Healthcare is facing a crisis where patients often wait 2 to 3 months to see specialists. Clinical staff feel overwhelmed, with 93% reporting burnout. Rural communities find it hard to access even basic care. At the same time, traditional healthcare delivery methods can’t keep up with the growing demand for patients.
Telehealth apps are changing this situation. They reduce specialist wait times from months to days and lower hospital operating costs by up to 20%. Some remote patient monitoring programs return $130 for every $10 invested. With the telehealth market projected to reach $250 billion annually in the U.S., healthcare organizations are seeing that building these apps has become an essential part of modern care delivery.
At Intellivon, we have developed telehealth apps for growing enterprises facing this change. Our teams design AI-driven virtual care ecosystems where telehealth becomes a seamless part of everyday clinical operations. This blog is based on that experience. It outlines our entire development process from scratch, including important clinical features, compliance rules like HIPAA and GDPR, and strategies for effective scaling.
Key Takeaways Of The Telehealth App Market
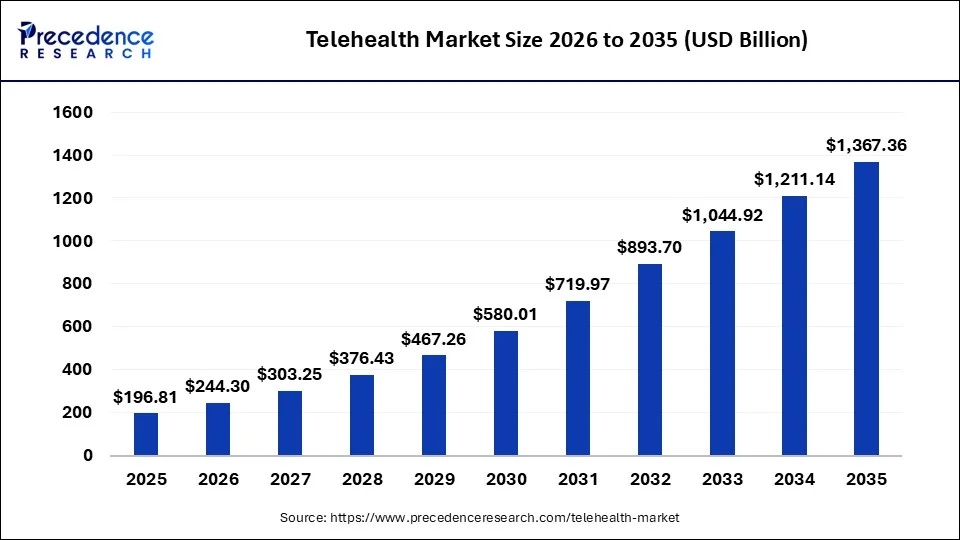
According to Grand View Research, the global telehealth market reached approximately USD 123 billion in 2024 and is projected to cross USD 455 billion by 2030. Growth is tracking at an annual rate of nearly 25% over the forecast period. More importantly, utilization has stabilized at scale rather than declining.
This confirms that virtual care is now operationally embedded within mainstream healthcare delivery.
Key Market Insights
- The global telehealth market is estimated at USD 120–130 billion in 2024 and is expected to reach USD 400–455+ billion by 2030, depending on scope definitions and segments included.
- Compound annual growth rates range from 11.5 % to nearly 25%, driven by broadband expansion, smartphone adoption, and the maturation of digital care reimbursement frameworks.
- Virtual care platforms represent a smaller but faster-growing segment. This category is valued at approximately USD 13–15 billion in 2024 and is projected to exceed USD 110–247 billion by the early 2030s, with 25–30 % annual growth.
- Post-pandemic utilization remains consistently high. Large healthcare networks now report more than one million virtual visits annually across nationwide footprints.
- Patient loyalty remains strong. Nearly nine in ten patients indicate a preference to continue using virtual care for future healthcare interactions.
- Provider adoption has moved beyond pilots. Enterprise-wide deployment is now common, with centralized virtual care hubs, RPM programs, and AI-driven population health models becoming standard operating practice.
From a business standpoint, these market signals explain why large healthcare enterprises are entering this space aggressively. Unified telehealth and virtual care platforms are now treated as long-term infrastructure investments that directly influence utilization control, workforce efficiency, and revenue protection.
Well-executed enterprise virtual care programs are already delivering 15–30% reductions in avoidable admissions, 20–40% improvements in patient engagement, and measurable operating margin expansion within the first 18–24 months, making the ROI case increasingly difficult to ignore.
What Is a Telehealth App?
A telehealth app is a digital platform that enables care delivery beyond physical facilities. It connects patients, clinicians, and care teams through secure digital channels. However, at the enterprise level, it serves a broader operational role. It governs how care is accessed, delivered, and followed up across populations.
In practice, modern telehealth apps support digital intake, virtual consultations, and remote monitoring within one coordinated system. In addition, they enable structured follow-ups and escalation workflows. As a result, care teams gain continuous visibility instead of fragmented data points. This continuity directly influences clinical outcomes and operational efficiency.
From an enterprise standpoint, a telehealth app also enforces governance. It manages identity, consent, workflows, and data security across services. Therefore, organizations can scale virtual care without increasing compliance risk. This control becomes critical as volumes grow.
Ultimately, telehealth apps function as operating layers. They sit between patients and clinical systems. When designed correctly, they extend care capacity, reduce avoidable utilization, and support long-term delivery strategies.
Telehealth vs Telemedicine vs Virtual Care
These terms are often used interchangeably. However, they represent different scopes of care delivery. For enterprise teams, this distinction is not semantic. It directly affects platform architecture, compliance design, and long-term scalability.
Telemedicine focuses on replacing in-person visits. At the same time, telehealth expands into broader digital services. On the other hand, virtual care goes further by reshaping how care is delivered across time, settings, and populations. Understanding these differences early prevents costly redesigns later.
Comparison of Care Models
| Dimension | Telemedicine | Telehealth | Virtual Care |
| Primary purpose | One-to-one clinical visits | Digital health services | Continuous care delivery model |
| Typical use case | Video consultation for acute issues | Consults, education, follow-ups | Ongoing monitoring and care orchestration |
| Scope of care | Episodic | Multi-touch but fragmented | Longitudinal and coordinated |
| Technology focus | Video and scheduling | Video, messaging, basic RPM | Platforms, workflows, data integration |
| Enterprise readiness | Low | Moderate | High |
| Example | Virtual urgent care visit | Teleconsult plus follow-up chat | RPM-driven chronic care program |
In real-world deployments, many organizations start with telemedicine. Over time, they add telehealth features. Eventually, they shift toward virtual care as complexity increases. Each stage introduces new operational demands.
Why This Distinction Matters During Development
Development decisions change significantly based on the chosen model. Telemedicine apps can rely on simple workflows. Telehealth platforms require broader integration and security controls. Virtual care systems demand orchestration across data, teams, and timelines.
In the context of building a telehealth app, aiming for virtual care readiness from the start protects long-term investment. It allows organizations to evolve without rebuilding core infrastructure later.
Types of Telehealth Apps You Can Build
Enterprises adopt different telehealth models based on care scope, risk exposure, and operational maturity. Therefore, selecting the right model early shapes architecture, investment, and timelines.
Each category increases complexity in a predictable way. Understanding this progression helps leaders avoid underbuilding or overengineering. It also clarifies when a platform must evolve.
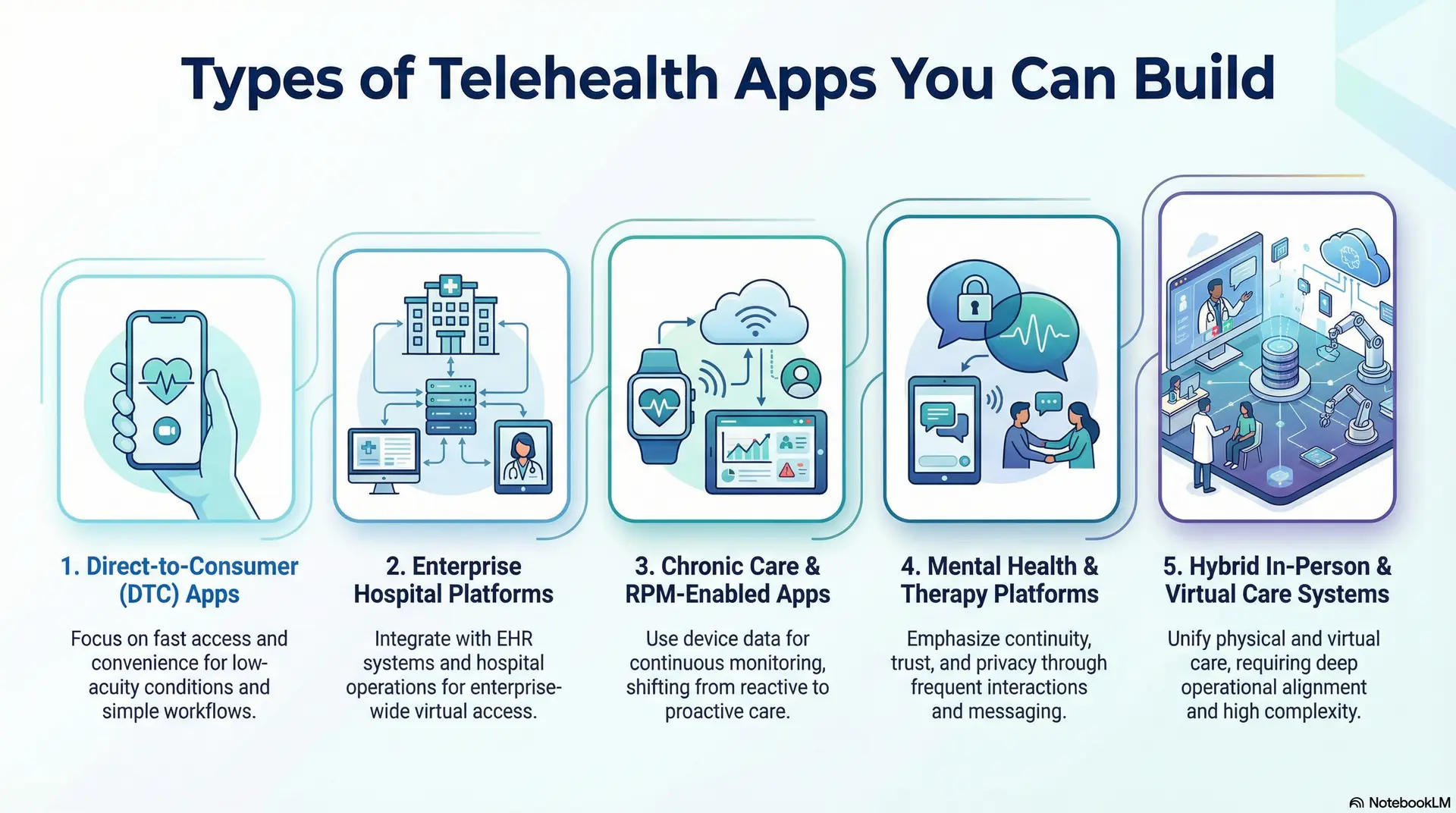
1. Direct-to-Consumer (DTC) Telehealth Apps
DTC telehealth apps focus on fast access and convenience. They typically support virtual consultations, scheduling, and basic prescriptions. As a result, they work well for low-acuity conditions and self-directed care.
However, clinical workflows remain relatively simple. Integration requirements also stay limited. This model suits organizations testing digital demand or launching new services quickly.
2. Enterprise Hospital Telehealth Platforms
Enterprise hospital platforms extend beyond virtual visits. They integrate with EHR systems, clinician workflows, and hospital operations. Therefore, governance and interoperability become central design concerns.
These platforms often support multiple departments and care pathways. As usage grows, reliability and compliance requirements increase. This model fits health systems seeking enterprise-wide virtual access.
3. RPM-Enabled Telehealth Apps
Chronic care platforms introduce continuous monitoring into virtual care. They ingest data from devices and trigger escalation workflows. As a result, care teams shift from reactive visits to proactive intervention.
This model requires stronger data pipelines and analytics. It also demands clear clinical thresholds and ownership. Complexity increases due to longitudinal care responsibility.
4. Mental Health and Therapy Platforms
Mental health platforms emphasize continuity and trust. They support frequent interactions, messaging, and structured care plans. Therefore, engagement and privacy controls become critical.
These apps often require flexible scheduling and asynchronous communication. Regulatory sensitivity also increases across regions. This model suits organizations focused on behavioral health access and retention.
5. Hybrid In-Person and Virtual Care Systems
Hybrid platforms unify physical and virtual care delivery. They coordinate visits, diagnostics, and follow-ups across settings. As a result, operational alignment becomes essential. These systems demand deep integration with on-site workflows.
They also require consistent data visibility across teams. This model represents the highest complexity but offers the greatest flexibility.
When to Choose Each Model
Complexity rises as care becomes continuous and integrated. During these situations, DTC apps offer speed with a limited scope. At the same time, hospital platforms add governance and scale, chronic and mental health models introduce longitudinal responsibility, and hybrid systems combine all layers into one operating model.
For enterprises, the right choice depends on strategic intent. Short-term access goals require simpler builds. Long-term care transformation demands robust platforms. Clarity here prevents costly redesigns later.
How Virtual Telehealth Care Platforms Reduce Hospital Admissions by 50%
Hospital admissions remain one of the most expensive breakdowns in any care delivery system. They consume limited bed capacity and increase payer exposure. They also introduce avoidable clinical risk when the intervention comes too late. Virtual telehealth care platforms address this problem upstream.
By replacing episodic visits with continuous digital oversight, care teams intervene earlier. As a result, admissions, readmissions, and inpatient length of stay decline in a sustained way.
For enterprises evaluating how to build a telehealth app, these outcomes emerge from deliberate platform design that prioritizes continuity, visibility, and escalation control.
1. Integrated Virtual Care for High-Risk Populations
Admission reduction accelerates when virtual care focuses on high-risk patients. Large-scale programs offer a clear signal here. One such initiative, MeCare, demonstrates how integrated virtual care changes chronic disease management outcomes. After enrollment, emergency department presentations declined by 76%. Hospital admissions also fell by 50%.
In addition, the average inpatient length of stay dropped by 12%. This eased pressure on beds and reduced operational strain across clinical teams. These gains matter because they compound across populations, not just individual cases.
Importantly, the financial impact remained positive even after operating costs were included. The program delivered a median net savings of approximately A$ 982 per patient per month. This result highlights a critical lesson for platform builders. Sustained admission reduction comes from continuous virtual oversight, not isolated teleconsultations or appointment-based care.
2. Remote Monitoring to Prevent Acute Deterioration
Remote monitoring becomes most valuable when it prevents deterioration before escalation. This is where telehealth app architecture directly influences outcomes. Evidence from a US cost-utility study on remote pulse-oximetry monitoring for moderately ill COVID-19 patients illustrates this clearly. Patients managed through home-based monitoring experienced an 87% reduction in hospitalizations. Mortality also declined by 77% compared with usual care.
From a financial standpoint, the impact was equally significant. The intervention delivered average savings of US$11,472 per patient within a three-week period. At the same time, quality-adjusted life years improved. These results reinforce why real-time physiological data ingestion must sit at the core of a telehealth platform, not as an add-on feature.
3. Postpartum Hypertension and Readmission Prevention
Targeted virtual care programs show strong results in high-risk, time-sensitive populations. Postpartum hypertension is a clear example. In a hospital-led telehealth and remote patient monitoring program, readmission rates declined from 3.7% to 0.5%. These outcomes were reported in PubMed-indexed clinical studies.
The model combined frequent digital check-ins with automated blood pressure data ingestion. It also included rapid escalation pathways when thresholds were breached. This structure matters because it removes delay from decision-making. Care teams act on signals, not symptoms alone.
For organizations building telehealth apps, this demonstrates how focused program design can neutralize one of the most persistent drivers of early readmissions.
These outcomes explain why leading health systems no longer treat virtual care as a digital add-on. They view it as admission-reduction infrastructure. When telehealth platforms are built around continuous oversight, escalation logic, and real-time data flows, they reclaim inpatient capacity. They also deliver recurring cost savings that compound month after month.
Core Features of an Enterprise-Grade Telehealth App
A telehealth app succeeds or fails based on how its features support real clinical and operational workflows. At the enterprise level, features are not standalone capabilities. They function as coordinated controls across access, care delivery, and governance.
Therefore, each feature must align with compliance, scalability, and accountability requirements. This section breaks down the core feature sets required for enterprise-grade telehealth platforms.
1. Patient-Facing Features
Patient-facing features shape adoption, trust, and continuity of care. However, in enterprise environments, they must also support downstream clinical workflows. Design decisions here directly affect data quality and escalation speed.
Therefore, simplicity at the interface level must coexist with rigor behind the scenes. Each feature below plays a specific role in that balance.
1. Secure Onboarding and Identity Verification
Secure onboarding establishes trust from the first interaction. It verifies patient identity while minimizing friction. Enterprise platforms often combine document verification, biometric checks, and secure authentication.
As a result, patient records remain accurate across systems. This foundation prevents downstream errors and compliance exposure.
2. Smart Intake and Symptom Capture
Smart intake replaces unstructured conversations with guided data collection. Patients enter symptoms, history, and risk indicators through adaptive forms. Therefore, clinicians receive structured, review-ready information.
This reduces consultation time and improves triage accuracy. Over time, it also supports population-level analytics.
3. Appointment Scheduling
Scheduling must balance patient convenience with clinical availability. Enterprise telehealth apps integrate calendars across departments and providers. As a result, capacity utilization improves without manual coordination.
Automated reminders reduce no-shows and rescheduling overhead. This feature directly impacts operational efficiency.
4. Video Consultations
Video consultations enable real-time clinical interaction. However, enterprise platforms require more than stable connections. They must support documentation, consent capture, and session auditing.
Therefore, video becomes part of a governed workflow. This ensures clinical continuity and compliance across visits.
5. Prescriptions, Care Plans, and Follow-Ups
Post-consultation actions define care quality. Telehealth apps must support digital prescriptions, care plans, and follow-up tasks.
As a result, care continues beyond the visit itself. Automated follow-ups reinforce adherence and engagement. This feature closes the loop in virtual care delivery.
2. Clinician-Facing Features
Clinician-facing features determine adoption among care teams. They must reduce cognitive load while improving decision-making. Therefore, usability and clarity become critical at scale. These features also influence throughput and care quality. Each component below supports clinical efficiency and safety.
A. Clinical Dashboards
Dashboards provide a consolidated view of patient status. They surface priorities, alerts, and upcoming tasks.
As a result, clinicians spend less time searching for information. Dashboards also support role-based views across specialties. This improves coordination within care teams.
B. Structured Patient Data Views
Structured data views replace fragmented records. They present symptoms, vitals, and history in a consistent format.
Therefore, clinicians assess risk faster and with greater confidence. These views also support decision support tools. Over time, they enable better outcomes analysis.
C. Documentation and Notes
Documentation remains a core clinical requirement. Telehealth platforms must support structured and free-text notes.
As a result, clinicians document efficiently without disrupting care flow. Notes integrate directly into enterprise records. This ensures continuity across virtual and in-person settings.
D. Escalation and Referral Workflows
Escalation workflows manage risk when conditions worsen. They route cases to specialists or in-person care. Therefore, response times improve during critical moments.
Referral tracking ensures accountability across teams. This feature protects patient safety at scale.
3. Admin and Operations Features
Admin and operations features enable governance and scale. They ensure the platform remains compliant and auditable. Without these controls, growth introduces risk instead of value.
Therefore, these features form the backbone of enterprise telehealth platforms. Each supports oversight and decision-making.
A. Role-Based Access Control
Role-based access defines who can see and do what. It aligns permissions with responsibilities across teams.
As a result, sensitive data remains protected. Access policies also support regulatory requirements. This feature is essential for enterprise compliance.
B. Audit Logs
Audit logs create a traceable record of activity. They track access, changes, and clinical actions.
Therefore, organizations maintain accountability. Logs also support investigations and audits. This feature builds trust with regulators and partners.
C. Billing and Reimbursement Logic
Billing logic connects care delivery to revenue. Telehealth apps must support multiple reimbursement models.
As a result, financial operations remain accurate. Automated billing reduces manual errors. This feature protects margins as volume grows.
D. Analytics and Reporting
Analytics transform operational data into insight. They track utilization, outcomes, and efficiency. Therefore, leaders make informed decisions.
Reporting also supports compliance and performance monitoring. This feature enables continuous improvement.
Core features define how telehealth platforms perform under real conditions. They influence adoption, outcomes, and scalability. Therefore, enterprises must view features as system controls, not checklists. When designed together, these capabilities enable sustainable virtual care. This foundation supports growth while managing risk.
Enterprise-Grade Telehealth App Architecture
Architecture determines whether a telehealth app scales cleanly or collapses under pressure. At the enterprise level, architecture is not a technical afterthought. It defines how care workflows, data, and compliance interact.
Therefore, each layer must be clearly separated yet tightly coordinated. This structure reduces risk while supporting long-term growth.
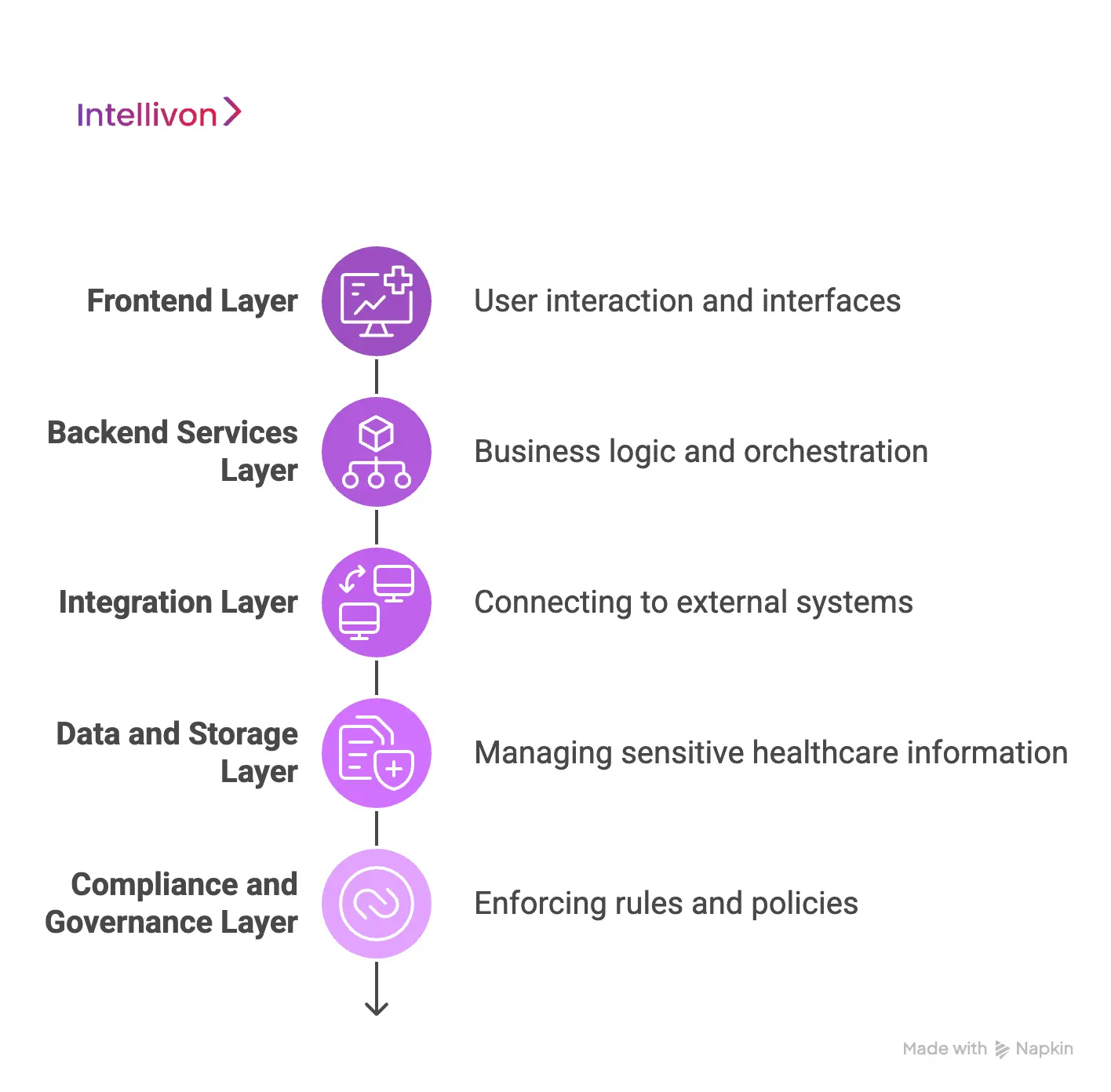
1. Frontend Layer
The frontend layer defines how users interact with the platform. It includes all interfaces used by patients, clinicians, and administrators. Therefore, this layer must balance usability with security. Design decisions here directly affect adoption and efficiency. A well-built frontend simplifies complex workflows without hiding critical controls.
What happens here
- Patients access care, submit data, and attend visits
- Clinicians review information and manage sessions
- Admin teams monitor operations and configurations
Common technologies
- React, Angular, Vue for web interfaces
- Swift and Kotlin for native mobile apps
- Design systems and accessibility frameworks
2. Backend Services Layer
The backend services layer handles business logic and orchestration. It processes requests, enforces workflows, and manages system behavior. Therefore, reliability and scalability become critical.
This layer connects user actions to data and integrations. Poor design here leads to bottlenecks and operational failure.
What happens here
- Scheduling and availability management
- Video, chat, and asynchronous messaging
- Clinical workflow execution and rules
Common technologies
- Node.js, Java, or .NET for service logic
- Microservices and API gateways
- Message queues and event brokers
3. Integration Layer
The integration layer connects the telehealth platform to external systems. It ensures data flows reliably across the healthcare ecosystem. Therefore, interoperability and error handling are essential.
This layer often determines enterprise readiness. Without strong integration, virtual care remains siloed.
What happens here
- Exchange with EHR and EMR systems
- Lab, diagnostic, and pharmacy connectivity
- Payment and billing coordination
Common technologies
- HL7, FHIR, and healthcare APIs
- Integration platforms and middleware
- Secure API management tools
4. Data and Storage Layer
The data and storage layer manages sensitive healthcare information. It stores patient records, session data, and operational logs. Therefore, security and performance must coexist.
This layer also supports analytics and reporting. Design choices here affect compliance and insight quality.
What happens here
- PHI storage and retrieval
- Encryption and key management
- Data separation across tenants
Common technologies
- Encrypted relational and NoSQL databases
- Cloud storage with access controls
- Key management and encryption services
5. Compliance and Governance Layer
The compliance and governance layer enforces rules across the platform. It controls identity, access, and policy execution.
Therefore, this layer protects the organization at scale. It also enables audit readiness and regulatory alignment. Without it, growth introduces unacceptable risk.
What happens here
- User identity and access management
- Consent tracking and enforcement
- Audit logging and policy controls
Common technologies
- IAM platforms and authentication services
- Consent management frameworks
- Audit and policy engines
Enterprise telehealth platforms succeed when architecture supports reality. Each layer must work independently yet remain coordinated. Therefore, shortcuts create long-term constraints. A layered approach enables scalability, compliance, and resilience. This foundation turns telehealth into durable infrastructure.
Telehealth App Compliance & Regulatory Requirements
Compliance defines whether a telehealth app can operate at enterprise scale. It shapes architecture, workflows, and data handling decisions. Therefore, regulatory requirements cannot be treated as legal checklists.
They influence trust, adoption, and long-term viability. This section outlines the core compliance domains every enterprise telehealth platform must address.
1. HIPAA Compliance (United States)
HIPAA governs how protected health information is accessed, stored, and shared. Telehealth apps must enforce safeguards across technical and operational layers. Therefore, access controls, encryption, and audit trails are mandatory.
Breaches expose organizations to regulatory penalties and reputational damage. Compliance also requires clear accountability across vendors and systems.
2. GDPR and International Data Regulations
GDPR reshapes how personal health data is processed across regions. It emphasizes data minimization, transparency, and user rights. Therefore, telehealth apps must support consent withdrawal and data access requests.
Cross-border operations increase complexity further. Compliance here affects global scalability and deployment strategy.
3. Consent Management and Patient Rights
Consent governs when and how care interactions occur. Telehealth apps must capture, store, and enforce consent digitally.
Therefore, consent logic must integrate directly into workflows. Patient rights include access, correction, and revocation. Weak consent handling creates legal and ethical risk.
4. Data Residency and Cross-Border Access
Data residency laws restrict where health data can be stored. Telehealth platforms operating globally must respect local requirements. Therefore, data architecture must support regional segregation.
Cross-border access requires strict controls and justification. This layer protects organizations from jurisdictional violations.
5. Audit Readiness and Reporting
Audit readiness ensures organizations can demonstrate compliance at any time. Telehealth apps must log actions, access, and changes systematically. Therefore, reporting cannot be manual or fragmented.
Automated audit trails reduce operational burden. They also support payer and regulator reviews.
Compliance cannot be bolted onto a live platform. Retrofitting controls introduces cost, delay, and risk. Therefore, compliance must guide architecture from the start. Early design choices determine audit readiness and scalability. Enterprises that design for compliance move faster with confidence.
Step-by-Step Telehealth App Development Process
Telehealth platforms succeed when the build follows clinical reality, not software habits. Enterprises need alignment across care teams, operations, and risk owners. Therefore, the development process must create clarity before code is written. Each step below reduces rework, compliance exposure, and adoption friction.
Intellivon applies this approach to deliver controlled rollouts that scale. The goal stays simple: predictable outcomes with enterprise-grade execution.
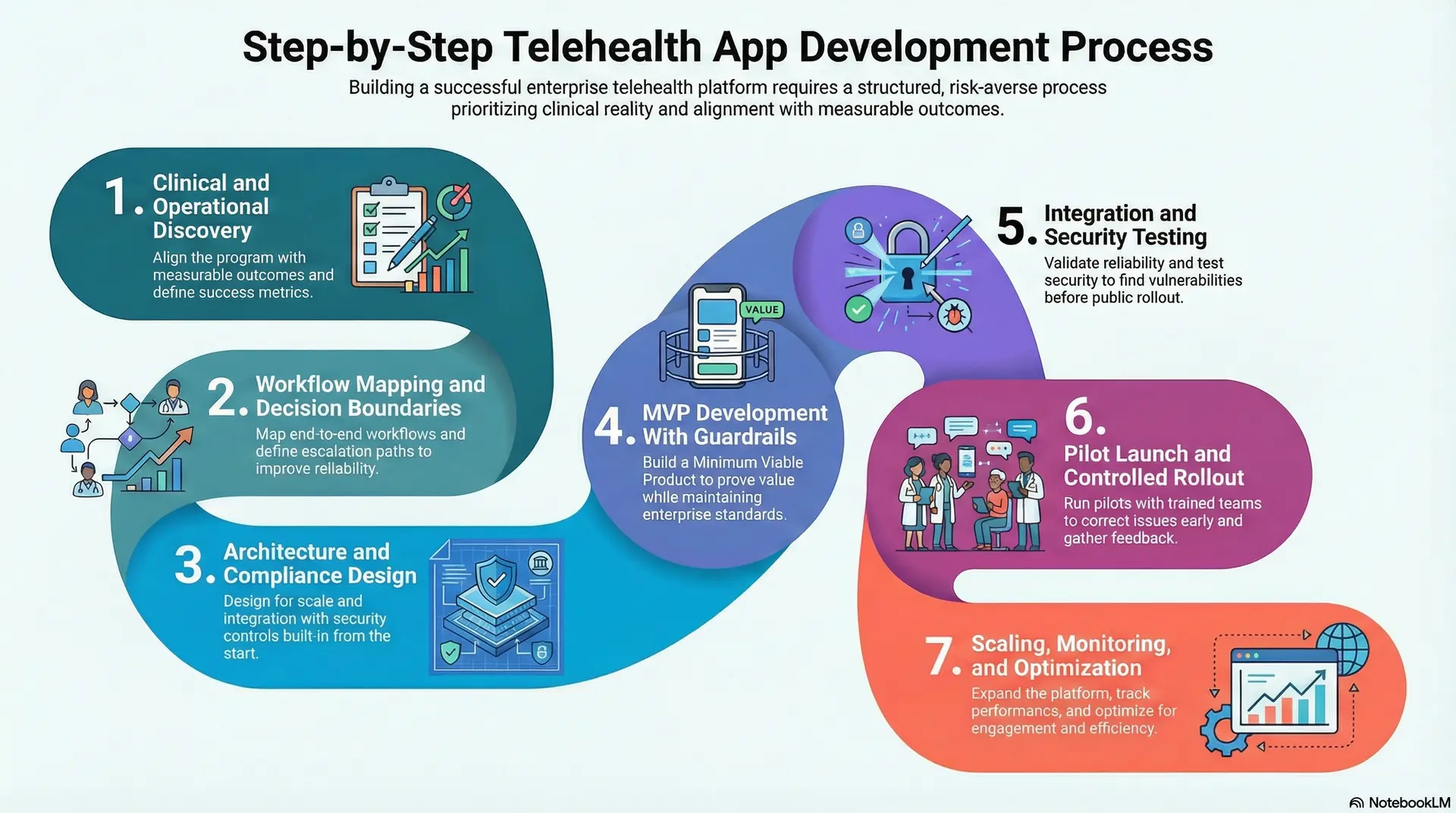
1. Clinical and Operational Discovery
Intellivon starts by aligning the program with measurable clinical and business outcomes. The team interviews clinical leaders, operations, and compliance stakeholders. Therefore, assumptions are replaced with workflow evidence and real constraints.
Discovery also clarifies patient cohorts, acuity levels, and service boundaries. In addition, success metrics are defined for access, quality, and cost. This stage sets the decision framework for every build choice.
2. Workflow Mapping and Decision Boundaries
We map end-to-end workflows across intake, triage, consults, and follow-ups. The team identifies decision points that require human judgment. Therefore, automation stays safe and clinically appropriate.
Escalation paths are defined for deterioration, non-adherence, and red flags. In addition, ownership is assigned across teams to avoid gaps. This step reduces risk and improves operational reliability.
3. Architecture and Compliance Design
Our experts design the architecture around scale, integration, and regulatory controls. Security and compliance requirements are translated into technical guardrails. Therefore, controls are built into the platform, not layered later. Data flows are defined across EHRs, devices, and analytics systems.
In addition, consent, auditability, and access policies are formalized. This stage creates a foundation that survives audits and growth.
4. MVP Development With Guardrails
Intellivon builds the MVP to prove value without introducing uncontrolled risk. Feature scope is tied to defined workflows and measurable outcomes. Therefore, the MVP ships with governance, logging, and role controls.
Critical integrations are prioritized to avoid isolated pilots. In addition, usability is tested with real clinical users. This approach creates momentum while protecting enterprise standards.
5. Integration and Security Testing
Our healthcare app engineers validate integration reliability under realistic load conditions. Security testing covers identity, access, and data protection controls. Therefore, vulnerabilities are found before rollout, not after incidents.
Clinical workflows are tested for edge cases and escalation accuracy. In addition, audit logs and reporting are verified for completeness. This step ensures the platform behaves predictably in production.
6. Pilot Launch and Controlled Rollout
Intellivon runs pilots with clear cohort selection and operational readiness checks. Care teams receive training aligned with actual workflows. Therefore, adoption issues surface early and can be corrected quickly. Rollout plans include escalation support and performance monitoring.
In addition, feedback loops are structured and time-bound. This controlled approach prevents scale from amplifying early mistakes.
7. Scaling, Monitoring, and Optimization
We scale platforms through phased expansion across regions, services, or populations. Monitoring tracks uptime, response times, and clinical workflow performance. Therefore, leaders can see impact trends and operational bottlenecks. Optimization focuses on throughput, engagement, and avoidable utilization reduction.
In addition, governance evolves with new regulations and program scope. This step turns a launch into durable infrastructure.
Cost to Build an Enterprise-Grade Telehealth App
At Intellivon, enterprise telehealth apps are built as regulated care delivery platforms. They are not treated as lightweight virtual tools. Therefore, cost planning aligns with clinical risk, compliance exposure, and long-term scalability. The objective is deliberate investment in safety, reliability, and operational readiness. Budgets are structured for real healthcare environments, not short-term pilots.
When budget constraints exist, scope is refined collaboratively with stakeholders. However, regulatory, security, and governance requirements are never compromised. HIPAA, GDPR, and regional healthcare regulations remain enforced throughout delivery. Therefore, architecture and compliance decisions stay protected from day one. This approach balances cost discipline with sustainable compliance and long-term ROI.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Compliance Alignment | Care model definition, requirements analysis, regulatory mapping, and KPI alignment | $6,000 – $12,000 |
| Architecture & Secure Platform Design | Scalable architecture, PHI segregation, encryption strategy, and resilience planning | $8,000 – $15,000 |
| Workflow Mapping & Clinical Logic | Clinical workflows, triage rules, escalation paths, and care journeys | $8,000 – $14,000 |
| Backend & Integration Development | EHR, pharmacy, labs, billing, and third-party integrations | $12,000 – $22,000 |
| Frontend & Role-Based Interfaces | Patient, clinician, and admin dashboards with usability controls | $10,000 – $20,000 |
| Security & Privacy Engineering | Encryption, access control, audit logs, monitoring, and threat detection | $8,000 – $15,000 |
| Testing & Compliance Validation | Security testing, workflow validation, and audit readiness checks | $6,000 – $10,000 |
| Deployment & Scalability Setup | Cloud deployment, monitoring, high availability, and performance tuning | $6,000 – $12,000 |
Total initial investment: $50,000 – $150,000
Ongoing maintenance and optimization: 15–20% of initial build annually
Hidden Costs Enterprises Should Plan For
Even well-scoped telehealth programs face pressure when hidden costs are ignored. Therefore, planning for these early protects timelines and budgets. Common hidden cost drivers include:
- Integration complexity increases due to legacy EHR systems and a fragmented healthcare infrastructure
- Compliance overhead grows with recurring audits, reporting requirements, and regulatory updates
- Data governance requires continuous cleaning, mapping, and standardization across systems
- Cloud infrastructure costs rise with real-time video, monitoring, and analytics workloads
- Change management includes clinician, operations, and compliance training efforts
- Monitoring and optimization remain ongoing as usage patterns and regulations evolve
These costs compound over time if left unmanaged. They must be planned deliberately, not absorbed reactively.
Best Practices to Avoid Budget Overruns
Predictable telehealth costs require discipline from the first design decision. Therefore, successful enterprise programs follow proven cost-control practices:
- Start with a focused scope and validate outcomes before scaling across populations
- Embed compliance directly into the platform architecture instead of retrofitting controls
- Use modular components that can be reused across multiple care programs
- Optimize cloud usage by balancing real-time workloads with batch processing
- Maintain continuous observability across performance, security, and compliance metrics
- Plan for long-term platform evolution, not just initial deployment
This approach stabilizes delivery, protects budgets, and preserves enterprise investment as care models change.
Request a tailored proposal from Intellivon’s healthcare team to receive a delivery roadmap aligned with your $50,000–$150,000 budget, compliance priorities, and long-term growth strategy.
Common Mistakes When Building Telehealth Apps
Many telehealth initiatives fail even with strong budgets and executive support. The issues usually surface after launch, not during planning. Early design decisions compound once usage, regulation, and scale increase. As a result, platforms struggle under real clinical and operational pressure.
These failures are avoidable with the right execution model. Below are the most common mistakes enterprises make and how we address them correctly.
1. Treating Telehealth as a Video Application
Many teams approach telehealth as a video-first solution. They prioritize calls while ignoring intake, follow-ups, and escalation workflows. As a result, care remains episodic and reactive. Clinical teams lack visibility beyond the visit itself.
A platform-led approach reframes telehealth as continuous care delivery. This structure ensures accountability before, during, and after each interaction.
2. Ignoring Real Clinical Workflow Complexity
Some platforms are designed without validating real clinical workflows. On paper, the system appears functional and efficient. However, daily use exposes gaps that force manual workarounds.
Clinicians then lose trust in the platform. Workflow-first discovery aligns the system with real care delivery. This alignment supports adoption and long-term reliability.
3. Underestimating Compliance
Compliance is often treated as a late-stage checkbox. Teams assume security features can be added after launch. This creates risk when audits, expansion, or incidents occur.
Retrofitting controls increases cost and delays timelines. A compliance-by-design model embeds regulation into architecture early. This protects speed while maintaining regulatory confidence.
4. Building Without an Integration Strategy
Telehealth apps often launch in isolation from core systems. EHRs, labs, and billing platforms are added later under pressure. As a result, data becomes fragmented and unreliable.
Operations then depend on manual reconciliation. An integration-first strategy connects systems from the start. This allows virtual care to operate as part of the enterprise ecosystem.
5. Scaling Before Governance Is Established
Some organizations scale telehealth usage before governance matures. Access controls, audit logs, and ownership remain unclear. Therefore, risk increases as adoption grows. Small issues become systemic failures.
Governance-first execution establishes controls before expansion. This enables growth without operational or compliance exposure.
6. Optimizing for Launch Instead of Longevity
Short-term launches often drive feature-heavy builds. However, long-term maintenance and evolution are ignored. As regulations and care models change, platforms struggle to adapt.
Technical debt accumulates quickly. A long-horizon design approach plans for change from day one. This protects enterprise investment beyond initial deployment.
Telehealth failures rarely stem from la ack of technology. They emerge from misaligned design and execution choices. Each mistake compounds as complexity increases.
Therefore, prevention matters more than correction. The right delivery approach emphasizes workflows, compliance, and scalability together. This is how telehealth platforms deliver durable enterprise value.
Conclusion
Enterprise telehealth platforms succeed when strategy, architecture, and compliance align from the first design decision. When built correctly, telehealth becomes an infrastructure that reduces admissions, protects margins, and supports long-term care delivery models. However, reaching that outcome requires discipline across workflows, integrations, governance, and continuous optimization as scale increases.
This is where an experienced enterprise delivery partner matters, guiding execution with clarity, accountability, and measurable business outcomes. Intellivon helps healthcare enterprises build telehealth platforms designed to scale safely, comply globally, and deliver durable operational value. The result is confident growth, predictable ROI, and virtual care systems that leaders can trust globally.
Build An Enterprise-Grase Telehealth App With Intellivon
At Intellivon, telehealth apps are built as enterprise care delivery platforms, not standalone virtual tools. The focus remains on compliance, scalability, and operational control from day one.
Every solution is designed for real-world healthcare complexity. Architecture stays compliance-led, with privacy, consent, and auditability embedded directly into workflows. As deployments expand across regions, care models, or populations, governance and performance remain stable. This ensures telehealth platforms scale without increasing clinical or regulatory risk.
Why Partner With Intellivon?
- Enterprise-grade telehealth platform design aligned with real clinical and operational workflows
- Proven experience integrating telehealth with EHRs, labs, pharmacies, and payer systems
- Compliance-by-design architecture supporting HIPAA, GDPR, consent enforcement, and audit readiness
- Secure role-based access control and full auditability across patient and provider actions
- AI-assisted workflows that support triage, documentation, and care continuity are responsible
- Cloud-native architecture built for high availability, resilience, and regional scalability
- Modular delivery approach enabling phased rollout and controlled expansion
- Continuous optimization framework covering performance, compliance, and adoption metrics
Book a strategy call to explore how an enterprise-grade telehealth app can operate as a trusted care delivery platform across your organization, with Intellivon as your long-term technology and compliance partner.
FAQs
Q1. What is a telehealth app, and how does it work?
A1. A telehealth app enables remote healthcare services through digital platforms. It supports virtual consultations, patient intake, documentation, and follow-ups. Enterprise telehealth apps also integrate compliance, workflows, and healthcare systems to deliver care safely at scale.
Q2. How much does it cost to develop a telehealth app?
A2. Enterprise-grade telehealth app development typically costs between $50,000 and $150,000. Costs depend on compliance requirements, integrations, AI features, and scalability needs. Ongoing maintenance usually adds 15–20% annually.
Q3. What features are essential in a telehealth app?
A3. Core features include secure video consultations, digital intake, provider dashboards, compliance controls, and system integrations. Enterprise platforms also require audit logs, role-based access, and care continuity workflows to operate reliably.
Q4. Are telehealth apps required to be HIPAA compliant?
A4. Yes, telehealth apps handling patient data in the US must comply with HIPAA. Compliance includes encryption, access control, auditability, and breach safeguards. Similar regulations apply globally, such as GDPR in the EU.
Q5. How is AI used in telehealth app development?
A5. AI assists telehealth apps through smart triage, documentation support, risk scoring, and operational analytics. It works within defined guardrails and supports clinicians rather than replacing clinical judgment.