Artificial intelligence is transforming how healthcare organizations predict risks, streamline operations, and personalize patient care. But as these systems evolve, so does the responsibility to protect the sensitive data that powers them. The 2025 HIPAA Security Rule update represents the most extensive regulatory change in two decades. It introduces mandatory controls around multi-factor authentication, encryption, continuous vulnerability testing, and incident response.
These requirements arrive amid an environment where breaches cost healthcare organizations an average of $10.22 million, according to IBM’s latest Cost of a Data Breach Report. This is why compliance cannot be treated as mere documentation and must be built into the technology itself.
At Intellivon, we create HIPAA-compliant AI health platforms. Our platforms combine security engineering, explainable AI, and resilient cloud architectures into compliant, scalable ecosystems that protect trust and drive measurable impact. This blog explores that journey, detailing how we create these scalable enterprise-ready platforms from the ground up.
Key Takeaways of the HIPAA-Compliant AI Health Platform Market
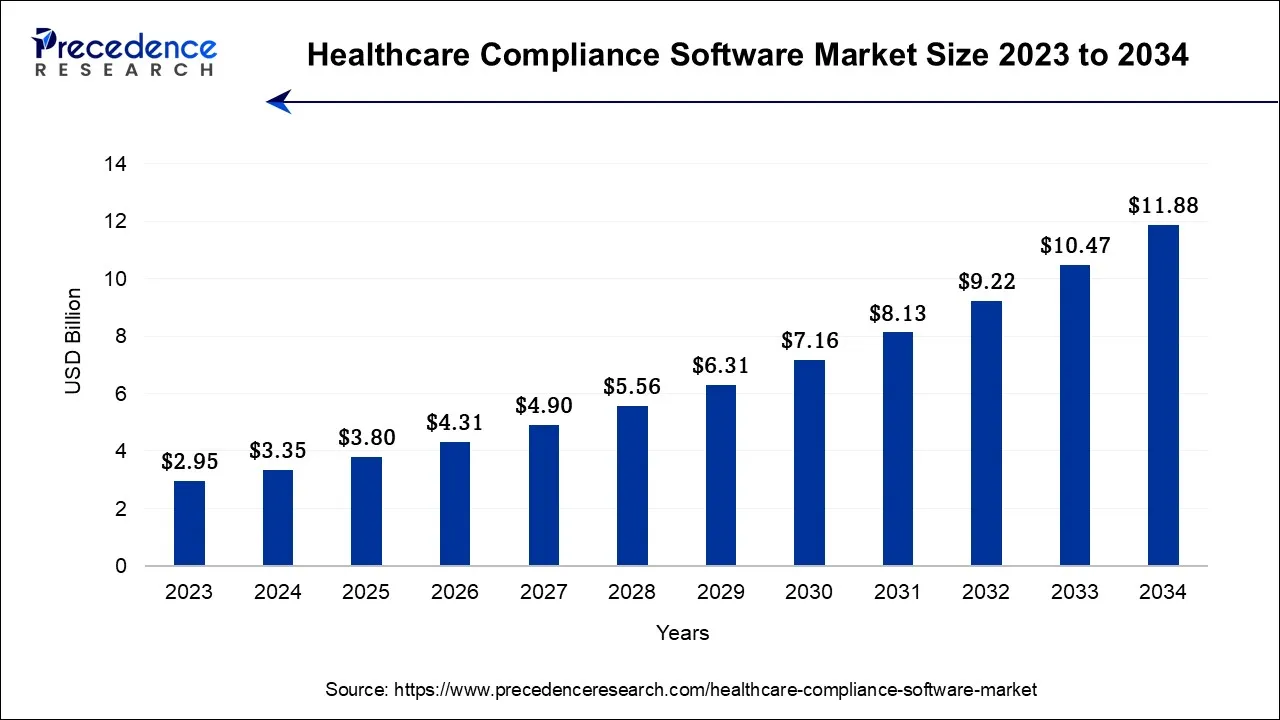
The global healthcare compliance software market is undergoing rapid transformation, fueled by stricter regulations and AI integration. Valued at USD 3.35 billion in 2024, the market is projected to reach USD 11.88 billion by 2034, expanding at a robust CAGR of 13.5%.
This growth reflects the healthcare sector’s mounting need for solutions that ensure privacy, automate governance, and align with emerging frameworks like the 2025 HIPAA Security Rule. As digital health ecosystems grow more interconnected, enterprises are investing in compliance-first AI platforms to mitigate legal, operational, and reputational risks.
Market Insights
- Regional Outlook: North America held the dominant 52% revenue share in 2023, driven by mature regulatory frameworks. The Asia-Pacific region is forecast to grow fastest during 2024-2034 as healthcare IT adoption accelerates.
- By Product Type: The cloud-based segment accounted for 56.3% of revenues in 2023, reflecting a shift toward scalable SaaS platforms. Meanwhile, on-premises systems are projected to post a 15.8% CAGR, supported by organizations seeking enhanced data control.
- By Category: Policy and procedure management tools led with a 25.4% share, while medical billing and coding compliance solutions are expected to grow fastest, supported by automation and claim-accuracy mandates.
- By End-use: Hospitals captured the largest 59% market share in 2023, while specialty clinics are set to expand at the quickest pace as they digitize workflows and adopt cloud-native compliance platforms.
Key Market Drivers
- Heightened enforcement of global healthcare data privacy regulations.
- Escalating healthcare data breaches and cyberattacks are accelerating compliance spending.
- Expanding use of EHRs and telemedicine, increasing exposure points for ePHI.
- Integration of AI and machine learning enables real-time risk detection and compliance automation.
Growth Opportunities
- Surge in cloud-based and AI-powered compliance ecosystems that reduce manual oversight.
- Demand for specialty-specific compliance modules tailored to clinical domains.
- Expansion into emerging markets with evolving healthcare IT infrastructures and digital health reforms.
As global compliance pressures intensify, healthcare enterprises can no longer treat data protection as an isolated function. The next decade will favor organizations that design AI platforms around HIPAA compliance from inception, embedding privacy, security, and resilience into their digital core to sustain both innovation and trust.
What Are HIPAA-Compliant AI Health Platforms?
A HIPAA-compliant AI health platform is software that uses artificial intelligence to process and analyze patient data securely. It’s built to meet all privacy, security, and auditing requirements of the Health Insurance Portability and Accountability Act (HIPAA).
The goal is to ensure every use of AI, whether for diagnosis, analytics, or automation, keeps patient data safe, confidential, and traceable at every step.
How These Platforms Work
These platforms integrate seamlessly with existing healthcare systems, like EHRs, lab databases, or imaging tools, and use AI models to deliver insights, automate documentation, and support clinical decisions.
All data flowing through the system is encrypted, access-controlled, and continuously monitored. Each action, whether data access, prediction, or update, is logged automatically, creating full transparency for compliance teams.
For instance, Epic Systems’ Cognitive Computing Platform runs predictive algorithms within its EHR ecosystem to flag patient risks in real time, maintaining HIPAA compliance through encryption, access control, and audit trails.
Understanding How AI Works in HIPAA-Compliant Health Platforms
Artificial intelligence can reshape healthcare, but it must operate within strict compliance boundaries. In HIPAA-compliant platforms, AI works inside a controlled, auditable, and secure ecosystem. Every layer, from data ingestion to prediction, is designed to keep patient information confidential, traceable, and regulator-ready.
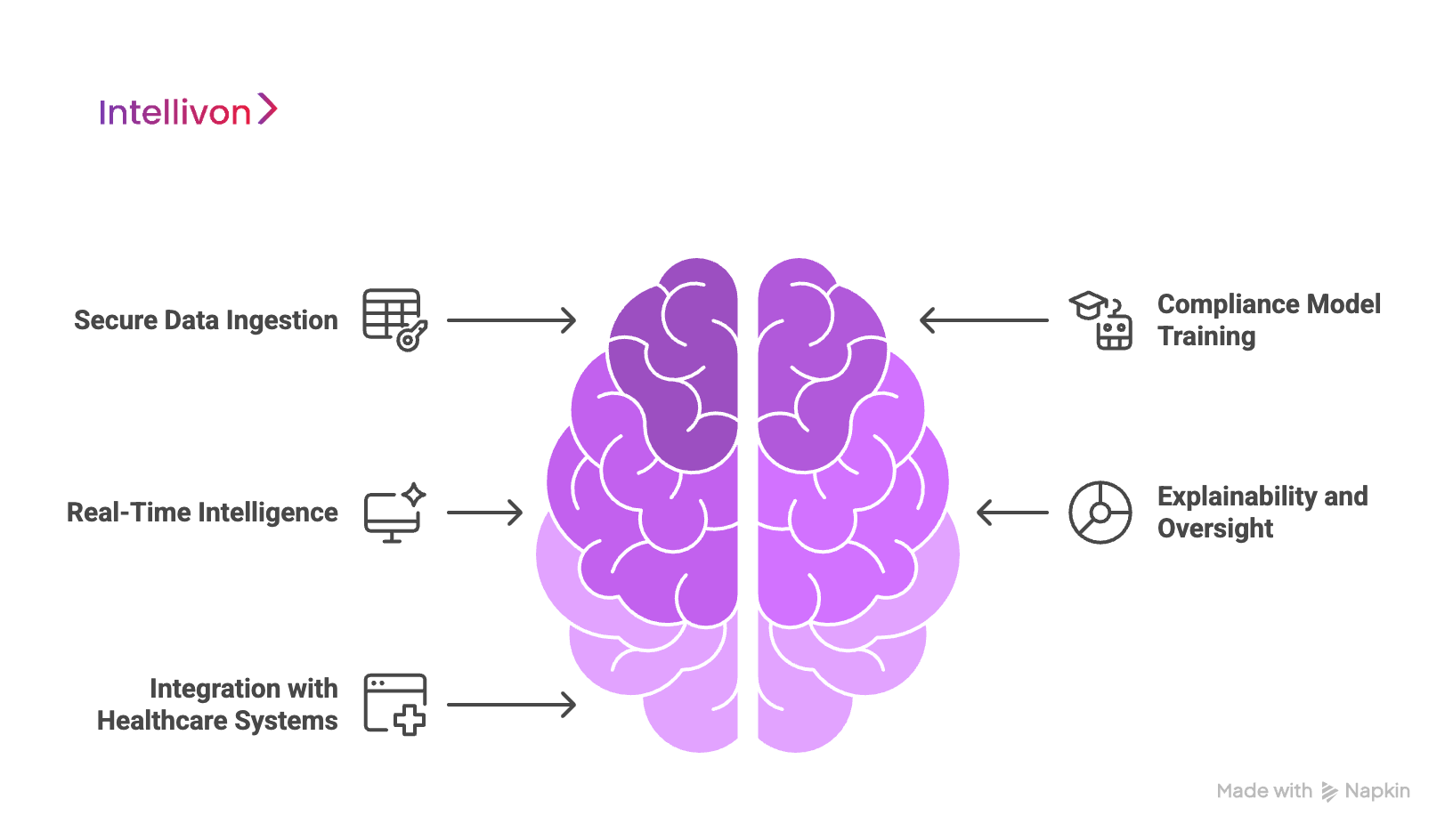
1. Secure Data Ingestion
The process begins with connecting EHRs, imaging systems, lab records, or IoMT devices. All incoming data is encrypted, validated, and checked for integrity before entering the AI environment.
De-identification or pseudonymization ensures that personally identifiable information never leaves protected zones. This reduces exposure risk while maintaining data utility for AI-driven insights.
2. Compliance Model Training
AI models are trained only within restricted environments, either on-premise or in HIPAA-eligible cloud clusters. During each training cycle, datasets, parameters, and outcomes are logged automatically for audit readiness.
Access is strictly role-based, and usage is monitored through compliance dashboards. This guarantees that algorithms learn from accurate, approved, and fully traceable data.
3. Real-Time Intelligence
Once deployed, the AI engine processes data in real time to predict risks or suggest next steps. It may flag clinical anomalies, recommend workflows, or automate routine documentation.
All inferences occur within secure execution zones, with full encryption maintained throughout. Every prediction, model call, or user interaction is recorded in immutable audit logs.
4. Explainability and Continuous Oversight
AI in healthcare must be explainable by design. Each system output includes confidence scores, rationale tracing, and data provenance visibility. Compliance teams and clinicians can view why a model made a specific recommendation.
Continuous monitoring tools also track bias, drift, and anomalies, triggering alerts or revalidation when needed.
5. Integration With Existing Healthcare Systems
HIPAA-compliant AI platforms integrate seamlessly with hospital systems using FHIR and HL7 APIs. This allows clinicians and administrators to view insights directly within familiar EHR interfaces.
No sensitive data is exported or stored outside approved environments. As a result, compliance and workflow efficiency evolve in tandem.
AI’s real power in healthcare lies in trust, and not just intelligence. HIPAA-compliant platforms turn data-driven innovation into something accountable, where every action is secure, explainable, and auditable.
Why Compliance Defines the Future of AI Health Platforms
HIPAA compliance has evolved from a regulatory checkbox to the core engineering principle of healthcare AI. According to IBM’s 2025 Cost of a Data Breach Report, the average U.S. breach cost reached $10.22 million, the highest across any industry.
These breaches disrupt operations, drain budgets, and erode patient trust, three factors that no AI platform can afford to overlook.
The Change Healthcare cyberattack illustrated this risk at scale. A single missing multi-factor authentication control exposed 192.7 million individuals’ records, crippling EHR, imaging, and payment workflows across 759 hospitals. This remains the largest exposure of protected health information ever recorded.
Regulatory Changes Are Redefining “Compliance”
The proposed 2025 HIPAA Security Rule update removes the “addressable” category, making MFA, encryption, and vulnerability testing mandatory for all covered entities and business associates.
Simultaneously, the FDA’s AI/ML Device Guidance requires threat modeling, patch pipelines, and SBOM documentation before AI systems reach production. This convergence pushes healthcare enterprises to design “security by architecture,” not “security by audit.”
Why Privacy and Performance Must Align
AI platforms must secure ePHI while maintaining real-time analytics and model precision. Encryption, segmentation, and role-based access should be native to data pipelines, and not bolted on after deployment. This balance ensures compliant intelligence without throttling algorithmic performance or clinical accessibility.
1. Continuous Governance
Compliance today demands living documentation. HIPAA-aligned systems must maintain evolving risk analyses, asset inventories, and workforce training logs that reflect every new release.
Regulators now expect governance to move at the same velocity as DevOps cycles, proving compliance isn’t static but continuous.
2. Verification Is the New Proof of Compliance
Healthcare still records the longest breach lifecycle, with an average of 279 days to detect and contain incidents.
To shorten that window, enterprises must embed annual penetration tests, quarterly vulnerability scans, and real-time audit logging into their platforms. These validation steps create the verifiable evidence regulators increasingly require.
3. Resilience Defines Patient Safety
Downtime now equals clinical risk. A July 2024 technology outage affected at least 759 U.S. hospitals, with over 200 losing access to imaging and fetal-monitoring systems.
Hospitals lose an average of $7,500 per minute during downtime caused by cyberattacks or IT failures.
Future-ready AI health platforms must design for recovery, like immutable backups, geographic redundancy, and 72-hour restoration, aligning with proposed HIPAA resilience expectations.
HIPAA compliance is the enabler of trustworthy AI. As machine learning becomes central to diagnostics and decision support, compliance must function as an engineering discipline.
Enterprises that embed regulatory logic into their architecture will gain the confidence of patients, regulators, and partners, and define what ethical, resilient, and scalable AI in healthcare truly means.
Key Risks When Building AI Health Platforms Without Compliance
Building AI healthcare systems without integrating compliance from the start creates long-term liabilities that extend far beyond regulatory penalties. For enterprises, these risks touch revenue, trust, and operational stability. Each unaddressed compliance gap eventually becomes a business risk that scales with every deployment.
1. Rising Cost of Non-Compliance
The financial consequences of a HIPAA breach can be severe. According to the U.S. Department of Health and Human Services (HHS), OCR settlements and penalties reached $39.8 million in 2024 alone.
Beyond fines, the average cost of a single healthcare data breach now stands at $10.22 million (IBM, 2025). These costs include detection, remediation, lost business, and legal exposure.
For AI-driven systems, the cost of a single misconfigured API or unsecured model endpoint can multiply quickly, especially when thousands of records are processed in seconds.
2. Breach Complexity and Data Sensitivity
AI systems amplify both data volume and vulnerability. Machine learning models often ingest structured and unstructured data from multiple systems, like EHRs, imaging archives, IoT sensors, and cloud applications. Without precise data lineage tracking, even small missteps can expose personally identifiable information (PII).
Once ePHI is compromised, tracing its path through the system becomes difficult. The lack of explainability or proper audit trails can delay investigations and escalate legal risk. As models become more autonomous, enterprises must build observability into every data transaction to maintain control.
3. The Change Healthcare Breach
The Change Healthcare cyberattack remains one of the clearest demonstrations of compliance failure at scale.
In 2024, attackers exploited a missing multi-factor authentication (MFA) control in a Citrix environment, gaining access to sensitive payment and health data. The breach disrupted 759 hospitals across the United States and exposed over 192 million patient records.
This incident showed that a single overlooked safeguard could collapse entire healthcare networks.
4. Operational Downtime and Workflow Disruption
Compliance gaps also lead to extended downtime during remediation. A 2024 JAMA Network Open study found that healthcare outages caused by cyber incidents can paralyze critical systems for five days or longer, directly affecting patient care.
In AI-enabled ecosystems, downtime halts predictive workflows, imaging analytics, and clinical automation, essentially freezing decision-making in environments that depend on real-time intelligence.
5. Loss of Trust and Market Position
Compliance violations erode brand credibility faster than almost any other factor. In healthcare, where trust underpins every data exchange, reputational recovery can take years.
Hospitals and insurers increasingly vet AI vendors for HIPAA, GDPR, and HITRUST certifications before integration. One failed audit or publicized breach can disqualify a vendor from procurement pipelines for entire contract cycles.
Compliance is a prerequisite for sustainable innovation. As AI becomes the operational core of healthcare systems, each design choice must account for governance, privacy, and auditability.
Key Features of a HIPAA-Compliant AI Health Platform Must Have
A compliant AI platform is intelligently designed to translate regulation into performance, scalability, and trust. Each feature must bridge technology, governance, and business value while ensuring compliance becomes a living process rather than a static checklist.
1. Automated Compliance Monitoring
Real-time dashboards give visibility into every compliance metric, like access logs, encryption status, and data transfer activities. AI-driven analytics detect anomalies across APIs, endpoints, and workflows, alerting administrators to potential breaches before they escalate.
By automating these checks, organizations replace reactive audits with proactive governance. Executives gain measurable insight into compliance posture across systems and departments.
2. Data Governance Modules
Patient consent management is a cornerstone of HIPAA compliance. Platforms must log, track, and enforce consent rules dynamically, across EHRs, cloud services, and AI pipelines.
Integration with FHIR and HL7 ensures consent data flows seamlessly between care systems, while automated access enforcement prevents unapproved use of patient information. This safeguards both data rights and institutional credibility.
3. Explainable AI (XAI)
Every prediction made by AI in healthcare must be explainable to humans. Frameworks like SHAP and LIME make it possible to trace how algorithms reach conclusions, providing both clinicians and auditors with interpretability.
This transparency builds accountability, helps identify bias, and allows models to pass regulatory review faster, an essential factor in scaling AI deployments across clinical environments.
4. Role-Based Access
Access governance defines who can view or modify ePHI. Role-based access control (RBAC) ensures that users only see what they need to perform their duties.
When integrated with enterprise IAM tools such as Okta, Azure AD, or AWS IAM, these systems automatically adjust privileges as roles change, aligning perfectly with HIPAA’s Minimum Necessary Access standard.
5. Data De-Identification
AI models thrive on large datasets, but compliance demands privacy. De-identification pipelines scrub identifiable details from patient data through tokenization, masking, and synthetic data techniques.
This approach enables model training and validation on realistic datasets without exposing PHI, maintaining alignment with HIPAA and GDPR requirements for data minimization and pseudonymization.
6. Audit Trails and Reporting Systems
HIPAA compliance requires detailed activity logs that prove control effectiveness. Automated audit trails capture every access, modification, and system change, storing immutable records that can be retrieved instantly during audits.
Integrating these logs with tools such as Splunk or the Elastic Stack enables enterprises to generate compliance reports on demand, reducing audit preparation time and ensuring traceability.
7. API Security Frameworks
Secure data exchange is the backbone of modern healthcare AI. APIs using FHIR, SMART on FHIR, and OAuth 2.0 protocols enable interoperability without compromising data privacy.
API gateways must enforce encryption, payload validation, and rate limiting to prevent unauthorized access. A strong API governance framework ensures compliance remains intact even in multi-vendor environments.
8. Business Associate Agreement (BAA)
Every vendor, cloud provider, or analytics partner handling ePHI must have a signed Business Associate Agreement (BAA). Managing these manually across dozens of integrations is error-prone.
HIPAA-compliant AI platforms now automate BAA tracking, renewal alerts, and compliance verification, ensuring every partner remains within regulatory alignment throughout the contract lifecycle.
9. DevSecOps Integration
Embedding DevSecOps-based security and compliance into the CI/CD pipeline ensures no code, model, or configuration goes live without validation. Tools such as Snyk, Prisma Cloud, or AWS Security Hub automate vulnerability scanning and policy checks.
This integration shifts compliance left, catching misconfigurations during development instead of after deployment, reducing downtime and audit remediation costs.
A HIPAA-compliant AI platform is built not only to protect but to prove protection at scale.
How We Create HIPAA-Compliant AI Health Platforms
We design AI healthcare ecosystems where compliance is embedded in the foundation. Our approach combines domain expertise, advanced architecture, and regulatory intelligence to deliver systems that stand up to both technical and legal scrutiny. Here’s how we build platforms that not only meet HIPAA requirements but redefine how enterprises approach healthcare AI.
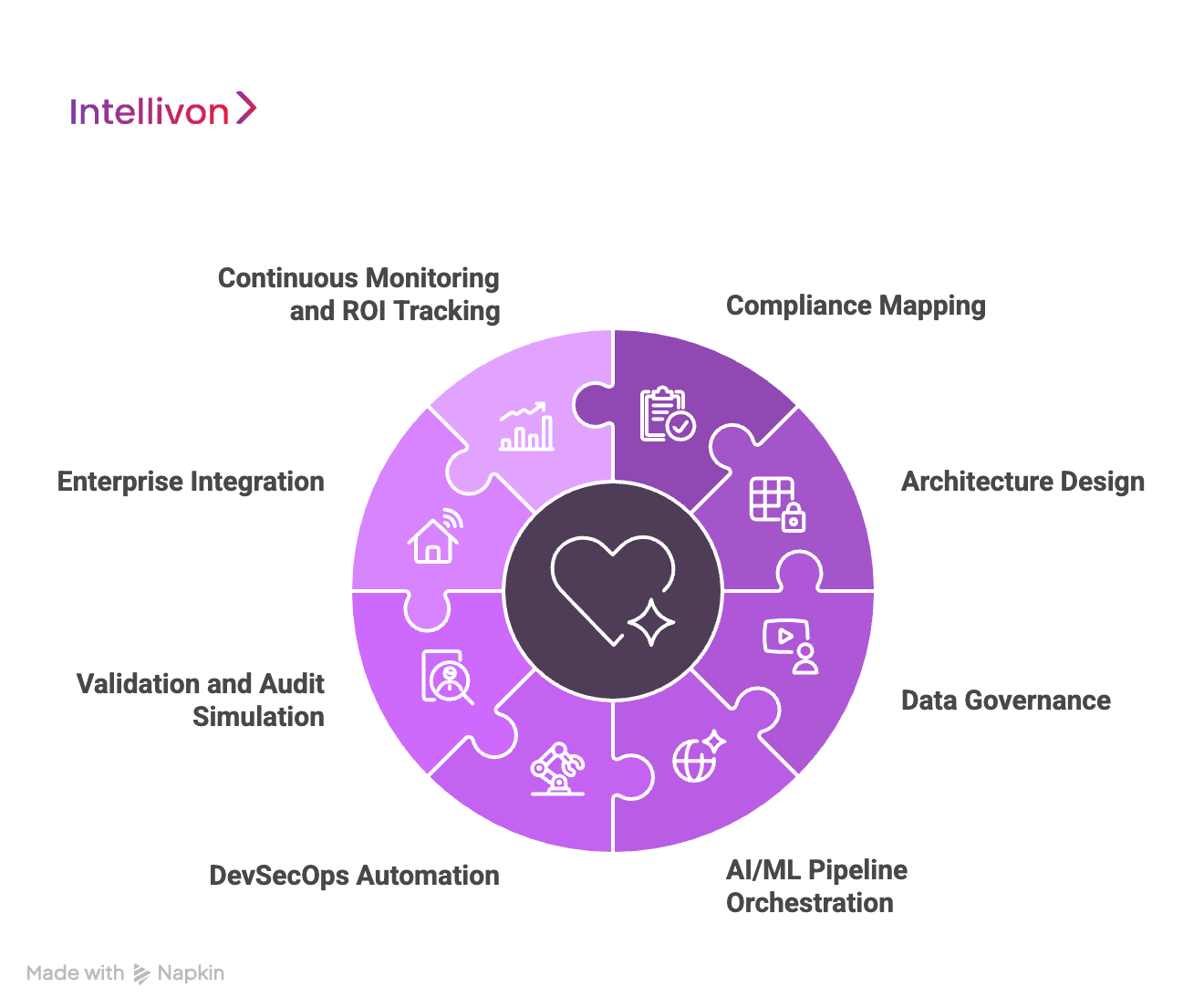
1. Compliance Mapping
Every engagement begins with a full compliance landscape assessment. Our teams audit current workflows, data pipelines, and infrastructure against HIPAA’s Privacy and Security Rules, NIST SP 800-66r2, and upcoming 2025 amendments.
The result is a compliance readiness blueprint, which is a detailed matrix mapping organizational controls, vulnerabilities, and modernization priorities. This document anchors every subsequent design choice, ensuring regulatory alignment before any code is written.
2. Architecture Design
Once the compliance gaps are mapped, we translate them into technical architecture. Each layer, which includes identity, storage, APIs, and AI pipelines, is designed with regulatory logic built in.
We apply zero-trust network principles, isolated PHI zones, and encryption-first frameworks using tools like AWS Lake Formation, HashiCorp Vault, and Kubernetes-native compliance policies. The goal is to make compliance enforceable by design, not dependent on manual oversight.
3. Data Governance
Patient trust starts with data discipline. We establish data lineage, consent tracking, and access auditability through custom governance modules integrated into FHIR and HL7 environments.
Every dataset entering the AI pipeline is verified for source authenticity, de-identification, and consent scope. These checks ensure that AI models never learn from unapproved or improperly tagged PHI, maintaining traceability for audits.
4. AI/ML Pipeline Orchestration
Our machine learning environments operate under compliance-aware orchestration. We integrate MLflow, Kubeflow, and AWS SageMaker with automated access control, model explainability, and risk scoring.
Every model version is tracked for data origin, bias evaluation, and compliance integrity. By enforcing policy-as-code, we guarantee that no model moves from experimentation to production without passing both performance and compliance gates.
5. DevSecOps Automation
Compliance must evolve with every deployment. We embed HIPAA checks directly into the CI/CD pipeline through automated scanners like Snyk, Prisma Cloud, and Terraform Sentinel.
This ensures that infrastructure-as-code, data connectors, and model updates are validated before release. Our systems continuously scan for drift, misconfigurations, and unapproved data flows, keeping the platform perpetually audit-ready.
6. Validation and Audit Simulation
Before any production release, we conduct multi-layer testing that goes beyond QA. Our security teams run penetration tests, vulnerability assessments, and audit simulations aligned with HHS OCR protocols.
We validate encryption strength, data flow boundaries, and role-based permissions under simulated breach scenarios. This process ensures real-world readiness, proving that the platform not only works but holds up under scrutiny.
7. Enterprise Integration
Compliance has no value if systems can’t communicate securely. We integrate AI platforms with existing EHRs, LIS, PACS, and payer systems using FHIR APIs, HL7, and SMART on FHIR frameworks.
Each connection is governed by encryption, scoped tokens, and consent validation to maintain trust across every touchpoint. The result is interoperability without exposure, intelligence that moves seamlessly while remaining compliant.
8. Continuous Monitoring and ROI Tracking
After deployment, compliance management becomes continuous. We implement real-time observability through SIEM systems like Splunk and Datadog, automated incident response workflows, and executive dashboards for compliance KPIs.
Each platform is benchmarked on uptime, breach risk reduction, and cost efficiency. This gives enterprise leaders tangible ROI on compliance investments, transforming regulatory adherence from a cost center into a measurable business advantage.
At Intellivon, every AI healthcare platform we build stands on the intersection of compliance, scalability, and trust. By embedding HIPAA alignment into the development lifecycle, we help global healthcare enterprises move faster, mitigate risk, and scale responsibly in one of the world’s most regulated industries.
Cost to Create a HIPAA-Compliant AI Platform
At Intellivon, the priority is to help healthcare enterprises build AI health platforms that are compliant, resilient, and enterprise-ready. Pricing is aligned with business goals, regulatory obligations, and scalability expectations, ensuring investments directly support patient safety, operational efficiency, and long-term data trust.
When initial budgets are constrained, our team refines the project scope collaboratively, without compromising HIPAA/GDPR alignment, FDA/EU AI Act readiness, or enterprise-grade reliability. Every build is structured to balance cost efficiency with sustainable compliance and measurable ROI.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Compliance Alignment | Requirement analysis, HIPAA mapping, regulatory scoping (FDA, EU AI Act), KPI definition | $6,000 – $12,000 |
| Architecture & Secure Design | Designing multi-layered infrastructure for PHI handling, encryption, and resilience | $8,000 – $15,000 |
| Data Integration & Interoperability | Integrating EHRs, IoMT, claims, and lab data using HL7/FHIR standards | $10,000 – $20,000 |
| AI Intelligence & Decision Layer | Building predictive models, clinical logic, explainable AI, and compliance dashboards | $12,000 – $25,000 |
| Security & Privacy Engineering | Encryption, access control, de-identification, continuous monitoring, and breach simulation | $8,000 – $15,000 |
| Platform Development & Interfaces | Role-based dashboards, analytics consoles, reporting and audit modules | $12,000 – $25,000 |
| Testing & Validation | HIPAA compliance testing, penetration testing, and model validation | $6,000 – $10,000 |
| Deployment & Scaling | Cloud rollout, monitoring setup, high availability, and elastic scaling | $6,000 – $12,000 |
Total Initial Investment Range: $50,000 – $150,000
Ongoing Maintenance & Optimization (Annual): 15–20% of initial build cost
Hidden Costs Enterprises Should Plan For
- Integration Complexity: Legacy EHRs and fragmented provider systems often need additional middleware and FHIR connectors.
- Compliance Overhead: HIPAA, GDPR, FDA, and EU AI Act require periodic audits, risk assessments, and documentation updates.
- Data Governance: Cleaning, mapping, and curating mixed-format healthcare data consume recurring resources.
- Cloud Infrastructure Spend: Operating real-time AI pipelines and compliance dashboards requires efficient compute scaling strategies.
- Change Management: Training staff and compliance officers on new workflows adds measurable transition costs.
- Model Drift & Monitoring: Predictive models must be retrained and revalidated to maintain accuracy and compliance.
Best Practices to Avoid Budget Overruns
Drawing from Intellivon’s enterprise delivery experience, the following principles consistently help healthcare organizations achieve predictable costs and faster go-live:
- Start with Focused Scope: Pilot within one specialty or department, measure ROI, then scale system-wide.
- Embed Compliance from Day One: Align architecture with HIPAA, GDPR, and FDA/EU AI Act standards early to avoid rework.
- Adopt Modular Design: Reuse secure pipelines, ML components, and dashboards across care units or markets.
- Optimize Cloud Spend: Blend batch and real-time analytics to balance cost with processing efficiency.
- Ensure Continuous Observability: Monitor uptime, latency, and compliance metrics through automated dashboards.
- Iterate for Longevity: Refine security controls, workflows, and models regularly to maintain resilience and adaptability.
Request a tailored proposal from Intellivon’s healthcare AI, and you’ll receive a roadmap aligned with your budget, compliance priorities, and growth vision.
Top 5 HIPAA-Compliant AI Healthcare Platforms in the USA
As healthcare AI adoption accelerates, only a few platforms truly meet HIPAA’s strict security and governance standards. These five platforms set the current benchmark for secure, scalable, and enterprise-ready AI healthcare solutions.
1. Hathr.AI
Hathr.AI is built on AWS GovCloud (FedRAMP High) and focuses on automating document-heavy healthcare workflows.
It helps providers extract insights from unstructured clinical data while keeping every file encrypted and access-controlled.
How they use AI: Hathr.AI uses large language models (LLMs) trained on clinical text to summarize patient notes, detect missing information, and automate documentation tasks. Its models are fine-tuned for healthcare terminology, delivering faster outcomes without ever compromising patient privacy.
2. BastionGPT
BastionGPT is a HIPAA-compliant conversational AI platform designed for clinicians, researchers, and medical scribes. It operates in secure, private environments with full BAA coverage and on-prem or virtual private cloud (VPC) hosting.
How they use AI: BastionGPT uses healthcare-tuned generative AI to transcribe consultations, create encounter summaries, and help clinicians complete documentation faster. It anonymizes PHI before processing and records every prompt and output for compliance tracking, combining speed with transparency.
3. CompliantChatGPT
CompliantChatGPT is built for healthcare networks and research teams that need secure AI chat interfaces for clinical data. It maintains HIPAA compliance through token-based access, encrypted storage, and continuous activity monitoring.
How they use AI: The platform uses natural language processing to analyze lab reports, summarize charts, and support patient communication. All AI interactions are logged, audited, and governed, making it a trusted blueprint for compliant, conversational healthcare AI.
4. Keragon
Keragon is a no-code healthcare automation platform built to connect EHRs, telehealth systems, and patient management tools under one secure framework. It’s fully HIPAA-compliant, with automatic BAA provisioning and encrypted workflow logging.
How they use AI: Keragon embeds AI helpers within its automation engine. Users can describe workflows in plain language, and the platform automatically builds triggers, rules, and logic steps. This enables healthcare teams to automate repetitive processes without writing code or violating compliance.
5. Healthie
Healthie powers over 40,000 U.S. providers with a HIPAA-secure platform for telehealth, patient management, and EHR operations. It’s designed for scalability, supporting solo practices and enterprise networks alike.
How they use AI: Healthie’s AI layer automates charting and note generation through its “AI Scribe” feature. It also analyzes data patterns to recommend workflow improvements and optimize patient engagement, helping providers save time while staying compliant.
Each of these platforms proves that compliance and innovation can progress together. For enterprises, they serve as blueprints for designing AI ecosystems that are secure, interoperable, and regulator-ready from day one.
Conclusion
Building a HIPAA-compliant AI health platform protects patient trust while driving real innovation. As AI becomes central to diagnostics, care delivery, and operations, compliance must move from an afterthought to the foundation of every system. The journey is complex and deeply technical, but it’s not one you should take alone.
Choosing the right technology partner means working with a team that understands both healthcare realities and regulatory nuance. The right partner helps you build a future where data, trust, and care can coexist securely.
Build Your HIPAA-Compliant AI Platform with Intellivon
At Intellivon, we design HIPAA-compliant AI health platforms that are secure, explainable, and built to scale across enterprise healthcare ecosystems. Each implementation aligns with the way hospitals, research institutions, and payer networks actually operate, bridging clinical intelligence with compliance confidence.
Our platforms unify predictive analytics, data governance, and resilience engineering into one enterprise-grade framework. You get actionable intelligence without compromising privacy, trust, or regulatory integrity.
Why Partner With Intellivon?
- Tailored Enterprise Platforms: Every build is aligned with your clinical workflows, governance frameworks, and risk posture to deliver measurable business and patient impact.
- Proven Healthcare Expertise: With 11+ years of delivery experience, 500+ AI solutions, and 200+ domain specialists, we’ve helped global healthcare enterprises transform operations securely.
- Compliance-First Architecture: Designed for full alignment with HIPAA, GDPR, FDA SaMD, and EU AI Act frameworks from day one, ensuring audit readiness and regulator trust.
- Future-Ready Design: Cloud-native, API-first systems integrate seamlessly with EHRs, PACS, LIMS, and payer infrastructure through hardened FHIR and HL7 gateways.
- Explainable and Transparent AI: Every prediction is traceable through explainability dashboards, rationale mapping, and audit logs for clinician and regulator review.
- Security and Reliability: Multi-layered encryption, zero-trust identity frameworks, and immutable event logs protect data integrity while maintaining uptime during incidents.
- Interoperability at Scale: Unified data pipelines, scoped access tokens, and continuous observability ensure smooth and compliant information exchange across all healthcare systems.
- Transparent Value Tracking: Executive dashboards track uptime, data integrity, ROI, and compliance metrics in real time, so leadership can monitor impact, not just implementation.
Book a free strategy call today to explore how Intellivon can help you build a secure, compliant, and scalable AI health platform that enhances care delivery, protects patient trust, and accelerates digital transformation.
FAQs
Q1. What are the key HIPAA requirements for AI health platforms?
A1. HIPAA requires every AI health platform to keep patient data private, secure, and auditable. That means using encryption, multi-factor authentication, and access control to protect ePHI. All data used for AI, whether for training or predictions, must be de-identified and traceable. Healthcare organizations and vendors also sign Business Associate Agreements (BAAs) to define who’s responsible for protecting that data.
Q2. How much does it cost to build a HIPAA-compliant AI system?
A2. Most HIPAA-compliant AI systems cost between $50,000 and $150,000 to build. The price depends on the number of integrations, data complexity, and security depth. Enterprises usually spend another 15–20% annually on monitoring, retraining, and audits. Investing in compliance early always saves money compared to fixing gaps later.
Q3. What tools help automate HIPAA compliance?
A3. Many tools now simplify compliance work. Drata, Vanta, and Tugboat Logic help collect evidence and generate audit reports automatically. For infrastructure, AWS Config and Prisma Cloud monitor system health and flag risks. In AI workflows, MLflow and Kubeflow track data lineage so teams can prove every model meets HIPAA standards.
Q4. What certifications strengthen HIPAA compliance?
A4. Certifications like SOC 2, HITRUST, and ISO 27001 show a company takes security seriously. They prove that systems follow strong privacy, encryption, and data-handling practices. For healthcare enterprises, these certifications provide extra assurance that their AI vendors meet industry-wide compliance expectations.
Q5. How do hospitals verify vendor HIPAA compliance before integration?
A5. Hospitals perform detailed vendor reviews before any integration. They look for signed BAAs, recent SOC 2 or HITRUST reports, and results from security audits. Vendors also need to prove they encrypt data, control access, and have an incident-response plan. This process ensures every connected platform protects patient data and meets regulatory standards from day one.





