Most organizations looking into a doctor consultation app are dealing with real operational challenges, like access gaps, limited clinician availability, and complicated compliance requirements. Meanwhile, patient expectations are shifting toward quicker, easier access without sacrificing trust or care quality.
In this context, a doctor consultation app acts as a layer for clinical interactions that connects scheduling, identity management, medical records, consent, documentation, and post-consultation tasks. Every design choice has an impact later on. Risk exposure, clinical reliability, and long-term scalability are determined early, often before the first consultation takes place.
This article examines doctor consultation app development from the ground up. It explores how these platforms function in regulated environments, how they fit in with current healthcare systems, and how they should be designed for long-lasting use rather than just temporary adoption. This view draws on Intellivon’s experience in delivering healthcare platforms where clinical workflows, AI-driven intelligence, compliance needs, and scalability must function together without adding operational risk.
Why Should You Invest in Doctor Consultation Apps Now
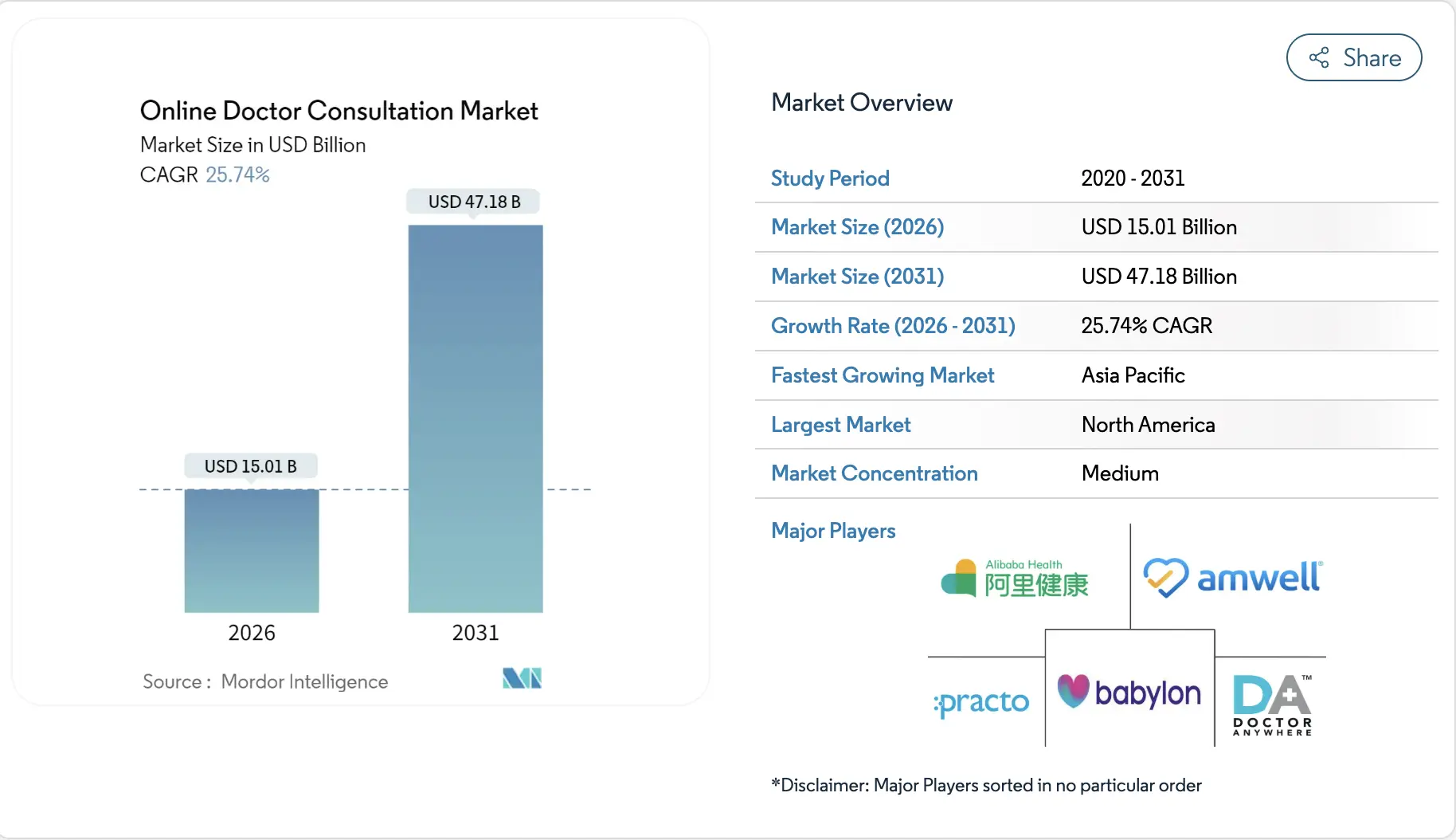
The online doctor consultation market is expected to reach USD 15.01 billion in 2026, up from USD 11.93 billion in 2025. By 2031, the market is projected to reach USD 47.18 billion. This reflects a compound annual growth rate of 25.74 percent between 2026 and 2031.
Growth Drivers:
- Smartphone penetration and chronic disease rise propel 12.1% CAGR for virtual consultations, expanding from USD 13.8 billion.
- Patient convenience and cost-efficiency cut travel/waiting times, saving USD 176-223 per cancer visit and USD 235 per digital encounter.
- Tech advances (AI, video tools) and government policies drive Asia-Pacific at the fastest pace, with video holding 60% share.
- Mental health focus and underserved access boost demand, with the AI telemedicine market expected to reach USD 27 billion by 2030.
Enterprise adoption of doctor consultation platforms is now driven by proven outcomes. Telehealth usage remained steady for the third consecutive year in 2023, with 83% of users returning and 25–30% of US visits expected to shift to remote care by 2026.
Hospitals embedding consultation platforms into RPM programs are seeing measurable results, including 52% monthly cost savings in heart failure care through reduced hospitalizations.
ROI trends are equally clear. Hypertension monitoring delivers an average 22.2% return, while virtual practitioner models generate 32% ROI over three years compared to negative returns in standard telehealth.
What Is a Doctor Consultation App?
A doctor consultation app is a digital platform that allows patients and clinicians to connect remotely through video, chat, or asynchronous consultations. In enterprise settings, it functions as more than a communication tool. It supports structured intake, identity verification, clinical documentation, and post-consultation follow-ups.
These platforms integrate with EHR systems to maintain continuity of care. They also enforce consent, data security, and audit controls. When designed correctly, a doctor consultation app becomes a governed layer for delivering care at scale.
Where Are These Apps Used?
Doctor consultation apps are not limited to virtual visits. In enterprise healthcare, they are deployed where access gaps, follow-up complexity, and operational load intersect.
Their value comes from how well they support existing care models rather than replacing them. When aligned with workflows, these platforms extend clinical reach without increasing administrative burden.
1. Primary and Preventive Care
Primary care teams use consultation apps for routine consultations, early symptom assessment, and preventive guidance. This reduces unnecessary clinic visits while keeping care accessible.
Patients receive timely attention, and clinicians manage higher volumes without sacrificing quality. Over time, this improves continuity and trust.
2. Specialist Consultations and Second Opinions
Specialist access often creates delays. Consultation apps allow specialists to review cases remotely and provide second opinions efficiently.
Follow-up visits also move online, reducing travel and scheduling friction. This model works well for dermatology, mental health, and post-procedure reviews.
3. Long-Term Condition Management
Chronic care programs rely on regular clinical touchpoints. Consultation apps support ongoing engagement alongside RPM data.
Clinicians intervene earlier when risks appear, rather than waiting for scheduled visits. This approach improves outcomes while reducing hospital admissions.
4. Post-Discharge and Transitional Care
Hospitals use consultation apps to maintain contact after discharge. Virtual check-ins help identify complications early and prevent readmissions.
Care teams monitor recovery without overwhelming outpatient clinics. As a result, transitions become smoother and safer.
5. Employer and Insurer-Led Care Models
Employers and insurers deploy consultation platforms to expand access at controlled costs. At the same time, employees receive care faster, while organizations benefit from predictable utilization. These models work especially well when combined with subscription or bundled care structures.
Doctor consultation apps succeed when applied to real care delivery needs. Across primary, specialty, chronic, and enterprise models, their role is consistent. They improve access, reduce friction, and support scalable care without disrupting clinical workflows.
Types of Doctor Consultation Apps You Can Build
Doctor consultation apps are not one-size-fits-all solutions. Each model supports a different care strategy and operational goal. Enterprises that choose the wrong model often face workflow friction later.
The sections below outline the most common models used at scale.

1. On-Demand Consultation Apps
On-demand consultation apps prioritize immediate access to care. Patients connect with the next available clinician without scheduling. This model works well for low-acuity concerns and early symptom assessment.
Enterprises use it to reduce emergency department load. It also lowers call center volume and wait times. Clear triage rules are essential to avoid misuse. Escalation pathways must be defined from the start.
2. Scheduled Appointment Apps
Scheduled consultation apps support planned, structured care delivery. Patients book appointments based on clinician availability. Clinicians prepare in advance, which improves consultation quality. This model fits primary care and routine follow-ups.
Staffing and workload remain predictable over time. Here, documentation workflows are easier to standardize. At the same time, enterprises often pair this model with in-person services.
3. Specialist Consultation Platforms
Specialist consultation platforms expand access to expert care. Here, clinicians review cases remotely and provide second opinions. At the same time, follow-up visits also shift online when appropriate. This reduces wait times for specialty services. It works well for dermatology, mental health, and post-procedure reviews. Diagnostic data integration is critical here. Case routing must be tightly governed.
4. Chronic Care Consultation Apps
Chronic care consultation apps support long-term condition management. Patients engage with care teams on a recurring basis. These apps often integrate with RPM systems. At the same time, clinicians monitor trends and intervene earlier.
This reduces avoidable hospitalizations. Care plans remain consistent across touchpoints. Patient adherence improves over time.
5. Enterprise Subscription-Based Platforms
Subscription-based platforms provide continuous access for defined populations. Employers, insurers, and large providers use this model. Revenue becomes predictable through recurring fees.
Here, utilization is managed through structured access rules. At the same time, care delivery scales without linear cost increases. This model works well in preventive and primary care. Governance is key to sustainability.
Each doctor consultation app model serves a distinct purpose. Success depends on matching the model to care delivery goals. Enterprises that align strategy early avoid costly rework later. The right structure enables scale, stability, and long-term value.
Doctor Consultation Apps Generate Over 32% ROI in 3 Years
Return on investment is no longer speculative in virtual care. Enterprise data now shows a clear separation between standard telehealth deployments and structured doctor consultation platforms. When built as operational systems, these platforms generate consistent financial returns within a defined time horizon.
This gap exists because the economics are fundamentally different.
1. Why Virtual Models Outperform Standard Telehealth
Standard telehealth often replicates in-person workflows on video. As a result, costs scale alongside usage. Virtual practitioner models work differently. They redesign care delivery around remote-first operations, supported by structured intake, triage, and follow-up workflows.
This shift improves clinician utilization. It reduces idle time and avoids unnecessary escalation to higher-cost care settings. Over time, these efficiencies compound, which explains the 32% ROI seen over three years.
2. Cost Control Comes From Operational Design
Telehealth alone does not reduce costs if underlying workflows remain unchanged. Virtual practitioner models control cost by design. Care pathways are standardized. Repeat interactions are automated where appropriate. High-risk cases escalate early, while low-risk cases resolve faster.
Because of this structure, operating margins improve as usage grows. In contrast, standard telehealth platforms often see margins decline as clinician hours and administrative overhead increase.
3. Predictable Economics Enable Long-Term Planning
A 32% ROI over three years provides financial clarity. It allows healthcare enterprises to plan staffing, expansion, and technology investment with confidence. Subscription-based access, recurring consultations, and reduced no-show rates further stabilize revenue.
This predictability is what makes doctor consultation apps viable as long-term enterprise platforms rather than short-term digital initiatives.
Virtual practitioner models consistently outperform standard telehealth because they redesign care delivery, not just digitize it. A 32% ROI over three years reflects disciplined operational thinking, not market timing.
Core Features of a Doctor Consultation App
Enterprise doctor consultation apps rely on workflow-driven features that support care delivery, clinician efficiency, and operational governance at scale.
1. Patient-Side Features
Patient-side features shape how care begins and continues. In enterprise environments, these features must reduce friction while capturing reliable clinical data.
The goal is not convenience alone. It is safe access, clear communication, and continuity across every interaction.
A. Structured Clinical Intake
Patients begin with guided intake rather than free-form chat. Symptoms, history, medications, and red flags are captured in a structured flow. This reduces back-and-forth during consultations. Clinicians receive review-ready information before joining. Risk signals surface early. As a result, consultations stay focused and efficient.
B. Secure Video and Messaging
Video and messaging are delivered within a secure environment. Patients can switch between live and asynchronous modes when appropriate. This flexibility supports different care needs.
Encryption and access controls protect sensitive data. Session quality remains consistent across devices. Trust is preserved throughout the interaction.
C. Appointment and Follow-Up Management
Patients can book, reschedule, and track consultations easily. Follow-up instructions are stored in one place. At the same time, reminders reduce missed appointments.
Patients understand the next steps without additional calls. This improves adherence and satisfaction. Care continuity remains intact.
2. Doctor-Side Features
Doctor-side features must protect clinician time and decision quality. Poorly designed tools increase cognitive load. Enterprise platforms focus on clarity, context, and workflow alignment to support consistent care delivery.
A. Consultation Workspace
Clinicians work from a single consultation view. Intake data, patient history, and prior notes are visible upfront. Switching between systems is minimized.
Documentation happens alongside the consultation. This reduces errors and saves time. Decisions are made with full context.
B. Clinical Documentation Support
Notes, summaries, and follow-up plans are captured efficiently. Templates align with care protocols, and documentation meets compliance requirements without slowing clinicians down.
Records sync with EHR systems automatically. This reduces duplication. Audit readiness improves over time.
C. Intelligent Case Routing
Cases are assigned based on specialty, availability, and risk level. Under this, high-risk cases escalate automatically, and clinicians receive cases suited to their expertise.
This balances workloads across teams. Response times improve. Care quality remains consistent.
3. Admin & Operations Features
Admin and operations features determine whether the platform scales. Enterprises need visibility, control, and governance. These capabilities ensure clinical and business objectives stay aligned as usage grows.
A. User and Access Management
Roles define what patients, clinicians, and staff can access. Here, permissions follow least-privilege principles, identity verification is enforced at entry points, and changes are logged for audit purposes.
This reduces security risk, and compliance becomes manageable.
B. Workflow and Policy Configuration
Administrators configure care pathways and escalation rules. Policies adapt to different service lines, and changes do not require code deployments.
This flexibility supports evolving care models, where governance remains centralized and operational risk stays controlled.
C. Analytics and Performance Monitoring
Dashboards track utilization, outcomes, and operational metrics. Leaders see where bottlenecks form.
Here, performance trends guide staffing and investment decisions, and data support continuous improvement. At the same time, financial and clinical insights stay connected, and strategy becomes data-driven.
Core features determine whether a doctor consultation app supports real care delivery or creates operational drag. This alignment is what enables sustainable adoption across enterprise healthcare systems.
AI-Powered Features That Improve Clinical Outcomes
AI delivers value in doctor consultation apps when it removes friction rather than authority. Its role is to support clinical judgment, streamline operational workflows, and surface relevant context at the right time.
When implemented carefully, AI reduces cognitive load for clinicians and improves consistency across care delivery. The focus remains on enabling better decisions, not automating diagnosis.

1. AI-Driven Symptom Intake and Triage
AI enhances symptom intake by guiding patients through structured, adaptive questionnaires that adjust based on responses. This approach captures ca learer clinical context before a consultation begins, which reduces clarification time during live interactions.
Early warning signals surface naturally through pattern recognition. The final assessment always remains with the clinician, supported by better information rather than replaced by automation.
2. Risk Flagging and Escalation Support
AI continuously reviews intake data and consultation inputs to identify potential risk indicators. When predefined thresholds are reached, the system highlights cases that may require faster attention or escalation.
This helps teams respond consistently across large patient volumes.
Low-risk cases continue through standard workflows without unnecessary interruption. Escalation remains guided by human oversight, with AI acting as an early signal rather than a decision-maker.
3. Smart Case Routing to the Right Clinician
AI supports case routing by matching consultations to clinicians based on specialty, availability, and urgency. This reduces manual coordination while improving alignment between patient needs and clinical expertise.
Workloads are distributed more evenly across care teams. Response times improve without increasing staffing pressure. Routing logic stays transparent, with administrators retaining control over assignment rules.
4. Clinical Documentation Assistance
AI assists clinicians by organizing consultation inputs into structured documentation drafts. Key details surface automatically, allowing clinicians to review, refine, and finalize records efficiently.
This reduces time spent on repetitive documentation tasks. Notes align with clinical and compliance standards from the outset. Accountability remains firmly with the clinician, while administrative effort declines.
5. Follow-Up and Care Reminder Support
AI helps maintain continuity after consultations by managing follow-up timelines and care reminders. Patients receive timely prompts aligned with care plans, which improves adherence without manual outreach.
Clinicians gain visibility into pending follow-ups without tracking each case individually. Missed actions decline as workflows stay consistent. Care extends beyond the consultation without increasing operational load.
By improving intake quality, prioritization, routing, documentation, and follow-up, AI strengthens both clinical and operational outcomes. When designed with clear boundaries, it enhances care delivery while preserving trust, accountability, and clinical control.
Compliance & Regulatory Requirements You Cannot Ignore
Compliance shapes architecture, workflows, and governance from day one. This is why enterprises that treat compliance as a post-build task often face rework, delays, or operational risk later.
When designed correctly, regulatory alignment supports trust, scale, and predictable operations. At the same time, the sections below outline the core compliance areas that must be addressed at the foundation level.
1. HIPAA and Patient Data Protection
HIPAA requirements influence how data flows through the platform. Under this layer, patient information must remain encrypted at rest and in transit. At the same time, access controls limit who can view, edit, or share sensitive data.
Audit logs track every interaction for accountability. Session data, recordings, and notes follow strict retention rules. When these controls are embedded into architecture, security becomes consistent rather than manual.
2. GDPR and Consent Management
GDPR compliance centers on consent, transparency, and data rights. Here, patients must clearly understand how their data is used. At the same time, consent needs to be captured, stored, and enforced across workflows.
Access, correction, and deletion requests must be supported without breaking care continuity.
Data minimization reduces exposure across systems. These requirements influence identity, storage, and integration design from the start.
3. Telemedicine Laws Across Regions
Telemedicine regulations vary by region and must be respected. In the US, licensing and state-level rules affect who can provide care and where. Additionally, in the UK and EU, data residency and professional standards shape delivery models.
Enterprise platforms must support jurisdiction-based rules. At the same time, flexibility at the architecture level prevents compliance conflicts as services expand.
4. Clinical Safety and Audit Readiness
Clinical safety extends beyond data protection. Here, platforms must support clear escalation paths and role accountability. At the same time, decision support tools require defined boundaries. Additionally, documentation needs to meet audit standards consistently.
Review mechanisms help identify gaps before issues escalate. When audit readiness is built into workflows, compliance becomes routine rather than reactive.
Compliance determines whether a doctor consultation app can scale safely. When regulatory controls are embedded early, platforms operate predictably across regions and use cases.
Technology Stack for a Doctor Consultation App
A doctor consultation app relies on a layered technology stack where each layer supports clinical workflows, security, and scalability without compromising performance or compliance.
Technology choices shape how reliably a doctor consultation app operates at scale. For enterprises, the stack must support secure care delivery, real-time interactions, and regulatory control. Below is a practical view of how the stack is structured.
1. Frontend Layer
The frontend layer manages all user interactions. Patients and clinicians access consultations, schedules, and records through this interface. It must remain responsive across devices and networks.
Clear design reduces friction during critical moments. Accessibility and performance matter as much as visual polish.
Common Technologies Used
- React, Angular, or Vue for web applications
- Swift for iOS and Kotlin for Android
- WebRTC-compatible UI components for video
- Accessibility and localization libraries
2. Backend and Application Layer
The backend layer handles business logic and workflow orchestration. It manages consultations, user roles, scheduling, and data flow between systems. This layer enforces rules around access, escalation, and documentation.
Reliability here determines platform stability. APIs must remain consistent as integrations expand.
Common Technologies Used
- Node.js, Java, or .NET for application services
- REST and GraphQL APIs
- Microservices architecture for scalability
- Workflow orchestration engines
3. Video and Real-Time Communication Layer
This layer powers live consultations and messaging. It must deliver stable video under varying network conditions. Low latency and session security are critical.
Recording, if enabled, must follow compliance rules. Failover handling ensures consultations continue smoothly.
Common Technologies Used
- WebRTC for real-time communication
- Media servers such as Kurento or Janus
- Secure signaling servers
- Network monitoring and quality adaptation tools
4. Cloud Infrastructure Layer
The cloud layer supports scalability and availability. It ensures the platform handles peak usage without disruption. Data storage, compute, and networking are managed here.
Geographic distribution supports regional compliance. Infrastructure must recover quickly from failures.
Common Technologies Used
- AWS, Azure, or Google Cloud Platform
- Containerization with Docker and Kubernetes
- Auto-scaling and load balancing services
- Managed databases and storage services
5. Security, Identity, and Compliance Layer
This layer protects patient data and enforces governance. Identity verification controls who can access the system.
Encryption safeguards data across all layers. Audit trails provide accountability. Compliance requirements are enforced consistently rather than manually.
Common Technologies Used
- OAuth 2.0 and OpenID Connect for identity
- Role-based access control systems
- Encryption and key management services
- Audit logging and compliance monitoring tools
Each layer plays a specific role in performance, security, and scalability. When designed together, the platform supports reliable operations across regions and use cases. This layered approach reduces risk and enables long-term enterprise growth.
How We Create an Enterprise-Grade Doctor Consultation App
At Intellivon, a doctor consultation app is approached as a clinical operating layer rather than a standalone digital product. Our teams combine healthcare domain understanding with enterprise architecture and applied AI expertise.
Each decision is grounded in how care is actually delivered. The process below reflects how Intellivon builds consultation platforms that enterprises can operate with confidence.
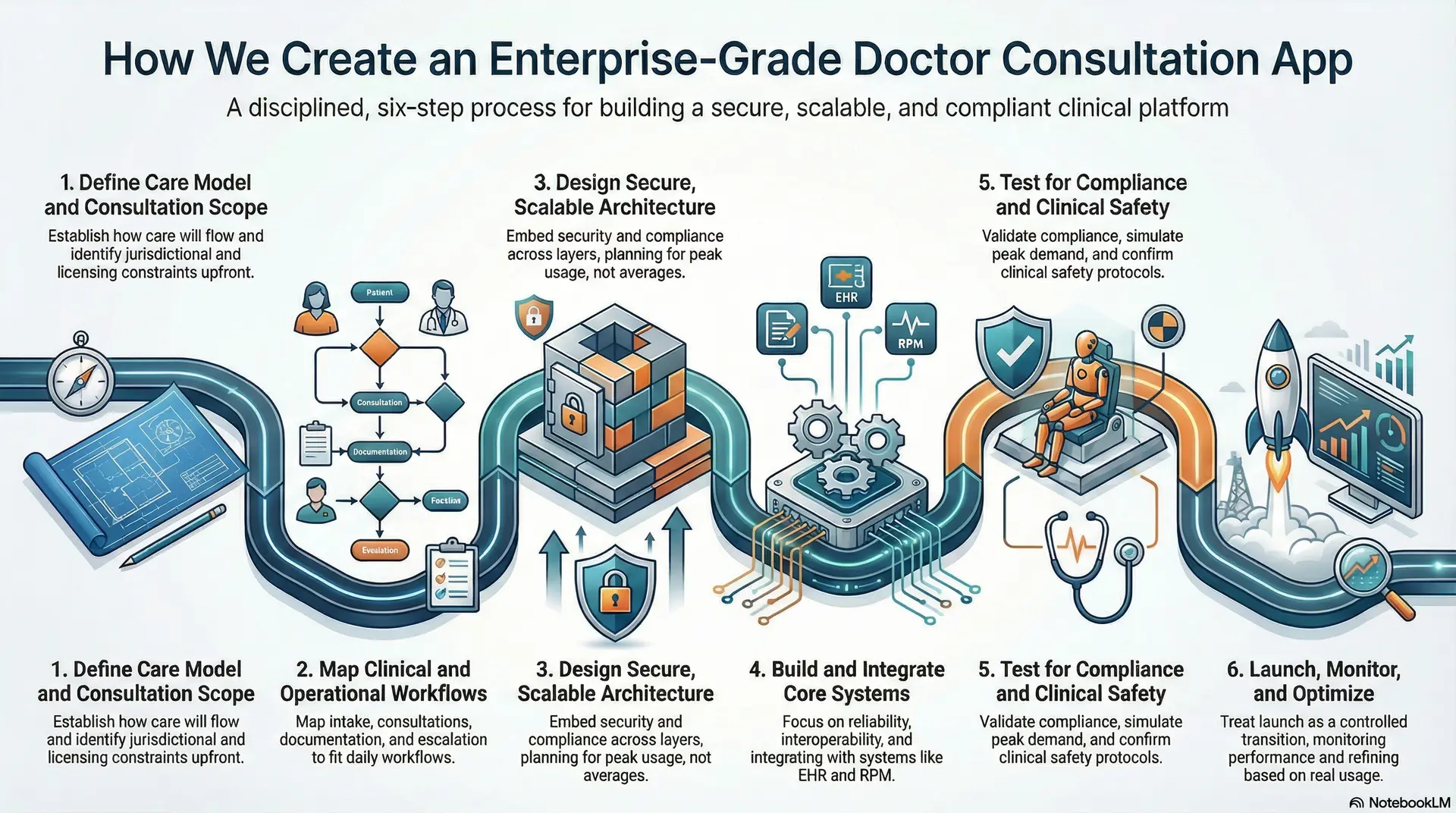
Step 1: Define Care Model and Consultation Scope
Intellivon begins by establishing how care will flow through the platform across different consultation types. Under this step, on-demand, scheduled, specialist, and chronic care models are evaluated in relation to clinical responsibility and risk.
At the same time, escalation boundaries are clarified early to prevent misuse, and jurisdictional and licensing constraints are identified upfront. Consequently, this step ensures the platform supports safe delivery rather than unchecked access. Scope decisions remain tied to operations and compliance. The result is a care model built for scale.
Step 2: Map Clinical and Operational Workflows
Our experts work closely with clinical and operations teams to understand how care moves today. Here, intake, consultations, documentation, escalation, and follow-up are mapped end-to-end. At the same time, existing systems and manual handoffs are reviewed without assumptions. Bottlenecks and risk points surface naturally through this process.
Under this step, the platform is shaped to fit daily workflows rather than disrupt them. This alignment reduces friction during rollout. Adoption becomes easier as a result.
Step 3: Design Secure, Scalable Architecture
Intellivon designs architecture with security and compliance embedded across layers. Under this step, data flows, access controls, and audit requirements are defined together rather than separately. Consequently, regional regulations and data residency needs are accounted for early.
Scalability planning focuses on peak usage, not averages. At the same time, integration standards are established upfront. This foundation supports growth without rework. Stability remains intact as complexity increases.
Step 4: Build and Integrate Core Systems
Development focuses on reliability and interoperability throughout the build phase. Under this system, consultation workflows evolve alongside identity, access, and integration layers. Additionally, EHR, RPM, and third-party systems are integrated using enterprise-grade standards. AI capabilities are introduced carefully as decision support.
Each component is validated before full integration. Here, dependencies are managed deliberately. This approach reduces downstream risk during deployment.
Step 5: Test for Compliance and Clinical Safety
Testing at Intellivon reflects real-world conditions rather than ideal scenarios. Here, compliance workflows are validated across patient journeys. Load testing simulates peak demand patterns. At the same time, clinical safety reviews confirm escalation and fallback behavior.
At the same time, audit trails and documentation are examined closely, and issues surface early and are resolved before launch. This protects both patient outcomes and enterprise credibility.
Step 6: Launch, Monitor, and Optimize
Launch is treated as a controlled transition into live operations. In this step, Intellivon monitors performance, usage patterns, and clinical signals closely. At the same time, early insights guide optimization efforts. Consequently, governance remains active after go-live.
AI models and workflows are refined based on real usage. As adoption grows, scaling remains predictable. As a result, continuous improvement supports long-term value creation.
Enterprise-grade doctor consultation apps demand discipline across care delivery, compliance, and technology. Intellivon’s approach aligns these elements from the start.
The result is a consultation platform designed for real healthcare environments rather than short-term experimentation.
Cost to Build a Doctor Consultation App
At Intellivon, doctor consultation apps are built as regulated care delivery platforms rather than lightweight virtual tools. Cost planning is directly tied to clinical risk, compliance exposure, and long-term scalability. The objective is to invest deliberately in safety, reliability, and operational readiness so the platform performs in real healthcare environments. Budgets are structured to support sustained usage, not short-term pilots or isolated feature launches.
When budget constraints exist, scope is refined collaboratively and pragmatically. Regulatory, security, and governance requirements are never compromised during this process. HIPAA, GDPR, and regional telemedicine regulations remain enforced throughout delivery. Architecture and compliance decisions are protected from day one. This approach balances cost discipline with sustainable compliance and long-term ROI.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Compliance Alignment | Care model definition, requirements analysis, regulatory mapping, KPI alignment | $6,000 – $12,000 |
| Architecture & Secure Platform Design | Scalable architecture, PHI segregation, encryption strategy, resilience planning | $8,000 – $15,000 |
| Workflow Mapping & Clinical Logic | Clinical and operational workflows, triage rules, escalation paths, care journeys | $8,000 – $14,000 |
| Backend & Integration Development | EHR, pharmacy, labs, billing, third-party system integrations | $12,000 – $22,000 |
| Frontend & Role-Based Interfaces | Patient, clinician, and admin dashboards with usability and accessibility controls | $10,000 – $20,000 |
| Security & Privacy Engineering | Encryption, access control, audit logs, monitoring, threat detection | $8,000 – $15,000 |
| Testing & Compliance Validation | Security testing, workflow validation, regulatory, and audit readiness checks | $6,000 – $10,000 |
| Deployment & Scalability Setup | Cloud deployment, monitoring, high availability, performance tuning | $6,000 – $12,000 |
Total initial investment: $50,000 – $150,000
Ongoing maintenance and optimization: 15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped doctor consultation programs face pressure when hidden cost drivers are overlooked. Planning for these early protects timelines and budgets while reducing friction during scale.
- Integration complexity often increases due to legacy EHRs and fragmented systems
- Compliance overhead grows with recurring audits and evolving regulations
- Data governance requires continuous cleaning, mapping, and standardization
- Cloud costs rise with real-time video, monitoring, and analytics workloads
- Change management includes clinician, operations, and compliance training
- Monitoring and optimization remain ongoing as usage and regulations evolve
Best Practices to Avoid Budget Overruns
Based on Intellivon’s enterprise healthcare delivery experience, these practices consistently lead to predictable costs and faster go-live while protecting long-term value.
- Start with a focused scope and validate outcomes before scaling
- Embed compliance into architecture from the first design decision
- Use modular components that can be reused across care programs
- Optimize cloud usage by balancing real-time and batch workloads
- Maintain continuous observability across performance and compliance
- Plan for long-term evolution rather than initial deployment alone
Request a tailored proposal from Intellivon’s healthcare team to receive a delivery roadmap aligned with your $50,000–$150,000 budget, compliance priorities, and long-term growth strategy.
Top Examples Of Doctor Consultation Apps
The most successful doctor consultation apps did not grow by adding features quickly. They scaled by aligning technology with real care delivery models. Each example below shows how leading platforms use AI to support clinicians, manage demand, and maintain consistency without replacing medical judgment.
These platforms illustrate what enterprise-ready execution looks like in practice.
1. Teladoc Health
Teladoc Health operates as a global virtual care platform supporting primary, specialty, and chronic care services. The app connects patients with clinicians through scheduled and on-demand consultations while integrating long-term care programs.
AI is used to guide symptom intake, route cases to appropriate clinicians, and support chronic condition monitoring. Risk signals surface early, helping clinicians prioritize attention without automating diagnosis. This approach allows Teladoc to scale across regions while maintaining clinical oversight.
2. Amwell
Amwell focuses on enterprise healthcare delivery for hospitals, insurers, and large employers. The platform supports virtual visits, post-discharge care, and specialty consultations within existing care networks.
AI assists with patient intake, visit preparation, and clinician matching based on availability and expertise. Operational analytics help organizations manage capacity and utilization. AI remains embedded within workflows rather than acting independently.
3. Doctolib
Doctolib began as a scheduling platform and evolved into a broader consultation and care coordination system across Europe. The app supports both in-person and virtual consultations while maintaining strong data protection standards.
Here, AI is applied to appointment optimization, patient reminders, and workflow efficiency. These capabilities reduce no-shows and administrative load. Clinical decision-making remains fully clinician-led.
Babylon Health
Babylon Health combines virtual consultations with AI-supported health assessments. The platform uses AI-driven symptom checkers to structure patient input before consultations.
Clinicians receive an organized context, which improves efficiency and consistency. AI also supports population-level insights and care prioritization. Final diagnoses and treatment decisions remain with licensed professionals.
These platforms demonstrate a consistent pattern. AI supports intake, prioritization, and operational efficiency while clinicians retain decision authority. Each app scales because workflows, compliance, and technology evolve together.
Conclusion
Doctor consultation apps have moved beyond convenience-driven digital initiatives. For enterprises, they now function as core care delivery systems that shape access, efficiency, and long-term operating models. Success depends on how well clinical workflows, compliance controls, and technology decisions align from the start.
When built correctly, these platforms reduce operational strain, improve clinician utilization, and unlock sustainable ROI. The opportunity is not just cost reduction, but controlled growth across regions and care models. With the right architecture and execution partner, doctor consultation apps become durable healthcare assets rather than short-lived pilots.
Build a Doctor Consultation Platform With Intellivon
At Intellivon, doctor consultation platforms are built as regulated care delivery systems rather than surface-level digital interfaces. Here, the focus stays on compliance, scalability, and operational control from the very beginning. Every decision is shaped by clinical responsibility, data protection, and long-term enterprise use rather than short-term rollout speed.
Each platform is engineered for real healthcare environments where risk tolerance is low and accountability is high. Architecture remains compliance-led, with privacy, consent, and auditability embedded directly into workflows. As platforms expand across regions, specialties, or patient populations, governance and performance remain predictable. This approach allows consultation programs to scale without increasing clinical, regulatory, or operational risk.
Why Partner With Intellivon?
- Enterprise-grade consultation architecture aligned with real clinical and operational workflows
- Proven integration expertise across EHRs, labs, pharmacies, billing, and payer systems
- Compliance-by-design delivery supporting HIPAA, GDPR, consent enforcement, and audit readiness
- Secure role-based access control with full action-level auditability
- AI-assisted workflows for triage, documentation, and care continuity with human oversight
- Cloud-native, scalable infrastructure built for high availability and regional expansion
- Modular delivery model enabling phased rollout and controlled growth
- Continuous optimization across performance, compliance, and adoption metrics
Book a strategy call to explore how a doctor consultation platform can operate as a trusted enterprise care delivery layer across your organization, with Intellivon as your long-term technology and compliance partner.
FAQs
Q1. How much does it cost to build a doctor consultation app?
A1. The cost to build a doctor consultation app typically ranges from $50,000 to $150,000 for an enterprise-grade platform. This pricing depends on care scope, compliance requirements, integrations, and scalability needs. At the same time, apps built for regulated environments require additional investment in security, auditability, and governance. Ongoing maintenance usually adds 15–20% of the initial build cost per year. Lower-cost builds often struggle to scale safely.
Q2. Is a doctor consultation app HIPAA compliant by default?
A2. No, a doctor consultation app is not HIPAA compliant by default. Compliance depends on how the app is designed, hosted, and operated. Additionally, data encryption, access controls, audit logs, and secure integrations must be built into the architecture. At the same time, HIPAA compliance also requires process controls, not just technology. Apps that treat compliance as an add-on usually face rework and delays.
Q3. How long does it take to develop a consultation app?
A3. Development timelines typically range from 4 to 6 months for an enterprise-ready consultation platform. This includes discovery, workflow design, compliance alignment, development, testing, and deployment. Consequently, simpler pilots may launch faster, but they often require rebuilding later. At the same time, timeframes increase when integrations, multi-region compliance, or AI capabilities are involved.
Q4. Can AI be used in doctor consultation apps safely?
A4. Yes, AI can be used safely when positioned as decision support rather than diagnosis. Here, AI commonly assists with symptom intake, triage support, case routing, documentation, and follow-up reminders. Additionally, clinical judgment always remains with licensed professionals. Clear boundaries, auditability, and human oversight are essential to maintain trust and compliance.
Q5. What’s the difference between telemedicine and consultation apps?
A5. Telemedicine often refers to virtual visits delivered through video or chat. However, doctor consultation apps go further. Additionally, they support structured intake, clinical workflows, documentation, escalation, and follow-ups within a governed system. At the same time, in enterprise settings, consultation apps function as care delivery layers rather than standalone communication tools.