Diagnostic errors remain one of healthcare’s most persistent challenges, contributing to nearly 10% of patient deaths worldwide. Imaging departments, which are often the backbone of modern diagnosis, are stretched thin by rising complexity and scan volumes that outpace staffing capacity. AI medical imaging tools are transforming this reality by identifying subtle abnormalities, prioritizing high-risk cases, and helping clinicians make faster, more confident decisions. The goal is to extend radiologists’ capabilities through scalable, intelligent automation that delivers precision and consistency at enterprise scale.
At Intellivon, we have partnered with leading healthcare enterprises to design and deploy such systems from the ground up. By combining advanced computer vision, explainable AI, and compliance-ready data pipelines, our platforms have helped organizations cut turnaround times, strengthen diagnostic accuracy, and elevate patient outcomes. In this guide, we will walk you through our end-to-end development process for enterprise-grade, precision-driven AI medical imaging tools.
Why Enterprises Must Adopt AI Medical Imaging Tools Now
Hospitals and diagnostic networks are under mounting pressure to deliver faster, more accurate results with limited radiology staff. AI medical imaging tools are closing that gap by improving diagnostic precision, reducing workload, and cutting turnaround time across every major modality.
What’s changed is the level of maturity. These tools are no longer experimental; they’re clinically validated, regulator-approved, and operating reliably at scale.
1. Clinical Validation at Scale
Large, peer-reviewed studies have confirmed AI’s real-world impact in screening and detection.
- A 2025 Nature Medicine study involving 460,000 women found that AI-assisted mammography achieved a 17.6% higher cancer detection rate without increasing recalls.
- The Swedish MASAI trial (Lancet Oncology, 2023) demonstrated that AI-supported reading was non-inferior to double reading while significantly cutting radiologist workload.
For large healthcare enterprises, this translates to faster throughput, fewer rechecks, and measurable ROI through higher operational efficiency.
2. Proven Workflow Gains in Acute Care
AI is driving measurable improvements in emergency and time-critical imaging workflows.
- In stroke triage, FDA-cleared platforms like Viz.AI (De Novo 2018) deliver automated LVO alerts within 5–10 minutes, enabling earlier interventions and reducing ischemic damage.
- In chest X-ray triage, AI systems consistently cut report turnaround times and accelerate escalation for critical findings.
For hospitals managing thousands of scans daily, those minutes directly translate into higher survival rates, optimized staff utilization, and stronger patient trust.
3. Data-Driven Reliability
Enterprise-grade reliability begins with data transparency and reproducibility.
Most FDA-cleared imaging AI models are trained on large, publicly validated datasets such as MIMIC-CXR (377,000+ images) and CheXpert (224,000 images).
These datasets enable external benchmarking, cross-institution testing, and compliance-ready governance, which are critical for healthcare systems scaling AI across multiple sites.
4. Regulatory Maturity and Monitoring
AI imaging tools are now part of a well-defined regulatory ecosystem. With over 520 FDA-cleared AI/ML medical devices approved as of mid-2025, radiology remains the leading category.
This level of oversight gives enterprise leaders confidence that today’s tools have passed rigorous safety, validation, and risk management reviews, and are paving the way for secure, large-scale adoption.
What This Means For Enterprises
AI medical imaging tools have moved beyond proof-of-concept. They are now clinically proven, regulator-approved, and enterprise-ready. In modern healthcare systems, the question is how quickly to integrate them across operations to enhance both outcomes and efficiency.
Understanding AI Medical Imaging Tools
AI medical imaging tools are software systems that interpret scans and return structured, decision-ready outputs. They detect patterns, measure regions, and flag urgency so clinicians can focus where it matters.
These tools sit alongside PACS, RIS, and EHR. They pull DICOM studies, run analysis, and return overlays, measurements, and summaries that fit existing reporting workflows.
They cover a range of functions, like detection and classification of findings, segmentation and quantification for therapy planning, triage for time-critical cases, and automation that speeds structured reports. In mature deployments, they also support quality checks, protocol adherence, and post-market performance monitoring across multiple sites.
How AI transforms the Imaging Workflow
AI shortens the distance between scan and decision. It prioritizes the right cases, standardizes measurements, and reduces unwarranted variation between readers.
Turnaround times drop because routine normals do not block urgent studies. As a result, diagnostic confidence rises because findings are highlighted, measured, and linked to prior context.
For operations leaders, the effect includes backlogs shrinking and throughput improving without compromising safety.
Key Takeaways of the AI Medical Imaging Market
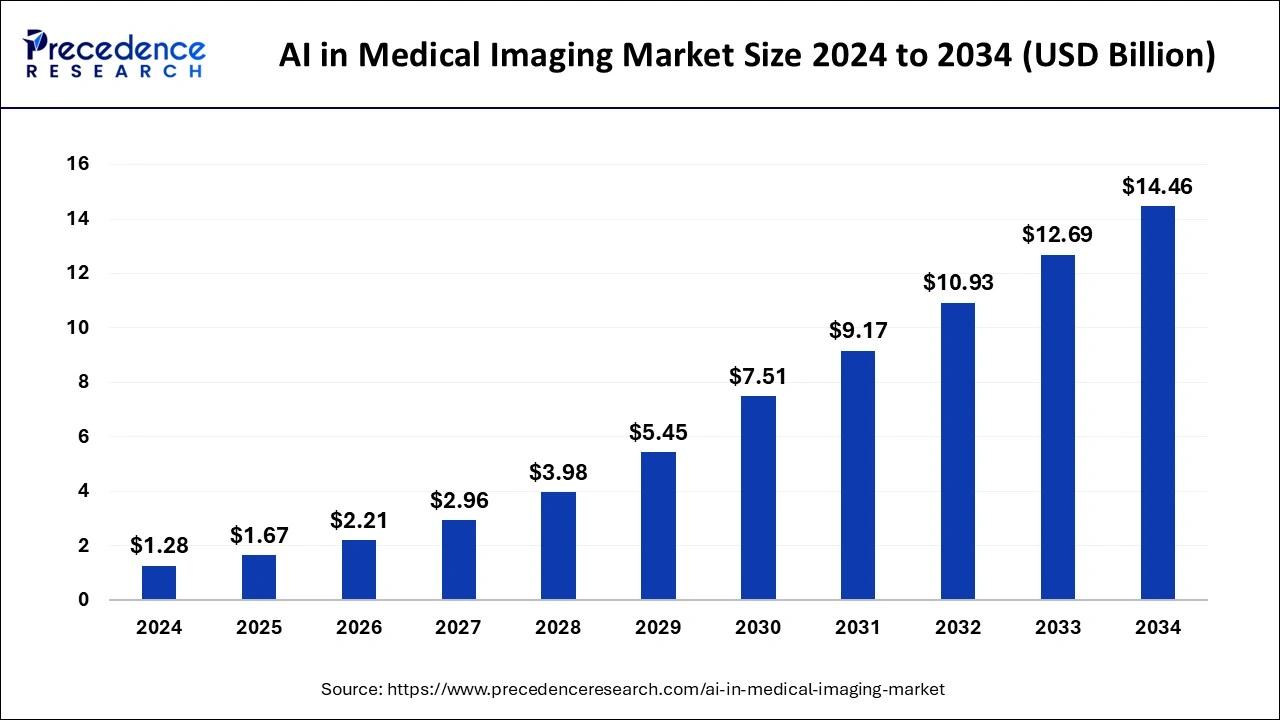
Key Takeaways:
- Core applications of AI in medical imaging include image acquisition, segmentation, interpretation, and workflow automation that collectively reduce radiologist workload, minimize diagnostic errors, and improve patient outcomes.
- Regional distribution shows North America and Europe leading the market due to established healthcare infrastructure and regulatory support, while Asia-Pacific emerges as the fastest-growing region on the back of rapid digital health adoption.
- Key industry participants include Siemens Healthineers, GE Healthcare, Philips, IBM Watson Health, Aidoc, Zebra Medical Vision, and Qure.ai, all investing heavily in scalable AI-powered imaging ecosystems.
- Technological drivers such as deep learning, computer vision, and natural language processing are being integrated with imaging modalities like MRI, CT, X-ray, and ultrasound to unlock new levels of automation and precision.
- Regulatory frameworks like the EU AI Act are shaping development and deployment, enforcing transparency, clinical safety, and robust quality management across AI-enabled devices.
Enterprise Adoption Drivers
- The shortage of radiologists is acute: Imaging volumes are growing approximately 3-4% annually, while the radiologist workforce grows far more slowly due to limited residency positions and high attrition.
- Increasing imaging volumes are driven by aging populations and expanded use of advanced modalities such as CT, MRI, and PET scans, with standard outpatient imaging volumes projected to rise about 10% and advanced imaging about 14% over the next decade.
- FDA momentum is strong with over 520 AI/ML-enabled medical devices cleared for marketing in the US as of 2025, most focused on radiology applications, reflecting the clinical impact AI is poised to have in diagnostics and workflow optimization.
Competitive Dynamics
- Aidoc: Leading AI healthcare solutions provider with total funding over $250M including a $110M Series D in early 2025. Ranked 44th fastest-growing North American tech company in 2023, known for its AI Care Platform that integrates multiple AI solutions into clinical workflows.
- Viz.ai: A leader in AI-powered disease detection and care coordination, with $282.5M total funding, revenue around $85M, and recognized for machine learning innovation with consecutive Edison Awards up to 2025.
- PathAI: Recognized for AI-powered pathology tools, ranked 420th fastest-growing North American tech company in 2024 with 260% growth. Focused on accelerating clinical trials and enhancing diagnostic accuracy in pathology
These insights portray a rapidly expanding, technology-driven market with significant opportunities for improving healthcare delivery through AI-enabled imaging solutions globally.
Types of AI Medical Imaging Tools
In AI medical imaging, each category serves a distinct clinical purpose, from identifying abnormalities to automating full diagnostic reports. Together, they enable faster, safer, and more consistent decisions across departments and modalities.
1. Detection and Classification Tools
These tools act as the first line of analysis, scanning imaging data to identify signs of disease or abnormality. They are trained on millions of annotated scans to recognize features that even experienced clinicians might miss.
In mammography, for example, AI models detect microcalcifications linked to early-stage cancer. In chest imaging, they classify nodules or infiltrates that may indicate pneumonia, tuberculosis, or malignancy.
By assigning probability scores to each region, these systems help prioritize high-risk cases and reduce diagnostic uncertainty in high-volume settings.
2. Segmentation and Quantification Tools
Segmentation tools outline anatomical structures or lesions on the image, while quantification algorithms calculate their size, volume, or density. This is critical for treatment planning, especially in oncology and cardiology, where precise measurement determines the course of therapy.
For instance, brain tumor segmentation tools automatically map tumor boundaries in MRI scans and quantify progression across follow-up studies. Quantification also supports research and clinical audits by offering objective, reproducible metrics instead of subjective visual estimates.
3. Workflow and Triage Automation Tools
These tools optimize how radiology departments handle workloads. They automatically identify urgent cases, such as suspected strokes, pulmonary embolisms, or pneumothorax, and move them to the top of the radiologist’s queue. Alerts are sent instantly to the appropriate specialists, ensuring that no critical scan is overlooked.
In enterprise networks with thousands of daily scans, triage automation reduces bottlenecks, accelerates time-to-diagnosis, and improves resource allocation without requiring new infrastructure.
4. Multi-Modal Predictive Analytics Tools
Predictive analytics tools go beyond visual interpretation. They integrate imaging data with patient demographics, lab results, and genomic information to forecast disease risk or treatment response.
A typical use case is predicting tumor recurrence after therapy or identifying patients likely to develop cardiac complications based on imaging biomarkers.
These systems bring preventive medicine closer to reality, transforming imaging from a diagnostic tool into a forward-looking decision support system.
5. Reporting and Decision-Support Tools
Reporting tools combine AI-generated insights with structured templates to speed up documentation and maintain consistency. They extract measurements, insert them into predefined sections, and even generate draft findings that radiologists can edit before signing off.
Decision-support layers cross-check findings against clinical guidelines, improving compliance and standardization.
For large hospital networks, this means faster report turnaround, fewer errors, and a unified diagnostic language across all branches.
These five categories of AI medical imaging tools work together to create a continuous intelligence pipeline, from scan acquisition to diagnosis and documentation.
Architecture of AI Medical Imaging Tools
Modern AI medical imaging platforms combine clinical data pipelines, deep learning infrastructure, and governance layers that ensure every inference is secure, compliant, and auditable. The architecture defines how images move from scanners to insights, and how models evolve safely once deployed.
1. Data Ingestion and Integration
The pipeline starts at the source, which is imaging modalities such as CT, MRI, X-ray, and ultrasound. Studies flow into the hospital’s Picture Archiving and Communication System (PACS) or Vendor Neutral Archive (VNA).
From there, integration APIs or HL7/FHIR gateways push selected studies to the AI platform. This layer focuses on interoperability, ensuring that data from multiple vendors, regions, and systems arrives in a consistent, DICOM-compliant format.
2. Pre-Processing and Standardization
Before analysis, images are cleaned and standardized. Algorithms remove noise, correct orientation, and normalize resolution.
Patient identifiers are stripped or encrypted to maintain HIPAA and GDPR compliance. The system also classifies studies by modality and body part, routing them to the appropriate model. Standardization at this layer ensures reliability across diverse hospital infrastructures.
3. Model Training and Validation Layer
At the core sits the deep learning environment, which is a scalable GPU or cloud-native cluster running computer vision architectures such as convolutional neural networks (CNNs) and vision transformers.
This layer manages dataset curation, annotation workflows, and performance benchmarking. Every model is trained on de-identified, balanced data and validated using metrics like sensitivity, specificity, AUC, and Dice coefficient.
4. Inference and Orchestration Layer
Once validated, models move into the inference pipeline. Here, the platform processes incoming studies in real time, generating heatmaps, annotations, and structured outputs.
Orchestration services manage load balancing across multiple nodes, ensuring that the system can handle thousands of concurrent scans. Results are returned to the PACS or radiologist viewer as overlays or structured fields.
5. Governance and Monitoring Layer
This is the compliance backbone. It handles encryption, access control, audit logs, and role-based authentication.
Monitoring dashboards track model drift, latency, and accuracy across hospital sites. When performance drops, retraining pipelines trigger automatically under MLOps supervision. Every inference is recorded for traceability, meeting FDA, ISO 13485, and IEC 62304 standards.
How We Build AI Medical Imaging Tools for Enterprises
Our process of building AI medical imaging tools bridges clinical precision, regulatory discipline, and deep technical expertise. Below is the 8-step process we follow when building AI medical imaging tools for large hospitals, MedTech firms, and diagnostic networks.
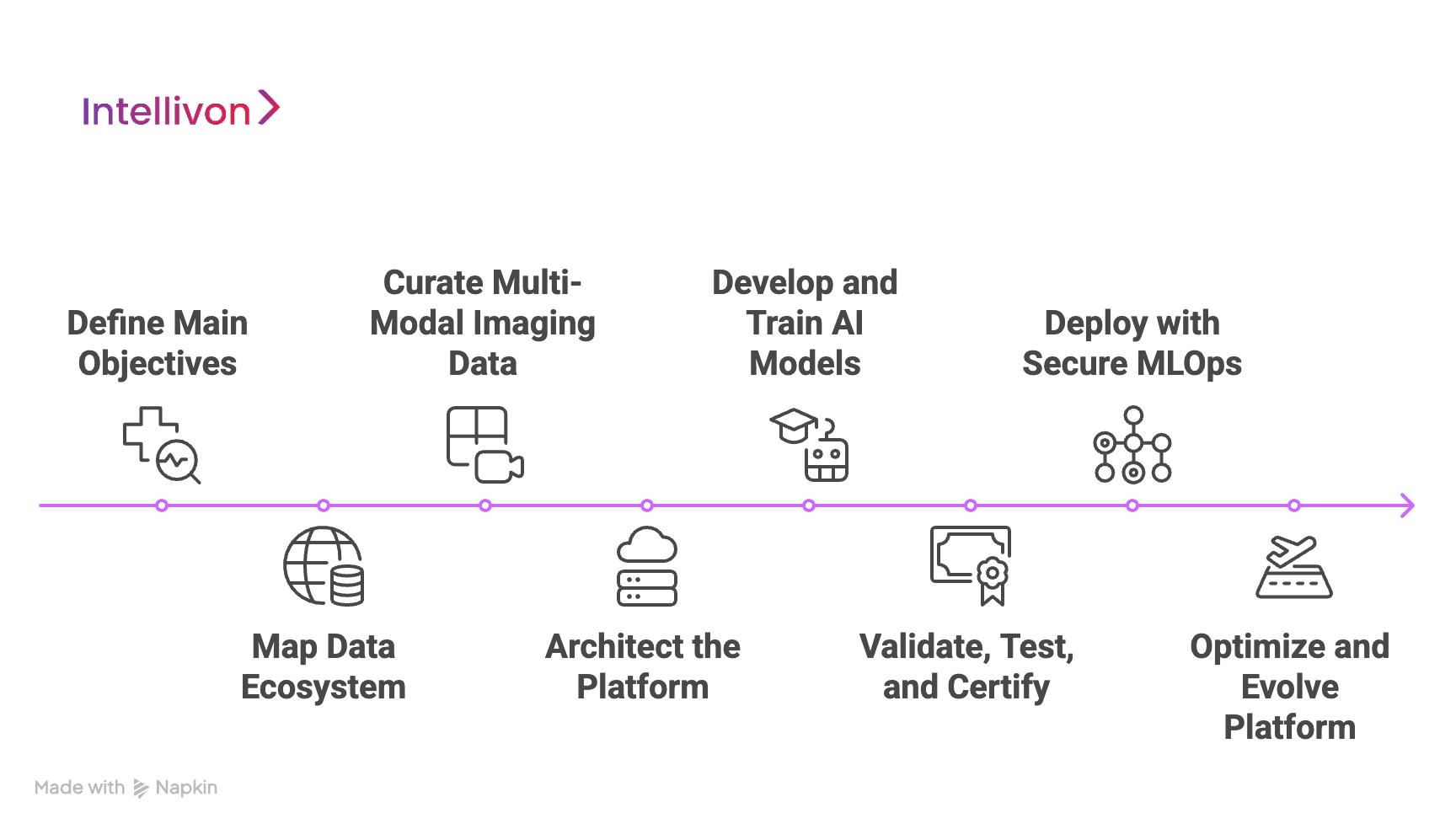
Step 1: Define Main Objectives
Every project begins with clarity. We work with clinical and operational leaders to identify diagnostic pain points, define the target use case (e.g., stroke triage, tumor segmentation, mammography screening), and establish measurable ROI goals.
This alignment ensures that the solution is not only technically sound but also commercially and clinically relevant.
Step 2: Map Data Ecosystem
We audit the existing data infrastructure, which includes PACS, RIS, EHR, and cloud systems, to understand data flow, format, and accessibility.
During this stage, our teams set clear compliance boundaries based on HIPAA, GDPR, and FDA SaMD standards.
Data access is secured through encryption and anonymization protocols, ensuring privacy without compromising the integrity of datasets.
Step 3: Curate Multi-Modal Imaging Data
Our data engineers source, cleanse, and annotate large, diverse imaging datasets. We combine internal hospital archives with public datasets like MIMIC-CXR, CheXpert, and TCIA, ensuring both volume and variability.
Through Intellivon’s semi-automated labeling workflows, annotation accuracy improves while manual effort is reduced.
Step 4: Architect the Platform
We design a cloud-native architecture that connects seamlessly with enterprise PACS and EHR systems through FHIR and HL7 interfaces.
Each build follows modular principles, like ingestion, pre-processing, inference, and governance layers, ensuring that the system can scale across multiple hospital sites and imaging modalities.
Step 5: Develop and Train AI Models
Our AI scientists develop models using convolutional neural networks, vision transformers, and multi-modal fusion approaches. We prioritize explainability (XAI) and model interpretability, producing outputs that clinicians can trust.
Training and validation are conducted on de-identified, balanced datasets, with benchmarks established for accuracy, sensitivity, and specificity.
Step 6: Validate, Test, and Certify
Before deployment, every model undergoes multi-phase validation, which includes clinical, statistical, and technical.
We prepare documentation aligned with FDA 510(k), EU MDR, and ISO 13485 requirements. Intellivon’s regulatory teams collaborate with clients to streamline audits, ensuring faster market readiness and long-term compliance confidence.
Step 7: Deploy with Secure MLOps
Deployment is executed using Intellivon’s enterprise-grade MLOps pipeline. This ensures automated version control, model drift detection, and real-time performance tracking across locations.
Our systems integrate seamlessly with hospital IT environments, maintaining uptime and traceability while enabling federated updates for global scalability.
Step 8: Optimize and Evolve Platform
After launch, we continuously refine models using new anonymized data, update compliance frameworks, and expand capabilities to new modalities or use cases.
Through iterative learning and active monitoring, the platform evolves, becoming faster, smarter, and more valuable with each cycle.
At Intellivon, our approach combines technical depth, regulatory discipline, and clinical collaboration to deliver systems that scale securely and deliver measurable ROI.
Real-World Enterprise Examples of AI Medical Imaging
AI medical imaging tools are transforming how leading healthcare enterprises diagnose, triage, and treat patients at scale. The following examples highlight how hospitals and health systems around the world are deploying these platforms to enhance accuracy, speed, and patient outcomes.
1. Mayo Clinic
The Mayo Clinic has implemented deep learning models for brain tumor segmentation in MRI studies, reducing manual contouring time by over 70%. These AI tools assist radiologists and oncologists in mapping tumor boundaries and monitoring treatment response, improving both precision and productivity.
For large healthcare networks, this automation means consistent measurements across multi-site imaging centers and faster treatment planning for critical neuro-oncology cases.
2. Cleveland Clinic
Cleveland Clinic adopted an AI triage platform to prioritize chest X-rays showing potential pneumonia, pneumothorax, or cardiac abnormalities. Clinical trials have shown that such systems reduce report turnaround time by up to 28%, allowing radiologists to focus first on urgent cases.
By integrating the tool with their existing PACS and RIS systems, Cleveland Clinic achieved operational efficiency without changing core workflows, which is a key factor for enterprise-wide adoption.
3. Mount Sinai Health System
Mount Sinai introduced AI-supported mammography reading systems trained on millions of annotated scans. A 2025 Nature Medicine study across 460,000 women showed that AI-assisted mammography achieved a 17.6% higher cancer detection rate without increasing recall rates.
For enterprise hospitals, these results demonstrate how AI can expand screening capacity, maintain diagnostic quality, and alleviate radiologist workloads in large-scale screening programs.
4. NHS England
The National Health Service (NHS) in England has rolled out AI-based breast screening solutions across multiple trusts.
Early evaluations indicate that AI support can reduce radiologist workload by up to 44% while maintaining detection performance. This enterprise-level deployment shows how coordinated governance and central infrastructure can enable safe, large-scale AI integration across public healthcare systems.
5. Johns Hopkins Medicine
Johns Hopkins Medicine uses Viz.AI, an FDA-cleared stroke triage platform, to detect large vessel occlusions (LVOs) within minutes of scan acquisition. The system sends real-time alerts to specialists, cutting door-to-needle time and improving outcomes for stroke patients.
This integration exemplifies how AI imaging tools enhance time-critical care pathways and save lives by ensuring faster clinical response in high-stakes environments.
Across these examples, AI imaging tools have proven their enterprise value, improving diagnostic precision, optimizing operations, and reducing human workload.
Enterprise Use Cases of AI Medical Imaging Tools
AI medical imaging tools are reshaping how healthcare enterprises operate, from diagnostics and treatment planning to claims management and preventive care. Their applications now extend well beyond radiology departments, supporting clinical, operational, and administrative functions across the enterprise. Below are the most impactful use cases seen in large-scale deployments today.
1. Hospital Networks and Diagnostic Chains
Enterprise hospital systems use AI imaging tools to manage massive scan volumes efficiently. Automated triage, anomaly detection, and structured reporting shorten diagnostic cycles and reduce backlog. For example, a multi-site network can centralize radiology reading through AI-assisted prioritization, ensuring urgent cases are reviewed first.
2. MedTech
Global OEMs like Siemens Healthineers and GE Healthcare embed AI modules directly into scanners for real-time image optimization. These systems enhance acquisition quality, detect motion artifacts, and automatically adjust imaging parameters based on patient anatomy.
3. Remote Diagnostic Services
AI imaging tools enable remote reading networks to operate at scale. Automated pre-screening highlights abnormal studies before human review, while secure cloud infrastructure ensures compliance across geographies.
4. Clinical Research
Pharmaceutical and research enterprises use AI-powered imaging analytics to quantify treatment response, assess biomarkers, and standardize image-based endpoints in trials. This approach speeds up clinical validation and reduces the subjectivity of manual reads.
5. Health Insurance Platforms
Insurance providers integrate AI imaging tools for fraud detection and claim verification. Automated image analysis verifies reported injuries or disease states, minimizing false claims while ensuring faster reimbursement.
6. Preventive Health Programs
Public health initiatives increasingly rely on AI imaging for early disease detection and risk stratification. Tools trained on large datasets identify early signs of lung cancer, diabetic retinopathy, or cardiac abnormalities long before symptoms appear.
7. Digital Twin Systems
Enterprises pursuing full digital transformation use AI imaging data to feed hospital digital twins, which are virtual replicas of care operations. These systems simulate patient flow, imaging demand, and resource allocation in real time.
8. Enterprise Analytics
AI medical imaging platforms also serve as enterprise data hubs. They generate structured analytics on imaging quality, diagnostic accuracy, turnaround times, and utilization patterns.
Across these use cases, AI medical imaging tools prove their value as strategic assets, and not isolated technologies. For modern healthcare organizations, AI imaging adoption has become a central component of digital transformation and long-term competitiveness.
How We Ensure Compliance in AI Medical Imaging Tools
In healthcare, innovation without compliance is a risk, not a breakthrough. Every AI medical imaging tool must meet stringent regulatory, ethical, and security standards before it can operate inside a clinical environment. Our process ensures that AI innovation moves as fast as safety and governance allow, without compromise.
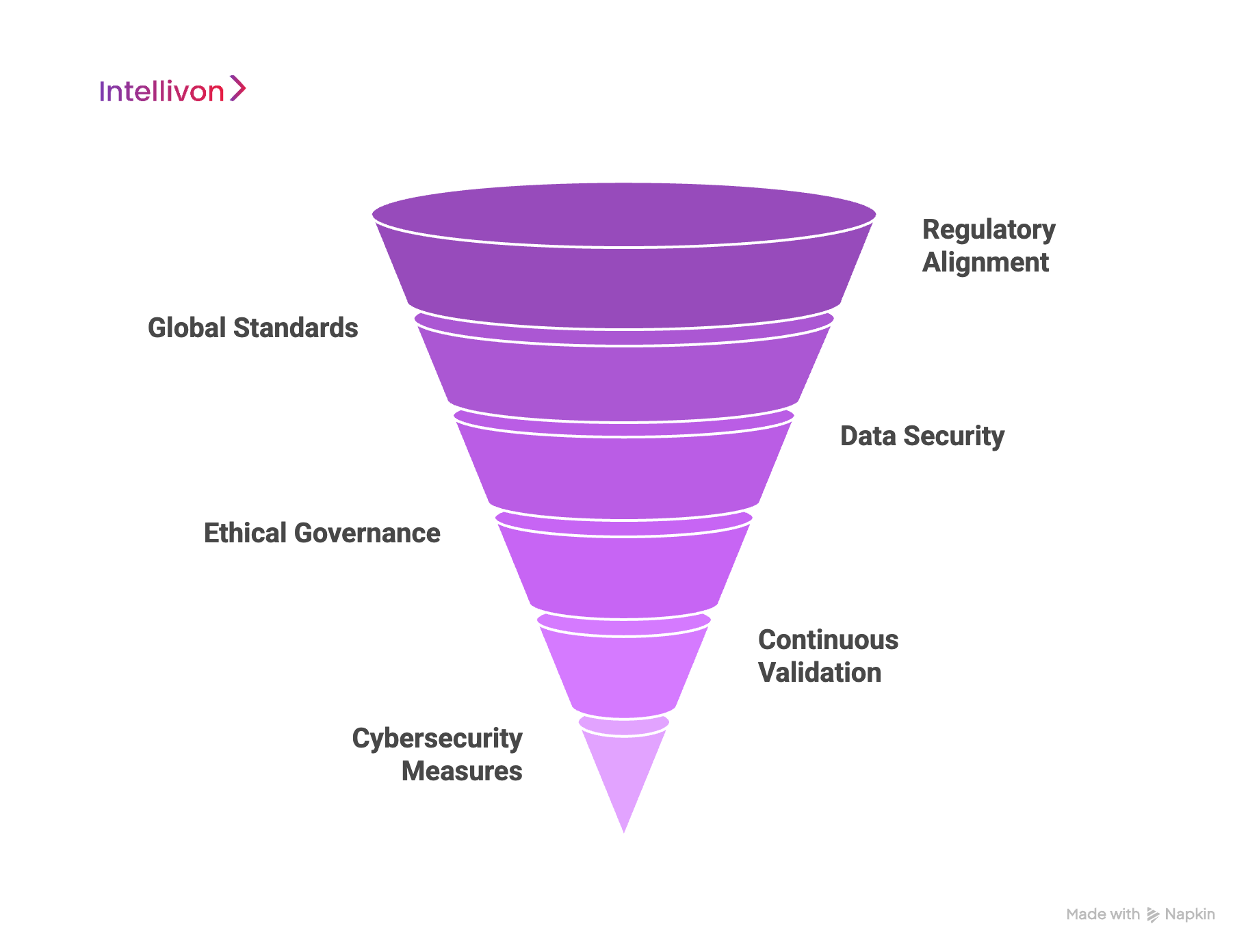
1. Regulatory Alignment
Compliance begins at the concept stage. Intellivon aligns every project with the relevant regulatory frameworks from the start, including FDA 510(k) and De Novo pathways, EU MDR, and UKCA.
This early alignment streamlines documentation and validation, ensuring that models are developed under recognized Software as a Medical Device (SaMD) protocols.
2. Global Standards
Each AI imaging build follows globally accepted quality and safety standards such as ISO 13485 (medical device quality management), IEC 62304 (software lifecycle processes), ISO 14971 (risk management), and SOC 2 for data security.
Intellivon’s enterprise projects are structured to meet or exceed these benchmarks, ensuring interoperability with existing hospital systems and long-term certification readiness.
3. Data Security
Patient data lies at the heart of imaging AI, and protecting it is non-negotiable. We embed HIPAA, GDPR, and NIST-aligned safeguards into every data pipeline. Imaging datasets are anonymized using de-identification scripts that preserve diagnostic value while removing personal identifiers.
Encryption is applied both in transit and at rest, supported by granular role-based access controls.
4. Ethical Governance
Compliance extends beyond legal standards and includes ethical responsibility. Our compliance experts implement fairness checks and bias-detection audits to ensure model performance remains consistent across gender, ethnicity, and hardware variations.
Explainable AI modules (XAI), such as saliency maps and confidence scores, make every decision traceable for clinical review.
5. Continuous Validation
Once deployed, the platforms continue to be monitored, audited, and improved. Automated MLOps pipelines track accuracy, sensitivity, and drift across hospital networks.
Alerts are generated when performance deviates from baseline, triggering retraining or recalibration under defined governance protocols.
6. Cybersecurity Measures
Medical imaging systems are frequent targets for cyberattacks. To mitigate this, Intellivon integrates a zero-trust architecture, secure API gateways, and periodic vulnerability assessments across all endpoints.
Every deployment undergoes penetration testing and compliance review aligned with the FDA’s cybersecurity guidelines for medical devices.
By embedding compliance into every stage of development, Intellivon ensures that every AI medical imaging platform we build is safe, explainable, and globally deployable.
Our compliance-first engineering model allows enterprises to innovate confidently, expand internationally, and meet the highest clinical and regulatory benchmarks, transforming governance from a burden into a strategic advantage.
Overcoming Challenges To Develop AI Medical Imaging Tools
Implementing AI medical imaging tools across enterprise healthcare systems comes with its share of complexities. The challenge lies in how to scale it safely, integrate smoothly, and deliver consistent ROI in regulated environments.
We address these challenges head-on through a combination of secure architecture, robust governance, and continuous optimization. Each challenge below is paired with the practical solution our teams apply in real enterprise deployments.
1. Data Scarcity and Annotation Bottlenecks
AI models need large, well-labeled datasets, which is something most hospitals lack. Medical images are often fragmented across departments and stored without uniform metadata, making them hard to train on. Manual annotation adds another layer of delay, as labeling requires radiologist expertise and strict compliance oversight.
We implement hybrid data pipelines that combine public datasets like MIMIC-CXR, CheXpert, and TCIA with hospital-specific archives. Our semi-supervised annotation workflows reduce manual effort while maintaining diagnostic precision. All data is de-identified under HIPAA and GDPR standards, ensuring compliance during training.
2. Integration with Legacy Infrastructure
Many hospitals rely on legacy PACS, RIS, and EHR systems built decades ago. These systems often lack API support or standardized data exchange formats, leading to interoperability issues that stall AI adoption.
We design middleware integration layers using HL7 and FHIR standards to connect AI platforms with existing infrastructure. Our solutions ensure seamless data exchange without altering current workflows. This approach minimizes disruption while creating a scalable bridge between old systems and new intelligence layers.
3. Clinician Trust and Workflow Adoption
Radiologists often hesitate to rely on AI outputs, fearing overreliance or workflow disruption. If the interface is unintuitive or the reasoning behind AI predictions is unclear, adoption suffers.
We build clinician-first interfaces with embedded explainability features like heatmaps, probability scores, and audit trails. These tools allow radiologists to verify AI findings before sign-off, turning the system into a trusted assistant rather than a black box. Our design philosophy centers on augmentation, not replacement.
4. Regulatory and Audit Complexity
Global healthcare enterprises operate across multiple jurisdictions, each with unique compliance rules. Meeting FDA, CE, HIPAA, and MDR requirements simultaneously can be time-consuming and expensive.
Our compliance-by-design framework embeds global regulatory standards from the initial design phase. Every build includes pre-mapped documentation for FDA 510(k), EU MDR, and ISO 13485, enabling faster submissions and reducing audit friction. Intellivon’s compliance team assists clients through every stage of certification and post-market surveillance.
5. Model Drift
As clinical data evolves, AI models may lose accuracy, which is a phenomenon known as drift. Differences in imaging hardware, patient demographics, or disease prevalence can impact performance across sites
We deploy MLOps-driven monitoring systems that track model metrics like sensitivity and specificity in real time. When drift is detected, automated retraining is initiated under human supervision. This ensures sustained accuracy and adaptability across hospital networks, regardless of location or equipment.
6. Cybersecurity and Data Risks
Medical imaging systems are prime targets for cyberattacks due to their high data volume and network exposure. Breaches can compromise patient safety and violate regulatory obligations.
We implement a zero-trust architecture fortified with multi-layer encryption, secure API gateways, and endpoint monitoring. All AI imaging platforms undergo periodic penetration testing and adhere to the FDA’s cybersecurity guidelines for medical devices, minimizing exposure to ransomware or data theft.
7. High Implementation Costs
Developing, validating, and deploying AI imaging systems across multiple sites can be expensive, especially for organizations without prior AI infrastructure.
Our modular architecture allows phased deployment, starting with high-impact use cases like stroke triage or chest X-ray automation. This staged approach spreads investment over time, ensures faster ROI, and supports scalability as adoption grows. Cloud-native environments further reduce upfront infrastructure costs.
8. Lack of Standardization Across Models
Hospitals often deploy multiple AI tools from different vendors, each with its own interface and reporting logic. This fragmentation complicates governance and analytics.
We provide a unified orchestration layer that integrates multiple AI models under one governance framework. It standardizes data output formats, performance dashboards, and audit logs, giving enterprises full control and visibility across their AI ecosystem.
The challenges of AI imaging adoption are complex, but not insurmountable. Intellivon’s enterprise-grade approach, by combining compliance, interoperability, and lifecycle monitoring, transforms these roadblocks into advantages.
Conclusion
AI medical imaging tools are reshaping the foundation of modern diagnostics. They enable faster, more accurate, and scalable care delivery while helping hospitals overcome staffing shortages, compliance burdens, and rising imaging volumes. As adoption accelerates, the focus is shifting from experimentation to sustainable, enterprise-wide integration.
However, success requires the right strategy, governance, and clinical alignment. Partnering with an experienced AI solution provider ensures that systems are built securely, validated thoroughly, and scaled responsibly, empowering healthcare enterprises to unlock the full potential of intelligent, data-driven diagnostics.
Build Your Enterprise-Grade AI Imaging Platform with Intellivon
At Intellivon, we design AI medical imaging platforms that combine diagnostic precision, regulatory compliance, and enterprise scalability. Our systems empower healthcare organizations to deliver faster, safer, and more consistent outcomes while integrating seamlessly with existing hospital infrastructure. Every platform is engineered to meet clinical, operational, and compliance standards, helping enterprises unlock measurable ROI from day one.
Why Partner With Intellivon?
- Compliance-First Design: Every platform aligns with FDA 510(k), HIPAA, GDPR, and EU MDR frameworks, ensuring clinical trust, data protection, and regulatory readiness from the ground up.
- Seamless System Integration: Our architectures connect effortlessly with PACS, RIS, and EHR environments through FHIR and HL7, enabling full interoperability without disrupting workflows.
- Explainable and Transparent AI: Built-in explainability dashboards, confidence scores, and audit trails give radiologists complete insight into how AI decisions are made, building trust across clinical teams.
- Scalable Cloud-Native Infrastructure: Elastic deployment options allow hospitals to scale across modalities, sites, and geographies with high availability and consistent performance.
- MLOps-Driven Reliability: Continuous monitoring, drift detection, and retraining pipelines ensure models remain accurate, validated, and compliant as imaging data evolves.
- Enterprise-Grade Security: Zero-trust architecture, end-to-end encryption, and real-time threat detection protect patient data while maintaining uninterrupted access for authorized clinicians.
- Proven Healthcare Expertise: With years of experience in delivering large-scale AI healthcare solutions, we bring validated frameworks, domain expertise, and measurable success metrics to every project.
Book a strategy call with Intellivon today to explore how an enterprise-grade AI imaging platform can strengthen your diagnostic accuracy, streamline operations, and prepare your healthcare network for the next generation of intelligent medical imaging.
FAQs
Q1. How do large hospitals and diagnostic enterprises start building AI medical imaging tools from scratch?
A1. This query targets leaders exploring internal AI initiatives. It should walk readers through where to begin, data collection, vendor evaluation, compliance assessment, and ROI forecasting.
Q2. What’s the average time and cost to develop an enterprise-grade AI medical imaging platform?
A2. A highly searched question that blends financial and operational feasibility. Your answer can include phase-wise cost ranges ($150K–$400K) and typical build timelines (6–12 months).
Q3. What regulatory and compliance frameworks must AI imaging tools meet for global deployment?
A3. Enterprise buyers will ask this to plan FDA 510(k), CE MDR, HIPAA, and GDPR compliance early. This builds trust and differentiates Intellivon’s compliance-first architecture.
Q4. How can enterprises secure patient data while training and deploying AI imaging models?
A4. Security and data governance are primary concerns. This query lets you highlight encryption, anonymization, federated learning, and tokenization for cross-institution collaboration.
Q5. How do hospitals ensure the clinical accuracy and reliability of AI imaging predictions?
A5. Decision-makers want evidence that AI outputs are safe. Cover validation protocols, bias testing, explainability (XAI), and continuous monitoring frameworks.