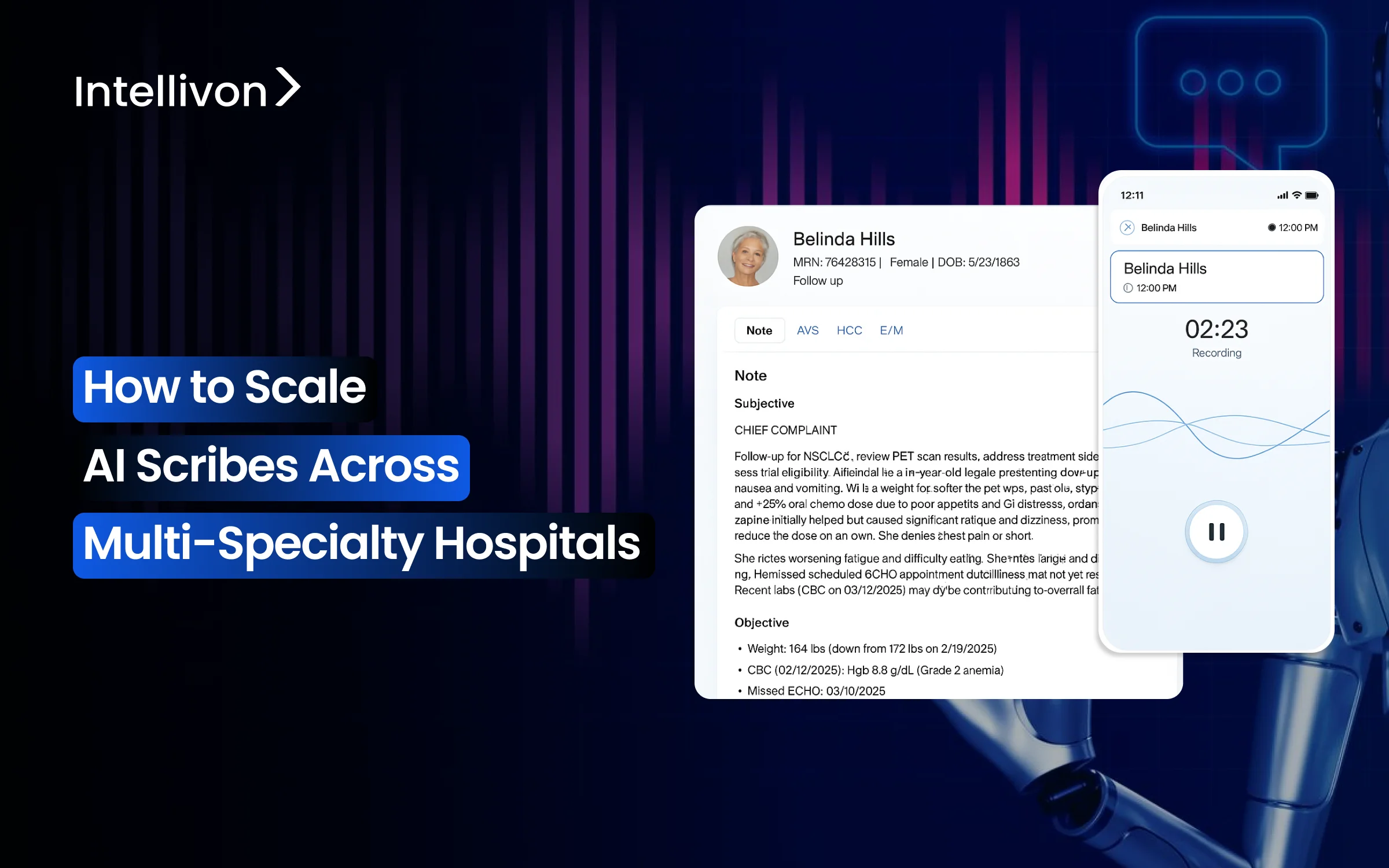
Documentation challenges hurt hospital efficiency, and multi-specialty environments face an even tougher situation. Here, each department uses its own clinical language, has different documentation needs, and follows unique workflows. Many hospitals try using AI scribes in one department but find that the solution does not work well when applied to other specialties. To successfully scale AI scribes throughout multi-specialty hospitals, organizations need platforms that fit the complexity of each department while keeping things consistent. These systems must capture specific terminology, integrate with different EHR templates, manage various encounter types, and provide structured documentation that meets the standards of each department.
At Intellivon, we scale AI scribes in multi-specialty hospitals by developing enterprise platforms that fit the needs of each department from the start. Our ambient documentation systems handle specialty-specific terms in real time, work reliably in noisy clinical settings, fit smoothly with current EHR workflows, and adhere to strict regulations in telehealth and in-person visits. This blog explains how we strategically scale AI scribes across various multi-specialty hospital departments.
Key Takeaways of the AI Scribe Platforms Market
HTF Market Intelligence reports that AI-enabled clinical documentation is becoming one of the fastest-growing segments in digital health. Ambient AI scribes function as advanced intelligent clinical documentation platforms. The market, valued at just over USD 3 billion today, is forecasted to surge past USD 26 billion, supported by a projected 24 percent annual growth rate.
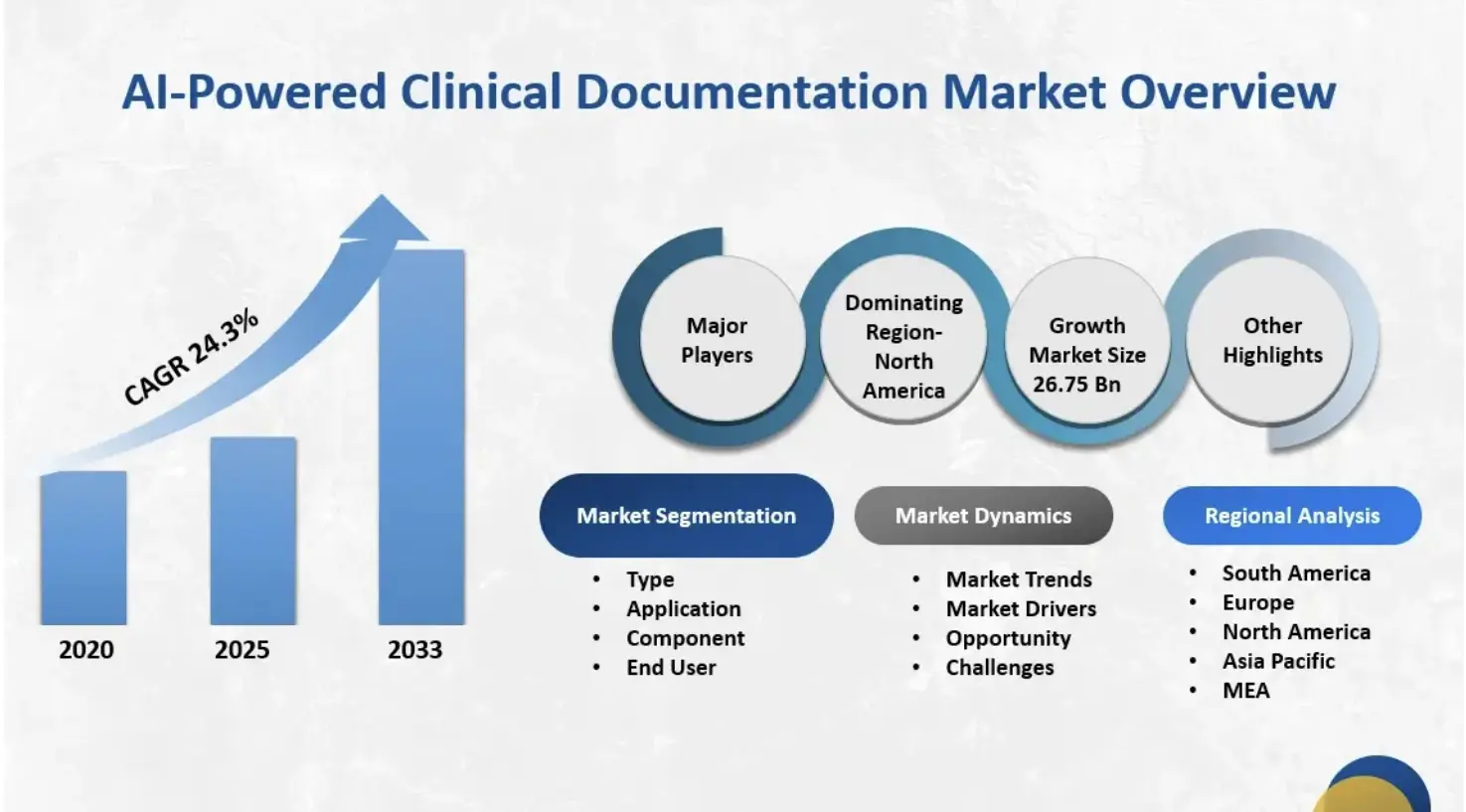
Key Market Insights:
- The ambient scribe category is the fastest-growing segment in clinical AI, generating an estimated $600 million in annual revenue in 2025.
- It exceeds revenue from any other single clinical AI application, growing 2.4x year-over-year.
- The global AI medical scribe software market reached approximately $1.12 billion in 2024.
- Forecasts suggest a compound annual growth rate of about 20.4% through 2033.
Adoption Rates and Penetration
- By the end of 2025, an estimated 30%–60% of healthcare providers will be using ambient scribe tools.
- Within large health systems, adoption is already near 35%.
- Market analysts expect adoption to level off at around 40% over the next three years as early demand stabilizes.
Key Drivers of Enterprise Adoption
- Burnout mitigation remains the primary driver influencing purchasing decisions.
- Additional motivators include improved care quality, revenue optimization, and faster deployment compared to human scribe models.
- Case studies show ambient scribes can save providers more than eight hours per week.
- Some systems report up to 75% lower documentation costs compared to traditional human scribe programs.
- These savings are central to ROI justification for enterprise buyers.
Competitive Landscape and Differentiators
- The U.S. market includes more than 60 vendors.
- Major EHR providers like Nuance (Microsoft), Oracle, and Epic control roughly 33% of the market.
- AI-native companies such as Abridge hold around 30%, while Ambience has close to 13%.
- Growing competition is pushing vendors to expand from “just scribing” to broader clinical and administrative automation.
- Many platforms now bundle documentation, coding support, compliance workflows, and revenue cycle automation.
Investment and Market Maturity
- More than $975 million has been invested in ambient AI scribe companies in 2025.
- These investments show strong confidence in the technology, but also indicate a crowded and rapidly maturing landscape.
- Analysts expect widespread saturation in ambulatory healthcare within the next 24–36 months.
Healthcare enterprises that secure ambient scribe workflows protect patient trust and shield themselves from legal, financial, and reputational damage. Strong safeguards turn automation into a sustainable advantage, not a cybersecurity risk.
How AI Scribe Platforms Work Across Multi-Specialty Hospitals
A scalable AI scribe platform must work the same way in every department, even when each specialty documents care differently. It should understand diverse clinical conversations, adapt to different environments, and produce consistent notes across the entire hospital. When a single platform supports all departments reliably, hospitals can expand usage without redesigning workflows.
1. Conversation Capture
A scalable platform captures natural conversations in clinics, inpatient units, and virtual visits. It identifies speakers, tracks sudden topic shifts, and stays accurate in noisy or crowded rooms.
This creates a stable baseline for emergency medicine, primary care, and specialty clinics. When the platform performs consistently across these conditions, hospitals can extend usage without retraining staff. This consistency is one of the strongest indicators of platform readiness for enterprise scale.
2. Specialty Language
A unified platform must understand terminology used in different specialties and interpret it correctly. Cardiology discussions focus on diagnostic reasoning, while pediatrics often involves parents and children speaking together. Oncology requires careful interpretation of long treatment plans.
When the system handles these variations naturally, each department receives drafts that match its expectations. This reduces edits and builds trust across the hospital.
3. Note Structuring
A scalable platform generates structured notes that reflect the correct format for each encounter type. Surgical teams need clear pre-operative and post-operative sections, while primary care needs broader detail covering chronic issues and preventive care. Emergency medicine requires concise summaries that support rapid decisions.
When the platform applies these structures automatically, clinicians review instead of rewriting. This keeps chart closure steady even as usage grows.
4. EHR Integration
A platform built for scale integrates deeply with the EHR so notes flow to the correct chart and encounter without extra steps. It pulls relevant clinical context like medications or labs when needed. Strong integration reduces errors and removes friction for coding and billing teams.
As more departments adopt the platform, consistent EHR alignment keeps documentation quality stable. This prevents bottlenecks that slow enterprise expansion.
5. Real-Time Adaptation
A scalable platform follows clinical conversations as they shift direction, pace, or complexity. Emergency visits move quickly, while telehealth adds audio variations and different patient environments. The system must adjust instantly so note quality stays consistent across care settings. This adaptability allows hospitals to expand usage into diverse workflows. Reliable performance under changing conditions supports long-term scaling.
6. High-Volume Stability
A platform built for enterprise use must handle heavy documentation loads from multiple departments at once. Performance cannot decline during peak hours or when encounter volume increases. Stable processing ensures notes remain fast, predictable, and accurate across the hospital.
When the platform maintains speed and quality under high load, leaders can scale adoption without disrupting clinical flow. This is essential for system-wide deployment.
A single AI scribe platform can scale across multi-specialty hospitals only when it adapts to departmental differences while delivering consistent performance. Platforms that meet these requirements reduce administrative strain, improve documentation quality, and support reliable growth across the entire system.
Specialty-Specific Challenges AI Scribes Must Solve
A multi-specialty hospital does not operate as a single workflow. Each department communicates differently, documents at a different pace, and requires a different level of detail. A platform built for enterprise scale must understand these differences and adapt without slowing clinicians or increasing correction work.
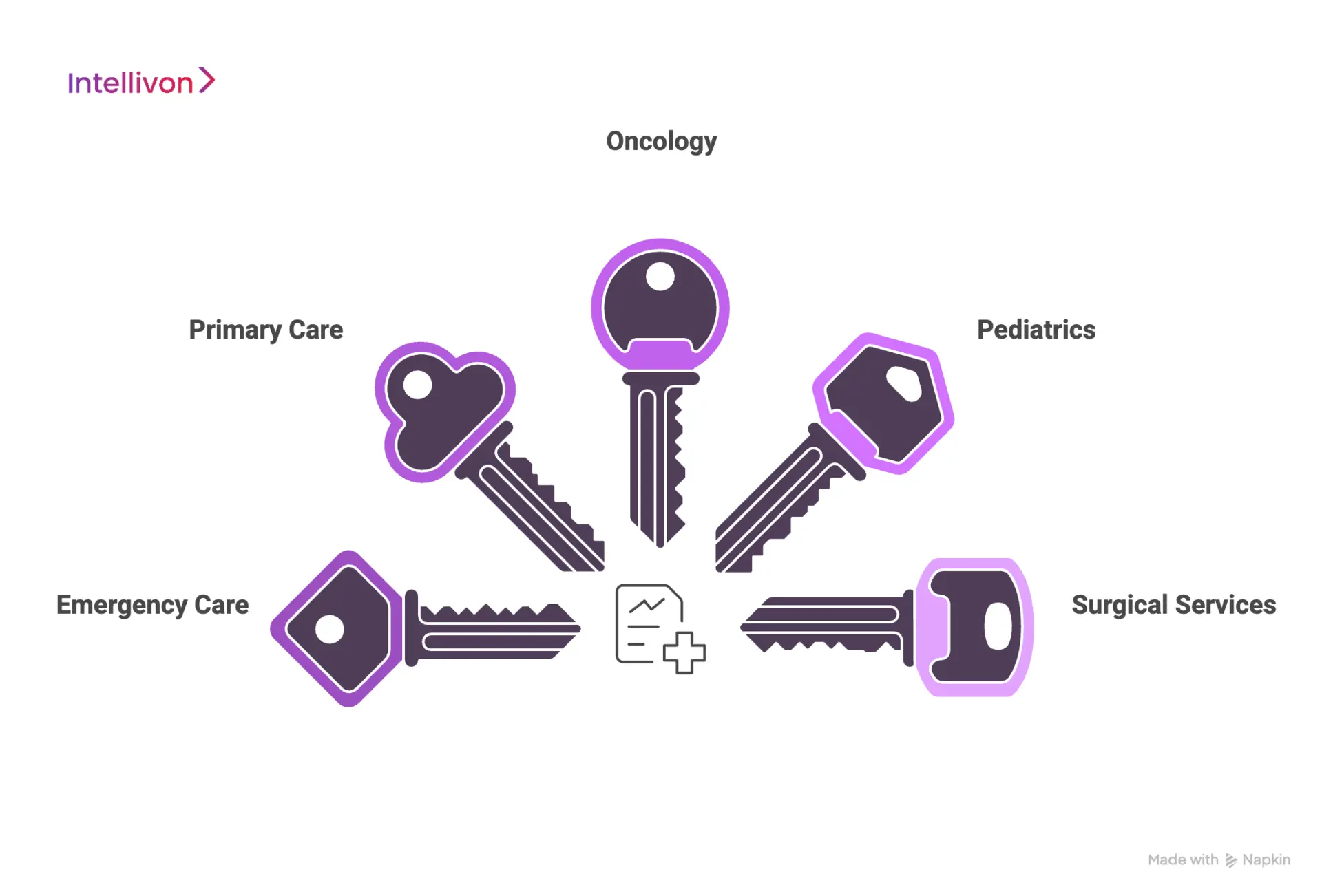
1. Emergency Care
Emergency medicine moves quickly and shifts direction often. Clinicians work in loud rooms, speak rapidly, and handle frequent interruptions. The platform must track these transitions and still produce clear summaries.
Burnout rates are already highest among emergency physicians, as shown in a study on emergency clinician strain. Reliable performance here signals the platform can handle pressure and unpredictability at scale.
2. Primary Care
Primary care clinicians manage chronic conditions, preventive care, medications, and lifestyle factors in one visit. Conversations are broad, and documentation takes significant time. Research shows clinicians spend about 145.9 minutes a day in the EHR, including late-night charting, according to a time-use analysis of primary care documentation.
A scalable platform must organize wide-ranging discussions into clear structures. Strong performance here delivers fast reductions in after-hours work and chart delays.
3. Oncology
Oncology requires careful documentation of treatment plans, medication changes, and ongoing progress. Notes often reflect sensitive decisions and long-term care.
A pilot in cancer care showed clinicians used AI-generated drafts regularly when accuracy stayed consistent, as seen in a study on ambient AI in oncology visits. A scalable platform must maintain continuity across visits and present information reliably for high-risk cases.
4. Pediatrics
Pediatric visits involve clinicians, children, and parents speaking together, often with fragmented dialogue. The platform must separate voices and capture key details clearly. A related pilot in complex care settings found that clinician efficiency shaped adoption patterns, as noted in a study on digital scribe feasibility.
When the AI-powered platform handles these dynamics well, pediatric teams spend less time correcting notes and more time moving patients through the clinic.
5. Surgical Services
Surgical documentation spans pre-operative evaluation, procedural details, and post-operative care. Teams rely on precise, structured notes for safe handoffs. A health system using ambient AI reported saving 15,791 documentation hours across 2.5 million encounters, according to a deployment analysis of AI scribe efficiency.
The platform must interpret procedural language accurately and organize details that support coordination between OR, recovery, and follow-up units.
A single AI scribe platform can scale only when it understands how each specialty communicates and documents care. When the system adapts to these patterns, it reduces rework, strengthens consistency, and supports reliable enterprise-wide performance.
How 45% of Clinical Documentation Time Blocks AI Scribe Scaling
Clinical documentation is now one of the strongest operational bottlenecks in multi-specialty hospitals. A large time-motion study found clinicians spend 44.9% of their total clinical time interacting with the EHR, which is more than with patients themselves.
Several studies show documentation alone consumes 34–55% of a physician’s workday, depending on specialty and setting. After-hours work adds even more strain. Primary care physicians spend an average of 145.9 minutes per day in the EHR, including 60–70 minutes of late-night “pajama time.”
Another national review spanning millions of outpatient visits found clinicians spending 36.2 minutes per encounter in the EHR, even when appointments were scheduled for only 30 minutes.
These numbers seem small, but across a full schedule, they escalate quickly. A clinician managing 20 patients daily can lose 8–10 hours per week to documentation alone, driving delays, burnout, and inconsistent workflows across entire departments.
Why This Workload Makes Multi-Specialty Scaling Difficult
Documentation pressure influences throughput, financial performance, and clinician stability. A UK-wide evaluation found clinicians spend 13.5 hours weekly on documentation, nearly one-third of their working time.
Source: https://bjgp.org/content/69/685/e460
Research also shows burnout rises sharply once after-hours EHR use exceeds 90 minutes per day, a threshold many hospital clinicians cross regularly. The challenge deepens across specialties. In one large system, documentation time per visit ranged from 23.5 to 47.9 minutes, depending on the department and site.
Such variation makes standardization difficult and inflates administrative and billing overhead. Each specialty brings distinct workflows, terminology, and conversational patterns, all of which must be supported before AI scribes can scale reliably across the enterprise.
2025 As The Inflection Point for Ambient AI
Recent deployments show that ambient AI has finally matured for real clinical environments. A year-long ambient scribe rollout across 2.5 million encounters saved 15,791 documentation hours, equal to 1,794 clinician workdays.
In another multi-site study involving 1,430 clinicians, burnout prevalence dropped from 51.9% to 38.8% after just 30 days of ambient scribe use, with overall cognitive workload scores also declining.
These improvements show that ambient AI is an operational enabler capable of improving stability, efficiency, and documentation quality across diverse specialties.
What This Means for Enterprise Scaling
Once hospitals address these hidden documentation pressures, they unlock three key advantages:
- Higher clinical capacity without adding staff: Reduced documentation time frees clinicians to manage more patient encounters without compromising quality.
- Stronger and faster revenue cycles: Shorter chart closure improves coding accuracy and reduces billing delays.
- Improved clinician well-being and retention: Cutting after-hours documentation decreases burnout and stabilizes clinical teams across departments.
Nearly half of a clinician’s workday is now consumed by the EHR. This reality is what makes scaling AI scribes across multi-specialty hospitals so challenging. As ambient AI reaches enterprise maturity, health systems that address these documentation burdens head-on are the ones positioned to scale successfully, unlocking greater efficiency, consistency, and workforce stability.
The Architecture Of A Scalable AI Scribe Platform
A hospital can only scale an AI scribe when the platform is built on a strong architectural, layered foundation. When these layers work together, the platform delivers consistent accuracy, reliable performance, and safe deployment across the entire hospital system.
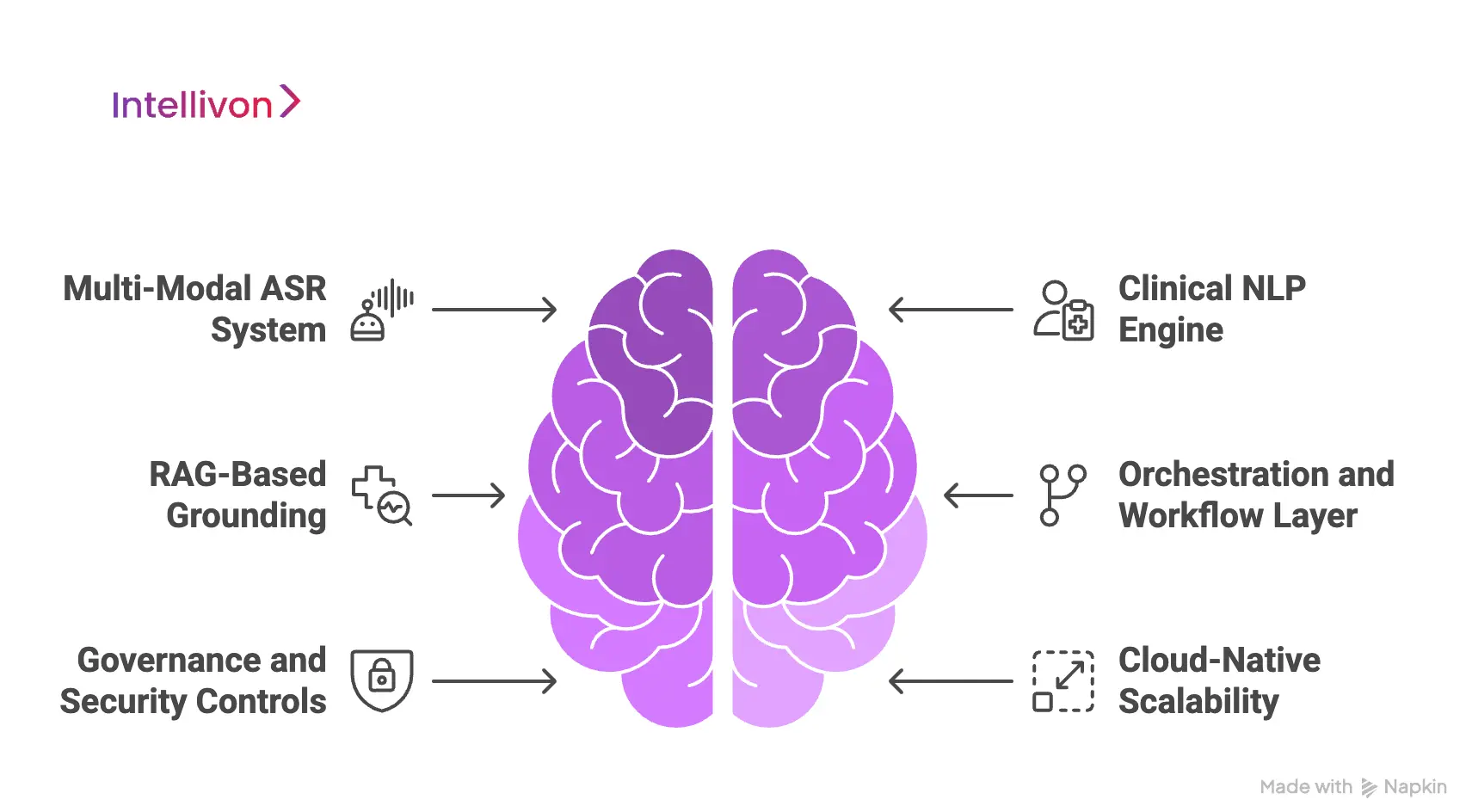
1. Multi-Modal ASR System
The speech layer must handle real clinical conversations without slowing teams down. It needs to recognize accents, reduce background noise, and follow rapid shifts in dialogue.
Real-time diarization separates speakers so the platform captures each contribution clearly. This creates a stable base for primary care, emergency units, and specialty clinics. Strong ASR performance signals readiness for enterprise expansion.
2. Clinical NLP Engine
The NLP layer interprets medical language and organizes it into a meaningful structure. It extracts SOAP elements, identifies diagnoses, and generates ICD or CPT suggestions when needed.
Clinical summarization must follow safety constraints to prevent errors, and each specialty uses different terminology, so the models must adapt across departments. This helps the platform produce drafts that feel natural to clinicians.
3. RAG-Based Grounding
The platform must check information against real patient data to maintain accuracy. Retrieval layers pull vitals, medications, allergies, and labs from the EHR during note creation. This grounding prevents hallucinations and supports stronger clinical trust.
It also aligns documentation with the patient’s current medical status. Grounded generation keeps notes consistent across visits and specialties.
4. Orchestration and Workflow Layer
This layer manages user sessions, access controls, audit logs, and workflow routing. It supports multiple hospitals, clinics, and departments under one platform.
The orchestration layer keeps documentation tied to the correct chart and encounter. It also manages permissions and ensures operational consistency. Strong orchestration prevents fragmentation and supports smooth scaling across the enterprise.
5. Governance and Security Controls
The platform must follow strict privacy and security guidelines. It needs encryption, access boundaries, and complete traceability for all activity. Hospitals require alignment with HIPAA, GDPR, and internal governance standards.
These controls protect PHI and support internal review processes. A secure foundation allows expansion into high-risk clinical departments.
6. Cloud-Native Scalability
The performance layer must support high encounter volume without slowing down. Horizontal scaling keeps inference fast during peak hours. Low latency ensures note generation stays predictable as more clinicians adopt the platform.
Cloud-native infrastructure maintains consistency across inpatient, outpatient, and telehealth environments. This stability is essential for system-wide deployment.
A scalable AI scribe platform relies on an architecture that supports accuracy, speed, and reliability across all clinical settings. When these layers function together, hospitals can expand usage confidently and maintain consistent documentation quality across every specialty.
Compliance & Governance Framework for Scaling AI Scribes
A scalable AI scribe platform must follow a strict compliance and governance framework. Hospitals operate under complex privacy, safety, and regulatory expectations, which become harder to manage as usage expands across departments.
A strong framework protects patient data, simplifies audits, and supports safe deployment at enterprise scale.
1. Data Privacy Controls
The platform must protect patient information in every step of note creation. It needs strong encryption, access control, and secure data handling across all environments. Clinical conversations often include sensitive details, so privacy controls must prevent exposure.
Clear data boundaries help hospitals meet local and international regulations. These controls form the baseline for safe expansion.
2. Access and Role Management
A scalable platform needs fine-grained access controls across clinicians, coders, administrators, and support teams. Each user role should have defined permissions that limit what they can view or modify.
This prevents unauthorized access and helps maintain clean audit trails. Hospitals can manage departments, teams, and locations under one system. Strong role management supports controlled expansion into new units.
3. Auditability and Traceability
Every interaction within the platform must be traceable. The system should log access, edits, version changes, and workflow actions for review. Hospitals rely on these logs during internal audits and regulatory checks.
Clear traceability helps identify issues early and supports governance teams. Reliable audit data becomes more important as usage grows across specialties.
4. Safety and Quality Controls
A scalable platform must include built-in guardrails for clinical accuracy. Safety layers should detect missing context, unclear statements, or inconsistencies in generated drafts. Hospitals also need oversight tools to review quality across departments.
These controls reduce the risk of documentation errors as more clinicians adopt the system. Strong safety design supports trust and long-term reliability.
5. Regulatory Alignment
The platform must align with HIPAA, GDPR, and region-specific health regulations. It should support internal compliance programs through clear policies, transparent processes, and predictable data handling. Hospitals need assurance that documentation stays within approved boundaries for every specialty.
This alignment reduces risk and simplifies governance decisions. Strong regulatory design allows the platform to scale across multiple sites.
6. Enterprise Governance Model
Scaling requires a governance model that supports oversight across departments and locations. Hospitals need structured processes for onboarding, monitoring, and continuous improvement.
Governance teams should have visibility into performance, quality, and safety metrics. A unified model keeps documentation practices consistent as usage expands. This prevents fragmentation and ensures enterprise-wide standardization.
A strong compliance and governance framework is essential for scaling AI scribes safely across a hospital system. When privacy, access, auditability, safety, and regulatory alignment work together, hospitals can expand the platform with confidence and maintain consistent quality across all specialties.
Our Process of Building Scalable AI Scribe Platforms For Multi-Specialty Hospitals
Intellivon follows a structured process to design, build, and deploy AI scribe platforms that scale across every specialty. Each step focuses on accuracy, workflow alignment, and enterprise reliability. This ensures hospitals can expand usage confidently while maintaining consistent performance.
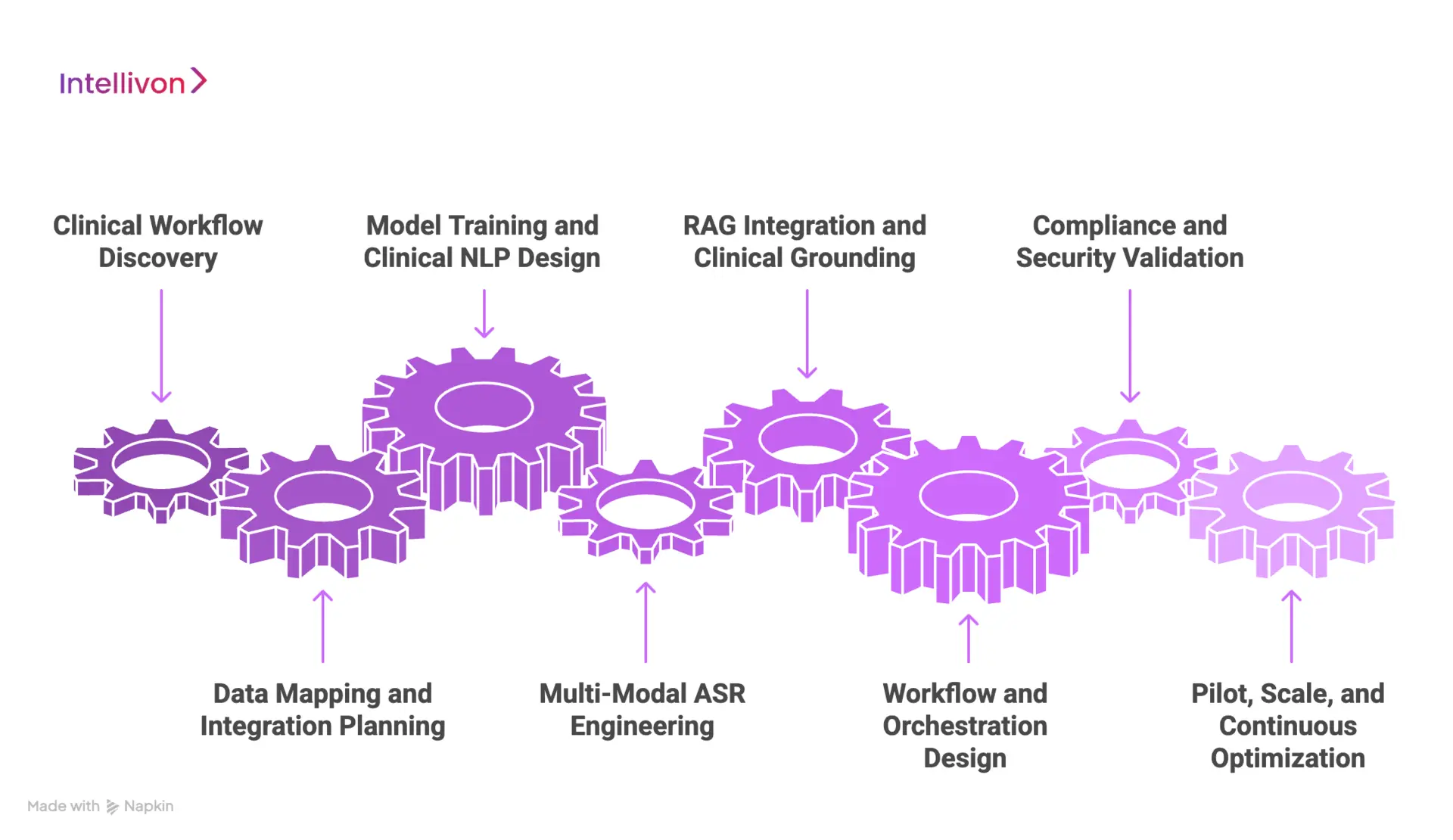
1. Clinical Workflow Discovery
We begin by understanding how each department documents care. Our team studies communication patterns, note templates, and specialty-specific requirements.
This helps us design a platform that fits real clinical environments. Strong discovery reduces friction during adoption. It also creates clear foundations for specialty-wide scaling.
2. Data Mapping and Integration Planning
Intellivon maps the hospital’s EHR structure, coding rules, and documentation workflows. We identify the data elements needed for accurate grounding and safe note generation.
This includes medications, labs, allergies, and encounter types. Early mapping prevents integration issues as usage expands. It also prepares the platform for multi-department deployment.
3. Model Training and Clinical NLP Design
Our team builds and tunes language models for each specialty. We train on varied clinical patterns so the platform understands terminology and context across departments.
Summarization rules are aligned with safety constraints to prevent errors. This ensures the system produces drafts that feel natural to clinicians. Strong NLP performance accelerates trust and adoption.
4. Multi-Modal ASR Engineering
We built a speech engine that handles real clinical audio. It manages accents, noise, and interruptions without reducing accuracy.
Real-time diarization separates speakers during fast conversations. Reliable ASR performance supports consistent results across inpatient, outpatient, and telehealth environments. This stability enables enterprise-scale usage.
5. RAG Integration and Clinical Grounding
Intellivon integrates retrieval layers directly with the EHR. The system pulls vitals, medications, and recent tests during note creation.
This grounding prevents hallucinations and keeps documentation aligned with the patient record. It also helps clinicians trust the system’s outputs. Accurate grounding is essential for multi-specialty scalability.
6. Workflow and Orchestration Design
We design routing rules and permissions that reflect how the hospital operates. The platform manages sessions, access levels, and audit history for all users.
This ensures notes move to the right clinician and encounter without extra steps. Strong orchestration supports smooth deployment across many units. It also keeps documentation practices consistent.
7. Compliance and Security Validation
Intellivon validates every layer of the platform against HIPAA, GDPR, and internal governance standards. Security controls protect PHI from ingestion to writeback. Audit logs support internal review and quality oversight.
This framework allows hospitals to deploy the platform safely across high-risk specialties. Strong compliance design reduces enterprise-level risk.
8. Pilot, Scale, and Continuous Optimization
We begin with a focused pilot and expand usage as performance stabilizes. Intellivon monitors accuracy, adoption, and latency across departments. Feedback loops help refine templates and workflows.
As results improve, hospitals can scale the platform system-wide. Continuous optimization keeps quality high long after deployment.
Intellivon’s process ensures hospitals receive a platform that performs reliably across all specialties. Each step builds the technical, clinical, and operational foundations needed for safe and scalable adoption.
Cost To Build A Platform That Scales AI Scribes Across Multi-Specialty Hospitals
At Intellivon, our priority is to help healthcare enterprises build AI scribe platforms that are compliant, resilient, and designed for system-wide scale. Pricing aligns with hospital goals, regulatory scope, and the level of specialty variation across departments. Every investment aims to improve patient safety, operational efficiency, and documentation accuracy.
When budgets are tight, Intellivon refines the scope with clinical and IT leaders. We never compromise HIPAA or GDPR alignment. We prepare for FDA and EU AI Act readiness from the earliest design stages. Every build balances cost efficiency with sustainable compliance and clear ROI visibility.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Compliance Alignment | Requirements, specialty mapping, risk analysis, HIPAA controls, EU AI Act scoping, KPI definition | $6,000 – $12,000 |
| Architecture & Secure Design | Multi-layer architecture, PHI handling design, encryption controls, IAM structure, resilience planning | $8,000 – $15,000 |
| Audio Capture & Edge Setup | Room audio design, telehealth connectivity, consent flows, noise filtering, speaker diarization | $6,000 – $12,000 |
| ASR, NLP & Note Generation | Medical ASR tuning, specialty terminology models, SOAP templates, summarization rules, confidence scoring | $12,000 – $25,000 |
| EHR Integration & Interoperability | FHIR, HL7, SMART on FHIR, routing logic, multi-hospital compatibility | $10,000 – $20,000 |
| Security & Privacy Engineering | RBAC, MFA, tokenization, redaction, key management, continuous monitoring | $8,000 – $15,000 |
| Platform UX & Interfaces | Clinician review UI, coder workflows, audit console, admin dashboard | $10,000 – $20,000 |
| Testing & Validation | HIPAA verification, penetration testing, model validation, safety testing | $6,000 – $10,000 |
| Pilot & Training | Limited rollout, feedback cycles, clinical template refinement, training playbooks | $6,000 – $10,000 |
| Deployment & Scaling | Cloud deployment, high availability setup, observability, elastic scaling pipelines | $6,000 – $12,000 |
Total Initial Investment Range: $50,000 – $150,000
Ongoing Maintenance & Optimization (Annual): 15–20% of the initial build
Hidden Costs Enterprises Should Plan For:
- Integration complexity: Legacy EHR configurations may require middleware and additional mapping.
- Compliance overhead: Audits, risk reviews, and documentation require recurring effort.
- Data governance: Normalizing mixed data formats across specialties needs steady resources.
- Cloud spend: Real-time processing pipelines and storage require ongoing cost controls.
- Change management: Training clinicians and coders introduces measurable transition overhead.
- Model drift: Periodic retraining preserves accuracy, fairness, and regulatory posture.
Best Practices to Avoid Budget Overruns:
- Start with a focused scope: Begin with one specialty, prove impact, then scale.
- Embed compliance early: Avoid expensive redesigns later.
- Adopt modular design: Reuse AI pipelines and templates across specialties.
- Optimize cloud usage: Combine real-time and batch processing to control compute costs.
- Ensure observability: Track uptime, latency, and integration health continuously.
- Iterate for longevity: Update controls, refine workflows, and recalibrate models regularly.
Request a tailored proposal from Intellivon’s healthcare AI experts. We will align your roadmap with budget, compliance obligations, and system-wide scalability goals.
Common Pitfalls Faced When Scaling AI Scribes Across Multi-Specialty Hospitals
Many hospitals start with a small pilot and expect the same setup to work across every department. But each specialty documents care differently, and these differences create friction during scaling. Without a clear plan, performance becomes uneven, and clinician trust declines. Our team helps hospitals avoid these issues by building platforms designed for multi-specialty environments from day one.
1. Ignoring Specialty Differences
Documentation in oncology looks nothing like documentation in pediatrics or emergency medicine. Each specialty has its own language, pace, and clinical priorities. When this variation is ignored, the platform generates inconsistent drafts that frustrate clinicians.
We study each department’s workflow before scaling, so accuracy stays high across the entire system. This creates a consistent experience for users.
2. Insufficient EHR Alignment
A superficial EHR connection can break documentation flow. Notes may miss the correct chart, encounter type, or clinical context. This forces clinicians to fix errors manually.
Our platform integrates deeply through FHIR, HL7, and SMART-on-FHIR, so every note lands exactly where it should. Strong alignment removes friction and keeps documentation reliable across specialties.
3. Audio Limitations in Real Environments
Clinical audio is rarely clean or predictable. Busy clinics, telehealth visits, and emergency departments each create unique challenges. When the ASR cannot handle these conditions, accuracy drops sharply.
We design audio pipelines that manage noise, accents, movement, and interruptions. This keeps performance steady wherever clinicians work.
4. Weak Governance and Compliance Planning
Scaling increases responsibility around privacy, access control, and audit requirements. Without governance, hospitals face a higher risk and slower approval cycles.
Our team sets up clear policies, role boundaries, and audit trails early in the project. This protects PHI and supports safe expansion into high-risk units. Strong governance becomes the backbone of long-term scale.
5. Poor Change Management Support
Clinicians need guidance when shifting to AI-assisted documentation. If training or onboarding feels rushed, adoption drops quickly. This slows progress and limits how far the platform can expand.
We support teams with training materials, review workflows, and specialty-specific templates. This helps clinicians adapt smoothly and builds confidence in the platform.
Scaling AI scribes across a multi-specialty hospital requires more than strong technology. Hospitals need a platform that adapts to real workflows, integrates deeply with the EHR, and supports teams through the transition. We help organizations avoid these challenges so they can scale with confidence and maintain consistent performance across every department.
Conclusion
Scaling AI scribes across a multi-specialty hospital is a strategic shift that touches every part of clinical operations. Success depends on strong architecture, deep EHR integration, and thoughtful change management. Hospitals that approach this as an enterprise transformation, not a single-department rollout, see the greatest improvements in accuracy, speed, and clinician workload.
A carefully designed platform creates consistency across diverse specialties and maintains reliability even as volume grows. With the right foundations, health systems can move beyond pilots and build a future where documentation supports care instead of slowing it down.
Scale Your AI Scribes Across Multi-Specialty Hospitals With Intellivon
At Intellivon, we build AI scribe platforms that are ready for multi-specialty complexity from day one. Our focus is on medical-grade accuracy, regulatory strength, and system-wide scalability. The result is a platform that supports primary care, oncology, pediatrics, surgery, and emergency medicine under one architectural roof.
Our solutions cut down manual documentation, reduce after-hours charting, and stabilize billing workflows. They integrate into existing EHR and clinical systems without forcing clinicians to change how they work. You get a single platform that scales smoothly across hospitals, departments, and care settings.
Why Partner With Us
- Compliance-First Architecture: Every platform is designed around HIPAA, GDPR, and enterprise governance requirements. We plan for FDA and EU AI Act expectations from the start..
- Healthcare-Tuned AI Models: Our ASR and clinical NLP engines are tuned for real-world hospital environments. They handle specialty terminology, variable audio conditions, and complex visit structures.
- Deep EHR and System Integration: We integrate through FHIR, HL7, SMART-on-FHIR, and existing interface engines. Notes land in the right chart, encounter, and template.
- Cloud-Native, Enterprise Scale: The platform is built to support multi-hospital networks. It maintains low latency during peak hours and scales horizontally as usage grows.
- Continuous Model and Workflow Optimization: We monitor accuracy, latency, and adoption across specialties. Feedback loops guide model tuning, template refinement, and workflow updates.
- Security and Governance Built-In: Access control, encryption, and detailed audit logs are part of the core design. Governance teams gain clear visibility into usage, changes, and system behavior.
- Proven Enterprise Delivery Experience: Our team has deep experience building healthcare AI systems for complex environments.
Book a strategy session with Intellivon to explore how a scalable AI scribe platform can support your multi-specialty hospitals, reclaim clinical time, and strengthen documentation quality across your entire network.
FAQs
Q1. How do you scale an AI scribe across multiple hospital specialties?
A1. Scaling requires a platform built to handle different clinical languages, workflows, and note structures. It must integrate deeply with the EHR and adapt to each department without extra work for clinicians. Strong governance and continuous optimization support smooth expansion across units.
Q2. What features should a hospital-grade AI scribe platform include?
A2. A hospital-grade platform needs strong ASR, clinical NLP, EHR interoperability, and real-time grounding with patient data. It should manage noise, accents, and rapid conversations. Security, compliance, and auditability must be part of the core design.
Q3. How long does it take to deploy AI scribes across a large health system?
A3. Most hospitals begin with a focused pilot and expand once workflows and performance stabilize. Full deployment timelines vary based on integration depth, specialty variation, and training needs. Strong planning shortens the rollout and improves adoption.
Q4. What are the biggest challenges in scaling AI scribes across specialties?
A4. Common challenges include specialty variation, audio complexity, shallow EHR integration, and limited governance planning. Each of these issues affects accuracy and clinician trust. A structured roadmap helps avoid delays during system-wide expansion.
Q5. Do AI scribes work the same way in every department?
A5. No, each specialty documents care differently. The platform must understand unique terminology, note patterns, and clinical priorities. Systems built for multi-specialty environments deliver the most consistent performance.