Patient data gets stuck because healthcare IT teams approach integration like a plumbing issue. Each new partner adds another direct connection. Every workflow change means rewriting data mappings. Eventually, data moves between systems, but nobody trusts it anymore. They ask questions like ‘Is this record complete? Is it current? Can I really use it to make care decisions?’
The issue worsens as care spreads across organizations. A patient may visit three different facilities in a week with an ER, a specialty clinic, and an imaging center. Clinicians need that patient’s history right away an not after someone hunts down the right system and requests access. At the same time, compliance officers also need to show exactly who accessed what data and when.
A real data exchange platform for hospitals has to work in actual clinical settings and help close this gap. That’s what we help organizations build at Intellivon. We collaborate with hospitals, EHR vendors, and partner networks to create data systems that protect patient identity, enforce consent rules, and create the audit trails regulators require. In this blog, we will draw from our experience to show you how we build such scalable platforms suited for enterprises from the ground up.
Why Enterprises Need Cross-Hospital Data Exchange Platforms Now
Enterprises now need cross-hospital data exchange platforms because regulatory frameworks such as TEFCA are pushing standardized data sharing across care networks. At the same time, care coordination demands are rising, while data silos continue to create inefficiencies that cost the healthcare industry billions every year.
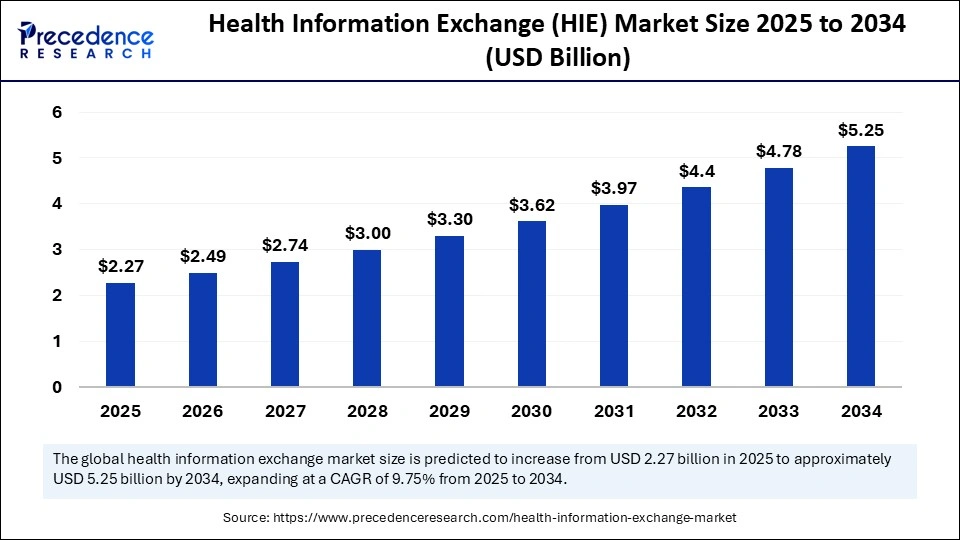
As a result, the market for Health Information Exchange solutions is growing rapidly, helping providers share data securely and in real time across organizations. The global Health Information Exchange (HIE) market is valued at about USD 2.27 billion in 2025. It is expected to grow to nearly USD 5.25 billion by 2034, with steady annual growth of around 9.75%.
Key Growth Drivers:
- Regulatory Momentum: TEFCA is accelerating nationwide data exchange adoption. As a result, Epic network expansions and hybrid exchange models are growing at roughly 13% annually.
- Digital Transformation Shift: Centralized exchange models hold about 46% market share in 2025. However, organizations are gradually moving toward hybrid models to support scale, aging populations, and rural access needs.
- Operational Efficiency: Real-time data sharing reduces duplicate tests, strengthens AI-driven analytics, and improves population health outcomes. Meanwhile, North America leads with about 42% share, largely driven by cloud-based HIE adoption.
Modern exchange platforms can drive 20–30% faster decisions, support chronic care coordination for nearly 60% of adults, and unlock over $15B in potential savings. Leading players like InterSystems and Cerner already scale to millions of patient records.
However, without a strong data exchange infrastructure, silos continue to slow AI/ML adoption and weaken payer–provider data connectivity.
What Is A Cross-Hospital Data Exchange Platform?
A cross-hospital Data Exchange Platform is an enterprise data infrastructure that enables hospitals, clinics, labs, and partners to securely share patient information in real time. It connects different EHR systems, standardizes clinical data, and enforces identity, consent, and access controls.
As a result, care teams can view the complete patient context across organizations. Therefore, providers make faster decisions, reduce duplicate tests, and improve coordination across the entire care network.
The Core Jobs It Must Do
A cross-hospital Data Exchange Platform must ensure the right data reaches the right care team at the right time. Therefore, enterprises must design platforms around real clinical and operational workflows.
As a result, exchange becomes a reliable infrastructure that supports daily care decisions and long-term network growth.
1. Enable Real-Time Clinical Data Access
Care teams need patient data instantly, especially during emergencies and transitions. Therefore, platforms must support real-time queries and event-based data sharing.
In addition, they must normalize data from multiple EHR systems. As a result, clinicians see the complete patient context without waiting for manual reconciliation.
2. Maintain Patient Identity Accuracy
Patient matching errors create clinical and financial risk. Therefore, platforms must include enterprise-grade identity matching and duplicate management workflows.
In addition, they must maintain audit history for merges and corrections. As a result, organizations protect patient safety and maintain trust in shared records.
3. Enforce Consent and Data Access Policies
Data sharing must follow patient consent and regulatory requirements. Therefore, platforms must enforce access rules automatically across partners.
In addition, they must track who accessed data and why. As a result, organizations maintain compliance while enabling secure collaboration.
4. Support Scalable Partner and Network Growth
Healthcare networks continue to expand through partnerships and acquisitions. Therefore, platforms must onboard new partners without rebuilding integrations.
In addition, they must standardize data exchange models across organizations. As a result, exchange remains stable as networks grow.
When these core functions work together, data exchange becomes operational infrastructure instead of integration overhead. Therefore, enterprises gain reliable data sharing, lower risk exposure, and stronger care coordination.
The Business Drivers Pushing Hospitals to Exchange Data Now
Hospitals are accelerating data exchange investments due to regulatory pressure, value-based care risk, network expansion, and rising operational cost leakage from disconnected patient data.
Therefore, data exchange has moved from an IT improvement project to a core business strategy. In addition, external pressure from regulators, payers, and partner networks continues to increase. As a result, organizations must exchange data reliably to remain competitive and compliant.
1. Regulatory Pressure Is Forcing Standardized Data Sharing
Governments and regulatory bodies now expect providers to exchange patient data across networks. Therefore, organizations must prove they can share data securely and consistently.
In addition, frameworks like TEFCA are pushing nationwide interoperability expectations. As a result, hospitals must build exchange infrastructure that supports long-term compliance instead of temporary integration fixes.
2. Value-Based Care Models Are Increasing Financial Risk
Payment models now tie revenue directly to patient outcomes and care continuity. Therefore, organizations lose revenue when they cannot track patient journeys across providers.
In addition, readmission penalties and quality metrics depend on complete patient data. As a result, cross-hospital exchange directly protects revenue and reduces cost leakage.
3. Network Expansion Is Increasing Data Complexity
Healthcare systems are growing through partnerships, acquisitions, and specialty collaborations. Therefore, patient data must move across multiple organizations and EHR environments.
In addition, partner ecosystems now include labs, imaging centers, and post-acute providers. As a result, manual or interface-based exchange models cannot scale reliably.
4. Operational Costs From Data Silos Continue to Rise
Disconnected data creates duplicate tests, delayed care decisions, and manual reconciliation work. Therefore, organizations spend more time fixing data gaps instead of improving care delivery.
In addition, silos reduce the effectiveness of analytics and automation initiatives. As a result, enterprises lose efficiency and slow down digital transformation programs.
Data exchange is no longer optional for modern healthcare networks. Instead, it directly supports compliance, revenue protection, and operational efficiency.
Therefore, organizations that invest in exchange platforms create a long-term strategic advantage. In addition, they build the foundation needed for advanced analytics, AI adoption, and coordinated care delivery across expanding care ecosystems.
HIE Use Cuts Readmissions by 57% and Saves ~$605K Annually
Financial impact often determines whether data exchange programs move forward or stall. Therefore, decision makers need proof that exchange improves outcomes and reduces avoidable costs. Research shows that when providers use shared exchange data after discharge, readmission odds drop by about 57% . In addition, one study estimated roughly $605K in annual savings from avoided readmissions in a community network.
These results matter because readmissions remain one of the largest cost drivers in healthcare. Meanwhile, value-based contracts continue to penalize preventable returns to care. As a result, organizations that cannot share patient context across hospitals struggle to control cost leakage and care continuity.
1. Why Readmissions Are a Cross-Hospital Data Problem
Most readmissions do not happen because care teams lack clinical skill. Instead, they often happen because teams lack complete patient context during transitions. For example, discharge medication changes may not reach the next care setting. Similarly, follow-up care plans may not be visible to outside providers.
Therefore, when hospitals exchange real-time patient data, teams can:
- Verify medication changes quickly
- Confirm follow-up care plans
- Identify high-risk patients earlier
- Reduce duplicate testing during transitions
As a result, care becomes coordinated across organizations instead of fragmented across systems.
2. Where Exchange Platforms Deliver the Most Financial Value
Exchange value usually appears first in high-volume workflows. Therefore, enterprises often see ROI in:
- Post-discharge monitoring: Reduces preventable returns within 30 days
- Emergency department encounters: Provides outside history immediately
- Chronic condition management: Improves visibility across long care journeys
- Network referral management: Prevents loss of patient context between facilities
In addition, these workflows scale across hospitals. Therefore, savings grow as network exchange maturity increases.
3. Why Point Integrations Cannot Sustain These Gains
Many organizations initially try to solve readmission risk using direct integrations. However, interface-based models break when networks expand. Each new partner adds complexity, maintenance cost, and governance risk.
Therefore, enterprises shift toward platform-based exchange because it:
- Centralizes identity matching
- Standardizes consent enforcement
- Maintains audit trails automatically
- Scales partner onboarding safely
As a result, data exchange becomes an operational infrastructure instead of project work.
The 57% readmission reduction signal is more than a clinical improvement metric. It demonstrates how shared patient data directly reduces cost exposure and operational risk. In addition, the estimated $605K annual savings show that exchange platforms create measurable financial return even at a regional scale.
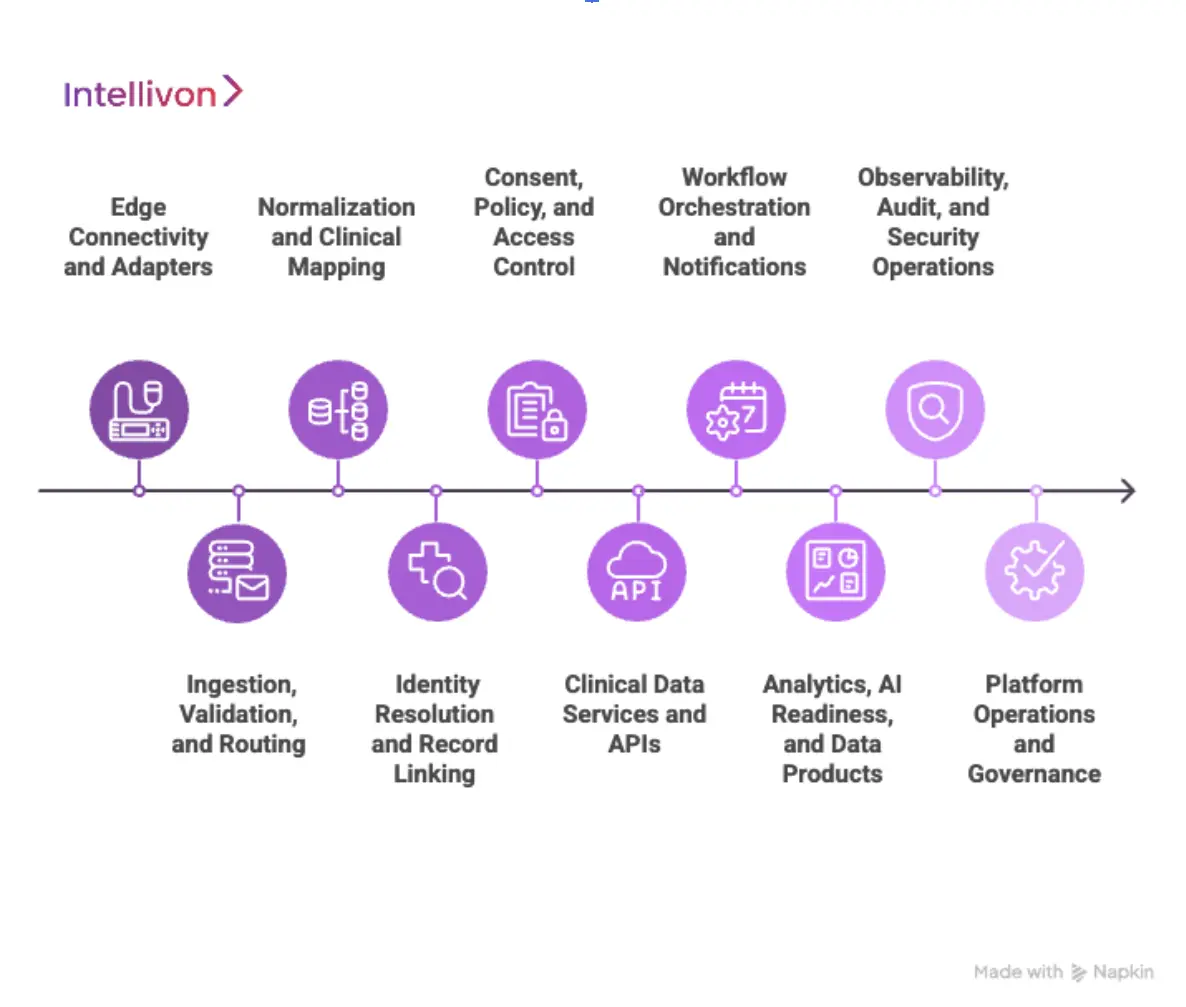
Architecture for Cross-Hospital Exchange Platforms
A strong exchange platform needs a clean architecture that teams can operate for years. Therefore, you should design it in layers with clear boundaries and ownership.
In addition, layered architecture reduces change risk when new hospitals, EHRs, or partners join. As a result, you can scale the exchange without rewriting core logic every time.
1) Edge Connectivity and Adapters
This layer connects to hospital systems and partner endpoints. Therefore, it supports multiple standards and transport methods from day one. In addition, it isolates vendor-specific complexity at the edge, so the core stays stable.
Typical inputs
- HL7 v2 feeds (ADT, ORU, ORM)
- C-CDA documents
- FHIR APIs
- SFTP files when unavoidable
2) Ingestion, Validation, and Routing
This layer receives messages, validates them, and routes them to the correct workflows. Therefore, it prevents bad data from flowing downstream. In addition, it assigns trace IDs so teams can debug and audit exchange events fast.
Core jobs
- Schema and rules validation
- Deduping messages at the transport level
- Routing by facility, service line, and event type
- Error handling and retry queues
3) Normalization and Clinical Mapping
This layer converts incoming data into a consistent internal structure. Therefore, exchange works across hospitals even when source systems differ. In addition, it supports terminology mapping so clinical meaning stays consistent.
Core jobs
- Map to a canonical model (often FHIR resources internally)
- Normalize units, codes, and reference ranges
- Apply terminology services (ICD, SNOMED, LOINC, RxNorm)
4) Identity Resolution and Record Linking
This layer determines who the patient is across hospitals. Therefore, it reduces safety risk and operational rework. In addition, it maintains merge history and supports controlled correction workflows.
Core jobs
- EMPI or MPI matching (deterministic + probabilistic)
- Duplicate detection and resolution workflows
- Cross-org identifier mapping
- Audit trails for merges and unmerges
5) Consent, Policy, and Access Control
This layer decides whether a user, system, or partner can access data for a specific purpose. Therefore, it turns privacy requirements into enforceable rules. In addition, it keeps policy decisions consistent across every channel.
Core jobs
- Consent capture and lifecycle management
- Purpose-based access controls
- Break-glass logic with strict audit
- Partner-specific policy enforcement
6) Clinical Data Services and APIs
This layer delivers data to apps, systems, and workflows. Therefore, it supports both clinician-facing needs and operational automation. In addition, it lets you serve multiple patterns without rebuilding the platform.
Delivery patterns
- Query and response APIs
- Push subscriptions and event notifications
- Document exchange plus discrete clinical data
- Bulk export for population and reporting use cases
7) Workflow Orchestration and Notifications
This layer connects the exchange to real operational actions. Therefore, data movement triggers outcomes, not just storage. In addition, it supports cross-hospital workflows where timing matters.
Common workflows
- ADT alerts to care, team,s and coordinators
- Referral intake and scheduling handoffs
- Discharge plan and medication reconciliation prompts
- Care gap outreach for high-risk cohorts
8) Analytics, AI Readiness, and Data Products
This layer turns exchanged data into enterprise intelligence. Therefore, leaders can measure impact and run network-level programs. In addition, it supports governed AI usage because it stabilizes data inputs.
Enterprise outputs
- Population health measures
- Leakage and referral analytics
- Risk stratification inputs
- Model monitoring and bias checks, when AI is used
9) Observability, Audit, and Security Operations
This layer proves reliability and supports compliance. Therefore, teams can trace every event end-to-end. In addition, security teams can detect anomalies before they become incidents.
Core jobs
- Central logging, metrics, and alerting
- End-to-end traceability per transaction
- Audit reports for access and disclosure
- Incident response workflows and evidence capture
10) Platform Operations and Governance
This layer keeps the platform manageable as it scales. Therefore, new hospitals and partners are on board faster. In addition, it ensures standards stay consistent across teams.
Core jobs
- Partner onboarding playbooks and checklists
- Change control for mappings and policies
- Versioning for APIs and canonical models
- SLA management and operational runbooks
Layered architecture makes cross-hospital exchange predictable and scalable. Therefore, each team can own a layer without breaking others.
In addition, the platform can expand across hospitals, partners, and regions while keeping identity, consent, and audit controls intact. As a result, leaders get reliable data exchange that supports care coordination today and an AI-ready strategy tomorrow.
Data Standards Strategy In A Cross-Hospital DXP
Most hospitals cannot replace legacy standards overnight. Therefore, enterprises must support HL7 v2, C-CDA, and older workflows while moving toward modern FHIR-based exchange.
In addition, forcing a sudden migration increases operational risk and clinician disruption. As a result, successful organizations adopt a phased standards strategy that modernizes exchange without breaking existing care workflows.
1. Use FHIR As The Internal Canonical Data Model
FHIR works best when it standardizes data inside the platform, not just at the API layer. Therefore, teams should normalize incoming data into FHIR resources before downstream processing.
In addition, this approach keeps clinical meaning consistent across hospitals and EHRs. As a result, analytics, AI models, and clinical workflows can rely on stable data structures.
Why this matters
- Creates consistent data meaning across organizations
- Simplifies future partner onboarding
- Supports modern app ecosystems and APIs
- Enables long-term AI and analytics readiness
2. Continue Supporting Legacy Standards At The Edge
Legacy standards still power core hospital workflows. Therefore, platforms must support HL7 v2 feeds, C-CDA documents, and older transport methods. In addition, isolating legacy complexity at the connectivity layer protects the core platform. As a result, hospitals can modernize gradually without disrupting daily operations.
Typical legacy inputs
- HL7 v2 ADT, lab, and order messages
- C-CDA transition of care documents
- Batch or file-based clinical data feeds
3. Use Terminology Mapping To Preserve Clinical Meaning
Data format conversion alone is not enough. Therefore, platforms must include terminology services to map clinical codes consistently. In addition, standard code mapping reduces interpretation errors across hospitals. As a result, clinicians and analytics systems can trust the exchanged data.
Common terminology standards
- SNOMED CT for clinical concepts
- LOINC for lab observations
- RxNorm for medications
- ICD for diagnoses and billing
4. Phase Modernization Based On Business Value
Modernization should follow care and operational priorities. Therefore, organizations should upgrade high-impact workflows first. In addition, early success builds internal trust and funding support. As a result, standards transformation becomes sustainable instead of disruptive.
Common phased approach
- Normalize ADT and patient identity first
- Modernize the lab and medication exchange next
- Expand to imaging, notes, and specialty data
- Enable full FHIR APIs for partner ecosystems
A strong standards strategy balances modernization and operational safety. Therefore, organizations should adopt FHIR as the core data foundation while supporting legacy standards at the edge.
In addition, terminology governance ensures that data keeps the same meaning across hospitals. As a result, enterprises can scale exchange, support new partners, and prepare for advanced analytics without creating operational chaos.
Security, Privacy, and Compliance Controls You Must Design In
Security and privacy failures can shut down exchange programs quickly. Therefore, organizations must design controls into the platform from day one. In addition, retrofitting compliance later increases cost and operational risk.
As a result, leading enterprises treat security and privacy as core platform capabilities, not external review steps.
1. Enforce Identity-Centric Access Control
Every data request must connect to a verified identity. Therefore, platforms must enforce strong authentication and role-based access controls.
In addition, purpose-based access ensures users only see data needed for their workflow. As a result, organizations reduce insider risk and unauthorized data exposure.
Key capabilities
- Multi-factor authentication
- Role-based and attribute-based access control
- Session monitoring and anomaly detection
- Context-aware access policies
2. Build Consent Enforcement Into Data Flows
Consent must control data movement, not just data storage. Therefore, platforms must evaluate consent rules before releasing data.
In addition, consent status must update dynamically as patient preferences change. As a result, organizations can share data safely across hospitals and partners.
Core controls
- Consent capture and lifecycle tracking
- Cross-organization consent enforcement
- Emergency access with strict audit logging
- Partner-specific data sharing restrictions
3. Encrypt Data Across All Exchange Stages
Patient data must remain protected during transmission and storage. Therefore, platforms must enforce encryption for data in motion and at rest.
In addition, strong key management prevents unauthorized decryption. As a result, organizations reduce breach risk and meet regulatory requirements.
Security foundations
- TLS for network transmission
- Database and storage encryption
- Centralized key lifecycle management
- Secure secrets storage
4. Maintain Full Audit and Traceability Coverage
Audit readiness is critical for compliance and investigations. Therefore, platforms must log every access event and data exchange transaction. In addition, logs must support long-term retention and rapid search. As a result, organizations can prove compliance during audits and incident reviews.
Audit requirements
- User activity logging
- API and system access tracking
- Data disclosure history
- Automated audit report generation
5. Design Multi-Tenant Security Boundaries
Cross-hospital platforms must isolate data across organizations. Therefore, systems must enforce tenant-level data separation. In addition, policy enforcement must remain consistent across tenants. As a result, organizations can safely onboard partners without increasing exposure risk.
Tenant protection controls
- Logical and data-level isolation
- Partner-specific encryption keys
- Independent access policy enforcement
- Segmented monitoring and alerting
Strong security and compliance architecture enables safe data exchange at scale. Therefore, organizations must design identity, consent, encryption, and audit controls into the core platform.
In addition, these controls support regulatory compliance while enabling secure collaboration. As a result, enterprises can expand exchange networks confidently while protecting patient data and organizational reputation.
How We Build A Cross-Hospital Data Exchange Platform
Cross-hospital exchange succeeds when teams build it like long-term infrastructure. Therefore, we start with operational realities, not ideal diagrams. In addition, we design every layer for auditability, safety, and scale from day one. As a result, enterprises avoid fragile integrations and build a platform they can expand across hospitals and partners with confidence.
1. Align The Platform To Business Outcomes
We begin by defining what the platform must change in real operations. Therefore, we map the workflows that drive cost, risk, and care quality.
In addition, we confirm which partners, hospitals, and service lines matter first. As a result, the platform launch targets measurable outcomes, not vague interoperability goals.
What we lock early
- Priority workflows such as ED lookup, referrals, and discharge exchange
- Data domains such as meds, labs, problems, and care plans
- Stakeholders for clinical, compliance, security, and operations
- KPIs tied to readmissions, duplication, and throughput
2. Establish Governance, Identity, And Consent Foundations
Exchange breaks when governance starts late. Therefore, we define data ownership, policy rules, and change control upfront.
In addition, we design identity resolution and consent enforcement as core platform services. As a result, the platform remains trustworthy as hospitals and partners join.
Key deliverables
- Identity strategy using EMPI or MPI with correction workflows
- Consent models tied to purpose-based access
- Partner onboarding policy and approvals
- Audit model for every access and disclosure event
Step 3: Build The Connectivity And Ingestion Layer
We then connect to real hospital systems in the formats they already use. Therefore, we support HL7 v2, C-CDA, and FHIR without forcing disruptive upgrades.
In addition, we add validation, routing, and error handling from the start. As a result, data quality improves before it reaches clinical workflows.
What we implement
- Standard adapters for common EHR and ancillary systems
- Validation rules and retry queues
- Trace IDs for end-to-end tracking
- Secure transport and partner handshake methods
Step 4: Normalize Data Into A Canonical Clinical Model
After ingestion, we normalize data so it stays consistent across hospitals. Therefore, we map incoming formats to a canonical model, often using FHIR resources internally.
In addition, we apply terminology mapping so the clinical meaning stays stable. As a result, downstream applications and analytics can rely on predictable structures.
Core components
- Normalization pipelines with version control
- Terminology services for LOINC, RxNorm, SNOMED, and ICD
- Data quality scoring and exception handling
- Record provenance and source attribution
Step 5: Deliver Exchange Through Real Workflow Services
A platform must support daily workflows, not only API calls. Therefore, we implement query, push, and event-based exchange patterns aligned to use cases.
In addition, we design response behavior for speed and reliability under peak load. As a result, care teams and operational teams experience immediate value.
Common workflow services
- ED lookup for outside history
- Admit, discharge, transfer alerts
- Discharge package exchange to partner facilities
- Referral handoff data services
- Lab and imaging result routing across organizations
Step 6: Embed Security, Audit, And Observability
We then harden the platform for real operations. Therefore, we instrument every transaction with logging, monitoring, and audit-ready trails. In addition, we define incident response flows and evidence capture. As a result, enterprises can prove compliance and maintain uptime during high-pressure periods.
What we include
- Role-based and attribute-based access controls
- Consent enforcement in every release decision
- Immutable audit logs and reporting
- Monitoring dashboards, alerts, and runbooks
Step 7: Scale Partner Onboarding With A Repeatable Model
Scale requires repeatability. Therefore, we create a standard onboarding playbook for hospitals, labs, and partners. In addition, we use templates for mappings, policies, and testing. As a result, onboarding becomes a controlled process, not a custom engineering effort each time.
Operational playbook
- Partner certification checklist
- Data mapping and validation test suites
- Security and privacy approvals
- Go-live monitoring and stabilization plan
Step 8: Expand Into Analytics And Enterprise AI Readiness
Once exchange stabilizes, leaders want intelligence and automation. Therefore, we build governed data products for population health and operational insights. In addition, we support AI enablement with strong lineage, monitoring, and controls. As a result, enterprises can scale analytics safely without data drift and trust failures.
Typical expansion outcomes
- Network-wide risk stratification inputs
- Leakage and referral analytics
- Care gap identification for chronic cohorts
- Workflow automation with oversight
A cross-hospital exchange platform must earn trust through reliability, not promises. Therefore, Intellivon builds these platforms as regulated, enterprise-grade infrastructure designed for scale from the start.
In addition, our step-by-step delivery model reduces risk while delivering early operational wins. As a result, enterprises gain a platform that supports compliance, improves coordination, and enables growth across expanding care networks.
Cost Of Building A Cross-Hospital Data Exchange Platform
At Intellivon, cross-hospital data exchange platforms are built as a regulated healthcare data infrastructure, not as interoperability features layered onto existing hospital systems. The focus stays on creating platforms that operate safely across hospitals, EHR vendors, partner ecosystems, and evolving regulatory environments.
When budget constraints exist, scope is refined with intent. However, identity matching, consent enforcement, security controls, and auditability are never reduced. Therefore, enterprises avoid remediation costs that typically appear after launch.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Exchange Strategy | Exchange scope definition, partner mapping, regulatory alignment, data domain prioritization | $5,000 – $10,000 |
| Secure Platform Architecture Design | Layered exchange architecture, identity flows, consent enforcement, audit design | $7,000 – $14,000 |
| Governance & Policy Framework | Data sharing rules, consent models, partner onboarding workflows, audit policy | $6,000 – $12,000 |
| Connectivity & Core Integrations | Initial EHR integration, core partner connectivity, routing setup | $12,000 – $28,000 |
| Clinical Data Normalization & Terminology | FHIR mapping, terminology services, data quality pipelines | $8,000 – $18,000 |
| Identity Resolution Setup (MPI / EMPI Foundation) | Matching configuration, duplicate workflows, and identity governance setup | $7,000 – $15,000 |
| Security, Privacy & Compliance Controls | Encryption, access enforcement, monitoring setup, consent enforcement | $6,000 – $14,000 |
| Testing & Compliance Validation | Functional testing, data validation, security testing, and audit readiness validation | $5,000 – $10,000 |
| Deployment & Scale Readiness | Cloud or hybrid deployment, monitoring dashboards, performance tuning | $4,000 – $9,000 |
Total initial investment: $50,000 – $150,000
Ongoing maintenance and optimization: ~15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped exchange programs face pressure when indirect cost drivers are ignored. Therefore, planning for these early protects budgets, timelines, and compliance posture as partner networks and data volume grow.
- Integration complexity increases as hospitals, EHRs, and partner systems expand
- Compliance overhead grows due to audits, reporting, and regulatory updates
- Governance requires continuous policy tuning, consent reviews, and partner rule enforcement
- Infrastructure costs increase as data exchange volume and analytics workloads grow
- Change management includes onboarding clinical, IT, compliance, and operations teams
- Continuous monitoring becomes critical as the exchange becomes mission-critical
Best Practices To Avoid Budget Overruns
Based on Intellivon’s experience delivering enterprise healthcare data platforms, these practices consistently drive controlled costs and predictable outcomes.
- Start with clearly defined exchange workflows before expanding partner networks
- Embed identity, governance, consent, and auditability into core architecture
- Use modular platform components that scale without redesign
- Plan terminology and interoperability strategy early
- Maintain observability across performance, security, and compliance
- Design for regulatory evolution instead of one-time certification
Request a tailored proposal from Intellivon’s healthcare platform experts to receive a delivery roadmap aligned with your budget constraints, compliance exposure, and long-term cross-hospital data exchange strategy.
Top Examples Of Cross-Hospital Data Exchange Platforms
Several real-world platforms already enable cross-hospital data exchange at scale. Therefore, studying how they work helps enterprises understand what successful exchange looks like in production environments.
In addition, these platforms show how data moves across hospitals using a mix of standards, identity matching, and governance controls. As a result, organizations can visualize how exchange supports real care workflows, not just technical connectivity.
1. Epic Care Everywhere
Epic Care Everywhere enables hospitals to retrieve patient records from other healthcare organizations during care delivery. Therefore, clinicians can request outside records directly inside their workflow. In addition, the platform supports exchange across Epic and non-Epic systems.
How data exchange happens
- Hospitals query external organizations for patient records
- Clinical summaries and documents are exchanged in real time
- FHIR APIs enable patient-directed and app-based data sharing
- Identity matching connects patient records across organizations
As a result, care teams can access outside medical history instantly during treatment.
2. InterSystems HealthShare
InterSystems HealthShare creates a unified longitudinal patient record across multiple hospital systems. Therefore, providers can view a single patient timeline across organizations. In addition, the platform normalizes data before sharing it.
How data exchange happens
- Data is ingested from multiple EHR systems
- Clinical data is normalized into a common data model
- Exchange occurs through APIs, messaging, and query workflows
- Analytics and workflow tools use unified patient data
As a result, hospitals exchange data while maintaining consistent clinical meaning.
3. HealthShare Exchange (Regional HIE Model)
HealthShare Exchange connects hospitals, providers, and payers across a regional network. Therefore, providers can access recent patient care data regardless of where care happened. In addition, the platform supports event notifications.
How data exchange happens
- Hospitals send clinical data to a shared exchange network
- Providers query the network during patient encounters
- Event alerts notify providers when patients receive care elsewhere
- Clinical and payer data combine for care coordination workflows
As a result, providers gain visibility across regional care journeys.
4. VA and DoD Bidirectional Health Information Exchange
The VA and Department of Defense exchange clinical data across federal healthcare systems. Therefore, military and veteran providers can access patient records across organizations. In addition, the exchange supports large national-scale operations.
How data exchange happens
- Structured clinical data flows between federal EHR systems
- Pharmacy, lab, imaging, and encounter data exchange automatically
- Identity correlation links patient records across agencies
- Exchange occurs continuously as care events happen
As a result, providers maintain continuity of care across national systems.
5. Hixny Regional Exchange Network
Hixny connects hospital and provider data across New York regions. Therefore, providers can access patient data regardless of care location. In addition, the network integrates into the statewide exchange infrastructure.
How data exchange happens
- Hospitals send clinical data to a shared regional exchange
- Providers retrieve patient data during encounters
- Data feeds into statewide exchange networks
- Identity matching prevents duplicate patient records
As a result, providers gain a complete patient view across regions.
These platforms show that successful cross-hospital exchange depends on standardized data models, strong identity matching, and real-time access workflows. Therefore, exchange platforms must support query, event, and API-based data sharing simultaneously.
Conclusion
Cross-hospital data exchange is becoming core healthcare infrastructure. Therefore, organizations that invest early gain stronger care coordination, better cost control, and faster clinical decisions. In addition, exchange platforms create the foundation for analytics, automation, and AI-driven care models.
As networks grow and regulations tighten, reliable data sharing becomes a competitive advantage. Intellivon helps enterprises build secure, scalable exchange platforms that support long-term growth, compliance readiness, and real operational resilience across care ecosystems.
Build a Cross-Hospital Data Exchange Platform With Intellivon
At Intellivon, cross-hospital data exchange platforms are built as regulated healthcare data infrastructure designed for secure, compliant data sharing across hospitals and partner ecosystems. Every architecture and delivery decision prioritizes governance, identity integrity, consent enforcement, and audit-ready data access. As a result, exchange platforms operate reliably across EHR systems, hospitals, and exchange networks from day one.
As exchange expands across regions and partners, stability becomes critical. Governance, performance, and audit readiness remain consistent as data volume and connections grow. Organizations retain control over identity, consent, and data access without introducing fragmentation or regulatory risk.
Why Partner With Intellivon?
- Enterprise-grade healthcare data platform architecture for multi-hospital environments
- Proven delivery across hospital networks, HIE ecosystems, and interoperability programs
- Compliance-by-design architecture with built-in audit trails and policy enforcement
- Advanced identity matching and patient record linking capabilities
- Consent-driven data exchange across partners and jurisdictions
- Secure modular platform supporting cloud, hybrid, and on-prem deployments
- Real-time exchange support across query, event, and API-based data flows
- Scalable partner onboarding frameworks and governance workflows
- AI-ready data infrastructure supporting analytics, automation, and predictive insights
- Full observability across performance, security, and compliance operations
Book a strategy call to explore how Intellivon can help you build and scale a cross-hospital data exchange platform with confidence, compliance control, and long-term enterprise value.
FAQs
Q1. What is a cross-hospital data exchange platform?
A1. A cross-hospital data exchange platform is an enterprise data infrastructure that enables hospitals, clinics, labs, and partners to securely share patient data in real time. It connects different EHR systems, standardizes clinical data, and enforces identity, consent, and access controls. As a result, care teams can view complete patient history across organizations and make faster, safer clinical decisions.
Q2. How is a data exchange platform different from an HIE?
A2. An HIE typically focuses on regional data sharing networks and centralized data access. However, a data exchange platform is broader and acts as an enterprise infrastructure. It supports multiple exchange models, partner ecosystems, and workflow integrations. Therefore, organizations use exchange platforms to support a long-term interoperability strategy, not only regional data access.
Q3. Do I need FHIR to build a cross-hospital data exchange?
A3. You do not need FHIR everywhere on day one. However, most modern exchange platforms use FHIR as the internal data model or API layer. In addition, organizations usually continue supporting HL7 v2 and document standards at the edge. As a result, enterprises can modernize exchange safely while maintaining legacy workflows.
Q4. What data should we exchange first between hospitals?
A4. Most organizations start with high-impact continuity of care data. This typically includes patient demographics, encounters, medications, allergies, lab results, and care plans. Therefore, providers gain immediate clinical value. In addition, starting with core clinical data reduces implementation risk and speeds early ROI.
Q5. What are the biggest risks when scaling hospital-to-hospital data sharing?
A5. The biggest risks usually involve identity matching failures, inconsistent consent enforcement, and weak governance controls. In addition, poor data normalization can create clinical safety issues. As a result, organizations must design identity, consent, security, and audit controls into the core platform architecture from the start.