Most healthcare platforms are built around features, but chronic care platforms need to be built around systems. In practice, when Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) are deployed independently, organizations inherit complexity that compounds with scale. As a result, teams spend time coordinating tools instead of improving care. Over time, leadership loses a clear view of performance across the care continuum.
In contrast, an RPM + CCM hybrid system approaches the problem differently. It treats monitoring, care coordination, compliance, and billing as interconnected parts of a single operating environment. In real-world deployments, HealthSnap has shown that this approach enables chronic care programs to grow without losing control. However, building such a system requires architectural discipline, regulatory awareness, and a clear understanding of how care is delivered over time.
Based on our experience, at Intellivon, we have built and scaled chronic care platforms where RPM and CCM are delivered together as part of one governed system. This blog draws directly from that experience to explain how an RPM + CCM hybrid system like HealthSnap is built, step by step, from foundational design decisions to enterprise-scale execution.
Key Takeaways Of The RPM + CCM Hybrid System Market
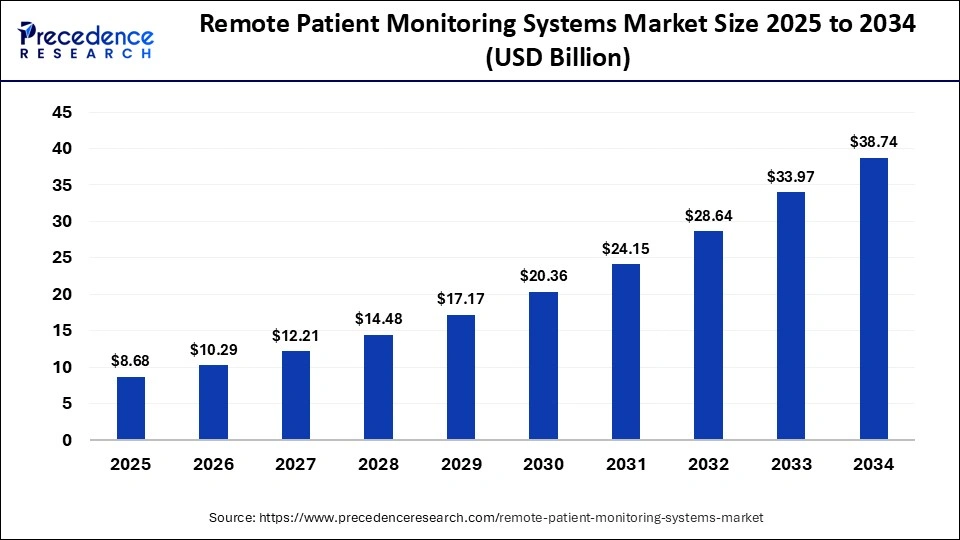
Remote patient monitoring has moved into a high-growth phase. The global market, valued at USD 8.68 billion in 2024, is projected to cross USD 10 billion in 2025 and expand to roughly USD 38.74 billion by 2034, driven by sustained annual growth of around 18 %.
Market Insights:
- CCM market growth: CCM reached $5.7B in 2024 and is projected to hit $12.1B by 2030 at a 13.2% CAGR, with software segments scaling toward $37.2B by 2032.
- Hybrid adoption surge: RPM claims grew 29%, and CCM claims 23% between 2022 and 2023, driven by expansion into underutilized Medicare populations and concurrent billing models.
- Chronic disease impact: Cardiology leads RPM adoption as cardiovascular disease, diabetes, and hypertension drive nearly 90% of total U.S. healthcare spending.
- Reimbursement momentum: CMS RPM codes (99453–99458) and CCM codes (starting 99490) support $50–$100 per patient per month, with RPM usage up 10× since 2019.
- Technology and regional trends: AI triage, cellular devices, and FHIR/HL7 interoperability are accelerating growth, with Asia-Pacific leading CAGR and North America holding 40% of global RPM share.
- Hybrid platform leaders: HealthSnap leads with 80+ EHR integrations and major health system partnerships, alongside platforms such as Optimize Health, Cadence, Accuhealth, Vivify, Prevounce, and Tenovi.
- Enterprise ROI potential: Hybrid RPM + CCM programs reduce readmissions by 20–30%; with only ~4% CCM utilization today, a 1,000-patient program at 75% efficiency can unlock $2–3M annually.
Taken together, these trends point to a clear shift in how chronic care platforms are being evaluated. Market growth, reimbursement momentum, and rising disease burden are no longer independent signals. They are converging into a strong case for hybrid RPM + CCM systems that can scale clinically, operate efficiently, and remain audit-ready as volumes increase.
What Defines an RPM + CCM “Hybrid System”?
An RPM + CCM hybrid system is defined by how monitoring and care management operate together inside a single, governed platform. It is not a bundle of services. It is an operating model designed for scale.
At its core, the system combines continuous physiologic monitoring with structured, longitudinal care workflows. RPM supplies real-time signals such as vitals, trends, and risk flags. CCM provides the framework to act on those signals through care plans, follow-ups, medication management, and coordinated clinical time.
However, what makes the system “hybrid” is not shared billing or blended compliance. Those remain separate by design. Instead, the hybrid nature comes from shared infrastructure. Patient identity, data pipelines, task routing, and clinical dashboards are unified, so care teams work from one environment.
As a result, every data point has a defined path to action. Monitoring does not sit idle, and care management is not delayed. Together, they create a repeatable, accountable system for chronic care delivery at enterprise scale.
Understanding Remote Patient Monitoring (RPM) Systems
Remote Patient Monitoring systems collect ongoing physiological data such as blood pressure, glucose, and weight from patients outside clinical settings.
In practice, a cardiac care program may use connected blood pressure devices to detect early deterioration, allowing care teams to intervene days before a hospitalization would otherwise occur.
Understanding Chronic Care Management (CCM) Systems
Chronic Care Management systems support ongoing coordination for patients with multiple long-term conditions. They structure care plans, medication reviews, and non-visit follow-ups.
For example, a diabetes and hypertension program may use CCM workflows to track adherence, adjust treatment plans, and coordinate provider outreach between scheduled appointments.
Why Integrating RPM and CCM Is Important
Taken together, RPM and CCM support different parts of the chronic care journey. However, chronic care starts to break down when monitoring and care management operate in isolation. Data accumulates without follow-through. At the same time, care plans move forward without real-time context.
As a result, gaps emerge between insight and action. A hybrid approach closes this gap by aligning monitoring signals with structured care workflows.
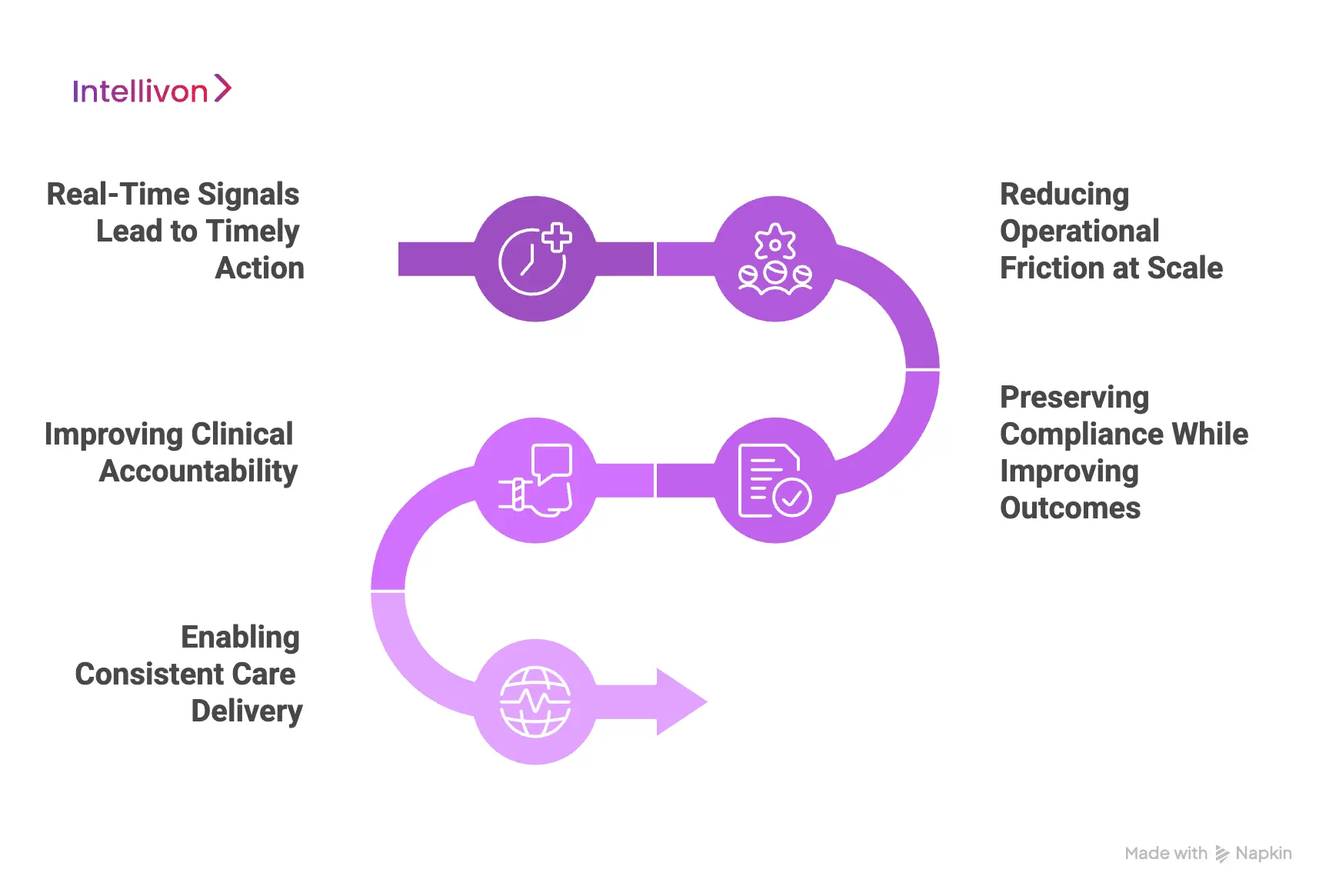
1. Turning Real-Time Signals Into Timely Action
RPM generates continuous insight. However, insight alone does not change outcomes. What matters most is how quickly signals lead to follow-ups, medication reviews, or care plan adjustments.
In practice, when RPM feeds directly into CCM workflows, interventions happen earlier. Therefore, teams act before issues escalate to the next scheduled visit.
2. Reducing Operational Friction at Scale
As programs grow, disconnected tools slow teams down. For example, switching systems and reconciling data adds manual overhead. Over time, coordination becomes inefficient.
Because of this, a unified environment removes friction points. As a result, care teams respond faster, and workflows remain manageable as patient volumes increase.
3. Preserving Compliance While Improving Outcomes
Regulatory boundaries do not disappear in a hybrid model. Instead, RPM and CCM retain separate billing, documentation, and audit logic. What changes is how execution is managed.
By design, shared infrastructure captures actions correctly. Consequently, compliance risk decreases while clinical continuity is preserved.
4. Improving Clinical Accountability
When systems remain separate, ownership is often unclear. As a result, alerts surface without clear responsibility, and follow-through becomes inconsistent.
With integrated workflows, accountability becomes explicit. Therefore, every signal leads to a documented response and clear follow-up.
5. Enabling Consistent Care Delivery
Distributed care models introduce variation over time. Without shared workflows, teams interpret data differently across locations. This inconsistency affects outcomes.
Through integration, care delivery becomes standardized. As a result, thresholds, escalation rules, and care protocols remain aligned regardless of location.
Taken together, integrating RPM and CCM strengthens more than clinical workflows. Ultimately, it brings clarity, consistency, and accountability to chronic care operations. For enterprises scaling these programs, integration becomes the foundation for sustainable growth rather than a technical afterthought.
How an RPM + CCM Hybrid Workflow Works Inside A Healthcare System
A hybrid RPM + CCM workflow succeeds when it behaves like a single operating system for chronic care. Monitoring signals flow into structured care actions, and every action has clear ownership, documentation, and time capture. The steps below show how this works inside an enterprise healthcare environment, from enrollment to monthly reporting.
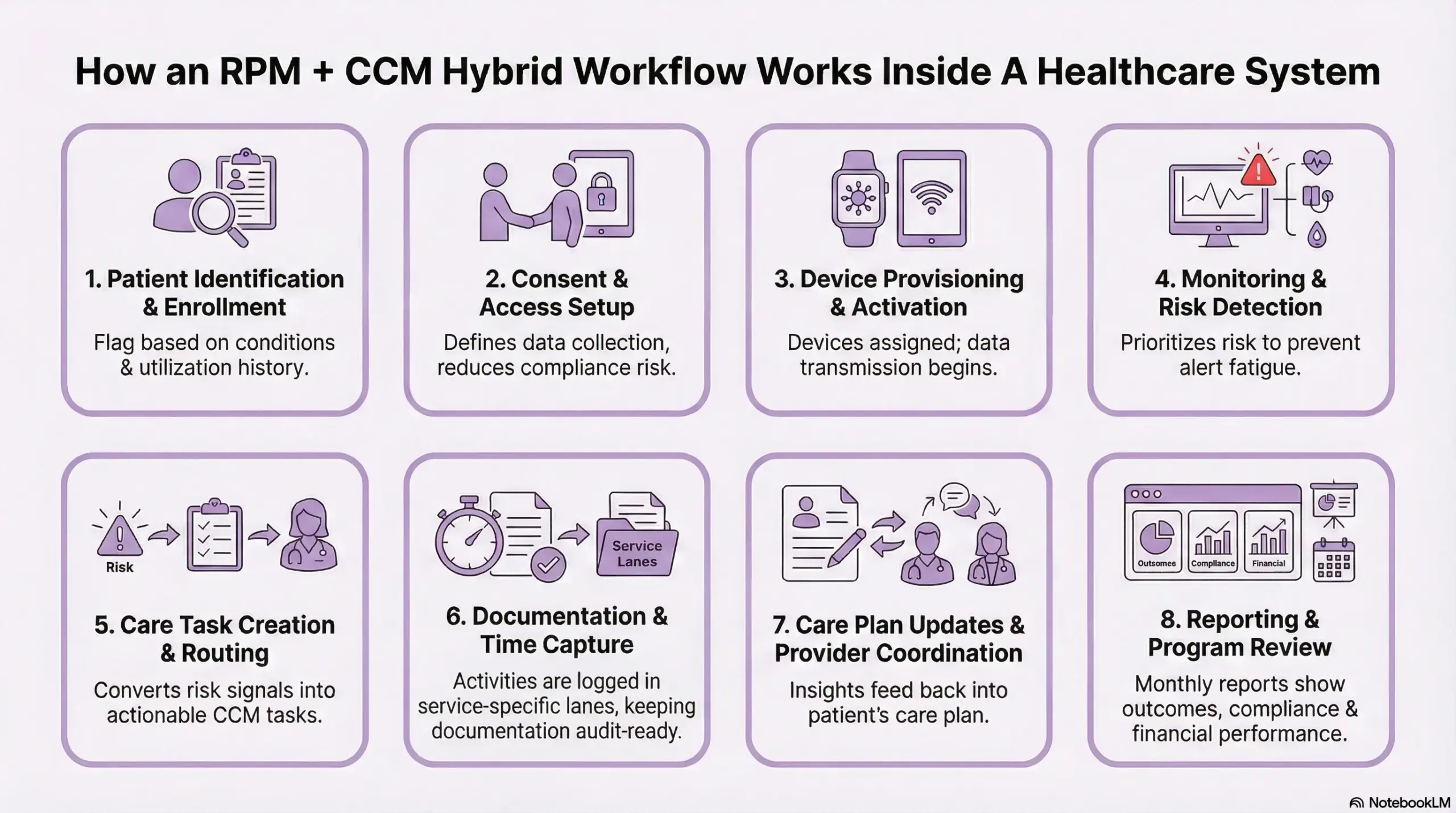
Step 1: Patient Identification and Enrollment
Most programs begin with EHR-driven patient identification. Teams flag patients based on chronic conditions, utilization history, or risk indicators. Enrollment follows a standardized process, so eligibility and consent are captured correctly.
Strong enrollment sets the foundation. Weak enrollment leads to downstream gaps in engagement and documentation.
Step 2: Consent and Access Setup
Consent defines how data is collected, shared, and acted upon. Role-based access is configured so clinicians, care managers, and support teams operate within governed boundaries.
This step reduces compliance risk and prevents access issues later in the workflow.
Step 3: Device Provisioning and Activation
Devices are assigned and configured according to care protocols. Data transmission begins through cellular or app-based connectivity, and initial readings confirm patient readiness.
Early support at this stage improves adherence and reduces drop-off.
Step 4: Monitoring and Risk Detection
Vitals are evaluated continuously against thresholds and trends. The system prioritizes risk instead of reacting to isolated readings.
This protects teams from alert fatigue and keeps attention focused on patients who need intervention.
Step 5: Care Task Creation and Routing
When risk is identified, the system converts signals into CCM tasks. Outreach, medication reviews, education, and care plan updates are created with clear ownership.
This is where hybrid systems outperform RPM-only tools. Data turns into action without manual coordination.
Step 6: Documentation and Time Capture
Activities are logged in service-specific lanes. RPM monitoring time and CCM coordination time are captured separately. Documentation remains structured and audit-ready.
This separation protects billing integrity as programs scale.
Step 7: Care Plan Updates and Provider Coordination
Insights from monitoring and outreach feed back into the care plan. Providers are looped in through EHR workflows or secure messaging when clinical decisions are required.
Over time, this creates a more responsive and adaptive care model.
Step 8: Reporting and Program Review
Monthly reporting surfaces outcomes, compliance readiness, and financial performance. Leadership gains visibility into capacity, risk trends, and program ROI.
This step turns chronic care into a managed service line rather than an ongoing pilot.
An RPM + CCM hybrid workflow works when each step is intentional and repeatable. Monitoring supplies insight, care management delivers action, and governance keeps the system scalable. When designed correctly, this workflow enables enterprises to manage chronic populations with consistency, accountability, and control.
RPM and CCM Hybrid Systems Achieved 0.51% Lower HbA1c
Hybrid RPM and CCM systems show their real value when monitoring data leads to timely, structured clinical action. In supported telemonitoring programs, patients did not just generate better data. They experienced measurable improvements in metabolic and cardiovascular outcomes because that data was actively used within care management workflows.
This is where hybrid systems differ from RPM-only deployments. The outcomes are not driven by devices alone. They emerge when monitoring is paired with consistent follow-up, care plan adjustments, and accountable clinical time.
1. Continuous Monitoring Improves Glycemic Control
Supported telemonitoring programs achieved 0.51 percent lower HbA1c compared to usual care. This improvement reflects more than improved visibility. It indicates earlier interventions, medication reviews, and patient outreach driven by ongoing data trends.
In enterprise settings, this matters because HbA1c improvement is rarely achieved through episodic visits alone. Hybrid systems allow care teams to identify deterioration early and respond within days rather than months. Over time, these small adjustments compound into sustained glycemic control across populations.
2. Better Blood Pressure Reductions
The same supported telemonitoring models showed reductions in ambulatory blood pressure, including 3.06 mmHg lower systolic and 2.17 mmHg lower diastolic readings. These shifts are clinically meaningful at a population level, especially for patients with multiple chronic conditions.
From an operational perspective, these results highlight the role of CCM workflows. Blood pressure improvement requires medication titration, adherence monitoring, and follow-up conversations. Hybrid systems make these actions routine instead of reactive by embedding them directly into care workflows.
3. Why RPM-Only Programs Produce the Same Results
RPM programs that operate without a care management layer often struggle to deliver similar outcomes. Data is collected, alerts are generated, but follow-through depends on manual effort or ad hoc processes. As patient volumes increase, this model becomes unsustainable.
Hybrid RPM and CCM systems address this gap by assigning ownership to every signal. Elevated readings translate into documented actions, clinical time, and accountable follow-up. This structure is what allows outcomes like improved HbA1c and blood pressure control to scale across large patient populations.
What This Means for Enterprise Healthcare Programs
For organizations managing chronic populations, these outcome improvements are not isolated clinical wins. They translate into fewer escalations, better contract performance, and more predictable care delivery. Even modest reductions in HbA1c and blood pressure reduce downstream utilization when applied across thousands of patients.
This is why enterprises evaluating RPM investments increasingly look beyond device capabilities. The differentiator is how effectively monitoring integrates into structured care management at scale.
Compliance-First Design Considerations for Hybrid RPM + CCM Systems
Hybrid RPM + CCM systems only scale when compliance is built into the platform itself. Retrofitting controls later creates risk, slows teams, and exposes programs during audits. A compliance-first design treats regulation as an operating constraint, not a documentation task.
1. Separate Services, Separate Accountability
RPM and CCM must remain distinct in how time, documentation, and billing are captured. Hybrid platforms succeed when these lanes are enforced technically, not left to manual discipline. This separation protects reimbursement integrity as volumes increase.
2. Consent and Eligibility Built Into Workflows
Consent, eligibility checks, and service enrollment should occur inside the workflow, not outside it. When these steps are embedded, downstream actions stay compliant by default and reduce reliance on manual checks.
3. Audit-Ready Documentation by Design
Every interaction should generate structured, time-stamped records tied to the correct service. This approach simplifies audits and reduces the operational burden on care teams and compliance staff.
4. Role-Based Access and Data Controls
Access must reflect clinical responsibility. Role-based permissions ensure teams only see and act on what they are authorized to manage, limiting exposure and misuse.
Compliance-first design allows hybrid RPM + CCM systems to grow without friction. When governance is embedded into workflows, enterprises gain scale, confidence, and long-term sustainability.
Compliance Rules That Need To Be Followed BY Hybrid RPM+CCM Systems
Hybrid RPM + CCM systems succeed only when both services meet their independent CMS compliance requirements. The platform may be unified, but regulatory rules are not. Below are the actual, non-negotiable rules enterprises must design around.
1. RPM Compliance Rules (Remote Patient Monitoring)
RPM is regulated as a physiologic monitoring service and must meet all of the following:
- FDA-Defined Medical Devices: RPM must use FDA-cleared medical devices when collecting physiologic data such as blood pressure, glucose, or weight.
- Minimum Data Transmission Requirement: Patients must transmit data on at least 16 days within a 30-day period to qualify for ongoing RPM reimbursement.
- Distinct Service Components: RPM requires documented evidence of device setup and patient education, ongoing device supply and data transmission, and clinical review and treatment management.
- Time-Based Clinical Monitoring: Clinical time billed for RPM must reflect actual data review and patient management activities and cannot overlap with CCM time.
2. CCM Compliance Rules (Chronic Care Management)
CCM is governed as a care coordination service with its own criteria:
- Patient Eligibility Requirement: Patients must have two or more chronic conditions expected to last at least 12 months or until death.
- Documented Comprehensive Care Plan: A structured care plan must be created, maintained, and accessible to the care team and patient.
- Minimum Monthly Time Threshold: CCM requires at least 20 minutes of non-face-to-face clinical care per calendar month, documented and attributable.
- Patient Consent and 24/7 Access: Explicit patient consent is required, along with access to care management services outside regular visits.
Rules for Using RPM and CCM Together
Hybrid systems must also enforce these shared constraints:
- No Double Counting of Time: The same clinical activity cannot be billed under both RPM and CCM.
- Separate Documentation and Audit Trails: Notes, time logs, and billing evidence must clearly indicate which service was delivered.
- Service-Specific Eligibility Checks: Eligibility must be validated independently for RPM and CCM, even for the same patient.
Compliance in hybrid RPM + CCM systems is not about simplification. It is about precision. Enterprises that succeed treat RPM and CCM as parallel, regulated services delivered through shared infrastructure. When these rules are enforced at the system level, programs remain audit-ready, scalable, and financially defensible.
Core Architecture Required to Build a HealthSnap-Style Platform
A HealthSnap-style platform is not defined by features. It is defined by how well the system holds up under scale, regulatory scrutiny, and operational complexity. Enterprise architecture must support continuous monitoring, longitudinal care management, and parallel compliance without creating bottlenecks for care teams.
When architecture is weak, RPM and CCM drift apart. When it is strong, both services operate predictably inside one governed system.
1. Unified Data and Identity Layer
Every hybrid platform starts with a shared data foundation. Patient identity must be resolved across devices, EHR records, care plans, and historical interactions. This layer normalizes data from multiple sources so RPM readings and CCM activities reference the same patient context.
At scale, this prevents duplication, mismatched records, and fragmented decision-making. It also ensures that insights generated in one workflow remain usable across the entire care continuum.
2. Monitoring and Signal Processing Engine
RPM data arrives continuously and in high volume. Enterprise platforms cannot rely on raw thresholds alone. This layer evaluates trends, rate of change, and patient history to surface meaningful risk signals.
By prioritizing relevance over volume, the system protects care teams from alert fatigue. As patient counts grow, this engine becomes critical to maintaining response quality without increasing staffing linearly.
3. Care Orchestration and Workflow Engine
This layer connects data to action. When a signal crosses a defined risk threshold, the platform generates structured CCM tasks such as outreach, medication review, or care plan updates. Each task has clear ownership, timelines, and documentation requirements.
Enterprise-grade orchestration ensures consistency. Care delivery does not depend on individual discretion. It follows defined workflows that can be audited, optimized, and scaled across regions and service lines.
4. Compliance and Time Attribution Services
Hybrid platforms must enforce separation technically, not procedurally. RPM and CCM operate in parallel lanes with distinct time tracking, documentation, and billing logic. Every action is logged with service context and role attribution.
This design protects reimbursement integrity and simplifies audits. Compliance teams gain visibility without slowing clinical operations, even as programs expand.
5. Interoperability and Enterprise Integration Layer
Enterprise adoption depends on fit, not replacement. Integration with EHRs, identity systems, analytics platforms, and billing infrastructure is essential. Support for HL7 and FHIR standards allows data to move cleanly across systems.
Platforms like HealthSnap scale because they embed into existing ecosystems rather than forcing organizations to replatform core systems.
A HealthSnap-style platform succeeds when architecture aligns monitoring, care coordination, and compliance from the start. When data, workflows, and governance are designed together, RPM and CCM scale as one system. This architectural discipline is what separates enterprise platforms from short-term solutions.
How Intellivon Builds an RPM + CCM Hybrid System Like HealthSnap
At Intellivon, we build RPM + CCM hybrid systems as long-term operating platforms, not short-term implementations. Every step is designed to support scale, compliance, and measurable outcomes without introducing operational drag. The process below reflects how these systems are built from the ground up.
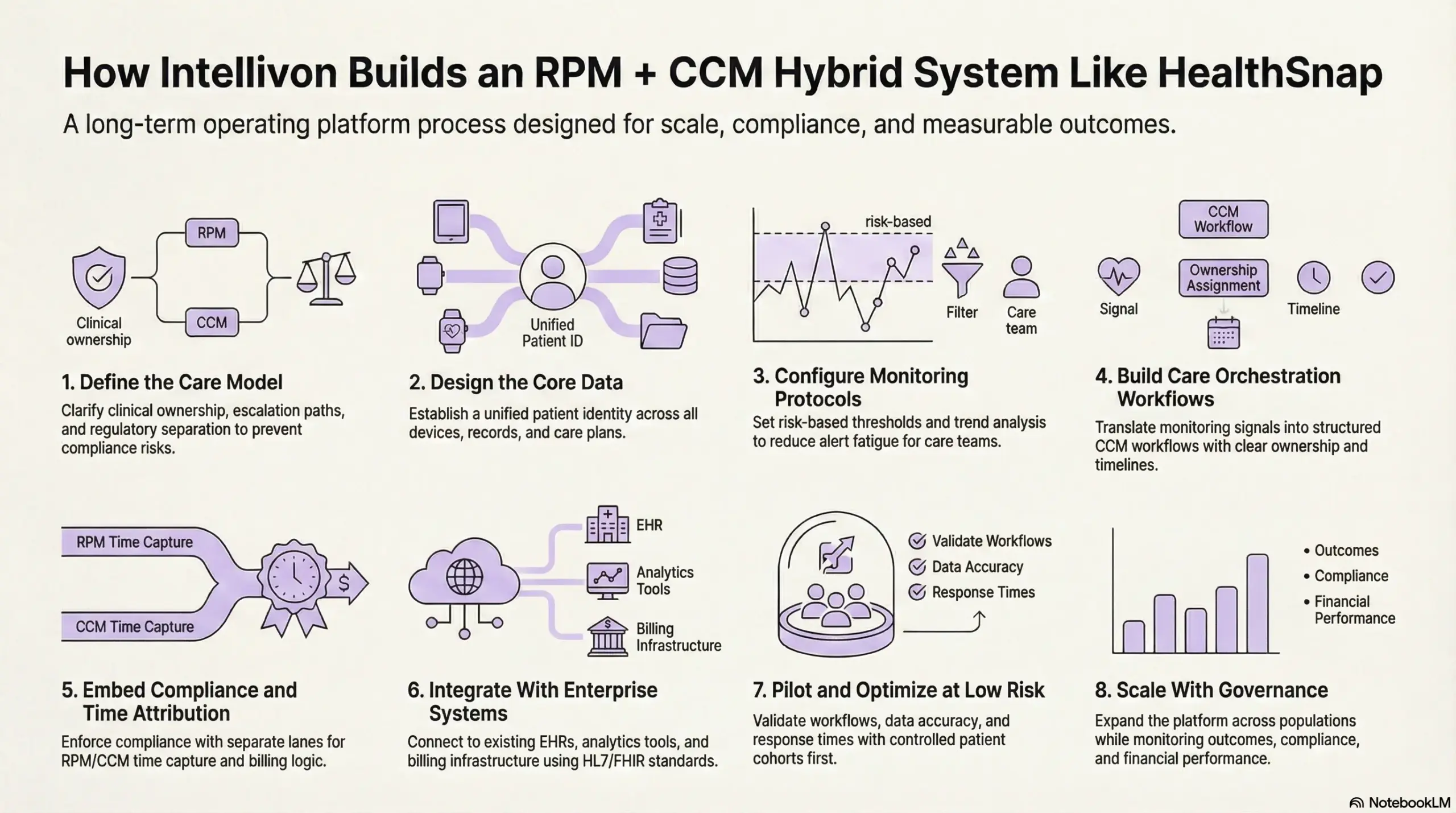
Step 1: Define the Care Model
We begin by clarifying how RPM and CCM will function as parallel services within one system. This includes defining clinical ownership, escalation paths, and regulatory separation.
By locking these boundaries early, we prevent billing overlap, documentation gaps, and downstream compliance risk. This step ensures the platform reflects real care delivery, not abstract assumptions.
Step 2: Design the Core Data
A unified patient identity is established across devices, EHR records, care plans, and historical interactions.
Data normalization rules are applied so that monitoring signals and care activities reference the same clinical context. This foundation eliminates duplication and enables consistent decision-making as patient volumes increase.
Step 3: Configure Monitoring Protocols
RPM protocols are configured by condition, risk level, and care goals. Thresholds are paired with trend analysis so the system prioritizes meaningful deterioration over isolated spikes.
This approach reduces alert fatigue and ensures care teams focus on patients who truly need intervention.
Step 4: Build Care Orchestration Workflows
Monitoring signals are translated into structured CCM workflows. Outreach, medication reviews, education, and care plan updates follow predefined paths with clear ownership and timelines.
Consistency matters here. Care delivery should not depend on individual discretion when programs scale across teams and regions.
Step 5: Embed Compliance and Time Attribution
Compliance is enforced through system behavior. RPM and CCM activities run in separate lanes with distinct time capture, documentation, and billing logic.
Every action is tagged to the correct service and role. This design keeps programs audit-ready without adding administrative burden to care teams.
Step 6: Integrate With Enterprise Systems
The platform is integrated into existing EHRs, identity systems, analytics tools, and billing infrastructure.
Support for HL7 and FHIR standards allows data to move cleanly without disrupting core operations. Enterprises adopt faster when systems fit naturally into their technology stack.
Step 7: Pilot and Optimize at Low Risk
Before scaling, workflows are piloted with controlled cohorts. We validate data accuracy, response times, documentation quality, and reporting outputs.
Feedback from clinical and operational teams is used to refine protocols. This step prevents small issues from becoming systemic failures later.
Step 8: Scale With Governance
Once validated, the platform scales across populations and service lines. Governance frameworks monitor outcomes, compliance, capacity, and financial performance.
Adjustments are made continuously as care models evolve. This ensures the system remains resilient as complexity grows.
Building an RPM + CCM hybrid system requires discipline at every stage. By aligning architecture, workflows, and compliance from the outset, Intellivon enables enterprises to scale chronic care programs with confidence. The result is a platform that supports growth without sacrificing control, reliability, or trust.
What Is The Cost To Build an RPM + CCM Hybrid System?
Building an RPM + CCM hybrid system does not require a single, large upfront investment. Most enterprises start with a focused foundation that supports remote monitoring, structured care management, compliance separation, and core integrations. From there, the platform evolves as patient volumes grow and chronic programs expand.
At Intellivon, we structure costs around platform maturity, not feature count. This phased approach allows organizations to launch faster, validate outcomes early, and scale RPM and CCM together without introducing compliance or operational risk.
Estimated Cost Breakdown (USD 95,000–260,000)
| Cost Component | What It Covers | Estimated Range |
| Discovery & Hybrid Care Model Design | RPM and CCM service boundaries, workflows, escalation logic, compliance separation, outcome KPIs, and platform architecture | $12,000 – $24,000 |
| Patient Enrollment & Eligibility Workflows | CCM eligibility checks, RPM enrollment, consent capture, baseline assessments, and continuity logic | $14,000 – $32,000 |
| RPM Device & Data Ingestion Layer | Device provisioning logic, data normalization, cellular/app ingestion, and monitoring readiness checks | $16,000 – $38,000 |
| Care Coordination & CCM Workflow Engine | Task routing, outreach workflows, care plan updates, escalation paths, and clinician overrides | $14,000 – $34,000 |
| Signal Processing & Risk Prioritization | Thresholds, trend analysis, risk scoring, and alert-to-task conversion with governance | $12,000 – $30,000 |
| EHR & Enterprise Integrations | HL7/FHIR integration, identity sync, documentation exchange, and provider workflows | $18,000 – $42,000 |
| Identity, Consent, and Access Governance | Role-based access, consent lifecycle management, audit controls, and SSO options | $8,000 – $18,000 |
| Compliance, Security, and Audit Controls | HIPAA safeguards, encryption, logging, time attribution, and audit-ready reporting | $8,000 – $16,000 |
| Analytics & Program Reporting | RPM utilization, CCM activity, outcomes tracking, and executive dashboards | $6,000 – $16,000 |
| Testing, Pilot, and Stabilization | QA, workflow validation, pilot rollout, clinician feedback, and system tuning | $6,000 – $20,000 |
Typical MVP Range: $95,000 – $145,000
Enterprise-Ready Phase 1 Platform: $170,000 – $260,000
Final costs vary based on integration depth, governance requirements, and the level of clinical oversight required from launch.
Factors That Influence the Cost of RPM + CCM Hybrid Systems
Cost in hybrid systems is driven by care complexity and governance, not interface count. Understanding these drivers early helps enterprises avoid rework and budget overruns.
1. Depth of Hybrid Care Design
Basic monitoring with limited follow-up costs less than supporting multi-condition care plans, escalation tiers, and structured CCM workflows. Greater rigor increases cost but reduces risk at scale.
2. Integration With Existing Healthcare Infrastructure
Light integration surfaces data. Deeper integration synchronizes documentation, provider workflows, and billing context. While more expensive, it prevents fragmentation and operational drag.
3. Compliance and Time Attribution Requirements
Hybrid systems must enforce strict separation between RPM and CCM time, documentation, and billing. Engineering this correctly increases upfront cost but protects long-term reimbursement.
4. Identity, Roles, and Access Control
Enterprise platforms support patients, clinicians, care managers, and administrators. Managing consent and access across roles adds complexity but is essential for audit readiness.
5. Analytics and Executive Visibility
Basic reports show activity. Enterprise analytics explain outcomes, utilization trends, and financial performance. This depth supports defensible ROI discussions and program optimization.
How RPM + CCM Hybrid System Like HealthSnap Generates Revenue
An RPM + CCM hybrid system generates revenue by aligning regulated care delivery with predictable, recurring reimbursement. The model works when monitoring and care management are delivered through a single platform while billing and compliance remain separate. This creates steady monthly revenue without relying on episodic visits.
1. RPM-Based Monthly Reimbursement
RPM revenue is driven by device setup, data transmission, and ongoing clinical monitoring. Once patients are enrolled and transmitting data consistently, reimbursement becomes recurring.
As patient volume grows, RPM creates a stable baseline of monthly revenue tied directly to active engagement.
2. CCM Care Coordination Revenue
CCM adds a second revenue stream focused on non-face-to-face care coordination. Monthly reimbursement is earned through documented care planning, follow-ups, medication reviews, and provider coordination.
Because CCM applies to patients with multiple chronic conditions, revenue scales with population complexity rather than visit frequency.
3. Concurrent RPM and CCM Billing
Hybrid systems allow eligible patients to be enrolled in both programs at the same time. When workflows are designed correctly, RPM monitoring and CCM coordination generate parallel revenue without double-counting time or activities.
This is where platforms like HealthSnap unlock higher per-patient lifetime value.
4. Improved Retention and Program Longevity
Revenue durability depends on retention. Hybrid systems improve engagement by combining real-time monitoring with proactive outreach.
Patients stay enrolled longer, which increases cumulative revenue per patient while reducing churn-related acquisition costs.
5. Enterprise-Level Financial Visibility
Because all activity flows through one platform, leadership gains clear visibility into utilization, margins, and reimbursement performance.
This enables accurate forecasting, capacity planning, and controlled expansion across service lines.
An RPM + CCM hybrid system generates revenue by turning chronic care into a recurring, well-governed service line. When monitoring and care coordination work together inside a compliant platform, revenue grows predictably, scales efficiently, and supports long-term enterprise sustainability.
Conclusion
Hybrid RPM + CCM systems represent a shift in how chronic care is designed and scaled. When monitoring and care management operate inside a single, governed platform, outcomes improve, and operations become predictable. The real advantage is not devices or dashboards. It is the ability to translate patient data into timely, accountable care at enterprise scale.
For organizations planning long-term growth, this model turns chronic care into a reliable service line rather than an ongoing pilot. At Intellivon, we build these platforms with compliance, scalability, and outcomes at the core. The result is a system that supports growth while maintaining control, trust, and financial clarity.
Build an RPM + CCM Hybrid System Like HealthSnap With Intellivon
At Intellivon, we build RPM + CCM hybrid systems as enterprise operating platforms, not monitoring tools or care management add-ons layered onto fragmented workflows. Our platforms are designed to govern how patients are enrolled into chronic care, how real-time signals translate into coordinated action, and how accountability is maintained across regulated services, care teams, and enterprise infrastructure.
Each solution is engineered for healthcare organizations operating at scale. Platforms are infrastructure-first and compliance-led, with RPM and CCM delivered as parallel services through a shared system. As programs expand across populations, regions, and value-based contracts, clinical oversight, data integrity, and financial control remain intact.
Why Partner With Intellivon?
- Hybrid-first platform architecture aligned with chronic care delivery, regulatory separation, and enterprise-scale operations
- Deep interoperability expertise across EHRs, device ecosystems, identity platforms, analytics stacks, and billing systems
- Compliance-by-design delivery supporting HIPAA, CMS audit readiness, role-based access, and service-specific governance
- AI-assisted care orchestration that prioritizes risk, routes action, and supports clinicians without replacing judgment
- Enterprise delivery model with phased rollout, KPI-driven validation, and controlled scale across chronic care programs
Talk to Intellivon’s healthcare platform architects to explore how an enterprise-grade RPM + CCM hybrid system can integrate into your existing ecosystem, reduce operational friction, protect regulatory integrity, and scale chronic care with confidence.
FAQs
Q1. Can RPM and CCM be used together in the same healthcare program?
A1. Yes, RPM and CCM can be used together when delivered as parallel services within a single platform. Each service must follow its own eligibility, documentation, and billing rules. Hybrid systems work by sharing data and workflows while keeping compliance and time tracking separate.
Q2. What is an RPM + CCM hybrid system in healthcare?
A2. An RPM + CCM hybrid system is a platform that delivers remote monitoring and chronic care management through shared infrastructure. RPM supplies real-time patient data, while CCM structures follow-ups, care plans, and coordination. The system connects insight to action without merging regulatory requirements.
Q3. How does a hybrid RPM + CCM system improve patient outcomes?
A3. Hybrid systems improve outcomes by enabling earlier intervention and consistent follow-up. Monitoring data highlights risk sooner, and CCM workflows ensure those signals lead to outreach, medication reviews, or care plan updates. This reduces delays that often occur in episodic care models.
Q4. What compliance risks should enterprises consider when combining RPM and CCM?
A4. The primary risk is improper time and billing overlap. RPM and CCM must remain independently documented and billed. Hybrid platforms reduce this risk by enforcing service separation at the system level, ensuring audit-ready records as programs scale.
Q5. How much does it cost to build an RPM + CCM hybrid system?
A5. Costs typically range from $95,000 to $260,000, depending on scope, integrations, and governance needs. Most enterprises start with a focused MVP and expand in phases. A compliance-first architecture reduces rework and long-term operational costs.





