Clinicians today are overwhelmed by patient data, which is an incredible amount of information that they must handle for every decision. When working under time pressure in high-stakes environments, even the most skilled doctors can miss important details or overlook emerging patterns. A recent cross-hospital study found that 23% of seriously ill hospitalized patients experienced a diagnostic error, many with lasting or fatal consequences.
The fix is a clinical decision support system (CDSS) that works with healthcare providers to highlight the right information at the right time. This includes enhancing clinical decisions with smart systems that can analyze large datasets, identify potential risks, suggest evidence-based treatment options, and help reduce diagnostic errors. When done correctly, a CDSS becomes an essential tool that improves patient outcomes while lowering the cognitive load on care teams.
Over the years, we have created clinical decision support systems for healthcare organizations, aiming to improve diagnostic accuracy and streamline clinical workflows. Based on this experience, we are sharing this blog to guide you through the key components and process needed to build a CDSS that genuinely enhances care delivery.
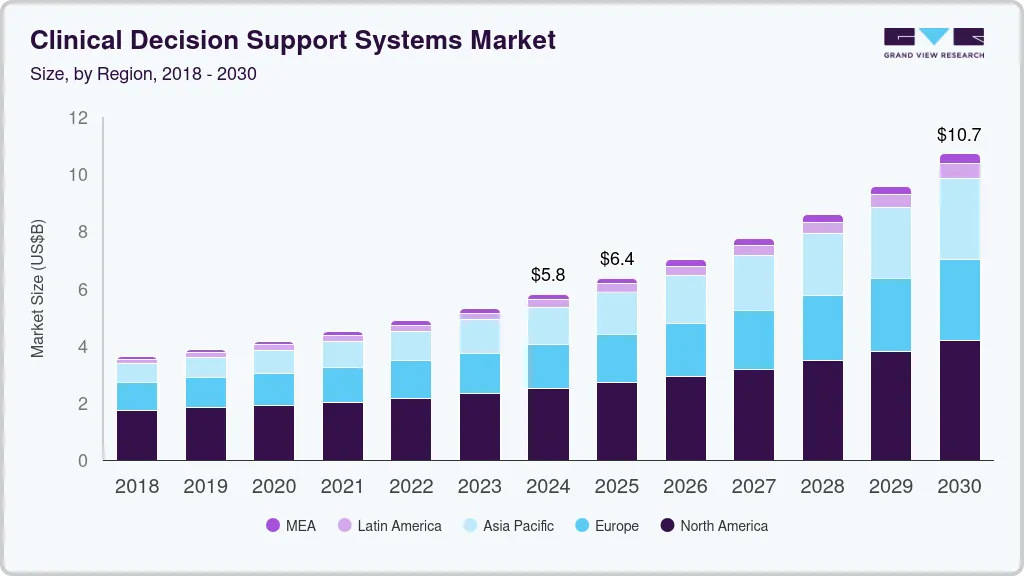
Key Takeaways of the Clinical Decision Support Market
The worldwide Clinical Decision Support Systems market was valued at approximately USD 5.79 billion in 2024 and is projected to grow to around USD 10.71 billion by 2030, expanding at a compound annual growth rate of 11.0% between 2025 and 2030.
Growth drivers of the CDSS market
- Rapid EHR and HCIT adoption is creating structured data and integration points for embedded CDSS across hospitals and health systems.
- Shift to value-based care and outcome-linked reimbursement, pushing providers to use CDSS to reduce errors, complications, and avoidable readmissions.
- Rising clinical complexity from aging populations and chronic disease burden, increasing reliance on tools that support diagnosis, risk stratification, and care planning.
- Advances in AI/ML, NLP, and predictive analytics are transforming CDSS from static rule-based alerts into high-value clinical intelligence platforms.
- Government initiatives promoting digital health, interoperability, and quality reporting are making CDSS central to meeting safety and compliance requirements.
- Regulatory frameworks for AI/ML SaMD and CDSS that enhance trust and accelerate enterprise procurement of FDA- and MDR-aligned solutions.
- Growth of cloud/SaaS delivery and API-based integration is lowering implementation barriers and enabling scalable enterprise deployments.
Enterprise Buying Behavior Is Shaping CDSS Architecture
- Large hospitals and IDNs prioritize enterprise-grade, deeply integrated CDSS embedded directly into CPOE and EHR workflows.
- On-premise or tightly governed cloud deployments are favored to meet strict data security, sovereignty, and governance requirements.
- Decision-makers increasingly reject standalone CDSS in favor of platform-level integration across clinical, imaging, and pharmacy systems.
AI-Enabled Diagnostics and FDA Oversight
- AI-enabled CDSS that influence diagnostic or treatment decisions increasingly qualify as Software as a Medical Device (SaMD).
- These systems now fall under FDA and EU MDR risk-based regulatory oversight.
- Regulatory guidance emphasizes Good Machine Learning Practice (GMLP), pre-specified change protocols, bias mitigation, and lifecycle monitoring.
- Hundreds of AI-enabled diagnostic and decision-support tools are now cleared or authorized, signaling a shift from experimentation to regulated clinical deployment.
Enterprise clinical decision support is rapidly evolving from basic alerting into regulated, AI-driven clinical intelligence embedded at the core of hospital operations. For large health systems, CDSS is becoming foundational to safe, compliant, and high-performance care delivery.
What Is a Clinical Decision Support System?
A Clinical Decision Support System is a digital intelligence layer embedded within healthcare IT that analyzes patient data, clinical knowledge, and predictive models to support real-time medical and operational decision-making across care environments.
In today’s hospital environment, data arrives faster than any human team can process on its own. Lab feeds, device signals, imaging, physician notes, and medication records all converge at once. A CDSS exists to organize that complexity into clear, time-sensitive guidance for care teams.
At the enterprise level, CDSS becomes part of the hospital’s core digital nervous system. It connects clinical knowledge with live patient data and turns both into practical insights that improve accuracy, safety, and consistency across departments.
Traditional CDSS vs Enterprise-Grade AI-Powered CDSS
| Traditional CDSS | Enterprise-Grade AI-Powered CDSS |
| Relies on fixed, manually coded rules | Learns from data and adapts over time |
| References static clinical guidelines | Uses real-time predictive modeling |
| Generates generic alerts | Delivers context-aware, probability-driven insights |
| Operates as a separate system | Embedded directly into EHR and CPOE workflows |
| Limited ability to handle complex cases | Designed for high-acuity, multi-condition care |
| Minimal audit and compliance tracking | Built with governance, validation, and audit trails |
The shift is fundamental. Traditional tools react to simple triggers. Enterprise-grade platforms reason across thousands of variables and evolve with clinical reality.
Core Functions of a Modern CDSS Platform
A modern CDSS is no longer confined to alerting clinicians about isolated risks. It operates as a multi-dimensional intelligence platform that supports diagnosis, therapy, population strategy, and hospital operations from a single decision layer.
Each function plays a distinct role, but the real value appears when they work together across the care continuum.
1. Diagnostic Support
This layer assists clinicians by correlating patient symptoms, lab values, imaging findings, and medical history to suggest likely diagnoses and flag atypical disease patterns. It acts as a second set of analytical eyes, especially valuable in complex or rare presentations.
2. Risk Stratification
Risk engines continuously assess patient data to identify those most likely to deteriorate, be readmitted, or experience complications. These insights allow care teams to intervene earlier rather than responding after a crisis occurs.
3. Care Pathway Optimization
The system recommends treatment pathways aligned with best practices while adapting to each patient’s evolving condition. This helps standardize care without removing clinical discretion.
4. Medication Safety and Interaction Checking
Drug safety engines validate dosages, detect contraindications, analyze multi-drug interactions, and adjust recommendations based on organ function, age, and comorbidities. This layer directly reduces preventable adverse drug events.
5. Population Health Intelligence
At the macro level, the platform aggregates patient data across cohorts to reveal trends in chronic disease management, preventive care gaps, and intervention outcomes. Leaders use these insights to guide long-term care strategies.
6. Operational Decision Intelligence
Beyond clinical care, CDSS supports decisions related to capacity planning, staffing levels, admission flow, and resource utilization. This bridges the gap between patient safety and financial performance.
A modern Clinical Decision Support System is no longer a narrow clinical tool. It is a cross-functional intelligence platform that shapes both medical and operational decisions at enterprise scale.
When these functions operate in unison, hospitals gain a clearer view of risk, performance, and opportunity across the entire care ecosystem.
Can CDSS Reduce the 60% Average Diagnostic Error?
Diagnostic errors remain one of healthcare’s most under-addressed patient safety risks. While clinicians operate under immense cognitive and time pressure, the clinical environment continues to grow more complex with expanding data volumes. A 2023 multi-disease analysis found that the average diagnostic error rate is approximately 11.1%, and for certain high-risk conditions, such as spinal infections, misdiagnosis can exceed 60%.
These numbers expose a systemic challenge that cannot be solved by clinical expertise alone. A modern Clinical Decision Support System (CDSS), when engineered correctly, directly targets this gap by augmenting human judgment with real-time, data-driven clinical intelligence.
1. Why Diagnostic Errors Persist
Diagnostic failures often stem from information overload, fragmented data sources, and time-compressed decision-making. Clinicians must synthesize labs, imaging, medication history, comorbidities, and evolving symptoms simultaneously.
Even subtle delays or missing correlations can lead to incorrect or delayed diagnoses, particularly in emergency, ICU, and complex specialty care.
Without an intelligent system to surface patterns across this data in real time, critical signals are easily buried inside routine clinical noise.
2. CDSS Targets Root Causes of Misdiagnosis
An enterprise-grade CDSS intervenes at the most failure-prone points in the diagnostic workflow. It continuously correlates structured EHR data, imaging results, lab trends, and unstructured clinical notes to identify deviations, hidden risk patterns, and probability-weighted diagnostic differentials.
Instead of relying solely on static alerts, predictive CDSS platforms actively anticipate deterioration, flag atypical disease trajectories, and validate clinician hypotheses against population-level evidence.
This shifts diagnostic decision-making from reactive pattern recognition to proactive clinical risk intelligence.
3. AI-Driven Decision Support Improves Diagnostic Accuracy
Real-world studies reinforce the scale of the problem CDSS aims to solve. A cross-hospital investigation of seriously ill hospitalized adults found that 23% of patients experienced a diagnostic error, many associated with long-term harm or fatal outcomes.
Parallel analyses from organizations such as Johns Hopkins Medicine continue to demonstrate how frequently diagnostic errors arise across both common and rare disease pathways.
By systematically analyzing what individual clinicians cannot continuously compute, AI-powered CDSS platforms consistently outperform manual detection of early clinical deterioration and atypical disease progression.
CDSS Reduces Error Without Replacing Clinical Judgment
Effective CDSS systems operate as a clinical co-pilot, providing ranked insights, probability-weighted risks, and evidence-linked recommendations while keeping final authority in human hands. This human-in-the-loop architecture improves safety, preserves clinician autonomy, and strengthens adoption across specialties.
As these systems become more explainable and workflow-embedded, clinicians’ trust continues to rise, particularly in radiology, oncology, cardiology, and acute care medicine.
Use Cases of Enterprise Clinical Decision Support Systems
Enterprise Clinical Decision Support Systems are used across diagnostics, acute care, chronic disease management, medication safety, population health, and hospital operations to reduce risk, improve outcomes, and standardize care at scale.
Below are the most common and high-impact enterprise use cases where CDSS delivers measurable clinical and financial value.
1. Diagnostic Decision Support
In emergency and critical care settings, speed and accuracy determine outcomes. CDSS supports clinicians by continuously analyzing symptoms, vitals, lab trends, and imaging findings to surface likely diagnoses and rare but high-risk conditions.
This is especially valuable in cases where early signs are subtle or evolve quickly. Stroke, sepsis, pulmonary embolism, and internal bleeding are common examples where early CDSS-driven pattern recognition can change patient trajectories within minutes.
For enterprise leaders, this translates into fewer missed diagnoses, reduced litigation exposure, and improved patient safety metrics across flagship facilities.
2. Predictive Risk Stratification
Modern CDSS platforms analyze evolving vitals, lab fluctuations, medication response, and comorbidities to predict who is likely to deteriorate or be readmitted.
These insights trigger early interventions before a crisis occurs. Rapid response teams can act sooner. ICU transfers become proactive instead of reactive. Discharge planning becomes more precise.
From a business standpoint, this directly impacts length of stay, penalty-driven readmissions, and ICU utilization costs.
3. Medication Safety and Clinical Pharmacology
Medication errors remain one of the most expensive and preventable sources of patient harm. Enterprise CDSS platforms validate dosages, detect contraindications, analyze multi-drug interactions, and adjust recommendations based on renal function, age, and disease severity.
In oncology, cardiology, and transplant medicine, this layer becomes mission-critical. It protects both clinical outcomes and institutional liability.
For leadership teams, the value appears in fewer adverse drug events, lower malpractice exposure, and stronger regulatory audit performance.
4. Evidence-Based Care Pathway
Variation in care is one of the largest hidden cost drivers in large health systems. CDSS helps standardize treatment without eliminating clinical judgment.
By embedding evidence-based guidelines directly into daily workflows, the system ensures that care decisions align with best practices while still adapting to patient-specific context. Deviations are flagged, not blocked, preserving autonomy while improving consistency.
Over time, this creates more predictable outcomes, stronger reporting, and tighter alignment with value-based care models.
5. Chronic Disease Management
At the population level, CDSS shifts from reactive treatment to a preventive strategy. It identifies care gaps, flags high-risk cohorts, and tracks long-term disease progression across thousands or millions of patients.
This is widely used in diabetes, cardiovascular disease, respiratory disease, and oncology follow-up programs. Leaders gain visibility into intervention effectiveness, preventive compliance, and long-term outcomes.
This intelligence informs payer negotiations, community health investments, and enterprise growth strategy.
Operational and Capacity Decision Support
Beyond bedside care, CDSS increasingly support hospital operations. It forecasts bed demand, predicts admission surges, optimizes staffing levels, and models patient flow in real time.
In high-volume systems, even small efficiency gains translate into millions in recovered capacity. Delayed discharges, overcrowded ICUs, and underutilized units become data-driven optimization problems instead of persistent bottlenecks.
Enterprise Clinical Decision Support Systems now influence far more than individual clinical decisions. They shape how hospitals diagnose, treat, prevent, and operate at scale. When deployed across these core use cases, CDSS becomes a structural advantage rather than a supporting tool.
Key Architecture of a Clinical Decision Support System
The architecture of a Clinical Decision Support System is a multi-layered enterprise framework that integrates clinical data sources, analytics engines, AI models, workflow systems, and governance controls to deliver real-time, audit-ready clinical intelligence inside hospital operations.
Below are the core layers that make a CDSS production-ready inside large health systems.
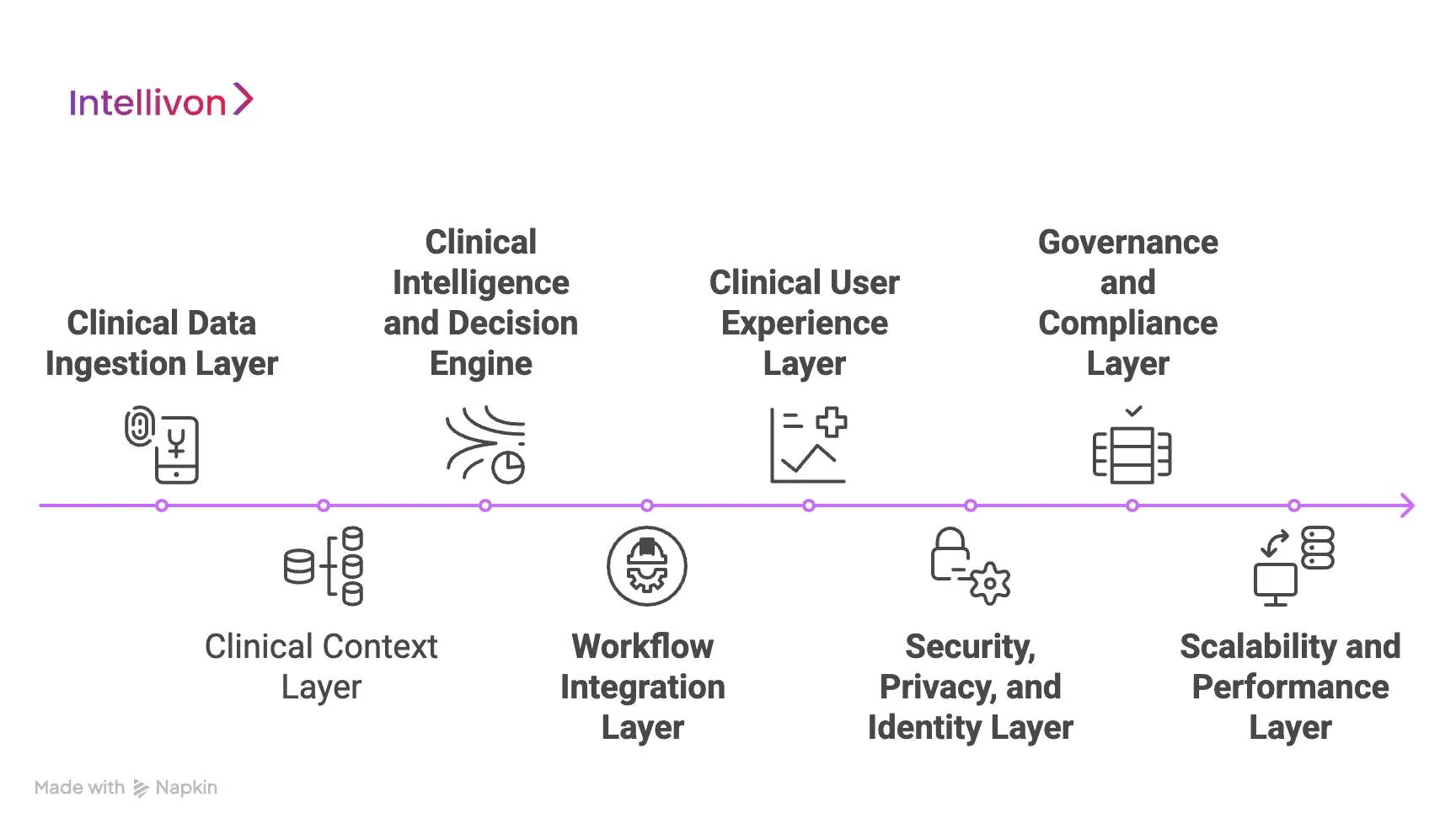
1. Clinical Data Ingestion Layer
This is where the system connects to the hospital’s digital ecosystem. It pulls structured and unstructured data from EHRs, laboratory systems, imaging platforms, pharmacy systems, medical devices, and remote monitoring tools.
The key architectural requirement here is reliability under load. Data must flow continuously, with near-zero latency and no loss during peak clinical activity. Interoperability standards act as the connective tissue, but enterprise engineering ensures the pipes never break.
For leadership teams, this layer determines how quickly new facilities, departments, and partner systems can be added without disrupting live operations.
2. Clinical Context Layer
Raw healthcare data is inherently inconsistent, where lab units can vary, diagnoses appear in different coding systems, and physician notes are unstructured and often incomplete.
This layer cleans, normalizes, and contextualizes incoming data so that downstream intelligence remains accurate. It maps clinical terms, resolves patient identities, aligns timestamps, and converts disparate inputs into a unified clinical truth.
Without this layer, even the most advanced AI models produce unreliable output. With it, decision support becomes clinically defensible.
3. Clinical Intelligence and Decision Engine
This is the analytical core of the platform. It contains the rule engines, predictive models, and inferencing logic that transform data into decisions.
In practical terms, this layer answers questions such as:
- Is this patient deteriorating faster than expected?
- Does this treatment plan align with outcomes in similar cases?
- Is this medication likely to trigger a complication given the current labs?
In enterprise systems, this engine blends deterministic clinical rules with probabilistic machine learning models. That hybrid approach preserves guideline compliance while enabling adaptive intelligence.
4. Workflow Integration Layer
Even the most accurate recommendation has no value if it arrives at the wrong time or in the wrong place. This layer embeds intelligence directly into daily clinical workflows.
Insights surface inside order entry, chart review, medication prescribing, discharge planning, and multidisciplinary rounds. Alerts are prioritized, and non-urgent guidance is delivered asynchronously.
Architecturally, this layer protects clinicians from alert fatigue while ensuring that critical risks interrupt workflows only when necessary. Adoption depends on this balance.
5. Clinical User Experience Layer
This is what clinicians and operational leaders actually see. It translates complex analytics into intuitive dashboards, ranked recommendations, and explainable risk indicators.
For bedside teams, the interface must be fast, uncluttered, and clinically relevant. For leadership, it must provide population-level visibility into outcomes, bottlenecks, and trends.
Poor design here undermines trust, whereas strong design turns decision support into a daily habit rather than a compliance requirement.
6. Security, Privacy, and Identity Layer
Every architectural component sits inside a security framework that controls who can access what, when, and under which conditions.
This layer enforces identity verification, role-based access, encryption, session monitoring, and breach detection. It must operate invisibly while meeting the strictest healthcare security expectations.
For enterprise risk teams, this is not an IT feature. It is a legal, financial, and reputational safeguard.
7. Governance and Compliance Layer
A production CDSS must explain not only what decision was made, but also how and why it was made. This layer records model versions, decision logic, data sources, clinician interactions, and override behavior.
It supports audits, regulatory reviews, clinical validations, and continuous quality improvement. It also enables leadership to prove that the system behaves safely over time, not just at launch.
Without governance baked into architecture, regulatory exposure grows with every deployment.
8. Scalability and Performance Layer
Healthcare never stops. Because of this, a CDSS must run during peak patient volumes, disasters, cyber incidents, and infrastructure failures.
This layer ensures high availability, automated failover, load balancing, data backups, and real-time monitoring. It is what allows the platform to grow from one hospital to a national network without re-engineering the core.
For boards and executives, this determines whether CDSS can support long-term expansion and digital transformation goals.
When each of these layers is designed with clinical reality and regulatory pressure in mind, CDSS evolves from a helpful tool into a strategic clinical intelligence platform.
AI and Machine Learning in Clinical Decision Support Systems
AI and machine learning inside a Clinical Decision Support System enable real-time risk prediction, diagnostic pattern recognition, treatment optimization, and continuous model learning using live clinical data and historical outcomes.
1. Predictive Analytics
Predictive models look forward rather than backward. They analyze subtle shifts in vitals, labs, medication response, and disease progression to estimate what is likely to happen next.
In practice, this allows care teams to:
- Identify sepsis hours before visible clinical collapse
- Predict ICU transfers before respiratory failure
- Anticipate readmission risk before discharge
- Flag silent bleeding, infection, or organ failure early
From a business perspective, this directly affects mortality, ICU utilization, penalties, and length of stay. Predictive intelligence shifts hospitals from reactive medicine to anticipatory care.
2. Machine Learning for Pattern Recognition
Human clinicians recognize patterns through experience. Machine learning does the same across millions of historical cases simultaneously.
Inside CDSS, ML models are used to:
- Detect rare disease signatures hidden inside common symptoms
- Correlate imaging, labs, and notes that appear unrelated at first glance
- Learn which treatment pathways perform best for specific sub-populations
- Adapt to local patient demographics rather than relying on generic datasets
This is especially powerful in oncology, critical care, cardiology, and complex diagnostics, where patient variability makes guideline-only decision-making insufficient.
For enterprise systems, the advantage is cumulative. The longer the platform runs, the more accurate it becomes.
3. Natural Language Processing
A large portion of clinical truth sits outside structured fields. It lives in progress notes, shift handovers, radiology narratives, pathology interpretations, and discharge summaries.
Natural Language Processing allows a CDSS to read and understand this narrative data. It extracts symptoms, findings, disease progression, and clinician intent, then connects them to structured signals like labs and medications.
In real deployments, this closes a major intelligence gap. Without NLP, decision support sees only half the patient story. With it, CDSS gains full clinical context.
4. AI-Driven Treatment Optimization
Beyond diagnosis, advanced CDSS platforms evaluate how patients respond to specific therapies across time. They learn which interventions lead to faster recovery, fewer complications, or lower mortality for specific patient profiles.
This enables:
- Personalized therapy recommendations
- Smarter escalation or de-escalation of care
- Continuous refinement of clinical pathways
- Evidence-backed deviation from rigid guidelines when justified
For leadership teams, this transforms CDSS into a long-term learning system rather than a fixed software asset.
5. Human-in-the-Loop
Enterprise CDSS is not autonomous medicine. Every recommendation is filtered through human judgment. Clinicians can accept, modify, or override suggested actions.
These interactions become part of the learning cycle. The system observes where clinicians disagree with AI and why. Over time, this feedback strengthens both the model and the trust relationship between clinicians and the platform.
This human-in-the-loop structure is what keeps CDS clinically safe, legally defensible, and widely adopted.
6. Model Governance and Bias Control
AI inside healthcare cannot operate like consumer technology. Models must be tested, monitored, validated, and revalidated continuously.
Enterprise-grade CDSS platforms include controls to:
- Track model performance over time
- Detect bias across age, gender, ethnicity, and comorbidities
- Validate predictions against real-world outcomes
- Roll back models safely if performance degrades
- Document every change for audit and regulatory review
For executives, this governance layer is what converts AI from a research experiment into a regulated clinical asset.
AI, machine learning, and predictive analytics turn a Clinical Decision Support System into a living clinical intelligence platform. When governed correctly, it gives them earlier signals, deeper context, and evidence-backed confidence at the exact moment decisions carry the greatest risk.
How We Build an Enterprise Clinical Decision Support System
At Intellivon, we approach Clinical Decision Support as a safety-critical layer of healthcare infrastructure. These systems influence diagnosis, treatment direction, patient outcomes, and institutional risk. Because of that, we do not treat CDSS as a software project. We treat it as an enterprise transformation initiative.
Our build process is shaped by how real hospitals function under pressure. It is designed to survive regulatory audits, clinician scrutiny, and the operational realities of large, multi-facility health systems.
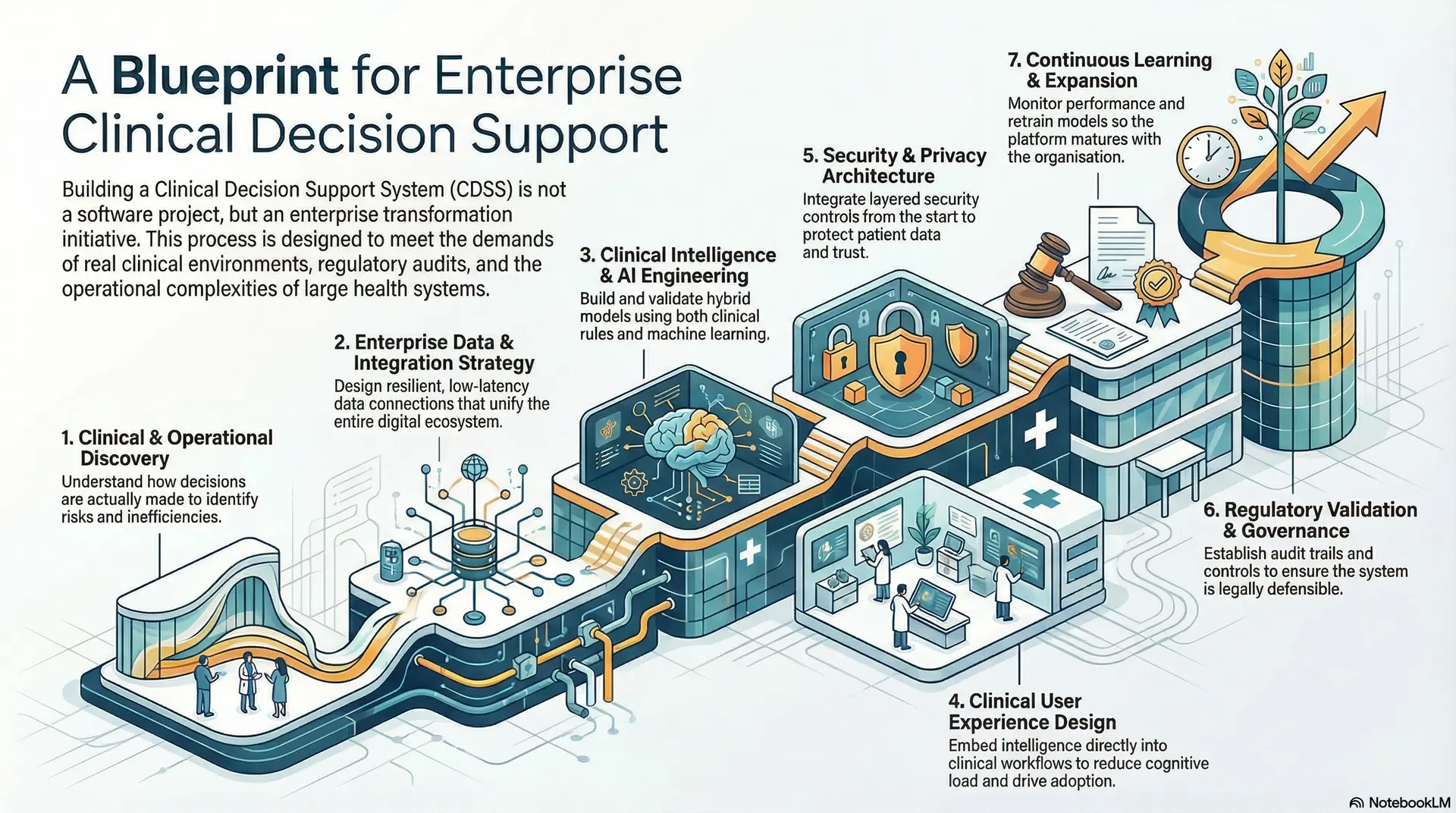
1. Clinical and Operational Discovery
We begin by understanding how decisions actually occur inside your organization. This goes beyond workflow diagrams and policy documents. We observe live clinical environments, study how physicians interpret data under time pressure, and identify where uncertainty, delays, and overrides most often occur.
This phase clarifies where diagnostic ambiguity creates patient risk, where operational inefficiencies affect outcomes, and where compliance exposure is highest. Just as importantly, it aligns clinical priorities with executive objectives around safety, cost, and performance. Without this alignment, even the most advanced CDSS struggles to gain meaningful traction.
2. Enterprise Data and Integration Strategy
Once objectives are defined, we design how data will move across the enterprise. Large health systems run on complex digital ecosystems that include multiple EHRs, laboratory platforms, imaging systems, pharmacy tools, medical devices, and external data exchanges.
Our integration strategy focuses on building resilient, low-latency connections that function reliably under peak clinical load. Data must flow continuously without interrupting live care delivery. At this stage, we also establish data governance rules so that patient identity, time alignment, and clinical context remain consistent across every source.
This layer ultimately determines how scalable and future-ready the CDSS will be as the organization adds new facilities, specialities, and partners.
3. Clinical Intelligence and AI Model Engineering
With clean, reliable data in place, we engineer the clinical intelligence layer. This includes building and validating predictive models, diagnostic inference engines, and decision logic tailored to your patient population and clinical use cases.
We combine evidence-based clinical rules with machine learning models trained on real-world outcomes. This hybrid approach ensures that the system remains aligned with medical guidelines while adapting to evolving disease patterns and treatment responses.
Every model is benchmarked against historical performance and validated with clinical stakeholders before it ever influences live decisions. At this stage, the goal is not just accuracy. It is clinical legitimacy and long-term trust.
4. Clinical User Experience Design
Decision support only delivers value when it appears inside everyday clinical workflows. We therefore embed intelligence directly into order entry, chart review, medication prescribing, and care coordination environments rather than forcing clinicians to consult a separate application.
User experience design focuses on cognitive load reduction. Information is prioritized, not flooded. High-risk insights interrupt workflows only when necessary. Lower-risk guidance appears contextually without slowing down care delivery.
This phase is where adoption is won or lost. If the system does not respect clinical time and attention, it will not be trusted or used.
5. Security Architecture and Privacy Engineering
Before any clinical system moves into live environments, it must meet strict privacy and security expectations. We design CDSS platforms with layered security controls that govern identity, access, encryption, monitoring, and breach detection across every component.
Security is integrated into the architecture from the start rather than added later. This ensures that patient data remains protected across clinical, operational, and analytical workflows without disrupting usability. From an enterprise standpoint, this layer protects institutional reputation, legal standing, and long-term digital trust.
6. Regulatory Validation and Governance Controls
Every enterprise CDSS must operate within formal regulatory boundaries. At this stage, we establish audit trails, decision traceability, model version control, and documentation for clinical validation and regulatory review.
This includes defining how recommendations are generated, how clinicians interact with them, how overrides are recorded, and how model performance is monitored over time. Governance frameworks ensure that the system remains defensible years after deployment, not just at launch. For leadership teams, this is what converts CDSS from experimental technology into a regulated, enterprise-grade clinical asset.
8. Continuous Learning and Expansion
After go-live, CDSS enters a continuous improvement cycle. Models are retrained as populations change, clinical pathways evolve with updated evidence, and new use cases are added as organizational priorities shift.
Performance monitoring, bias detection, and outcome tracking remain active throughout the system’s lifecycle. This ensures the platform matures alongside the enterprise rather than becoming outdated after initial success.
When designed with clinical reality, regulatory rigor, and enterprise scalability in mind, CDSS becomes a durable intelligence foundation that improves safety, consistency, and organizational performance year after year.
Tech Stack Used in Clinical Decision Support System Development
The technology stack of a Clinical Decision Support System typically includes secure data integration frameworks, cloud or hybrid infrastructure, AI and machine learning platforms, interoperability standards, clinical-grade databases, security layers, and analytics visualization tools designed for regulated healthcare environments.
The technologies used must therefore support real-time performance, regulatory compliance, long-term scalability, and continuous improvement at enterprise scale.
Frontend and Interface Technologies
The clinical interface must be fast, responsive, and familiar to care teams. Most enterprise CDSS platforms use modern web frameworks such as React, Angular, or Vue.js to build dashboards, alert panels, and embedded EHR overlays.
These interfaces are typically rendered within existing clinical workstations rather than as standalone apps. Integration with EHR frontends such as Epic and Cerner ensures that clinicians do not have to switch contexts during critical workflows. The goal at this layer is speed, clarity, and zero disruption to daily practice.
2. Backend Application
The backend layer handles decision orchestration, rule execution, data routing, and system logic. Enterprise CDSS platforms are commonly built using Node.js, Java with Spring Boot, or .NET Core.
Microservices are typically containerized using Docker and orchestrated with Kubernetes. This allows each clinical service, such as risk scoring, alerting, or drug interaction checking, to scale independently while maintaining high availability across hospital networks.
3. Clinical Databases Tech
Clinical decision support depends on both transactional and analytical data. For real-time workloads, relational databases such as PostgreSQL, MySQL, and Oracle Database are widely used.
For large-scale analytics and model training, enterprise deployments rely on data lakes and warehouses such as Amazon S3 with Snowflake, Google BigQuery, or Azure Data Lake. This separation ensures that live clinical performance is never compromised by heavy analytical workloads.
4. Healthcare Interoperability Tech
CDSS platforms must continuously exchange data with EHRs, imaging systems, labs, pharmacy platforms, and external health networks. Healthcare messaging and APIs are handled using standards such as FHIR, HL7, and DICOM.
Integration engines such as Mirth Connect and Rhapsody manage message routing, transformation, and reliability across hospital ecosystems. These tools ensure that data arrives in real time and in the right clinical context.
5. AI and Machine Learning Technologies
Predictive and adaptive intelligence inside CDSS is built using platforms such as TensorFlow, PyTorch, and scikit-learn.
Model lifecycle management is often handled using MLflow, while large-scale analytics and streaming insights rely on platforms such as Apache Spark and Apache Kafka.
For clinical text understanding, natural language processing pipelines are constructed using spaCy, Hugging Face, and transformer-based language models fine-tuned on medical data.
6. Security and Access Control Tech
Security layers control how patient data is accessed and protected across the CDSS platform. Identity and access management is often implemented using Okta or Auth0.
Data encryption and key management rely on HashiCorp Vault and cloud-native key services. Network security is strengthened with zero-trust frameworks, intrusion detection systems, and continuous vulnerability scanning across all workloads.
7. Cloud and Infrastructure Techn
Enterprise CDSS platforms are deployed on HIPAA-compliant cloud and hybrid infrastructure such as Amazon Web Services, Microsoft Azure, and Google Cloud Platform.
These environments provide elastic compute, global redundancy, disaster recovery, and performance monitoring that on-premise infrastructure alone cannot match. Many enterprises adopt hybrid deployments to retain sensitive workloads on private infrastructure while scaling analytics and AI in the cloud.
8. Monitoring and Audit Technologies
System health and clinical traceability depend on continuous monitoring and logging. Tools such as Prometheus, Grafana, and ELK Stack provide real-time visibility into uptime, latency, and data integrity.
Clinical audit trails and security event monitoring are strengthened using enterprise SIEM platforms such as Splunk. These records support regulatory audits, incident response, and long-term quality assurance.
The technology stack behind a Clinical Decision Support System reflects its role as safety-critical infrastructure.
Conclusion
Clinical Decision Support is no longer a peripheral innovation. It is becoming a structural requirement for health systems that must balance safety, scale, compliance, and performance in real time.
When designed with the right architecture, governance, and intelligence layer, CDSS shifts decision-making from reactive to predictive and from fragmented to system-wide. The result is not only better clinical outcomes, but also more resilient operations and stronger financial control.
Build a Clinical Decision Support System With Intellivon
At Intellivon, we build enterprise-grade Clinical Decision Support Systems that unify real-time clinical intelligence, predictive analytics, evidence-based guidance, and compliance-first governance into one secure decision operating layer.
Our platforms integrate seamlessly with EHRs, labs, imaging systems, pharmacy platforms, and care pathways without disrupting live hospital workflows or clinical autonomy.
Why Partner With Intellivon?
- Compliance-First Architecture: Every deployment aligns with HIPAA, GDPR, FDA SaMD considerations, EU MDR, and regional healthcare regulations with audit-ready governance embedded across clinical and AI layers.
- Interoperability-Driven Platform Engineering: Native support for FHIR, HL7, DICOM, and secure enterprise APIs enables real-time integration across EHRs, LIS, RIS, PACS, RCM systems, and population health platforms.
- Enterprise-Grade Clinical Intelligence: Our platforms support diagnostic decision support, predictive risk stratification, medication safety, and evidence-based care pathways across multi-hospital, multi-specialty networks.
- Human-in-the-Loop AI Governance: Every recommendation is explainable, traceable, and governed with clinician override, model versioning, and continuous performance monitoring for long-term regulatory defensibility.
- Zero-Trust Security Framework: Identity-first access controls, end-to-end encryption, immutable audit logs, and continuous threat detection protect PHI across all clinical workflows.
- Hybrid Cloud and On-Prem Deployment Flexibility: Architectures support regulated hybrid and private deployments for enterprises with data residency, latency, or sovereign cloud requirements.
Book a strategy call with Intellivon to explore how a custom-built Clinical Decision Support System can improve diagnostic accuracy, reduce clinical risk, strengthen regulatory compliance, and scale safe, predictive care across your enterprise.
FAQs
Q1. How long does it take to build an enterprise Clinical Decision Support System?
A1. Most enterprise CDSS projects take 6–12 months, depending on integrations, AI complexity, and regulatory scope. Discovery and architecture come first, followed by phased clinical deployment. At Intellivon, we prioritize staged rollouts so hospitals start seeing value early rather than waiting for a single full launch.
Q2. What regulations apply to enterprise Clinical Decision Support Systems?
A2. Enterprise CDSS must comply with HIPAA for data privacy and often fall under Software as a Medical Device (SaMD) rules. In the US, this brings oversight from the U.S. Food and Drug Administration. In Europe, the EU MDR applies. Governance must be engineered into the platform from the start.
Q3. Can a Clinical Decision Support System integrate with existing EHRs?
A3. Yes. Enterprise CDSS platforms integrate directly with hospital systems using FHIR, HL7, and DICOM. The system embeds into existing workflows, so clinicians do not need to switch platforms.
Q4. How accurate are AI-powered Clinical Decision Support Systems?
A4. Accuracy depends on data quality, validation rigor, and continuous monitoring. In real-world deployments, well-governed CDSS consistently improve early detection of deterioration and medication risk. Clinicians always retain final authority through human-in-the-loop controls.
Q5. What is the ROI of deploying a Clinical Decision Support System at scale?
A5. ROI comes from reduced diagnostic errors, fewer adverse events, shorter hospital stays, and lower readmission penalties. Financial gains also include reduced malpractice exposure and improved value-based care performance. Most enterprises see measurable impact within 12–18 months of full deployment.