Despite growing interest in women’s health, care delivery remains scattered across different specialties, providers, and digital tools. Patients frequently shift between OB-GYNs, mental health professionals, menopause specialists, and primary care without a unified care context. This lack of coordination leads to both clinical risks and inefficiencies.
HerMD has demonstrated that a dedicated telemedicine platform for women’s health can tackle these issues when properly designed. By combining clinical services, patient engagement, and secure data management into one platform, HerMD fosters long-term care while ensuring operational efficiency and compliance with regulations.
At Intellivon, we focus on creating high-quality digital health platforms that go beyond temporary pilot programs and develop into ongoing operations. In this blog, we use our experience to explain how to create a women’s health telemedicine app like HerMD from the ground up.
The Right Time To Invest In Building Women’s Health Apps
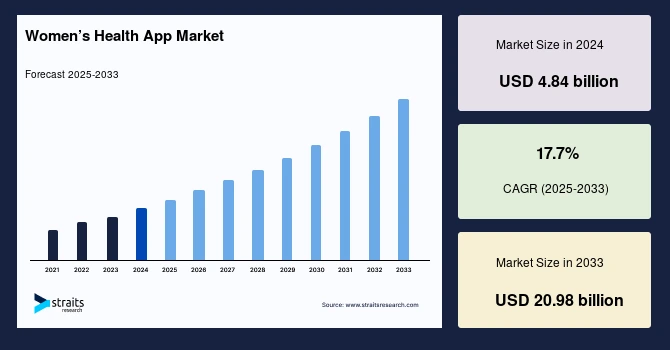
Women’s health applications are moving into a high-growth phase. The market, valued at USD 4.84 billion in 2024, is expected to scale rapidly, growing from roughly USD 5.7 billion in 2025 to more than USD 20 billion by 2033. This pace translates into a compound annual growth rate of 17.7%, according to Straits Research.
Growth Drivers Behind Women’s Telemedicine Apps
- Unmet clinical needs: High prevalence of PCOS, infertility, endometriosis, menopause symptoms, and maternal care gaps is driving demand for specialized digital platforms.
- Access through mobility: Smartphone penetration and improved connectivity are enabling telemedicine access across urban and emerging markets.
- Preventive care shift: Women increasingly favor proactive health tracking, education, and early intervention over episodic treatment.
- AI-led personalization: Predictive insights for cycles, fertility, and hormone trends increase engagement and clinical relevance.
- Policy and social change: Reduced stigma, employer wellness programs, and digital health initiatives are accelerating adoption.
Adoption & Performance of Women’s Health Apps
- Sustained usage growth: Women’s health app markets are projected to grow from USD 3–4 billion in 2024 to USD 21–27 billion by the mid-2030s.
- Regional indicators: In developed markets, nearly half of women aged 18–44 use digital tools for wellness, signaling broader global uptake.
- Telehealth integration: Apps embedding virtual consults see stronger retention across reproductive, mental, and menopause care.
- Mental health acceleration: Women-focused mental health solutions are among the fastest-growing digital health segments.
Growth Opportunities for Businesses Entering Women’s Telemedicine
- Vertical-first platforms: Build women-centered systems spanning fertility, pregnancy, menopause, pelvic, and mental health.
- B2B2C expansion: White-label telemedicine stacks for employers, payers, and provider networks support value-based care.
- AI decision support: Add predictive modules for hormone trends, fertility risk, and symptom triage into care workflows.
- Emerging market focus: Asia-Pacific and India present strong growth driven by public digital health programs and awareness.
- Hybrid care models: Combine apps with clinics, labs, and pharmacies to deliver integrated digital–physical care experiences.
What Is The Women’s Health Telemedicine App HerMD?
HerMD is a women’s health telemedicine platform built to address care gaps that traditional systems often overlook. It brings together OB-GYN care, menopause support, mental health, sexual wellness, and preventive services within a single digital environment.
By designing care around women’s real-life stages, HerMD moves beyond episodic virtual visits and supports ongoing clinical relationships.
What sets HerMD apart is how the platform integrates sensitive care delivery with trust and accessibility. Patients can engage with specialized providers through secure teleconsultations while maintaining continuity across visits. Care plans, follow-ups, and clinical context remain connected, reducing friction for both patients and care teams.
HerMD has helped reshape expectations around women’s digital health by proving that telemedicine can support long-term outcomes, not just access. Its platform model shows how focused digital infrastructure can drive engagement, improve care coordination, and create scalable women-first healthcare systems.
Features That Make The HerMD App Stand Out
HerMD is not designed as a general telehealth app adapted for women’s care. Its features are built around the clinical, emotional, and operational realities of women’s health. Each capability supports continuity, trust, and long-term engagement rather than one-off virtual visits.
1. Integrated Multi-Specialty Care
The platform connects OB-GYNs, menopause specialists, mental health professionals, and primary care providers within a shared care environment. This allows care teams to collaborate without fragmenting patient history or clinical context.
2. Longitudinal Care Journeys
HerMD supports care over time, not just during isolated appointments. Patients can return for follow-ups, ongoing symptom tracking, and evolving care plans that reflect changing health needs across life stages.
3. Privacy-First Data Handling
Women’s health data requires heightened sensitivity. The platform applies strict access controls, consent management, and secure data storage to protect intimate health information at every step.
4. Flexible Teleconsultation Models
HerMD enables both real-time video visits and asynchronous communication. This flexibility helps patients access care when schedules are unpredictable, while clinicians manage workload more effectively.
5. Continuity-Driven Patient Experience
From intake to follow-up, the experience is designed to reduce repetition and friction. Clinical notes, treatment decisions, and patient history remain connected across interactions.
HerMD’s feature set reflects a deeper understanding of women’s healthcare delivery. By prioritizing continuity, privacy, and coordinated care, the platform sets a clear benchmark for what modern women’s health telemedicine apps should deliver at scale.
What Makes HerMD’s Business and Revenue Models Scalable for Enterprises?
Women’s health platforms succeed or fail based on how well their business design supports clinical depth and operational scale. HerMD stands out because its business and revenue models are built to grow without compromising care quality, compliance, or patient trust. The platform balances consumer accessibility with enterprise-grade structure, making it suitable for long-term expansion.
Business Models of HerMD
HerMD operates on a platform-first business model that supports multiple care pathways under one digital umbrella. This approach allows the organization to expand services, locations, and partnerships without rebuilding core infrastructure.
1. Hybrid Digital and In-Person Care Model
HerMD combines telemedicine with physical clinics. Patients can move seamlessly between virtual consultations and in-person visits, which improves care continuity and supports higher-acuity services when needed.
2. Women-Centric Vertical Specialization
Instead of offering broad telehealth services, HerMD focuses exclusively on women’s health. This specialization enables deeper clinical protocols, targeted care pathways, and stronger brand trust.
3. Scalable Provider Network
The platform supports distributed provider teams across specialties and locations. Standardized workflows and shared patient context allow HerMD to scale clinician capacity without increasing operational complexity.
4. Enterprise-Ready Platform Design
HerMD’s model supports expansion through new clinics, markets, and service lines. The platform adapts to regulatory requirements and operational differences without fragmenting the care experience.
HerMD’s business model is designed for controlled growth. By aligning digital access with physical care and operational governance, the platform scales while maintaining clinical and brand consistency.
Revenue Models of HerMD
HerMD’s revenue strategy reflects the diversity of women’s healthcare needs and payer dynamics. The platform avoids reliance on a single revenue stream, which improves financial resilience as it grows.
1. Visit-Based Telemedicine Revenue
Virtual consultations generate direct revenue while lowering delivery costs. This model supports access and allows flexible pricing across care types.
2. In-Person Clinical Services
Physical clinic visits, diagnostics, and procedures contribute higher-margin revenue. These services complement telemedicine rather than competing with it.
3. Hybrid Care Pathway Monetization
Patients often move between virtual and in-person care. This blended approach increases lifetime value by supporting longer care relationships.
4. Partnerships and Employer Programs
HerMD can collaborate with employers, payers, and health networks. These partnerships enable population-based programs and recurring revenue opportunities.
By combining telemedicine, clinical services, and partnerships, HerMD creates predictable and scalable revenue streams. This structure supports sustainable growth while aligning financial performance with patient outcomes.
Women’s App Delivered 91.7% Certainty In Post-Partum BP Readings
Post-partum hypertension is common, dangerous, and often missed. The issue is not clinical knowledge. It is a follow-up. New mothers struggle to return for in-office checks, while care teams lack reliable visibility once patients leave the hospital.
A randomized clinical trial showed what changes when blood pressure monitoring moves into a women’s health app. BP ascertainment reached 91.7% with remote monitoring, compared to 58.4% through in-office follow-up. Patients in the remote arm submitted a median of 15 readings, creating a continuous signal instead of a single data point.
1. Why Post-Partum BP Monitoring Breaks Traditional Care Models
Post-partum care is time-compressed and fragmented. Patients are discharged quickly, schedules are disrupted, and symptoms escalate quietly.
In-office follow-ups rely on patients returning at the right time. As a result, hypertension is detected late, or not at all. From an enterprise perspective, this increases readmission risk, liability exposure, and downstream costs.
Remote monitoring shifts the burden away from appointments and into daily life, where data is actually generated.
2. How Women’s Health Apps Achieve Higher BP Certainty
The improvement to 91.7% BP ascertainment did not come from better clinicians. It came from better system design.
Women’s health apps enable:
- At-home BP capture using validated devices
- Automated reminders tied to post-partum timelines
- Simple data submission flows that fit daily routines
Instead of relying on a single visit, clinicians receive repeated measurements. This produces confidence in trends, not guesses based on one reading.
3. What 15 Median Readings Change for Clinical Decisions
A median of 15 BP readings per patient changes how care teams operate.
Clinicians can:
- Detect early escalation before symptoms worsen
- Adjust medications based on trends, not snapshots
- Intervene remotely without triggering unnecessary visits
For enterprises, this reduces avoidable admissions and supports protocol-driven care at scale. It also standardizes follow-up across populations, not just those who can return to clinics.
4. Operational Impact for Health Systems
Remote BP monitoring through a women’s health app delivers measurable operational value.
It improves follow-up compliance without adding staff, creates auditable data trails for quality reporting, and supports equity by removing barriers tied to transportation, work schedules, and caregiving responsibilities.
Most importantly, it transforms post-partum care from reactive to proactive.
The jump from 58.4% to 91.7% BP ascertainment is not incremental. It reflects a structural shift in how post-partum care is delivered. Women’s health apps turn monitoring into a continuous process, not a one-time event.
What Features Are Required In A Women’s Health Telemedicine App?
A woman’s health telemedicine app must support more than virtual consultations. It needs to manage sensitive data, enable continuity across life stages, and operate reliably at enterprise scale. The features below are foundational, not optional, for platforms expected to deliver long-term value.
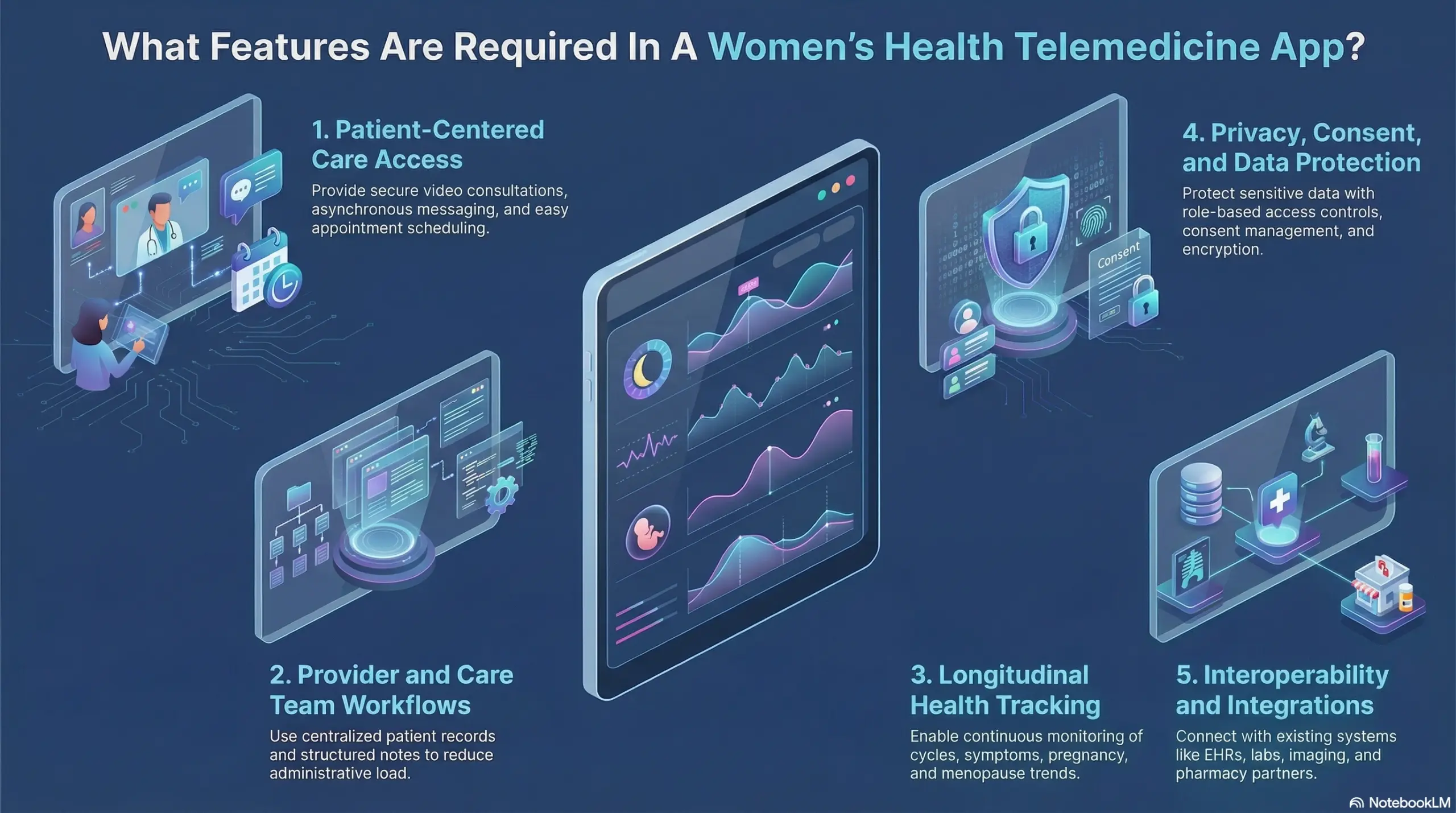
1. Patient-Centered Care Access
Women’s health care often spans years and involves multiple specialties. Platforms must support easy access without forcing patients through repetitive intake or disconnected visits.
Key capabilities include:
- Secure video and audio consultations
- Asynchronous messaging for follow-ups
- Appointment scheduling with reminders
- Digital intake tailored to women’s health needs
These features reduce friction and improve engagement across busy life stages.
2. Provider and Care Team Workflows
Clinical teams need tools that reduce administrative load while preserving clinical context. Without this, platforms struggle as volume grows.
Essential provider features include:
- Centralized patient records across visits
- Structured documentation and clinical notes
- Care coordination across specialties
- Task management and follow-up tracking
Well-designed workflows support consistency and clinician adoption.
3. Longitudinal Health Tracking
Women’s health requires continuity. Platforms must track changes over time, not just record isolated interactions.
Common tracking capabilities include:
- Cycle and symptom monitoring
- Pregnancy and post-partum tracking
- Menopause symptom trends
- Remote vital monitoring, where applicable
Longitudinal data enables proactive care and better decisions.
4. Privacy, Consent, and Data Protection
Sensitive health data demands strict governance. Trust depends on how well platforms protect patient information.
Core privacy features include:
- Role-based access controls
- Explicit consent management
- Encrypted data storage and transmission
- Comprehensive audit trails
These controls support compliance and patient confidence.
5. Interoperability and Integrations
Enterprise platforms must connect with existing healthcare systems. Isolation creates risk and inefficiency.
Integration requirements include:
- EHR and practice management systems
- Labs, imaging, and pharmacy partners
- Secure APIs for future expansion
Interoperability ensures scalability and operational alignment.
A women’s health telemedicine platform succeeds when features align with real-world care delivery. By prioritizing continuity, privacy, and operational efficiency, enterprises can build platforms that support both clinical excellence and sustainable growth.
How Do Women’s Health Telemedicine Apps Handle Sensitive Patient Data Securely?
Women’s health platforms manage some of the most sensitive clinical data in healthcare. Reproductive health, mental health, sexual wellness, and post-partum records demand a higher standard of security and governance. Trust depends on how well these systems protect information at every touchpoint.
1. Identity, Access, and Role Controls
Access to patient data must be intentional and limited. Not every user needs full visibility.
Platforms apply role-based access controls to ensure clinicians, care coordinators, and support staff see only what is required. Identity verification, session controls, and access logging prevent misuse and support accountability across teams.
2. Consent Management and Patient Control
Consent is not a one-time checkbox, but an ongoing process. Women’s health apps allow patients to grant, modify, or revoke consent for specific data types and providers.
This flexibility respects patient autonomy and supports compliance across evolving care journeys.
3. Data Encryption and Secure Storage
Data protection extends beyond transmission. Platforms encrypt information both in transit and at rest.
Secure storage environments, key management practices, and regular security testing reduce exposure and protect against unauthorized access.
4. Audit Trails and Compliance Readiness
Visibility matters for governance. Comprehensive audit logs track data access, changes, and clinical actions.
These records support regulatory audits, internal reviews, and risk management without disrupting care delivery.
Secure handling of sensitive data is foundational to women’s health telemedicine. Platforms that embed security, consent, and governance into their core architecture earn patient trust and reduce enterprise risk while enabling scalable care delivery.
What Compliance Requirements Apply To Women’s Health Telemedicine Platforms?
Compliance is not a checklist item for women’s health telemedicine. It shapes architecture, workflows, and daily operations. Platforms that treat compliance as an afterthought struggle to scale, especially when handling reproductive, mental health, and post-partum care.
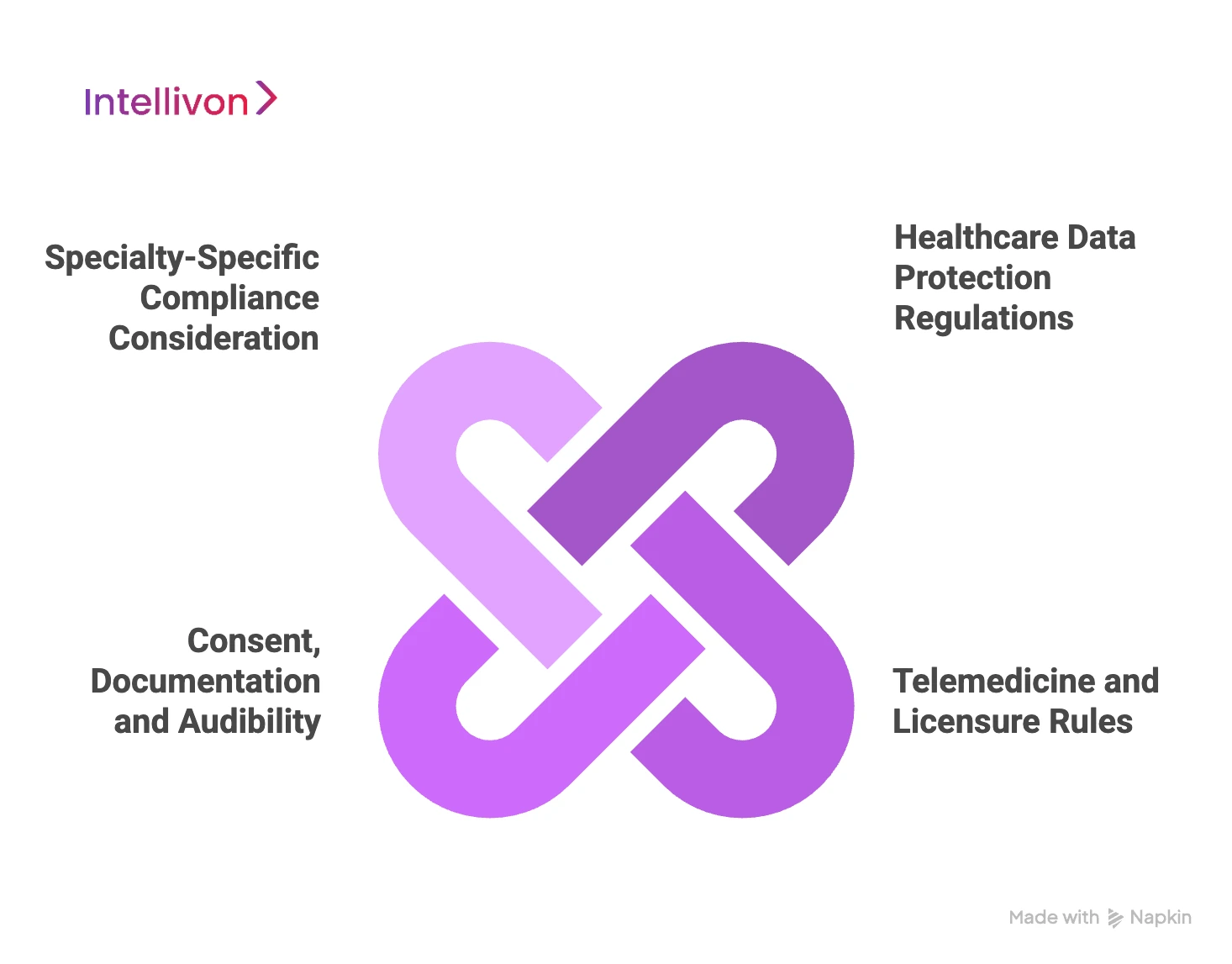
1. Healthcare Data Protection Regulations
Women’s health platforms must meet strict data protection standards from day one. In the United States, HIPAA and HITECH govern how patient data is stored, accessed, and shared.
For platforms serving global users, GDPR adds requirements around consent, data minimization, and patient rights. These regulations influence database design, access controls, and audit readiness.
2. Telemedicine and Licensure Rules
Virtual care is regulated at the state and regional level. Providers must be licensed where the patient is located at the time of care. Platforms need built-in checks to manage provider eligibility, location awareness, and service restrictions.
Without this, enterprises face regulatory exposure as they expand across regions.
3. Consent, Documentation, and Auditability
Women’s health care involves heightened consent requirements. Platforms must capture informed consent for telemedicine, data sharing, and sensitive services.
Every interaction, decision, and data change must be documented with clear audit trails to support compliance reviews and legal inquiries.
4. Specialty-Specific Compliance Considerations
Certain women’s health services introduce additional oversight. Reproductive health, mental health, and medication management may require enhanced documentation, prescribing controls, and privacy safeguards.
Platforms must adapt workflows to these clinical realities without slowing care delivery.
Compliance defines whether a women’s health telemedicine platform can grow safely. Enterprises that embed regulatory requirements into platform design reduce risk, protect trust, and create a foundation for sustainable expansion across services and geographies.
How Do Women’s Health Apps Integrate With EHRs And Pharmacies?
Women’s health telemedicine apps cannot operate in isolation. To deliver safe and continuous care, they must connect seamlessly with existing clinical and medication systems. Integration is what turns a digital experience into an operational care platform.
1. EHR Integration for Clinical Continuity
EHR connectivity ensures that patient history does not reset with every visit. Women’s health apps integrate with EHR systems using standards such as FHIR and HL7.
This allows clinical notes, lab results, diagnoses, and care plans to move securely between systems. Clinicians gain full context, while patients avoid repeating sensitive information.
2. Pharmacy Integration for Medication Management
Medication workflows are central to women’s health care. Apps connect with pharmacy systems to support e-prescribing, refill requests, and medication status updates.
This reduces delays, improves adherence, and ensures prescriptions align with ongoing care plans, especially for hormonal and post-partum treatments.
3. Lab and Diagnostic Connectivity
Many women’s health decisions depend on diagnostics. Integration with labs and imaging providers enables test ordering, result retrieval, and follow-up within the app.
Care teams can act quickly, while patients receive clear guidance without switching platforms.
4. Secure APIs and Data Governance
Integrations must remain controlled. Women’s health platforms use secure APIs, authentication layers, and data governance policies to manage third-party access.
This protects patient data while allowing systems to scale and evolve.
EHR and pharmacy integration is essential for women’s health telemedicine platforms. When done correctly, it supports continuity, safety, and operational efficiency, enabling enterprises to deliver coordinated care without fragmentation.
How Is AI Used in Women’s Health Telemedine Apps?
AI has become a foundational layer in modern women’s health telemedicine apps, but its real value lies in how deliberately it is applied. In enterprise-grade platforms, AI is used to strengthen care delivery, reduce operational strain, and improve clinical consistency, while keeping human clinicians firmly in control.
When implemented correctly, AI enhances decision-making rather than automating care blindly.
1. Intelligent Intake and Clinical Triage
AI-driven intake systems help structure patient information before a consultation begins. By analyzing reported symptoms, medical history, and contextual signals, AI can surface potential risk factors and care priorities early.
This allows care teams to route patients to the appropriate specialists, identify urgent cases faster, and reduce time spent on manual screening. Clinicians enter each visit with a clearer picture, which improves efficiency and reduces missed signals in complex women’s health cases.
2. Longitudinal Pattern and Trend Analysis
Women’s health data is inherently longitudinal, spanning cycles, pregnancies, post-partum phases, and menopause transitions. AI models are well-suited to detect patterns that are difficult to identify through episodic review.
By analyzing trends across symptoms, vitals, lab results, and treatment responses, AI can flag deviations from baseline and emerging risks. This supports earlier intervention and more personalized care across fertility, pregnancy, and chronic conditions.
3. Clinical Decision Support for Providers
AI supports clinicians by organizing information and highlighting relevant insights, not by replacing judgment. Decision support tools compare patient data against clinical guidelines, historical outcomes, and similar cases.
This helps providers maintain consistency across care teams and locations. It also reduces cognitive load during complex decision-making, especially in multi-specialty women’s health environments where care pathways overlap.
4. Patient Engagement and Care Adherence
Sustained engagement is critical for outcomes in women’s health. AI helps personalize how patients interact with their care plans over time.
Through tailored reminders, educational prompts, and follow-up notifications, AI encourages adherence without overwhelming patients. This results in better continuity, improved satisfaction, and more reliable clinical outcomes at scale.
AI delivers value in women’s health telemedicine when it is embedded into clinical and operational workflows. By improving visibility, supporting informed decisions, and strengthening engagement, AI enables platforms to scale responsibly while maintaining care quality and trust.
How We Build Women’s Health Telemedicine Apps Like HerMD
Building a women’s health telemedicine platform requires more than video visits and scheduling. You need secure data handling, clinical workflow depth, and integrations that work inside real healthcare operations. At Intellivon, we build enterprise-grade women’s health platforms designed to scale across service lines, regions, and care models.
Below is our 8-step build process, used to take platforms from concept to production with predictable outcomes.
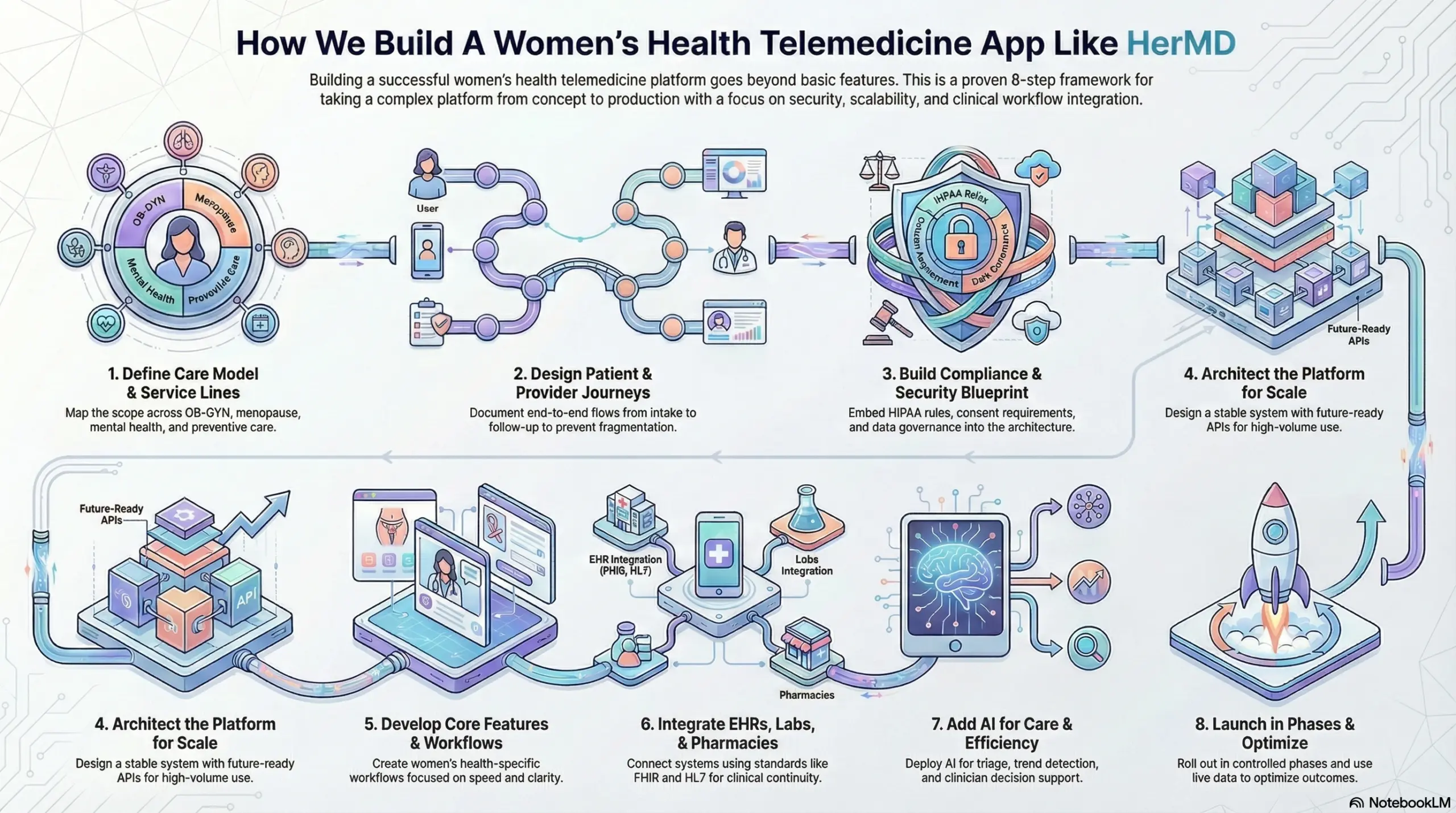
Step 1: Define the Care Model and Service Lines
We start by mapping your women’s health scope across OB-GYN, menopause, sexual health, mental health, and preventive care. Then we define which services run virtual-first, hybrid, or in-person. This shapes clinical workflows, staffing, and unit economics.
Step 2: Design the Patient and Provider Journeys
Next, we design end-to-end journeys from intake to follow-up. We document patient flows, provider tasks, escalation rules, and care coordination points. This prevents fragmented experiences and reduces operational burden later.
Step 3: Build a Compliance and Security Blueprint
We translate HIPAA, consent requirements, audit needs, and data governance into platform requirements.
This includes identity controls, role-based access, encryption strategy, and audit trails. Security becomes embedded in architecture, not added after launch.
Step 4: Architect the Platform for Scale
We design scalable system architecture with clear service boundaries and future-ready APIs.
This includes scheduling, telemedicine, messaging, care plans, and reporting. The goal is stability under volume, not a fragile MVP.
Step 5: Develop Core App Features and Clinical Workflows
We build patient and provider experiences with women’s health-specific workflows.
This includes structured intake, longitudinal tracking, follow-up pathways, and care plan management. We focus on speed for clinicians and clarity for patients.
Step 6: Integrate EHRs, Labs, and Pharmacies
We connect the platform to EHR systems, lab partners, and pharmacy workflows using healthcare standards like FHIR and HL7, where applicable.
This ensures clinical continuity and reduces duplicated documentation.
Step 7: Add AI Where It Improves Care and Efficiency
We deploy AI modules for triage support, trend detection, decision support, and engagement prompts. We keep clinicians in control and design governance around model outputs. AI becomes a reliability layer, not a risk layer.
Step 8: Launch in Phases and Optimize With Real Data
We roll out the platform in controlled phases, starting with pilot cohorts and measurable KPIs. Then we optimize workflows, retention, clinical outcomes, and cost drivers using live operational data.
This approach supports safe scaling across regions and service lines.
Intellivon builds these platforms as enterprise systems that support growth, not short-term deployments. If you are planning to launch or modernize a women’s health telemedicine app, talk to Intellivon about building a platform that is secure, scalable, and ready for long-term care delivery.
How Much Does It Cost To Build A Women’s Health Telemedicine App Like HerMD?
Building a women’s health telemedicine app like HerMD does not require a massive, upfront technology investment. Most successful enterprises begin with a focused, compliant foundation that supports core care delivery, privacy, and integrations, then expand capabilities as utilization grows.
At Intellivon, we structure costs around platform maturity, not feature overload. This approach helps organizations launch faster, validate demand, and scale without locking capital into unnecessary complexity early on.
Estimated Cost Breakdown (USD 60,000–160,000)
| Cost Component | What It Covers | Estimated Range |
| Discovery & Platform Design | Care model definition, workflows, architecture, and compliance planning | $8,000 – $15,000 |
| Patient & Provider App Development | Teleconsults, scheduling, messaging, care journeys | $15,000 – $30,000 |
| Women’s Health Workflows | OB-GYN, menopause, mental health, post-partum flows | $10,000 – $20,000 |
| Telemedicine Infrastructure | Video, async care, notifications, session controls | $8,000 – $15,000 |
| EHR, Lab & Pharmacy Integrations | FHIR/HL7 connectors, prescriptions, diagnostics | $10,000 – $25,000 |
| Security & Compliance Controls | HIPAA, consent, RBAC, audit trails | $7,000 – $15,000 |
| AI Enablement (Optional Phase) | Intake triage, trend analysis, engagement logic | $8,000 – $15,000 |
| Testing, Launch & Stabilization | QA, pilot rollout, performance tuning | $6,000 – $10,000 |
Typical MVP Range: $60,000 – $100,000
Enterprise-Ready Phase 1 Platform: $120,000 – $160,000
The final cost depends on how much clinical depth, control, and scalability you need from day one.
Factors Affecting the Cost of Building Women’s Health Telemedicine Platforms
The cost of a women’s health telemedicine app is not driven by screens alone. It is shaped by care complexity, compliance depth, and integration scope. These factors determine long-term sustainability.
1. Scope of Women’s Health Services
Platforms covering basic teleconsults cost less than those supporting fertility, pregnancy, menopause, and mental health together. Each additional service introduces workflow and compliance requirements.
2. Compliance and Data Sensitivity
Women’s health data demands stricter consent, access control, and auditability. Deeper governance increases engineering effort but reduces long-term risk.
3. Integration Depth
Connecting to one EHR differs from supporting multiple systems, labs, and pharmacies. Each integration adds mapping, testing, and maintenance overhead.
4. Longitudinal Care and Monitoring
Apps designed for one-time visits cost less than those tracking symptoms, vitals, and outcomes over time. Longitudinal care requires stronger data models.
5. AI and Analytics Expectations
Basic reporting is cheaper than predictive insights and real-time clinical dashboards. Advanced analytics require robust data pipelines.
How to Stay Within Budget Without Compromising Control
Enterprises stay within budget by building in phases. Start with core telemedicine, women’s health workflows, and compliance. Validate engagement and outcomes. Then expand integrations, AI, and analytics based on real usage data.
At Intellivon, we help organizations build women’s health telemedicine platforms that balance speed, control, and scalability. If you are evaluating costs or planning a phased rollout, talk to Intellivon about building a women’s health platform that delivers value without overextending capital.
What Tech Stack Is Used To Build A Women’s Health Telemedicine App?
A woman’s health telemedicine app needs more than standard mobile development. It must support secure video care, longitudinal health data, integrations with clinical systems, and compliance-grade controls. The right stack prioritizes reliability, auditability, and scale.
Below is a practical enterprise stack, organized by layer, with example technologies under each.
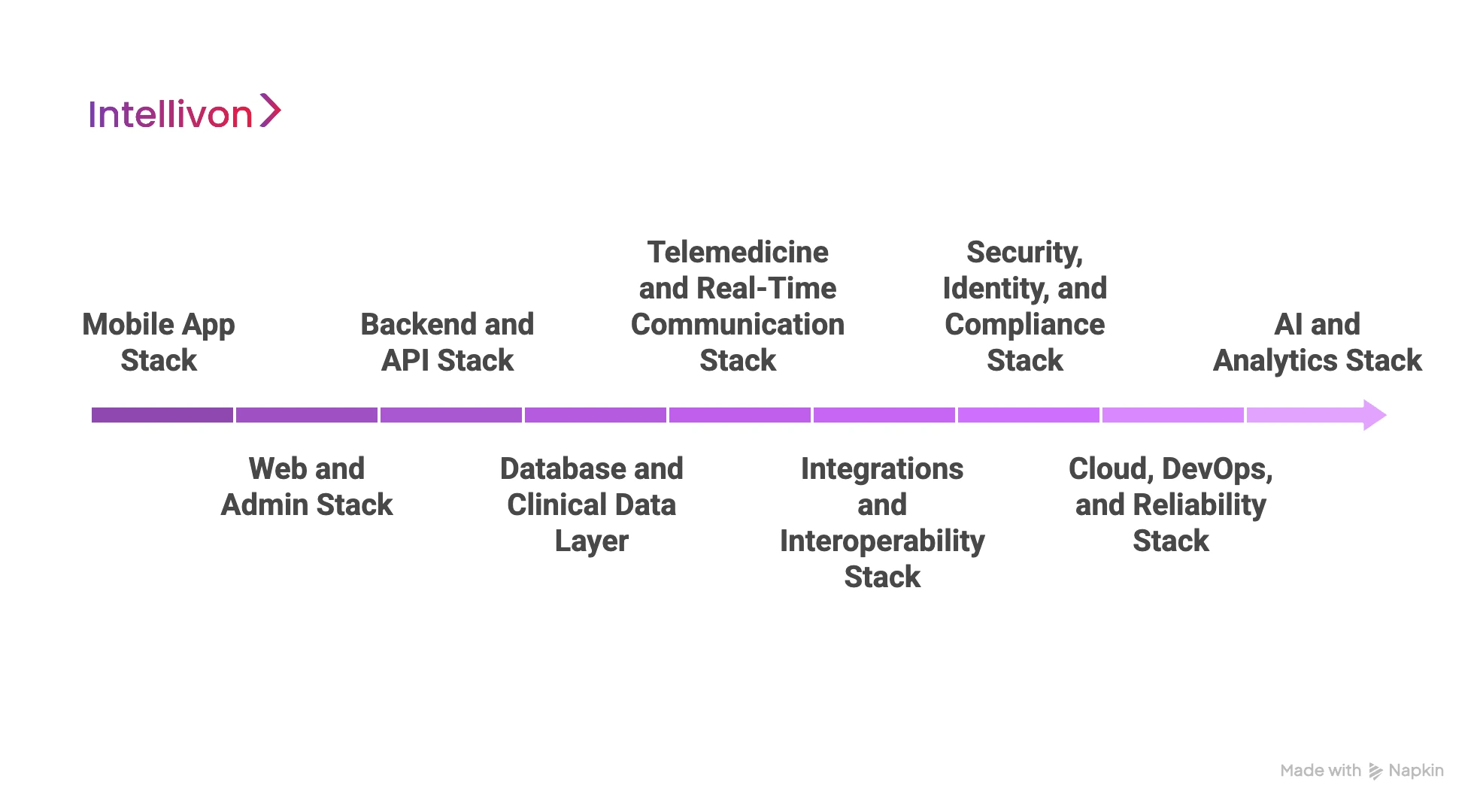
1. Mobile App Stack
This layer must support fast UI, secure sessions, and stable performance across devices. It also needs clean patterns for onboarding, consent, and follow-ups.
Common technologies:
- iOS: Swift, SwiftUI
- Android: Kotlin, Jetpack Compose
- Cross-platform: React Native, Flutter
2. Web and Admin Stack
Enterprises need web portals for care teams, admins, and operations. These dashboards manage scheduling, documentation, triage, and reporting.
Common technologies:
- Frontend: React, Next.js, Angular
- Admin UI frameworks: Material UI, Ant Design
- State and data: Redux, React Query
3. Backend and API Stack
The backend runs the care platform. It handles identity, scheduling, messaging, records, and integration workflows. Clean service boundaries matter as the scope expands.
Common technologies:
- APIs: Node.js (NestJS), Java (Spring Boot), Python (FastAPI), .NET
- Architecture: Microservices, modular monolith, event-driven services
- API patterns: REST, GraphQL
4. Database and Clinical Data Layer
Women’s health platforms store sensitive, longitudinal data. You need structured storage for records and flexible models for symptoms and tracking.
Common technologies:
- Relational: PostgreSQL, MySQL
- NoSQL: MongoDB, DynamoDB
- Time-series and events: TimescaleDB, Kafka topics, event stores
- Search: Elasticsearch, OpenSearch
5. Telemedicine and Real-Time Communication Stack
Video and messaging must work reliably under real-world network constraints. This layer also supports waiting rooms, session controls, and recording rules when needed.
Common technologies:
- Video and RTC: Twilio Video, Vonage (TokBox), Agora, WebRTC
- Messaging: Twilio Conversations, Sendbird, Firebase
- Notifications: APNs, FCM
6. Integrations and Interoperability Stack
Interoperability is where many platforms fail. You need stable connectors, message mapping, and error recovery that teams can operate.
Common technologies and standards:
- Standards: FHIR, HL7 v2, CCD, NCPDP (pharmacy)
- Integration engines: Mirth Connect (NextGen), Redox, MuleSoft
- APIs and messaging: REST, SFTP, Kafka, queues
7. Security, Identity, and Compliance Stack
Women’s health apps require stronger controls due to the sensitivity of data and consent requirements. Security must be built into every layer.
Common technologies:
- IAM: OAuth 2.0, OIDC, Auth0, Okta, AWS Cognito
- Encryption and keys: KMS (AWS/Azure/GCP), HashiCorp Vault
- Logging and audit: CloudWatch, ELK stack, Splunk
- Security testing: SAST/DAST tools, dependency scanning
8. Cloud, DevOps, and Reliability Stack
Enterprise leaders care about uptime, audit readiness, and predictable scaling. This layer ensures safe releases and stable operations.
Common technologies:
- Cloud: AWS, Azure, Google Cloud
- Containers: Docker, Kubernetes
- CI/CD: GitHub Actions, GitLab CI, Jenkins
- Infrastructure as code: Terraform, CloudFormation
- Observability: Prometheus, Grafana, OpenTelemetry
9. AI and Analytics Stack
AI adds value when tied to workflows like intake, triage, and trend analysis. Analytics should support both clinical and business KPIs.
Common technologies:
- ML frameworks: PyTorch, TensorFlow, scikit-learn
- MLOps: MLflow, SageMaker, Vertex AI, Azure ML
- Data pipelines: Airflow, dbt, Spark
- Warehousing: Snowflake, BigQuery, Redshift
- BI: Power BI, Tableau, Looker
A women’s health telemedicine app needs a stack built for trust, continuity, and scale. The best approach is to choose proven technologies that support compliance, interoperability, and long-term platform evolution. At Intellivon, we design tech stacks around your care model and enterprise constraints, so the platform performs under real operational load.
Conclusion
Women’s health telemedicine platforms are no longer experimental extensions of care. They are becoming core digital infrastructure for enterprises that want to deliver continuity, trust, and measurable outcomes at scale. Platforms like HerMD show what is possible when clinical depth, privacy, and operational discipline come together.
Building this kind of system requires a clear strategy, compliant architecture, and experience with real-world healthcare complexity. When done right, the platform becomes a growth enabler, not just a cost center.
At Intellivon, we build enterprise-grade women’s health telemedicine platforms designed for long-term impact. If you are planning to launch or scale one, we are ready to help you do it right.
Build A Women’s Health Telemedicine App With Intellivon
At Intellivon, we build women’s health telemedicine apps as enterprise care platforms, not consumer tools adapted from generic telehealth systems. Our platforms are designed to operate as secure, compliant digital care foundations that unify virtual care, longitudinal health data, clinical workflows, and enterprise integrations into one governed system.
Each solution is engineered for healthcare organizations delivering complex women’s health services across reproductive care, pregnancy, menopause, mental health, and preventive programs. Platforms are infrastructure-first, compliance-led, and built to support hybrid care models while delivering predictable operating costs, clinical consistency, and measurable ROI as patient volumes scale.
Why Partner With Intellivon?
- Platform architecture aligned with longitudinal women’s health workflows and sensitive data governance
- Deep interoperability expertise across EHRs, labs, pharmacies, identity systems, and care networks
- Compliance-by-design engineering supporting HIPAA, consent management, audit readiness, and role-based access
- AI-enabled care orchestration for intake intelligence, risk detection, and sustained patient engagement
- Enterprise delivery model with phased rollout, KPI-driven optimization, and long-term scalability
Talk to Intellivon’s healthcare platform architects to explore how a HerMD-style women’s health telemedicine app can be built to support growth, trust, and real-world care delivery at scale.
FAQs
Q1. What is a women’s health telemedicine app?
A1. A women’s health telemedicine app is a digital care platform designed to support women across reproductive health, pregnancy, menopause, mental health, and preventive care. Unlike generic telehealth tools, it enables longitudinal care, sensitive data handling, and coordinated clinical workflows across multiple life stages.
Q2. How much does it cost to build a women’s health telemedicine app?
A2. The cost typically ranges from $60,000 to $160,000 for an enterprise-ready Phase 1 platform. Final pricing depends on care scope, compliance depth, integrations with EHRs and pharmacies, and whether AI or remote monitoring features are included from the start.
Q3. What regulations apply to women’s health telemedicine platforms?
A3. Women’s health telemedicine platforms must comply with HIPAA and HITECH in the U.S., along with state-level telemedicine and licensure rules. Platforms serving international users may also need to meet GDPR requirements, especially around consent, auditability, and data minimization.
Q4. How does AI improve women’s health telemedicine apps?
A4. AI improves women’s health apps by supporting intake triage, analyzing longitudinal health patterns, assisting clinical decision-making, and improving patient engagement. When embedded into workflows, AI helps care teams act earlier while maintaining clinical oversight and trust.
Q5. How long does it take to build a women’s health telemedicine app?
A5. A focused MVP can be built in 12–16 weeks, while an enterprise-ready platform typically takes 4–6 months. Timelines vary based on compliance requirements, integration scope, and whether hybrid care or AI capabilities are included in the initial release.