A real-time clinical data sync platform transforms how an enterprise operates. It closes the gap between care delivery and leadership actions. Decisions are made faster because data is immediately available. Clinical teams no longer work around missing information. At the same time, finance and compliance gain better visibility instead of having to reconcile after the fact.
Over time, this changes how new services launch, how partners are onboarded, and how AI is trusted in real situations. The platform evolves from being just “IT infrastructure” to functioning as operational support.
This is where Intellivon’s experience matters. We create AI and healthcare data platforms that work within regulated, multi-provider ecosystems, rather than controlled lab environments. Our focus is on governance, interoperability, and long-term growth from the first design decision. For organizations ready to shift from reactive data management to proactive, intelligence-driven operations, this is a strategic step that can begin now. This blog discusses how we build such a platform from the ground up.

Why Enterprises Are Reprioritizing Real-Time Clinical Data Sync
Enterprises are now placing real-time clinical data sync higher on their strategic agenda. This shift is driven by persistent data silos, slower trial execution, and growing pressure to extract value from AI-driven insights.
At the same time, clinical programs are becoming more complex. Regulatory expectations are also rising across regions and partners. Together, these forces are pushing organizations to rethink how quickly and reliably clinical information moves across their ecosystems.
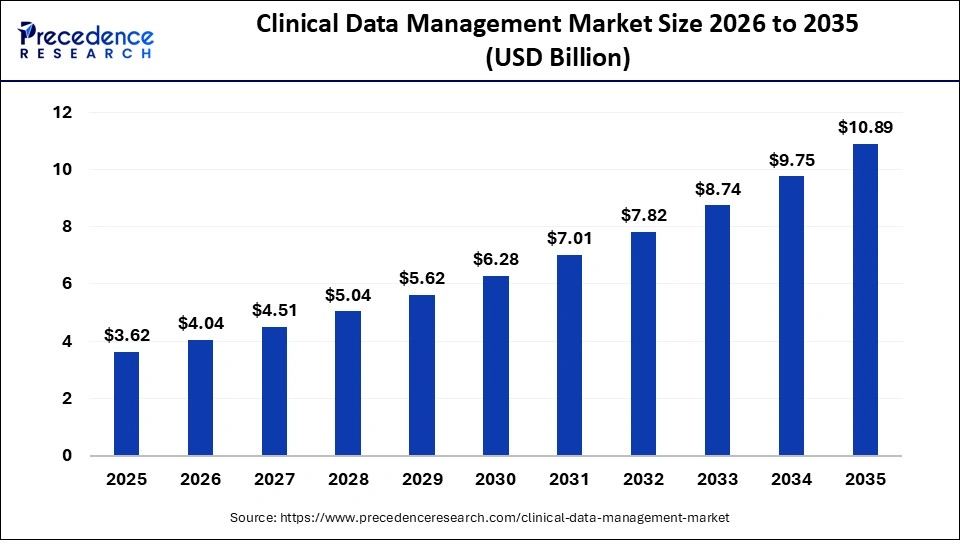
The global clinical data management market is gaining strong momentum, valued at USD 3.62 billion in 2025 and expected to reach USD 4.04 billion in 2026.
Growth does not slow after that, with the market projected to approach USD 10.89 billion by 2035, reflecting a steady CAGR of 11.64% between 2026 and 2035. This clearly shows that clinical data platforms are no longer niche investments but a core part of enterprise healthcare strategy.
Market Insights:
- Rising trial volumes and complexity: Global trials now generate large volumes of data from wearables, ePROs, and decentralized models, which increases the need for real-time data integration. Oncology currently holds a 35% share, while neurology is growing at nearly 13%.
- AI and ML integration: AI now supports faster data validation, shortening cycles by around 20%. It also enables anomaly detection and risk-based monitoring, helping reduce errors by 30% and lowering Phase III trial costs by nearly 18%.
- Shift toward decentralized and hybrid trials: Nearly 30% of trials are expected to follow decentralized or hybrid models by 2027. This is accelerating demand for cloud-based, interoperable platforms that can manage remote data from multiple sources.
- Stricter regulatory requirements: FDA and EMA mandates around data integrity are pushing enterprises toward standardized and compliant systems. Many are also exploring blockchain-based traceability to improve audit readiness by up to 25%.
Enterprises see clear operational gains when real-time clinical data sync is implemented well. Manual data transfers drop by nearly 70%, which reduces errors and prevents costly database lock delays in biopharma trials. At the same time, workflows become smoother, wait times shrink, and care delivery becomes more responsive through real-time workload balancing.
This also helps reduce staff fatigue by distributing effort more intelligently. In clinical research, faster trial completion, lower costs, and stronger data quality follow naturally when remote monitoring and automation are embedded into daily operations.
What Is A Real-Time Clinical Data Sync Platform?
A real-time clinical data sync platform is a system that ensures patient and clinical information moves accurately and instantly across healthcare systems, providers, and applications. It keeps data aligned as events happen, rather than after delays or manual updates. Unlike traditional data pipelines, it focuses on trust, consistency, and usability of information at the moment it is needed.
For enterprises, this means decisions are based on current and complete data, not yesterday’s records. Over time, it becomes the foundation for coordinated care, compliant operations, and scalable digital health initiatives.
Why This Is Not Just Another Integration Layer
At first glance, a real-time clinical data sync platform may look like another integration tool. Many enterprises already use APIs, middleware, or health information exchanges to move data between systems. However, these tools were built to connect systems, not to manage clinical truth in motion.
A real-time sync platform goes beyond connectivity. It focuses on keeping clinical information consistent, reliable, and usable as it moves across providers, partners, and applications. This difference matters when decisions, audits, and patient outcomes depend on what the data says at a given moment.
How a Real-Time Clinical Data Sync Platform Differs
| Capability | Traditional Middleware / APIs | HIEs | Real-Time Clinical Data Sync Platform |
| Core purpose | Move data between systems | Share records across organizations | Maintain trusted, live clinical data |
| Data timing | Often delayed or batch-based | Near real-time, mostly document-based | Truly real-time and event-driven |
| Focus | Connectivity | Data access | Data consistency and reliability |
| Error handling | Limited, mostly technical | Operational, not continuous | Built-in validation and correction |
| Governance | Outside the system | Often fragmented | Embedded into the platform |
| Enterprise role | Tactical IT tool | Exchange network | Strategic data infrastructure |
For enterprise leaders, the difference is not technical, but operational. While integration layers move data, a real-time clinical data sync platform manages how that data behaves across the enterprise.
It ensures that what flows between systems can be trusted, acted upon, and defended in audits. That shift is what makes it infrastructure, not just integration.
Enterprise Use Cases Driving Real-Time Clinical Data Sync Platforms
Real-time clinical data sync platforms are not built for technical elegance. They are built to solve operational problems that slow down care, inflate costs, and increase risk across healthcare enterprises.
When data moves late or inconsistently, entire workflows suffer. These platforms change that by ensuring clinical information is available when and where it is needed, without manual workarounds.
Below are the core use cases that are driving adoption across enterprises today.
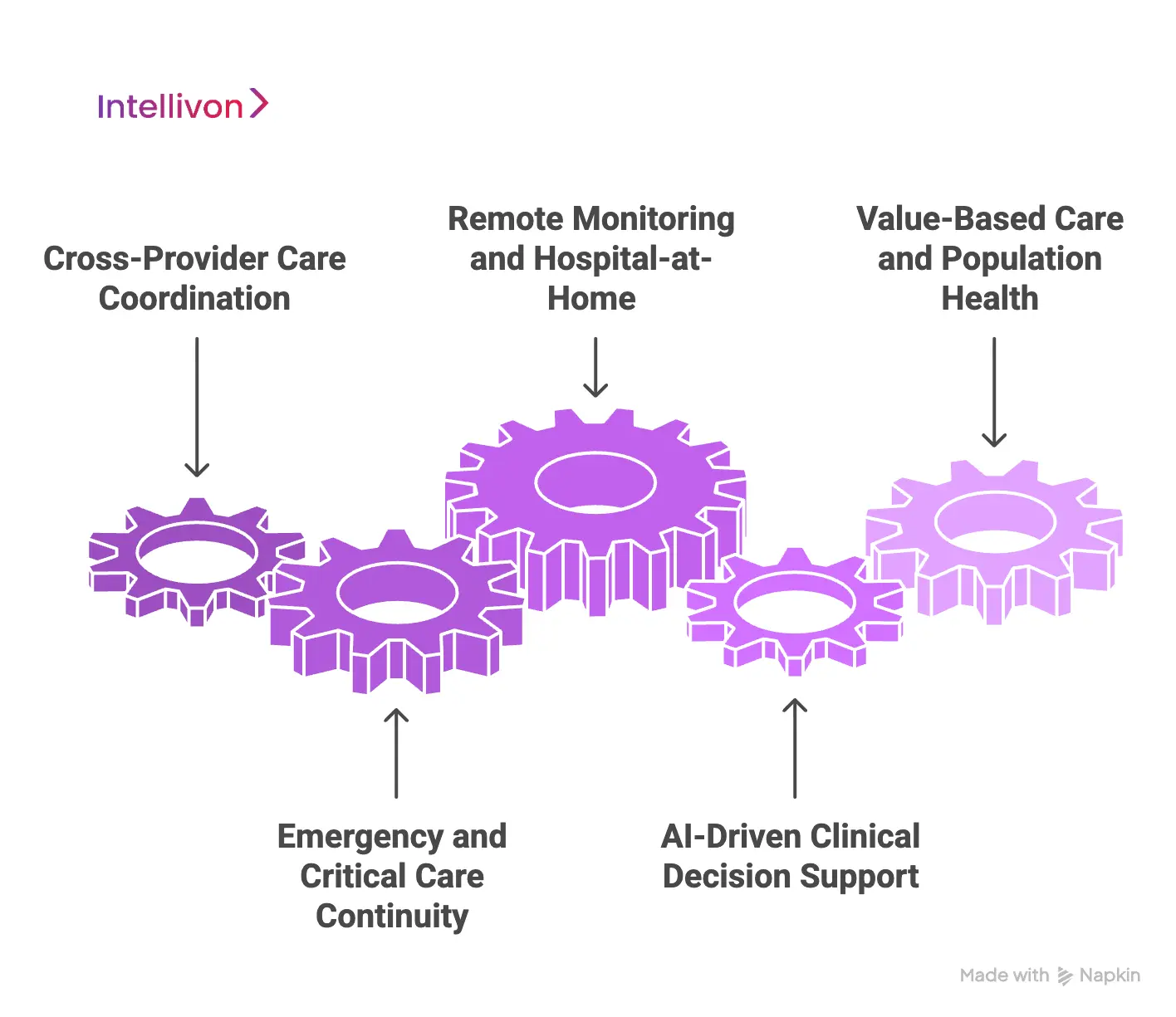
1. Cross-provider care coordination
Patients often receive care across hospitals, clinics, and specialists. When systems do not align in real time, clinicians work with an incomplete context.
A clinical data sync platform ensures that medication changes, diagnoses, and test results are visible across providers as they occur. This reduces repeated tests, prevents conflicting treatments, and supports safer handovers.
2. Emergency and critical care continuity
In emergency settings, delays in data can become clinical risks. Real-time sync ensures that allergy history, recent procedures, and vital records follow the patient instantly across departments and facilities.
This allows care teams to act with confidence, even when the patient arrives without documentation.
3. Remote monitoring and hospital-at-home
Wearables and connected devices generate continuous patient data outside traditional care settings.
Without real-time sync, much of this data remains underused. A sync platform ensures that remote readings flow directly into clinical workflows, enabling faster intervention and more responsive care models.
4. AI-driven clinical decision support
AI systems depend on current and accurate data. When inputs arrive late or fragmented, AI insights lose relevance.
Real-time data sync allows decision support tools to operate on live clinical signals, making them practical in everyday care rather than limited to retrospective analysis.
5. Value-based care and population health
Managing outcomes across large populations requires up-to-date information across providers and payers. Real-time sync enables faster risk identification, better care gap closure, and more accurate performance tracking.
This directly supports value-based contracts and long-term care optimization.
Across all these use cases, the pattern is clear. Real-time clinical data sync moves data from being a passive record into an active operational asset. For enterprises, this is what turns digital health investments into measurable performance gains.
58% Faster Data Capture and 99% Fewer Errors with Clinical Data Sync
Real-time clinical data sync changes how quickly and reliably information moves from care settings into clinical systems. Instead of relying on manual re-entry, data flows directly from source systems into trial and analytics platforms.
This shift may look operational on the surface, but its impact is strategic. It determines how fast teams move, how clean their data remains, and how much effort is spent fixing avoidable issues.
1. Faster data capture at the source
In a site-based comparison between EHR-to-EDC transfer and manual entry, the synced approach enabled teams to process 58% more data within the same time window.
This means the same staff, working the same hours, moved significantly more clinical information without increasing workload. Over time, this directly shortens data availability cycles and reduces pressure on downstream teams.
2. Near elimination of data entry errors
Speed alone is not enough if accuracy suffers. However, the same study showed a 99% reduction in data entry errors, with manual workflows producing 100 errors versus just 1 error through automated transfer.
For enterprises, this lowers query volumes, reduces rework, and strengthens audit readiness without adding control layers.
Together, these gains reposition clinical data sync as more than a process improvement. It becomes a practical lever for faster execution, stronger compliance, and scalable operations across complex clinical programs.
Interoperability as a Real-Time Clinical Data Sync Platform Capability
Interoperability is often treated as a technical requirement. In reality, it is a business capability. When systems fail to speak the same language, workflows break, teams slow down, and compliance risks rise.
A real-time clinical data sync platform treats interoperability as part of how the enterprise operates, not just how systems connect.
This shift matters because healthcare data does not live in one place. It moves across providers, partners, devices, and payers every day. The platform must make that movement reliable and usable.
1. Built for multi-system healthcare environments
Most enterprises run multiple EHRs, lab systems, imaging tools, and billing platforms. A sync platform ensures these systems stay aligned in real time, even when they follow different data standards.
This prevents delays caused by format mismatches and incomplete transfers.
2. Supports healthcare data standards naturally
A strong platform handles standards like FHIR, HL7, DICOM, and X12 without forcing rigid dependencies.
It allows systems to exchange data in their native formats while keeping meaning intact. This reduces custom work and simplifies partner onboarding.
3. Preserves data meaning across systems
Interoperability is mostly about preserving what that data represents. A real-time sync platform ensures that a diagnosis, a medication update, or a lab result means the same thing across every system it touches.
4. Enables faster ecosystem expansion
When interoperability is built into the platform, adding new partners becomes easier. Enterprises can onboard providers, research sites, and digital health tools without redesigning their data flows. This supports growth without increasing operational drag.
When treated as a platform capability, interoperability stops being a recurring problem and becomes a competitive advantage. It allows enterprises to scale care models, partnerships, and digital services with confidence, knowing their data will remain consistent across every connection.
Security Architecture for Cross-System Clinical Data Transfer
When clinical data moves across systems and organizations, security becomes more than a technical concern. It becomes a trust requirement. This is because patients, partners, and regulators expect every data movement to be safe, traceable, and controlled.
A real-time clinical data sync platform must therefore be designed with security at its core, not added later as a layer. This is especially important because healthcare data rarely stays within one boundary and flows between providers, research sites, payers, and digital tools every day.
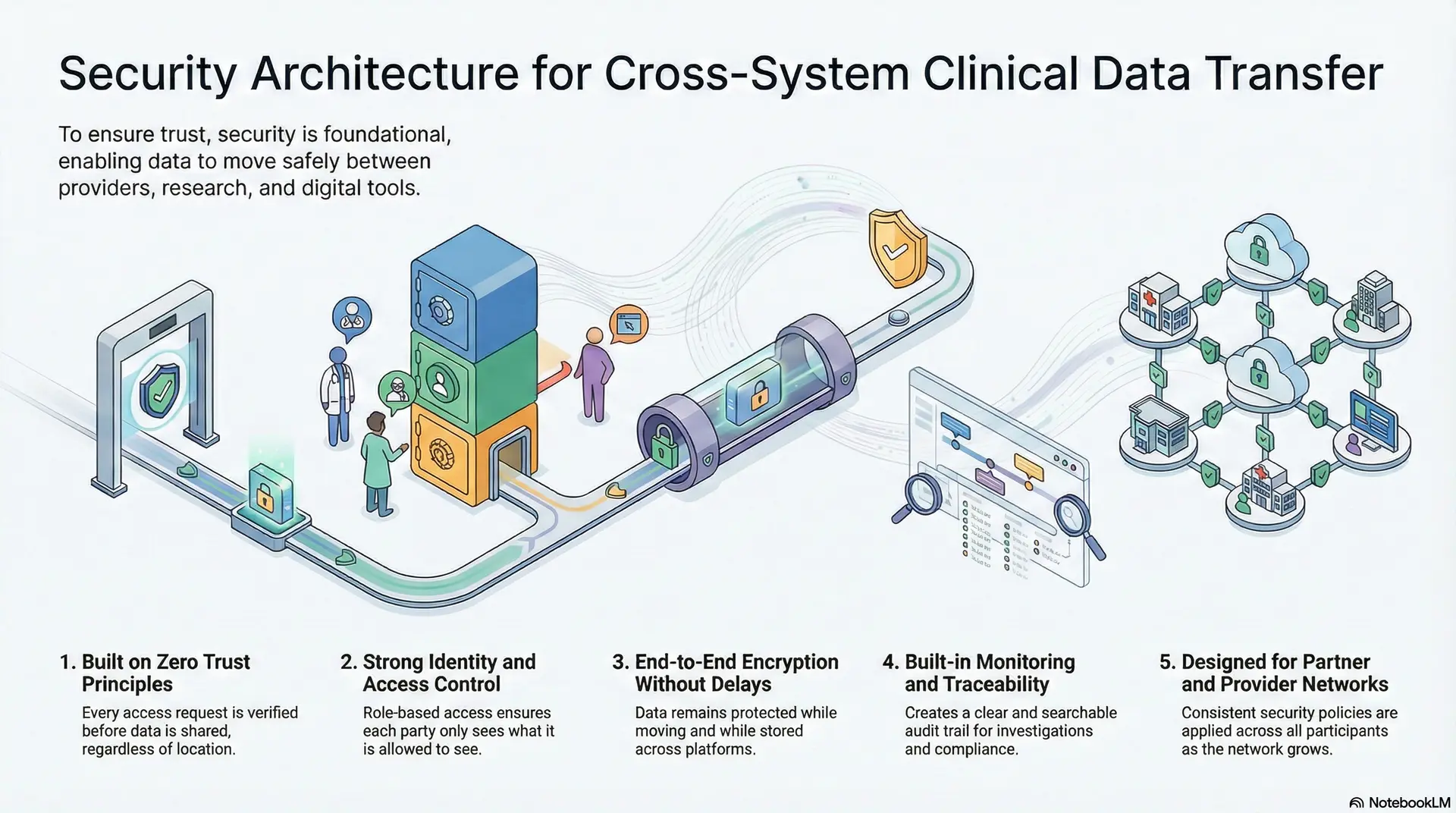
1. Built on zero trust principles
In a cross-system environment, no system can be assumed safe by default, regardless of where it sits in the network. Every access request is verified before data is shared. This applies even when the request comes from within the enterprise itself.
As a result, security does not depend on physical location or internal trust zones. This approach limits damage even if a connected system is compromised.
2. Strong identity and access control
Every user, system, and application must be clearly identified before accessing clinical data. Role-based access ensures that each party only sees what it is allowed to see. This prevents accidental exposure of sensitive information across providers and partners.
It also reduces the need for manual approvals that slow down operations. Security remains strong without becoming an operational barrier.
3. End-to-end encryption without delays
Clinical data must remain protected while moving and while stored across platforms. A real-time sync platform applies encryption across every stage of transfer. This protection does not slow down access to live information.
Care teams can still act quickly on critical data when it matters. At the same time, security and privacy requirements are fully met.
4. Built-in monitoring and traceability
Security does not stop once access is granted. The platform continuously monitors activity and records every data transfer. This creates a clear and searchable audit trail for investigations and compliance reviews.
It also helps enterprises detect unusual behavior early. Over time, this strengthens trust across the entire data ecosystem.
5. Designed for partner and provider networks
Security becomes harder as more systems join the ecosystem. A real-time sync platform applies consistent security policies across all participants.
This ensures that expanding the network does not weaken the security posture. Partners can connect without introducing hidden risks. Growth remains controlled and predictable.
When security is embedded into the architecture, cross-system data transfer becomes both safe and scalable. For enterprises, this means they can grow digital ecosystems without increasing risk or operational complexity.
Compliance and Data Governance Across Provider Networks
When clinical data moves across multiple providers, compliance and governance cannot remain local concerns. They become shared responsibilities across the entire network. A real-time clinical data sync platform must therefore manage not only how data flows, but also how it is controlled, audited, and defended.
Without this, even the most advanced interoperability or security model will fail under regulatory pressure.
1. Compliance must be built into the platform
Healthcare regulations do not apply only at the point of care. They apply at every stage where data is created, transferred, stored, and accessed. A strong sync platform embeds regulatory logic directly into how data moves across systems.
This reduces reliance on manual compliance checks and prevents violations before they occur. As a result, enterprises remain audit-ready without slowing down operations.
2. Consent cannot live only inside applications
Patient consent often varies across use cases, providers, and jurisdictions. If consent is handled only at the application level, it becomes inconsistent and hard to enforce across networks.
A real-time sync platform manages consent centrally and applies it wherever data flows. This ensures patient preferences are respected regardless of where or how data is used.
3. Data governance must operate in real time
Traditional governance models rely on periodic reviews and retrospective audits. In a real-time environment, that is no longer sufficient. The platform must enforce data quality rules, access policies, and retention controls as data moves.
This keeps information accurate, reliable, and compliant at every moment, not just at reporting time.
4. Auditability is a continuous requirement
Enterprises can no longer treat audits as isolated events. Regulators expect clear evidence of how data has been handled over time. A real-time sync platform maintains complete lineage and traceability for every data movement. This allows organizations to answer regulatory questions with confidence and speed.
5. Designed for cross-border and multi-region operations
Provider networks often span regions with different regulatory requirements. A strong governance model adapts to these differences without fragmenting the platform.
Rules around data residency, access rights, and reporting are applied dynamically. This allows enterprises to expand their networks while staying compliant everywhere they operate.
When compliance and governance are treated as core platform capabilities, real-time data exchange becomes sustainable at scale. For enterprises, this means growth, innovation, and regulatory confidence can move forward together rather than in conflict.
What Are The Features Of A Real-Time Clinical Data Sync Platfrom
A real-time clinical data sync platform is defined by how reliably it moves, manages, and protects information across healthcare systems. Its value does not come from a single function, but from how multiple capabilities work together to keep clinical data accurate, timely, and usable across the enterprise.
Below are the core features that distinguish a true clinical data sync platform from basic integration tools.
1. Real-time data synchronization
The platform ensures that updates made in one system appear across connected systems as they happen. This prevents delays caused by batch updates or manual refresh cycles.
Clinical teams, therefore, work with current information at every point of care. Over time, this reduces conflicting records between departments and partners. It also improves coordination without adding new operational steps.
2. Data validation and quality controls
As data moves, it is checked for completeness, accuracy, and consistency. Errors are flagged or corrected before they affect downstream workflows. This reduces the volume of queries and manual rework later.
It also increases trust in the data used for care, billing, and reporting. Over time, data quality becomes predictable rather than reactive.
3. Standards-based interoperability
The platform supports healthcare data standards such as FHIR, HL7, DICOM, and X12. This allows systems to exchange information without heavy customization. New partners and tools can be connected faster and with less friction.
Interoperability, therefore, becomes repeatable instead of project-specific. This shortens onboarding cycles across the enterprise.
4. Identity and patient matching
A strong platform ensures that records from different systems refer to the same patient correctly. It resolves duplicates and mismatches in real time as data flows. This prevents fragmented patient views across providers.
Accurate identity management also reduces clinical risk caused by misattribution. It is essential for both care quality and compliance.
5. Consent and access management
The platform controls who can access which data and under what conditions. It applies consent rules consistently across all connected systems.
This ensures patient preferences are respected at every point of data use. It also simplifies compliance across complex provider networks. Over time, access governance becomes embedded rather than enforced manually.
6. Monitoring and audit readiness
Every data movement is tracked and recorded by the platform. Enterprises gain visibility into who accessed what data and when. This supports investigations, compliance reviews, and internal audits.
It also reduces the effort needed to respond to regulatory requests. Over time, audit readiness becomes continuous rather than event-driven.
7. Scalability across networks
The platform is designed to grow as more systems, providers, and use cases are added. Performance remains stable even as data volumes increase. Enterprises can expand their digital ecosystems without redesigning their data foundation.
This prevents fragmentation as the organization evolves. Growth remains controlled and predictable.
Together, these features transform clinical data from a static record into a live enterprise asset. For healthcare organizations, this is what enables safer care, faster operations, and stronger regulatory confidence at scale.
How We Build Real-Time Clinical Data Sync Platforms for Enterprises
Building a real-time clinical data sync platform is not only about technology choices. It is about designing a system that can operate reliably in complex, regulated healthcare environments. Our approach focuses on long-term usability, compliance, and scalability rather than short-term integration wins.
Each step is shaped by how large healthcare enterprises actually function, not by how systems behave in controlled settings.
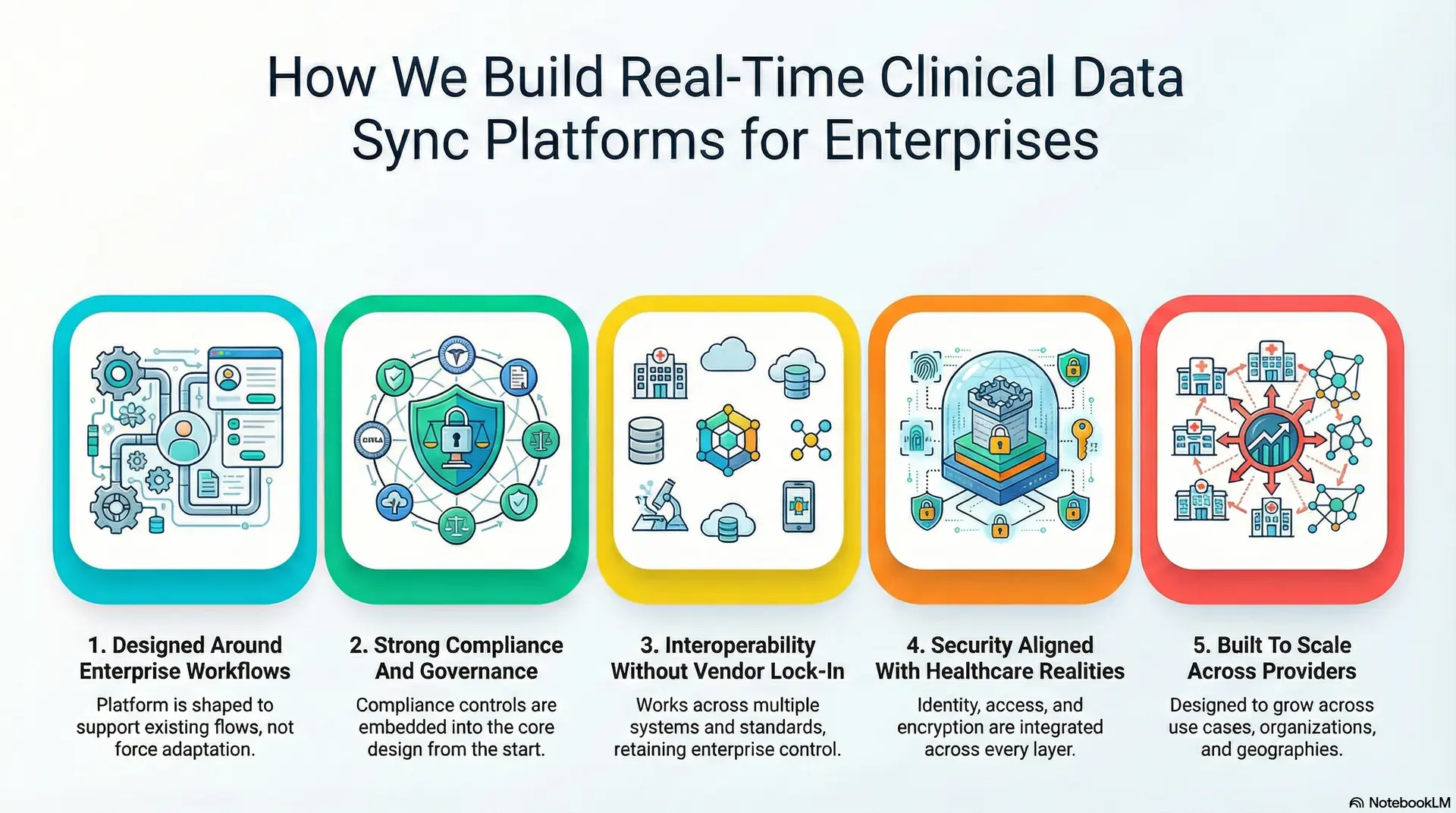
1. Designed Around Enterprise Workflows
We begin by understanding how data moves through real clinical and operational workflows. This includes care delivery, research operations, billing, and compliance processes.
The platform is shaped to support these flows instead of forcing teams to adapt to rigid systems. As a result, adoption becomes easier and operational disruption is minimized.
2. Strong Compliance And Governance
Rather than adding compliance controls later, we embed them into the core design. Consent management, audit trails, and access controls are treated as foundational components.
This allows enterprises to scale their data operations without increasing regulatory exposure. Over time, compliance becomes part of daily operations instead of a separate activity.
3. Interoperability Without Vendor Lock-In
We design platforms to work across multiple systems and standards without depending on a single vendor ecosystem. This allows enterprises to connect EHRs, devices, labs, and partner platforms with confidence.
As the technology landscape changes, the platform remains flexible. Enterprises retain control over their data strategy rather than surrendering it to tools.
4. Security Aligned With Healthcare Realities
Security is engineered to match the sensitivity and scale of healthcare data. Identity, access, and encryption are integrated across every layer of the platform.
This ensures that data remains protected as it moves across providers and partners. At the same time, clinical workflows remain fast and uninterrupted.
5. Built To Scale Across Providers
From the start, the platform is designed to grow across use cases, organizations, and geographies. Performance remains stable as data volumes and participants increase.
Regulatory differences across regions are handled without fragmenting the system. This allows enterprises to expand their networks without rebuilding their data foundation.
Our approach ensures that real-time clinical data sync platforms are not just deployed, but sustained and trusted at scale. For enterprises, this means gaining a strategic asset that supports growth, compliance, and innovation over the long term.
Cost Of Building A Real-Time Clinical Data Sync Platform
At Intellivon, real-time clinical data sync platforms are built as regulated healthcare data infrastructure, not as integration features layered onto existing systems. The focus stays on creating platforms that operate reliably across providers, partners, regions, and evolving healthcare regulations. Every design decision accounts for data governance, interoperability, security, and long-term compliance exposure from the start.
When budget constraints exist, scope is refined with intent. However, security controls, consent enforcement, auditability, and data integrity mechanisms are never reduced. Therefore, enterprises avoid remediation costs that often surface after launch. Predictability replaces rework, and long-term ROI remains protected.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Regulatory Alignment | Data scope definition, use case prioritization, jurisdiction mapping, and healthcare compliance assessment | $9,000 – $15,000 |
| Secure Architecture Design | Event-driven sync design, identity flows, consent logic, interoperability planning | $11,000 – $18,000 |
| Governance & Policy Framework | Access rules, data sharing policies, audit workflows, and exception handling | $9,000 – $16,000 |
| Backend & Enterprise Integrations | EHRs, lab systems, imaging, payer systems, device platforms | $18,000 – $32,000 |
| Data Normalization & Mapping | Semantic alignment, standard harmonization, terminology management | $10,000 – $17,000 |
| Role-Based Interfaces & Admin Tools | Clinical, compliance, and operations dashboards with access controls | $10,000 – $18,000 |
| Security & Compliance Controls | Encryption, monitoring, intrusion detection, and access enforcement | $11,000 – $19,000 |
| Testing & Regulatory Validation | Functional testing, security audits, compliance readiness | $7,000 – $12,000 |
| Deployment & Scale Readiness | Cloud or hybrid deployment, monitoring, and performance tuning | $8,000 – $14,000 |
Total initial investment: $93,000 – $161,000
Ongoing maintenance and optimization: ~15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped clinical data sync programs face pressure when indirect cost drivers are ignored. Planning for these early protects budgets, timelines, and compliance posture as data volumes and ecosystem complexity grow.
- Integration complexity rises as new EHRs, devices, and partner systems are added
- Compliance overhead increases due to audits, reporting obligations, and regulation updates
- Governance requires continuous policy tuning, consent reviews, and exception handling
- Infrastructure costs grow with data throughput, analytics, and monitoring workloads
- Change management includes onboarding clinical, compliance, and operations teams
- Continuous monitoring becomes essential as regulatory scrutiny increases
Best Practices to Avoid Budget Overruns
Based on Intellivon’s experience delivering enterprise healthcare data and AI platforms, these practices consistently lead to controlled costs and predictable outcomes.
- Start with a clearly defined data sync scope before expanding use cases or regions
- Embed governance, auditability, and security into the core architecture
- Use modular components that scale without redesign
- Plan interoperability early to avoid expensive retrofitting
- Maintain observability across performance, compliance, and data quality
- Design for regulatory evolution rather than one-time certification
Request a tailored proposal from Intellivon’s healthcare and AI experts to receive a delivery roadmap aligned with your budget constraints, compliance exposure, and long-term clinical data sync strategy.
Common Enterprise Failures in Clinical Data Sync Programs
Many clinical data sync initiatives fail not because of poor technology, but because of how they are planned and governed. Enterprises often underestimate the operational, regulatory, and organizational complexity involved.
When these factors are overlooked, even well-funded programs struggle to deliver value. Understanding these common failures helps organizations design platforms that scale reliably instead of collapsing under real-world pressure.
1. Treating sync as an IT project
The failure begins when clinical data sync is seen as a technical upgrade rather than an enterprise capability. In such cases, ownership remains isolated within IT teams, disconnected from clinical, compliance, and operations leadership. This leads to systems that technically work but fail in daily workflows.
We avoid this by aligning platform design with business, clinical, and regulatory stakeholders from the start. This ensures the system serves enterprise objectives, not just technical goals.
1. Underestimating governance and compliance
Many programs focus on moving data faster, but neglect how that data should be governed. When compliance is treated as an afterthought, enterprises face audit risks and operational rework. This often leads to delays and loss of trust across the organization.
We ensure governance and compliance are built into the platform itself, not layered later. As a result, regulatory alignment remains stable as scale increases.
2. Designing for one use case only
Some platforms are built around a single project or department. While this may succeed initially, it creates fragmentation when new use cases are added. Enterprises then face parallel systems and rising maintenance costs.
We design platforms to support multiple use cases from the beginning. This prevents structural limitations that restrict growth.
3. Allowing vendor lock-in
When critical data flows depend on proprietary tools, enterprises lose control over their own platforms. Over time, this reduces flexibility and increases long-term costs. It also limits the ability to adapt as technology or regulations change.
We avoid this by designing vendor-neutral architectures that keep strategic control within the enterprise.
4. Ignoring operational adoption
Even the best-designed systems fail if teams do not use them effectively. When workflows are disrupted or unclear, adoption slows, and workarounds appear. This weakens data reliability and consistency.
We ensure that platform design aligns with how teams actually work. This supports smoother adoption and sustained usage.
Clinical data sync programs succeed when they are treated as enterprise platforms, not technical shortcuts. By avoiding these common failures, organizations can build systems that remain reliable, compliant, and valuable as their ecosystems grow.
Conclusion
Real-time clinical data sync is no longer a supporting function. It is becoming a defining capability for how modern healthcare enterprises operate and compete. When data moves reliably across systems, decisions improve, risks decline, and teams work with greater clarity. Over time, this changes how care is delivered, how trials are run, and how partnerships scale.
Enterprises that invest early gain more than efficiency. They build a foundation for AI, automation, and new care models that can evolve with regulation and market demands. In this context, clinical data sync becomes not just an operational upgrade, but a growth enabler.
Build a Real-Time Clinical Data Sync Platform With Intellivon
At Intellivon, real-time clinical data sync platforms are built as regulated healthcare data infrastructure, not as integration layers stitched between systems. Every architectural and delivery decision prioritizes governance, compliance, and enterprise-scale interoperability. This ensures the platform performs reliably across real healthcare environments, not just controlled deployments.
As healthcare ecosystems expand across providers, regions, and business models, stability becomes critical. Governance, performance, and audit readiness remain consistent as scale increases. Enterprises retain control over their data and operations without introducing fragmentation, regulatory exposure, or operational drag.
Why Partner With Intellivon?
- Enterprise-grade healthcare data platform architecture
- Proven delivery across regulated, multi-provider ecosystems
- Compliance-by-design with continuous audit readiness
- Secure, modular, cloud-native infrastructure
- AI-ready data pipelines with governance and oversight
Book a strategy call to explore how Intellivon can help you build and scale a real-time clinical data sync platform with confidence.
FAQs
Q1. What is a real-time clinical data sync platform used for?
A1. A real-time clinical data sync platform is used to keep patient and clinical data aligned across systems as events happen. It ensures information remains accurate and consistent across providers, research sites, and applications. This supports safer care, faster operations, and stronger compliance at scale.
Q2. How is clinical data sync different from healthcare integration tools?
A2. Integration tools mainly move data between systems. Additionally, a clinical data sync platform manages how that data behaves across the enterprise. It governs accuracy, timing, access, and compliance, which makes it a strategic infrastructure layer rather than a technical connector.
Q3. Why is real-time data sync important for healthcare enterprises?
A3. Healthcare enterprises depend on timely and reliable information to make decisions. Real-time sync reduces delays, prevents data conflicts, and improves audit readiness. At the same time, it also enables AI and automation to operate on current clinical signals instead of outdated records.
Q4. What are the main challenges in building a clinical data sync platform?
A4. Common challenges include managing interoperability across systems, ensuring security during data transfer, enforcing consent and compliance, and scaling across providers and regions. At the same time, without addressing these early, platforms often fail to deliver long-term value.
Q5. How much does it cost to build a real-time clinical data sync platform?
A5. The cost varies based on scope, integrations, compliance requirements, and scale. Because of this, enterprise-grade platforms typically require an initial investment that ranges from mid-five to low-six figures, with ongoing costs tied to maintenance, optimization, and regulatory updates.