Perimenopause affects a large and economically active population, yet it remains one of the most underdiagnosed and fragmented areas of modern healthcare. Symptoms often span physical, cognitive, and emotional domains, but care delivery is still scattered across episodic consultations, generic wellness tools, and delayed referrals. At the same time, enterprises are under growing pressure to support women’s health in a way that is clinically credible, legally sound, and reputationally safe.
Digital platforms like January have validated the need for specialized perimenopause support. What remains unresolved is how to scale such care responsibly within enterprise ecosystems that demand integration, compliance, and measurable outcomes.
This blog explores how enterprises can build perimenopause telehealth platforms that deliver lasting value. Grounded in Intellivon’s expertise in designing enterprise-grade AI healthcare solutions, it focuses on creating systems that support growth, resilience, and trust at scale.
Key Takeaways of the Perimenopause Platform Market
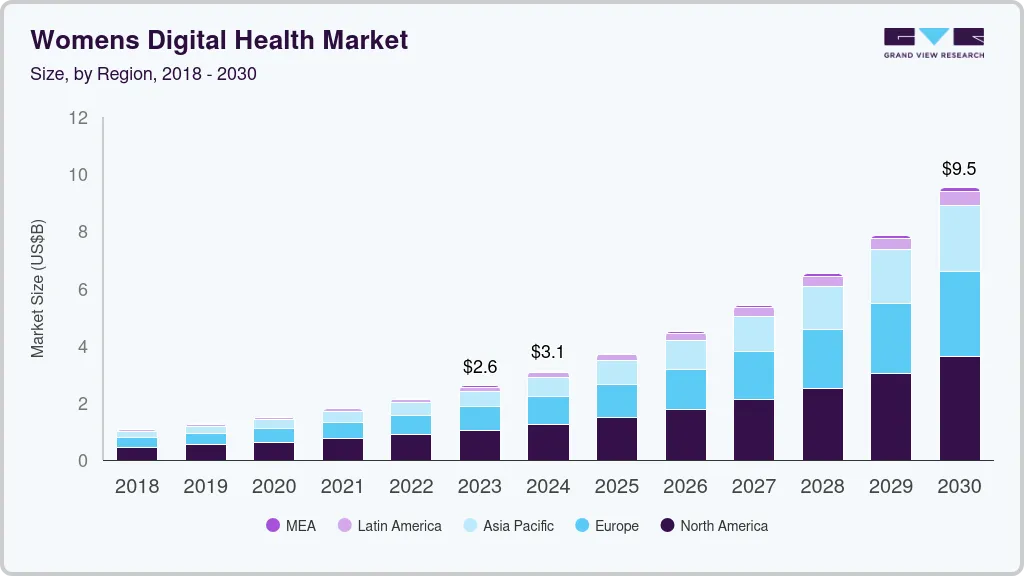
The women’s digital health market has entered a high-growth phase, scaling from roughly USD 2.6 billion in 2023 toward an estimated USD 9.53 billion by the end of the decade, with annual growth exceeding 20%.
Market Insights:
- The overall global menopause economy, including therapies, consumer products, and clinical services, is currently valued in the range of USD 19–21 billion across 2024–2025. Market projections indicate expansion to approximately USD 27–33 billion by 2032–2033, supported by steady annual growth of around 5–6 percent.
- Within the femtech landscape, menopause-focused solutions represent one of the fastest-accelerating segments. Some forecasts estimate menopause-centric femtech alone could approach USD 27.6 billion by 2030, driven by demographic shifts, including an estimated 1.3 billion women entering post-menopausal age by the end of the decade.
Women’s Digital Health and Femtech Ecosystem
- The women’s digital health market stood at roughly USD 2.6–3.1 billion during 2023–2024. Current projections suggest this category could scale to between USD 9.5 and 12.6 billion by 2030–2032, reflecting sustained annual growth close to 19–20 percent.
- Looking more broadly, the global femtech sector, encompassing all technology-led women’s health solutions, is valued at approximately USD 39.3 billion in 2024 and is expected to reach nearly USD 97.3 billion by 2030, representing a compound annual growth rate of about 16 percent.
Menopause and Perimenopause Digital Segments
- The menopause-focused femtech segment alone is estimated at around USD 3.0 billion in 2024. Analysts expect this segment to grow to approximately USD 7.45 billion by 2030, supported by a CAGR of roughly 16.2 percent.
- A narrower subset of menopause-related digital tools, such as hormone-balancing and symptom-management applications, is currently valued at about USD 1.3 billion in 2024, with strong year-over-year expansion anticipated.
Unmet Need and Adoption Signals
- Despite growing market value, menopause care remains significantly underserved. Industry commentary has described this gap as a “USD 150 billion blind spot,” noting that while the menopause market was valued at USD 15.4 billion in 2021 and is expected to reach USD 24.4 billion by 2030, nearly three-quarters of women who seek medical help still do not receive effective treatment.
- Independent evaluations of menopause-focused apps reveal a fragmented quality landscape. Among more than 400 menopause-related apps identified in one review, only about 20 met basic quality standards, and very few demonstrated any level of scientific or clinical validation.
Drivers Accelerating Perimenopause Platform
- Women’s digital health solutions overall are projected to grow from approximately USD 3.1–3.3 billion in 2024–2025 to nearly USD 10.1–10.8 billion by 2034–2035. Analysts frequently cite the rapid emergence of menopause and perimenopause platforms as a key contributor to this growth.
- Structural drivers include a growing population of midlife women in the workforce, increased openness around menopause-related health discussions, and rising employer interest in menopause benefits as part of broader women’s health, retention, and longevity strategies.
Implications For Perimenopause Telemedicine Platforms
- Market analysts and investors expect the global femtech sector to sustain growth of roughly 16% annually through 2030, with menopause, perimenopause, and longevity-focused solutions among the most attractive segments.
Adoption patterns further support this trajectory. Women consistently rank among the most active users of digital health and telemedicine services, positioning perimenopause platforms as a natural progression from earlier mHealth behaviors such as cycle tracking, fertility care, and digital mental health support.
What Is The Perimenopausal Telehealth Platform January?
January is a digital care platform built specifically for women navigating perimenopause and early menopause. Instead of treating symptoms in isolation, it focuses on ongoing care over time, where treatment evolves as symptoms change.
The platform combines virtual consultations with clinicians trained in menopause care, structured symptom tracking, and evidence-based treatment plans. As a result, women are not forced to restart their story at every visit. Care builds week by week, creating continuity that traditional telehealth often lacks.
Importantly, January does not position itself as a general wellness app. It operates closer to a specialty care model, using digital access to reduce wait times and improve consistency. However, clinical judgment remains central, with technology supporting monitoring and follow-up rather than replacing medical decision-making.
For enterprises, platforms like January signal a shift. Perimenopause care is moving from fragmented support toward structured, accountable digital healthcare delivery.
How does the platform work?
Perimenopause platforms work best when they guide women through a clear, repeatable care journey. Therefore, the workflow must feel structured, but still personal. It should also keep clinicians in control while reducing operational friction.
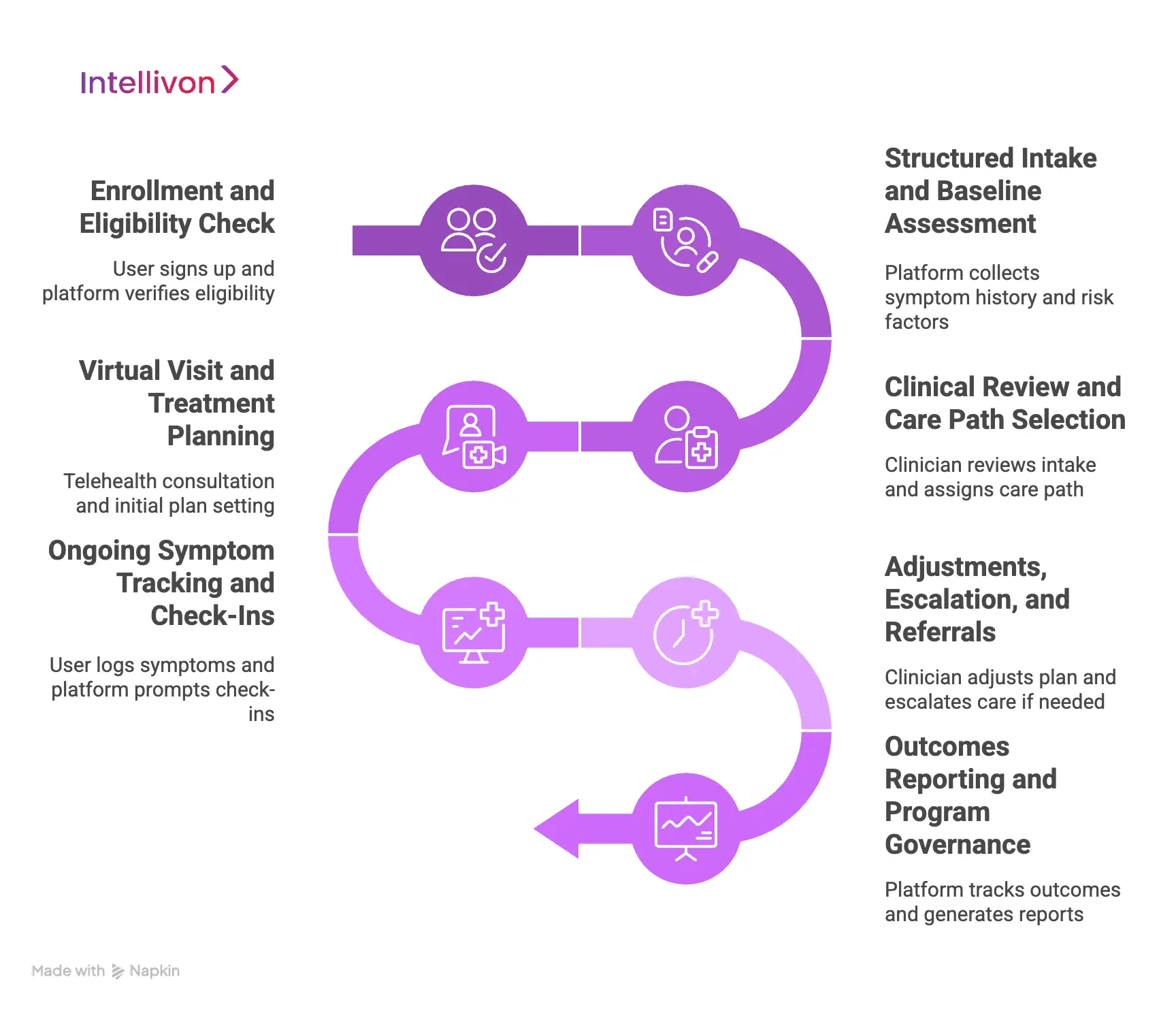
Step 1: Enrollment And Eligibility Check
The user signs up through an employer benefit, health plan, or direct access flow. In addition, the platform verifies eligibility, captures basic demographics, and confirms consent for sensitive health data.
Step 2: Structured Intake And Baseline Assessment
Next, the platform collects symptom history, cycle patterns, medications, and relevant risk factors. It also uses standardized questionnaires to create a baseline that clinicians can trust.
Step 3: Clinical Review And Care Path Selection
Then, a clinician reviews the intake and assigns a care path. For example, some users need lifestyle-first support, while others require hormone therapy evaluation or comorbidity screening.
Step 4: Virtual Visit And Treatment Planning
After that, the user attends a telehealth consultation. The clinician confirms key signals, rules out red flags, and sets an initial plan. This plan may include education, labs, prescriptions, or follow-up scheduling.
Step 5: Ongoing Symptom Tracking And Check-Ins
Over time, the user logs symptoms and adherence signals in short weekly flows. Meanwhile, the platform prompts check-ins and flags worsening patterns that require clinician attention.
Step 6: Adjustments, Escalation, And Referrals
If symptoms persist, the clinician adjusts the plan. Additionally, the platform supports escalation to in-person care, specialty referrals, or additional testing when needed.
Step 7: Outcomes Reporting And Program Governance
Finally, the platform tracks outcomes, engagement, and care quality. For enterprises, it also generates governance-ready reporting while protecting individual privacy.
In short, the platform works as a longitudinal care loop. It starts with structured intake, then moves into clinician-led planning, and finally relies on regular tracking and adjustments to sustain results.
Why Perimenopause Is Harder To Platform Than Other Women’s Health Use Cases
Perimenopause is harder to platform because it involves long-term symptom variability, diagnostic uncertainty, and heightened clinical and enterprise risk that cannot be handled through episodic or rule-based digital care.
This complexity forces enterprises to think differently about how digital care should be designed, governed, and scaled.
1. Symptoms Rarely Fit Neat Diagnostic Buckets
Perimenopause symptoms often look indistinguishable from mental health challenges, thyroid disorders, chronic stress, or burnout. Fatigue, mood changes, sleep disruption, and cognitive fog are common, yet none of them point clearly to one cause. Because of this, many women cycle through providers without resolution.
From a platform perspective, this makes simple symptom checklists insufficient. Effective systems must support pattern recognition across weeks and months, not just capture isolated inputs. Without this longitudinal view, digital care risks reinforcing the same fragmentation women already experience offline.
2. Care Requires Ongoing Adjustment
Most women’s health use cases can be addressed through defined stages. Perimenopause cannot. Treatment plans often require gradual adjustment, careful monitoring, and frequent reassessment. What works for a patient one month may stop working the next.
This means platforms must be built for continuity by default. Follow-ups, symptom tracking, and iterative care planning are not enhancements. They are foundational capabilities. Telehealth models that prioritize speed over persistence tend to break down in this category.
3. Trust Plays A Larger Role
Many women enter perimenopause care after years of being dismissed or misdiagnosed. As a result, trust becomes a central determinant of engagement. If the platform feels generic, overly automated, or detached from clinical judgment, users disengage quickly.
Therefore, credibility matters more here than in many other digital health programs. Clinical oversight, clear explanations, and visible accountability are essential to sustaining participation over time.
4. Enterprise Risk And Visibility Are Higher
Perimenopause platforms handle highly sensitive health data and influence nuanced care decisions. In addition, the social and regulatory context around women’s health continues to evolve. Together, these factors raise the stakes for enterprises.
Poorly governed platforms can introduce clinical risk, data exposure, or reputational fallout. This makes perimenopause care a category where enterprise-grade architecture, compliance, and oversight are non-negotiable.
Perimenopause is harder to pinpoint because it resists simplification. Successful platforms recognize it as a long-term, high-trust care challenge rather than a transactional health service.
What Platforms Like January Get Right
Perimenopause platforms fail when they try to simplify a complex transition. Platforms like January work because they acknowledge that complexity and design around it.
Instead of forcing perimenopause into generic telehealth molds, they reshape care delivery to fit how symptoms evolve and how trust is built over time. This approach offers several lessons for enterprises evaluating similar platforms.

1. They Design For Longitudinal Care
Rather than centering the experience on isolated visits, platforms like January are built around continuity. Care plans evolve across months, not appointments. Symptom tracking feeds directly into follow-up conversations, allowing clinicians to see trends rather than fragments.
As a result, patients are not required to re-explain their history at every interaction. This continuity reduces friction, improves care quality, and supports more informed clinical decisions.
2. They Keep Clinical Judgment At The Core
Automation plays a supporting role, not a leading one. Platforms like January rely on clinicians to interpret symptoms, assess risk, and guide treatment decisions. Technology is used to organize information and surface patterns, not to replace medical expertise.
This balance matters. In a category defined by ambiguity, over-automation erodes trust quickly. By keeping humans clearly in charge, these platforms maintain legitimacy with both patients and enterprises.
3. They Treat Trust As A Platform Feature
Trust is not assumed, but it is designed. Clear care pathways, consistent clinical touchpoints, and transparent communication all reinforce credibility. Users understand who is responsible for their care and how decisions are made.
Because many women arrive after years of dismissal, this emphasis on trust directly influences engagement and retention.
4. They Avoid Isolated Care Silos
Platforms like January do not operate as standalone wellness tools. They are designed to connect with labs, pharmacies, and broader care ecosystems. This allows treatment plans to move beyond advice and into actionable care.
For enterprises, this reduces fragmentation. It also makes digital care easier to align with existing healthcare infrastructure.
5. They Scale Without Diluting Care Quality
Growth does not come at the expense of rigor. Standardized workflows, clear escalation paths, and structured documentation allow platforms like January to scale while preserving clinical accountability.
This balance is essential. Platforms that grow without governance often struggle once enterprise scrutiny increases.
Platforms like January succeed because they respect the realities of perimenopause care. They prioritize continuity, clinical judgment, and trust while remaining operationally scalable.
Perimenopausal Telemedicine Apps Increased Weekly Engagement By 95%
Perimenopause care depends on continuity. Unlike episodic conditions, symptoms shift week by week. Therefore, digital platforms that maintain regular engagement create a feedback loop between awareness, care adjustment, and trust.
In practice, real-world evidence from perimenopause-focused digital programs shows that when women stay engaged, 95% outcomes improve. For enterprises, this distinction matters. Engagement is not a soft metric. Instead, it signals clinical impact, program durability, and long-term ROI.
What Women Actually Report At Baseline
At baseline, the most frequently logged symptoms reflected everyday functioning. These were not edge cases or secondary complaints. Instead, they directly affected work performance and daily life.
Specifically:
- Low energy was reported by 65 percent of users
- Low mood appeared in 59 percent
- Sleep problems affected 58 percent
- Stress or anxiety was also reported by 58 percent
Why Engagement Duration Changes Outcomes
The data shows a consistent relationship between engagement duration and symptom improvement. Compared with users who engaged for only two weeks, those who remained active longer experienced greater benefits.
For example:
- Four weeks of engagement aligned with an estimated reduction of −2.7
- Six weeks showed further improvement at −3.3
- Nine weeks delivered the strongest effect, with a reduction of −4.0
Importantly, confidence intervals remained statistically meaningful at higher engagement levels. Therefore, these improvements were not short-term novelty effects. Instead, they reflected the impact of sustained participation.
What This Means For Platform Design
Engagement does not persist by chance. Instead, it emerges from platforms built around longitudinal care rather than isolated interactions.
In effective perimenopause telemedicine platforms, this usually includes:
- Simple symptom logging that adapts over time
- Clear feedback between logged data and care decisions
- Regular clinical touchpoints that reinforce trust
- Low-friction workflows that fit into daily routines
From an enterprise standpoint, this reframes the problem. Engagement becomes something to engineer and govern. It is no longer a behavioral afterthought.
Why Enterprises Should Care About Engagement Metrics
For large organizations, engagement is not a vanity KPI. Instead, it signals whether a perimenopause program will deliver results or quietly fade after launch.
Higher engagement supports:
- Better symptom control and fewer escalations
- Stronger confidence in digital-first care delivery
- Clear justification for sustained investment
Without this signal, even well-funded programs struggle to scale. Perimenopause telemedicine platforms succeed when continuity is prioritized. The evidence says weekly engagement over time drives meaningful symptom improvement.
Therefore, for enterprises, the key question is not whether users will sign up. It is whether the platform is designed to keep them engaged long enough to create value. Platforms that solve for this become durable care assets rather than short-term benefits experiments.
Core Architecture Of A Perimenopause Telehealth Platform
Perimenopause care cannot sit on lightweight telehealth stacks. The platform must operate as a regulated healthcare infrastructure, capable of evolving with patients over the years while meeting enterprise expectations around security, uptime, and governance. Architecture decisions made early directly determine whether the platform can scale or quietly break under real-world complexity.
Below is a practical, enterprise-ready architecture model that supports perimenopause care end-to-end.
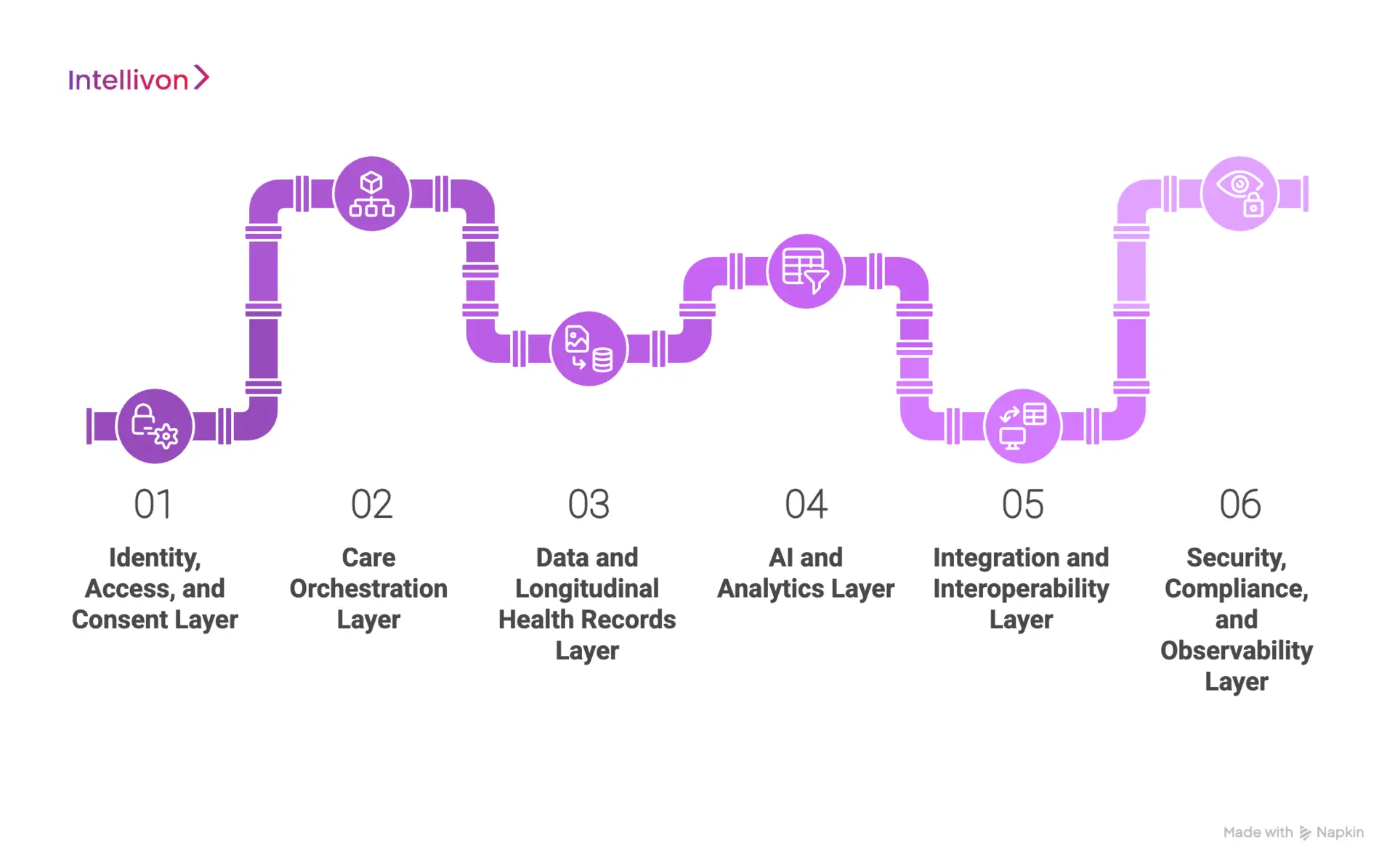
1. Identity, Access, And Consent Layer
This layer controls who can access the platform and under what conditions. It also governs consent for highly sensitive reproductive and hormonal health data.
Core responsibilities include secure user authentication, role-based access for clinicians and care teams, and fine-grained consent management that can be updated or revoked over time.
Common technologies used
- OAuth 2.0 and OpenID Connect for authentication
- Enterprise IAM platforms such as Okta or Azure Active Directory
- Consent management services built on secure policy engines
- Encryption standards like AES-256 and TLS 1.2+
This layer protects enterprises from data exposure and compliance risk from day one.
2. Care Orchestration Layer
This layer defines how care actually happens. It manages intake, assessments, follow-ups, escalations, and documentation across the full perimenopause journey.
Workflows must support iteration. Care plans change. Symptoms fluctuate. Clinicians need visibility across time, not isolated visits.
Common technologies used
- Workflow engines such as Camunda or Temporal
- Clinical rules engines for care path guidance
- Secure documentation services with audit logging
- Microservices built using Spring Boot or Node.js
Without strong orchestration, perimenopause platforms revert to fragmented care.
3. Data And Longitudinal Health Records Layer
Perimenopause care depends on trend visibility. This layer stores symptom logs, treatment history, lab results, and clinician notes in a structure optimized for time-based analysis. Data must remain queryable, auditable, and interoperable.
Common technologies used
- Relational databases like PostgreSQL for structured records
- Time-series databases such as InfluxDB for symptom tracking
- Object storage, like Amazon S3, for documents and reports
- FHIR-based data models for interoperability
This layer enables continuity, clinical insight, and reporting.
4. AI And Analytics Layer
AI plays a supporting role in perimenopause platforms. It identifies patterns, flags risk signals, and assists clinicians without automating medical decisions. Models must remain explainable and governable.
Common technologies used
- Python-based ML stacks using TensorFlow or PyTorch
- Feature stores for longitudinal signal management
- MLflow for model versioning and monitoring
- Analytics platforms such as Apache Spark or Snowflake
This layer turns raw data into actionable insight while keeping humans in control.
5. Integration And Interoperability Layer
Perimenopause platforms cannot operate in isolation. This layer connects the platform to EHRs, labs, pharmacies, employer systems, and analytics tools. Clean integration reduces manual work and operational risk.
Common technologies used
- HL7 and FHIR APIs for clinical interoperability
- API gateways like Kong or AWS API Gateway
- Secure messaging and event streaming with Kafka
- ETL pipelines for reporting and analytics
Integration is what makes digital care usable at enterprise scale.
6. Security, Compliance, And Observability Layer
This layer ensures the platform remains secure, compliant, and operationally visible as usage grows. It supports audits, incident response, and continuous improvement.
Common technologies used
- SIEM tools such as Splunk or Azure Sentinel
- Continuous monitoring with Prometheus and Grafana
- Compliance automation tools for HIPAA and GDPR readiness
- Infrastructure-as-code using Terraform
Enterprises rely on this layer to maintain trust and control.
A perimenopause telehealth platform succeeds when architecture matches care reality. Each layer must support long-term engagement, clinical judgment, and enterprise governance. When designed correctly, the platform becomes a durable healthcare asset rather than a fragile digital experiment.
How AI Works In A Perimenopause Telehealth Platform
AI plays a careful, supporting role in perimenopause care. The goal is not automation for speed, but intelligence for clarity. Because symptoms evolve gradually and vary widely, AI helps clinicians make sense of change over time while keeping decision-making firmly in human hands.
When designed correctly, AI reduces cognitive load for care teams and improves continuity for patients. Below is how this works in practice.
1. AI-Assisted Intake
AI helps organize complex intake data into a usable baseline. It groups symptoms, flags risk factors, and highlights patterns that may otherwise be missed during first consultations.
This allows clinicians to focus on interpretation rather than data cleanup. As a result, early care decisions are better informed without adding clinical burden.
2. Longitudinal Pattern Detection
Over time, AI models track symptom frequency, severity, and co-occurrence. Rather than reacting to single data points, the platform surfaces trends that emerge across weeks or months.
For example, AI can detect whether fatigue correlates with sleep disruption or treatment changes. Therefore, clinicians gain a clearer picture of what is driving symptom progression.
3. Clinical Attention Prioritization
AI helps identify users who may need closer review. Worsening symptoms, adherence drops, or unusual patterns can trigger alerts for care teams.
This prioritization ensures clinical time is directed where it matters most. Importantly, AI flags do not dictate care. They simply guide attention.
4. Decision Support, Not Decision Automation
AI supports clinicians with summaries, comparisons, and contextual insights. It does not generate diagnoses or prescribe treatments.
This distinction is critical. In perimenopause care, over-automation can undermine trust. AI works best when it clarifies options rather than replacing judgment.
5. Governance And Explainability
Enterprise platforms require visibility into how AI operates. Models must be explainable, auditable, and monitored for bias across age, ethnicity, and comorbidities.
Regular reviews and clear governance processes ensure AI remains safe as the platform scales.
AI strengthens perimenopause telehealth when it acts as an intelligence layer, not a control system. By supporting pattern recognition, prioritization, and continuity, AI helps care teams deliver better outcomes while preserving clinical authority and enterprise trust.
Integrating Perimenopause Telehealth Into Healthcare Ecosystems
Perimenopause care cannot operate in isolation. When platforms sit outside existing healthcare ecosystems, they create fragmented records, manual work, and clinical blind spots. For enterprises, this fragmentation increases risk and limits long-term value.
Successful platforms are designed to connect seamlessly across the healthcare stack. Integration is not a technical afterthought. It is a core requirement.
1. Connecting With EHR And Clinical Systems
Perimenopause telehealth must align with existing clinical records. Clinicians need access to longitudinal context, not separate data silos.
When platforms integrate with EHR systems, symptom trends, treatment updates, and care notes can flow back into the primary record. As a result, digital care complements in-person services rather than competing with them.
This continuity supports better clinical decisions and reduces duplication.
2. Pharmacy And Lab Integration
Treatment often involves prescriptions, labs, and follow-up testing. Without integration, care teams rely on manual coordination.
Integrated pharmacy workflows allow prescriptions to be issued, tracked, and adjusted within the same care loop. Lab integrations enable test ordering and result ingestion without breaking continuity.
Therefore, care becomes actionable rather than advisory.
3. Employer And Benefits System Alignment
In enterprise settings, access is often governed by benefits eligibility. Platforms must integrate with employer and payer systems to manage enrollment, coverage rules, and reporting.
This alignment ensures that only eligible users access services while protecting individual health privacy. It also enables aggregate reporting without exposing personal data.
For enterprises, this creates operational clarity.
4. Care Escalation And Referral Pathways
Not all perimenopause care can remain virtual. Some cases require in-person evaluation or specialty referral.
Integrated platforms support smooth escalation. Care teams can route patients to appropriate services without losing context or documentation. This reduces friction during handoffs and preserves accountability.
5. Data Governance And Interoperability Standards
Integration must follow healthcare standards. Secure APIs, standardized data models, and audit-ready logs are essential.
When interoperability is handled correctly, platforms remain flexible as ecosystems evolve. New partners can be added without rework.
Integration determines whether perimenopause telehealth becomes a trusted care extension or a disconnected add-on. Platforms that connect cleanly across healthcare ecosystems deliver continuity, reduce risk, and support enterprise-scale adoption.
How Intellivon Builds Enterprise-Grade Perimenopause Telehealth Platforms
Building a perimenopause telehealth platform that enterprises can trust requires more than strong engineering. It requires a disciplined build approach that accounts for clinical ambiguity, sensitive data, and enterprise operating realities. At Intellivon, platforms are developed through a clearly defined, eight-step process designed for scale, scrutiny, and longevity.
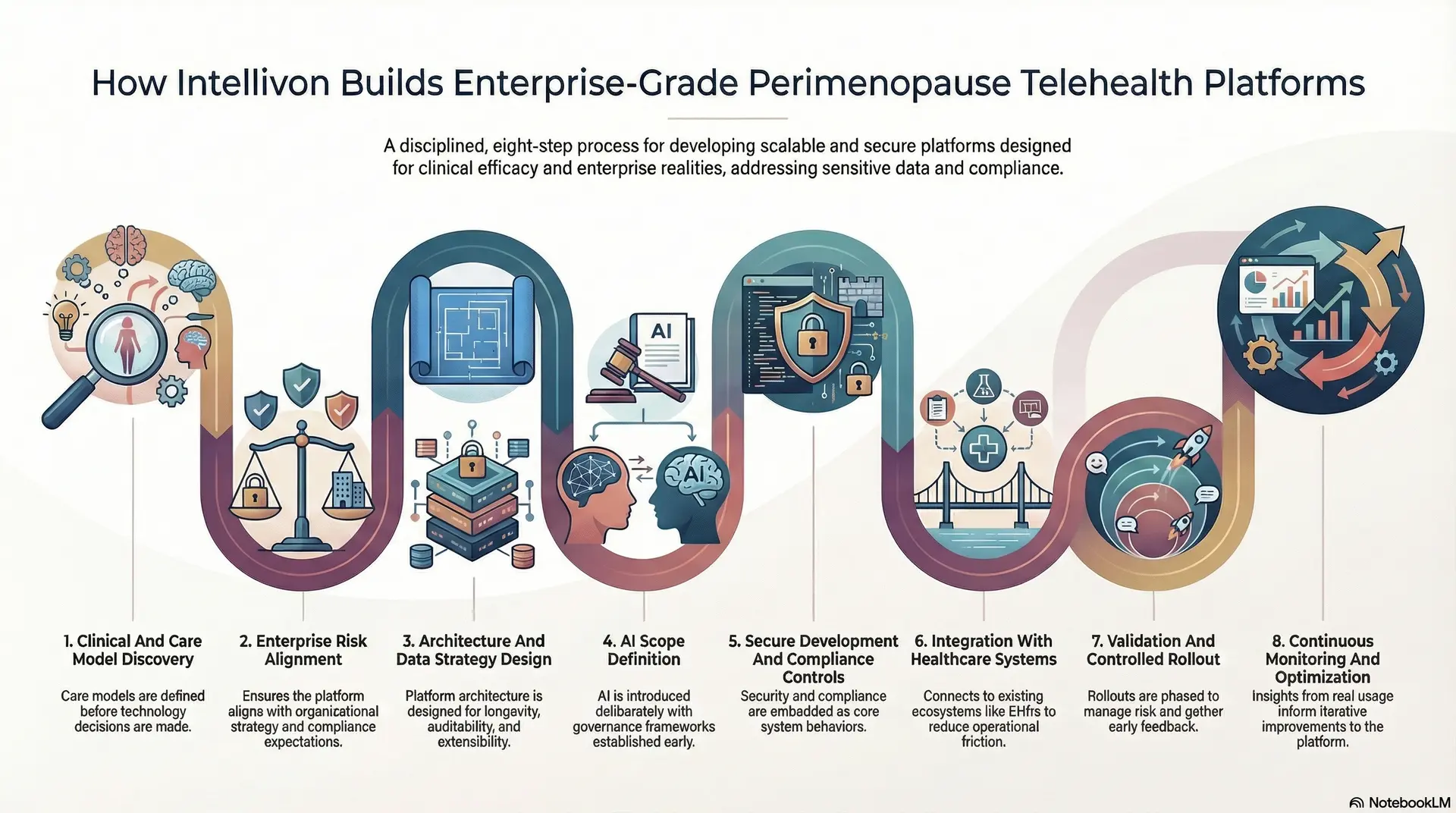
Step 1: Clinical And Care Model Discovery
The process begins with understanding how perimenopause care actually unfolds over time. This includes mapping symptom variability, escalation thresholds, follow-up cadence, and clinician responsibilities.
The goal at this stage is clarity. Care models are defined before technology decisions are made, ensuring the platform supports real clinical workflows rather than forcing artificial ones.
Step 2: Enterprise Risk Alignment
Next, enterprise-specific constraints are addressed. These include regulatory exposure, workforce demographics, benefits structure, and reputational considerations.
This step ensures the platform aligns with organizational strategy while accounting for internal approval processes, legal review, and compliance expectations.
Step 3: Architecture And Data Strategy Design
Once care and enterprise requirements are clear, platform architecture is designed for longevity. This includes decisions around modular services, data separation, multi-tenancy, and interoperability.
Special attention is given to longitudinal data storage, auditability, and future extensibility, as perimenopause care often spans years.
Step 4: AI Scope Definition
AI is introduced deliberately and with boundaries. This step defines where AI adds value, such as intake structuring or trend detection, and where it must remain advisory.
Governance frameworks are established early. Model explainability, monitoring, and bias controls are defined before deployment, not after.
Step 5: Secure Development And Compliance Controls
With architecture and governance in place, secure development begins. Identity management, access controls, encryption, and audit logging are embedded throughout the platform.
Compliance requirements such as HIPAA and regional data regulations are addressed as part of core system behavior, not external checklists.
Step 6: Integration With Healthcare Systems
The platform is then connected to existing ecosystems. This includes EHRs, labs, pharmacies, and employer or payer systems where applicable.
Integration ensures perimenopause care does not exist in isolation and reduces operational friction across teams and vendors.
Step 7: Validation And Controlled Rollout
Before broad deployment, the platform undergoes clinical validation, workflow testing, and security review.
Rollouts are phased to manage risk and gather early feedback. This approach allows refinements without disrupting care delivery or enterprise operations.
Step 8: Continuous Monitoring And Optimization
After launch, the platform is actively monitored. Engagement trends, care outcomes, and operational signals are reviewed regularly.
Insights from real usage inform iterative improvements, ensuring the platform evolves with patient needs, clinical practice, and enterprise priorities.
Enterprise-grade perimenopause platforms are built through discipline, not shortcuts. By following a structured, eight-step approach, Intellivon helps organizations move from concept to scalable care infrastructure that stands up to clinical, operational, and executive scrutiny.
Cost of Developing A Perimenopause Telehealth Platform
Building a perimenopause telehealth platform does not require a single, oversized investment at the outset. Most enterprises begin with a focused foundation that supports longitudinal care, clinical oversight, sensitive data governance, and safe escalation pathways. From there, the platform expands as patient volumes increase and care programs mature.
At Intellivon, we structure costs around platform maturity rather than feature accumulation. This phased approach allows enterprises to launch faster, validate outcomes early, and scale perimenopause care with controlled clinical, operational, and financial risk.
Estimated Cost Breakdown (USD 90,000–240,000)
| Cost Component | What It Covers | Estimated Range |
| Discovery & Perimenopause Care Model Design | Symptom frameworks, care pathways, escalation logic, clinician roles, outcome KPIs, and platform architecture aligned to perimenopause care | $12,000 – $22,000 |
| Longitudinal Enrollment & Intake Workflows | Eligibility rules, structured intake, baseline assessments, ongoing symptom tracking, and continuity logic | $14,000 – $30,000 |
| Care Pathway Orchestration Engine | Protocol-driven journeys, follow-ups, treatment adjustments, escalation thresholds, and clinician override controls | $14,000 – $32,000 |
| AI-Supported Pattern Detection & Risk Flagging | Intake structuring, longitudinal trend analysis, symptom correlation, and clinician-facing alerts with governance controls | $12,000 – $28,000 |
| EHR, Lab, And Pharmacy Integrations | HL7/FHIR interfaces, lab result ingestion, prescription workflows, and safe care handoffs | $16,000 – $40,000 |
| Identity, Consent, And Access Governance | Role-based access, SSO options, consent lifecycle management, and audit-ready access controls | $8,000 – $18,000 |
| Compliance And Security Controls | HIPAA safeguards, encryption, secure logging, AI traceability, and clinical audit trails | $8,000 – $16,000 |
| Analytics And Outcomes Reporting | Longitudinal symptom trends, engagement metrics, care outcomes, and executive-level dashboards | $6,000 – $16,000 |
| Testing, Pilot, And Stabilization | QA, clinical workflow testing, phased rollout, clinician feedback loops, and platform tuning | $6,000 – $18,000 |
Typical MVP Range: $90,000 – $140,000
Enterprise-Ready Phase 1 Platform: $160,000 – $240,000
Final costs vary based on integration depth, AI governance requirements, and the level of clinical oversight required from day one.
Factors That Influence The Cost Of Perimenopause Telehealth Platforms
Cost in perimenopause platforms is driven by clinical complexity and governance, not screen count. Understanding these factors early helps enterprises avoid rework and budget overruns later.
1. Depth Of Perimenopause Care Design
Managing basic education and check-ins costs less than supporting multi-symptom journeys with hormonal evaluation, escalation tiers, and clinician review. Greater rigor increases cost but significantly reduces risk at scale.
2. Integration With Existing Care Ecosystems
Light integration may only surface patient context. Deeper integration includes prescriptions, labs, referrals, and documentation sync. While more expensive, this prevents fragmented care and operational inefficiency.
3. AI Governance And Clinical Oversight
Simple analytics are inexpensive. Costs rise when enterprises require explainable AI outputs, bias monitoring, confidence thresholds, and enforced human review. These controls are essential in regulated care environments.
4. Identity And Multi-Role Access
Single-user platforms are cheaper. Enterprise deployments require patients, clinicians, care coordinators, and administrators, along with consent that persists, renews, and revokes over time.
5. Analytics And Executive Visibility
Basic reporting explains what happened. Enterprise analytics explains why outcomes changed and where to intervene next. This depth increases cost but enables defensible ROI conversations.
How Enterprises Stay Within Budget
Budget discipline comes from phased delivery. Enterprises typically start with intake, longitudinal care pathways, clinician oversight, core integrations, and compliance controls. Outcomes are validated through a focused rollout before expanding automation or additional services.
Equally important, KPIs should be defined early. Most cost overruns occur when the scope expands mid-build. A strong foundation allows perimenopause telehealth platforms to scale with confidence rather than correction.
Conclusion
Perimenopause is no longer a fringe healthcare concern. It sits at the intersection of clinical complexity, workforce wellbeing, and enterprise responsibility. Platforms that treat it as a lightweight telehealth feature rarely survive real-world use. Those that succeed are designed for continuity, governance, and long-term care delivery.
For enterprises, the opportunity extends beyond cost control. Well-designed perimenopause platforms improve engagement, stabilize outcomes, and strengthen trust with a population that has historically been underserved. They also reduce fragmentation across care systems by integrating clinical judgment, data, and technology into a single operating model.
Build A Perimenopause Telehealth Platform With Intellivon
At Intellivon, we build perimenopause telehealth platforms as enterprise operating systems, not standalone virtual care tools layered onto existing workflows. Our platforms are designed to govern how women enter longitudinal care, how symptoms are monitored and adjusted over time, and how accountability is maintained across clinicians, AI-assisted workflows, and enterprise infrastructure.
Each solution is engineered for healthcare organizations operating at scale. Platforms are infrastructure-first, compliance-led, and purpose-built to support perimenopause as a long-term care journey rather than a series of isolated consultations. As programs expand across populations, regions, and benefit models, clinical oversight, data integrity, and operational control remain intact.
Why Partner With Intellivon?
- Perimenopause-first platform architecture aligned with longitudinal care, clinical continuity, and accountable outcomes
- Deep interoperability expertise across EHRs, labs, pharmacies, identity systems, and enterprise benefits platforms
- Compliance-by-design delivery supporting HIPAA, audit readiness, role-based access, and governed AI usage
- AI-assisted care orchestration that enhances pattern recognition and prioritization without replacing clinical judgment
- Enterprise delivery model with phased rollout, KPI-led validation, and controlled scale across care programs
Talk to Intellivon’s healthcare platform architects to explore how an enterprise-grade perimenopause telehealth platform can integrate into your existing ecosystem, protect sensitive health data, strengthen clinical trust, and scale safely without introducing operational or regulatory risk.
FAQs
Q1. What is a perimenopause telehealth platform?
A1. A perimenopause telehealth platform is a digital care system designed to support women through the perimenopausal transition over time. Unlike general telehealth, it focuses on longitudinal symptom tracking, clinician-led care, and ongoing treatment adjustments. These platforms combine virtual consultations, structured intake, symptom monitoring, and follow-ups.
Q2. How is perimenopause telehealth different from general women’s health platforms?
A2. Perimenopause platforms are built for clinical ambiguity and long care timelines. Symptoms evolve gradually and overlap with mental health, sleep, and metabolic issues. As a result, care requires continuity, escalation logic, and clinician judgment. General women’s health platforms often rely on episodic visits or static content.
Q3. Can perimenopause telehealth platforms integrate with existing healthcare systems?
A3. Yes. Enterprise-grade platforms are designed to integrate with EHRs, labs, pharmacies, and employer benefits systems. Integration ensures care does not exist in isolation and reduces manual coordination. It also allows symptom trends and treatment updates to flow into longitudinal health records. This continuity is critical for enterprise adoption and clinical accountability.
Q4. How does AI support perimenopause telemedicine without increasing clinical risk?
A4. AI is used as a decision-support layer, not an automation engine. It helps structure intake data, detect symptom patterns over time, and flag cases that need clinician review. Importantly, AI does not diagnose or prescribe. Human oversight remains central. This approach improves efficiency while preserving trust and regulatory safety.
Q5. How long does it take to build a perimenopause telehealth platform?
A5. Most enterprises launch a focused Phase 1 platform within 4–6 months. This typically includes intake, longitudinal care workflows, clinician oversight, core integrations, and compliance controls. Additional automation and analytics are layered in over time.





