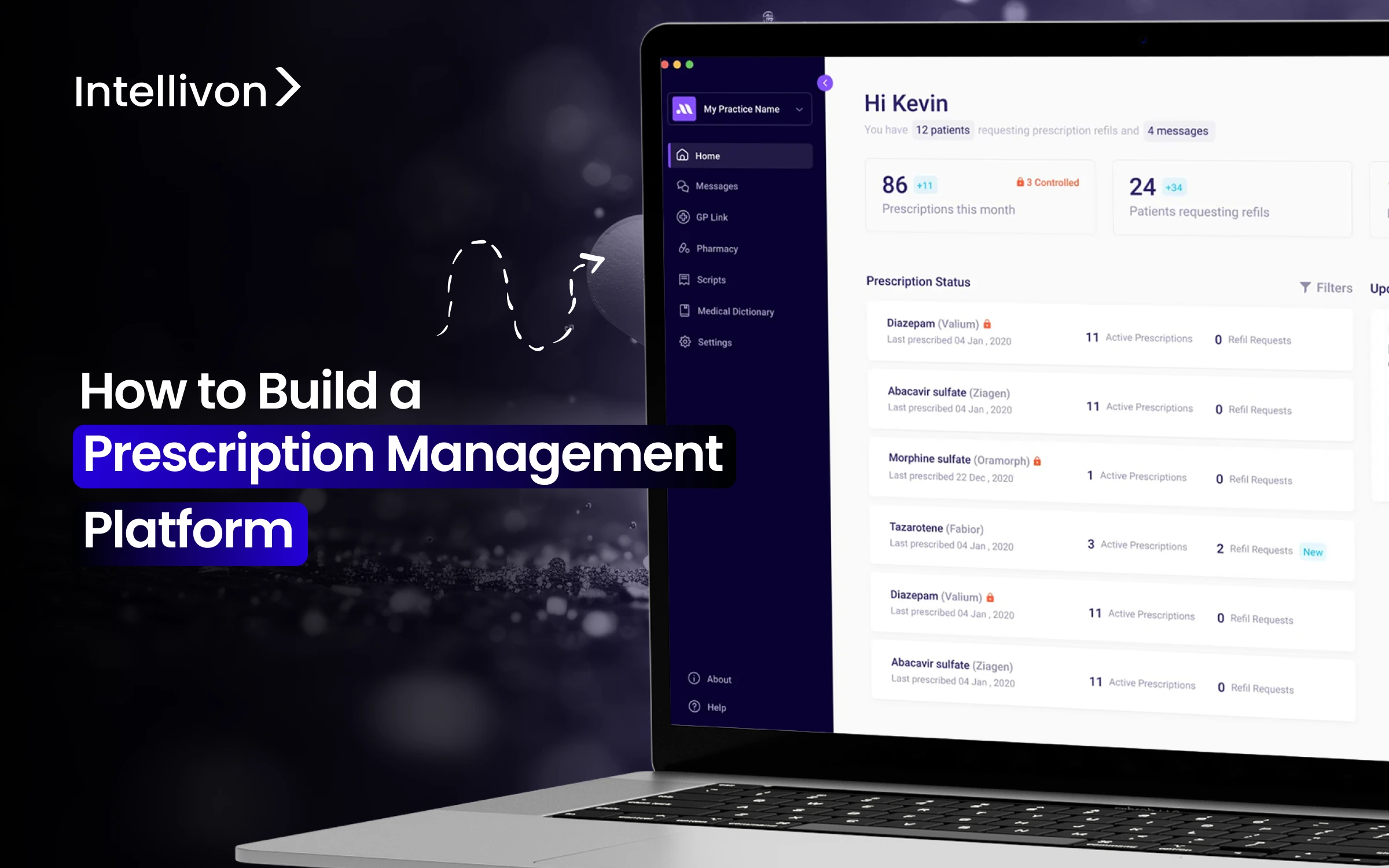
Healthcare organizations lose millions in value each year because their prescription management systems are fragmented. Disconnected prescribing tools, manual approvals, and pharmacy silos bring compliance risks, delay treatment, and increase the chance of medication errors. On a large scale, these gaps put a strain on clinical teams and expose the organization to regulatory scrutiny.
Legacy systems do not communicate well between departments or facilities. At the same time, compliance is harder to enforce as care delivery expands through mergers, new locations, or digital channels. Prescription management platforms impact risk management, patient safety, and the ability to grow without disruption. A well-designed platform creates a governed, traceable workflow for prescriptions that supports growth rather than limits it.
At Intellivon, we have spent more than a decade creating healthcare platforms that combine interoperability and workflow improvement. Based on this experience, we are using this blog to explain the essential steps to build a prescription management platform that supports real clinical workflows, enterprise compliance, and long-term operational strength.
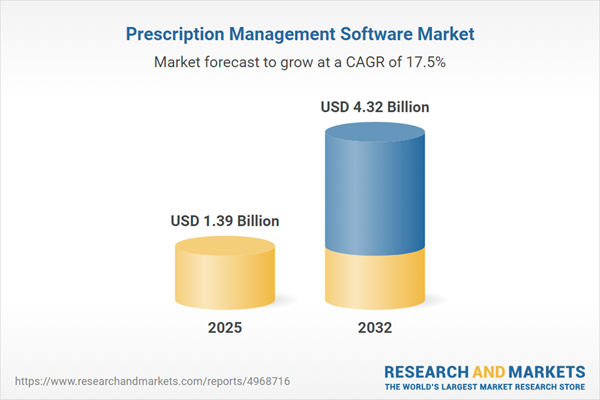
Key Takeaways Of The Prescription Management Platform Market
The prescription management software market is scaling quickly across global healthcare systems. The market grew from USD 1.19 billion in 2024 to USD 1.39 billion in 2025 and is projected to reach USD 4.32 billion by 2032, growing at a steady 17.48% CAGR.
This growth reflects a shift in how large healthcare organizations view prescription management. It is no longer an operational add-on. It is becoming core digital infrastructure.
Key Growth Drivers
- Rising prescription volumes and chronic disease prevalence increase pressure to reduce medication errors and adverse drug events.
- Regulatory mandates for e-prescribing and controlled substance prescriptions accelerate platform adoption across regions.
- Healthcare cost pressure and workforce shortages force automation of prescribing, reconciliation, dispensing, and refill workflows.
Technology and Solution Trends
- Integrated platforms combining prescribing, pharmacy, billing, and analytics are outperforming siloed systems.
- AI-driven medication optimization and predictive adherence modeling are emerging as competitive differentiators.
- Patient-facing tools such as refill apps, reminders, and home delivery are increasingly embedded into enterprise systems.
Regional Outlook and Opportunity Areas
- North America leads adoption due to mature EHR ecosystems and safety-focused reimbursement models.
- Asia-Pacific is the fastest-growing region, driven by hospital digitization and national e-health initiatives.
- High-value opportunities favor interoperable enterprise platforms and AI-enhanced prescribing intelligence.
Prescription management platforms are strategic systems that protect revenue, reduce clinical risk, and support scalable care delivery across complex, distributed operations.
What Is a Prescription Management Platform?
A prescription management platform is an enterprise system that digitizes, governs, and automates the full medication lifecycle from prescribing to fulfillment, monitoring, and audit. Instead of relying on disconnected tools or manual steps, it creates a governed workflow that moves prescriptions securely from clinicians to pharmacies and patients.
At its core, the platform standardizes prescription creation. It enforces structured orders, clinical validations, and secure digital signatures. From there, it manages approvals, pharmacy routing, refills, and insurance checks in a single system.
For large healthcare organizations, this platform functions as a regulated infrastructure. It integrates with EHRs, pharmacy systems, payer networks, and patient applications using healthcare interoperability standards. Every prescription action is logged, traceable, and auditable.
Types of Prescription Management Platforms
Enterprise prescription management platforms exist in multiple forms, each designed to solve a specific layer of prescribing, dispensing, compliance, or population-scale medication management.
Prescription management platforms are not one-size-fits-all. Understanding these categories helps enterprises identify gaps in their current ecosystem and invest where impact is highest.
1. Prescriber-Centric E-Prescribing Platforms
These platforms focus on digitizing the act of prescribing at the point of care. They support structured orders, digital signatures, drug interaction checks, and controlled substance workflows.
They are often the first step in moving away from paper prescriptions. However, they usually stop at order creation rather than managing the full medication lifecycle.
Used in: Physician groups, outpatient clinics, ambulatory networks, specialty practices.
2. EHR-Embedded Prescription Management Modules
Many enterprise EHR systems include native prescription functionality tightly coupled with patient records. This reduces context switching and aligns prescribing with clinical documentation.
While effective for core workflows, these modules can struggle in multi-vendor environments or complex pharmacy networks.
Used in: Hospitals, integrated delivery networks, large health systems running a single EHR vendor.
3. Pharmacy-Centric Medication Management Platforms
These platforms prioritize dispensing, inventory control, medication reconciliation, and pharmacy compliance. They focus on what happens after a prescription is written.
They provide strong operational efficiency but limited control over upstream prescribing behavior.
Used in: Hospital pharmacies, retail pharmacy chains, specialty pharmacies, mail-order operations.
4. End-to-End Prescription Management Platforms
These systems manage the complete medication journey. Prescribing, pharmacy routing, refills, adherence tracking, prior authorization, and audits operate within one governed framework. They are designed for scale, regulatory complexity, and multi-site operations.
Used in: Multi-hospital systems, national provider networks, and enterprises growing through mergers or acquisitions.
5. Payer-Integrated Prescription and Authorization Platforms
These platforms sit between providers and insurers. They enforce formularies, manage prior authorizations, and validate coverage in real time.
They reduce prescribing delays caused by insurance friction but rely heavily on integration quality.
Used in: Payer-provider organizations, value-based care networks, and large accountable care organizations.
6. Chronic Care and Population Medication Platforms
Built for longitudinal medication management, these platforms focus on adherence, polypharmacy risk, and cohort-based insights rather than single encounters. They support proactive medication optimization across large patient populations.
Used in: Chronic disease programs, population health initiatives, and remote and home-based care models.
Enterprises rarely rely on a single prescription management platform type. Most operate several in parallel. The organizations that scale safely are those that understand these categories clearly and ensure they are coordinated rather than fragmented.
Use Cases of Prescription Management Platforms
Prescription management platforms solve recurring enterprise problems by standardizing prescribing, reducing errors, automating approvals, and improving medication adherence at scale.
These systems address operational risk, regulatory exposure, and preventable care delays. Each use case below reflects where enterprises see a measurable impact first.
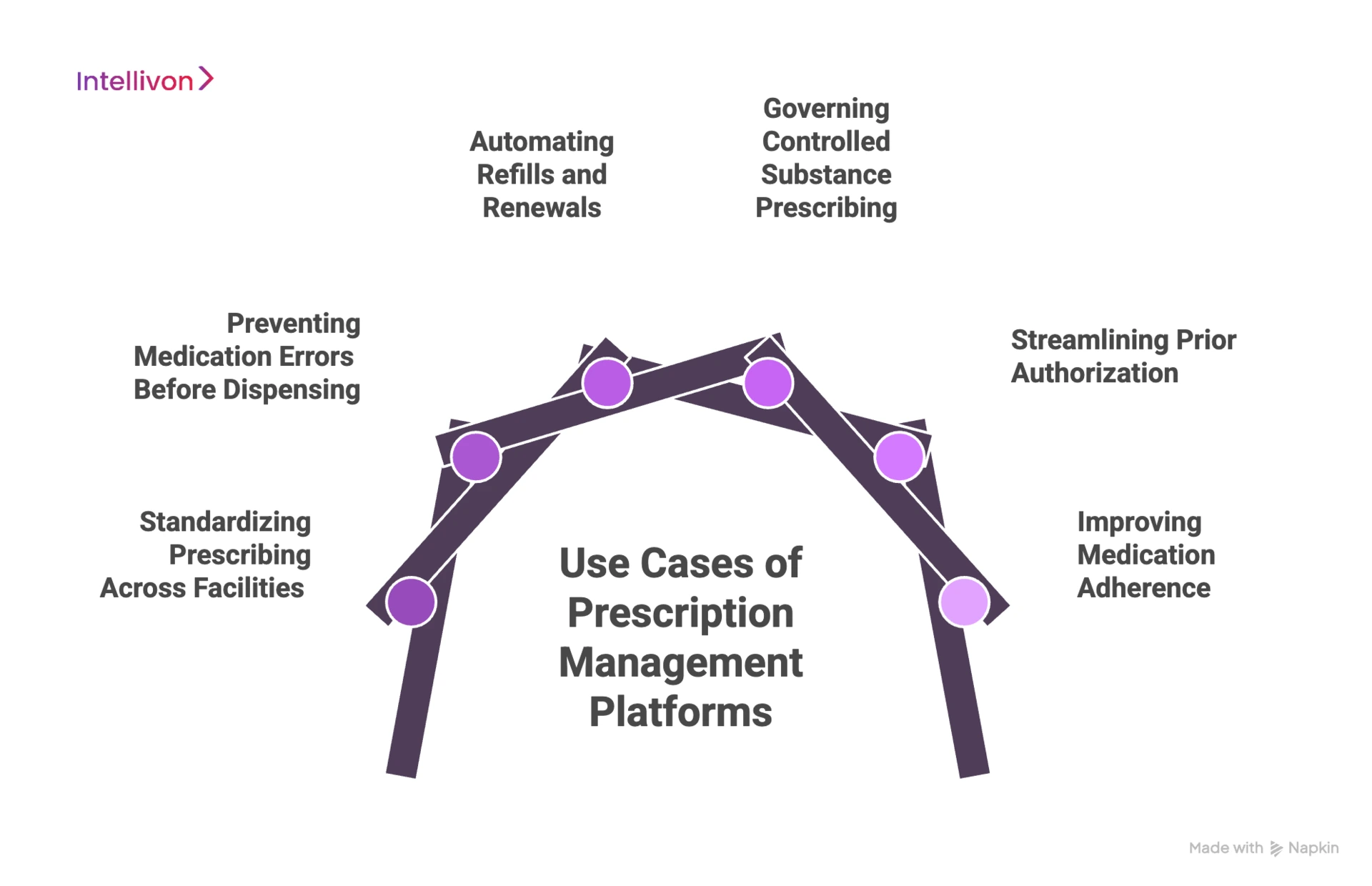
1. Standardizing Prescribing Across Facilities
In large systems, prescribing practices often vary by location or department. This creates inconsistency, risk, and audit challenges. Prescription management platforms enforce standardized order sets and dosage defaults. Clinical rules apply uniformly across the organization.
As a result, prescribing quality becomes predictable and easier to govern.
2. Preventing Medication Errors Before Dispensing
Most medication errors occur during order creation. Missing fields, unclear instructions, and interaction oversights are common causes. Prescription platforms validate prescriptions in real time. They flag unsafe doses, allergies, and duplicate therapies instantly.
Therefore, fewer unsafe orders reach the pharmacy.
3. Automating Refills and Renewals
Refill requests consume clinical and pharmacy time. Manual handling slows care and frustrates patients. These platforms automate refill approvals using predefined rules. Renewal schedules are tracked automatically.
As a result, refill turnaround improves without adding staff.
4. Governing Controlled Substance Prescribing
Controlled medications require strict oversight. Weak governance exposes enterprises to regulatory penalties. Prescription platforms enforce identity verification and access controls. Every prescription action is logged and traceable.
This ensures audit readiness across all facilities.
5. Streamlining Prior Authorization
Insurance mismatches delay prescriptions and increase abandonment rates. Clinicians often adjust therapy late in the process. These systems integrate coverage and authorization checks at prescribing time. Alternatives surface when coverage fails.
Therefore, prescriptions move faster and with fewer disruptions.
6. Improving Medication Adherence
Long-term outcomes depend on consistent medication use. Missed refills often go unnoticed until complications arise. Prescription platforms track refill behavior across populations. Care teams intervene earlier.
This supports value-based care and outcome accountability.
Prescription management platforms deliver value by solving everyday enterprise problems at scale. When implemented correctly, they reduce risk, streamline operations, and support safe growth across complex healthcare environments.
PMP Systems Reduce 99% Risk in Medication Errors
Well-designed prescription management platforms can reduce medication errors by up to 99% and adverse drug events by up to 98% by standardizing, validating, and governing prescriptions end-to-end.
At scale, even small error rates translate into major exposure. Large hospitals process millions of prescriptions annually across inpatient, outpatient, and pharmacy networks. A high-performing prescription management platform removes error-prone manual steps before they cascade into clinical or financial consequences.
1. Eliminates Errors at the Source
Most prescription errors do not originate from complex clinical judgment. They stem from missing fields, unclear instructions, duplicate therapies, or overlooked interactions. Prescription management platforms address these issues at the point of order entry.
Core safeguards include standardized order templates, mandatory data fields, and real-time validation. Drug–drug interactions, allergy conflicts, and dose range issues are flagged instantly. As a result, errors are intercepted before a prescription ever reaches the pharmacy.
For clinicians, this means fewer clarifications and fewer callbacks. For the enterprise, it means fewer near-miss reports and far less downstream correction work.
2. Why Error Reduction Matters Beyond Patient Safety
Medication errors carry a hidden operational cost. Each preventable adverse drug event often leads to longer hospital stays, unplanned readmissions, and avoidable investigations. Over time, these events inflate operating costs and strain already limited bed capacity.
When prescription management platforms eliminate entire categories of errors, they directly reduce this financial drag. The impact compounds across departments, locations, and care settings. What starts as a safety improvement becomes a margin protection mechanism.
In addition, stronger prescribing controls reduce malpractice exposure and improve audit defensibility. A clear, traceable medication trail strengthens trust with payers, regulators, and partners.
3. Using Prescription Data to Prevent Systemic Risk
Modern prescription platforms do more than validate individual orders. They aggregate prescribing data across the organization to surface patterns that humans cannot easily detect.
This visibility helps identify high-risk drug combinations, inconsistent prescribing behaviors, and departments that may need targeted intervention. Order sets and alerts can then be refined based on real usage data, not assumptions.
Over time, the organization moves from reacting to isolated incidents to proactively shaping a safer prescribing behavior system-wide.
The near-99% reduction in medication errors reflects what happens when prescribing workflows are engineered with structure, automation, and governance.
Core Features of an Enterprise Prescription Management Platform
Enterprise prescription management platforms operate as governed systems that standardize prescribing, reduce risk, and scale medication workflows across complex healthcare organizations.
The features below reflect what global healthcare organizations require in practice.
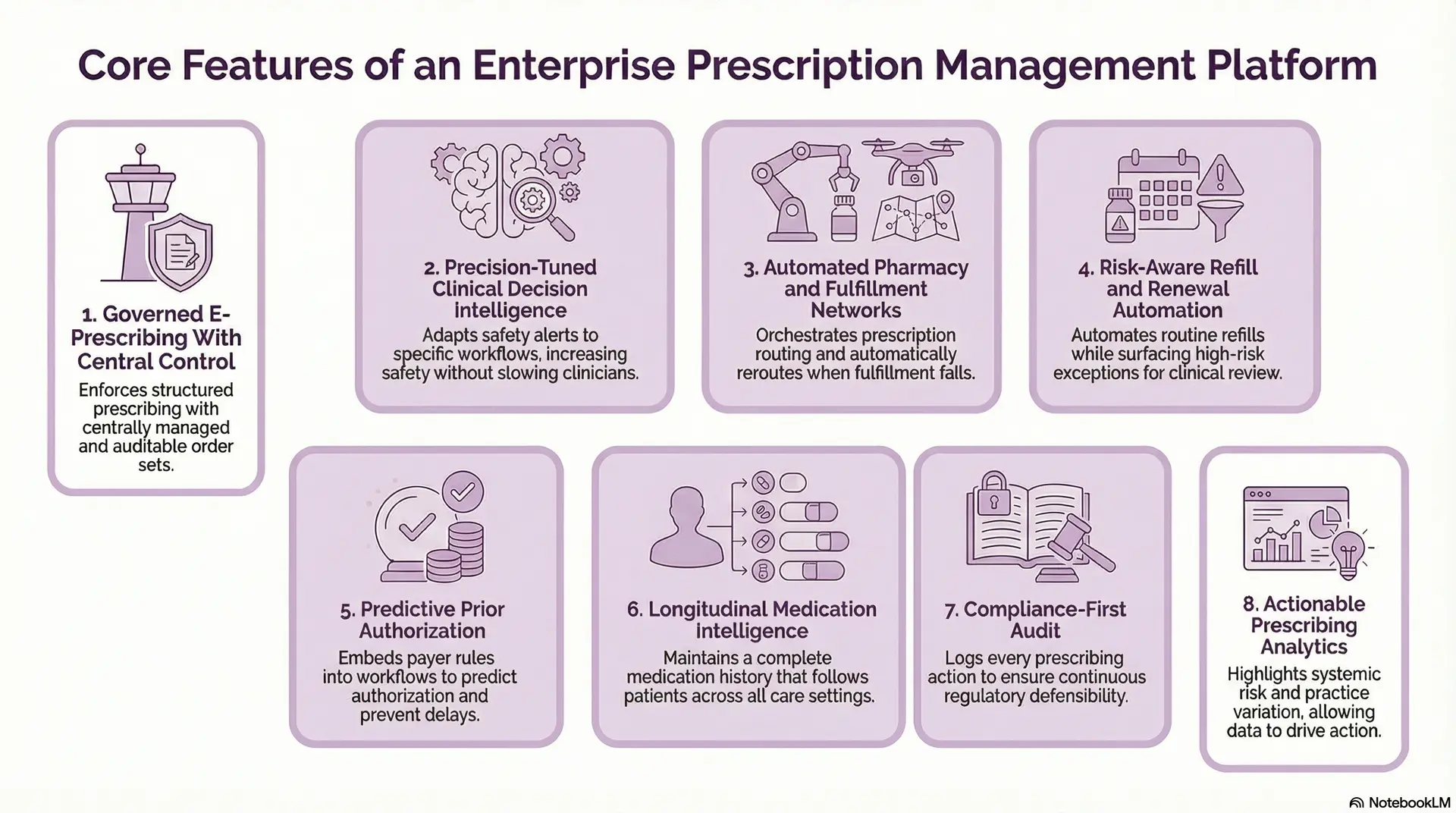
1. Governed E-Prescribing With Central Control
Enterprise platforms enforce structured prescribing through centrally managed order sets. Clinical rules apply consistently across departments, facilities, and regions.
Changes to templates and defaults are versioned and auditable. Exceptions are tracked, not hidden. This turns prescribing into a controllable enterprise process.
2. Precision-Tuned Clinical Decision Intelligence
Clinical decision support must adapt to real-world workflows. Enterprise systems allow alerts to be configured by specialty, risk level, and care setting.
Override behavior is measured and reviewed over time. Alerts improve through feedback rather than becoming ignored noise. As a result, safety increases without slowing clinicians.
3. Automated Pharmacy and Fulfillment Networks
Enterprise environments span retail, specialty, mail-order, and in-house pharmacies. Prescription platforms must orchestrate routing, and not just integrate endpoints.
The system automatically reroutes when fulfillment fails. Status updates propagate without manual intervention. This maintains continuity of care across fragmented pharmacy networks.
4. Risk-Aware Refill and Renewal Automation
Automation at enterprise scale must respect clinical risk. Platforms apply different rules based on drug class, therapy duration, and patient context. Routine refills proceed automatically, and exceptions surface early.
Therefore, access improves without exposing the organization to liability.
5. Predictive Prior Authorization
Coverage validation must occur before prescriptions are finalized. Enterprise platforms embed payer rules directly into prescribing workflows.
Authorization likelihood is predicted using historical patterns. Acceptable alternatives are presented when friction appears. This prevents downstream delays and abandoned prescriptions.
6. Longitudinal Medication Intelligence
Enterprise platforms maintain medication history across inpatient, outpatient, and external sources. Prescriptions follow patients as they move across care settings.
Refill gaps and duplication risks surface early. Interventions become proactive instead of reactive. This supports chronic care and population health strategies.
7. Compliance-First Audit
Every prescribing action is logged with identity, time, and context. Role-based access and identity verification enforce least-privilege control. Compliance monitoring operates continuously, not only during audits.
This ensures regulatory defensibility at scale.
8. Actionable Prescribing Analytics
Enterprise analytics focuses on decisions, and not dashboards. The platform highlights systemic risk, cost leakage, and practice variation. At the same time, Insights feed governance and clinical policy refinement, and data drives action.
As a result, prescription management supports enterprise strategy rather than isolated reporting.
An enterprise prescription management platform functions as a regulated infrastructure. When designed correctly, it reduces risk, stabilizes operations, and enables healthcare organizations to scale without sacrificing safety, compliance, or control.
Regulatory and Compliance Requirements For Prescription Management Platforms
Enterprise prescription management platforms must embed regulatory controls into daily prescribing and fulfillment workflows to ensure safety, traceability, and audit readiness.
Compliance gaps cascade across facilities, pharmacists, clinicians, and payers in hospitals. This makes regulatory alignment a design requirement, not a legal afterthought.
1. HIPAA and HITECH: Safeguarding Prescription Data
Prescription data contains protected health information at every step. HIPAA and HITECH require organizations to enforce strict controls on how this data is accessed, stored, and shared.
Enterprise prescription platforms encrypt data both in transit and at rest. Role-based access ensures only authorized users can issue, modify, or view prescriptions. Detailed audit logs track every action.
For large enterprises, this creates consistent privacy protection across teams and locations without slowing clinicians down.
2. DEA and Controlled Substance Regulations
Controlled substances demand heightened oversight. Manual prescribing and partial digital workflows create compliance gaps and audit exposure.
Enterprise platforms support electronic prescribing of controlled substances with identity proofing and multi-factor authentication. Digital signatures are mandatory, and not optional. At the same time, prescription activity is fully traceable.
This allows organizations to meet DEA requirements while maintaining lawful clinical flexibility.
3. FDA and Clinical Safety Expectations
Prescription management platforms increasingly embed clinical intelligence when systems influence clinical decisions, transparency, and validation matter.
Enterprise platforms version clinical rules, safety checks, and decision logic. Changes are recorded and reviewable over time.
This supports trust in automated safeguards and protects organizations when safety processes are questioned.
4. State, Regional, and Cross-Border Requirements
E-prescribing laws vary by geography and drug class. What is permitted in one state may be mandated in another.
These platforms apply region-specific rules automatically based on location. For international operations, GDPR and data residency requirements are enforced by design. As organizations expand, compliance scales with them instead of requiring system redesign.
Regulatory compliance defines how prescription management platforms must operate under real-world pressure. Enterprises that embed compliance into daily workflows reduce risk, protect operational continuity, and remain adaptable as regulations evolve.
How AI Works in Modern Prescription Management Platforms
In enterprise prescription management, AI helps predict risk, guide prescribing decisions, automate routine workflows, and turn prescription data into system-level intelligence.
Its value comes from how quietly and consistently it improves outcomes at scale.
1. Anticipate Medication Risks
Traditional safety checks rely on static rules. AI-based systems go further by learning from past outcomes, patient complexity, and prescribing behavior across the network.
This allows the platform to identify patients who are more likely to experience adverse drug events, therapy complications, or medication-related readmissions. The signal appears early, often before a prescription is dispensed.
For large enterprises, this capability changes how safety is managed. Risk is predicted, not discovered after an incident.
2. Reducing Insurance Friction
Prior authorization remains one of the most disruptive points in prescription workflows. The delay is mostly due to administrative issues and not clinical.
AI helps by analyzing historical payer decisions, denial patterns, and coverage nuances. At the moment of prescribing, the system can estimate approval likelihood and surface alternatives when risk is high.
This shifts friction upstream. Clinicians make informed choices sooner, and patients face fewer delays at the pharmacy.
3. Context-Aware Clinical Decision Support
AI-driven prescription platforms study how clinicians interact with alerts over time. They track what is overridden, accepted, or ignored, and correlate those actions with outcomes.
Over time, decision support becomes context-aware. High-risk situations interrupt workflows. Low-value noise fades away. This makes safety mechanisms effective without becoming obstructive.
4. Automating Without Removing Accountability
Not every prescription decision requires human review. At enterprise scale, that expectation is neither realistic nor safe.
AI identifies which refill requests, renewals, and approvals are stable and low-risk. These actions move forward automatically under governed rules. Anything outside defined thresholds is escalated.
This balances efficiency with accountability. Workload decreases while clinical responsibility remains intact.
5. Prescription Data Transformation
When prescription data spans hundreds of providers and locations, patterns emerge that individuals cannot detect.
AI aggregates this volume of data to identify outlier prescribing behavior, unusual cost drivers, and emerging medication risks. Leadership can see where intervention is needed long before problems escalate.
This capability moves prescription management from operational monitoring to strategic oversight.
6. Regulated AI Governance
Enterprise AI must be transparent, measurable, and controllable. Black-box behavior creates regulatory and legal risk. Modern prescription management platforms log AI-driven decisions, track performance over time, and monitor for drift or bias. Updates are reviewed, not pushed blindly.
This governance framework allows organizations to adopt AI confidently without compromising trust or compliance.
AI strengthens prescription management when it is embedded into real workflows and governed like any other enterprise system.
Tech Stack Used To Build Prescription Management Platforms
Enterprise prescription management platforms rely on secure, interoperable, and scalable technologies that support regulated workflows, high availability, and AI-driven intelligence.
Below is how leading enterprises structure their technology foundation.
1. Backend Application and API Layer
- Java / Kotlin / .NET Core: Power core prescribing engines, validation logic, and high-availability enterprise services.
- Python: Supports AI models, analytics pipelines, and orchestration logic alongside core systems.
- FastAPI / Spring Boot: Expose secure, performant APIs for EHRs, pharmacies, and payer integrations.
2. Healthcare Interoperability and Data Exchange
- FHIR (MedicationRequest, MedicationDispense): Standardizes prescription data exchange across EHRs and care systems.
- HL7 v2: Enables integration with legacy hospital and pharmacy systems.
- X12: Supports insurance eligibility and prior authorization workflows.
3. Data Storage and Persistence
- PostgreSQL: Stores structured prescription, audit, and transaction data reliably.
- MongoDB: Manages semi-structured clinical and workflow metadata.
- Redis: Handles real-time session state, caching, and workflow orchestration.
4. AI, Analytics, and Intelligence Layer
- TensorFlow / PyTorch: Train models for risk prediction, adherence analysis, and authorization intelligence.
- Apache Spark: Processes large-scale prescription and population data for analytics.
- MLflow: Manages model versioning, performance tracking, and auditability.
5. Security, Identity, and Compliance
- OAuth 2.0 / OpenID Connect: Enforces secure authentication and authorization across users and systems.
- HashiCorp Vault: Manages encryption keys, secrets, and controlled access credentials.
- AES-256 / TLS 1.2+: Protects prescription data at rest and in transit.
6. Workflow Automation and Messaging
- Apache Kafka: Enables real-time prescription events and pharmacy status updates.
- RabbitMQ: Coordinates asynchronous workflows such as refills and approvals.
- Temporal / Camunda: Manages long-running, regulated medication workflows.
7. Infrastructure and Scalability
- Kubernetes: Orchestrates microservices for scalability and resilience.
- Docker: Standardizes deployment across environments.
- AWS / Azure / GCP: Provides compliant cloud infrastructure with regional controls.
8. Observability and Operational Monitoring
- Prometheus: Tracks system and workflow health metrics.
- Grafana: Visualizes performance, risk indicators, and operational trends.
- ELK Stack: Centralizes logs for audit, security, and incident investigation.
The technology stack behind an enterprise prescription management platform directly shapes its reliability, compliance posture, and ability to scale. When built on secure, interoperable, and AI-ready foundations, these platforms evolve from operational tools into long-term digital infrastructure for healthcare organizations.
How We Build Prescription Management Platforms
At Intellivon, we treat prescription management as critical healthcare infrastructure. These platforms influence patient safety, regulatory exposure, clinical productivity, and financial performance. As a result, our development process is designed to work in real enterprise environments, and not idealized software scenarios.
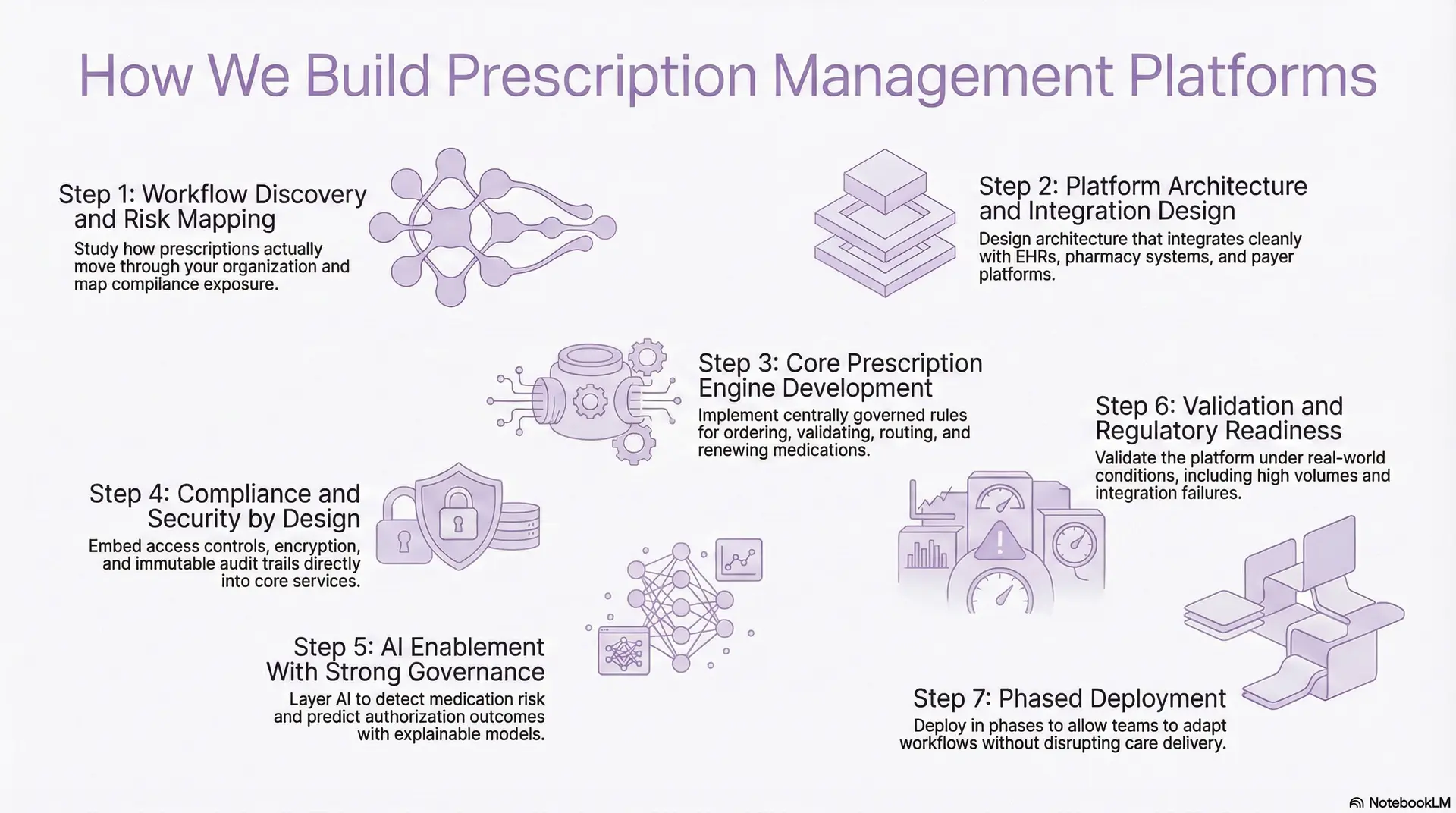
Step 1: Workflow Discovery and Risk Mapping
We begin by studying how prescriptions actually move through your organization. This includes outpatient clinics, inpatient units, specialty programs, pharmacies, and payer touchpoints.
We examine how clinicians prescribe today, where approvals slow down, and how refills are managed across sites. Equally important, we identify informal workarounds that exist because current systems do not scale. From a risk perspective, we map where compliance exposure accumulates. This often includes controlled substances, cross-location workflows, and manual overrides.
This phase ensures the platform solves real operational risk rather than theoretical problems.
Step 2: Platform Architecture and Integration Design
Enterprise healthcare environments are heterogeneous. No prescription platform exists in isolation.
We design architecture that integrates cleanly with EHRs, pharmacy systems, payer platforms, and analytics stacks. Interoperability standards are selected intentionally to support both current vendors and future changes.
We also design for organizational evolution. Acquisitions, new service lines, and regional expansion are factored into the integration strategy from day one. This prevents architectural rewrites as the enterprise grows.
Step 3: Core Prescription Engine Development
The prescription engine governs how medications are ordered, validated, routed, and renewed. At enterprise scale, this logic must be consistent, enforceable, and observable.
We implement centrally governed rules for prescription creation, validation checks, pharmacy routing, and refill scheduling. Every exception is visible and reviewable. Importantly, we separate clinical decision logic from workflow automation.
This allows updates without destabilizing core operations. The result is a prescription engine that scales without losing control.
Step 4: Compliance and Security by Design
We embed identity management, role-based access controls, encryption, and audit logging directly into the platform’s core services. Prescription activity is always attributable to a verified user.
Controlled substance workflows receive additional safeguards, including strong authentication and immutable audit trails. This supports DEA, HIPAA, and regional requirements simultaneously. As a result, compliance remains continuous rather than reactive.
Step 5: AI Enablement With Strong Governance
Once core workflows are stable, we layer AI to detect medication risk, predict authorization outcomes, and identify prescribing patterns that warrant review. Each model is aligned to a specific business or safety objective.
AI decisions are explainable and monitored. Model drift, bias, and performance degradation are tracked. This ensures intelligence improves outcomes without introducing regulatory or clinical risk.
Step 6: Validation and Regulatory Readiness
Before going live, we validate the platform under real-world conditions. Test scenarios include high prescription volumes, exception handling, pharmacy rejections, and integration failures.
Clinical validation ensures decision support behaves correctly across specialties. Security testing verifies data protection and access boundaries. We also confirm regulatory readiness before deployment. This reduces surprises during audits or inspections.
Step 7: Phased Deployment
Enterprise adoption requires control, and not speed alone. We deploy in phases, often starting with a subset of facilities or medication classes. This allows teams to adapt workflows without disrupting care delivery.
Training is role-specific and continuous. Adoption metrics are monitored closely after launch. This approach accelerates value while protecting operations.
Intellivon builds prescription management platforms as durable enterprise systems. By aligning workflow reality, regulatory rigor, and intelligent automation, we help healthcare organizations reduce risk, improve efficiency, and scale medication operations with confidence.
Cost To Build A Prescription Management Platform
For healthcare enterprises, hospital groups, and digital health companies, the cost of building a prescription management platform depends less on ambition and more on scope discipline and phased execution. Organizations that start with a focused medication workflow, such as e-prescribing, refills, or controlled substances, can launch an enterprise-grade platform within a controlled budget.
At Intellivon, we structure prescription management to build around phase-wise cost models. Each phase aligns with leadership budget cycles, regulatory readiness, and near-term operational ROI. This approach avoids large upfront capital burn while keeping the platform scalable from day one.
Estimated Phase-Wise Cost Breakdown (Prescription Management Platform)
| Phase | Description | Estimated Cost (USD) |
| Discovery & Regulatory Blueprint | Prescribing workflow mapping, risk assessment, HIPAA/DEA/EPCS readiness, scope definition | 8,000 – 15,000 |
| Interoperability & Integration Design | EHR, pharmacy, formulary, and payer integration design | 12,000 – 25,000 |
| Core Prescription Engine Development | E-prescribing logic, validation rules, routing, and refill workflows | 25,000 – 45,000 |
| Clinical Decision Support & AI Setup | Interaction checks, risk signals, and authorization intelligence | 18,000 – 35,000 |
| Security, IAM & Compliance Controls | Role-based access, encryption, audit logs, EPCS workflows | 10,000 – 18,000 |
| Analytics & Governance Dashboards | Prescribing trends, risk indicators, operational metrics | 8,000 – 15,000 |
| Testing, QA & Regulatory Validation | Clinical accuracy testing, security audits, and performance validation | 8,000 – 14,000 |
| Pilot Deployment & Training | Live rollout, clinician training, workflow optimization | 10,000 – 18,000 |
Total Initial Investment Range:
USD 110,000 – 185,000
This investment supports a secure, compliant, enterprise-ready prescription management pilot for one high-impact use case within a live clinical or pharmacy environment.
Annual Maintenance and Optimization Costs
Ongoing costs cover infrastructure, integrations, compliance maintenance, analytics refinement, and AI model tuning.
- 12–20% of the initial build cost annually
- Approx. USD 14,000 – 35,000 per year
When platforms are engineered with modular architecture and governed AI pipelines, these costs remain predictable over time.
Hidden Costs Healthcare Organizations Should Plan For
Even well-planned prescription management initiatives include recurring cost variables that are often underestimated:
- Expansion into additional clinical departments or specialties
- New pharmacy or payer integrations during growth
- Regulatory documentation updates as prescribing laws evolve
- Increased cloud usage driven by prescription volume growth
- Ongoing AI model recalibration to maintain safety and accuracy
- Clinician training as workflows mature or policies change
Planning for these early protects multi-year budgets and audit readiness.
Best Practices to Stay Within the USD 100K–200K Budget
Healthcare organizations that control prescription management costs successfully tend to:
- Start with one high-risk or high-volume prescribing workflow
- Avoid multi-region and multi-formulary complexity in phase one
- Use modular architectures that allow features to be added later
- Embed compliance and security controls from day one
- Track operational ROI and risk reduction metrics early
This ensures the platform proves both clinical and financial value before broader capital investment.
If you are planning a prescription management platform, we can provide a tailored cost estimate and phased rollout plan aligned with your enterprise strategy and compliance requirements.
Overcoming Common Challenges In Building Prescription Management Platforms
Enterprise prescription management platforms fail when real-world clinical complexity, regulatory variability, and organizational scale are underestimated during design and rollout.
The most successful enterprises are those that address these challenges head-on, rather than simplifying them away.
1. Fragmented Prescribing Workflows
In large health systems, prescribing does not follow a single workflow. Inpatient environments, specialty clinics, outpatient practices, and partner networks often operate very differently.
When prescription platforms assume uniform workflows, friction appears immediately. Clinicians bypass systems, create workarounds, or revert to manual steps. Over time, this fractures adoption and data consistency.
At Intellivon, we design platforms to support multiple prescribing patterns within a governed framework. Workflows adapt by role, specialty, and care setting, while compliance and safety rules remain centralized. This balance preserves flexibility without losing control.
2. Alert Fatigue and Declining Clinical Trust
Many enterprises deploy prescription systems with strong decision support, only to see clinicians override alerts within weeks. Generic alerts do not reflect patient context, specialty nuance, or organizational priorities. As a result, clinicians stop engaging, and risk increases silently.
Intellivon solves this by building precision-tuned decision support. Alert behavior is continuously analyzed, refined, and governed. The platform learns which signals prevent harm and which create noise. Over time, trust is restored because interruptions feel justified.
3. Regulatory Drift With Regulation Changes
Prescription regulations do not stand still. This is because DEA rules change, state mandates expand, and data privacy frameworks evolve. Because of this, many platforms struggle to keep up without costly rework.
Enterprises often discover compliance gaps only during audits, mergers, or geographic expansion. At that point, remediation is expensive and disruptive.
Our experts build compliance as a configurable policy, not hard-coded logic. Here, regulatory rules are modular, versioned, and region-aware. This allows organizations to adapt quickly as mandates change, without destabilizing core workflows.
4. Scaling Prescription Operations Post Merger
Growth through acquisition introduces immediate prescription complexity. Newly acquired entities bring different EHRs, pharmacies, workflows, and prescribing norms.
Without a unifying platform, organizations operate parallel prescription systems indefinitely. This creates visibility gaps and uneven risk profiles.
Intellivon designs prescription management platforms as unifying layers. They normalize data, coordinate workflows, and provide enterprise-level oversight without forcing immediate system replacement. This allows faster operational alignment after M&A activity.
5. Inability to Translate Prescription Data
Many enterprises collect vast prescription data but struggle to use it. Reports exist, but they rarely change behavior. Leaders see metrics without knowing what to fix. This creates a false sense of control while risk accumulates beneath the surface.
We embed analytics directly into governance and workflow refinement. Prescribing data feeds decision support updates, policy adjustments, and targeted interventions. Insight leads to action, not just dashboards.
Enterprise prescription management challenges are rarely obvious at launch. They emerge under scale, complexity, and change. Intellivon builds platforms that acknowledge this reality, addressing deep operational and regulatory friction so healthcare organizations can scale medication delivery safely, confidently, and sustainably.
Conclusion
Prescription management has become core healthcare infrastructure, not a back-office function. At enterprise scale, fragmented prescribing systems increase risk, slow operations, and limit growth. A unified, intelligent prescription management platform brings consistency, compliance, and control across complex care environments.
At Intellivon, we build prescription management platforms designed for real-world scale. By combining interoperability, compliance-first design, and governed AI, we help healthcare organizations reduce risk, improve efficiency, and grow with confidence.
Build a Prescription Management Platform With Intellivon
At Intellivon, we build enterprise-grade prescription management platforms that unify prescribing, pharmacy operations, payer workflows, and compliance governance into one controlled medication ecosystem. Our platforms connect clinicians, pharmacies, insurers, and patients without disrupting live clinical operations or existing EHR environments.
Each solution is engineered for large healthcare enterprises: compliant by design, resilient under high prescription volumes, interoperable across vendors, and built to deliver measurable clinical, operational, and financial ROI from day one.
Why Partner With Intellivon?
- Compliance-First Platform Architecture: Every deployment aligns with HIPAA, HITECH, DEA EPCS, GDPR, where applicable, and evolving prescribing mandates, with audit-ready governance embedded at every layer.
- Interoperability-Driven Engineering: Native support for FHIR, HL7, X12, and secure enterprise APIs enables seamless integration with EHRs, pharmacy systems, PBMs, and payer platforms.
- Multi-EHR and Pharmacy Network Expertise: We integrate across Epic, Cerner, Allscripts, regional HIS platforms, retail, and specialty pharmacies without forcing system replacement.
- Enterprise-Scale Prescription Orchestration: High-availability architectures support multi-hospital networks, mail-order pharmacies, and specialty workflows under peak prescription demand.
- AI-Powered Safety and Workflow Intelligence: Built-in intelligence detects medication risk, predicts authorization outcomes, reduces exception handling, and improves prescribing quality at scale.
- Zero-Trust Security and Identity Controls: End-to-end encryption, strong identity verification, and least-privilege access protect prescription data without slowing clinical workflows.
Book a strategy call with Intellivon to explore how a custom-built prescription management platform can reduce medication risk, streamline workflows, and scale safely across your healthcare enterprise.
FAQs
Q1. What is a prescription management platform in healthcare?
A1. A prescription management platform is an enterprise system that digitizes and governs the full medication lifecycle. It manages prescribing, validation, pharmacy routing, refills, prior authorizations, and audits within a single controlled workflow.
Q2. How long does it take to build a prescription management system?
A2. For enterprises, an initial production-ready prescription management platform typically takes 4 to 6 months to deploy. This usually includes workflow discovery, regulatory alignment, core prescribing functionality, and pilot rollout.
Q3. What regulations apply to digital prescription platforms?
A3. Digital prescription platforms must comply with HIPAA and HITECH for patient data protection, DEA EPCS requirements for controlled substances, and state-level e-prescribing mandates. Platforms offering clinical decision support must meet FDA safety expectations around traceability and validation.
Q4. Can prescription platforms integrate with EHR and pharmacy systems?
A4. Yes. Enterprise prescription management platforms are designed to integrate with EHRs, pharmacy systems, PBMs, and payer platforms using standards such as FHIR, HL7, and X12. This allows prescriptions to move seamlessly across clinical, pharmacy, and insurance workflows.
Q5. What is the ROI of prescription management software for hospitals?
A5. Hospitals see ROI through reduced medication errors, faster refill and authorization cycles, lower administrative workload, and improved compliance. Many organizations also reduce avoidable adverse drug events, readmissions, and audit exposure.