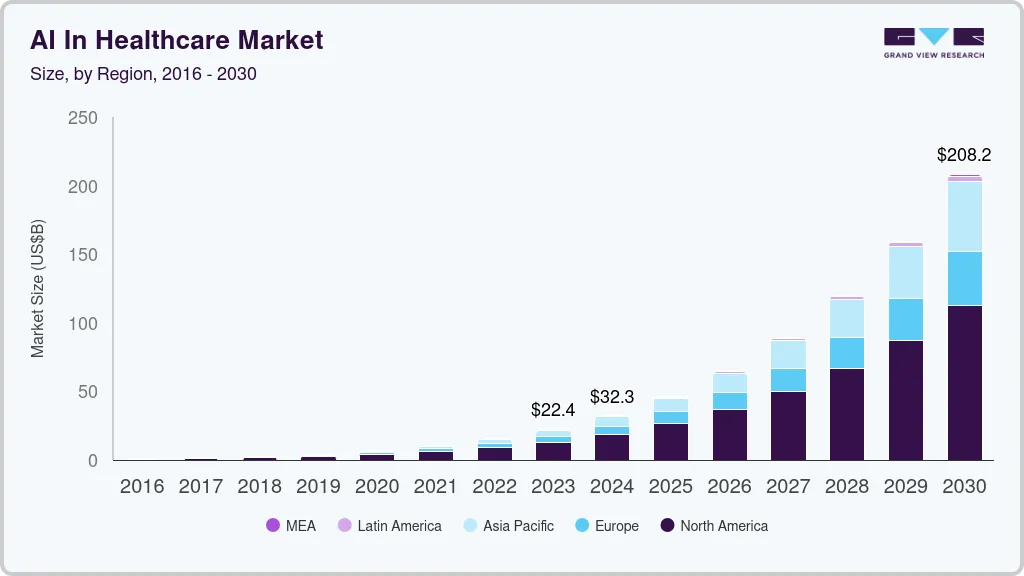
Key Takeaways:
- The global healthcare compliance software market will rise from $3.7B in 2025 to $8.18B by 2032 at a 12% CAGR.
- AI in healthcare compliance is becoming a core differentiator across hospitals, insurers, and pharma.
- In H1 2025 alone, breaches in U.S. healthcare impacted over 29M individuals.
- The average breach affects 65,000+ people, with one August 2025 incident hitting 2.69M records.
- Healthcare faces the highest breach costs globally, $7.42M on average per incident.
- 87% of breaches in August 2025 were caused by hacking and IT incidents.
- 99.2% of compromised data was stolen from network servers.
- Expanding privacy laws (HIPAA, GDPR) are fueling demand for real-time, AI-driven compliance platforms.
- Cloud and SaaS-based compliance solutions are gaining favor for scalability and integration with EHR/telehealth.
- The surge in telemedicine, EHR adoption, and cross-border trials is pushing enterprises toward adaptive compliance systems.
These market forces and breach statistics highlight a critical truth: AI healthcare compliance platforms are becoming the foundation for safeguarding patient data and sustaining enterprise resilience in a high-risk digital health ecosystem.
Types of AI Healthcare Compliance Platforms
Not every compliance challenge in healthcare is the same. That’s why AI compliance platforms come in several forms, and each is tuned to a different slice of the regulatory landscape.
1. HIPAA Compliance Platforms
These platforms are designed to safeguard Protected Health Information (PHI). They monitor access to electronic health records (EHRs), flag unusual activity, and automate breach detection.
For example, if an employee tries to open hundreds of patient files in a short window, the system can immediately generate alerts.
2. Billing & Claims Compliance Platforms
Insurers and provider billing departments face daily exposure to CMS regulations.
AI-driven billing compliance tools review claims in real time, checking coding accuracy, flagging suspicious patterns, and preventing improper submissions.
3. Clinical Trial & FDA Compliance Platforms
Research hospitals, pharmaceutical companies, and biotech firms need to manage strict FDA requirements around trial data integrity and reporting.
AI platforms in this category ensure clinical data is captured, stored, and shared in line with FDA standards, while keeping audit trails regulator-ready. This is especially relevant for enterprises running multi-site studies or handling sensitive genomic data.
4. Enterprise Risk & Governance Platforms
Some healthcare enterprises operate across states, with multiple business units and payer-provider models. Governance-focused platforms give executives a single compliance dashboard, pulling together HIPAA, CMS, FDA, and state-specific rules.
They also apply predictive analytics to highlight where compliance risks may emerge next quarter or next year, enabling proactive governance.
5. Identity & Access Compliance Platforms
Access control is a major compliance requirement. These platforms use AI to enforce role-based access, detect login anomalies, and automate onboarding and offboarding workflows. For COOs and CIOs, they reduce the risk of insider threats and credential misuse while maintaining operational efficiency.
6. Cloud & Infrastructure Compliance Platforms
As more healthcare data moves into the cloud, infrastructure-level compliance is non-negotiable. These platforms continuously monitor cloud workloads for HIPAA compliance, enforce encryption policies, and generate automated audit evidence. Enterprises rely on them to keep hybrid or multi-cloud deployments secure without adding manual overhead.
Most large US healthcare organizations don’t rely on a single platform type. Instead, they adopt a hybrid approach, where a hospital may use HIPAA compliance monitoring alongside billing compliance checks, while a payer integrates fraud detection with enterprise governance dashboards. The strength of AI compliance systems lies in how these different layers work together to create continuous, organization-wide assurance.
Understanding the US Healthcare Compliance Landscape
For any healthcare enterprise, compliance is a web of overlapping federal, state, and industry-specific mandates. Managing this complexity without automation strains compliance teams, raises audit risks, and increases exposure to regulatory penalties.
1. HIPAA and HITECH
- HIPAA sets the foundation for protecting patient data, covering privacy, security, and breach notification.
- HITECH strengthened HIPAA by introducing tougher penalties and encouraging the adoption of electronic health records (EHRs).
Together, they govern how protected health information (PHI) is collected, stored, shared, and secured.
2. CMS Regulations
For hospitals and insurers, the Centers for Medicare & Medicaid Services (CMS) rules define how claims must be submitted and coded. Non-compliance results in rejected claims, revenue loss, and potential fraud investigations. AI-powered billing compliance systems reduce this exposure by validating claims before they reach CMS.
3. FDA Requirements
Pharmaceutical firms, biotech enterprises, and research hospitals must follow FDA guidelines to ensure the integrity of clinical trial data and medical devices. Compliance platforms here provide audit-ready reporting and ensure that data collection meets Good Clinical Practice (GCP) standards.
4. OCR and OIG Oversight
- The Office for Civil Rights (OCR) enforces HIPAA and investigates data breaches.
- The Office of Inspector General (OIG) issues compliance guidance on billing practices, fraud prevention, and ethical conduct.
Both act as watchdogs, and their audits often result in multi-million-dollar settlements for enterprises that fall short.
State Privacy Laws
Beyond federal rules, states like California have introduced CCPA/CPRA, adding layers of consumer data protection. For multi-state healthcare systems, this means compliance shifts by geography, requiring flexible platforms that adapt to different jurisdictions.
Why Enterprises Struggle Without AI
Manual compliance relies on periodic audits and human oversight. In large enterprises handling millions of patient records and claims, this is unsustainable. Data silos, fragmented systems, and ever-changing regulations create blind spots that no manual team can fully cover.
This is why compliance platforms powered by AI are gaining traction. They deliver continuous monitoring, automated regulatory mapping, and real-time alerts, giving enterprises a way to manage compliance at scale.
How AI Healthcare Compliance Platforms Work in Enterprises
To understand the value of these platforms, it helps to see how they operate inside a healthcare enterprise. Instead of reacting to compliance gaps after an audit, AI platforms keep watch in real time, across all critical workflows.
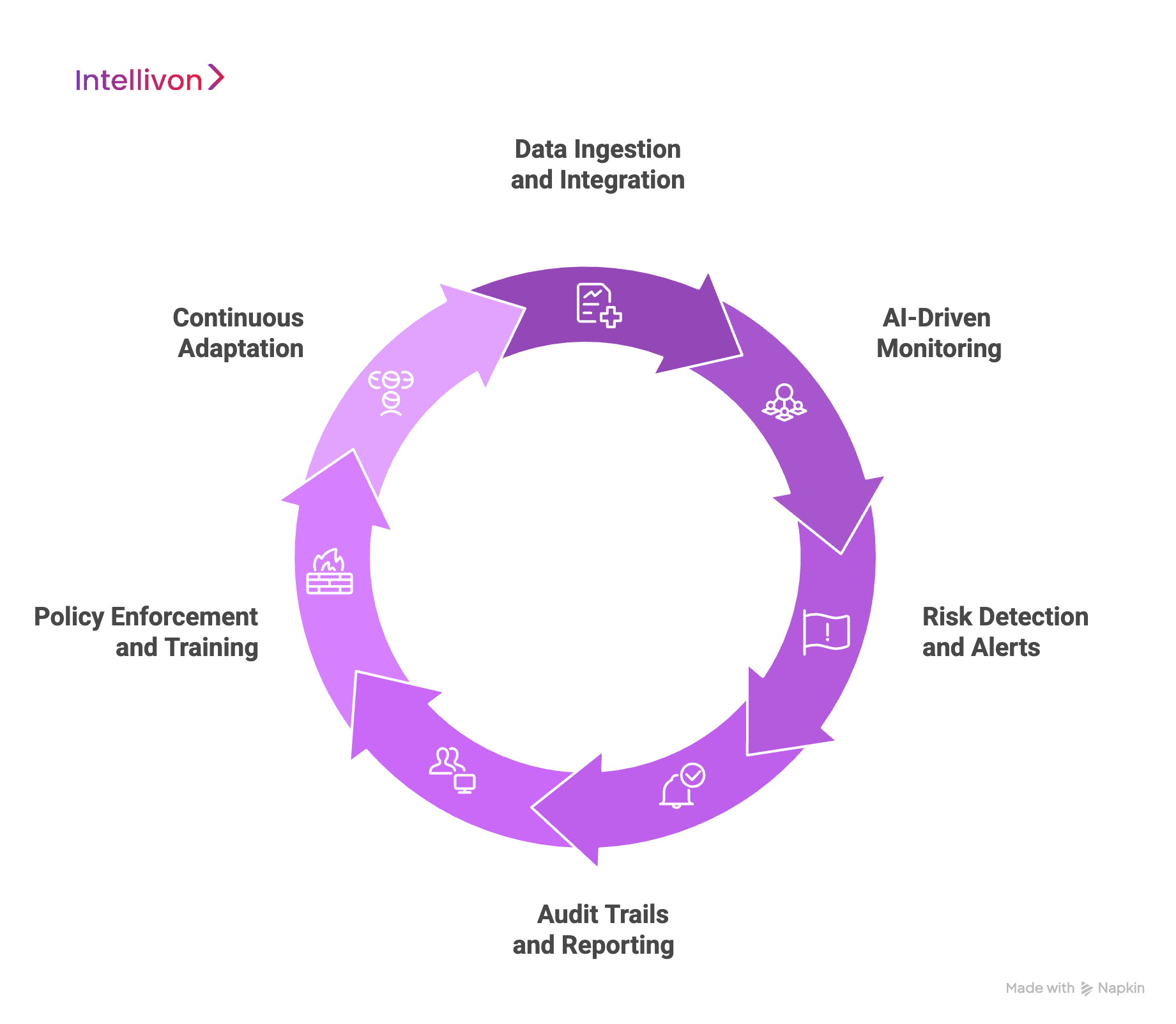
1. Data Ingestion and Integration
The platform connects with core systems:
- Electronic Health Records (EHRs) such as Epic or Cerner
- Billing and claims systems tied to CMS
- Lab, pharmacy, and imaging data
- Patient portals and telehealth platforms
By bringing this information together, the system gains a complete view of where regulatory risks may surface.
2. AI-Driven Monitoring
Once data flows in, AI models and rules engines start monitoring:
- Privacy checks to track PHI access and detect unusual activity
- Billing audits to validate codes and prevent errors before claims are submitted
- Fraud detection to spot suspicious patterns in payments or records
- Data sharing oversight to ensure PHI is not sent outside approved networks
This turns compliance into a continuous process, not a quarterly review.
3. Risk Detection and Alerts
The platform uses anomaly detection to flag potential violations:
- A clinician logging in from two states within an hour
- A claim coded in a way that suggests upcoding
- A large file download from a non-administrative account
Executives and compliance officers receive role-based alerts, ensuring the right teams act quickly.
4. Audit Trails and Reporting
Every system action is logged, creating an immutable audit trail. Reports can be generated instantly, mapped to HIPAA, CMS, or FDA requirements. What once took weeks of manual preparation becomes available in minutes.
5. Policy Enforcement and Training
Beyond monitoring, platforms enforce rules in daily workflows. Staff attempting to access restricted records may be blocked automatically. Training modules and compliance reminders can also be deployed, ensuring teams stay aligned with the latest policies.
6. Continuous Adaptation
Regulations evolve, and these platforms adapt by integrating natural language processing (NLP) models that can interpret new guidelines and adjust compliance checks accordingly. This keeps enterprises aligned with changes in HIPAA rules, CMS updates, or state privacy laws, without needing to rebuild workflows.
Example:
Consider a hospital where a staff member mistakenly emails PHI to an unauthorized third party. The platform detects the transmission, quarantines the email, notifies the compliance officer, and logs the incident for OCR reporting. What could have become a regulatory violation with financial penalties instead becomes a controlled, documented event.
This is how compliance platforms change the game: by turning reactive firefighting into proactive governance.
How AI Works in Healthcare Compliance Platforms
AI transforms compliance from a static checklist into a dynamic, predictive system. Instead of relying solely on human oversight, these platforms embed intelligence into daily operations, catching risks in real time and anticipating future vulnerabilities.
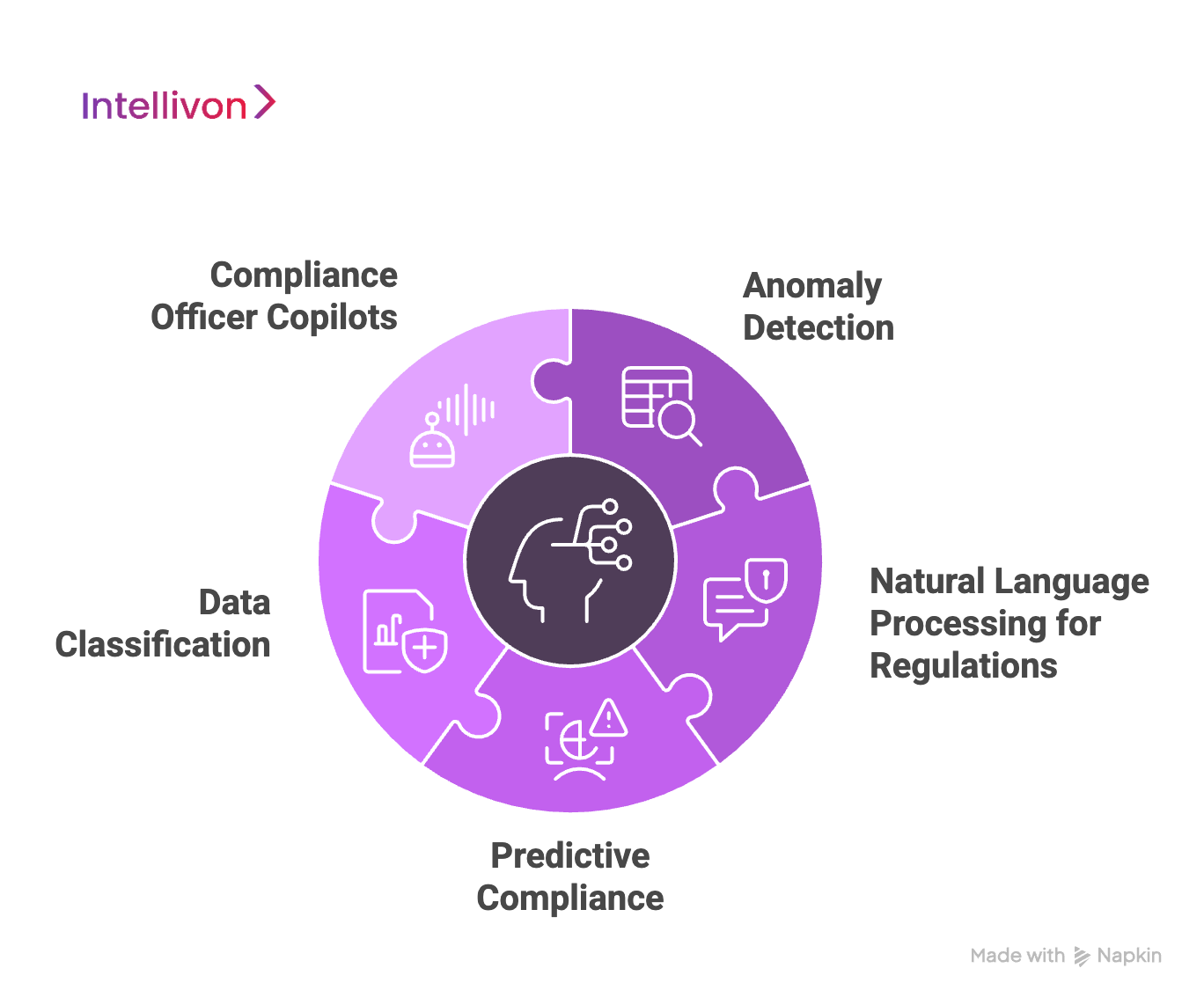
1. Anomaly Detection
AI models are trained to recognize unusual behavior across healthcare systems. This includes irregular billing patterns, sudden spikes in PHI access, or login attempts from unexpected locations. By spotting outliers, the platform helps compliance teams intervene before small issues escalate into regulatory violations.
2. Natural Language Processing for Regulations
Regulatory updates are often written in complex legal language. NLP enables platforms to interpret new rules, whether from HIPAA, CMS, or FDA, and convert them into actionable policies. Enterprises benefit by staying compliant without manually re-coding rules each time laws evolve.
3. Predictive Compliance
Rather than only responding to violations, AI can forecast where risks are likely to emerge. For example, a department consistently showing borderline billing practices may be flagged for review before an audit. This predictive layer shifts compliance from being reactive to being a forward-looking risk management strategy.
4. Data Classification (PHI vs. Non-PHI)
Not all data carries the same regulatory weight. AI engines classify information automatically, separating protected health information (PHI) from operational or anonymized data. This ensures that sensitive records receive stricter safeguards while reducing unnecessary overhead on non-PHI data.
5. Compliance Officer Copilots
Some platforms include AI copilots, which are assistive tools that give compliance leaders conversational insights. Instead of digging through endless logs, a compliance officer can ask: “Which departments had the highest number of PHI access alerts last month?” The AI surfaces insights instantly, saving time and enabling smarter executive decisions.
By combining anomaly detection, predictive analytics, and intelligent copilots, enterprises gain visibility, control, and agility. The result is a compliance function that not only reduces risk but also strengthens trust across the entire healthcare ecosystem.
Features of AI Healthcare Compliance Platforms
For healthcare enterprises, features are what separate a basic compliance tool from a true strategic platform. The right capabilities reduce risk, strengthen governance, and streamline daily operations. Understanding these features helps decision makers choose solutions that align with scale, complexity, and long-term growth.
Core Features
1. Real-Time Monitoring
Continuous monitoring is the foundation of modern compliance. Instead of relying on periodic manual audits, the platform keeps a live watch over EHR access, billing activity, and PHI movement. It reduces the time between incident and response, which is often the difference between a contained event and a regulatory violation.
2. Automated Regulatory Mapping
Healthcare regulations evolve constantly with new CMS billing codes, HIPAA updates, state-level privacy laws, and FDA trial requirements. Manually updating policies across enterprise systems is costly and error-prone. AI-driven regulatory mapping solves this by converting legal text into system rules. When regulators issue new guidance, the platform adapts automatically, ensuring compliance teams don’t have to rewrite workflows by hand.
3. Audit-Ready Reporting
Audit preparation is one of the most resource-draining parts of compliance. Platforms equipped with immutable logging and automated reporting eliminate that burden. Every access event, billing decision, and data transfer is logged in real time.
4. Fraud and Billing Compliance Checks
Fraudulent or inaccurate claims can lead to penalties, lost revenue, and damaged trust. AI-driven platforms validate claims before submission, cross-checking them against CMS rules and detecting patterns of potential fraud.
5. Identity and Access Control
Insider threats and credential misuse are growing challenges. Advanced identity and access features use AI to enforce strict role-based permissions, monitor behavioral patterns, and block unusual activity before it escalates. Enterprises gain confidence that only authorized personnel are handling sensitive health data, and accountability is strengthened across the workforce.
6. Cloud-Native Scalability
Healthcare enterprises are managing unprecedented volumes of data from EHRs, wearables, imaging, and telehealth. Cloud-native platforms provide the elasticity needed to scale compliance monitoring without costly on-premises infrastructure.
Advanced Features for Enterprise-Grade Operations
1. Predictive Compliance Analytics
Reactive compliance only catches violations after they occur. Predictive analytics changes the game by spotting risk trends early. Using machine learning, the platform identifies departments, workflows, or data channels that are showing patterns consistent with future non-compliance.
2. Cross-Border Compliance Support
Healthcare enterprises increasingly operate across state or national borders. Each jurisdiction has unique requirements, such as California’s CPRA, Europe’s GDPR, or FDA versus EMA trial guidelines. Compliance platforms with cross-border capabilities adapt policies automatically to regional laws, ensuring that enterprises don’t face legal exposure simply by expanding their footprint. It reduces the complexity of managing compliance at scale and supports global growth strategies.
3. Automated Incident Response
Speed matters when a breach occurs. Automated incident response enables the platform to take immediate containment actions, such as quarantining suspicious data flows, disabling compromised accounts, or notifying compliance officers in real time. This reduces dwell time(the period between a breach and its discovery), which is critical for both regulatory reporting and damage control.
4. Integrated Staff Training
Integrated training modules deliver context-sensitive reminders and e-learning directly within daily workflows. For example, if a nurse attempts to access a restricted record, the system can display a compliance reminder or block the action with an explanation. This turns training from a once-a-year activity into a continuous reinforcement mechanism.
5. Third-Party Vendor Monitoring
Modern healthcare ecosystems rely on telehealth platforms, cloud vendors, research partners, and payment providers. Each introduces new compliance risks. Vendor monitoring features extend oversight beyond internal systems, tracking whether external partners meet HIPAA, CMS, or FDA requirements.
Emerging Features Shaping the Future
1. Blockchain Audit Trails
Blockchain-enabled audit trails create a permanent, tamper-proof record of compliance events. Regulators and auditors gain complete trust in the integrity of the logs, while enterprises can demonstrate stronger accountability. This feature is especially relevant for pharma companies and research hospitals handling sensitive trial data.
2. AI Copilots for Compliance Officers
Compliance officers often sift through mountains of data to find risks. AI copilots streamline this by acting as interactive assistants. Leaders can ask natural language questions such as, “Show me the top five risk trends in claims this quarter”, and receive immediate insights. This turns compliance from a back-office function into a strategic partner for executives.
3. Robotic Process Automation (RPA)
Many compliance checks are repetitive: validating claims, reviewing access logs, or matching documents against regulatory templates. RPA automates these low-value tasks, freeing compliance teams to focus on higher-level governance and risk strategy. Enterprises gain both efficiency and accuracy.
By combining core, advanced, and emerging features, AI healthcare compliance platforms give enterprises a pathway to maturity. Some start with essential HIPAA and billing safeguards, while others deploy enterprise-wide governance and predictive analytics from day one. The right mix depends on scale, risk profile, and growth ambitions.
How We Develop AI Healthcare Compliance Platforms
Building an AI-powered compliance platform is not a one-size-fits-all exercise. At Intellivon, we follow a structured methodology that balances regulatory precision with enterprise scalability. Each stage is designed to align with strict compliance standards while ensuring the system is practical for real-world healthcare operations.

Step 1: Regulatory and Risk Alignment
Every development begins with a compliance-first approach. We map enterprise needs against regulatory frameworks such as HIPAA, HITECH, CMS billing requirements, FDA guidelines, and state-level privacy laws.
This ensures the platform is built with a clear understanding of both legal obligations and organizational risk priorities. Executives gain confidence that compliance is not bolted on later but designed from the start.
Step 2: Data Architecture and Ingestion
Healthcare enterprises generate massive volumes of structured and unstructured data. We design pipelines that connect seamlessly to EHR systems, billing platforms, lab data, pharmacy systems, and telehealth tools.
By incorporating both structured data, like claims, and unstructured data, like physician notes, the platform achieves a comprehensive risk view. APIs ensure smooth integration without disrupting existing workflows.
Step 3: Data Quality and Feature Engineering
Compliance systems are only as strong as the data they process. Our approach emphasizes cleansing, normalization, and enrichment of raw data. We create high-value features such as abnormal billing patterns, login frequency anomalies, or unusual PHI access.
These features fuel machine learning models, helping them identify compliance risks that humans may overlook.
Step 4: Model Development and Training
We combine interpretable models like logistic regression and gradient boosting with more advanced deep learning where complexity demands it. Ensemble methods improve accuracy by blending model strengths.
Each model is tested for fairness and bias, ensuring compliance decisions cannot be challenged on discriminatory grounds. This dual focus on accuracy and accountability is critical for both regulators and executives.
Step 5: Stress Testing and Validation
Before deployment, models undergo rigorous stress testing. We simulate scenarios such as billing surges, insider misuse, or high-volume PHI access during a cyberattack.
Backtesting against historical claims and breach records validates accuracy under real-world conditions.
Step 6: Explainability and Compliance Governance
Compliance cannot be a black box. We embed explainability tools such as SHAP and LIME to show why a model flagged a transaction or user. Audit logs are automatically generated, linked to regulatory frameworks, and stored in immutable records.
Step 7: Deployment and Integration
The platform is deployed using a cloud-native, microservices-based architecture. This allows scalability while maintaining strict security. APIs connect the platform to existing healthcare IT systems, enabling real-time compliance checks within workflows.
Executives see results quickly: claims validated before submission, suspicious logins flagged at login, and trial data tracked for FDA standards.
Step 8: Continuous Monitoring and Adaptive Learning
Compliance is never static. Once live, the platform continuously monitors data flows, risk events, and regulatory updates. Machine learning models adapt to new patterns such as emerging fraud schemes or revised CMS rules.
Automated retraining pipelines ensure performance doesn’t degrade over time. For enterprises, this means compliance remains aligned not just today but as regulations and risks evolve.
Book a strategy call with Intellivon today and discover how our AI-driven compliance platforms can protect your enterprise and keep you ahead of regulatory risks.
Cost of Developing an AI Healthcare Compliance Platform
At Intellivon, we recognize that healthcare enterprises need compliance platforms that are both secure and cost-effective. That’s why our pricing is designed to be flexible and aligned with your requirements, not a one-size-fits-all package.
If costs risk exceeding your planned budget, we work with you to streamline the scope while safeguarding core compliance value.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Compliance Strategy | Requirement gathering, KPI alignment, regulatory mapping (HIPAA, CMS, FDA) | $6,000 – $10,000 |
| Architecture & Data Design | Platform blueprint, data pipelines, interoperability planning (EHR, billing, labs) | $8,000 – $14,000 |
| Model Development & Integration | Machine learning models, anomaly detection, NLP for regulations, API integrations | $12,000 – $20,000 |
| Platform Development & Customization | Compliance dashboards, rules engine setup, enterprise workflow customization | $14,000 – $22,000 |
| Security & Regulatory Alignment | Encryption, role-based access control, audit trails, HIPAA/FDA/CMS validation | $6,000 – $12,000 |
| Testing & Validation | Stress tests, breach simulations, performance optimization, bias/fairness audits | $6,000 – $12,000 |
| Deployment & Scaling | Cloud rollout, monitoring dashboards, multi-site governance setup | $5,000 – $10,000 |
Total Initial Investment Range: $50,000 – $100,000
Ongoing Optimization (Annual): $5,000 – $10,000
Factors That Influence Cost
The actual investment varies depending on:
- Complexity of IT infrastructure and number of EHR/billing integrations
- Volume of patient data and real-time monitoring needs
- Deployment model (cloud, hybrid, or on-premises)
- Regulatory mandates to be covered (HIPAA, CMS, FDA, state laws)
- Depth of customization vs. pre-built components used
- Advanced features such as predictive compliance analytics or vendor monitoring
Request a tailored quote from Intellivon’s AI engineers today. We’ll design a healthcare compliance platform that aligns with your budget, protects your enterprise, and scales as regulations evolve.
Top US Healthcare Enterprises Using AI Compliance Platforms
AI compliance platforms are not theoretical. Leading healthcare organizations in the United States are already using them to reduce risk, safeguard patient data, and improve operational efficiency. Each enterprise applies AI differently depending on its size, scope, and compliance priorities.
1. Mayo Clinic
Mayo Clinic operates one of the largest EHR ecosystems in the world. It uses AI-driven compliance tools to monitor PHI access across thousands of physicians, researchers, and staff. Real-time alerts reduce the risk of unauthorized access, ensuring HIPAA requirements are continuously met.
2. Cleveland Clinic
Cleveland Clinic manages a vast volume of Medicare and Medicaid claims. AI compliance platforms here focus on billing accuracy, coding validation, and fraud detection. For executives, this reduces exposure to CMS penalties while improving claim acceptance rates.
3. Kaiser Permanente
As both a provider and insurer, Kaiser Permanente faces complex compliance obligations across hospitals, clinics, and payer services. Its platforms unify multiple compliance functions, like HIPAA monitoring, claims validation, and vendor oversight, into a single governance framework. This integrated approach allows executives to view compliance across the enterprise in real time.
4. UnitedHealth Group
UnitedHealth Group, the largest U.S. health insurer, processes billions of claims annually. AI systems are deployed to detect fraudulent activity, validate CMS rules, and ensure HIPAA-secure data sharing with providers. The scale of automation reduces manual review workloads and enhances regulatory readiness.
5. Mount Sinai Health System
Mount Sinai operates both as a care provider and a research institution. AI compliance platforms help ensure data integrity in FDA-regulated clinical trials while also securing patient data across hospital networks. Automated reporting tools make audit preparation faster and more reliable.
Hospitals tend to adopt AI platforms for HIPAA monitoring and EHR oversight, while insurers prioritize claims validation and fraud detection. Integrated health systems like Kaiser and Mount Sinai deploy a hybrid approach that covers privacy, billing, and research compliance. This demonstrates that the value of AI compliance is not confined to one function but extends across the healthcare enterprise.
Conclusion
AI healthcare compliance platforms are no longer optional. With regulations expanding, breaches rising, and costs of violations at record highs, enterprises need systems that provide continuous oversight, predictive risk management, and audit readiness. Yet building and scaling such platforms requires expertise across healthcare regulations, data security, and advanced AI.
This is why selecting the right solution provider matters. The right partner ensures compliance is not just maintained but embedded into daily operations, turning a regulatory burden into a framework for resilience, operational efficiency, and long-term trust.
Build Your Next AI Healthcare Compliance Platform With Intellivon
At Intellivon, we bring years of experience building enterprise-grade healthcare compliance platforms powered by AI. Our solutions are secure, scalable, and designed to align with strict regulatory frameworks. We partner with healthcare enterprises to transform compliance into a proactive strength, thereby reducing risk, safeguarding patient trust, and driving operational efficiency.
Why Partner with Intellivon?
- Tailored Healthcare Solutions: Every platform is designed to fit your compliance needs, IT environment, and regulatory obligations.
- Security and Compliance First: HIPAA safeguards, encryption, audit trails, and governance are embedded from day one.
- Proven ROI for Healthcare Enterprises: Our platforms cut audit preparation time, reduce claim denials, and scale with your growth.
- End-to-End Delivery: From compliance assessment to enterprise rollout, we manage the full development and integration journey.
- Specialized Expertise: Our dedicated healthcare AI team ensures your platform delivers measurable results across clinical, billing, and operational compliance.
Book a discovery call with Intellivon’s AI engineers today and see how a compliance platform can protect your enterprise while unlocking efficiency and long-term resilience.
FAQs
Q1. Is compliance only with HIPAA in the US?
A1. No. While HIPAA is the cornerstone of healthcare data protection, enterprises must also comply with CMS billing requirements, FDA clinical trial regulations, and evolving state privacy laws like California’s CPRA. Large systems often face overlapping obligations across multiple regulators.
Q2. Can this integrate with Epic/Cerner?
A2. Yes. Modern compliance platforms connect directly with leading EHR systems such as Epic and Cerner through APIs and FHIR/HL7 standards. This ensures continuous monitoring of PHI access, audit trails, and billing workflows without disrupting clinical operations.
Q3. How secure is PHI in these platforms?
A3. PHI security is central. Platforms use encryption, role-based access controls, and immutable audit logs. They also undergo HIPAA, SOC 2, and ISO 27001 compliance validations. For enterprises, this means patient data remains protected against both insider misuse and external breaches.
Q4. How fast can enterprises deploy?
A4. Deployment timelines vary by scope and integration needs. A mid-sized health system can often implement a baseline platform in 12–16 weeks. Larger enterprises requiring advanced features and multi-site rollouts may take longer, but phased deployments allow compliance benefits to be realized early.
Q5. What ROI should a health system expect?
A5. ROI comes in several forms: reduced penalties, faster audits, fewer denied claims, and stronger patient trust. Enterprises often see audit preparation time cut by 60–70%, claim