Hospitals face constant pressure to handle documentation, and clinicians spend long hours writing notes, correcting charts, and finishing documentation after their shifts. This process slows down care, delays billing, and contributes to burnout. AI scribes can help alleviate this burden, but large health systems often have trouble figuring out if these tools provide real benefits. Time savings, coding accuracy, and lower denial rates are important. However, without a clear ROI framework, leaders cannot fully understand the financial and operational effects of AI documentation.
At Intellivon, we deploy AI scribe platforms in busy clinical environments, specialty departments, and settings that require strict compliance. Our experience with top healthcare organizations shows that ROI becomes clear when documentation, revenue cycle performance, and workforce stability are measured together. In this blog, we will explain how we assess the ROI of AI scribe deployments by using real baselines, layered metrics, and financial signals that mirror the realities of large healthcare enterprises.
Key Takeaways of the AI Scribe Platforms Market
This growth reflects higher demand for accurate clinical documentation, wider telemedicine adoption, and increasing reliance on AI-powered speech recognition and NLP to improve speed and accuracy. Hospitals are shifting from manual or outsourced transcription to automated scribing because the economics and operational outcomes are stronger.
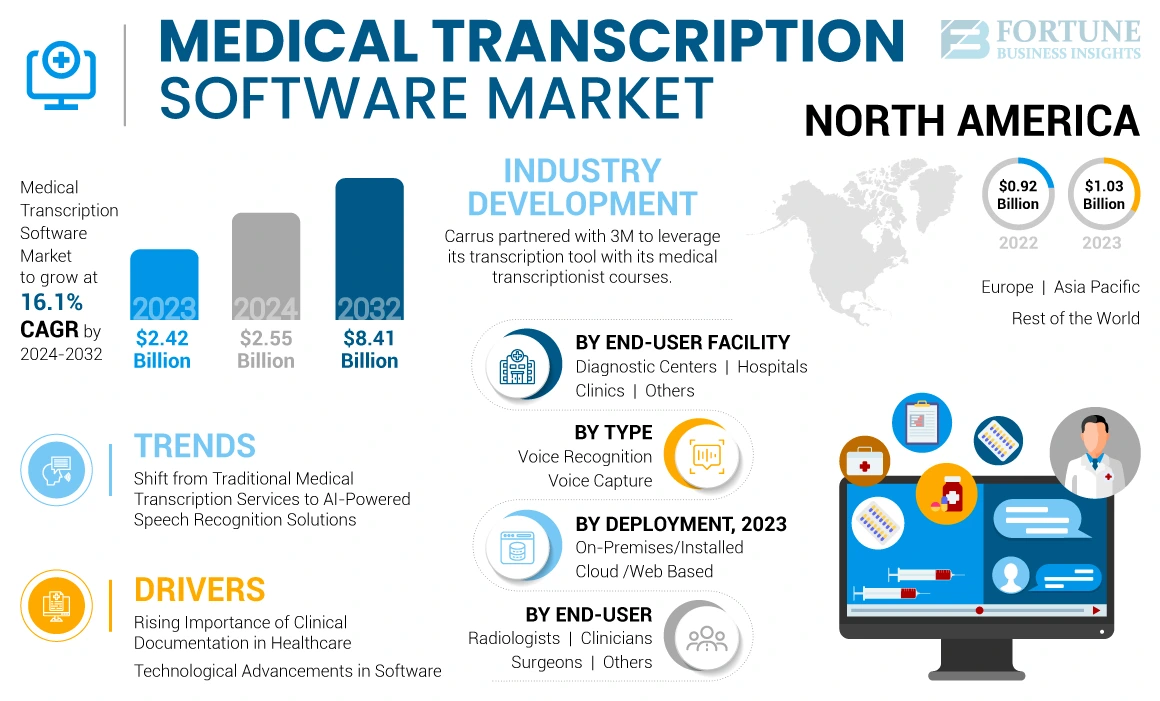
Key Market Drivers:
- The ambient AI scribe platform market was valued at approximately $600 million in 2025, with adoption expected to reach 40% of large hospital systems by 2028.
- Ambient AI scribes save physicians up to two hours per day and reduce documentation errors by 30%.
- Emergency medicine, psychiatry, and outpatient care show the highest adoption due to burnout reduction and workflow efficiency.
- ROI payback periods fall between 18 and 24 months, driven by faster chart closures, higher coding accuracy, and a 25% gain in patient throughput.
- More than 80% of clinicians report better patient interactions and improved satisfaction due to reduced “pajama time.”
- Cloud deployments now account for over 50% of implementations, enabling faster onboarding and smooth EHR integration with Epic and Cerner.
- Fewer than 10 vendors hold more than 75% market share, and many are expanding into real-time clinical decision support.
- Compliance remains a top adoption driver, with platforms adding audit trails and encryption to meet strict healthcare regulations.
Ambient AI scribing has shifted from early adoption to enterprise scaling. Hospitals now treat it as core infrastructure for efficiency, patient experience, and financial performance.
What Is an Ambient AI Scribe Platform?
An ambient AI scribe platform listens to clinical conversations and turns them into structured notes. It captures physician–patient dialogue, understands medical terminology, and drafts documentation that syncs with the EHR.
The result is accurate, compliant clinical notes without typing or workflow disruption. Hospitals use it to cut charting time, improve billing completeness, and strengthen audit readiness.
How They Work
These platforms follow a clear workflow from recording the consultation to generating final notes. Each layer plays a specific role, so hospitals get accurate documentation without extra effort from clinicians.
1) Audio Capture at the Point of Care
The platform securely records consultations in rooms or telehealth sessions. It handles background noise and identifies speakers. Recording activates only within approved workflows.
2) Real-Time Speech Recognition (ASR)
A medical ASR engine converts speech to text as the visit unfolds. It handles accents, interruptions, and specialty vocabulary. Healthcare-trained models improve accuracy over time.
3) Medical NLP for Structure and Context
NLP detects symptoms, medications, allergies, and procedures. It maps terms to clinical ontologies to avoid ambiguity, and these entities feed downstream note creation and coding.
4) Draft Note Generation in Clinical Formats
The system prepares a structured SOAP or specialty-specific template. It captures clinical reasoning, orders, assessments, and plans. On the other hand, confidence scores flag items for review.
5) AI-Assisted Coding Suggestions
ICD and CPT suggestions align with the documented exam and plan. The platform shows supporting evidence for billing teams. This improves revenue integrity and reduces denials.
6) Clinician Review and Sign-Off
Physicians review, edit, and approve with minimal clicks. Inline controls make corrections fast and traceable. Every change is logged for audits.
7) EHR Integration and Interoperability
Approved notes post to the EHR via FHIR, HL7, or SMART on FHIR. The platform supports Epic, Cerner, Meditech, and other systems. It keeps routing and departmental workflows unchanged.
8) Security, Compliance, and Monitoring
Encryption, PHI redaction, and RBAC protect data at every stage. Continuous monitoring tracks drift and system health. Detailed logs support HIPAA, GDPR, and internal reviews.
In short, ambient scribing removes manual typing without changing how clinicians work. Hospitals get faster documentation, cleaner notes, and stronger revenue capture with less operational friction.
Understanding ROI for AI Scribe Deployments in Healthcare Enterprises
Evaluating ROI for AI scribe deployments requires more than measuring documentation time. In large healthcare systems, clinical notes influence financial performance, compliance risk, billing accuracy, and overall care throughput. This makes ROI multi-layered, with gains appearing across several parts of the organization, and not just at the clinician level.
What ROI Really Means for AI Scribe Deployments
AI scribes create value across both clinical and administrative workflows. Teams see gains through faster note completion, more accurate documentation, and smoother downstream processes in coding and billing. These improvements reduce operational friction and strengthen financial outcomes, forming the foundation of ROI.
1. Time Recovered for Care Delivery
Shorter documentation cycles give clinicians more time for patients. This improves throughput without adding staff. It becomes one of the earliest and most measurable forms of return.
2. Operational Efficiency Across Departments
Faster chart closure supports coding teams, billing teams, and quality teams. When notes move faster, every downstream task moves faster. This reduces delays and improves organizational rhythm.
3. Better Use of Workforce Capacity
AI scribes reduce after-hours work and lower administrative load. This supports clinician well-being and helps stabilize staffing, which is an important ROI component for large systems.
Why Documentation Influences Both Costs and Revenue
Clinical documentation quality shapes reimbursement outcomes. Every note influences coding specificity, claim acceptance, audit readiness, and financial accuracy. When notes are complete and consistent, organizations reduce losses caused by denials, downcoding, and missing billable items.
1. Direct Impact on Coding Specificity
Clearer documentation helps coders assign correct levels of service. This increases revenue per encounter and reduces underbilling tied to incomplete notes.
2. Fewer Errors That Trigger Denials
Missing or unclear documentation is a major cause of claim denials. AI-generated notes reduce these errors, lowering rework costs and accelerating reimbursement.
3. Stronger Compliance and Audit Protection
Structured, complete notes reduce audit flags and compliance risk. This protects the organization from costly reviews and penalties, which are key financial considerations in ROI.
Revenue Benefits AI Scribes Can Unlock For Healthcare Enterprises
AI scribes strengthen the financial core of a healthcare enterprise. They improve how clinical notes translate into revenue, reduce losses caused by documentation gaps, and increase the accuracy of claims submitted to payers.
When documentation becomes more consistent and complete, revenue flow becomes stronger and more predictable. These improvements form a key part of ROI evaluation for large health systems.
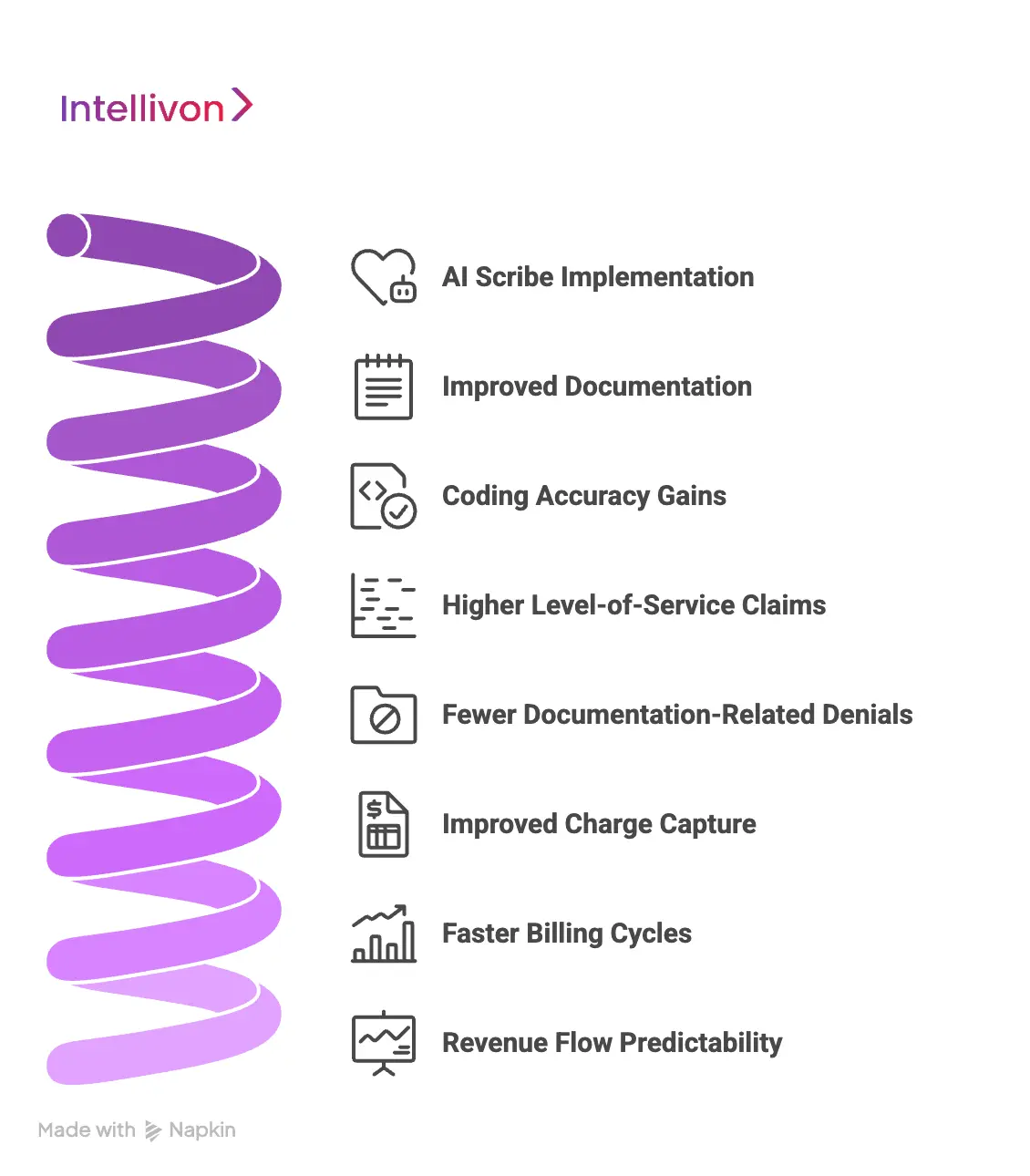
1. Coding Accuracy Gains
AI-generated notes help capture clinical details that often get missed during busy encounters. More accurate documentation supports more accurate coding.
This reduces underbilling and improves the financial return on each visit. Even small improvements in coding accuracy deliver meaningful revenue when scaled across thousands of encounters.
2. Higher Level-of-Service Claims
Many encounters qualify for higher levels of service but are billed lower due to incomplete notes. AI scribes provide clearer, fuller documentation, making it easier for coders to justify the correct CPT level.
This leads to a noticeable uplift in reimbursement without adding work for clinicians.
3. Fewer Documentation-Related Denials
A significant share of denials comes from missing or inconsistent information. AI scribes reduce these errors by generating structured, complete notes.
Fewer denials mean fewer reworks and less time spent correcting claims. This improves cash flow and reduces operational waste, both of which are key drivers of ROI.
4. Improved Charge Capture
Incomplete documentation often results in missed billable items. AI scribes help ensure that all relevant services, assessments, and procedures are captured accurately.
This increases revenue per encounter without requiring additional clinician effort. Stronger charge capture directly impacts financial performance.
5. Faster Billing Cycles
When notes are completed faster, coding and billing teams can work sooner. This shortens the time between service delivery and reimbursement.
Shorter cycles improve cash flow and reduce administrative backlog. Faster billing becomes a measurable financial benefit within the first months of deployment.
6. Revenue Flow Predictability
Consistent documentation creates more predictable claims, fewer corrections, and steadier reimbursement patterns. Predictability allows leaders to manage budgets, staffing, and resources more effectively.
This stability is a core component of ROI and becomes even more valuable at enterprise scale.
Together, these improvements turn documentation quality into a measurable financial engine. AI scribes help enterprises protect revenue, accelerate reimbursement, and strengthen long-term ROI.
How Manual Documentation Consumes Over 500 Minutes of Clinician Time Every Week
Manual documentation has become one of the biggest hidden drains on ROI across enterprise health systems. In a study analyzing 100 million outpatient encounters, physicians spent 16 minutes and 14 seconds in the EHR per visit, with nearly a quarter of that time dedicated solely to documentation.
Every minute in the EHR is a minute that cannot be billed, cannot support patient care, and cannot strengthen productivity. These losses reduce operational ROI across the entire system.
A national assessment found primary-care physicians spending a median of 36.2 minutes per visit in the EHR, with 6.2 minutes completed after hours. This after-hours documentation is unpaid labor. It fuels burnout, increases attrition, and drives locum and recruitment costs, which are major negative ROI pressures.
Individually, these minutes seem small. But they multiply fast. A clinician seeing 20 patients a day loses 9–10 hours each week to documentation alone.
At enterprise scale, across hundreds or thousands of clinicians, this becomes a multi-million-dollar inefficiency that suppresses revenue throughput, clinical capacity, and workforce stability.
Documentation Waste Erodes Enterprise ROI
Clinical Documentation affects every financial and operational factor tied to ROI. A UK analysis found clinicians spending 13.5 hours per week on documentation, which is nearly one-third of a full-time schedule. Every hour recovered can support more encounters, reduce overtime, and prevent burnout-related turnover.
EHR overload is also a strong predictor of burnout. AMA research shows burnout drives unplanned exits and lower productivity, increasing expensive reliance on locums. These are among the most damaging ROI leakages in healthcare.
Documentation delays slow coding and billing, inflate accounts receivable cycles, and reduce cash flow. In some multi-site systems, documentation time ranges from 23.5 to 47.9 minutes per visit. Variability becomes inefficiency. Inefficiency becomes ROI drag.
Major ROI Gains Achieved Through Automation
In 2025, ambient AI documentation reached the maturity required for measurable enterprise return.
A year-long deployment across a major U.S. health system saved 15,791 clinician hours across 2.5 million encounters. This reclaimed capacity reduces overtime and lowers the cost per encounter.
Another multi-site study of 1,430 clinicians found that ambient documentation reduced burnout from 51.9% to 38.8% after 30 days. Lower burnout improves retention, reduces replacement costs, and stabilizes clinical productivity, which are all major ROI drivers.
Automated Documentation as a Direct ROI Lever
Automated clinical documentation is now a financial and operational strategy that improves throughput, documentation quality, cost structure, and workforce sustainability at enterprise scale. Here is why:
1. Increased Revenue Throughput
When documentation time drops, clinicians gain capacity. They can see more patients without expanding headcount, increasing revenue without higher labor costs.
2. Faster, Cleaner Documentation
Quicker chart closure improves coding accuracy and reduces rework. This shortens revenue cycles and strengthens cash flow.
3. Lower Replacement Cost
Less after-hours documentation reduces burnout. Better retention lowers recruitment, onboarding, and productivity-gap costs, which are some major hidden ROI wins.
Manual documentation drains ROI through lost time, slow billing, high labor costs, and increased turnover. AI-driven documentation reverses these patterns.
It restores capacity, reduces operational waste, and strengthens financial performance, thereby making it one of the most direct ROI levers available to healthcare enterprises today.
Key Factors That Drive ROI of AI Scribe Deployment
The ROI of AI scribe deployments depends on how well the technology improves documentation workflows, strengthens financial processes, and reduces operational friction.
AI scribes influence several parts of the organization at once, which makes these factors critical for predicting measurable returns. When these drivers move in the right direction, ROI compounds quickly across clinical and administrative teams.
1. Documentation Quality and Completeness
Stronger documentation quality is one of the most important ROI drivers. AI scribes help clinicians capture more complete, structured, and detailed notes without relying on memory or manual typing.
Better documentation supports coding accuracy, reduces denials, and creates a more reliable financial record. These improvements directly affect reimbursement and overall financial performance.
2. Clinician Time Savings
Reducing documentation time is the earliest and most visible ROI gain. AI scribes help clinicians close charts faster, reduce after-hours work, and move through encounters with less effort.
Even a small time reduction per visit becomes significant when multiplied across busy schedules. This recovered time improves capacity, reduces overtime costs, and supports clinician well-being.
3. Coding and Billing Efficiency
Cleaner documentation accelerates the revenue cycle. When notes are complete and consistent, coders work faster and billers submit claims sooner. Fewer documentation gaps lead to fewer queries, fewer reworks, and fewer delays.
This improves cash flow, strengthens coding specificity, and reduces the financial drag caused by slow documentation.
4. Reduction in Denials and Compliance Risk
Documentation issues are a common source of denials and audit flags. AI scribes reduce these risks by capturing required details more reliably. Fewer denials mean fewer operational costs and faster reimbursements.
Stronger documentation also lowers compliance exposure, which protects the organization from unexpected penalties and regulatory issues.
5. Workforce Stability and Burnout Reduction
Documentation pressure is a major contributor to burnout and turnover. AI scribes reduce administrative load, support better work-life balance, and help clinicians spend more time on patient care. This improves retention and reduces costly turnover.
Lower burnout also leads to more consistent productivity, which strengthens ROI across the enterprise.
6. Consistency Across Departments and Specialties
Large health systems struggle with documentation variability. AI scribes create more uniform note quality, regardless of the site or specialty. This consistency helps coding teams work more efficiently and reduces performance gaps across the organization.
A more predictable workflow supports more predictable financial outcomes, making ROI easier to measure and sustain over time.
These factors determine how quickly and effectively ROI appears after deployment. When documentation improves, time is recovered, denials decrease, and teams work more efficiently. Together, these changes form the foundation of a strong, measurable, enterprise-wide return on investment for AI scribe adoption.
Overcoming Enterprise Barriers That Distort ROI Calculations
ROI often appears inconsistent in large health systems because enterprise workflows vary widely and create hidden frictions. These barriers distort early ROI readings unless addressed deliberately and systematically.
1. Inconsistent Documentation Workflows
Large health systems rarely operate with uniform documentation behaviors. Each site uses different note structures, template habits, and EHR patterns. These inconsistencies make it difficult to compare performance across locations and often create misleading ROI signals during early deployment phases.
Intellivon’s Solution:
We standardize workflows through specialty-aligned templates, onboarding playbooks, and configuration libraries. Our deployment model builds consistency without forcing teams to change EHR habits. This reduces variability and supports more accurate ROI measurement across locations.
2. Specialty-Level Complexity
Documentation burden varies dramatically across specialties with differing terminology, encounter structures, and clinical depth. Without specialty tuning, early ROI appears uneven because the platform performs differently depending on the complexity of the specialty.
Intellivon’s Solution:
We train specialty-tuned language models that understand unique terminology, encounter flow, and narrative structure. Each model improves with site-specific feedback, allowing ROI gains to appear at different speeds while maintaining accuracy in every department.
3. Variable Audio Quality
Enterprise clinics have diverse acoustic conditions, from quiet exam rooms to high-traffic outpatient floors. When audio varies across sites, AI may appear inconsistent even though the underlying model is performing correctly, distorting early ROI interpretation.
Intellivon’s Solution:
Our ambient speech capture layer uses adaptive noise filtering and multi-speaker separation. We audit room conditions, recommend hardware improvements, and calibrate models based on real audio patterns. This prevents false dips in accuracy and stabilizes performance early in deployment.
4. Delayed Chart Closure
Some clinicians close charts immediately, while others batch-complete them at the end of the day or week. When chart closure varies widely across clinicians, financial teams see inconsistent downstream performance, making ROI appear lower than it actually is.
Intellivon’s Solution:
We design workflows that support same-day note review with automated reminders, smart summarization, and EHR-integrated checkpoints. This speeds up chart closure and ensures ROI reflects true platform performance, not inconsistent habits.
5. Differences in Coding and Billing
Even with better documentation, ROI is suppressed if coding teams lack the staffing or bandwidth to process improved notes. This creates a mismatch between clinical efficiency gains and financial visibility, making ROI appear weaker in early months.
Intellivon’s Solution:
Intellivon integrates structured note outputs that reduce coder queries and rework. Our RCM-aligned documentation structure improves coding throughput and supports cleaner claims. This allows billing teams to work faster and improves revenue cycle performance across sites.
6. Uneven Clinician Adoption
Some clinicians adapt quickly to AI scribes, while others take longer to trust the workflow or adjust their dictation style. Uneven usage creates inconsistent early results, making ROI look unpredictable across departments. Poor adoption in a few high-volume specialties can disproportionately lower overall ROI readings for the entire system.
Intellivon’s Solution:
We run multi-week adoption programs with role-based training, best-practice guides, and real-time support. Intellivon also provides usage analytics so leaders can identify who needs help, accelerating adoption and stabilizing ROI curves across departments.
7. IT, Compliance, and Integration Delays
Enterprise deployments require collaboration across IT, security, privacy, and EHR teams. Long review cycles or integration backlogs delay go-lives and slow measurable impact. When internal processes move slowly, ROI appears delayed even though the AI platform is ready to perform.
Intellivon’s Solution:
Our deployment framework includes pre-built compliance documentation, templated security reviews, and EHR integration accelerators. We coordinate closely with IT and compliance teams to remove bottlenecks and ensure each site deploys smoothly and quickly.
Enterprise barriers can delay or distort early ROI signals, but each one is solvable with the right strategy. Intellivon’s deployment model addresses these barriers directly, ensuring ROI becomes visible faster and stays consistent across the organization.
How We Evaluate The ROI Of Your AI Scribe Deployments
At Intellivon, ROI comes from measurable improvements, and not assumptions. We track how AI scribes change documentation time, revenue flow, coding accuracy, compliance strength, and workforce stability. This gives your leadership a clear, evidence-driven view of value across all departments.
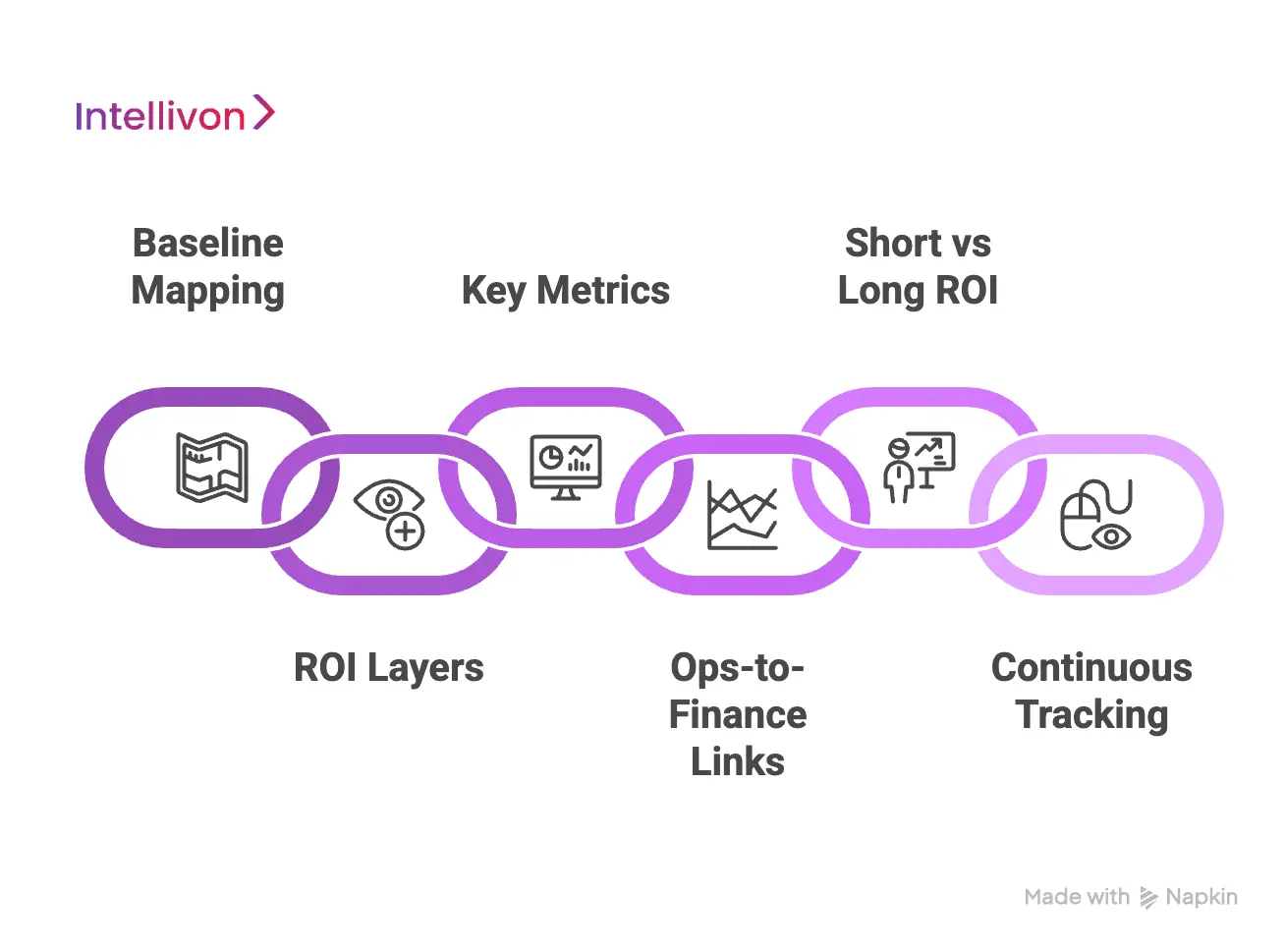
1. Baseline Mapping
We begin by measuring your current documentation workload. This includes EHR time per encounter, after-hours charting, chart completion lag, denial patterns, and coding variability.
We segment results by specialty and site to avoid blended averages that hide real issues. Every ROI gain is later compared to this baseline.
2. ROI Layers
ROI extends far beyond time savings. We measure impact across five areas: clinical productivity, documentation quality, operational efficiency, revenue integrity, and workforce stability. Each layer uses its own metrics and financial interpretation.
This multi-dimensional model shows both direct and indirect returns across your enterprise.
3. Key Metrics
We define all metrics upfront to keep ROI transparent. For time, we track encounter-level EHR usage and after-hours work. At the same time, for revenue, we measure denial rates, coding specificity, rework volumes, and billing timelines. At the end , for the workforce, we monitor overtime, burnout signals, and retention trends. These metrics feed ROI dashboards used throughout deployment.
4. Ops-to-Finance Links
Operational gains only matter when they translate into financial impact. We map every improvement to a downstream financial result. Faster chart closure accelerates coding and reimbursement.
Cleaner documentation reduces denials and supports better coding accuracy. Lower after-hours work stabilizes staffing and lowers burnout-related costs. We model each change across conservative, expected, and high-return scenarios.
5. Short vs Long ROI
AI scribes generate value in phases. Short-term gains include faster documentation, lower chart backlog, and reduced after-hours work. Long-term gains include fewer denials, cleaner claims, stronger coding performance, and lower turnover.
Intellivon structures ROI around these timelines so you see how value expands quarter by quarter.
6. Continuous Tracking
ROI tracking begins on day one. Intellivon monitors usage, specialty-level impact, and documentation trends throughout deployment.
When ROI varies across departments, we identify the cause, adjust workflows, and tune models to normalize performance. This ensures ROI continues to grow instead of flattening over time.
Intellivon’s ROI framework delivers a clear, defensible view of clinical, financial, and operational impact. We measure what matters and connect each improvement to meaningful outcomes, ensuring ROI grows consistently across your enterprise.
What Strong ROI Looks Like for AI Scribe Deployments
Strong ROI appears when AI scribes improve documentation workflows, accelerate billing outcomes, and stabilize the clinical workforce. These gains show up in several measurable areas that signal a direct, sustained return for enterprise healthcare systems.
1. Faster Documentation Cycles
Strong ROI appears when clinicians recover meaningful time every day. Most enterprise deployments see 15–25 minutes saved per clinician per day, depending on specialty and encounter volume. This reclaimed time increases capacity, reduces interruptions, and limits workflow bottlenecks. Faster documentation also lowers cognitive load across high-volume clinics.
2. Cleaner, More Accurate Notes
Improved note quality is a core ROI signal. AI scribes usually drive a 10–20% improvement in note accuracy, which supports stronger coding and fewer missing elements. Cleaner notes reduce ambiguity for coders and improve consistency across sites. These gains enable more predictable financial outcomes.
3. Lower Denials and Rework
Denials drop sharply when documentation improves. Organizations typically see an 8–15% reduction in documentation-related denials within the first 90 days. Fewer denials mean less rework and fewer coder queries, which shortens billing cycles. This directly improves reimbursement speed and overall revenue flow.
4. Higher Coding Specificity
Coding uplift is one of the strongest ROI contributors. AI-generated notes often enable a 5–12% increase in CPT coding specificity, particularly in primary care, endocrinology, cardiology, and ortho clinics. Higher specificity leads to cleaner claims, fewer downcoded encounters, and stronger per-visit revenue.
5. Reduced After-Hours Charting
A reduction in evening charting is a clear sign of ROI. Most enterprises report a 40–60% decrease in after-hours documentation after adoption. This lowers burnout risk and stabilizes workforce retention. Better work-life balance also reduces reliance on locum support, improving long-term financial performance.
6. Shorter Billing Timelines
Strong ROI includes faster reimbursement and smoother cash flow. When documentation improves, billing timelines shrink consistently. Combined with cleaner claims and fewer denials, organizations see more predictable movement through the revenue cycle. This reliability strengthens budgeting and financial planning.
7. Consistent Performance Across Sites
Sustained ROI requires uniform improvement across departments. AI scribes help standardize note structure, reduce specialty-level variability, and improve cross-site consistency. This removes bottlenecks and ensures downstream teams operate efficiently, regardless of clinic or specialty mix.
Strong deployments move multiple metrics at once, proving that AI scribes deliver system-wide value, and not isolated workflow gains.
Best Practices to Maximize ROI of AI Scribe Deployment
AI scribes deliver strong ROI when deployments are structured, consistent, and aligned across clinical, coding, and IT teams. These practices help enterprises reduce variability, stabilize performance, and unlock measurable improvements in time, revenue, and workflow efficiency.
1. Standardize Workflows
Consistent workflows improve accuracy and predictability. Standardized templates and encounter structures help AI scribes capture details reliably across sites. This reduces documentation variability and prevents downstream bottlenecks for coding and billing teams.
2. Train by Specialty
Specialties are documented differently. Tailored training ensures clinicians use the system correctly and receive accurate note drafts from day one. Specialty-specific alignment also improves completeness and reduces the need for corrections.
3. Monitor Early Signals
Early metrics show how fast ROI will scale. Track documentation time, chart closure patterns, denial rates, and after-hours work during initial rollout. Quick adjustments to workflows or audio setup help stabilize performance early.
4. Engage Coding Teams
Coders determine how documentation translates into revenue. Their feedback strengthens note structure and ensures AI-generated content captures every billable detail. This collaboration speeds up billing, reduces rework, and improves coding specificity.
5. Support Clinician Adoption
Clinician adoption drives ROI. Provide clear guidance, simple workflows, and real-time support to build confidence in the system. Strong adoption reduces friction, accelerates learning, and makes value visible across departments.
6. Optimize Audio Quality
Audio quality has a direct effect on accuracy. Better microphone placement, quieter rooms, and clear speaking habits improve transcription results. Consistent audio improves reliability and reduces correction time.
7. Align IT and Compliance
Deployment moves faster when IT and compliance teams collaborate from the start. Pre-defined integrations, security documentation, and review checklists minimize delays. This alignment strengthens compliance and keeps enterprise rollout on schedule.
8. Review ROI Regularly
ROI evolves over time. Monthly reviews help leaders track improvements in documentation speed, coding accuracy, denial reduction, and workforce stability. Continuous evaluation keeps teams aligned and ensures performance continues improving.
ROI increases when organizations deploy AI scribes with structure, specialty-level alignment, and continuous monitoring. These practices help enterprises convert documentation improvements into measurable financial and operational gains.
Conclusion
AI scribe deployments create meaningful ROI only when enterprises evaluate impact across documentation speed, coding accuracy, revenue cycle performance, and workforce stability. The strongest returns appear when clinical workflows improve, billing becomes faster, and clinicians spend less time working after hours.
Clear baselines, consistent measurement, and transparent financial links help leaders see how documentation improvements translate into real operational gains. As healthcare systems face tighter margins and rising workload demands, understanding ROI becomes essential. The organizations that measure it well will scale AI scribes with confidence and unlock sustainable value across every department they serve.
Scale ROI of Your AI Scribe Platform With Intellivon
At Intellivon, we build AI scribe platforms that deliver measurable ROI from day one. Our systems reduce documentation time, improve coding accuracy, and accelerate billing cycles, while fitting naturally into existing EHR workflows. Every deployment is engineered for clinical reliability, operational efficiency, and financial impact across large healthcare enterprises.
Why Partner With Intellivon?
- ROI-Driven Architecture: Designed to improve documentation speed, reduce denials, and strengthen revenue capture with measurable outcomes at each stage of deployment.
- Clinical-Grade AI Models: Specialty-tuned ASR, NLP, and summarization models trained on real-world clinical language for accuracy that clinicians can trust.
- Seamless EHR Integration: FHIR, HL7, and SMART on FHIR connectors ensure notes post to the correct chart, encounter, and timestamp—without manual effort.
- Enterprise-Scale Performance: Low-latency processing, high availability, and elastic scaling support multi-hospital usage during peak load without performance drops.
- Continuous Optimization: MLOps pipelines monitor drift, retrain models, and refine accuracy as usage grows to ensure long-term ROI expansion.
- Zero-Trust Security: Encryption across all layers, strict identity controls, audit trails, and continuous threat detection protect PHI without slowing workflows.
- Outcome-Focused Delivery: ROI frameworks, specialty-level benchmarks, and alignment with coding and billing teams ensure financial impact is visible early.
Book a strategy call with Intellivon to evaluate how AI scribe automation can increase throughput, reduce documentation burden, and deliver sustained ROI across your healthcare network.
FAQs
Q1. How do you measure the ROI of an AI scribe in a hospital?
A1. ROI is measured by comparing documentation time, chart closure speed, coding accuracy, and denial rates before and after deployment. Financial impact comes from faster billing, fewer reworks, and reduced after-hours work. Strong ROI appears when both clinical productivity and revenue performance improve together.
Q2. What metrics matter most when evaluating AI scribe performance?
A2. Key metrics include EHR time per encounter, after-hours charting, coding specificity, denial reduction, and billing timelines. Workforce indicators such as burnout reduction and retention also influence ROI. These metrics offer a complete view of clinical and financial impact.
Q3. How quickly can healthcare enterprises see ROI from AI scribes?
A3. Most organizations see early ROI within 60–90 days as documentation time drops and chart backlog reduces. Financial gains follow as coding improves and denials decrease. Long-term ROI grows as adoption stabilizes and staffing pressure declines.
Q4. Can AI scribes improve revenue cycle performance?
A4. Yes. Cleaner notes lead to fewer coding queries, faster claim submissions, and lower denial rates. This strengthens cash flow and supports more predictable billing outcomes across departments.
Q5. Why does clinician adoption matter for AI scribe ROI?
A5. Adoption determines how consistently the system generates time savings and documentation improvements. When clinicians trust and use the tool regularly, ROI accelerates across departments. Low adoption slows impact and delays financial improvement.