Continuous patient monitoring is becoming essential for healthcare organizations that need to improve outcomes while managing limited resources. IoT health monitoring platforms help clinicians spot early signs of deterioration, decrease avoidable readmissions, and provide care outside of physical facilities. When implemented correctly, these platforms turn monitoring from a one-time task into a continuous, data-driven process that helps clinicians make proactive decisions.
However, delivering this value on a large scale is challenging. Platforms must manage high volumes of data, maintain uptime during critical moments, and provide reliable alerts for clinicians. Systems that create unnecessary noise, lose data integrity, or do not fit into existing workflows create more risks instead of less.
At Intellivon, we have spent over a decade developing enterprise-grade healthcare platforms that combine interoperability, workflow improvement, and AI-driven intelligence. Drawing on this experience, in this blog, we will discuss how we create such IoT health monitoring platforms from the ground up.
Key Takeaways of the IoT in Healthcare Market
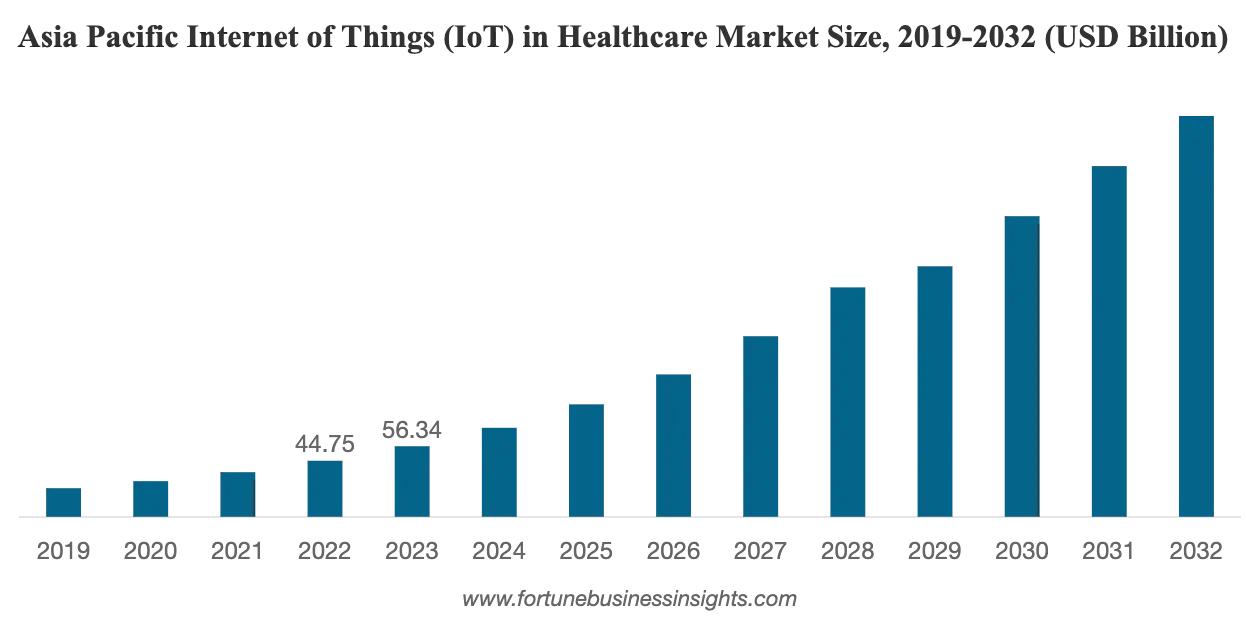
The IoT health market is expanding at a pace few healthcare technologies can match. Valued at USD 139.74 billion in 2023, it is projected to reach USD 822.54 billion by 2032, growing at a 21.3% CAGR.
In parallel, the remote patient monitoring market is moving from niche pilot programs to mainstream care delivery, projected to grow from USD 27–28 billion in 2024 to nearly USD 57 billion by 2030.
Growth Drivers:
- Rising chronic disease prevalence is forcing care beyond hospital walls.
- RPM reimbursement models and telehealth normalization make platforms financially viable
- Wearable and IoT device costs are falling, while adoption is accelerating.
- 5G, edge computing, and cloud-native platforms enable real-time, low-latency data flows.
- AI-driven analytics are moving monitoring from raw data to actionable insight.
- Integrated virtual care ecosystems are replacing point solutions.
- Asia-Pacific is emerging as the fastest-growing region for IoT health platforms.
Looking ahead, enterprise opportunity is consolidating around scalable platforms, not standalone devices. Health systems, payers, and employers are investing in device-agnostic IoT health monitoring platforms that aggregate data from wearables, medical-grade sensors, and home devices into interoperable, AI-ready data layers.
These platforms sit at the center of RPM programs, virtual wards, and population health strategies, positioning IoT health monitoring as a long-term growth lever rather than a short-term cost initiative.
What Is an IoT Health Monitoring Platform?
An IoT health monitoring platform is an enterprise system that continuously collects, processes, and analyzes patient health data from connected devices. These devices may include medical-grade sensors, wearables, home monitoring equipment, and bedside systems. The platform transforms raw signals into clinically meaningful insight that care teams can act on in real time.
Unlike consumer wellness apps, enterprise IoT health platforms are built for reliability, security, and clinical accountability. They operate under strict regulatory frameworks, maintain uptime during critical events, and integrate directly with EHRs and care coordination systems. Data does not sit in isolation. It flows into existing workflows where clinicians already make decisions.
At its core, the platform supports continuous monitoring, intelligent alerts, and structured clinical escalation. It enables earlier intervention, reduces unnecessary hospital visits, and supports long-term chronic care. For healthcare enterprises, it becomes foundational infrastructure that connects remote care, population health, and operational efficiency into one governed system.
How It Works
An IoT health monitoring platform operates as a continuous, closed-loop system. Each step is designed to move patient data smoothly from collection to clinical action. The goal is to surface the right signal, at the right time, to the right team, without disrupting care delivery.
Step 1: Connected Devices Capture Patient Signals
Medical-grade wearables, home monitoring devices, and bedside sensors continuously record vitals, activity, and condition-specific markers.
These measurements may stream in real time or at defined intervals based on clinical protocols. The platform treats each data point as part of a broader health trend, not an isolated reading.
Step 2: Data Is Secured and Ingested
Captured data travels through encrypted gateways or patient mobile apps into the core platform.
Device identity is verified, timestamps are validated, and readings are normalized into a standardized clinical format. This step ensures data consistency before it reaches analytics or clinical systems.
Step 3: Analytics Detect Risk and Prioritize Action
Time-series analytics and AI models continuously analyze incoming data for deterioration patterns.
Instead of firing raw alerts, the platform applies thresholds, context, and patient history. This reduces alert fatigue and focuses attention on clinically meaningful changes.
Step 4: Alerts Flow Into Clinical Workflows
When risk thresholds are met, alerts route into existing dashboards, EHRs, or care management tools. Each notification aligns with predefined escalation paths and clinical roles. Care teams receive actionable insight rather than ambiguous data signals.
This workflow transforms continuous monitoring into operational decision intelligence. At enterprise scale, it enables proactive care delivery while preserving clinical focus and system reliability.
Key Enterprise Use Cases of IoT Health Monitoring Platforms
Enterprise IoT health monitoring platforms deliver the most value when embedded into high-risk, high-volume workflows where early intervention directly affects outcomes and costs.
These use cases are operationally proven and tied directly to reimbursement, capacity, and clinical risk control.
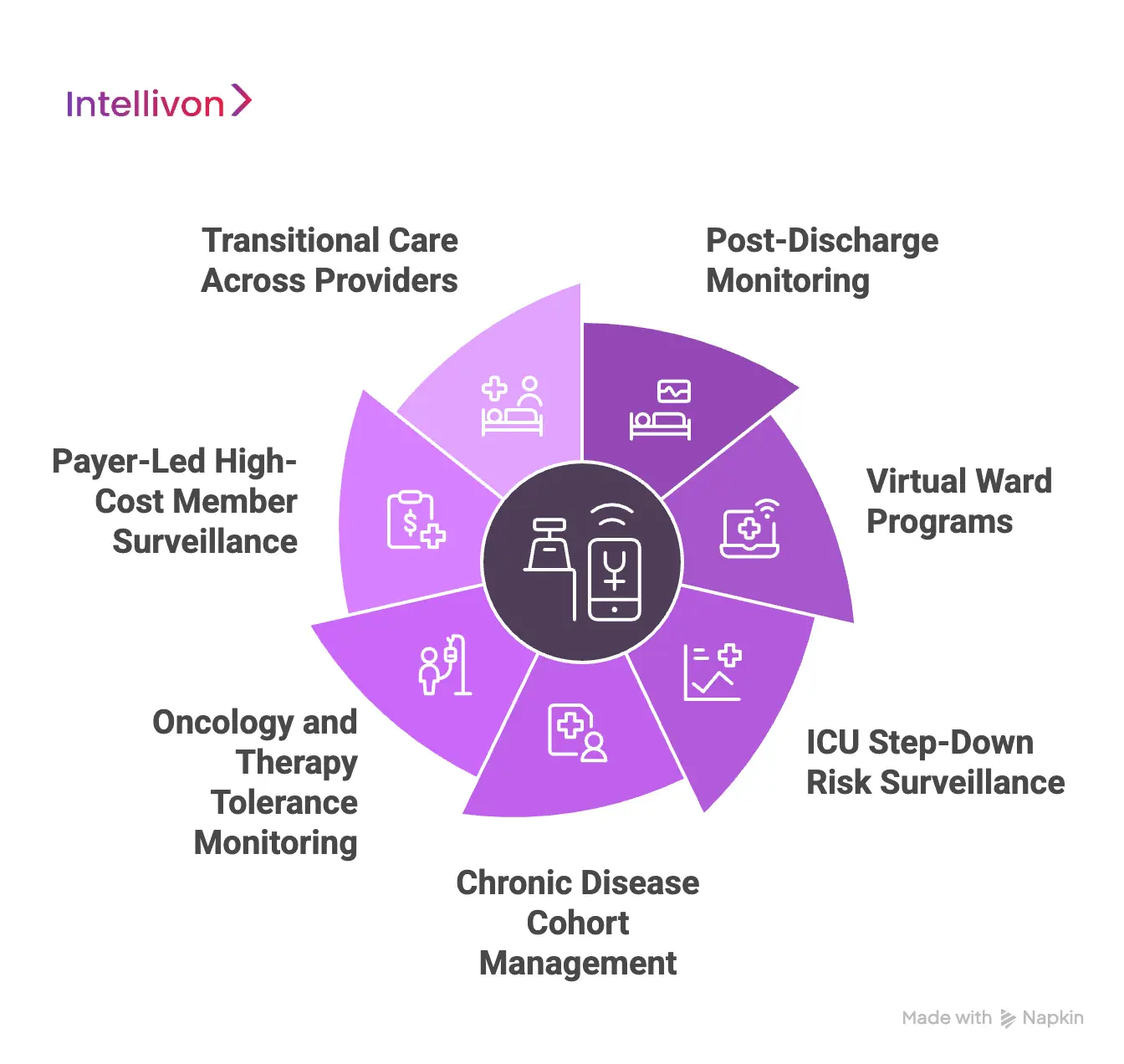
1. Post-Discharge Monitoring
Hospitals actively monitor heart failure, COPD, and post-surgical patients during the critical post-discharge window. IoT devices surface subtle changes in vitals days before symptoms become acute.
This allows care teams to intervene earlier and reduce avoidable readmissions.
2. Virtual Ward Programs
Virtual wards allow enterprises to deliver hospital-level oversight without physical beds. IoT platforms stream continuous vitals from patients recovering at home.
This model frees inpatient capacity while preserving clinical safety and visibility.
3. ICU Step-Down Risk Surveillance
Patients transitioning out of intensive care remain vulnerable to rapid decline. Continuous monitoring in step-down units closes the gap between ICU and general wards.
Enterprises use this to shorten ICU stays without increasing adverse events.
4. Chronic Disease Cohort Management
Large health systems manage thousands of chronic patients simultaneously. IoT platforms stratify patients by real-time risk rather than static diagnoses.
Care teams focus attention on patients trending toward deterioration instead of applying broad outreach.
5. Oncology and Therapy Tolerance Monitoring
Cancer therapies place sustained physiological stress on patients. Continuous monitoring helps detect adverse reactions, dehydration, and infection risk earlier. Clinicians adjust therapy plans based on trends, not delayed symptom reporting.
6. Payer-Led High-Cost Member Surveillance
Payers deploy IoT monitoring to identify members likely to generate emergency spend. Early outreach reduces hospital visits and escalations.
These programs are tightly aligned with value-based reimbursement models.
7. Transitional Care Across Providers
Care transitions introduce data gaps and handoff risk. IoT platforms maintain monitoring continuity across referrals, rehabilitation, and home care. This reduces complications caused by fragmented visibility.
These use cases succeed because they align technology with enterprise accountability. When IoT health monitoring platforms anchor critical workflows, they deliver sustained clinical impact and measurable financial returns at scale.
IoT Health Monitoring Cuts Admissions by 19–41%
Enterprise IoT health monitoring platforms consistently reduce readmissions and avoidable visits by enabling early intervention, continuous oversight, and data-backed clinical decisions.
Multi-site studies across the US demonstrate that when IoT health monitoring is embedded into real care workflows, it changes both clinical outcomes and cost structures.
A 2025 synthesis of RPM outcomes across 25 healthcare institutions paints a clear picture. Chronic-care programs backed by connected devices and clinical dashboards reduced chronic-complication admissions by 19–41%. These gains did not come from more data alone, but from timely action triggered by continuous insight.
1. Fewer Readmissions, Faster Financial Impact
Hospitals participating in mature RPM programs reported up to 85% reductions in readmission rates. One regional health system, Deaconess Health in Indiana, achieved a 50% drop in 30-day readmissions, translating into nearly USD 500,000 in direct savings from avoided penalties and inpatient costs.
These results matter at the enterprise level. Readmission penalties erode margins quickly, and IoT health monitoring platforms address the issue upstream by identifying deterioration days earlier, not after discharge failures occur.
2, Lower Clinical Load Without Sacrificing Care Quality
Beyond admissions, RPM programs significantly reduced day-to-day clinical demand. Some deployments reported 47% fewer overall medical visits and 51% fewer on-call emergency doctor interactions. Instead of replacing clinicians, IoT health monitoring platforms filtered noise, allowing teams to focus on patients who actually needed intervention.
The University of Pittsburgh Medical Center offers a strong example. UPMC reduced readmission penalties by 76% while maintaining patient satisfaction scores above 90%, proving that efficiency and patient experience can scale together.
These outcomes depend on platforms that combine device data, workflow-aware alerts, and integration into EHRs and care coordination systems. When RPM is treated as infrastructure rather than an add-on, healthcare organizations see durable ROI across clinical, operational, and financial dimensions.
Features of an Enterprise IoT Health Monitoring Platform
Enterprise IoT health monitoring platforms combine device control, real-time analytics, clinical workflows, and governance to deliver continuous care safely at scale.
The features below reflect how production-grade platforms are designed and evaluated by healthcare enterprises.
1. Device and Sensor Orchestration
The platform centrally manages medical-grade devices, wearables, bedside monitors, and home sensors across their entire lifecycle. This includes onboarding, identity verification, firmware updates, and ongoing device health monitoring.
Enterprises rely on this layer to ensure only authenticated and compliant devices generate clinical data.
At scale, device orchestration reduces operational risk. It prevents data gaps caused by malfunctioning or unverified hardware. It also enables rapid device replacement or reconfiguration without breaking downstream analytics and workflows.
2. High-Frequency Data Ingestion
IoT health monitoring platforms ingest large volumes of streaming data at high frequency. Vitals such as heart rate, SpO₂, and respiratory rate often arrive continuously rather than at scheduled intervals.
The platform must process this data in real time while retaining historical trends for longitudinal analysis.
Time-series processing enables trend evaluation instead of snapshot views. This distinction allows clinicians to recognize gradual deterioration earlier. It also forms the foundation for predictive analytics and risk scoring.
3. Clinical Rules Configuration
Clinical rules define how raw data becomes actionable insight. Enterprises configure thresholds, trend durations, and escalation logic based on clinical protocols and patient cohorts.
Alerts trigger when patterns indicate meaningful risk, not when a single value fluctuates briefly. Strong alert governance reduces clinician fatigue. It ensures notifications align with real clinical concern and workflow readiness. Over time, this builds trust in the monitoring system.
4. AI-Based Risk Scoring
AI models continuously analyze incoming vitals alongside context such as diagnosis, age, and historical data. The platform assigns dynamic risk scores that update as patient conditions evolve. These scores help teams prioritize attention across large monitored populations.
Importantly, AI augments clinical decision-making rather than replacing it. Clinicians retain control over final actions. AI provides early signals that might otherwise go unnoticed.
5. Care Workflow and Escalation Automation
Monitoring insight only creates value when it connects to action. Enterprise platforms route alerts into predefined care pathways rather than isolated dashboards. Tasks automatically reach the appropriate clinicians based on role, severity, and care program.
This automation reduces response delays. It also ensures consistency across teams and facilities. Every action is logged for continuity, accountability, and audit readiness.
6. EHR and Enterprise System Integration
Enterprise IoT platforms integrate bi-directionally with EHRs, care management systems, and analytics tools. Standards-based integration using FHIR and HL7 allows monitoring data to flow directly into the clinical record. This prevents data silos and duplicate documentation.
Integration ensures clinicians work within familiar systems. Monitoring insight becomes part of routine decision-making instead of a disconnected add-on.
7. Security, Privacy, and Compliance Enforcement
Security controls are foundational, not optional. Platforms encrypt PHI in transit and at rest while enforcing strict access policies. Role-based permissions ensure data visibility aligns with clinical responsibility.
Comprehensive audit logs record device interactions, data access, and clinical actions. These logs support regulatory audits, internal governance, and legal defensibility.
8. Program Analytics and Population Oversight
Beyond individual patients, enterprise teams need visibility into program performance. Dashboards track outcomes, alert effectiveness, adherence levels, and utilization trends. Leaders use these insights to refine protocols and resource allocation.
Population oversight transforms monitoring into a strategic asset. It allows organizations to measure ROI and adjust care models continuously.
These features work together to turn continuous monitoring into a dependable enterprise infrastructure. When properly implemented, IoT health monitoring platforms support safer care, stronger governance, and sustainable operational scale.
Core Architectural Layers of an Enterprise IoT Health Platform
An enterprise IoT health monitoring platform must remain stable under continuous data load while supporting clinical accountability. Its architecture is designed to move patient signals from devices to decisions without latency, data loss, or workflow disruption. Each layer plays a specific role in ensuring reliability, security, and scalability.
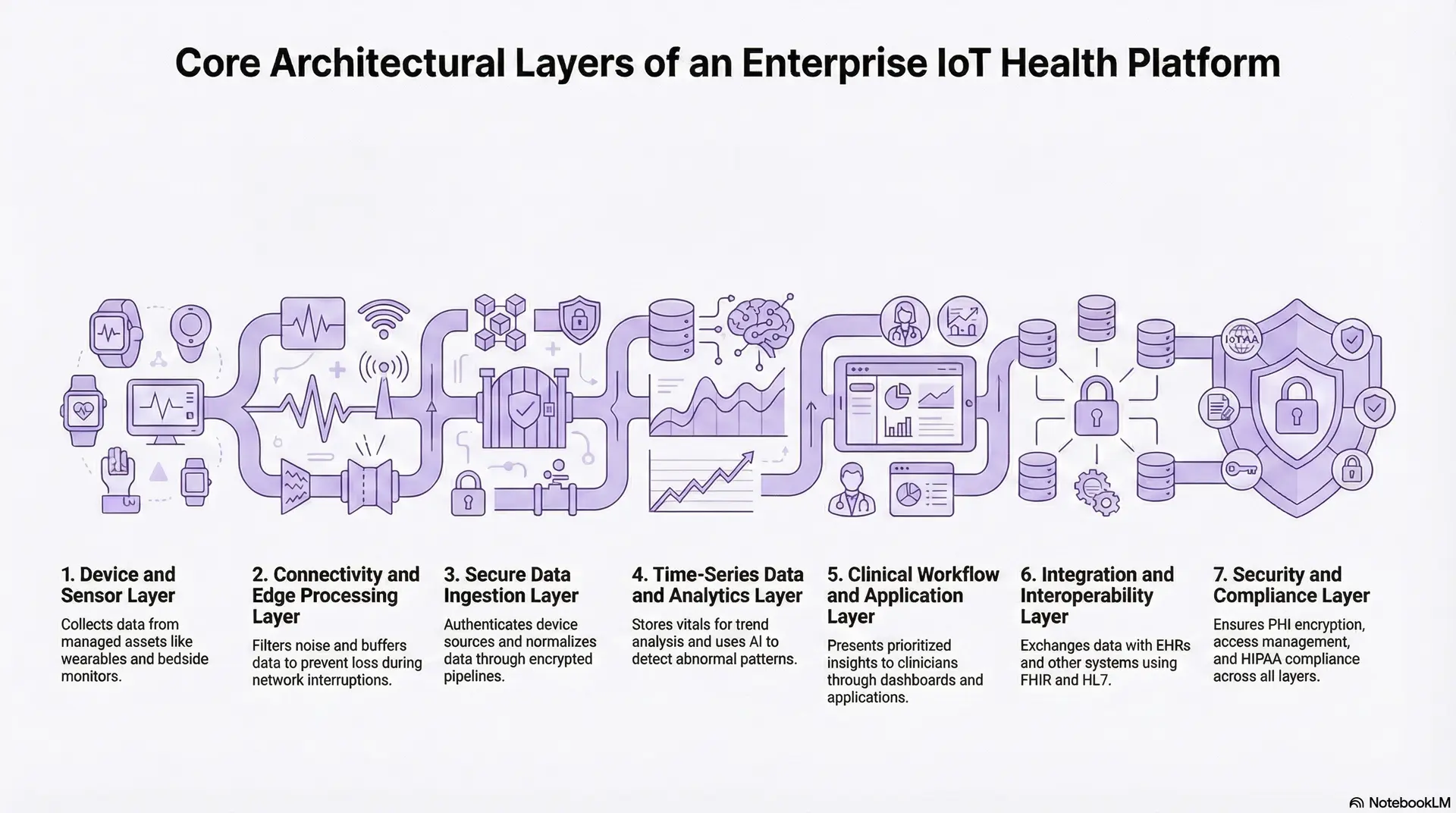
1. Device and Sensor Layer
This layer includes medical-grade wearables, bedside monitors, home devices, and ambient sensors. Devices are selected based on clinical accuracy, regulatory approval, and connectivity reliability. Enterprise platforms treat devices as managed assets, not plug-and-play peripherals.
The system continuously tracks device status, connectivity health, and data quality. Faulty or inactive devices are flagged early to avoid silent monitoring failures.
2. Connectivity and Edge Processing Layer
Devices transmit data through mobile apps, home gateways, or hospital networks. Edge processing filters noise, validates readings, and buffers data during network interruptions. This reduces latency and prevents data loss during connectivity gaps.
Edge logic is essential for time-sensitive monitoring. It ensures critical signals are captured even when cloud access is temporarily unavailable.
3. Secure Data Ingestion Layer
Validated data streams enter the platform through encrypted ingestion pipelines. The system authenticates device sources, timestamps readings, and normalizes data formats. This creates a consistent clinical data foundation across device types.
At scale, ingestion pipelines are built to handle continuous, high-frequency data without bottlenecks. This layer protects downstream analytics from corrupted or incomplete input.
4. Time-Series Data and Analytics Layer
The platform stores patient vitals as time-series data rather than static records. This allows trend analysis across minutes, hours, and days. Analytics engines evaluate patterns, persistence, and deviation from patient baselines.
AI models operate here to detect early deterioration, adherence issues, and abnormal patterns. Outputs are risk-aware signals, not raw data spikes.
5. Clinical Workflow and Application Layer
This layer includes clinician dashboards, care team workstations, and patient-facing applications. Interfaces present prioritized insights rather than overwhelming data streams. Views are tailored by role, care program, and urgency.
Applications integrate escalation logic, task assignment, and documentation. Monitoring becomes part of daily clinical operations instead of a parallel system.
6. Integration and Interoperability Layer
Enterprise platforms integrate with EHRs, care management tools, billing systems, and analytics platforms. Standards such as FHIR and HL7 support bi-directional data exchange. Monitoring data feeds directly into the longitudinal patient record.
Interoperability ensures monitoring does not increase clinician workload. It aligns IoT insight with existing enterprise systems and decision paths.
7. Security and Compliance Layer
Security controls span every architectural layer. PHI encryption, identity access management, and audit logging operate consistently across devices, data, and applications. Governance policies define who can access, act on, or modify information.
This layer supports HIPAA, GDPR, where applicable, and internal risk management. It enables trust from clinical, legal, and executive stakeholders.
A strong architecture is what allows IoT health monitoring platforms to scale safely. When each layer aligns around security, reliability, and workflow integration, continuous monitoring becomes enterprise-grade infrastructure rather than operational risk.
How AI Works in Enterprise IoT Health Monitoring Platforms
AI enables enterprise IoT health monitoring platforms to convert continuous device data into prioritized clinical insight without overwhelming care teams.
AI plays a focused role in enterprise IoT health monitoring. It is not deployed to automate medical decisions. Instead, it supports clinicians by identifying risk earlier, prioritizing attention, and reducing noise across high-volume data streams.
1. Predictive Risk Stratification
AI models analyze time-series vitals, symptom inputs, and historical patient data. The platform evaluates how readings change over time rather than reacting to single thresholds. This allows earlier identification of patients trending toward deterioration.
Risk scores update continuously as new data arrives. Care teams see who needs attention now, not just who already crossed a critical limit.
2. Anomaly Detection and Trend Analysis
AI monitors for deviations from a patient’s normal patterns. This includes subtle changes that static rules may miss. The system flags abnormal trends without triggering unnecessary alarms.
Trend-based detection improves sensitivity without increasing alert volume. It supports safer escalation in complex or chronic cases.
3. Alert Prioritization and Noise Reduction
AI helps suppress non-actionable alerts by factoring in context, persistence, and patient history. Notifications trigger only when changes remain significant over time.
This reduces alarm fatigue across clinical teams. Platforms use AI to rank alerts by urgency, and clinicians focus on the highest-risk patients first.
4. Population-Level Intelligence
Across large cohorts, AI identifies patterns that inform care models. The platform highlights emerging risks, adherence gaps, and outcome trends. Leaders use these insights to adjust protocols and allocate resources.
Population intelligence supports prevention strategies. It shifts monitoring from reactive response to strategic oversight.
5. Human-in-the-Loop Decision Support
AI outputs always remain reviewable and explainable. Clinicians see why risks are flagged and retain final authority over actions. Feedback from clinical decisions refines future model performance. This approach preserves trust while improving scale.
In enterprise IoT health monitoring, AI amplifies human judgment. When carefully governed, it enables earlier intervention, clearer prioritization, and long-term program optimization without compromising clinical control.
Overcoming Challenges in Building IoT Health Monitoring Platforms
Enterprise IoT health monitoring platforms fail when reliability, workflows, and governance are treated as add-ons rather than foundational design elements.
Developing an IoT health monitoring platform for enterprise healthcare introduces challenges that extend beyond technology. These platforms operate in clinical environments where delays, data gaps, or overload directly impact patient safety. Addressing these challenges requires architectural discipline, clinical alignment, and long-term operational thinking.
Challenge 1: Device Data Reliability and Continuous Visibility
Continuous monitoring relies on streams that must remain accurate and uninterrupted. In real deployments, devices disconnect, sensors degrade, and home networks remain unpredictable. When these failures are undetected, clinicians may operate on incomplete information without realizing it.
The way forward is to treat devices as managed infrastructure. Proven platforms implement automated device health checks, signal validation, and buffering mechanisms. When connectivity drops or data quality degrades, the system flags the issue operationally before it becomes a clinical blind spot.
Challenge 2: Alert Fatigue and Declining Clinical Trust
One of the fastest ways monitoring programs fail is through excessive alerts. Single-threshold triggers generate noise, leading clinicians to ignore notifications altogether. Over time, trust in the platform erodes.
Effective solutions shift alert logic from isolated readings to trend-based evaluation. By layering clinical rules with contextual analysis, alerts fire only when patterns indicate sustained risk. This restores confidence and ensures monitoring supports, rather than distracts from, care delivery.
Challenge 3: Poor Integration with Clinical Workflows
Monitoring systems often struggle because they operate outside the tools clinicians already use. Switching platforms, re-entering data, or checking separate dashboards slows adoption. Eventually, monitoring becomes optional rather than operational.
Successful implementations embed monitoring insight into EHRs, care coordination tools, and daily workflows. Standards-based integration allows data to flow into the systems where decisions already happen, reducing friction and improving response consistency.
Challenge 4: Security, Privacy, and Regulatory Exposure
Continuous monitoring expands the attack surface for sensitive health data. Multiple devices, transmission paths, and user roles increase security and compliance risks. Any gap can lead to regulatory exposure or loss of trust.
Mature platforms apply encryption, access controls, and audit trails consistently across all layers. Governance is enforced by design rather than policy alone. This approach protects patient data while simplifying compliance management as programs scale.
These challenges are design tests. Platforms that address them holistically move from pilot success to enterprise resilience. Those that do not struggle to scale safely or sustainably.
How We Develop Enterprise IoT Health Monitoring Platforms
Building an IoT health monitoring platform for enterprise healthcare is a multi-year infrastructure decision. Success depends on disciplined planning, clinical alignment, and engineering for scale from the first phase. Below is the process we follow to deliver platforms that perform reliably under real-world clinical pressure.
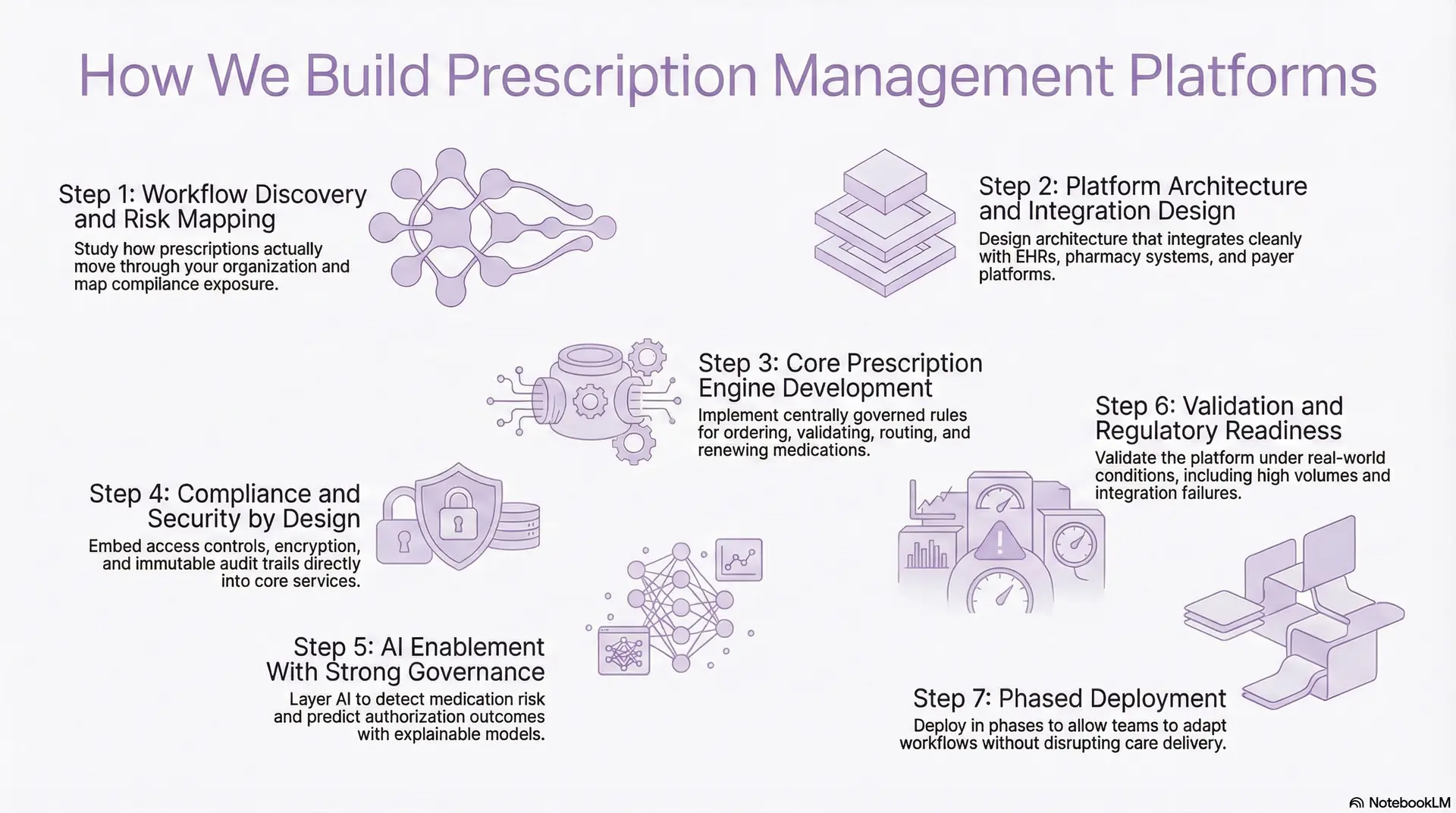
Step 1: Strategic Use Case Definition
Every initiative begins with a deep understanding of care delivery realities. We work with clinical leaders, operations teams, and IT stakeholders to identify where continuous monitoring can reduce risk or cost.
Use cases are evaluated based on clinical impact, operational feasibility, and scalability. This step prevents platform sprawl. It ensures development effort is focused on workflows that matter most to patient safety and enterprise performance.
Step 2: End-to-End Patient Journey Mapping
Once priorities are defined, patient journeys are mapped in detail. This includes transitions between care settings, escalation points, and handoffs between teams. Gaps where monitoring insight may be delayed or ignored are explicitly addressed.
Clear workflow mapping reduces resistance later. Teams see how monitoring fits into daily operations rather than disrupting them.
Step 3: Platform Architecture Design
The platform architecture is designed to support continuous data flow at scale. Cloud-native components enable elasticity, while modular services allow future expansion. Data models are optimized for time-series storage and longitudinal analysis.
Interoperability is treated as foundational. The architecture anticipates integration with EHRs, care management systems, and analytics platforms from the outset.
Step 4: Device Integration
Device selection focuses on clinical accuracy, regulatory approval, and deployment reliability. Devices are integrated with strong identity controls and lifecycle management. Connectivity, resilience, and data buffering are tested under real-world conditions.
This step establishes signal trust. Clinicians and operators must know that what they see reflects patient reality, not device artifacts.
Step 5: Analytics and AI Enablement
Analytics capabilities are layered once reliable data flows are established. Predictive models focus on identifying deterioration trends and prioritizing attention across monitored populations. Outputs are designed to be interpretable and clinically explainable.
Human oversight remains central. AI supports scale and speed without replacing clinical judgment or established protocols.
Step 6: Security and Compliance Engineering
Security controls are embedded across every layer of the platform. Data encryption, identity governance, and access controls are implemented consistently from device to application. Auditability supports regulatory review and internal accountability.
This approach minimizes long-term legal and operational risk. Compliance becomes an engineering outcome, not an administrative burden.
Step 7: Phased Deployment and Clinical Alignment
The platform is introduced through staged rollouts rather than enterprise-wide launches. Early deployments validate alert behavior, workflow fit, and staff readiness. Findings from pilot phases inform configuration updates before broader expansion.
Phased deployment protects care delivery. It allows refinement without exposing the organization to unnecessary risk.
Step 8: Optimization and Program Governance
Once live, performance and outcomes are continuously monitored. Alert effectiveness, adherence, and operational load are reviewed regularly. Governance frameworks guide updates as programs scale across facilities or regions.
This final step ensures longevity. The platform evolves with clinical needs rather than becoming rigid over time.
This structured approach transforms IoT health monitoring into a durable enterprise infrastructure. By aligning clinical reality, technical discipline, and governance from the start, organizations gain a platform built for growth, not fragility.
Cost to Develop an Enterprise IoT Health Monitoring Platform
For healthcare enterprises, hospital networks, and digital health providers, the cost of building an IoT health monitoring platform depends less on ambition and more on scope control and phased execution. Organizations that begin with a focused use case, such as post-discharge RPM or virtual ward monitoring, can launch an enterprise-grade platform without excessive upfront spend. Trying to cover every device, condition, and care model in phase one is where budgets usually spiral.
At Intellivon, we structure IoT health monitoring initiatives around phase-wise cost models. Each phase aligns with leadership budget cycles, regulatory readiness, and near-term operational ROI. This approach limits capital risk while ensuring the platform remains scalable, compliant, and architecturally future-proof from day one.
Estimated Phase-Wise Cost Breakdown
Enterprise IoT Health Monitoring Platform
| Phase | Description | Estimated Cost (USD) |
| Discovery & Clinical Blueprint | Care use-case definition, workflow mapping, RPM eligibility, compliance scoping | 12,000 – 20,000 |
| Platform Architecture & Data Design | Cloud-native architecture, time-series data model, scalability planning | 18,000 – 30,000 |
| Device Integration & IoT Pipeline Setup | Wearables, medical devices, gateways, ingestion pipelines | 25,000 – 45,000 |
| Analytics & AI Enablement | Risk scoring, trend analysis, alert prioritization logic | 20,000 – 40,000 |
| EHR & Enterprise Integrations | FHIR/HL7 integrations, care management alignment | 15,000 – 25,000 |
| Security, IAM & Compliance Controls | PHI encryption, role-based access, audit logging | 12,000 – 20,000 |
| Testing, QA & Clinical Validation | Data accuracy testing, workflow validation, performance audits | 10,000 – 18,000 |
| Pilot Deployment & Training | Live rollout, clinician onboarding, workflow tuning | 12,000 – 20,000 |
Total Initial Investment Range: USD 124,000 – 218,000
This investment supports a secure, compliant, enterprise-ready IoT health monitoring pilot for one high-impact program, such as RPM, virtual wards, or chronic care surveillance.
Annual Maintenance and Optimization Costs
Ongoing costs cover cloud infrastructure, device lifecycle management, compliance updates, integration support, analytics tuning, and AI model refinement.
- 12–20% of the initial build cost annually
- Approx. USD 15,000 – 45,000 per year
When platforms are built with modular services and governed analytics pipelines, these costs remain predictable as scale increases.
Hidden Costs Healthcare Organizations Should Plan For
Even well-planned IoT health monitoring programs introduce additional cost variables over time:
- Expansion into new care programs or disease cohorts
- Onboarding additional device vendors or sensor types
- Increased cloud streaming and storage costs as monitoring volume grows
- Regulatory updates affecting RPM, device data retention, or audit requirements
- Ongoing AI threshold tuning as patient populations diversify
- Clinical and operational training as programs mature
Accounting for these early protects multi-year budgets and reduces risk during audits or scale-up phases.
Best Practices to Stay Within the Budget
Healthcare organizations that control IoT platform costs effectively tend to:
- Start with one high-impact monitoring use case
- Limit device variety in initial deployments
- Use modular, cloud-native architectures
- Embed security and compliance controls from the outset
- Track clinical and operational ROI within the first six months
This ensures the platform proves real clinical and financial value before broader capital investment.
If you are planning an enterprise IoT health monitoring platform, we can help define a tailored cost estimate and phased rollout plan aligned with your care strategy, regulatory landscape, and long-term growth goals.
Examples of IoT Health Monitoring Platforms
Enterprise IoT health monitoring platforms succeed when they integrate devices, analytics, and workflows into scalable care models rather than operating as standalone tools.
Below are real-world platforms actively used by hospitals, health systems, and payers. Each example highlights how the platform works and the role it plays in enterprise care delivery.
1. Philips HealthSuite and eCareCompanion
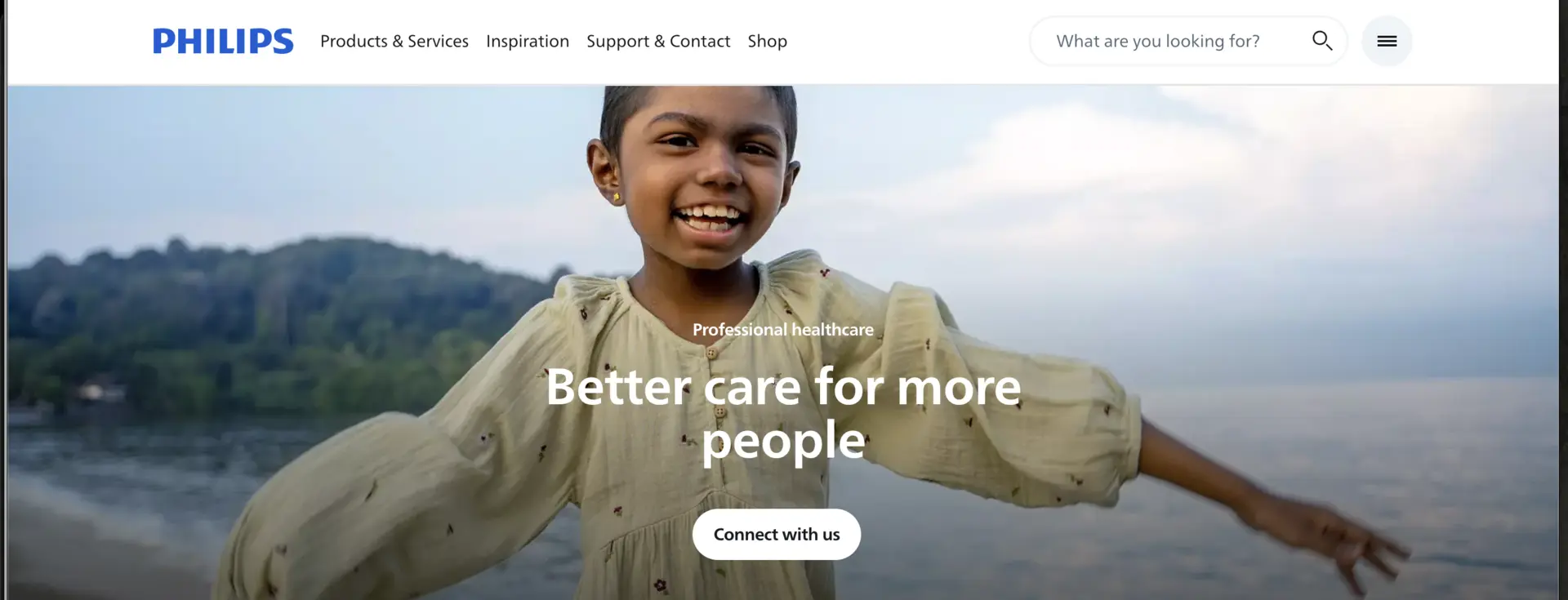
Philips HealthSuite operates as a cloud-based IoT and data platform that connects medical devices, patient apps, and clinician dashboards. It ingests continuous vitals from approved devices, normalizes data, and feeds insights into clinical systems. Care teams monitor patients through centralized dashboards with escalation workflows.
In enterprise use, the platform supports large RPM and virtual care programs. Health systems use it for chronic disease monitoring, post-discharge care, and population health analytics. Its strength lies in deep device interoperability and hospital-grade governance.
2. Biofourmis Biovitals Platform
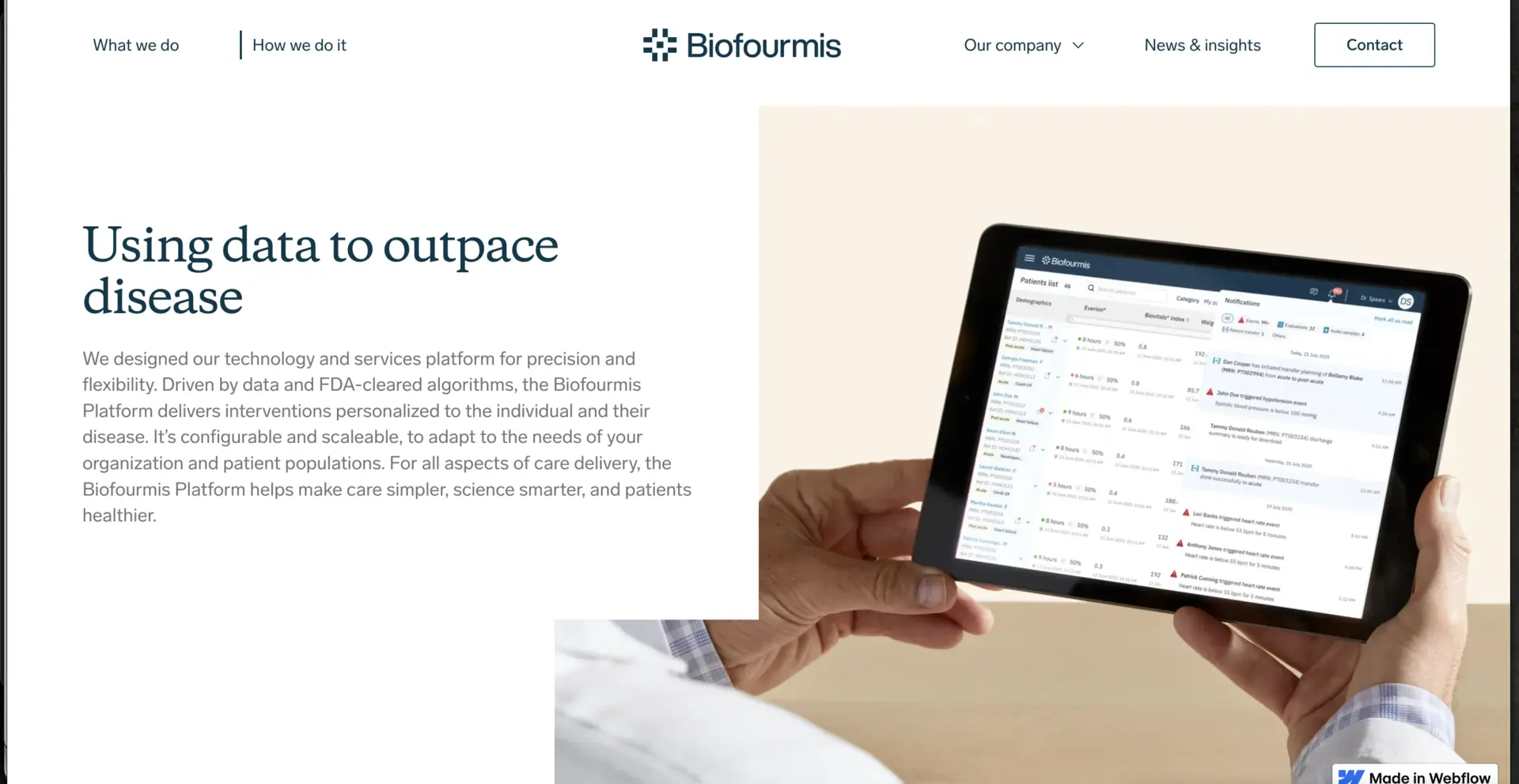
Biofourmis uses wearable sensors combined with AI models to track physiological trends continuously. The platform analyzes time-series data to detect early signs of deterioration and assigns dynamic risk scores. Alerts are routed to care teams based on severity and persistence.
Enterprises deploy Biofourmis for high-risk chronic care, oncology monitoring, and hospital-at-home programs. Its role is proactive risk identification, helping teams intervene earlier and reduce acute events across monitored populations.
3. Current Health (Best Buy Health)
Current Health integrates home monitoring devices with mobile connectivity and centralized care dashboards. The platform collects vitals, symptom reports, and adherence data in near real time. Data integrates with EHRs to support care coordination.
Health systems use it heavily for virtual wards and transitional care. It enables early discharge while maintaining inpatient-level visibility, helping enterprises release bed capacity without increasing risk.
4. Masimo SafetyNet
Masimo SafetyNet focuses on continuous wireless vital monitoring inside and outside the hospital. Wearable sensors transmit SpO₂, heart rate, and respiration to monitoring stations. Built-in analytics highlight subtle deterioration trends.
Hospitals use it to extend monitoring beyond ICUs into general wards. It plays a critical role in reducing unnoticed deterioration and unplanned ICU transfers while improving patient safety at scale.
5. Medtronic CareLink
Medtronic’s platforms collect continuous telemetry from implantable and wearable cardiac and diabetes devices. Data streams securely into clinician portals where trends and alerts guide intervention. The systems are tightly integrated with treatment hardware.
Enterprises rely on these platforms for long-term disease management programs. They enable continuous oversight for high-risk cardiac and diabetes populations and support value-based care outcomes.
These platforms illustrate how IoT health monitoring works in real enterprise environments. While their focus areas differ, each succeeds by embedding monitoring into care workflows, governance models, and operational strategy. For healthcare leaders, the takeaway is clear: enterprise value comes from platforms that connect data to decisions at scale.
Conclusion
Enterprise IoT health monitoring platforms are no longer optional infrastructure for healthcare organizations operating at scale. When designed correctly, they enable continuous visibility, earlier intervention, and smarter use of clinical resources. The real value lies not in devices alone, but in how data, workflows, and governance come together to support proactive care models that reduce risk and improve outcomes across populations.
Building these platforms requires disciplined architecture, clinical alignment, and a long-term view of compliance and scalability. With deep experience in enterprise healthcare platforms, AI-driven intelligence, and interoperability-first design, Intellivon helps organizations move beyond pilots to production-ready systems.
Build an Enterprise IoT Health Monitoring Platform With Intellivon
At Intellivon, we build enterprise-grade IoT health monitoring platforms that connect devices, data pipelines, analytics, and clinical workflows into one secure, real-time monitoring ecosystem. Our platforms unify wearable sensors, home devices, inpatient monitors, EHRs, and care management systems without disrupting live clinical operations.
Each solution is engineered for modern healthcare enterprises. Platforms are compliant by design, resilient under continuous data load, interoperable across devices and vendors, and built to deliver measurable clinical and operational ROI from the first phase of deployment.
Why Partner With Intellivon?
- Compliance-First Architecture: Every platform aligns with HIPAA, GDPR, where applicable, FDA-connected device considerations, and regional healthcare regulations, with audit-ready governance embedded across all layers.
- Device-Agnostic IoT Engineering: We integrate seamlessly with medical-grade devices, wearables, bedside monitors, and home sensors without locking enterprises into a single vendor ecosystem.
- Interoperability-Driven Platform Design: Native support for FHIR, HL7, secure APIs, and enterprise messaging enables smooth integration with EHRs, care management platforms, analytics stacks, and payer systems.
- Cloud-Native and Scalable Monitoring Infrastructure: Our architectures support high-frequency, time-series data streaming with elastic performance across multi-hospital and multi-region deployments.
- AI-Driven Risk and Alert Intelligence: Built-in analytics detect early deterioration, prioritize clinical action, and reduce alert fatigue while keeping clinicians firmly in control.
- Zero-Trust Security and PHI Protection: End-to-end encryption, identity-first access controls, and continuous monitoring protect sensitive health data without slowing clinical workflows.
Book a strategy call with Intellivon to explore how a custom-built IoT health monitoring platform can reduce risk, improve outcomes, and scale proactive care across your healthcare enterprise.
FAQs
Q1. How secure are IoT health monitoring platforms for enterprise healthcare?
A1. Enterprise IoT health monitoring platforms are secure when designed with compliance and governance built into the architecture. Mature platforms encrypt PHI in transit and at rest, enforce role-based access, and maintain immutable audit trails. Security must extend across devices, data pipelines, APIs, and user access. Without this end-to-end approach, risks increase rapidly as monitoring programs scale.
Q2. What devices can integrate with an enterprise IoT health monitoring platform?
A2. Enterprise platforms support medical-grade wearables, bedside monitors, home devices, and condition-specific sensors. Integration typically includes FDA-cleared or CE-approved devices, along with selected consumer wearables used in RPM programs. Device-agnostic design is critical, allowing organizations to add or replace devices without re-architecting the platform.
Q3. How long does it take to build an enterprise IoT health monitoring platform?
A3. Timelines depend on scope and deployment strategy. A focused, enterprise-ready pilot for RPM or virtual wards typically takes 4–6 months. Larger multi-facility platforms roll out in phases over 6–12 months, allowing clinical validation, workflow tuning, and controlled scaling without disrupting live operations.
Q4. What regulations apply to IoT health monitoring systems?
A4. IoT health monitoring platforms must comply with HIPAA and regional health data regulations, such as GDPR, where applicable. FDA considerations apply when platforms support clinical decision workflows or connected medical devices. Enterprises also need audit readiness, access governance, and data retention controls to satisfy payer and regulatory scrutiny.
Q5. What is the ROI of IoT health monitoring for hospitals and health systems?
A5. ROI typically comes from reduced readmissions, fewer emergency escalations, improved bed utilization, and lower staff workload. Enterprises also benefit from avoided penalties, better chronic care outcomes, and scalable virtual care models. When deployed correctly, IoT monitoring shifts care from reactive interventions to proactive prevention, driving both clinical and financial gains.