Hospitals are now using ambient AI scribes to help clinicians save hours on endless documentation tasks. These systems capture real-time doctor-patient conversations and convert them into structured notes within the EHR. However, as hospitals expand digital care, the stakes have changed. Today’s clinical environments require more than just transcription. They need systems that can understand complex interactions, fit specialty-specific workflows, and manage a web of regulatory requirements that is becoming more complicated.
At Intellivon, we create next-generation ambient AI scribe platforms designed for the challenges of 2025 and beyond. Our systems can handle the most difficult parts of modern healthcare, including multilingual encounters, fragmented EHR systems, and compliance rules that change faster than most vendors can keep up with. In this blog, we discuss the key features every ambient AI scribe platform in 2025 should have, from multi-agent orchestration to automated compliance checks, and how we design them to meet the changing needs of healthcare organizations that cannot afford downtime, mistakes, or vendor lock-in.
Key Takeaways of the AI Scribe Platforms Market
HTF Market Intelligence reports that AI-enabled clinical documentation is becoming one of the fastest-growing segments in digital health. Ambient AI scribes function as advanced intelligent clinical documentation platforms. The market, valued at just over USD 3 billion today, is forecasted to surge past USD 26 billion, supported by a projected 24 percent annual growth rate.
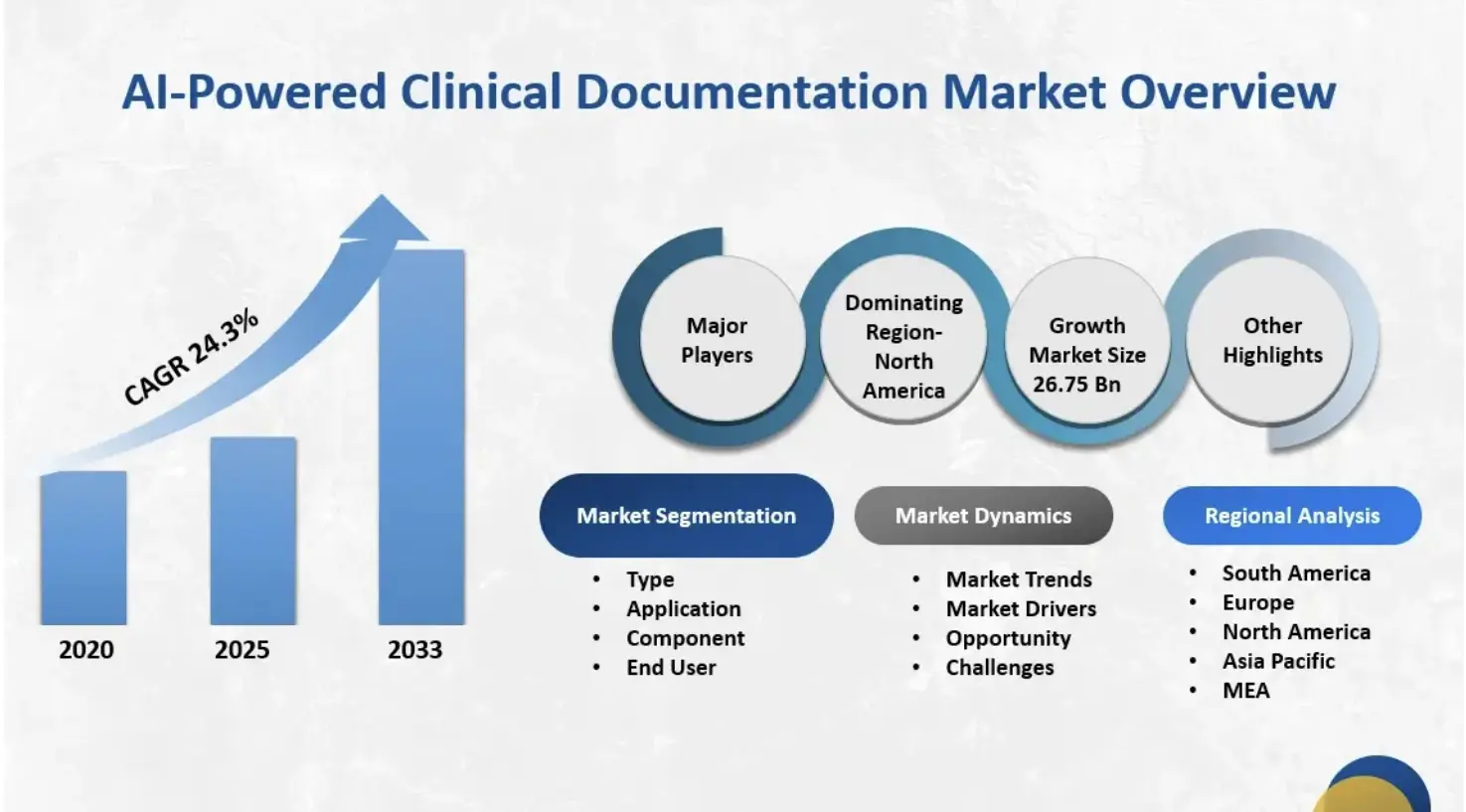
Key Market Insights:
- The ambient scribe category is the fastest-growing segment in clinical AI, generating an estimated $600 million in annual revenue in 2025.
- It exceeds revenue from any other single clinical AI application, growing 2.4x year-over-year.
- The global AI medical scribe software market reached approximately $1.12 billion in 2024.
- Forecasts suggest a compound annual growth rate of about 20.4% through 2033.
Adoption Rates and Penetration
- By the end of 2025, an estimated 30%–60% of healthcare providers will be using ambient scribe tools.
- Within large health systems, adoption is already near 35%.
- Market analysts expect adoption to level off at around 40% over the next three years as early demand stabilizes.
Key Drivers of Enterprise Adoption
- Burnout mitigation remains the primary driver influencing purchasing decisions.
- Additional motivators include improved care quality, revenue optimization, and faster deployment compared to human scribe models.
- Case studies show ambient scribes can save providers more than eight hours per week.
- Some systems report up to 75% lower documentation costs compared to traditional human scribe programs.
- These savings are central to ROI justification for enterprise buyers.
Competitive Landscape and Differentiators
- The U.S. market includes more than 60 vendors.
- Major EHR providers like Nuance (Microsoft), Oracle, and Epic control roughly 33% of the market.
- AI-native companies such as Abridge hold around 30%, while Ambience has close to 13%.
- Growing competition is pushing vendors to expand from “just scribing” to broader clinical and administrative automation.
- Many platforms now bundle documentation, coding support, compliance workflows, and revenue cycle automation.
Investment and Market Maturity
- More than $975 million has been invested in ambient AI scribe companies in 2025.
- These investments show strong confidence in the technology, but also indicate a crowded and rapidly maturing landscape.
- Analysts expect widespread saturation in ambulatory healthcare within the next 24–36 months.
Healthcare enterprises that secure ambient scribe workflows protect patient trust and shield themselves from legal, financial, and reputational damage. Strong safeguards turn automation into a sustainable advantage, not a cybersecurity risk.
Understanding How Ambient AI Scribe Platforms Work
Ambient AI scribes quietly transform how documentation happens. They listen, interpret, and record clinical encounters in real time, automating every step, from conversation capture to compliant note creation, without interrupting care.
1. Secure Data Capture
Each encounter begins with secure, multi-channel audio capture. The system records through microphones or telehealth streams, filters background noise, and distinguishes between speakers. Advanced acoustic models adapt to different accents and room dynamics seamlessly.
All data travels through encrypted channels and is processed on secure edge devices, ensuring PHI remains local and compliant with HIPAA, GDPR, and hospital policies.
2. Speech Recognition and Context Extraction
Once captured, advanced ASR converts spoken language into precise transcripts. But accuracy alone is not enough.
NLP models trained on medical language interpret meaning, identifying symptoms, diagnoses, and medications. They separate patient concerns from clinician notes, forming the contextual backbone needed for structured, reliable documentation.
3. Real-Time Note Generation
Next, large language models generate draft notes in real time. Using structured SOAP or narrative formats, they draw on past data, including lab results, imaging, and prior diagnoses, through Retrieval-Augmented Generation (RAG).
This ensures every record reflects clinical continuity, building a complete and coherent patient narrative across encounters.
4. Compliance and Human Review
Before notes enter the EHR, compliance modules automatically verify completeness, terminology accuracy, and policy alignment.
Clinicians remain the final authority by reviewing and approving drafts within seconds. This process keeps trust intact while removing hours of administrative work from every shift.
5. EHR and Workflow Integration
Once validated, the note syncs automatically to the correct patient file within the EHR. Seamless integration across mobile and desktop tools ensures clinicians can access documentation from anywhere, whether in a hospital, clinic, or telehealth session.
By fitting naturally into existing workflows, the scribe enhances efficiency without changing behavior.
An ambient AI scribe merges recognition, reasoning, and compliance into a single automated flow. It gives clinicians the time to focus on patients and not paperwork.
How Ambient AI Scribes Save 15,791 Hours of Documentation Per Year?
One ambient AI scribe health system saved 15,791 hours of documentation time in a single year after deploying an ambient AI scribe across 2.5 million encounters. That is equivalent to freeing nearly 1,800 full workdays, directly reinvested into patient care.
This operational gain was recorded by The Permanente Medical Group, which tracked measurable improvement in documentation efficiency. Here is how ambient AI scribes are solving traditional clinical documentation burdens:
1. Reducing Burnout by 13.9 Percentage Points
In a multicenter quality-improvement study across six health systems, clinician burnout rates dropped from 51.9% to 38.8% after 30 days of ambient scribe use. Participants also spent nearly one hour less on after-hours charting per shift.
The study tied these improvements directly to reduced administrative friction.
3. Shorter Notes and Faster Closures
A separate pilot covering 46 clinicians across 17 specialties showed that the average time spent in the EHR dropped from 50.6 minutes to 35.4 minutes per day.
Same-day chart closure rates improved from 66.2% to 72.4%, proving that AI-assisted workflows shorten documentation cycles and speed follow-ups.
4. Compounding Efficiency
Another trial found that median daily EHR time decreased by 19.95 minutes per clinician, adding up to more than 80 hours saved per provider each year.
At the system scale, those minutes compound into thousands of hours and measurable cost savings.
5. Benchmark for Adoption and Trust
By late 2024, a survey of 43 major U.S. health systems found ambient clinical documentation to be the only AI use case with 100% active adoption and 53% reporting strong success.
This level of maturity is unusual for clinical technology because it signals that ambient AI has crossed from pilot to enterprise standard.
6. From Hours Saved to Revenue Recovered
Hospitals using ambient AI scribes report increased billing precision and fewer missed codes.
Independent ROI validation shows an average $13K annual uplift per clinician, largely from more accurate coding and faster chart completion.
7. Model Accuracy Outpacing General LLMs
A 2024 arXiv benchmark of a domain-specific “Sporo AI Scribe” model achieved F1 = 75.3, outperforming baseline LLMs such as GPT-3.5 and Llama 3.2 on clinical summarization tasks.
This demonstrates how smaller, fine-tuned models can outperform large generic ones in healthcare settings.
8. Core Investment Area
According to the State of AI in Healthcare 2025 report, ambient AI documentation now ranks among the top three enterprise AI investment priorities, alongside diagnostic imaging and predictive analytics.
This shift signals a broad consensus where documentation automation is no longer peripheral and is a part of the strategic infrastructure.
Ambient AI scribes reshape operational capacity, enable better revenue capture, and restore clinicians’ attention to patient care. For enterprises evaluating next-generation documentation systems, these figures form the proof of why investing now creates a measurable impact within a single fiscal cycle.
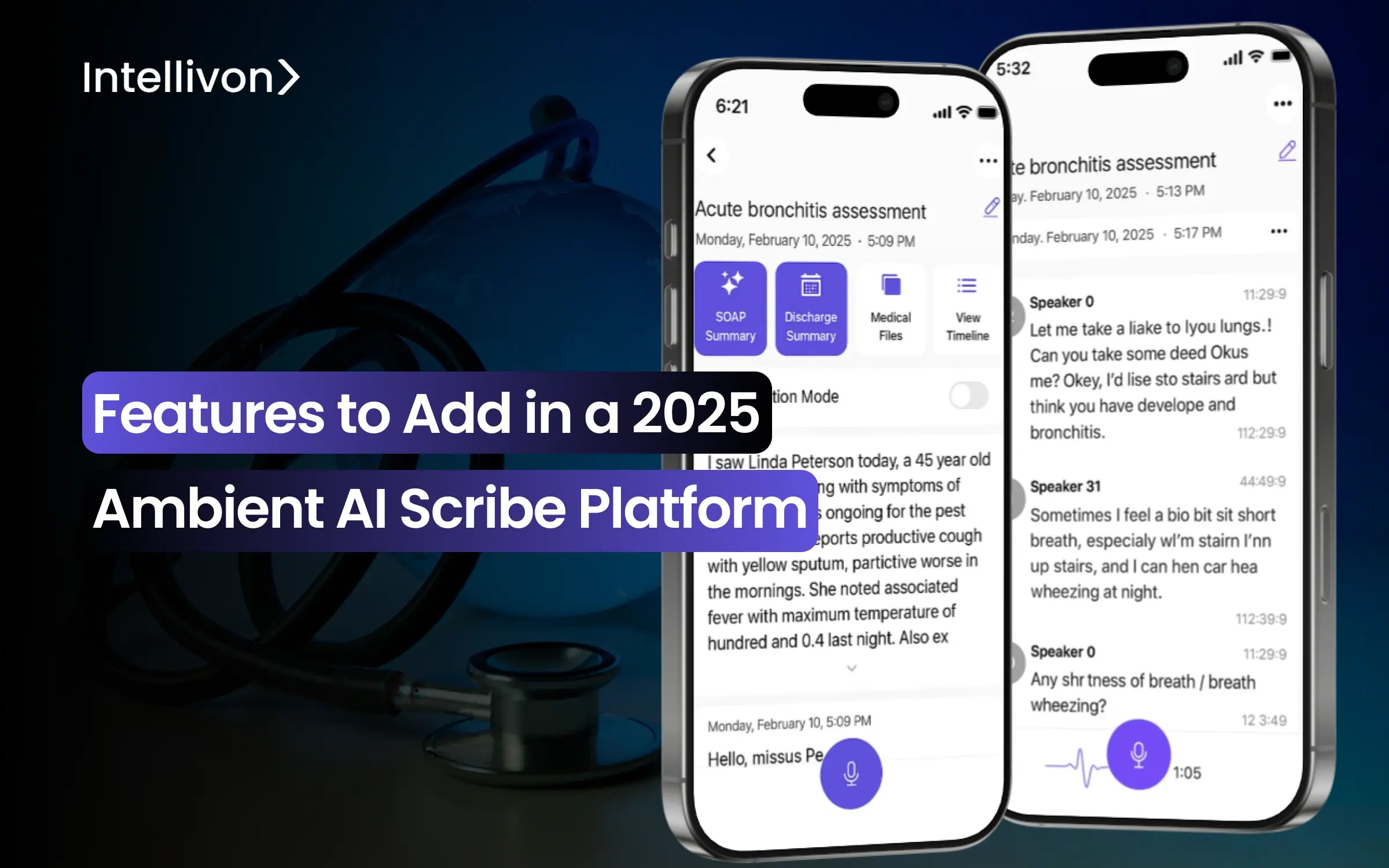
Must-Have Features in a 2025 Ambient AI Scribe Platform
The expectations for documentation technology have changed. Hospitals need intelligent, compliant systems that understand context, adapt to workflow, and scale across departments. The following features define what every 2025-ready ambient AI scribe must deliver to meet enterprise standards for accuracy, trust, and growth.
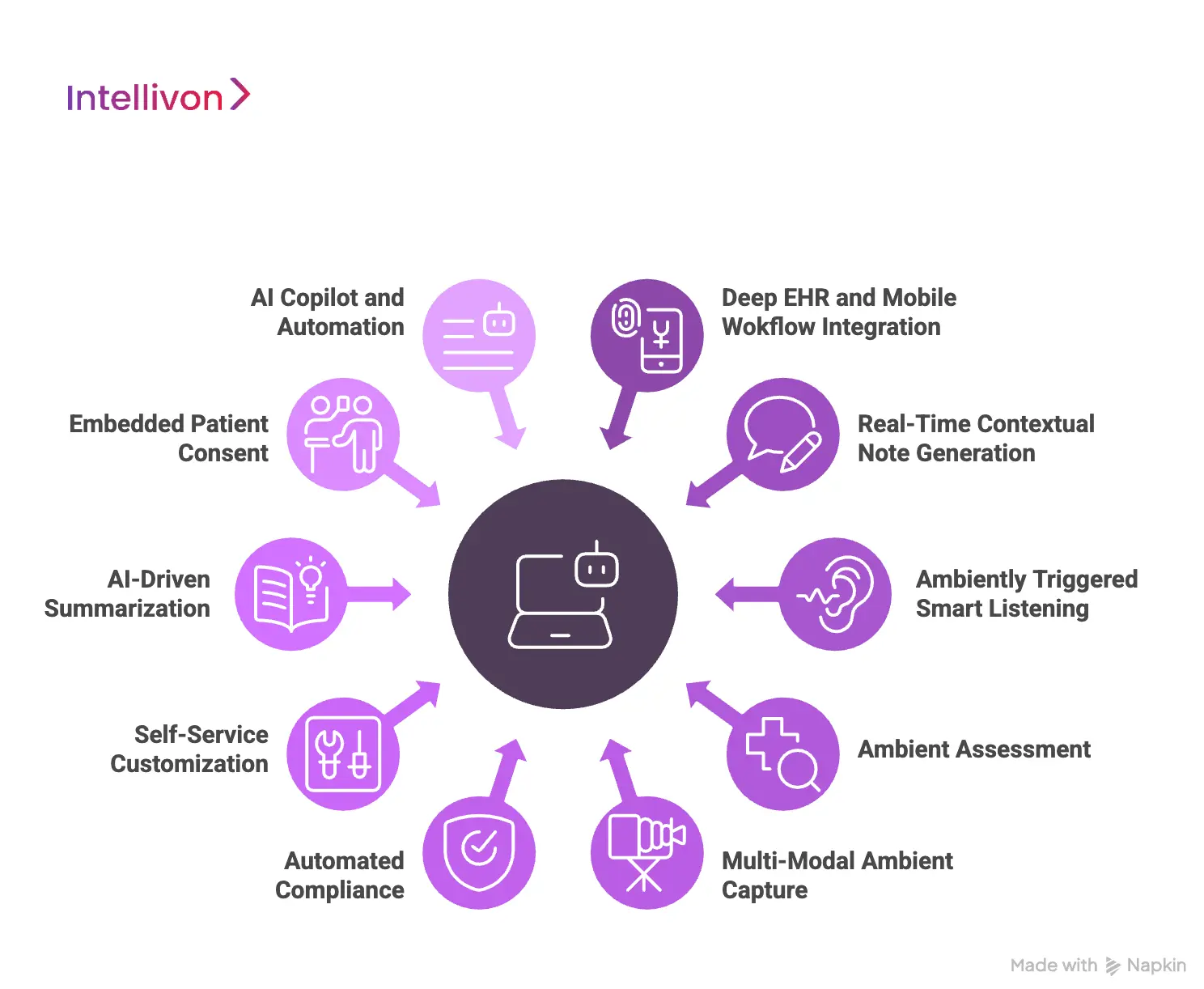
1. Deep EHR and Mobile Workflow Integration
Modern scribes live inside EHRs and mobile tools and are not standalone tools anymore. Documentation happens where care occurs, not after the fact.
Zero-click note creation, instant synchronization, and unified mobile access eliminate friction entirely. When clinicians can dictate or approve from any device, productivity rises naturally and adoption becomes effortless.
2. Real-Time Contextual Note Generation
These systems listen intelligently, not mechanically. They identify conditions, comorbidities, and follow-ups as the conversation unfolds, automatically proposing ICD-10 and CPT codes.
For enterprises, this means better revenue integrity and compliance accuracy. By the time a clinician signs off, coding is already aligned, thereby cutting rework and audit risk dramatically.
3. Ambiently Triggered Smart Listening
Privacy-aware listening defines the next generation. Instead of always recording, the system detects when a consultation begins and activates only when contextually relevant.
This ensures personal conversations never enter the dataset. It is a small change with a big impact, which is maintaining continuous intelligence without crossing privacy boundaries.
4. Ambient Assessment
Today’s scribes can rebuild an entire patient journey automatically. They connect symptoms, lab data, and treatment notes across visits to form a complete medical narrative.
For clinicians, that means fewer blind spots. For administrators, it brings unprecedented visibility into care quality, outcomes, and long-term trends.
5. Multi-Modal Ambient Capture
2025 ambient AI scribe platforms move beyond voice and understand gestures, integrate scanned images, and support multilingual documentation for diverse patient populations.
This multimodal intelligence ensures every interaction is captured accurately, whether through speech, visuals, or translation. The result is inclusivity without complexity.
6. Automated Compliance
Every note passes through a built-in validation layer before reaching the EHR. The AI flags inconsistencies, missing sections, or potential compliance risks in real time.
Designed around frameworks like HIPAA, GDPR, and the EU AI Act, this step gives compliance teams cleaner data and fewer late-stage corrections.
7. Self-Service Customization
No two clinicians document alike. Modern scribes let users customize templates, phrasing, and structure instantly, and no IT request is required.
That autonomy accelerates adoption, reduces change fatigue, and keeps enterprise rollouts nimble even across large hospital networks.
8. AI-Driven Summarization
These platforms extend their intelligence beyond clinicians. They generate simplified, patient-ready summaries that translate medical notes into understandable language.
It reflects a dual benefit, where there is improved communication for patients and greater transparency for compliance teams monitoring literacy mandates.
9. Embedded Patient Consent
Transparency is now a design principle. Visual indicators, voice consent capture, and immutable audit logs make every recording and note verifiable.
This strengthens patient trust while giving enterprises defensible compliance records, which is a necessity in regulated, multi-jurisdiction healthcare systems.
10. AI Copilot and Automation
The modern ambient scribe handles scheduling, prior authorization, and billing tasks, and is becoming a true operations copilot.
For leadership teams, that means measurable ROI, which includes faster cycles, fewer handoffs, and unified automation driving both clinical and administrative efficiency.
Each of these capabilities reflects a deeper shift from passive documentation to active intelligence. The 2025 ambient AI scribe is an integrated decision layer that learns, adapts, and scales with the enterprise itself.
Advanced Features Driving 2025 Innovation
The most advanced ambient AI scribes go beyond automation. They combine reasoning, collaboration, and privacy-centered intelligence that scales across enterprise healthcare systems.
1. Context-Aware Multi-Agent Orchestration
Modern ambient scribes use multiple specialized AI agents that collaborate in real time. One manages transcription, another ensures compliance, while others retrieve medical data or validate logic.
This orchestration creates a self-correcting workflow, where every agent performs its task independently but communicates constantly through a shared reasoning layer. The result is faster processing, higher reliability, and reduced system errors, which is crucial for large health networks managing thousands of concurrent encounters daily.
For enterprise IT teams, this modular design also means easier scaling and maintenance without downtime.
2. Retrieval-Augmented Generation (RAG)
Accuracy defines trust in clinical AI, and RAG makes it possible. Instead of generating content from a static model, RAG systems retrieve relevant information from structured knowledge bases like EHRs, SNOMED CT, or institutional policies before composing notes.
This ensures every summary or recommendation is grounded in real-world evidence, reducing hallucination and increasing factual reliability.
Enterprises gain not only better documentation accuracy but also audit-ready explainability, which is an essential advantage for regulated healthcare environments.
3. Federated and Edge Learning
Federated learning allows ambient scribes to train across multiple hospital systems without moving sensitive patient data. Each node updates the central model using encrypted parameters rather than raw records, ensuring compliance with HIPAA, GDPR, and emerging AI governance laws.
Combined with edge inference, hospitals can process data locally with minimal latency, achieving real-time transcription and compliance assurance even in low-connectivity environments. This approach enables continuous learning while preserving institutional control over every data point.
4. Neuro-Symbolic Reasoning
Neuro-symbolic reasoning merges neural networks’ pattern recognition with rule-based medical reasoning. Before finalizing a note, the AI cross-checks relationships between symptoms, diagnoses, and medications against known clinical guidelines.
This hybrid reasoning prevents contradictions, like mismatched dosages or incorrect symptom associations, before they reach the record.
It is explainable AI that mirrors a clinician’s thought process, giving enterprises both accuracy and interpretability.
5. Voice-Activated Clinical Copilot Mode
Beyond documentation, advanced systems now act as interactive copilots. Clinicians can ask natural-language questions, like “Summarize the last three visits,” “Show abnormal labs,” or “Draft the discharge plan.”
The AI retrieves and summarizes information instantly, merging speech recognition, retrieval, and reasoning in one interaction. This creates an entirely new user experience where clinicians converse with their documentation system instead of typing into it.
For enterprises, it translates into higher adoption, lower burnout, and measurable productivity gains. These five innovations define the next frontier of ambient AI scribes in healthcare enterprises.
Platform Architecture of a 2025 Ambient AI Scribe System
At Intellivon, we build ambient AI scribe architectures that merge intelligence, compliance, and scalability into one cohesive ecosystem. Every layer is purpose-built to deliver accuracy, resilience, and security across hospital networks, clinics, and digital health platforms worldwide.
1. Data Ingestion and Capture Layer
Every intelligent system begins with data, and how it’s captured defines everything that follows. Our architecture records clinician-patient interactions through secure microphones, mobile devices, or telehealth channels, filtering noise and distinguishing between speakers automatically.
Edge processing ensures raw audio is anonymized before it leaves the source, keeping PHI fully protected under HIPAA, GDPR, and regional data policies. This creates the foundation for structured, compliant inputs that can be processed in real time without compromising privacy or fidelity.
2. Multi-Agent Intelligence Layer
At the heart of every Intellivon build lies a coordinated network of AI agents. Each agent is designed for a distinct function, like transcription, context extraction, summarization, compliance validation, or knowledge retrieval.
They operate in parallel, orchestrated through a real-time control layer that enables simultaneous listening, reasoning, and verification. This modular structure allows enterprises to evolve without disruption, and new functions, compliance checks, or integrations can be added without ever rebuilding the core.
3. Knowledge and Retrieval Layer (RAG Stack)
Accuracy is non-negotiable in clinical documentation. RAG layer ensures every output is grounded in real, verifiable data. By connecting directly to trusted repositories, like EHRs, medical ontologies, and institutional knowledge bases, the system retrieves relevant information before generating a note.
This eliminates hallucinations, creates fully auditable output, and ensures that every record produced can stand up to both clinical review and compliance scrutiny.
4. Model Management and Learning Layer
AI in healthcare learn responsibly and cannot remain static. We design this layer to govern how models evolve safely over time. Federated learning allows hospitals to train locally on anonymized data, improving accuracy without ever sharing patient records externally.
Every update is encrypted, version-controlled, and fully auditable, while differential privacy safeguards individual identity even in aggregate learning. For multi-site enterprises, this creates a living, unified intelligence network that improves continuously while preserving strict compliance boundaries.
5. Compliance and Security Layer
We treat compliance like an architectural principle. Our zero-trust framework enforces encrypted communication, identity-based access, and immutable audit logs across every interaction.
Automated redaction modules remove sensitive identifiers before model access, while built-in consent workflows and risk scoring engines ensure every transaction aligns with hospital policy and regulatory frameworks.
6. Integration and Workflow Layer
Technology only succeeds when it disappears into the workflow. Using FHIR, HL7, and SMART-on-FHIR APIs, our systems integrate seamlessly with existing EHRs and third-party hospital software.
Notes sync automatically, coding recommendations trigger billing actions, and summaries flow into patient portals in real time.
7. Analytics and ROI Layer
Every enterprise initiative must prove its impact. Our architecture concludes with an intelligence layer designed to quantify performance, adoption, and return on investment.
Dashboards track documentation time saved, compliance accuracy, and department-level utilization, while real-time analytics identify bottlenecks and improvement opportunities.
For decision-makers, this closes the loop for turning AI adoption into measurable business outcomes that support scaling with confidence.
At Intellivon, our ambient scribe architecture transforms documentation from an administrative burden into a strategic intelligence layer.
Our Process Of Building an Ambient AI Scribe Platform
At Intellivon, we approach the development of ambient AI scribe platforms as a long-term strategic partnership, and not a one-time build. Every system we design is engineered for precision, scalability, and clinical trust, thereby blending advanced AI engineering with deep domain expertise in compliance and healthcare operations.
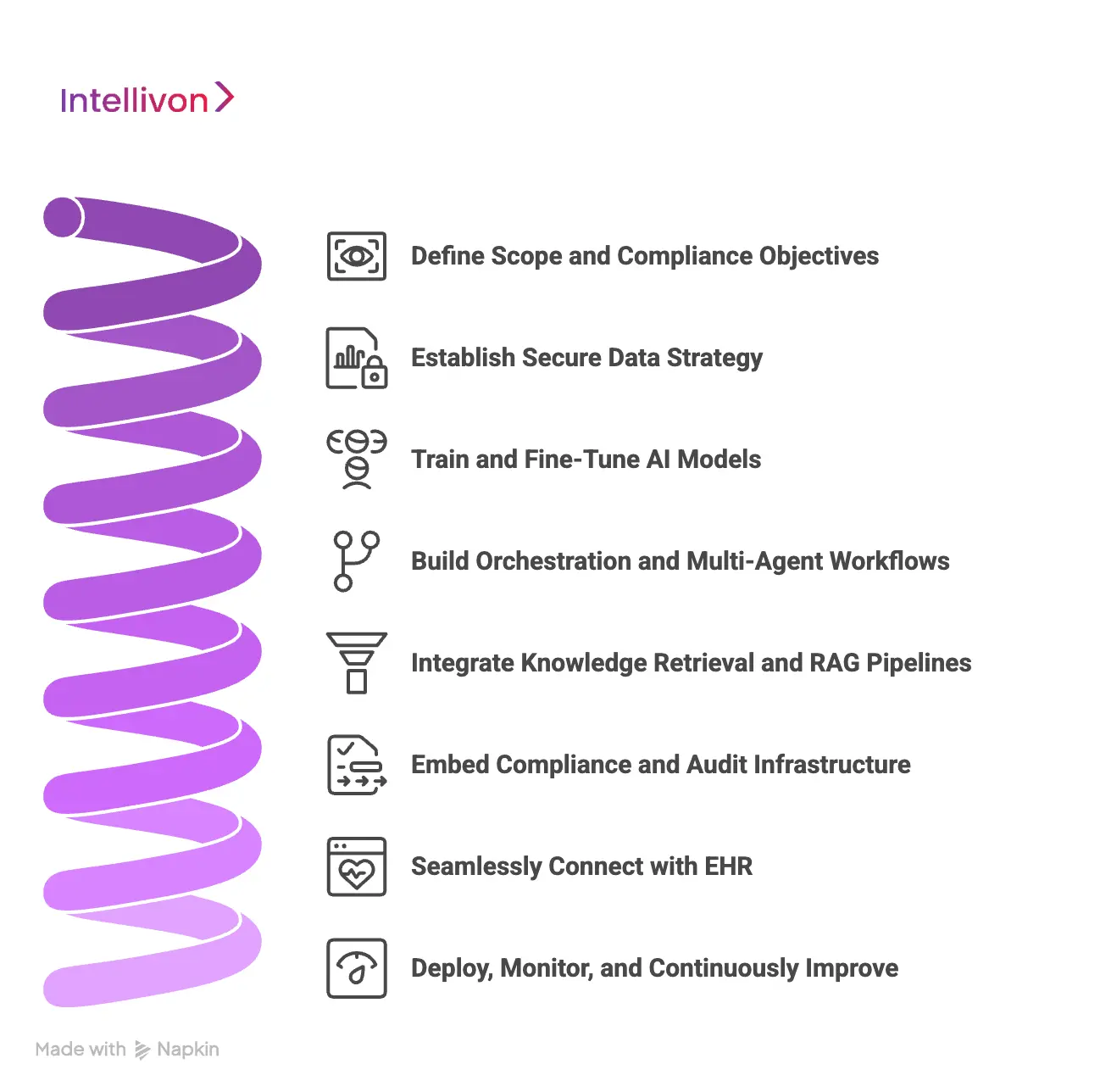
1. Define Scope and Compliance Objectives
Every successful project begins with clarity. We start by identifying the platform’s purpose, collaborating with clinical and IT leaders to define documentation use cases, workflow touchpoints, and compliance baselines.
From HIPAA and GDPR to the FDA’s SaMD and the EU AI Act, every architectural decision is aligned with regional and institutional standards. This ensures compliance is not added later, but rather it is built into the foundation.
2. Establish Secure Data Strategy
Data is the backbone of every scribe system. Our engineers design end-to-end pipelines that balance accessibility with protection, collecting and de-identifying real clinical audio, transcripts, and metadata under strict PHI governance.
Each dataset is encrypted, version-controlled, and tagged for provenance. We also use synthetic augmentation to capture edge cases, rare conditions, and diverse accents, ensuring balanced and bias-aware training datasets.
3. Train and Fine-Tune AI Models
We train each model using a hybrid approach, where we combine open-source frameworks with proprietary healthcare datasets. Our ASR engines are tuned for medical speech, overlapping dialogue, and variable acoustics, while NLP and LLM layers learn the nuance of specialty-specific terminology.
Through human reinforcement techniques such as RLHF and RLAIF, our models evolve to understand context, tone, and intent, thereby producing documentation that clinicians can trust instantly.
4. Build Orchestration and Multi-Agent Workflows
Intellivon’s architectures are modular by design. We deploy multiple AI agents, like transcription, summarization, reasoning, and compliance, each performing specialized tasks while communicating in real time through an orchestration layer.
Using lightweight protocols like gRPC and event streaming, these agents operate collaboratively and efficiently. This structure lets enterprises scale horizontally, adding new capabilities without disrupting existing workflows.
5. Integrate Knowledge Retrieval and RAG Pipelines
Accuracy defines enterprise trust. To eliminate hallucinations, we integrate Retrieval-Augmented Generation (RAG) pipelines that connect directly to institutional knowledge bases, clinical guidelines, and EHR repositories.
Our engineers build vector databases using embeddings such as BioBERT or ClinicalBERT, grounding every generated note in a verified context. The result is traceable, evidence-based documentation that aligns perfectly with your internal governance standards.
6. Embed Compliance and Audit Infrastructure
We build compliance into the system’s DNA. Automated audit logging, PHI redaction, and consent-tracking workflows are integrated from the start.
Our compliance specialists work alongside engineers to implement zero-trust access controls and versioned policy checkpoints. Each deployment includes immutable audit trails for both regulators and internal governance teams, thereby guaranteeing end-to-end traceability and accountability.
7. Seamlessly Connect with EHR
True innovation is invisible. Our integration specialists ensure the Scribe platform connects effortlessly with existing EHR systems, like Epic, Cerner, Meditech, or custom software, through FHIR and HL7 APIs.
Mobile-responsive interfaces sync across devices, supporting telehealth platforms, billing systems, and scheduling tools. This creates an uninterrupted documentation experience that fits naturally into clinical routines.
8. Deploy, Monitor, and Continuously Improve
Once live, our MLOps pipelines ensure performance remains stable and compliant. We monitor latency, accuracy, and compliance drift in real time while enabling local model improvements through federated learning.
Each client site contributes anonymized insights that strengthen the global network, allowing the system to learn continuously without retraining from scratch. The result is a self-optimizing scribe platform that evolves with every clinical interaction.
Top 5 Examples of AI Scribe Platforms
The true test of an ambient AI scribe is how it performs under enterprise-scale pressure. Leading health systems now demand proven tools that deliver measurable efficiency, real-world adoption, and compliance confidence.
The following five platforms have emerged as the benchmarks for large-scale ambient AI documentation, combining accuracy, reliability, and operational ROI.
1. Nuance DAX Copilot (Microsoft)
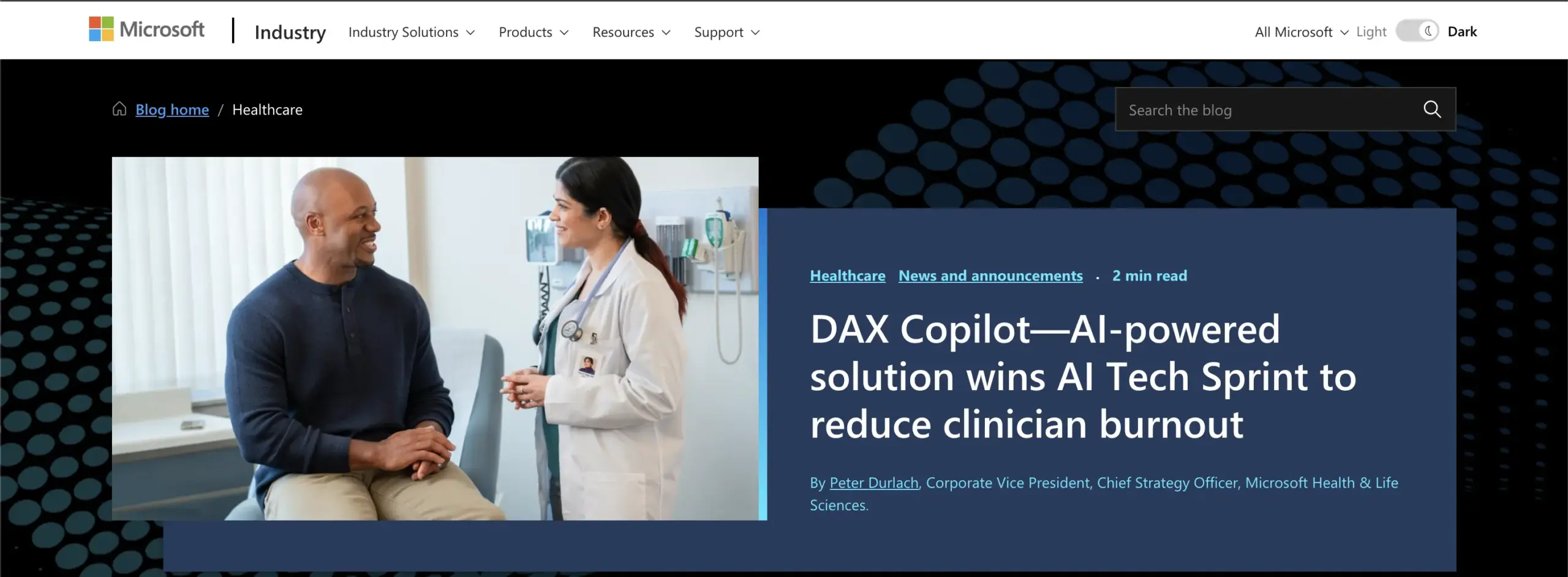
Nuance DAX Copilot remains the industry standard for large hospitals and enterprise EHR environments. Integrated directly into Epic and Cerner systems, it enables clinicians to capture complete notes hands-free while moving between desktop and mobile through Epic Haiku.
Across major health networks, DAX deployments have shown consistent results. One study reported a 20% reduction in time spent per note, a 9% rise in same-day chart closures, and a 30% drop in after-hours work. The Permanente Medical Group, one of its largest adopters, credited the platform with reclaiming more than 15,000 clinician hours in a single year.
Its strength lies in scale, which includes the ability to handle millions of encounters without lag or downtime, supported by Microsoft’s enterprise infrastructure and end-to-end compliance management.
2. Abridge
Abridge has rapidly positioned itself as the most clinician-friendly scribe platform in the market. Its growth across large integrated delivery networks (IDNs) has been driven by measurable improvements in cognitive load, satisfaction, and EHR adoption.
In independent evaluations, clinicians using Abridge reported 78% lower cognitive strain, 90% spending more time engaging with patients, and a 53% increase in professional fulfillment. The company’s partnership with Epic, highlighted at the 2025 UGM Conference, underscored its growing enterprise acceptance.
What makes Abridge stand out is its adaptive listening and summarization, where it understands tone, context, and intent. For executives, its success lies in blending human-centric design with large-scale deployment readiness.
3. Suki
Suki approaches documentation from a workflow-first perspective. Designed to reduce “pajama time”, which is the hours clinicians spend finishing charts after shifts, it focuses on speed, minimal latency, and intuitive design.
Enterprises using Suki have reported up to 72% faster documentation and nearly six fewer after-hours hours per clinician per week. It integrates with all major EHR systems, including Epic, Oracle Health, athenahealth, and Meditech, making it one of the most versatile tools available.
Beyond transcription, Suki also functions as a voice-enabled copilot, which is capable of handling tasks like coding and order entry. For organizations seeking an AI that can multitask within clinical workflows, it offers measurable operational uplift with minimal training time.
4. Augmedix
Augmedix has distinguished itself through its dual strength in technology and clinical operations. Unlike pure software solutions, its hybrid model combines real-time ambient AI with human oversight to maintain accuracy at scale, which is a balance that large hospitals find appealing.
A 2025 enterprise study involving 1,086 clinicians found that users of Augmedix were 25% less likely to reduce their working hours, saving hospitals an estimated $5.5 million annually in retained workforce capacity. Its structured documentation formats and proven interoperability make it a dependable choice for enterprise rollouts.
The platform’s greatest asset is its scalability, where it handles high patient volumes while preserving note quality and compliance consistency across departments.
5. DeepScribe
DeepScribe has built its reputation on specialty-level precision and customization. Used across outpatient networks and specialty clinics, it tailors note structures to match each provider’s documentation style.
Organizations using DeepScribe have reported dramatic reductions in charting time. Its AI models are designed to learn clinician preferences, ensuring that every draft aligns with both personal style and hospital policy.
For large healthcare enterprises, DeepScribe’s appeal lies in its adaptability, which is a lightweight deployment model that scales across departments without disrupting legacy workflows.
These five platforms have proven that measurable ROI is achievable when AI is embedded seamlessly into clinical workflows.
Conclusion
The evolution of ambient AI scribes marks a turning point in how healthcare organizations approach documentation. These platforms have moved far beyond transcription. They now reason, validate, and integrate seamlessly across clinical systems, reducing cognitive load and restoring valuable clinician time.
As healthcare systems scale, the value of automation will no longer be measured by hours saved alone but by the quality and consistency of insights it enables. Ambient AI scribes are shaping a future where technology fades into the background, and care teams can focus fully on what matters most, which is the patient.
Build Your Ambient AI Scribe Platform with Intellivon
At Intellivon, we design ambient AI scribe platforms that bring together medical-grade precision, regulatory compliance, and enterprise-level scalability.
Our solutions eliminate manual documentation, reduce after-hours charting, and safeguard revenue integrity, all while integrating effortlessly into existing EHR and telehealth ecosystems.
Why Partner With Intellivon?
- Compliance-First Architecture: Each deployment is aligned with HIPAA, GDPR, FDA SaMD, and EU AI Act frameworks.
- Healthcare-Tuned AI Models: Our ASR, NLP, and generative documentation systems are trained on clinical-grade datasets, recognizing medical speech patterns, specialty-specific terminology, and real-world encounter dynamics.
- Seamless EHR Interoperability: We integrate directly through FHIR, HL7, and SMART on FHIR protocols.
- Scalable Cloud-Native Infrastructure: Built for multi-hospital ecosystems, our architecture supports low-latency inference, high availability, and elastic scaling.
- Continuous Model Optimization: Through MLOps pipelines, our systems detect drift, retrain on verified datasets, and continuously improve model accuracy over time.
- Zero-Trust Security Framework: We implement encryption at every layer, strict identity controls, and segmentation.
- Proven Healthcare Expertise: With years of experience delivering enterprise healthcare AI systems, our experts bring validated architectures, compliance maturity, and measurable performance outcomes to every project.
Book a strategy call with Intellivon to discover how a custom-built ambient AI scribe platform can help your organization reclaim clinical time, improve documentation accuracy, and scale seamlessly across your healthcare network.
FAQs
Q1. What makes ambient AI scribes different from standard transcription tools?
Ambient scribes understand context, generate structured notes, and integrate directly into workflows instead of producing static transcripts.
Q2. How do ambient AI scribes ensure compliance and data privacy?
They run inside HIPAA- and GDPR-aligned environments with end-to-end encryption, role-based access, and automated PHI redaction.
Q3. How long does it take to build a custom enterprise-grade ambient AI scribe?
It takes 4–6 months for MVPs typically to build a custom enterprise-grade ambient AI scribe, with scalability and compliance milestones built in.
Q4. What’s the average ROI of deploying an ambient AI scribe?
Enterprises report a 40–60% reduction in documentation time and significant billing accuracy improvements within six months.
Q5. Can ambient AI scribes adapt to different medical specialties?
Yes, through fine-tuning and customizable templates, thereby enabling high accuracy across cardiology, pediatrics, orthopedics, and more.