Care delivery in enterprises today generates a lot of information, but decisions are often scattered. This is because clinically-driven guidance frequently depends on fixed logic, personal judgment, or separate tools. As digital health programs develop and scale, the gap between available data and practical insights becomes more obvious in operations, outcomes, and experiences.
As a result, many organizations are moving from one-time interventions to ongoing health guidance. They need systems that provide recommendations based on context, behavior, and timing. AI-driven recommendation engines support this change by turning scattered data into relevant health actions that can grow without adding to the clinical workload.
This is where Intellivon’s expertise comes in. We create AI health recommendation engines from scratch as enterprise decision systems. Each platform is designed for compatibility, audit readiness, and long-term growth. At the same time, our focus is on control, reliability, and measurable impact, rather than experimentation without responsibility. Drawing on this experience, we are using this blog to discuss how we build these engines from the ground up and keep them compliant even as they scale.
Why Enterprises Are Investing in AI Health Recommendation Engines Now
At the same time, healthcare-specific AI recommendation segments post a 19% CAGR through 2030, propelled by personalized medicine demands.
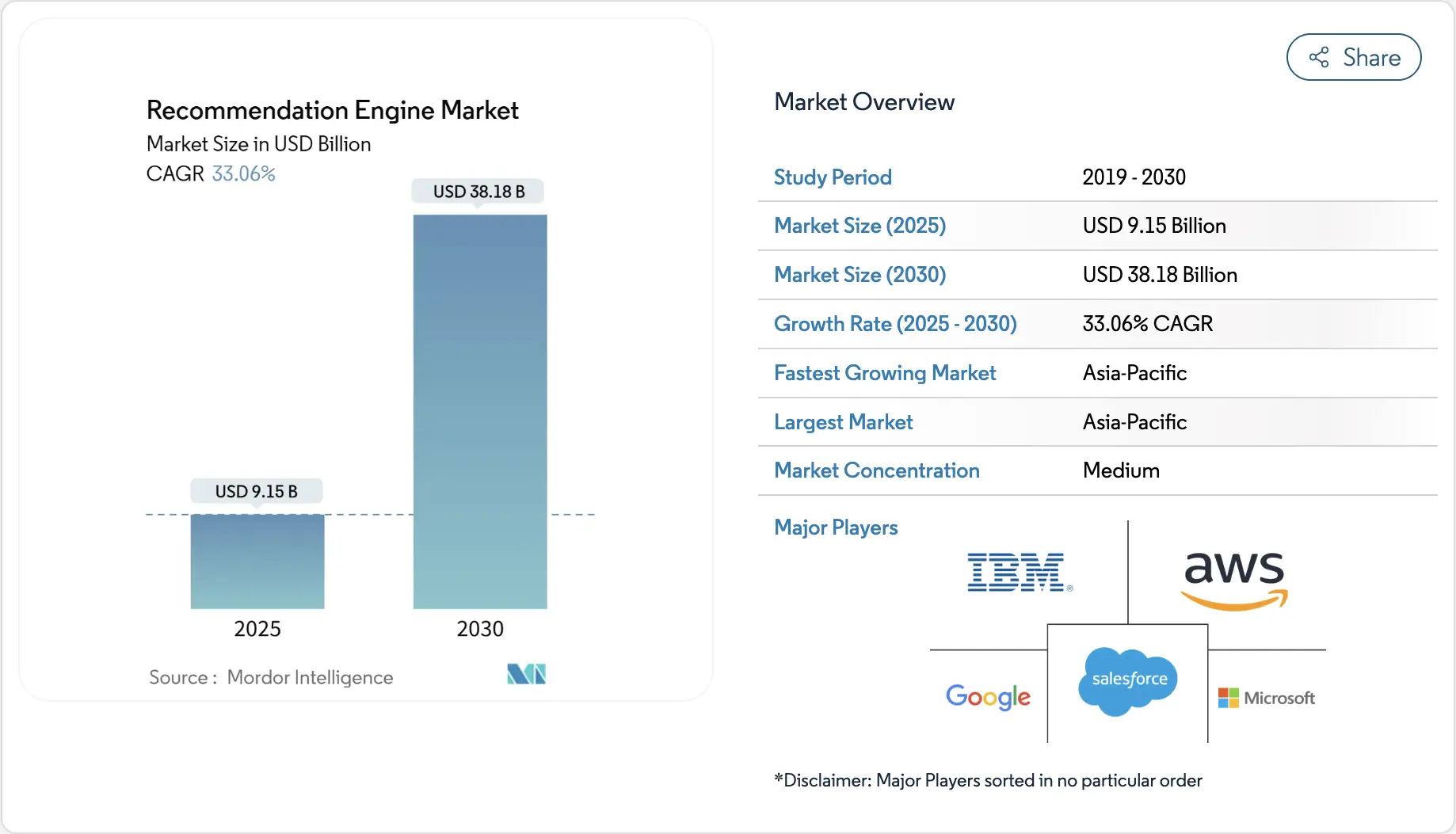
Market Insights:
- Chronic disease management and personalized care plans drive demand, as AI flags risks and optimizes medication using real-time patient data.
- Enterprise integration with telehealth platforms and EMRs reduces clinician workload, supporting adoption amid workforce shortages and value-based care models.
- Regulatory pressure for HIPAA-compliant AI and payer incentives tied to outcomes accelerate B2B deployment across hospitals and payer organizations.
- Enterprises embed recommendation engines in virtual care for triage and risk prediction, with U.S. systems like Mayo Clinic scaling AI to improve outcomes.
- Cloud-hybrid architectures, holding 64% share, ease legacy EMR integration, while 2026 agentic AI trends target ROI and readmission reduction.
Enterprises are adopting AI health recommendation engines to reduce care variability, improve engagement, and operationalize personalization without increasing clinical overhead.
1. Shifting from Reactive Care to Continuous Health Guidance
Care delivery has traditionally operated in isolated episodes. Patients engage during visits, then disappear between interactions. However, outcomes increasingly depend on what happens outside clinical encounters.
Research published on PubMed shows that AI-supported clinical decision systems have contributed to approximately 25% reductions in hospital readmissions, signaling earlier and more accurate interventions
AI health recommendation engines enable this shift by delivering guidance based on evolving patient context. As a result, care becomes adaptive rather than reactive. This model aligns closely with value-based contracts that reward sustained outcomes over episodic activity.
2. Scaling Personalization Without Scaling Teams
Personalization increases decision complexity. Clinicians already manage heavy cognitive and administrative workloads. Adding manual personalization does not scale.
AI health recommendation engines absorb this decision load by continuously analyzing patient history, risk signals, and treatment responses. These systems surface context-aware recommendations without adding workflow friction.
According to research summarized on ambient clinical documentation, AI-assisted systems significantly reduce documentation and administrative burden for clinicians
3. Monetization and ROI Alignment Across Care Programs
Enterprises increasingly tie digital investments to measurable financial outcomes. AI health recommendation engines support this alignment by improving accuracy earlier in care pathways.
Electronic prescribing and AI-supported decision tools have been shown to reduce medication and prescribing errors by up to 30%, improving treatment reliability and safety
Improved accuracy drives downstream value. At the same time, fewer errors reduce avoidable complications, lower liability exposure, and stabilize cost structures. In addition, personalized recommendations improve adherence and engagement, which strengthens retention in value-based and risk-sharing models. As a result, recommendation engines become both a clinical asset and a revenue enabler.
What Is an AI Health Recommendation Engine in Healthcare?
An AI health recommendation engine is a decision intelligence system that analyzes longitudinal patient, clinical, and behavioral data to deliver context-aware health actions at scale.
An AI health recommendation engine functions as a decision layer, not a conversational tool. It evaluates data over time, then determines what action makes sense next. This includes guidance for patients, prompts for clinicians, and signals for care teams. The focus stays on decisions, not dialogue.
Unlike chatbots, these engines do not rely on scripted responses. Unlike alerts, they do not trigger based on single thresholds. Instead, they interpret patterns across history, risk, behavior, and outcomes.
Enterprises deploy engines rather than isolated AI models for control and consistency. A single model solves a narrow task. An engine governs how multiple models, rules, and policies work together. This approach supports scale, auditability, and integration across apps, EHRs, and care programs. As a result, personalization becomes reliable, explainable, and operationally sustainable.
How AI Health Recommendation Engines Work
In an enterprise setup, a recommendation engine sits between data systems and care workflows. It does not replace clinicians or care programs. Instead, it turns scattered signals into consistent “next best actions.”
These actions can reach patients, clinicians, and care teams through the tools they already use. Therefore, the engine must handle integration, governance, and performance at scale.
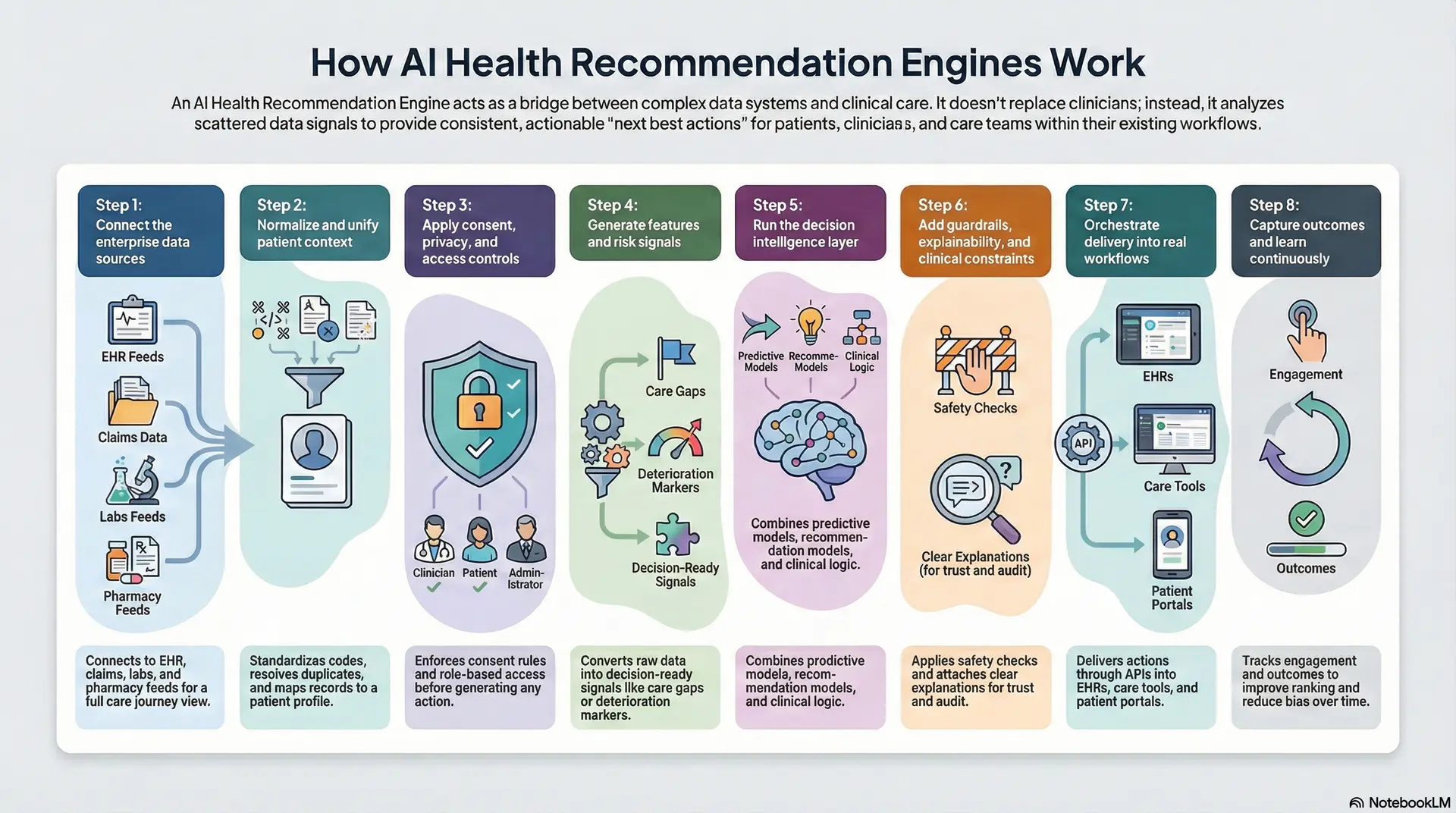
Step 1: Connect the enterprise data sources
The engine starts by connecting to the systems that hold patient context. This often includes EHR data, claims, lab results, pharmacy feeds, remote monitoring, and app activity.
In addition, it may ingest SDOH signals and care management notes. The goal is coverage across the full care journey. Without this, recommendations become narrow and unreliable.
Step 2: Normalize and unify patient context
Healthcare data arrives in different formats and levels of quality. Therefore, the engine standardizes codes, timestamps, units, and identities. It resolves duplicates and maps records to a longitudinal patient profile.
In addition, it applies data quality checks and completeness scoring. This step prevents false confidence later in the workflow.
Step 3: Apply consent, privacy, and access controls
Before the engine generates any action, it enforces policy. It checks consent, purpose limitation, and data minimization rules. It also enforces role-based access across clinicians, care teams, and support staff.
In addition, it logs who accessed what and why. This is what makes the system audit-ready in real operations.
Step 4: Generate features and risk signals
Next, the engine converts raw data into decision-ready signals. It creates features such as trend changes, gaps in care, medication risk, or deterioration markers. It also detects patterns across time, not single events.
However, it must avoid “noise” that creates alert fatigue. Therefore, it prioritizes signals that correlate with outcomes and actionability.
Step 5: Run the decision intelligence layer
This is the core reasoning step. The engine runs predictive models, recommendation models, and clinical logic together. It can combine machine learning outputs with guideline rules and enterprise policies.
In addition, it can apply eligibility logic for programs and coverage constraints. The output becomes a ranked set of actions, not a single answer.
Step 6: Add guardrails, explainability, and clinical constraints
Before actions are delivered, the engine applies safety checks. It filters unsafe suggestions, conflicts, and contraindications. It also attaches an explanation that is easy to audit and review.
Therefore, clinicians can see what drove the recommendation. This step builds trust and reduces adoption friction.
Step 7: Orchestrate delivery into real workflows
Recommendations only matter when they show up in the right place. The engine delivers actions through APIs into EHR workflows, care management tools, telehealth apps, and patient portals.
It also chooses timing and channel based on context and urgency. In addition, it can route actions to the right role, such as nurse, pharmacist, or coach. This is how personalization becomes operational, not theoretical.
Step 8: Capture outcomes and learn continuously
Finally, the engine tracks what happened after each recommendation. Did the patient engage, ignore, or escalate? Did the clinician accept, modify, or override? It also tracks clinical and operational outcomes over time.
Therefore, the system can improve ranking, reduce bias, and tune thresholds. This feedback loop is what turns a one-time build into a durable capability.
AI recommendation engines succeed when they behave like governed infrastructure. They unify data, enforce policy, produce explainable actions, and fit inside existing workflows. As a result, personalization scales without adding chaos to care delivery.
Personalized Recommendations Drive a 30% Reduction in Diagnostic Errors
Diagnostic error remains one of the hardest risks for large care networks to manage. These issues rarely stem from inadequate clinical skill. Instead, they arise when decisions are made without full patient context, often under intense time pressure and operational strain.
Personalized treatment recommendation systems have demonstrated up to a 30% reduction in diagnostic errors by evaluating patient-specific clinical patterns rather than relying on fixed care rules.
1. Why Diagnostic Errors Continue to Occur
Even well-integrated hospital systems struggle to maintain diagnostic consistency across locations. Patient information is frequently scattered across EHR components, care settings, and legacy records. Clinicians must reconstruct context mentally while managing high patient volumes.
Traditional clinical decision support tools depend heavily on rule-based alerts. Although helpful, they fail to adapt to complex cases involving comorbidities or varied treatment responses. As a result, diagnostic variation persists across enterprise-scale care delivery.
2. How Personalized Systems Improve Decision Accuracy
Personalized treatment platforms operate above legacy CDSS frameworks and assess patient context more comprehensively. These systems evaluate longitudinal records, comorbid conditions, medication history, and prior outcomes together.
Predictive models trained on real-world clinical data then surface recommendations aligned with both evidence and individual risk profiles. This context-aware approach has been associated with up to 30% fewer diagnostic errors in organizations using AI-driven personalization.
3. Impact on Readmissions
The impact extends beyond diagnosis alone. Health systems deploying individualized and predictive care strategies report up to a 20% reduction in 30-day readmissions, particularly among chronic and high-risk populations.
Global health authorities have identified diagnostic error as a major patient safety concern. Industry research also shows that AI-supported decision systems reduce readmissions by improving treatment accuracy earlier in the care journey.
Why This Matters
For enterprise leaders, a 30% reduction in diagnostic errors delivers compounding benefits. Fewer misdiagnoses lower avoidable complications, reduce liability exposure, and improve operational consistency across facilities.
Improving diagnostic accuracy at this level strengthens enterprise risk posture while bringing greater reliability to distributed care environments.
Core Use Cases of AI Health Recommendation Engines Across Enterprises
AI health recommendation engines support prevention, chronic care, engagement, and clinical decision support through personalized, data-driven health actions.
Enterprises usually adopt recommendation engines to fix specific breakdowns in care delivery. These systems are applied where inconsistency creates risk, cost, or inefficiency. The following use cases reflect where deployments deliver clear operational and clinical value.
1. Risk-Based Health Nudges
Preventive care depends on identifying risk before escalation. In practice, risk signals sit across labs, history, engagement data, and missed screenings. Clinicians rarely have time to connect these signals manually.
Recommendation engines analyze these inputs continuously and surface early risk indicators. They generate screening reminders, lifestyle guidance, and follow-up prompts based on risk progression. As patient behavior changes, recommendations adjust. This keeps prevention active instead of episodic.
2. Chronic Condition Management at Scale
Chronic condition programs struggle with consistency as scale increases. Guidance often remains static even when patient response changes.
Recommendation engines support diabetes, cardiac, and respiratory care by updating guidance based on vitals, medication response, adherence, and symptoms. Care plans evolve over time rather than resetting at each visit. This allows enterprises to manage large chronic populations with fewer manual interventions.
3. Post-Consultation and Care Follow-Ups
Care gaps often appear after a consultation. Instructions are given, but follow-through depends on patient action or staff outreach.
These AI-powered recommendation engines automate next-step guidance using visit context and risk level. They trigger reminders for diagnostics, medications, education, or follow-up visits. This reduces missed steps without expanding care teams. Follow-up becomes consistent and trackable.
4. Member and Patient Engagement Optimization
Engagement varies by timing, channel, and frequency. Generic outreach performs poorly because it ignores prior behavior.
These engines adjust outreach based on response patterns. They determine when to engage, how often, and through which channel. Over time, communication becomes more targeted. This improves adherence and program participation without increasing message volume.
These use cases address different points in the care journey, but they rely on the same capability. A centralized decision system that adapts to context. When deployed together, they reduce variability, limit manual effort, and improve predictability across enterprise care programs.
How AI Works In Health Recommendation Engines
In enterprise healthcare, AI works as a structured decision system that connects data, logic, and feedback.
Each stage plays a defined role in turning signals into usable guidance. The goal is consistency, safety, and scale across real care workflows.
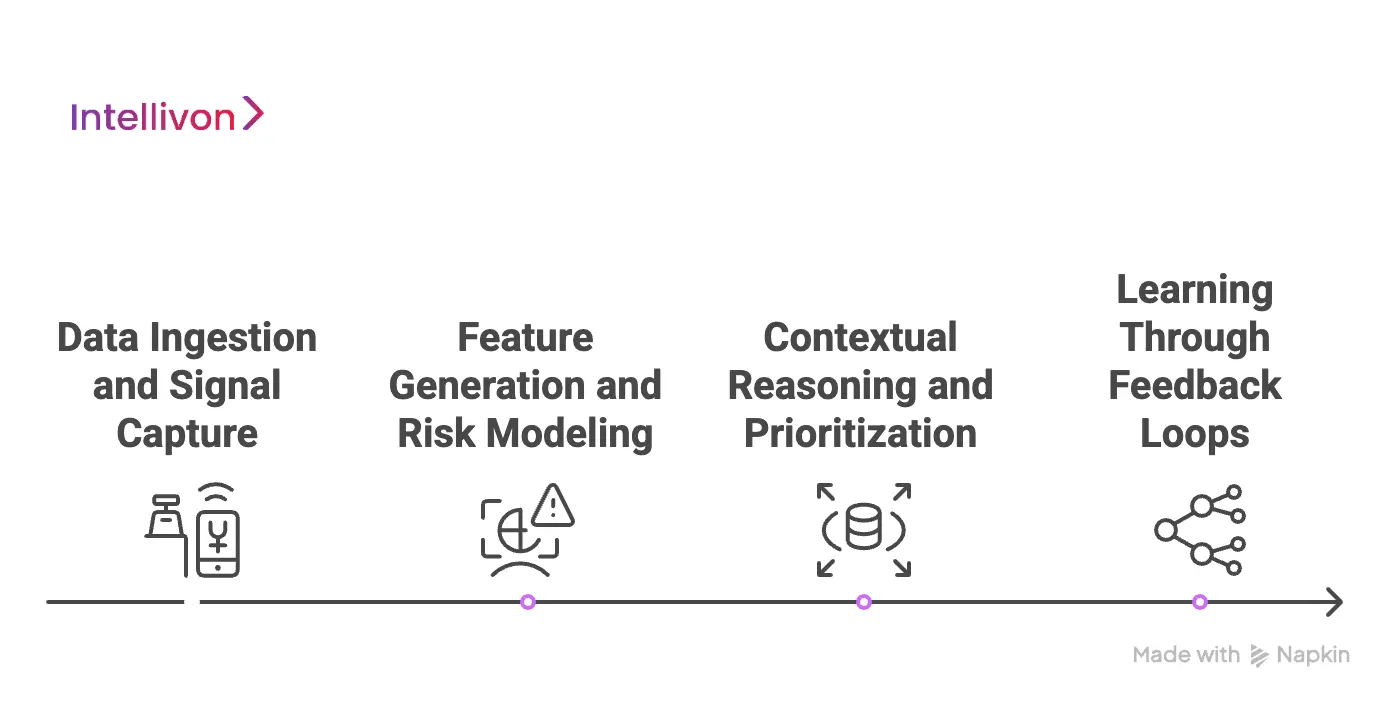
1. Data Ingestion and Signal Capture
The engine first connects to enterprise systems such as EHRs, claims platforms, labs, devices, and care applications. It ingests both historical and real-time data to understand patient context.
Rather than reacting to isolated events, it tracks patterns and trends over time. This longitudinal view reduces blind spots and improves reliability. As a result, recommendations are grounded in complete context, not partial snapshots.
3. Feature Generation and Risk Modeling
Once data is ingested, the system converts it into structured decision signals. These include risk trends, gaps in care, medication exposure, and behavioral indicators. Predictive models then estimate likelihoods tied to outcomes such as deterioration or non-adherence.
The focus stays on relevance rather than volume. This prevents noise from overwhelming clinicians and care teams.
4. Contextual Reasoning and Prioritization
Model outputs alone do not drive decisions. The engine evaluates them alongside clinical rules, enterprise policies, and care constraints. It weighs urgency, risk level, and appropriateness together.
Recommendations are ranked instead of triggered automatically. This supports clinician judgment and reduces alert fatigue across workflows.
5. Learning Through Feedback Loops
After recommendations are delivered, the system tracks what happens next. It records acceptance, overrides, and downstream outcomes. This feedback is used to refine future recommendations.
Over time, accuracy improves, and bias is reduced. The engine adapts without requiring constant manual tuning.
AI adds value in recommendation engines when it behaves like governed infrastructure. It connects data, applies reasoning, and learns from outcomes. When designed correctly, it scales consistent guidance across enterprises without adding operational complexity.
Architecture Of An AI Health Recommendation Engine For Enterprises
In enterprise healthcare, architecture determines whether a recommendation engine can scale safely. These systems must handle sensitive data, complex workflows, and regulatory pressure without breaking trust. A layered architecture keeps responsibilities clear, where each layer solves a specific problem while supporting the next one.
1. Data Integration and Ingestion Layer
This layer connects the engine to enterprise data sources across the care ecosystem. It ensures that clinical, operational, and behavioral data flows reliably into the system. The focus is on coverage and continuity, not speed alone. Without stable ingestion, downstream intelligence becomes unreliable.
Data is pulled from source systems in real time or batches. Events are timestamped and routed for processing. Lineage is preserved for traceability and audits.
Technologies used
- HL7 and FHIR interfaces
- Secure REST and event-based APIs
- Streaming ingestion pipelines
- Batch ETL and ELT processes
- Encrypted data connectors
2. Data Normalization and Patient Context Layer
Healthcare data arrives fragmented and inconsistent. This layer standardizes and unifies it into a longitudinal patient view. It ensures that recommendations are based on accurate and complete context rather than partial records.
Clinical codes, units, and identifiers are normalized. Duplicate records are resolved. Patient timelines are built across encounters and care settings.
Technologies used
- Terminology mapping services
- Master patient index resolution
- Schema transformation engines
- Data quality validation rules
- Longitudinal record builders
3. Consent, Privacy, and Governance Layer
Enterprise systems must enforce privacy before intelligence is applied. This layer ensures data use aligns with consent, regulation, and internal policy. Governance is embedded directly into the workflow.
Consent is validated before processing begins, role-based access is enforced, and all data access is logged for audit readiness.
Technologies used
- Consent management frameworks
- Role-based access control (RBAC)
- Attribute-based access policies
- Audit logging and traceability tools
- Data masking and tokenization
4. Intelligence and Decision Modeling Layer
This layer generates the recommendations themselves. It combines predictive models with clinical logic and enterprise rules. Ultimately, the goal is decision support that adapts to context while remaining explainable.
In this layer, features are generated from patient data, risk and outcome models are executed, and clinical and operational constraints are applied together.
Technologies used
- Predictive and classification models
- Rules engines and decision trees
- Feature stores and signal pipelines
- Model inference services
- Policy-based decision logic
5. Orchestration and Delivery Layer
Recommendations only create value when delivered into real workflows. This layer controls where, when, and to whom actions are sent. It ensures guidance appears inside existing tools.
Actions are routed to EHRs, care platforms, or patient apps. Timing and channel are selected based on urgency and role. Escalation paths are applied when needed.
Technologies used
- Workflow orchestration engines
- API-based action delivery
- Notification and messaging services
- Context-aware routing logic
- Channel selection algorithms
6. Feedback and learning layer
Enterprise engines must improve over time. This layer captures outcomes and refines decision quality. Here, learning is continuous but governed.
The system records acceptance, overrides, and outcomes. Performance is monitored across populations. Models and rules are adjusted carefully.
Technologies used
- Outcome tracking pipelines
- Feedback ingestion services
- Model monitoring and drift detection
- Bias and fairness evaluation tools
- Controlled retraining workflows
A layered architecture turns AI health recommendation engines into durable enterprise systems. Each layer enforces clarity, control, and accountability.
When designed this way, recommendation engines scale safely, integrate cleanly, and support consistent decision-making across complex care environments.
How We Approach AI Health Recommendation Engine Development
At Intellivon, AI health recommendation engines are treated as enterprise decision systems, not standalone models. The approach prioritizes control, explainability, and operational fit from the outset.
Each step is designed to reduce risk while creating measurable value. This ensures the platform performs reliably in real healthcare environments
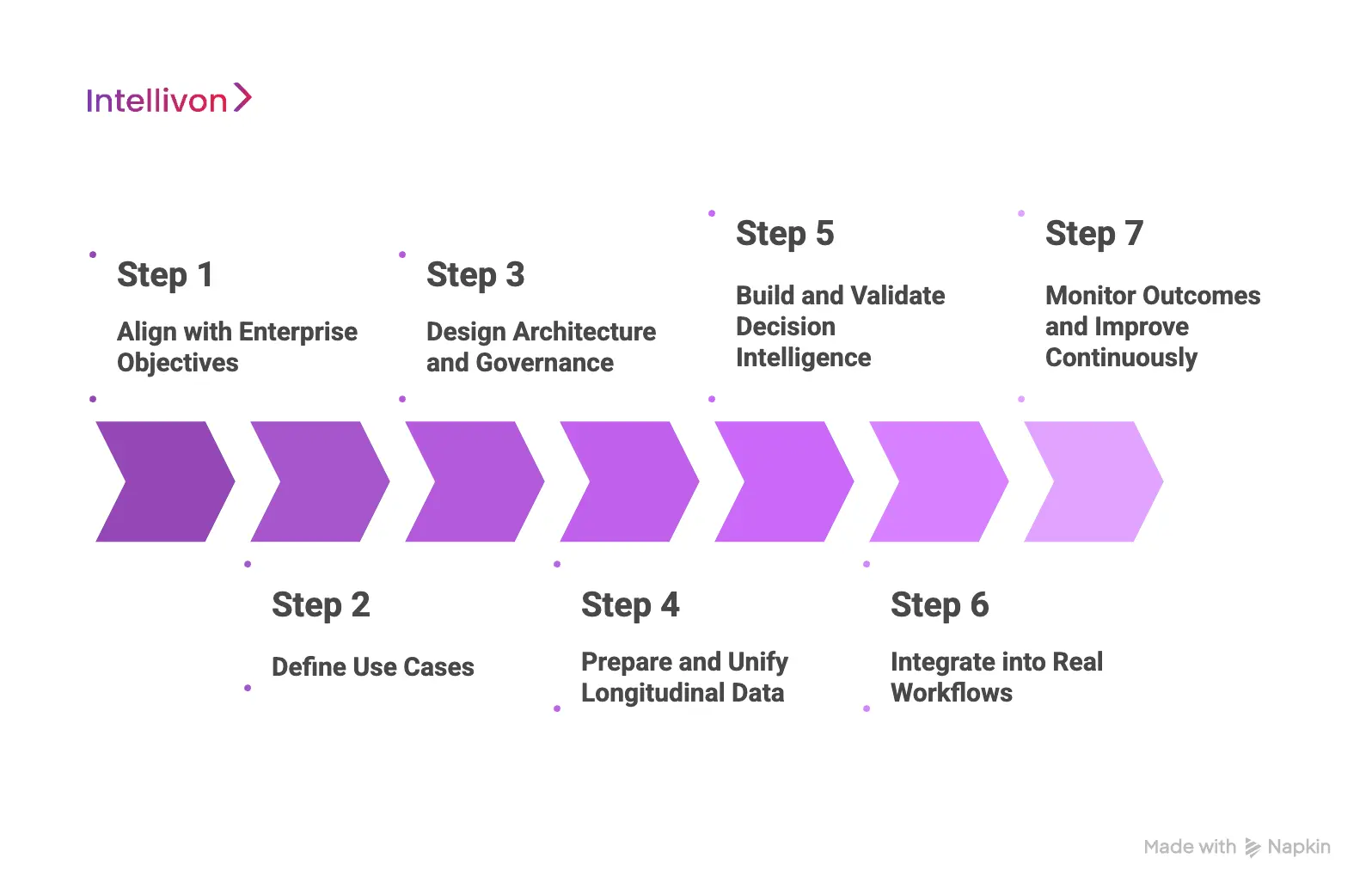
Step 1: Align with Enterprise Objectives
Every engagement begins with clarity on impact. Under the engines that we build, our experts ensure that we map clinical priorities, financial goals, and operational constraints together.
This helps identify where recommendations must influence outcomes. Additionally, care journeys are prioritized based on risk and value. At the same time, all downstream decisions trace back to this alignment.
Step 2: Define Use Cases
Clear boundaries prevent misuse and overreach. Under this step, Intellivon focuses on what the engine should recommend and where human judgment must remain final.
Escalation paths and ownership are defined early. This reduces adoption friction and protects clinical trust. At the same time, ambiguity is removed before development begins.
Step 3: Design Architecture and Governance
Architecture is established before intelligence is built. Under this step, our healthcare experts define the data flow, consent enforcement, access control, and auditability. At the same time, compliance is embedded directly into the design.
This avoids retrofitting controls later. As a result, the engine remains enterprise-ready as scale increases.
Step 4: Prepare and Unify Longitudinal Data
Recommendation quality depends on context. Data from multiple systems is normalized and unified into longitudinal patient views. Quality checks and lineage tracking are applied throughout. Incomplete or unreliable data does not move forward. This step sets the foundation for accurate decisions.
Step 5: Build and Validate Decision Intelligence
Models, rules, and decision logic are developed as a single system. Each recommendation is evaluated for accuracy, safety, and explainability.
Clinical and operational stakeholders review outputs before deployment. This shared validation builds confidence early. Complexity is avoided unless it adds clear value.
Step 6: Integrate into Real Workflows
Recommendations only matter when they fit existing work. Guidance is embedded directly into EHRs, care platforms, and patient-facing tools. Timing, channel, and role routing are configured carefully. This reduces alert fatigue and disruption. Adoption improves when workflows remain intact.
Step 7: Monitor Outcomes and Improve Continuously
Post-launch, usage patterns and outcomes are tracked closely. Overrides, performance drift, and bias are monitored across populations. Improvements are introduced in controlled cycles.
This keeps the system accurate over time. Continuous learning turns the engine into durable infrastructure.
This approach balances intelligence with governance. By structuring development into clear steps, enterprises gain recommendation engines that scale safely, earn trust, and deliver consistent impact without increasing operational complexity.
Cost To Build An AI Health Recommendation Engine
At Intellivon, AI health recommendation engines are built as regulated, enterprise-grade decision systems. Cost planning is tied to clinical impact, compliance exposure, and long-term scalability. The objective is to invest deliberately in safety, reliability, and measurable outcomes.
When budget constraints exist, scope is refined collaboratively. However, regulatory and governance requirements are never diluted. HIPAA and GDPR alignment, FDA and EU AI Act readiness, and enterprise-grade reliability remain intact throughout delivery. Each engagement balances cost discipline with sustainable compliance and long-term return on investment.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Compliance Alignment | Requirements analysis, regulatory mapping, and KPI definition | $6,000 – $12,000 |
| Architecture & Secure Design | Multi-layered design for PHI handling, encryption, and resilience | $8,000 – $15,000 |
| Data Integration & Interoperability | EHR, IoMT, claims, and lab integration via HL7/FHIR | $10,000 – $20,000 |
| AI Intelligence & Decision Layer | Predictive models, decision logic, and explainability controls | $12,000 – $25,000 |
| Security & Privacy Engineering | Encryption, access control, de-identification, and monitoring | $8,000 – $15,000 |
| Platform Development & Interfaces | Role-based dashboards, analytics, and audit reporting | $12,000 – $25,000 |
| Testing & Validation | Security testing, model validation, compliance checks | $6,000 – $10,000 |
| Deployment & Scaling | Cloud rollout, monitoring, and high availability | $6,000 – $12,000 |
Total initial investment: $50,000 – $150,000
Ongoing maintenance and optimization: 15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped programs face cost pressure if hidden factors are ignored. Planning for these early protects timelines and budgets.
- Integration complexity: Legacy EHRs and fragmented provider systems often require additional middleware and FHIR adapters.
- Compliance overhead: HIPAA, GDPR, FDA, and EU AI Act readiness demand recurring audits and documentation updates.
- Data governance: Cleaning, mapping, and curating mixed-format healthcare data requires ongoing effort.
- Cloud infrastructure spend: Real-time AI pipelines and monitoring dashboards must scale efficiently.
- Change management: Training clinical, operational, and compliance teams adds transition costs.
- Model drift and monitoring: Predictive models need periodic retraining and revalidation to remain accurate and compliant.
Best Practices to Avoid Budget Overruns
Based on Intellivon’s enterprise delivery experience, the following practices consistently lead to predictable costs and faster go-live.
- Start with a focused scope: Pilot within one department or care program, validate ROI, then scale.
- Embed compliance from day one: Align architecture early with HIPAA, GDPR, and FDA or EU AI Act requirements.
- Adopt modular design: Reuse secure pipelines, decision components, and dashboards across programs.
- Optimize cloud usage: Balance batch and real-time analytics to control compute costs.
- Ensure continuous observability: Track performance, compliance, and usage through automated dashboards.
- Iterate for longevity: Refine models, workflows, and controls regularly to maintain resilience.
Request a tailored proposal from Intellivon’s healthcare AI team, and receive a delivery roadmap aligned with your $50,000–$150,000 budget range, compliance priorities, and long-term growth strategy.
Challenges in AI Health Recommendation Engine Development
Enterprise-grade AI health recommendation engines fail more often due to execution gaps than technical limitations. At the same time, data realities, clinical adoption, regulatory exposure, and system integration all shape success. Additionally, addressing these challenges early determines whether the engine becomes trusted infrastructure or an unused layer.
Below are the most common challenges enterprises face, and how Intellivon addresses them in real deployments.
1. Fragmented and Inconsistent Data
Patient information lives across EHR modules, labs, claims systems, devices, and legacy platforms. Under these engines, formats differ, records overlap, and timelines break across care settings. At the same time, clinicians and systems must reconstruct context manually, which weakens decision accuracy. Additionally, recommendation engines built on partial data amplify this problem.
To address this, data unification is treated as a prerequisite, not a side task. Consequently, longitudinal patient views are created by normalizing codes, resolving identities, and validating completeness before intelligence is applied.
Quality thresholds determine what data moves forward. This ensures recommendations reflect the full context rather than fragmented snapshots.
2. Clinical Trust and Adoption Resistance
Clinical teams often resist systems that feel intrusive or opaque. Under this system, recommendations that appear without explanation or disrupt workflows are quickly ignored. At the same time, even accurate guidance fails if it interrupts care delivery. Additionally, adoption stalls when clinicians feel monitored rather than supported.
Trust is built by design and not through messaging. Under these engines, recommendations are ranked, contextual, and explainable. Additionally, each action includes reasoning that clinicians can review. At the same time, delivery is embedded inside existing workflows rather than added as a separate interface. This keeps judgment with clinicians while reducing cognitive load.
3. Compliance, Privacy, and Audit Readiness
Health recommendation engines operate under constant regulatory pressure. Under these systems, consent requirements, access controls, and audit obligations evolve across regions. Consequently, systems that treat compliance as a later phase expose enterprises to risk and rework. Additionally, regulatory gaps often surface only after deployment.
Governance is embedded directly into the architecture. Under this engine, consent validation, role-based access, and audit logging operate at every decision point. Data use is continuously monitored against policy. This approach keeps the engine audit-ready at scale and reduces long-term compliance costs.
4. Integration with Existing Systems
Many recommendation engines fail because they operate outside core systems. Under these systems, standalone tools force teams to switch contexts and duplicate effort. This increases friction and slows adoption. Enterprises need intelligence that fits into the systems already in use.
Integration is approached as orchestration, not replacement. Recommendations are delivered through APIs into EHRs, care management platforms, telehealth tools, and patient apps. Timing, routing, and role context are preserved. This keeps workflows intact while adding intelligence where it matters.
By addressing these challenges systematically, enterprises can deploy recommendation engines that scale safely, earn adoption, and deliver consistent value across care programs.
Conclusion
AI health recommendation engines are becoming foundational to how enterprises deliver consistent, high-quality care at scale. When built correctly, they reduce variability, support clinical judgment, and improve outcomes without adding operational strain. However, success depends on architecture, governance, and workflow alignment, not algorithms alone.
For organizations ready to move beyond pilots, the next step is intentional execution. With deep experience building enterprise-grade, compliant AI platforms, Intellivon helps healthcare leaders turn recommendation engines into durable decision infrastructure. This results in not just cost efficiency, but sustainable growth, predictable performance, and long-term trust across care programs.
Build Your AI Health Recommendation Engine with Intellivon
At Intellivon, we build AI health recommendation engines as long-term enterprise decision platforms, not experimental models or isolated features. Under our experts, each engine is designed to operate inside regulated healthcare environments, supporting clinical guidance, care orchestration, and engagement intelligence through a single governed architecture that integrates cleanly with existing systems.
Every solution is engineered for real-world scale and scrutiny. Here, delivery remains architecture-first and compliance-led, with privacy, consent, and auditability embedded directly into data pipelines and decision workflows. As deployment expands across care programs, regions, or populations, performance and governance remain predictable. This ensures recommendations drive measurable outcomes without increasing operational or regulatory risk.
Why Partner With Intellivon?
- Enterprise-grade recommendation engine design aligned with real clinical, operational, and payer workflows
- Proven interoperability across EHRs, care management systems, telehealth platforms, and secure integration layers
- Compliance-by-design architecture supporting HIPAA, GDPR, consent enforcement, audit readiness, and AI governance
- Explainable and controlled decision intelligence that supports clinicians without overriding judgment
- Scalable, cloud-native delivery with phased rollout, predictable growth, and continuous optimization
Book a strategy call to explore how an AI health recommendation engine can operate as a trusted decision infrastructure across your enterprise, with Intellivon as your long-term AI and compliance partner.
FAQs
Q1. What is an AI health recommendation engine used for in healthcare?
A1. An AI health recommendation engine helps healthcare enterprises deliver consistent, personalized guidance across prevention, treatment, and follow-up care. This system analyzes longitudinal clinical and behavioral data to recommend next best actions for patients, clinicians, and care teams.
These engines are commonly used to reduce care variability, improve adherence, and support decision-making at scale without increasing clinical workload.
Q2. How is an AI health recommendation engine different from clinical decision support systems?
A2. Traditional clinical decision support systems rely on static rules and alerts triggered by isolated events. Because of this, AI health recommendation engines evaluate patient context over time, including history, behavior, and outcomes.
They rank recommendations instead of firing alerts and adapt as conditions change. This makes them more suitable for complex, real-world enterprise care environments.
Q3. Are AI health recommendation engines HIPAA compliant?
A3. AI health recommendation engines can be HIPAA compliant when privacy, consent, and access controls are embedded into the architecture. Compliance depends on how data is ingested, processed, and audited. Enterprises typically require role-based access, encryption, consent enforcement, and full audit trails. Compliance must be designed in from the start, not added later.
Q4. What does it cost to build an AI health recommendation engine?
A4. For enterprises, the cost to build an AI health recommendation engine typically ranges from $50,000 to $150,000, depending on scope, integrations, and compliance requirements. Based on this, costs include architecture design, data integration, decision intelligence, security, and validation. Ongoing maintenance and optimization usually require 15–20% of the initial build annually.
Q5. How long does it take to deploy an AI health recommendation engine?
A5. Most enterprise deployments follow a phased rollout. Initial pilots can go live within a few months, while full-scale implementations take longer due to integration, governance, and validation. At the same time, timelines depend on data readiness, compliance needs, and workflow complexity. A phased approach helps enterprises show early value while scaling safely.