Healthcare is no longer just reactive. It is continuous, connected, and quietly predictive. Every heartbeat recorded by a wearable, every glucose change sent from a sensor, and every trend identified by analytics now holds clinical importance. Yet for many hospitals and digital health innovators, this data is often underused and scattered across devices, clouds, and care teams. This leads to delayed interventions, more readmissions, clinician burnout, and rising operational costs.
Organizations that move from passive monitoring to smart, AI-driven remote patient monitoring are changing this situation. They are transitioning from episodic treatment to real-time health insights. In this approach, deterioration is spotted early, outcomes improve noticeably, and care safely extends beyond hospital walls.
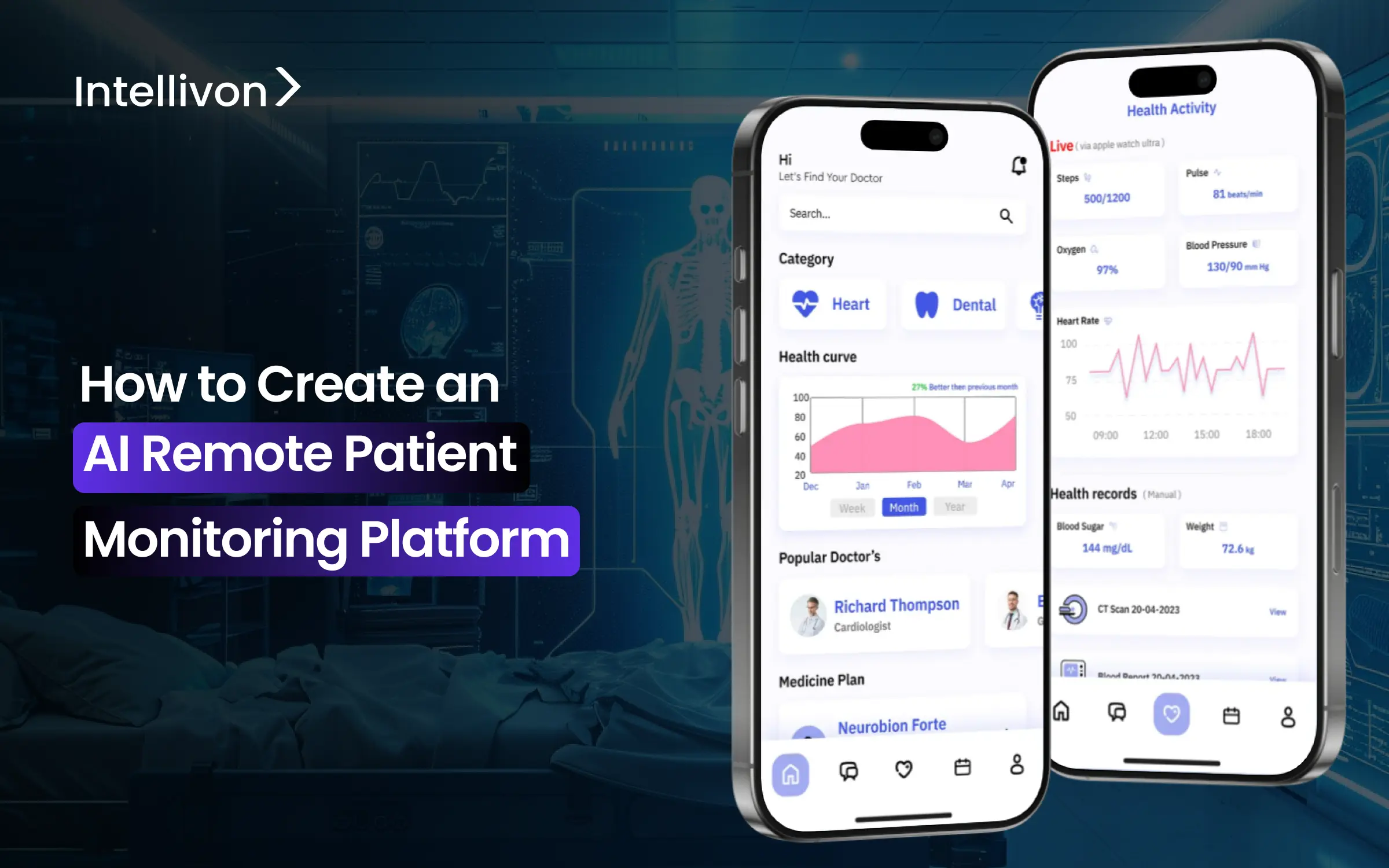
At Intellivon, we design and build AI remote patient monitoring platforms as high-quality clinical systems. Our teams create these platforms with a focus on compliance, predictive intelligence, and strong interoperability with EHR systems. In this guide, we explain how we develop AI-powered remote patient monitoring platforms from the ground up.
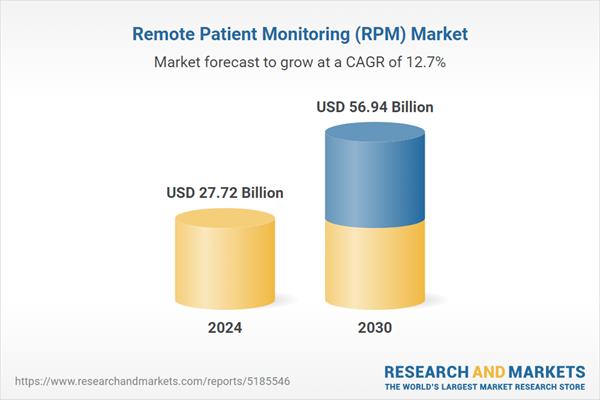
Key Market Insights Of The Remote Patient Monitoring (RPM) Market
The global remote patient monitoring market is expected to grow from USD 27.72 billion in 2024 to USD 56.94 billion by 2030, registering a compound annual growth rate (CAGR) of 12.7% during this period.
One of the key drivers behind this rapid expansion is the escalating incidence of hospital-acquired infections (HAIs). As healthcare systems seek to reduce inpatient exposure risks and improve post-discharge surveillance, remote monitoring is increasingly being adopted as a safer, data-driven alternative to traditional in-hospital follow-ups.
Key Drivers:
- SNS Insider estimates the broader remote patient monitoring market at USD 35.5B in 2024, reaching USD 92.0B by 2032 at a 12.69% CAGR.
- Grand View Research projects the remote patient monitoring system market at USD 22.0B in 2024, growing to about USD 110.7B by 2033 at 19.8% CAGR (device-heavy view).
AI in RPM: platform‑relevant stats
- SNS Insider values the “AI in remote patient monitoring” market at about USD 2.08B in 2024, projecting USD 14.51B by 2032 at a 27.52% CAGR for 2025‑2032.
- In AI‑RPM, AI‑enabled devices (wearables, biosensors, smart monitors) hold roughly 41% share as of 2024, while services (analytics platforms, AI‑driven workflows, virtual care services) are the fastest‑growing component.
- Within AI‑RPM, software and platforms account for about 21.2% market share and are highlighted as the fastest‑growing segment due to demand for advanced analytics, EHR integration, and interoperability.
- Continuous glucose monitors currently dominate AI‑RPM device revenue, while blood pressure monitors are one of the fastest‑growing device categories, linked to global diabetes and hypertension prevalence.
End‑user and application insights
- In overall RPM, hospitals currently dominate with around 47.5% share, but patient‑centric and home‑care segments are identified as the fastest‑growing as reimbursement and value‑based care models expand.
- Patient segments are also highlighted as the fastest‑growing end‑user category in both RPM and AI‑RPM due to rising self‑monitoring, chronic disease prevalence, and interest in personalized care.
- Industry analysts expect up to roughly 30% of the global population to be using some form of RPM solution (including wearables/sensors) around the mid‑2020s timeframe, with wearable sensor markets themselves projected in the tens of billions of dollars.
For healthcare enterprises, investing in AI-driven remote patient monitoring has become a competitive necessity. Those who build now position themselves at the center of value-based care, lower risk exposure, and long-term digital health leadership.
What Is an AI Remote Patient Monitoring (RPM) Platform?
An AI remote patient monitoring (RPM) platform is a digital healthcare system that collects continuous patient health data from connected devices and applies artificial intelligence to analyze, predict, and trigger real-time clinical actions. Unlike traditional monitoring that only records vitals, AI-powered RPM interprets patterns, detects early risk signals, and prioritizes patients who need immediate intervention.
These platforms integrate with EHRs, automate alerts for care teams, and support long-term management of chronic and post-acute conditions. The result is proactive care delivery, fewer emergency events, and scalable monitoring across large patient populations without increasing clinical workload.
How an AI Remote Patient Monitoring Platform Works
An AI remote patient monitoring platform operates as a continuous clinical intelligence loop. Data moves from the patient’s environment into secure systems, gets analyzed in real time, and returns to care teams as actionable insights. Each layer plays a precise role in transforming raw health signals into early intervention and coordinated care.
1. Data Ingestion from IoMT Devices and Wearables
Smart wearables and medical-grade IoMT devices capture vitals such as heart rate, oxygen saturation, glucose levels, blood pressure, and activity patterns. This data streams continuously through encrypted channels without manual input. The system ensures accuracy through device validation and signal-quality checks before processing begins.
2. Secure Cloud Processing Layer
Once ingested, data moves into a HIPAA-ready cloud environment. Here it is normalized, time-synced, and stored in secure patient records. This layer ensures uptime, scalability, and regulatory compliance while handling millions of data points daily across large patient populations.
3. AI and Machine Learning Analytics Engine
The AI engine analyzes incoming data against patient baselines and clinical risk models. It detects anomalies, predicts deterioration, and assigns dynamic risk scores. Instead of static thresholds, the system adapts with each new data pattern and patient response.
4. Clinical Dashboards and Intelligent Alerts
Insights surface through role-based dashboards for nurses, physicians, and care managers. Alerts are prioritized by urgency and clinical relevance. This prevents alert fatigue and ensures rapid response for high-risk patients.
5. EHR Integration and Care Coordination Layer
The platform synchronizes with hospital EHR systems using HL7 and FHIR standards. Monitoring data, alerts, and interventions flow directly into patient charts. Care teams across departments access the same real-time view.
6. Patient and Provider Interaction Loop
Patients receive reminders, feedback, and care instructions through mobile apps. Providers adjust care plans based on live trends. Each interaction feeds back into the AI models for continuous refinement.
An AI-powered RPM platform functions as a closed-loop care engine. It unifies devices, data, intelligence, and clinical action into one continuous workflow. This shift from periodic monitoring to real-time healthcare orchestration is what drives both clinical impact and enterprise scalability.
Top Use Cases of AI Remote Patient Monitoring Platform Development
AI-powered remote patient monitoring is being adopted where it directly impacts enterprise revenue, utilization control, and long-term care scalability. These are the most commercially proven deployments across global healthcare markets today.

1. Chronic Disease Management
Chronic conditions account for the highest recurring cost in healthcare portfolios. AI-powered RPM enables continuous tracking of vitals, medication adherence, and lifestyle signals.
Predictive models identify deterioration early, allowing enterprises to intervene before expensive hospital episodes occur. This directly improves performance under value-based care contracts.
Real-world example:
Omada Health uses AI-driven remote monitoring for diabetes and hypertension patients. Payers and employers use its data-driven programs to reduce long-term complication costs and claims volatility.
2. Post-Surgical Recovery Monitoring
Post-discharge complications are a major source of revenue leakage. AI RPM extends surgical care into the home by tracking recovery vitals, mobility patterns, and pain signals.
Enterprises reduce readmissions, protect bundled payments, and shorten recovery timelines without increasing in-person visits.
Real-world example:
Hinge Health uses AI-based remote monitoring and recovery analytics for post-operative orthopedic patients. Large employers and insurers deploy it to reduce rehabilitation costs and repeat surgical events.
3. Elderly and Assisted Care
Aging populations increase pressure on inpatient capacity and emergency services. AI-powered RPM enables continuous monitoring for falls, cardiac irregularities, hydration levels, and mobility decline in home and assisted living settings.
Enterprises reduce avoidable emergency transfers and long-term care expenses.
Real-world example:
CarePredict uses wearable sensors and AI to monitor elderly residents in assisted living facilities. Providers use their predictive alerts to reduce fall-related hospitalizations and optimize staffing models.
4. High-Risk Pregnancy Monitoring
High-risk pregnancies require close surveillance without frequent hospital visits. AI-enabled RPM tracks blood pressure, glucose, fetal heart trends, and maternal symptoms continuously.
This allows early detection of preeclampsia and gestational complications while reducing inpatient observation costs.
Real-world example:
Babyscripts provides AI-powered remote monitoring for high-risk pregnancies. Health systems use it to reduce emergency obstetric admissions and improve prenatal compliance.
5. ICU-to-Home Care Transition
Patients discharged from intensive care remain vulnerable to rapid deterioration. AI RPM enables stepped-down monitoring at home with predictive risk scoring. Enterprises free ICU beds faster while maintaining post-acute surveillance without extending hospital stays.
Real-world example:
Philips eICU extends critical care monitoring beyond the hospital using connected devices and AI-supported analytics. Health systems use it to manage post-ICU patients remotely and reduce rebound admissions.
6. Mental Health and Behavioral Monitoring
Mental health conditions often deteriorate silently between appointments. AI-powered RPM tracks behavioral activity, sleep trends, medication adherence, and engagement patterns.
Predictive models flag relapse risk before crises occur, reducing emergency psychiatric admissions.
Real-world example:
Mindstrong uses passive smartphone-based monitoring and AI analytics to identify early signs of cognitive and behavioral decline across large payer populations.
7. Cardiac and Respiratory Remote Care
Cardiac and respiratory conditions drive some of the highest emergency utilization rates. AI-powered RPM continuously monitors ECG, oxygen saturation, and respiratory patterns. Predictive alerts help enterprises prevent acute decompensation events.
Real-world example:
Biofourmis provides continuous AI-driven monitoring for heart failure and respiratory patients. Its enterprise deployments have demonstrated reductions in hospital admissions and improved value-based performance.
These use cases show that AI-powered RPM is now embedded into enterprise care delivery, payer strategy, and digital health business models. Organizations that deploy it strategically gain measurable control over utilization, revenue protection, and long-term patient engagement.
How AI-Powered RPMs Reduced Emergency Visits by 30–50%
Emergency departments were never designed for continuous care. Yet for years, they have absorbed the downstream impact of delayed intervention, poor follow-ups, and unmanaged chronic conditions. AI-enabled remote patient monitoring changes that equation. By shifting care from episodic visits to always-on clinical visibility, hospitals are now preventing deterioration before it escalates into emergency admissions. The impact is not theoretical. It is already showing up in utilization numbers, reimbursements, and operating margins.
Across structured RPM programs, emergency visits have dropped by 30–50% in monitored patient populations. This reduction directly translates into lower treatment costs, fewer penalties, and better capacity utilization across hospital networks.
1. Predictive Monitoring Stops Emergencies Before They Start
Traditional monitoring reacts to symptoms after they appear. AI-powered RPM platforms work differently. They analyze continuous streams of vitals, behavioral signals, and device data to detect risk trends early. Blood pressure drift, oxygen variability, cardiac irregularities, and medication non-adherence are flagged in real time.
This predictive layer enables care teams to intervene days or even weeks earlier. As a result, fewer patients deteriorate into emergency situations that require acute care.
2. Chronic Programs Prevent Up to 76% of Readmissions
Structured AI-driven RPM programs for chronic populations have demonstrated up to 76% prevention in hospital readmissions within targeted cohorts. For hospitals operating under value-based contracts, this is not just a clinical win. It directly protects revenue by reducing readmission penalties and improving quality performance scores.
From heart failure and hypertension to COPD and diabetes, continuous monitoring supported by AI triage changes long-term utilization patterns.
3. RPM Programs Deliver Direct Financial Returns
On the revenue side, RPM programs also function as a scalable business line. Industry models show monthly revenue of USD 120–150 per patient, with a practice managing 100 patients generating USD 144,000–180,000 annually. Typical ROI across combined technology and staffing investments ranges between 3x and 5x.
In addition, reimbursement through CPT codes 99453, 99454, 99457, and 99458 creates a predictable payer-backed revenue stream when programs are implemented correctly.
4. Operational Relief for Overloaded Care Teams
AI-driven monitoring also eases pressure on clinical staff. Automated alerts replace manual chart reviews. Risk-prioritized queues ensure nurses focus only on patients who truly need attention. This lowers alert fatigue, improves response times, and allows care teams to manage far larger populations without proportional staffing increases.
AI-powered RPM reshapes emergency utilization, protects hospital revenue, and creates a scalable care delivery model that performs under both value-based and fee-for-service frameworks. For enterprises focused on sustainable growth, this shift is already redefining how care is delivered and reimbursed.
Must-Have Features in AI Remote Patient Monitoring App Development
An enterprise-grade AI remote patient monitoring platform must combine real-time data capture, secure cloud processing, predictive analytics, and clinical system integration.
Core features span three layers: a patient-facing app for data capture and engagement, a provider dashboard for risk-based care decisions, and an enterprise control layer for compliance, governance, and scalability.
Together, these features enable continuous monitoring, early intervention, regulatory alignment, and financially sustainable operations across large patient populations.
1. Patient App Features
The patient app is the primary data entry point and engagement layer. If it fails, the entire monitoring system weakens.
- Vital Tracking: Continuous capture of heart rate, oxygen saturation, glucose, blood pressure, temperature, and activity from connected devices. Data syncs automatically without manual input.
- Medication Reminders: Automated, personalized schedules with missed-dose detection. This directly improves adherence and reduces hospitalization risk.
- Care Communication: Secure messaging for sharing symptoms, photos, and updates with care teams. This replaces delayed phone-based follow-ups.
- Alerts and Self-Reports: Patients receive immediate prompts for abnormal readings and can log symptoms in real time, adding critical context to vital data.
2. Provider Dashboard Features
This is where AI-driven intelligence converts raw data into clinical action and enterprise value.
- Clinical Views: Unified patient timelines that combine historical records with live monitoring streams for fast, informed decision-making.
- Risk Stratification: AI models assign dynamic risk scores so care teams focus first on the most vulnerable patients.
- Alert Management: Intelligent alert prioritization that filters signals from noise and prevents staff overload.
- Care Coordination Tools: Shared task lists, escalation workflows, and intervention tracking across departments and facilities.
3. Admin and Enterprise Control Layer
This layer determines whether the platform can operate at true enterprise scale.
- User Management: Role-based access controls for providers, care managers, administrators, and external partners.
- Audit Logs: Full traceability of data access, alerts, interventions, and system actions for compliance investigations.
- Compliance Reporting: Automated regulatory documentation for HIPAA, GDPR, and internal governance audits.
- Device Management: Centralized onboarding, provisioning, firmware updates, and decommissioning of thousands of monitoring devices.
An AI RPM platform is only as strong as the features that support engagement, intelligence, and governance at scale. Enterprises that get this foundation right gain not only better clinical visibility but also operational stability and long-term digital control over remote care delivery.
Advanced AI Features to Build a Remote Healthcare Monitoring Platform
Advanced AI features in remote healthcare monitoring turn continuous data into real-time clinical intelligence. These capabilities move platforms beyond tracking into prediction, automation, and decision support. For enterprises, they enable earlier intervention, lower care costs, and scalable operations without linear staffing growth.
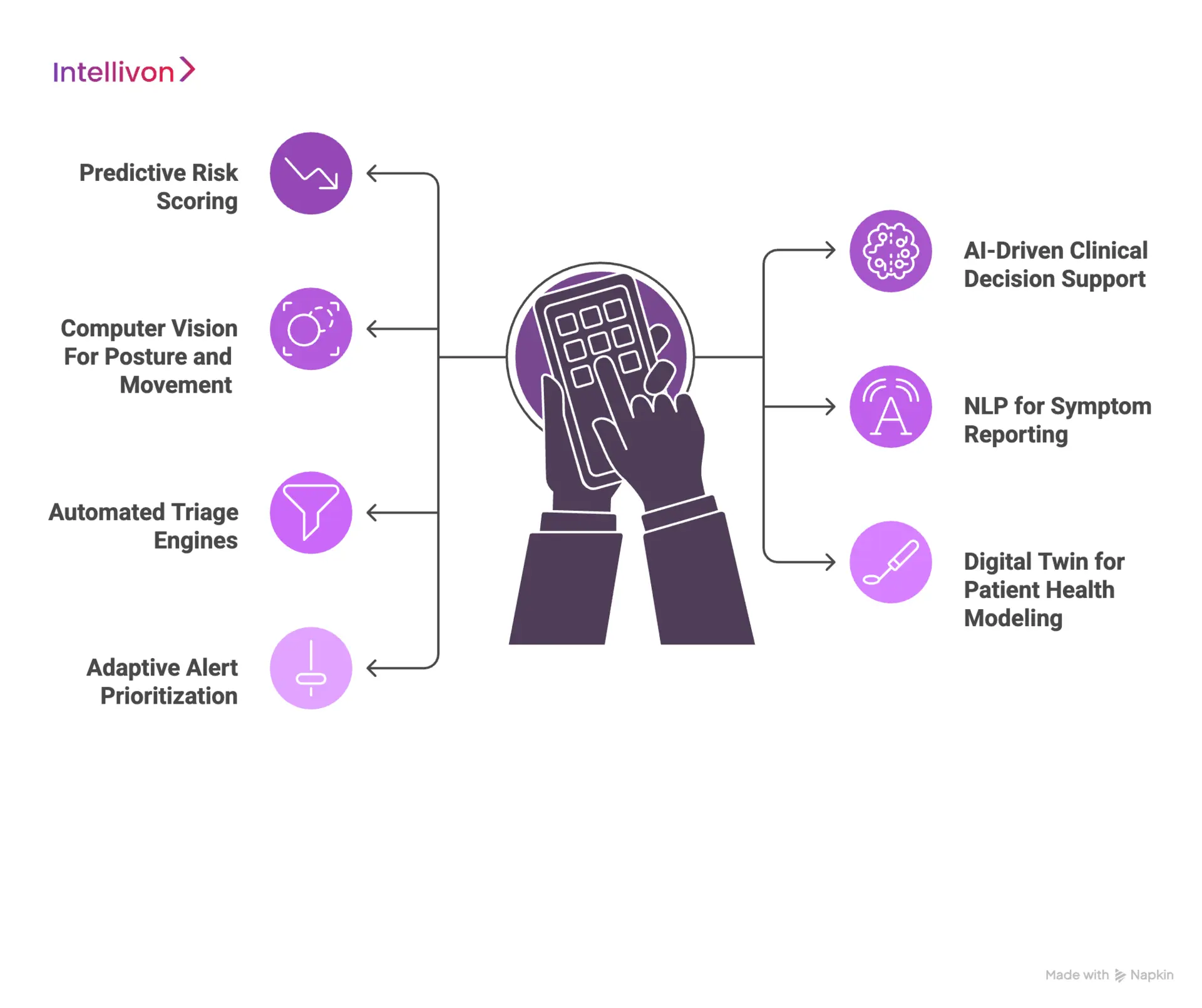
1. Predictive Risk Scoring
Predictive risk engines analyze longitudinal vitals, behavior trends, and clinical history to forecast deterioration before symptoms surface. Instead of reacting to threshold breaches, care teams act on probability-based risk signals. This directly reduces emergency utilization and protects value-based revenue.
2. AI-Driven Clinical Decision Support
Clinical decision support layers interpret patient data against evidence-based protocols. The system suggests interventions, flags guideline deviations, and supports faster clinical decisions. This improves consistency across large care teams while reducing dependency on manual judgment alone.
3. Computer Vision for Posture and Movement
Computer vision models analyze video and sensor-based movement patterns to detect falls, gait changes, and mobility decline. This is especially valuable in post-surgical recovery and elderly care. Enterprises prevent injuries without increasing in-person supervision.
4. NLP for Symptom Reporting
Natural language processing converts unstructured patient inputs into clinical signals. Symptoms entered as free text or voice notes are classified, scored, and routed for review. This eliminates manual triage of messages and accelerates response times.
5. Automated Triage Engines
AI-based triage systems prioritize incoming alerts based on severity, context, and historical outcomes. Low-risk cases are auto-routed for monitoring, while high-risk patients are escalated instantly. This enables enterprise teams to manage large populations without alert fatigue.
6. Digital Twin for Patient Health Modeling
Digital twins create a virtual representation of a patient’s health state using continuous data. These models simulate disease progression and treatment impact over time. Enterprises use them for long-term care planning, not just short-term intervention.
7. Adaptive Alert Prioritization
Adaptive alerting continuously recalibrates thresholds based on patient behavior and response patterns. This prevents repeated false alarms and ensures alerts remain clinically meaningful. Staffing efficiency improves without compromising patient safety.
Advanced AI features transform remote monitoring from a data collection system into a predictive care infrastructure. For enterprises, this means fewer emergencies, faster clinical decisions, and a care model that scales with intelligence rather than headcount.
Tech Stack for AI Remote Patient Monitoring Platform Development
An enterprise-grade AI remote patient monitoring platform requires a secure, scalable, and compliance-ready technology stack. It combines modern frontend frameworks, cloud-native backends, advanced AI/ML engines, encrypted data pipelines, and deep healthcare system integrations.
The right stack ensures real-time performance, regulatory alignment, and long-term scalability across large patient populations.
1. Frontend
The frontend must deliver real-time visibility, low-latency interactions, and accessibility across devices.
- Web dashboards: Built using React for dynamic clinical views and role-based interfaces.
- Mobile apps: Developed with Flutter or native iOS and Android for patient engagement and continuous background syncing.
- Data visualization: Interactive charts using enterprise visualization libraries for trend analysis and alert review.
The goal is fast rendering, offline resilience, and consistent performance across high-usage environments.
2. Backend
The backend acts as the orchestration layer for data ingestion, workflows, and enterprise integrations.
- API layer: Node.js or Spring Boot for high-throughput request handling.
- Microservices architecture: Independent services for alerts, users, devices, analytics, and reporting.
- Real-time processing: Event-driven queues using Apache Kafka.
This design ensures scalability during peak monitoring periods without system degradation.
3. AI and ML Stack
This layer converts raw vitals into predictive intelligence.
- Model development: TensorFlow and PyTorch for training predictive and triage models.
- Model lifecycle management: MLflow for versioning and validation.
- Real-time inference: Dedicated inference servers for sub-second alert generation.
These tools support continuous learning without disrupting live clinical workflows.
4. Cloud and DevOps
Cloud infrastructure determines availability, geographic resilience, and regulatory isolation.
- Primary cloud: AWS, Microsoft Azure, or Google Cloud with healthcare compliance certifications.
- Container orchestration: Kubernetes for workload isolation and auto-scaling.
- CI/CD pipelines: Automated security testing, deployment validation, and rollback support.
This stack supports continuous deployment without clinical downtime.
5. Database and Data Pipelines
Healthcare data requires both transactional accuracy and analytics scalability.
- Operational databases: PostgreSQL for patient records and system metadata.
- Time-series data: InfluxDB for high-frequency vitals.
- Analytics warehousing: BigQuery for long-term trend analysis and population health reporting.
Encrypted pipelines ensure data remains secure in transit and at rest.
6. Security and Compliance Layer
This layer determines whether the platform can operate across regulated markets.
- Identity and access: Keycloak for multi-tenant authentication.
- Encryption: End-to-end encryption using AES-256 and TLS 1.3.
- Audit and monitoring: Centralized logging through Splunk.
Security controls are embedded into every data pathway, not added afterward.
7. Integrations (EHR, Devices, APIs)
Interoperability defines enterprise adoption speed.
- EHR connectivity: FHIR and HL7 interfaces with systems like Epic and Cerner.
- Device integration: APIs for FDA-cleared wearables, glucose monitors, ECG patches, and pulse oximeters.
- Enterprise APIs: Secure REST and GraphQL endpoints for payer platforms, pharmacy systems, and analytics tools.
This integration layer ensures RPM becomes part of the core clinical infrastructure, not a siloed tool.
An enterprise AI RPM platform is only as strong as the stack beneath it. When each layer is engineered for scale, security, and interoperability, the result is a system that performs reliably under clinical pressure and grows smoothly with business expansion.
Our Process to Develop an AI Remote Patient Monitoring Platform
Intellivon develops AI remote patient monitoring platforms through a compliance-first, enterprise-grade delivery process.
The approach integrates clinical discovery, secure architecture, AI model engineering, device interoperability, and scalable deployment to ensure real-world performance, regulatory alignment, and measurable ROI.
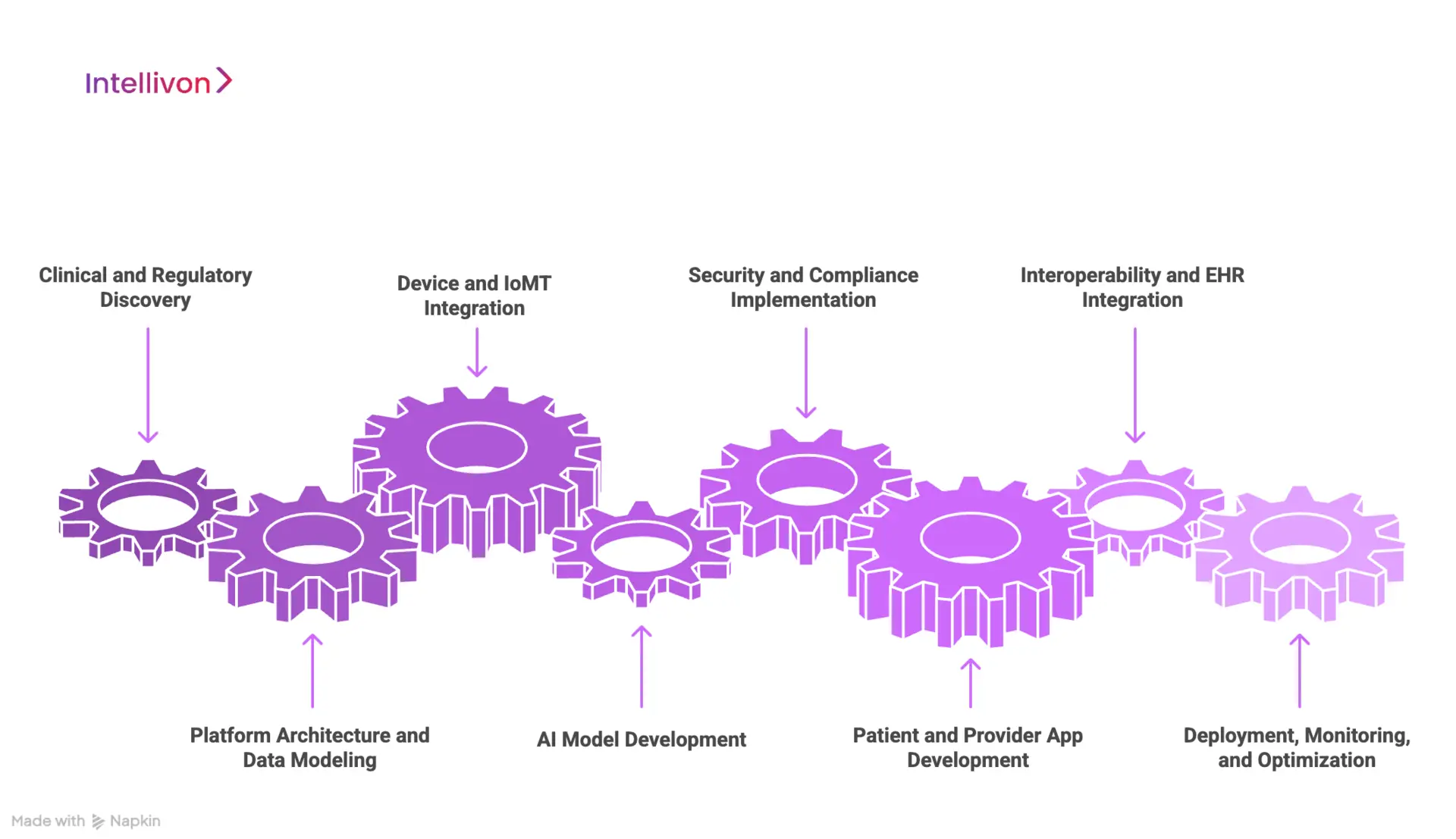
1. Clinical and Regulatory Discovery
We begin with deep clinical workflow mapping and regulatory assessment. This includes understanding care pathways, patient cohorts, reimbursement models, and regional compliance obligations.
The outcome is a validated business and clinical blueprint before a single line of code is written.
2. Platform Architecture and Data Modeling
Our architects design the full system structure across devices, cloud, AI, and enterprise systems. Data models are built for longitudinal patient records, real-time streaming, and population analytics.
This ensures performance does not degrade as usage scales.
3. Device and IoMT Integration
We integrate FDA-cleared wearables and medical devices into secure ingestion pipelines. Each device stream is validated for signal quality, latency, and reliability.
This ensures clinical-grade accuracy for downstream AI analysis.
4. AI Model Development
Our data science teams build predictive risk models, triage engines, and clinical decision support layers using real-world patient data.
Models are trained, validated, and stress-tested for bias, explainability, and clinical relevance before production deployment.
5. Security and Compliance Implementation
Security is architected into every layer. We implement encryption, identity management, audit logging, and access governance aligned with HIPAA, GDPR, SOC 2, and healthcare-specific security frameworks.
Compliance is embedded into workflows, not treated as a separate phase.
6. Patient and Provider App Development
We design patient apps for frictionless adoption and provider dashboards for operational speed. Interfaces are role-based, real-time, and optimized for high-volume monitoring environments.
7. Interoperability and EHR Integration
We connect the platform directly with hospital EHRs, payer systems, and care coordination tools using HL7 and FHIR standards.
This ensures monitoring data flows into existing clinical and revenue workflows without duplication.
8. Deployment, Monitoring, and Optimization
The platform is deployed on a scalable cloud infrastructure with continuous performance monitoring. Post-launch, we refine AI models, optimize alert logic, and adapt workflows based on real usage and outcome data.
Our development process is built for enterprise reality, not laboratory conditions. By unifying compliance, AI intelligence, interoperability, and cloud-scale engineering into one disciplined workflow, we deliver RPM platforms that perform reliably in live clinical environments and scale with long-term business growth.
Ensuring Compliance While Developing an AI Remote Patient Monitoring Platform
Compliance in AI remote patient monitoring is not a legal checkbox. It is a system-wide design discipline that shapes data architecture, access control, AI behavior, and audit readiness.
Enterprise-grade RPM platforms embed regulatory compliance directly into cloud infrastructure, AI workflows, and care delivery operations to ensure trust, scalability, and market eligibility across regions.
1. HIPAA
HIPAA compliance governs how patient health information is collected, stored, transmitted, and accessed. In RPM platforms, this applies to every data stream from wearables, mobile apps, cloud storage, AI inference, and provider dashboards.
Enterprise-grade enforcement includes end-to-end encryption, strict access controls, secure device authentication, and full audit trails for every interaction. Without this foundation, large health systems and payers will not approve deployment.
2. GDPR
For platforms operating across geographies, GDPR defines how personal data is processed, retained, and erased. AI RPM platforms must support explicit patient consent, data minimization, and right-to-erasure workflows.
From an enterprise perspective, GDPR readiness also enables multi-region expansion without rebuilding core architecture. Data residency controls and anonymization pipelines become essential for long-term scalability.
3. FDA SaMD
When AI models influence clinical decisions, they fall under Software as a Medical Device requirements. This impacts how models are trained, validated, updated, and monitored after deployment.
Enterprises must maintain full model traceability, version control, performance documentation, and post-market surveillance to remain compliant as algorithms evolve in production.
4. ISO 13485
ISO 13485 governs how medical software is built, tested, documented, and maintained. For AI RPM platforms, this standard enforces structured development lifecycles, risk management frameworks, and change control.
This discipline is what allows enterprises to move from pilot deployments to national or multi-country rollouts without regulatory friction.
5. SOC 2
SOC 2 addresses how systems protect data against unauthorized access, outages, and operational failures. It validates security controls across availability, confidentiality, and processing integrity.
For enterprise buyers, SOC 2 assurance is often a prerequisite for procurement, especially when RPM platforms integrate with core hospital IT systems.
6. HL7 and FHIR
Interoperability standards define how RPM platforms exchange data with hospital EHRs, laboratory systems, and payer platforms. HL7 and FHIR govern patient records, observations, encounters, and real-time updates.
Without strict adherence to these standards, RPM platforms remain isolated tools instead of an integrated clinical infrastructure.
7. Data Residency and Audit Readiness
Many regions require that patient data remain within national borders. Enterprise RPM architectures must support geo-fenced storage, regional failover, and jurisdiction-specific compliance controls.
Equally important is audit readiness. Every alert, intervention, login, and data access event must be traceable during regulatory inspections or payer audits.
Compliance is the trust layer that determines whether an AI RPM platform can operate at true enterprise scale. Organizations that embed regulatory alignment into architecture from the start move faster into new markets, onboard large health systems smoothly, and protect both revenue and reputation over the long term.
Cost to Build an AI Remote Healthcare Monitoring Platform
For healthcare enterprises and digital health companies starting with one or two high-impact monitoring programs, such as heart failure, post-surgical recovery, or chronic disease management, a lean but fully enterprise-grade AI RPM platform can be launched within a controlled budget. The key is phased execution.
At Intellivon, we design phase-wise cost models aligned with leadership budget cycles, regulatory obligations, and near-term ROI milestones.
Estimated Phase-Wise Cost Breakdown (AI RPM Platform)
| Phase | Description | Estimated Cost (USD) |
| Discovery & Compliance Blueprint | Clinical workflow mapping, cohort definition, RPM use-case prioritization, HIPAA/GDPR readiness | 8,000 – 15,000 |
| Device & Data Integration Design | Wearable/IoMT integration, data normalization, secure ingestion pipelines | 12,000 – 25,000 |
| Core RPM Platform Development | Patient and provider apps, alert workflows, and device management engine | 25,000 – 45,000 |
| AI Model Setup & Validation | Predictive risk models, triage logic, bias testing, and explainability setup | 18,000 – 35,000 |
| Security, IAM & Compliance Controls | Role-based access, encryption, audit logs, consent workflows | 10,000 – 18,000 |
| Clinical Dashboards & Analytics | Real-time dashboards, care performance KPIs, and reporting | 8,000 – 15,000 |
| Testing, QA & Security Validation | Clinical accuracy testing, load testing, penetration testing | 8,000 – 14,000 |
| Pilot Deployment, Training & Rollout | Live pilot deployment, staff onboarding, optimization | 10,000 – 18,000 |
Total Initial Investment Range: USD 110,000 – 185,000
This range supports a secure, scalable, enterprise-ready AI RPM pilot covering one high-impact patient population in a live clinical or payer environment.
Annual Maintenance and Optimization
Ongoing costs include cloud infrastructure, device management, model tuning, compliance monitoring, and platform support.
- 12–20% of the initial build cost annually
- Approx. USD 14,000 – 35,000 per year
These costs remain predictable when infrastructure and AI pipelines are engineered for scale from the start.
Hidden Costs Healthcare Organizations Should Plan For
Even well-scoped RPM programs carry recurring cost variables:
- Expansion into additional patient populations or departments
- New device integrations as monitoring programs grow
- Regulatory documentation updates as rules evolve
- Cloud usage increases with real-time data volumes
- Continuous AI model recalibration to prevent performance drift
- Clinical change management and staff re-training
Planning for these early keeps multi-year scaling financially controlled and audit-safe.
Best Practices to Stay Within the USD 100K–200K Budget
Organizations that control RPM build and expansion costs typically:
- Start with one high-risk, high-ROI patient cohort only
- Avoid multi-device and multi-region complexity in phase one
- Use modular platform architecture to add programs later
- Enforce security and regulatory alignment from day one
- Track ROI, readmissions, and utilization weekly during the first 90 days
This ensures the platform proves both clinical and financial value before larger capital deployment.
Get a Budget-Aligned RPM Build Plan from Intellivon
At Intellivon, we specialize in building enterprise-grade AI remote patient monitoring platforms within strict budget controls. We align clinical scope, AI depth, device integrations, and compliance layers to deliver measurable ROI without unnecessary capital burn.
Contact us for a tailored cost estimate and phased rollout plan aligned with your enterprise growth strategy.
Case Study: Building An AI RPM Platform For A Healthcare Enterprise
This case study shows how an enterprise healthcare network partnered with Intellivon to deploy a secure, EHR-integrated AI remote patient monitoring platform at scale. The goal was to extend care beyond hospital walls while reducing readmissions and operational strain.
The company is a multi-facility healthcare enterprise managing large post-discharge and chronic patient populations. While their core EHR workflows were mature, they lacked a unified RPM layer to monitor patients continuously outside clinical settings.
Business Problem
Care teams had limited post-discharge visibility. Readmission risk remained high for cardiac and chronic patients. Device data was fragmented, and existing systems could not support real-time monitoring or predictive risk detection at an enterprise scale.
Solution Architecture
Intellivon built a cloud-native AI RPM platform integrating wearable devices, secure data pipelines, predictive analytics, and SMART on FHIR–based EHR interoperability. The system enabled real-time vitals streaming, automated alerts, and centralized care dashboards.
AI Models Used
- Predictive risk scoring for early deterioration detection
- AI-driven triage and alert prioritization
- Long-term trend analytics for chronic condition monitoring
Results Achieved
- 35% reduction in hospital readmissions
- 25% increase in post-discharge patient engagement
- Faster clinical response through real-time alerting
- Scalable deployment across multiple care units without added staffing pressure
This deployment demonstrates how an enterprise-grade AI RPM platform can move beyond pilots into measurable business and care transformation. When architecture, AI, and compliance are aligned from the start, RPM becomes a long-term strategic growth asset, not just a monitoring tool.
Top AI Remote Patient Monitoring Platforms in the Market
AI-powered remote patient monitoring (RPM) is evolving fast. A handful of platforms now combine continuous vital-sign tracking, predictive analytics, and clinical-grade workflows, making them attractive for health systems, payers, and enterprises planning remote care programs. Below are five leading solutions worth evaluating.
1. Biofourmis
Biofourmis offers a mature, FDA-cleared platform that supports in-home care, chronic condition tracking, and acute-to-home transitions. Its “Care” solution integrates wearable sensors, real-time vitals monitoring, and AI-driven analytics to flag early risk.
Some deployments have cut 30-day readmissions by up to 50%, reduced the cost of care by nearly 38%, and enabled the detection of patient deterioration more than 20 hours earlier than standard care.
Its recent partnership with GE HealthCare underscores its enterprise credibility and ability to extend care outside traditional hospital settings.
2. Datos Health
Datos Health offers a flexible, device-agnostic RPM platform that supports multiple care pathways, from chronic disease management to post-acute monitoring and hybrid care delivery. Its AI-powered “Open Care” studio lets care teams build customized remote-care workflows without heavy coding.
Enterprises appreciate its adaptability: they can launch a diabetes program, then expand to cardiac rehab or oncology monitoring, all using the same underlying platform. That flexibility helps reduce vendor lock-in and supports long-term growth across clinical verticals.
3. Current Health
Current Health offers an FDA-cleared RPM solution that delivers “hospital-level insights” directly into patients’ homes. Its platform supports continuous vital-sign monitoring, multi-variable alarming, and contextual patient data.
This enables remote care teams to catch early clinical risks before emergency escalation.
4. HealthSnap
HealthSnap combines RPM and chronic care management (CCM) with a device-agnostic, cellular-enabled system.
Its 2025 partnership with a major academic medical system (for hypertension management) shows growing institutional trust and enterprise-scale adoption for remote care and monitoring workflows.
Adopting such platforms can accelerate your shift to remote care, reduce readmissions, and transform patient monitoring from episodic to continuous, all while preserving compliance, scalability, and financial viability.
Conclusion
AI-powered remote patient monitoring is no longer an experimental layer in healthcare. It has become a foundational platform for scaling care delivery, protecting margins, and meeting the growing demands of value-based models. Enterprises that treat RPM as core digital infrastructure rather than an add-on gain earlier intervention, better utilization control, and stronger continuity of care across populations.
The real question is no longer whether to adopt AI-driven monitoring, but how strategically it can be embedded into long-term enterprise architecture. Organizations that move with clarity, regulatory foresight, and scalable design will not only reduce risk and cost but will also define the next standard of continuous, connected healthcare delivery.
Build Your AI Remote Patient Monitoring Platform with Intellivon
At Intellivon, we design AI remote patient monitoring platforms that combine clinical intelligence, compliance-first architecture, and enterprise-scale reliability. Our systems integrate seamlessly with EHRs, IoMT devices, and core hospital IT to deliver secure, real-time, outcomes-driven remote care from day one.
Each platform is engineered for modern healthcare enterprises: interoperable, scalable, and built for measurable operational and financial ROI across chronic, post-acute, and high-acuity monitoring programs.
Why Partner With Intellivon?
- Compliance-first delivery aligned with HIPAA, GDPR, FDA SaMD, and global healthcare regulations
- Healthcare-trained AI models for predictive monitoring and intelligent triage
- Deep interoperability with EHR, devices, and enterprise systems via HL7, FHIR, and secure APIs
- Cloud-native scalability with continuous performance and model optimization
- Zero-trust security and human-in-the-loop governance for clinical accountability
Book a strategy call to explore how a custom AI RPM platform can scale care delivery, strengthen compliance, and unlock long-term enterprise growth.
FAQs
Q1. What regulations apply to AI remote patient monitoring platforms?
A1. AI RPM platforms must comply with HIPAA for patient data protection in the US, GDPR for data privacy in the EU, and FDA SaMD rules when AI influences clinical decisions. Large enterprises also require SOC 2, ISO 13485, and HL7/FHIR interoperability compliance to pass procurement and audits.
Q2. How accurate are AI remote patient monitoring systems?
A2. Enterprise-grade AI RPM platforms achieve 85–97% predictive accuracy depending on the condition, data quality, and model design. Accuracy improves continuously through MLOps pipelines, real-world data feedback, and clinical validation loops built into regulated deployments.
Q3. How long does it take to build an AI RPM platform?
A3. A production-ready AI RPM pilot typically takes 4–6 months for one patient cohort. Full enterprise rollout across multiple departments and devices usually requires 8–12 months, depending on integrations, compliance scope, and geographic deployment.
Q4. What devices can integrate with AI RPM platforms?
A4. AI RPM platforms integrate with FDA-cleared wearables, including ECG patches, glucose monitors, blood pressure cuffs, pulse oximeters, temperature sensors, spirometers, and activity trackers. Integration is handled through secure device APIs and healthcare-grade data ingestion pipelines.
Q5. What is the ROI of AI remote patient monitoring for hospitals?
A5. Hospitals typically see 3x–5x ROI within 12–24 months through reduced readmissions, lower emergency utilization, new reimbursable RPM revenue, and improved staffing efficiency. ROI is highest in chronic care, post-acute monitoring, and value-based care programs.