AI is being continuously integrated into healthcare functions in 2026 as a long-term operational choice. This decision shapes clinical reliability, regulatory risk, and financial planning for years. As AI becomes more integrated into care delivery, patient engagement, and operations, the question shifts from whether to invest to how to invest wisely and at scale.
In this context, the cost to build an AI healthcare app in 2026 typically ranges from $40,000 for a limited solution to over $400,000 for enterprise-grade platforms. Complex deployments can cost even more as integration and compliance needs grow. However, this figure alone does not fully explain what organizations are really paying for.
At Intellivon, AI healthcare platforms are designed as regulated digital systems rather than experimental tech. Every design decision is guided by factors like architecture, governance, and scalability from the very beginning. This blog explains where these costs come from, why they vary so much, and how to plan an AI healthcare investment that ensures control, resilience, and measurable growth.
Why Businesses Are Investing in AI Healthcare Apps
The growing emphasis on compliance is reshaping how AI healthcare apps are being designed and budgeted at the enterprise level. For organizations evaluating the cost to build AI-driven healthcare platforms, regulatory readiness is no longer a side consideration. It now sits at the center of architectural and financial planning.
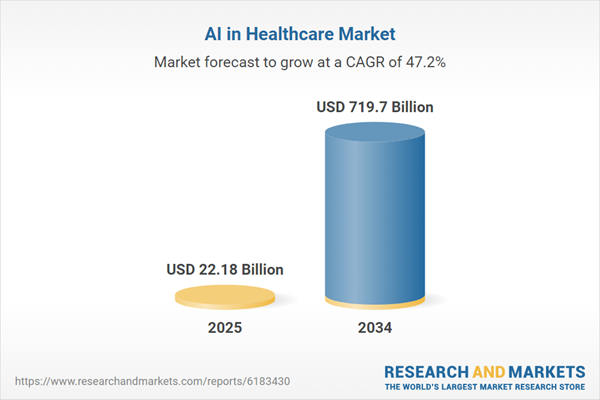
According to Research and Markets, the AI in healthcare market is entering a phase of exponential growth. In 2025, it is valued at USD 22.18 billion. By 2034, it is expected to reach USD 719.7 billion, expanding at a CAGR of 47.2%. However, this surge reflects more than rising adoption. It signals a deeper shift in how healthcare enterprises perceive digital platforms.
Enterprises increasingly expect AI-powered systems to manage privacy, automate governance, and reduce operational exposure by design. Therefore, investment decisions are now tied as much to compliance and risk control as to innovation itself.
Market Growth Drivers
Emerging frameworks such as the 2025 HIPAA Security Rule are accelerating this shift. As digital health ecosystems become more interconnected, compliance can no longer be treated as a layer added after deployment.
At the same time, enterprises are adopting AI to manage data growth, clinician shortages, and rising operational expenses. This adoption is being enabled by advances in diagnostics, ambient documentation, and virtual care integration, all of which require deeper system-level investment rather than surface-level application development.
Early pilots already show:
- 30–50% reductions in documentation workload
- 10–20% cost savings in high-friction areas such as prior authorization and imaging workflows
Why ROI Is Now Driving Budget Decisions
The ROI case for AI healthcare apps is becoming increasingly concrete for enterprises, which is changing how cost is evaluated during planning phases. Organizations now report:
- 15–25% faster revenue cycle processing, strengthening cash flow and financial stability
- 20–35% improvements in claims accuracy, reducing leakage and compliance risk
In parallel, AI-led care coordination and predictive interventions are driving 10–18% reductions in avoidable readmissions, improving both outcomes and cost efficiency.
At the same time, large-scale investments indicate where the market is heading. Leaders such as IBM, Oracle (Cerner), and Philips now hold major positions across AI healthcare platforms. Moreover, around 78% of organizations already use AI across core functions, while healthcare itself is growing at a 36.8% adoption CAGR.
Together, these trends explain why enterprises are no longer asking whether they should invest in AI healthcare apps, but how to structure that investment responsibly and at scale.
How Much Does It Really Cost to Build an AI Healthcare App in 2026?
The cost to build an AI healthcare app in 2026 typically ranges from $40,000 for focused pilots to $400,000+ for enterprise-grade platforms, depending on scale, compliance depth, and system complexity.
There is no single price for an AI healthcare app, because organizations build very different things under the same label. Some deploy a narrow AI feature to solve one problem. Others build full digital platforms that support clinical, financial, and operational workflows across regions.
Therefore, understanding cost begins with understanding what kind of system you are planning to build.
AI Healthcare App Cost Comparison by Deployment Type (2026)
| Deployment Type | Typical Use Case | Complexity Level | Expected Cost Range |
| Focused AI Pilot | Single AI function within one hospital or department | Low | $40,000 – $80,000 |
| Multi-Site Healthcare Platform | Multiple AI workflows across clinics or departments | Medium | $100,000 – $250,000 |
| Enterprise Healthcare Platform | Payer/provider systems spanning regions or markets | High | $300,000 – $400,000+ |
Tier 1: A Small, Focused AI Healthcare Solution
This tier applies when AI is introduced to solve one clear problem within a limited environment. For example, a hospital may deploy AI only for clinical documentation or appointment triage in one department.
Typical cost range:
$40,000 – $80,000
At this level, the scope remains controlled. The system usually:
- Supports a single AI use case
- Connects to a limited number of data sources
- Serves a small group of users
- Operates within one organization
Because of this, development remains focused and predictable. In addition, regulatory exposure stays limited, which keeps engineering effort manageable.
However, this tier is best suited for validation and early learning, not for large-scale transformation.
Tier 2: A Multi-Site AI Healthcare Platform
This tier applies when AI is rolled out across multiple facilities or departments. For instance, a healthcare group may use AI for diagnostics, patient engagement, and workflow automation across several clinics.
Typical cost range:
$100,000 – $250,000
Here, complexity increases naturally. The platform now:
- Handles multiple AI workflows
- Integrates with EHR systems
- Enforces role-based access
- Applies stronger compliance controls
As a result, cost rises not because AI becomes harder, but because the system must support more users, more data, and stricter governance. In other words, the platform must behave reliably under operational pressure.
This tier is where many enterprises begin seeing measurable returns from AI.
Tier 3: An Enterprise-Grade AI Healthcare Platform
This tier applies when AI becomes part of the core healthcare infrastructure. Examples include payer systems, cross-region provider networks, or national digital health platforms.
Typical cost range:
$300,000 – $400,000+
At this level, the platform must:
- Operate across regions or markets
- Enforce advanced regulatory compliance
- Monitor AI decisions continuously
- Support high availability and disaster recovery
- Scale without performance loss
Therefore, this is not simply a larger app. It is a digital healthcare infrastructure built for long-term operation, not short-term deployment.
Why Does This Cost Range Exist?
The wide range in healthcare app costs is not arbitrary. It exists because every added layer of scale introduces new demands.
In simple terms:
- More data requires stronger handling and security
- More users require better access control
- More regulations require deeper compliance engineering
- More scale requires a stronger system architecture
As a result, cost increases as responsibility increases.
What These Numbers Usually Include
Most development estimates typically cover:
- Application design and development
- Core AI feature integration
- Basic security measures
- Testing and initial deployment
This is enough to launch a working platform. However, it is not enough to guarantee long-term sustainability.
What These Numbers Often Exclude
Many organizations are surprised later by costs related to:
- Ongoing AI monitoring and tuning
- Major EHR rework or expansion
- Continuous compliance audits
- Infrastructure scaling as usage grows
Therefore, planning must extend beyond launch cost and include how the system will operate year after year.
Most organizations do not overspend because AI is expensive. They overspend because scope, scale, and responsibility are not mapped clearly from the beginning.
When cost is tied directly to purpose, AI healthcare investments become far more predictable and far more defensible at the enterprise level.
Type of AI Healthcare App And How It Affects Cost
Different types of AI healthcare apps carry different cost profiles depending on clinical risk, regulatory exposure, data complexity, and system integration depth.
Not all AI healthcare apps are built for the same purpose. As a result, they do not carry the same cost structure either. Two organizations may both say they are building “an AI healthcare app,” yet their budgets can differ dramatically because the systems they are building serve very different roles inside the enterprise.
Therefore, understanding what type of AI healthcare app you are building is one of the most important steps in estimating cost realistically.
To make this clearer, AI healthcare apps can be grouped into four broad categories based on how they function within healthcare operations.
A quick comparison of AI healthcare app types
| AI Healthcare App Type | Primary Role | Cost Impact | Main Cost Driver |
| Clinical AI Applications | Support clinical decisions | High | Validation, compliance, governance |
| Patient-Facing AI Applications | Engage and guide patients | Medium | UX, personalization, scale |
| Operational AI Applications | Optimize back-office workflows | Medium to High | System integration depth |
| Population & Predictive AI Applications | Forecast outcomes and risk | Medium | Data quality and analytics infrastructure |
This table gives a high-level view. However, the real cost behavior becomes clearer when we look at each type more closely.
1. Clinical AI Applications
(Higher cost due to clinical responsibility and regulatory exposure)
Clinical AI systems directly influence patient care. Because of that, they operate under the highest level of scrutiny.
These applications are typically used for:
- AI-powered clinical documentation and ambient scribing
- Diagnostic decision support
- Medical imaging and radiology analysis
- Triage and symptom assessment
Cost tends to be higher here because clinical systems must be safe, explainable, and auditable. In addition, they often require human oversight by design.
What usually drives cost in this category:
- Clinical validation and testing
- Strong compliance and audit layers
- Human-in-the-loop workflows
- Liability and governance controls
Therefore, cost increases not because the AI is complex, but because the responsibility attached to its decisions is high.
2. Patient-Facing AI Applications
(Moderate cost with a strong focus on experience and scale)
Patient-facing AI systems interact directly with users but do not usually make final clinical decisions. As a result, their regulatory exposure is lower compared to clinical AI.
These applications commonly include:
- Virtual health assistants
- AI chatbots for support and guidance
- Care navigation tools
- Personalized health coaching platforms
Here, cost is influenced less by compliance and more by how well the system can engage users at scale.
Key cost drivers in this category include:
- User experience design and accessibility
- Personalization and recommendation logic
- Multi-language and multi-device support
- Integration with patient portals and apps
Because deployment is faster and risk is lower, many organizations start their AI journey with patient-facing systems before moving deeper into clinical workflows.
3. Operational AI Applications
(Integration-heavy systems with strong ROI potential)
Operational AI focuses on the administrative and financial backbone of healthcare. While these systems rarely touch clinical decisions, they carry significant integration complexity.
Common use cases include:
- Billing and coding automation
- Claims processing and adjudication
- Scheduling optimization
- Prior authorization workflows
In this category, cost is driven more by system complexity than by AI sophistication.
What usually increases cost here:
- Integration with multiple legacy systems
- Complex business rules
- Data standardization across sources
- High reliability requirements
However, these systems often deliver some of the fastest financial returns, which is why enterprises frequently prioritize them early in AI adoption.
4. Population Health and Predictive AI Applications
(Data-heavy systems with ongoing cost profiles)
These AI systems focus on understanding patterns across large datasets rather than individual interactions. As a result, their cost behavior is shaped by data volume and analytics infrastructure.
Typical use cases include:
- Risk stratification
- Readmission prediction
- Capacity and demand forecasting
- Disease surveillance and early warning systems
Here, cost is influenced less by interfaces and more by how data flows through the system.
Primary cost drivers include:
- Data quality and data engineering effort
- Longitudinal data management
- Ongoing model tuning and updates
- Large-scale analytics infrastructure
Therefore, while initial build costs may appear moderate, long-term operational costs can be significant if data pipelines are not designed carefully.
Why this distinction matters for cost planning
Most organizations overspend not because AI is expensive, but because they choose the wrong system type for their actual business objective.
When cost is mapped to system purpose rather than abstract technology, budgeting becomes far more predictable. It also becomes easier to defend AI investments internally because each cost line connects directly to a business outcome.
In the next section, we will look at the specific factors that drive cost within these systems, so you can see where budgets expand or remain controlled in real-world deployments.
What Actually Drives the Cost of an AI Healthcare App?
The cost of an AI healthcare app is shaped more by data, compliance, integration, deployment, and long-term operations than by features or algorithms alone.
Most organizations assume that AI increases cost because the technology itself is complex. In practice, cost rises because AI healthcare apps must operate safely, securely, and reliably inside highly regulated and interconnected environments. Therefore, the real cost drivers sit deeper than user interfaces or even AI models.
Let’s examine the factors that most directly shape healthcare app cost in real-world deployments.
1. Data readiness
AI healthcare systems depend on clean, structured, and accessible data. However, healthcare data rarely exists in a form that can be used immediately. Records are often fragmented across systems, stored in different formats, and governed by varying access rules.
Therefore, significant effort goes into preparing data before AI can generate any value. This preparation includes cleaning, normalizing, and securing sensitive information, all of which add to the cost. In many projects, data readiness requires more time and budget than the AI model itself.
2. Compliance design
Compliance is not a legal afterthought in AI healthcare apps. It directly shapes how the system must be built. Privacy rules, consent management, auditability, and access controls must function continuously rather than only at launch.
As a result, engineers must design workflows that automatically enforce these requirements across every interaction. This increases development effort because compliance becomes part of system behavior, not a separate layer. Consequently, organizations that underestimate compliance design almost always face rework and rising costs later.
3. System integration
AI healthcare apps rarely operate on their own. They must connect seamlessly with EHRs, laboratory systems, billing platforms, identity services, and more. Each integration introduces technical and operational complexity because data standards, update frequencies, and reliability expectations differ across systems.
Therefore, integration work often consumes a larger share of the budget than anticipated. In many enterprise deployments, building reliable interoperability proves more expensive than developing the AI features themselves.
4. Deployment model
Where and how the AI healthcare app is deployed significantly affects both initial and ongoing cost. Cloud-only deployments usually offer speed and flexibility, while hybrid or on-prem models introduce additional security and infrastructure considerations.
When systems must operate across regions, cost rises further due to redundancy, performance tuning, and regulatory constraints. Therefore, infrastructure choices shape not just operating expenses but also the overall engineering scope from day one.
5. AI lifecycle management
Developing an AI model is only the beginning of the journey. Once deployed, the system must be monitored, updated, and retrained to remain accurate and reliable. Data patterns change over time, and models must adapt accordingly.
This introduces ongoing costs related to performance monitoring, model tuning, and anomaly detection. As a result, many organizations discover that AI operations become a larger cost center than initial development if not planned properly.
6. Clinical safety and oversight
When AI influences or supports clinical decisions, safety becomes a direct cost driver. Systems must be designed so that clinicians can understand, verify, and override AI outputs when necessary. This requires additional workflows, validation layers, and governance mechanisms.
Therefore, building AI that is safe for clinical use involves more than technical accuracy. It requires structural safeguards that increase development effort but protect organizations from far greater risk later.
Ultimately, the cost of an AI healthcare app grows in proportion to the responsibility the system carries within the organization. When organizations align investment with operational roles early, AI healthcare platforms become far more predictable, defensible, and scalable.
AI Healthcare App Development Cost by Phase
The cost to build an AI healthcare app in 2026 spreads across six key phases, with earlier planning and later scaling often consuming as much budget as actual development.
Because regulated healthcare adds oversight, governance, and integration demands, cost does not rise simply by adding features. Instead, it grows with responsibility and rigor.
The figures below break down typical enterprise spending patterns. These should be viewed as directionally accurate ranges based on real deployments, not exact vendor quotes.
AI Healthcare App Development Cost by Phase (2026)
| Development Phase | What Happens in This Phase | Typical Cost Range (USD) |
| Discovery & Clinical Workflow Mapping | Understanding care processes, defining scope, and aligning the system to real operations | $8,000 – $20,000 |
| AI Architecture & Data Strategy | Designing AI pipelines, data flow, security, and governance | $15,000 – $40,000 |
| Product Engineering & Integration | Building the app, AI models, and integrating with enterprise systems | $50,000 – $120,000 |
| Validation, Testing & Regulatory Readiness | Clinical validation, QA, compliance audits, security checks | $30,000 – $80,000 |
| Pilot Rollout & Feedback Loops | Limited deployment, user training, and early optimization | $20,000 – $50,000 |
| Scale, Governance & Optimization | Enterprise rollout, monitoring, governance, and long-term operations | $50,000 – $120,000+ |
Phase 1: Discovery and clinical workflow mapping
In this first phase, teams spend time understanding how care delivery and administrative processes actually work. Stakeholders, clinicians, operations teams, and IT leaders collaborate to map out workflows that the app must support.
The goal is to avoid costly misalignment later by clarifying scope, data access needs, and compliance boundaries up front.
Typical cost range: $8,000 – $20,000
Because this phase is primarily analytical and planning-oriented, it usually represents a small but critical portion of the overall budget. Investing adequately here prevents costly rework later in development.
Phase 2: AI architecture and data strategy
In this phase, architects and data engineers define how data will flow into and through the system. They decide where data lives, how it will be secured, how models will be trained, and how compliance will be enforced.
Decisions here strongly influence long-term operating cost because they determine reusability, scalability, and governance posture.
Typical cost range: $15,000 – $40,000
This phase often attracts a higher cost than discovery because it requires senior technical expertise and decisions that affect the entire lifecycle of the AI healthcare platform.
Phase 3: Product engineering and integration
This is often the largest single phase of effort. It includes building core user interfaces, engineering the AI components, and integrating with EHRs, labs, billing systems, identity providers, and other enterprise systems. Because healthcare ecosystems are heterogeneous, integration work can require custom connectors, standards translation (e.g., FHIR/HL7), and extensive testing.
Typical cost range: $50,000 – $120,000
Integration demands and engineering effort make this phase one of the most significant budget items.
Phase 4: Validation, testing, and regulatory readiness
Once the product is built, it must be validated against clinical expectations and tested against real-world workflows. This includes not only functional QA, but also performance checks, safety validations, compliance audits, and readiness for security and privacy reviews. Vendors often underestimate this phase, but enterprises cannot afford gaps here.
Typical cost range: $30,000 – $80,000
Most organizations spend this much because testing must simulate real clinical use and satisfy compliance auditors.
Phase 5: Pilot rollout and feedback loops
Deploying the app into a controlled pilot environment helps organizations gather real user feedback, understand performance, and refine workflows. This often includes training clinical staff, monitoring usage trends, and tuning the system based on early data. At this stage, operational processes begin to reveal costs that may not have appeared during development.
Typical cost range: $20,000 – $50,000
Pilot phases often have more operational cost than development cost, especially when multiple user groups are involved.
Phase 6: Scale, governance, and optimization
This final phase focuses on organizational readiness for full deployment. It includes operational governance, support structures, advanced security validation, ongoing AI monitoring, retrospective process tuning, and broader rollout planning.
Because complexity increases with scale, this phase often matches or exceeds earlier phase spend.
Typical cost range: $50,000 – $120,000+
Scaling responsibly in enterprise healthcare means investing not just in more servers, but in people, governance workflows, monitoring, and continuous compliance.
When an enterprise plans its AI healthcare app budget, it must allocate for each phase with a sense of proportion. Early planning ensures fewer surprises in development and validation. Mid-phase engineering and integration consume the bulk of the build cost. Late-phase rollout and governance ensure long-term survivability of the platform.
Taken together, these phase ranges align with broader healthcare app cost benchmarks, where total investment typically falls between $40,000 and $400,000+ for regulated, enterprise-ready solutions.
What Is the Total Cost of Ownership (TCO) of an AI Healthcare App?
The total cost of ownership of an AI healthcare app includes ongoing compute, monitoring, compliance, infrastructure, and governance costs that often exceed initial development investment.
The cost to build an AI healthcare app often receives the most attention during planning. However, that number is only the beginning. The real financial commitment begins after deployment, when the system must operate reliably under clinical, regulatory, and performance pressure.
Therefore, enterprises that budget only for development often find themselves surprised by operational expenses later. TCO is where AI healthcare investments either remain controlled or become unpredictable.
Understanding these ongoing costs is essential for realistic planning.
1. AI inference and compute
Once an AI healthcare app goes live, every interaction triggers computational work. Models must process data, generate outputs, and respond within clinical or operational time limits. As usage grows, compute demand increases in parallel.
Cost rises here not because models become more complex, but because volume increases. Therefore, organizations with rising patient traffic, multi-site deployments, or real-time workflows often see compute become one of the most persistent cost centers.
2. Model monitoring, drift detection, and retraining
AI models do not remain accurate indefinitely. Data patterns shift as care practices change, patient populations evolve, or workflows adapt. As a result, models must be monitored continuously and retrained periodically.
This introduces recurring costs related to performance evaluation, data labeling, and model updates. Without this layer, AI systems may degrade quietly, creating operational and clinical risk that is far more expensive than routine maintenance.
3. Security audits and compliance operations
Healthcare AI systems operate under continuous regulatory oversight. This means security testing, privacy assessments, and audit readiness cannot be one-time activities.
Over time, organizations must invest in repeated audits, vulnerability testing, access reviews, and policy updates. Therefore, compliance operations become a permanent cost line, not a launch requirement. In regulated environments, this often represents one of the most underestimated components of TCO.
4. Clinical validation updates
As AI systems evolve, clinical validation must evolve with them. New workflows, expanded use cases, or updated models require revalidation to ensure safety and reliability.
This involves clinician involvement, documentation, and sometimes third-party assessments. Consequently, even stable systems incur cost through validation cycles, especially in environments where AI influences care decisions directly.
5. Infrastructure scaling
As adoption grows, infrastructure must scale to support more users, more data, and higher performance expectations. This includes not only servers and storage, but also network capacity, redundancy, and disaster recovery mechanisms.
Therefore, infrastructure costs tend to rise gradually rather than appear suddenly. Organizations that plan only for initial capacity often face expensive upgrades later, rather than controlled growth.
6. Incident response and AI governance
No AI system operates without exceptions. Unexpected outputs, data issues, or integration failures require structured response mechanisms.
Maintaining governance frameworks, escalation paths, and cross-functional oversight introduces ongoing operational costs. However, this cost protects organizations from far larger financial and reputational risks, making it a necessary part of enterprise AI ownership.
Typical TCO scenarios by deployment scale
The total cost of ownership varies significantly depending on how widely the AI healthcare app is deployed. While exact numbers differ across organizations, typical annual TCO ranges look like this:
| Deployment Scale | Typical Annual TCO |
| Small-scale deployment | $25,000 – $60,000 |
| Multi-hospital network | $80,000 – $180,000 |
| Enterprise payer/provider platform | $200,000 – $500,000+ |
These figures reflect operational realities rather than development assumptions.
Why does TCO Defines Success More Than Build Cost
Enterprises rarely fail in AI healthcare because they underestimate the development cost alone. They struggle because ongoing costs were never mapped clearly against scale, usage, and responsibility.
When organizations plan for TCO from the beginning, AI healthcare apps shift from experimental investments to stable digital infrastructure. That shift is what ultimately determines whether AI delivers sustainable value or becomes a recurring financial surprise.
How Emerging Tech Is Changing the Cost of AI Development in 2026
Emerging technologies are shifting AI healthcare app costs from pure development spend toward operational, governance, and infrastructure investments.
The cost of building AI healthcare apps is no longer shaped only by how complex the model is. Increasingly, it is shaped by how the system operates over time. As new technologies mature, they change where organizations spend money rather than simply increasing or decreasing total cost.
Therefore, understanding emerging tech is not about predicting trends. It is about anticipating how cost structures will evolve across the AI lifecycle.
Let’s look at the technologies that are most directly influencing how AI healthcare investments are being planned for 2026.
Emerging Technologies Reshaping AI Healthcare App Cost in 2026
| Emerging Technology | What It Changes | Cost Impact Area | How It Alters Cost Structure |
| Generative AI | Speeds up development of conversational, documentation, and support workflows | Operations & Governance | Lowers build time but increases ongoing compute, safety, and monitoring costs |
| Agentic AI | Automates multi-step workflows with limited human intervention | Governance & Oversight | Reduces labor cost but raises supervision, traceability, and control costs |
| Edge AI / On-Device AI | Moves intelligence closer to devices and care delivery points | Infrastructure & Engineering | Lowers long-term cloud costs but increases system design and maintenance effort |
| Federated Learning | Trains models without centralizing sensitive healthcare data | Compliance & Architecture | Increases build complexity but reduces regulatory and data movement costs |
| Synthetic Data | Enables model training without using real patient records | Data Governance | Reduces data acquisition risk but adds validation and quality assurance cost |
| Privacy-Preserving AI | Protects patient data during processing and analysis | Compliance Operations | Raises engineering effort but lowers legal, audit, and breach exposure cost |
Emerging technologies do not simply make AI healthcare apps cheaper or more expensive. They redistribute cost across the system lifecycle. Some reduce development effort while increasing operational oversight. Others increase build complexity but lower regulatory and legal exposure.
Therefore, enterprises planning AI investments for 2026 must evaluate technology choices not only by what they enable, but by how they reshape long-term financial responsibility.
What Hidden Costs Delay AI Healthcare Projects?
Hidden costs in AI healthcare projects often emerge from integration complexity, security reviews, data readiness gaps, and delayed compliance alignment rather than from AI development itself.
Most AI healthcare projects do not exceed budgets because AI is unpredictable. They exceed budgets because certain costs are discovered too late. These costs rarely appear in initial proposals, yet they directly affect timelines, risk exposure, and financial planning.
Understanding these hidden costs early helps enterprises protect both budgets and delivery confidence.
1. Integration scope creep
AI healthcare apps rarely integrate with just one system. As projects progress, new data sources, workflows, and exceptions often surface.
This leads to:
- Additional connectors and APIs
- Unplanned interoperability work
- Longer testing cycles
Therefore, what begins as a simple integration can quickly expand into a major engineering effort.
2. Security and vendor reviews
Healthcare enterprises require rigorous security assessments before allowing new systems into production environments. These reviews involve multiple stakeholders and often evolve as the system design changes.
Common hidden costs include:
- Repeated penetration testing
- Security documentation cycles
- Infrastructure hardening beyond initial plans
As a result, security becomes a delivery driver, not just a technical checkbox.
3. Data access and rights management
Even when data exists, accessing it is rarely straightforward. Ownership, consent, and usage rights vary across departments and regions.
Hidden costs arise from:
- Legal and compliance coordination
- Consent framework redesigns
- Data de-identification workflows
Consequently, data readiness delays often become schedule delays.
4. Clinical adoption and training
AI healthcare systems succeed only when clinicians trust and use them. However, training and adoption are frequently under-budgeted.
This includes:
- Workflow redesign sessions
- Role-based training programs
- Ongoing change management
Without these, even well-built systems struggle to deliver value.
5. Late compliance alignment
When compliance is addressed after development begins, rework becomes inevitable. Small design choices made early can have large regulatory implications later.
This often leads to:
- Architecture revisions
- Documentation retrofitting
- Revalidation cycles
Therefore, delaying compliance alignment almost always costs more than addressing it upfront.
Hidden costs appear wherever uncertainty exists. The earlier organizations remove that uncertainty through planning, governance, and alignment, the more predictable AI healthcare projects become.
How to Optimize AI Healthcare App Development Cost
AI healthcare app costs can be optimized through architectural planning, phased deployment, and governance-first design without reducing clinical safety or regulatory compliance.
Cost optimization in healthcare AI is not about reducing investment. It is about placing investment where it delivers long-term control, resilience, and measurable outcomes. When organizations approach cost strategically, they avoid cutting corners that later create financial and operational exposure.
The goal is not to spend less, but to spend wisely.
1. Design the system in modular layers
Modular system design allows enterprises to build AI healthcare apps in independent, replaceable components rather than as a single, rigid system.
This helps organizations:
- Upgrade or replace AI models without rebuilding workflows
- Isolate compliance changes from application logic
- Expand functionality without destabilizing core operations
As a result, cost remains predictable even as requirements evolve.
2. Roll out in phases, not all at once
Phased deployment reduces upfront financial risk and allows teams to validate value before scaling further.
This approach enables enterprises to:
- Test assumptions early
- Control budget exposure
- Adjust architecture based on real usage
Therefore, cost optimization becomes a continuous process rather than a one-time exercise.
3. Reuse AI components across workflows
AI capabilities such as identity resolution, document classification, or anomaly detection often apply across multiple healthcare workflows.
By reusing these components:
- Development time decreases
- Maintenance effort reduces
- Consistency across systems improves
This avoids duplicating costs for similar capabilities across departments.
4. Choose hybrid AI architectures strategically
Not every function requires full AI automation. In many cases, combining rule-based logic with AI yields better control and lower cost.
Hybrid architectures:
- Reduce unnecessary compute usage
- Improve explainability
- Simplify compliance audits
As a result, organizations gain flexibility without sacrificing reliability.
5. Align compliance early with design
When compliance requirements shape architecture from the beginning, systems avoid expensive retrofitting later.
Early alignment allows:
- Consent management to integrate naturally
- Auditability to become part of workflows
- Security reviews to proceed smoothly
Therefore, compliance becomes a cost stabilizer rather than a cost accelerator.
The most successful AI healthcare platforms are not the cheapest to build. They are the most predictable to operate.
When enterprises optimize for governance, scalability, and adaptability, they control cost while protecting clinical integrity and regulatory standing. That is what transforms AI from a budget risk into a strategic asset.
Conclusion
Building an AI healthcare app is not a software decision. It is an operational and financial commitment that shapes how care, compliance, and growth intersect. When organizations plan costs across the full lifecycle, AI becomes predictable rather than risky.
With the right architecture, governance, and partner, AI shifts from being a budget concern to a long-term growth enabler.
Get Your AI Healthcare App Developed By Intellivon
At Intellivon, AI healthcare apps are built as regulated enterprise platforms, not as experimental AI features layered onto care systems. Every architectural and delivery decision prioritizes compliance, interoperability, and long-term operational reliability. This ensures platforms perform across providers, payers, and regions, not just during pilot deployments.
As AI programs scale across use cases and populations, stability becomes critical. Governance, performance, and audit readiness remain consistent as volumes grow.
Why Partner With Intellivon?
- Enterprise-grade AI healthcare architecture designed for regulated care environments
- Proven delivery across providers, insurers, and healthcare technology platforms
- Compliance-by-design approach with audit readiness and policy enforcement
- Secure, modular infrastructure supporting cloud, hybrid, and on-prem deployments
- Governed AI enablement for insights, automation, and decision support
- Deep interoperability expertise across EHRs, imaging, and claims systems
- ROI-focused delivery model aligned to enterprise performance metrics
- Scalable delivery frameworks for multi-region and multi-entity healthcare networks
Book a strategy call to explore how Intellivon can help you build and scale an AI healthcare app with confidence, control, and long-term enterprise value.
FAQs
Q1. How much does it cost to build a HIPAA-compliant AI healthcare app?
A1. A HIPAA-compliant AI healthcare app typically costs between $40,000 and $400,000+, depending on scale, integration depth, and governance requirements. Compliance increases cost because security, auditability, access control, and data handling must be engineered into the system from the start.
Q2. Is building AI in healthcare more expensive than traditional healthcare apps?
A2. Yes, AI healthcare apps are usually more expensive than traditional healthcare apps because they carry additional responsibilities. Beyond UI and workflows, AI systems must manage data quality, model behavior, monitoring, and regulatory traceability.
Q3. How long does it take to develop an AI healthcare app?
A3. Development timelines typically range from 3 to 6 months for focused pilots and 9 to 15 months for enterprise-grade platforms. Timelines depend less on coding speed and more on data readiness, integration scope, and compliance alignment.
Q4. What is the biggest cost driver in AI healthcare projects?
A4. The biggest cost driver is not the AI model itself, but how deeply the system integrates into clinical and operational workflows. As integration, compliance, and scale increase, so does cost.
Systems that influence care decisions or financial processes naturally require more safeguards. Therefore, responsibility, not technology, determines cost.
Q5. Can AI healthcare apps be built cost-effectively for pilots before scaling?
A5. Yes, many organizations start with focused AI pilots costing $40,000 to $80,000 to validate value before scaling. Pilots allow teams to test workflows, data access, and adoption without committing full enterprise budgets.
Q6. What’s the difference between the AI MVP cost and the enterprise deployment cost?
A6. An AI MVP focuses on a narrow use case with limited integrations and governance, keeping costs relatively low. Enterprise deployments, on the other hand, must support scale, compliance, interoperability, and long-term operations.