Clinical documentation has become one of healthcare’s biggest operational drains. Studies show physicians spend 1–2 hours of after-hours charting for every workday, and 5+ hours in the EHR for every 8 hours of patient care. The problem is the lack of a workflow that was never designed for the volume and complexity of modern healthcare.
Ambient AI scribe platforms solve this by capturing doctor–patient conversations in real time and converting them into structured clinical notes that flow directly into the EHR. This eliminates manual typing, cuts down after-hours work, improves accuracy, and returns clinicians’ attention to where it belongs: the patient.
AI ambient scribes must handle noisy clinical settings, adapt to different specialties, interpret medical terminology correctly, and comply with healthcare regulations. They also need to integrate into existing EHR systems without disrupting daily operations. At Intellivon, we build ambient AI scribe platforms engineered for these realities, delivering real ROI from the start. This blog explains how much these platforms cost to develop, the factors affecting this cost, and how we build these enterprise-grade health platforms from the ground up. 
Key Takeaways of the AI Scribe Platforms Market
The global medical transcription software market is expanding quickly as hospitals shift to AI-powered documentation and integrated EHR workflows. According to Mordor Intelligence, the global medical transcription and ambient scribe market will expand from $2.9B in 2025 to $7.6–$11.36B by 2032, driven by 15–19% CAGR and rapid EHR integration.
Ambient AI scribes have become the fastest-growing category within this market, reshaping how large enterprises handle clinical notes, appointment throughput, and physician workloads.
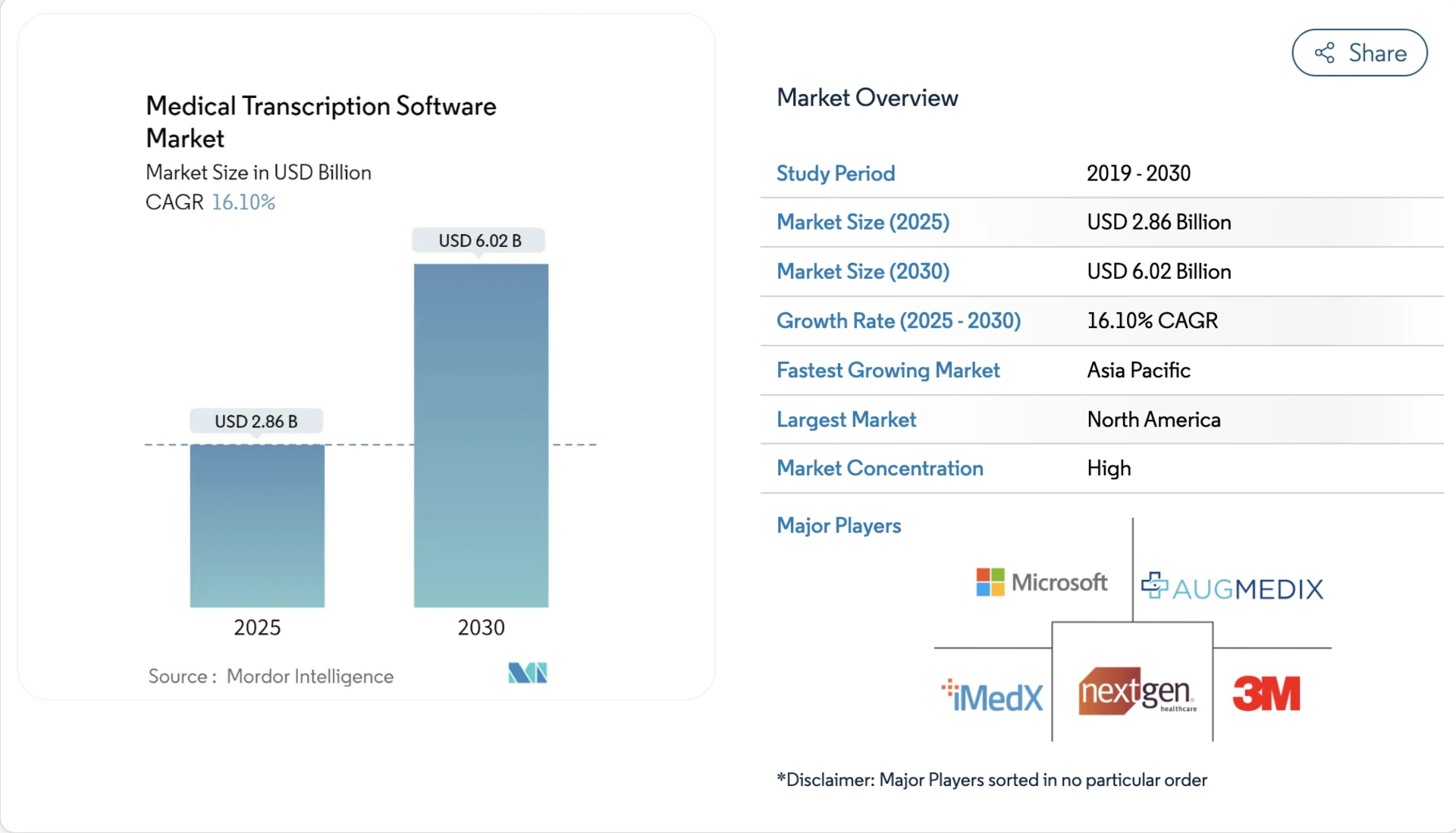
Market Insights:
- Cloud-based solutions now hold about 57% of the market share, due to easier scalability, lower operational costs, and multisite deployment benefits.
- Large hospital enterprises contribute the majority of revenue because they require real-time EHR-ready documentation and enterprise-scale workflows.
- Advanced speech recognition and NLP models are now embedded into most modern platforms, enabling real-time note generation instead of manual typing.
Ambient AI Scribe Market and Adoption
- Ambient AI scribes are now a breakout category, generating $600 million in 2025 with 2.4x year-over-year growth.
- According to Mordor Intelligence and Becker’s Hospital Review, ambient scribe platforms generated $600M+ in 2025 with 2.4x YoY adoption, and are used in 30–40% of large health systems, including Kaiser Permanente, UNC Health, and CoxHealth.
- Kaiser Permanente reports up to 70% physician usage, demonstrating successful long-term deployment across specialties and care settings.
- Leading ambient scribe vendors have raised nearly $1 billion in capital in 2025, signaling high investor confidence and sustained enterprise demand.
2025 Stats for Hospital Leadership
- Implementation of ambient scribes has reduced documentation costs by 40–60% for mid-market groups, saving up to $180,000 annually for 75-provider practices.
- Physicians using ambient scribes report a 9.3% increase in same-day appointment closure, enabling higher throughput and better patient access.
- One large healthcare system documented 2.5 million patient encounters via ambient scribes in 14 months, showing measurable reductions in burnout and turnover.
- 77% of after-hours clinical work is documentation. Ambient scribes solve this by generating EHR-ready SOAP notes in under 10 seconds.
- Enterprise deployments follow strict security models: military-grade encryption, zero-retention policies, and regional data residency.
Ambient AI scribes are now a strategic requirement for physician retention, operational cost control, and clinical quality. Early adopters are seeing ROI within 45 days, with measurable gains in documentation accuracy, patient experience, and clinician satisfaction.
What Is an Ambient AI Scribe?
An ambient scribe is an AI system that listens to clinician-patient conversations and produces structured, EHR-ready notes. It eliminates manual typing, reduces after-hours charting, and improves billing accuracy.
The result is accurate, compliant clinical notes without typing or workflow disruption. Hospitals use it to cut charting time, improve billing completeness, and strengthen audit readiness.
How Are They Different from Traditional AI Scribe Platforms?
Most hospitals have seen or tested basic AI scribe tools. They speed up dictation, but they still require extra steps. A clinician needs to start the recorder, speak in a structured format, and review dictated text before pushing it into the EHR. It saves time, but it still feels like documentation work.
Ambient scribing works differently. The system listens in real time during a natural conversation, separates voices, understands clinical language, and drafts the note without clinicians changing how they speak. There is no special script to follow and no “dictation mode” to remember. When technology adapts to clinical behavior instead of forcing behavior to adapt to technology, adoption happens faster, and the operational impact is much larger.
How They Work
The platform captures audio, converts speech to text, and detects medical entities like symptoms, diagnoses, and plans. It drafts a structured note and sends it to the EHR for review and signature. Security controls protect PHI, and usage logs support compliance. Through ambient AI scribe platforms, hospitals get accurate notes with minimal effort. Here is a step-by-step workflow:
1) Audio Capture at the Point of Care
The platform securely records consultations in rooms or telehealth sessions. It handles background noise and identifies speakers. Recording activates only within approved workflows.
2) Real-Time Speech Recognition (ASR)
A medical ASR engine converts speech to text as the visit unfolds. It handles accents, interruptions, and specialty vocabulary. Healthcare-trained models improve accuracy over time.
3) Medical NLP for Structure and Context
NLP detects symptoms, medications, allergies, and procedures. It maps terms to clinical ontologies to avoid ambiguity, and these entities feed downstream note creation and coding.
4) Draft Note Generation in Clinical Formats
The system prepares a structured SOAP or specialty-specific template. It captures clinical reasoning, orders, assessments, and plans. On the other hand, confidence scores flag items for review.
5) AI-Assisted Coding Suggestions
ICD and CPT suggestions align with the documented exam and plan. The platform shows supporting evidence for billing teams. This improves revenue integrity and reduces denials.
6) Clinician Review and Sign-Off
Physicians review, edit, and approve with minimal clicks. Inline controls make corrections fast and traceable. Every change is logged for audits.
7) EHR Integration and Interoperability
Approved notes post to the EHR via FHIR, HL7, or SMART on FHIR. The platform supports Epic, Cerner, Meditech, and other systems. It keeps routing and departmental workflows unchanged.
8) Security, Compliance, and Monitoring
Encryption, PHI redaction, and RBAC protect data at every stage. Continuous monitoring tracks drift and system health. Detailed logs support HIPAA, GDPR, and internal reviews.
In short, ambient scribing removes manual typing without changing how clinicians work. Hospitals get faster documentation, cleaner notes, and stronger revenue capture with less operational friction.
How Ambient Scribes Saves 15,700 Hours in Clinical Documentation
Ambient AI scribes are helping hospitals and clinics reclaim physician time previously consumed by documentation. They save up to 15,700 hours per physician in clinical documentation.
For instance, the Permanente Medical Group rolled out ambient AI scribes across 7,260 physicians and saved nearly 15,700 documentation hours in one year, equivalent to $2.8M–$3.45M in labour costs at $180–$220/hour.
These systems capture speech, convert it into structured notes, and reduce the after-hours burden that many doctors face each day. Here is how it is saving hours on clinical documentation in hospitals:
1. The Scale of the Documentation Burden
A national study of ambulatory physicians found that those who adopted team-based documentation support reduced their weekly documentation time by about 23.3 minutes, which is a 9.1% drop.
Yet other data suggest that physicians spend up to 5 hours in the EHR for every 8 hours of scheduled patient care and often continue working after hours. These figures show that documentation is central to physician workload.
2. After-Hours Work (“Pajama Time”)
Large‐scale data from more than 200,000 doctors across specialties reported an average of 1.2 hours spent on inbox and EHR tasks outside scheduled patient hours for every eight hours of scheduled work.
This after-hours documentation contributes significantly to burnout, longer days, and missed patient-care time.
3. Small Time Savings That Add Up
While systems still vary, the principle holds: reducing just a few minutes per encounter can scale quickly.
In a quality improvement study of 46 outpatient clinicians across 17 medical specialties, use of an ambient scribe tool was associated with note time per appointment dropping from 10.3 to 8.2 minutes, which results in a 20.4% reduction, and after-hours work time falling from 50.6 to 35.4 minutes per day, resulting in a 30% reduction.
In a full clinic day, this difference could rebound into an hour or more saved.
4. High-Use Deployments Show Strong Gains
In a large enterprise deployment at The Permanente Medical Group, ambient scribes were used for over 2.5 million patient encounters and yielded nearly 15,700 hours of physician documentation time saved, equivalent to about 1,794 eight-hour workdays.
These large gains illustrate that when workflow integration and adoption are strong, ambient-scribe systems can deliver meaningful time savings.
5. Why Workflow Fit and Specialty Matter
Not every clinician sees dramatic savings. Research emphasizes that note-composition strategy, specialty, system training, and audio/workflow quality all tie into outcome.
One commentary noted that per-encounter savings may be “seconds-to-low-single-minutes,” not always large. In other words, the architecture and context matter, which is one reason why enterprise-grade ambient-scribe builds cost six figures.
6. From Documentation Drain to Clinical Efficiency
Ambient scribes do not eliminate physician documentation, but they shift the burden away from manual typing toward dynamic capture and review.
By reclaiming time per patient, they free physicians for more visits, more patient-interaction time, and less after-hours work. Small per-visit gains, when multiplied across a packed schedule, can move the needle on capacity, physician wellness, and patient throughput.
Core Features of an Ambient Scribe Platform for Doctors
Hospitals are not looking for another transcription tool. They want something dependable across specialties, shifts, and EHR workflows in real clinical environments. An enterprise-grade ambient scribe needs a foundation that clinicians can trust every day. Here are some core features of an ambient scribe platform.
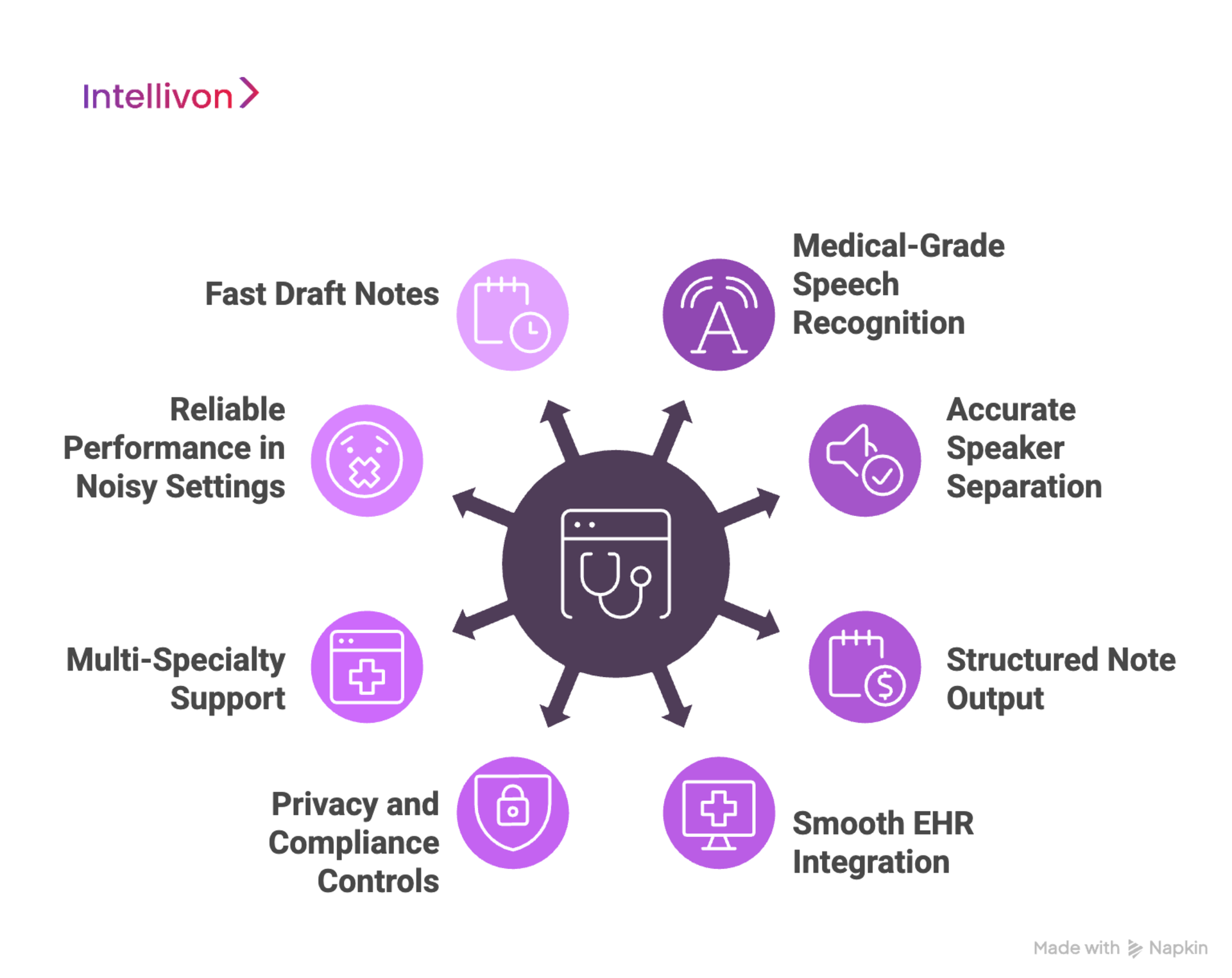
1. Medical-Grade Speech Recognition
Clinical conversations are full of complex terminology, abbreviations, brand names, and sudden topic changes. A strong ambient scribe understands this language, filters background noise, and focuses on what needs to go into the chart.
2. Accurate Speaker Separation
Charting only works when the system knows who said what. Enterprise scribes separate the clinician from the patient, recognize overlapping speech, and assign the right statements to the right voice. This reduces correction time and improves note quality.
3. Structured Note Output
Hospitals rely on consistent documentation standards. A reliable platform produces SOAP, H&P, consults, and follow-ups in the formats clinicians and coding teams already use, so notes are clear and billing-ready.
4. Smooth EHR Integration
No clinician wants to copy text between windows. Enterprise scribes send final notes directly into the correct encounter inside the EHR, using standards like FHIR and HL7. If the workflow feels natural, adoption is much easier.
5. Privacy and Compliance Controls
Enterprise healthcare runs on trust. Hospitals expect encryption, access controls, audit logging, and HIPAA alignment. Compliance teams want visibility into how data moves and who sees it.
6. Multi-Specialty Support
An outpatient pediatric visit sounds nothing like a trauma consult or a behavioral health session. Good scribes understand the language and structure of different departments, so they can scale across the enterprise instead of becoming a single-clinic tool.
7. Reliable Performance in Noisy Settings
Hospitals are busy places, teeming with alarms, hallway conversations, and telehealth echoes. The platform should capture clinical details without forcing staff to repeat themselves or change how they talk.
8. Fast Draft Notes
Clinicians expect a quick turnaround. Notes within the ambient AI scribe platform should be ready for review within minutes, helping them close encounters faster and avoid late-night charting.
Advanced Capabilities in Modern Ambient Scribes
Once the fundamentals are solid, advanced features begin to separate basic products from enterprise-ready platforms. They are:
1. Billing and Coding Intelligence
There is real value in capturing billable details the first time. Advanced scribes identify diagnoses, procedures, and key phrases that support accurate coding, reducing claim denials and coder queries.
2. Safety and Error Prevention
Ambient scribes should never invent clinical details. Modern systems include guardrails that flag uncertain information, check terminology, and keep summaries grounded in the conversation.
3. Care Plan and Summary Extraction
Some platforms turn the visit into a complete care plan, which includes diagnoses, medications, follow-up steps, all organized and ready for the chart. This saves time during handoffs and reduces missed details.
4. Multi-Language and Accent Support
Enterprises serve diverse communities. A high-quality scribe works across accents, dialects, and language switches, so every patient is documented accurately.
5. Enterprise Governance and Monitoring
IT teams need tools for user management, integration logs, retention settings, and usage analytics. Strong governance frameworks and guardrails keep the platform secure, scalable, and easy to manage long-term.
These features are the reason ambient scribes are gaining traction in large health systems. When the platform performs well across departments, protects clinical accuracy, and supports billing workflows, it becomes a core part of daily operations, and not just an add-on.
Phase-Wise Cost to Build an Ambient AI Scribe Platform
Building an ambient scribe for hospitals requires more than speech-to-text. The platform must be compliant, resilient, and ready for real clinical environments. Pricing aligns with business goals, regulatory scope, and scale. Every dollar should contribute to measurable gains in documentation accuracy, operational efficiency, and trusted data flows.
When budgets are tight, the scope can be refined without weakening compliance or safety. HIPAA and GDPR remain mandatory. FDA and EU AI Act readiness are part of long-term planning, not optional add-ons. Each build balances cost efficiency with sustainable governance and clear ROI visibility.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Compliance Alignment | Requirements, risk mapping, HIPAA controls, governance rules, KPI definition | $6,000 – $12,000 |
| Architecture & Secure Design | Multi-layer design for PHI handling, encryption, resilience, and IAM | $8,000 – $15,000 |
| Audio Capture & Edge Setup | Room microphones, telehealth connectors, consent flows, noise filtering, speaker identification | $6,000 – $12,000 |
| ASR, NLP & Note Generation | Medical ASR tuning, entity extraction, SOAP/H&P templates, confidence scoring | $12,000 – $25,000 |
| EHR Integration & Interoperability | FHIR, HL7, SMART on FHIR, routing rules for Epic, Cerner, Meditech | $10,000 – $20,000 |
| Security & Privacy Engineering | RBAC, MFA, tokenization, redaction, encryption keys, continuous monitoring | $8,000 – $15,000 |
| Platform UX & Interfaces | Clinician review UI, coding view, audit console, admin controls | $10,000 – $20,000 |
| Testing & Validation | HIPAA checks, penetration tests, safety validation, model QA | $6,000 – $10,000 |
| Pilot & Training | Limited rollout, feedback loops, template tuning, user playbooks | $6,000 – $10,000 |
| Deployment & Scaling | Cloud deployment, high availability, observability, and elastic scaling | $6,000 – $12,000 |
Total Initial Investment Range: $50,000 – $150,000
Ongoing Maintenance & Optimization (Annual): 15–20% of initial build
ROI Estimate: Hospitals typically recover development costs within 6–12 months. Savings come from reduced after-hours charting, increased appointment capacity, fewer denials, and faster billing cycles. Enterprise deployments report a 40–60% drop in documentation time and an annual savings of $180,000+ for 75-provider groups.
Hidden Costs Enterprises Should Plan For
Even well-scoped projects encounter operational overhead. Enterprises should anticipate:
- Integration depth: Legacy EHRs sometimes require middleware, mapping, or custom APIs.
- Compliance documentation: Audits, risk assessments, and security reports add recurring workload.
- Data governance: Normalizing mixed formats across departments takes steady effort.
- Cloud spend: Real-time inference and storage need cost controls to protect ROI.
- Change management: Training clinicians, coders, and support teams carries transition costs.
- Model drift: Periodic retraining keeps accuracy and safety intact as medical language evolves.
Best Practices to Prevent Budget Overruns
A well-planned deployment can stay within the $100K–$200K band. Hospitals that control long-term costs tend to:
- Start with a focused department, prove value, and scale after adoption.
- Build compliance into the architecture instead of treating it as a patch.
- Use modular AI pipelines that can power multiple clinical services.
- Optimize cloud usage with the right mix of batch and real-time workloads.
- Maintain observability, including uptime, latency, and integration health, so they are visible at all times.
- Recalibrate models and update templates as clinical practices change.
Request a tailored proposal from Intellivon’s healthcare AI experts. We align and build roadmaps with budget, compliance obligations, and scalability goals, so systems reach production faster and deliver sustainable ROI.
Tech Stack That Influences the Cost of Making Ambient Scribes
Building an ambient scribe looks simple on the surface, but in reality, the tech stack behind enterprise-grade accuracy is layered and specialized.
Each component, from audio pipelines, medical ASR, NLP models, security controls, to EHR interoperability, adds engineering depth and cost.
Hospitals also operate in high-risk environments. For this, the system must run securely, scale for thousands of encounters, and handle sensitive PHI without performance failures. That means more than “just an AI model.” It requires cloud orchestration, encryption, monitoring, dashboards, and a strong integration layer that IT teams can trust.
What Drives Cost in the Tech Stack
- Accuracy and speed: Models must work in real clinical settings, not labs.
- Security: PHI handling requires encryption, identity controls, and audit logs.
- Interoperability: EHR integration is often the most expensive part of the build.
- Scalability: The system needs to handle peak loads without slowing clinicians.
- Compliance: Guardrails, governance, and audit readiness are non-negotiable.
Below is a realistic breakdown showing how each layer contributes to total development spend.
Tech Components and Cost Impact
| Tech Component | Description | Cost Influence |
| Cloud Infrastructure | Compute, storage, load balancing, GPU inference for ASR/NLP workloads | $8,000 – $20,000 depending on volume and scaling strategy |
| Medical Speech Recognition (ASR) | Domain-tuned speech models that understand clinical language, accents, and background noise | $15,000 – $30,000 for training, customization, and optimization |
| Clinical NLP Pipelines | Entity extraction, symptom mapping, negation detection, and structured note generation | $10,000 – $25,000 based on specialty depth and note formats |
| Real-Time Audio Processing | Noise filtering, speaker separation, waveform processing, and telehealth connectors | $6,000 – $12,000, depending on edge devices and signal quality |
| EHR Integration Layer | FHIR, HL7, SMART on FHIR, encounter routing, and template mapping | $10,000 – $20,00,0 depending on the number of EHR systems |
| Security Stack | Encryption, access controls, MFA, tokenization, redaction, logging | $8,000 – $15,000 to meet HIPAA/GDPR requirements |
| Monitoring & Observability | Dashboards for uptime, latency, model health, and integration status | $4,000 – $8,000, depending on cloud tools and analytics depth |
| Admin & Reviewer Interfaces | UI for clinicians, coding teams, and compliance admins | $10,000 – $20,000, depending on custom workflows |
Why These Costs Matter
Hospitals buy outcomes and do not rely solely on features. A cheaper tech stack may work for small clinics, but it fails in enterprise settings where uptime, accuracy, and auditability matter. When a note enters the EHR, it becomes part of a legal and financial record. Every line of code should protect that reality.
Ongoing Operational Costs After Ambient Scribe Deployment
Once a scribe platform is live, hospitals need to keep it accurate, secure, and responsive. Operational spending covers cloud usage, model quality, EHR updates, and support for new departments joining the system. These costs are predictable and can be planned into annual budgets.
Annual Cost Breakdown
| Cost Category | What It Covers | Typical Annual Spend |
| Cloud Compute & Storage | Real-time audio processing, ASR inference, NLP pipelines, and encounter data storage | $8,000–$20,000 |
| Model Retraining & Accuracy Improvements | Updating language models for new terms, procedures, and templates; preventing model drift | $6,000–$15,000 |
| EHR and API Updates | Patching integrations when Epic, Cerner, Meditech, or third-party systems change standards | $3,000–$10,000 |
| Security & DevSecOps Monitoring | Audits, intrusion detection, encryption key rotation, PHI governance | $5,000–$12,000 |
| Support, Training & Change Management | Onboarding departments, refresher training, documentation, and user support | $3,000–$10,000 |
| Uptime & Performance Monitoring | Observability tools, telemetry dashboards, incident response, and failover systems | $2,000–$6,000 |
Most enterprises spend $15,000–$30,000 per year maintaining an ambient scribe platform. Larger health systems invest more, but they recover that cost quickly when documentation accuracy improves, after-hours charting drops, and appointment capacity increases.
Factors Affecting the Total Cost of Developing an Ambient Scribe Platform
No two hospital environments look the same. Documentation workflows, EHR setups, and specialty requirements vary widely, which is why ambient scribe pricing is not one-size-fits-all. The final cost depends on how deeply the platform integrates into clinical operations and what level of automation the organization expects.
1. Clinical Complexity
A simple primary care workflow is easier to automate than multi-specialty coverage. Orthopedics, cardiology, pediatrics, and behavioral health all use different terminology and note formats. Supporting multiple departments increases tuning, testing, and model training requirements.
2. Real-Time vs. Post-Visit Processing
Real-time draft notes are more expensive to build because they require higher compute resources, streaming pipelines, and low-latency architecture. Post-visit transcription is cheaper, but it delivers less operational benefit.
3. Integration Depth
Some hospitals use Epic or Cerner with standard APIs. Others have custom modules, legacy add-ons, or middleware that require special routing. The deeper the integration, the more engineering effort is needed to make notes land in the right encounter and timestamp.
4. Compliance and Regulatory Scope
Systems handling PHI need encryption, access controls, redaction, audit logs, and risk assessments. Hospitals preparing for FDA or EU AI Act readiness require additional safety checks, model documentation, and traceability layers, which increase the cost.
5. Audio Environment
Quiet outpatient clinics are easy. Trauma rooms, emergency departments, and telehealth calls introduce overlapping voices, alarms, and background noise. Handling this reliably adds cost to the audio and ASR pipelines.
6. Scalability and High Availability
If the platform will serve thousands of clinicians, it must support load balancing, fault tolerance, and disaster recovery. These infrastructure requirements increase cloud spend and engineering work.
7. Specialty Tuning and Templates
Each specialty introduces new language, documentation styles, and billing rules. More templates mean more NLP work and more validation during pilots.
Hospitals that understand these cost drivers can plan smarter budgets, set clear expectations, and avoid surprises later. The right build focuses on accuracy, speed, compliance, and smooth workflows, and not just transcription.
Revenue Models for Ambient AI Scribe Platforms
Ambient scribe platforms create a repeatable revenue stream for vendors and digital health companies. The right pricing model depends on clinical volume, deployment size, and how tightly the platform integrates with the EHR.
Below are the most common revenue models, how they work, what they cost in real markets, and examples of enterprise adoption.
1. Subscription Per Clinician (Per Seat)
This is the most widely used model. Each active clinician pays a monthly subscription fee to use the platform. It works because usage is predictable and billing scales as more departments adopt the tool.
Typical Pricing:
- $100–$350 per clinician per month for basic transcription + note generation.
- $400–$600 per clinician per month for enterprise-grade ambient scribe capabilities.
Market Example: Nuance DAX Copilot, used across large systems like Kaiser Permanente and UNC Health, is often cited in this price range.
Kaiser reported nearly 15,700 hours of documentation time saved across 7,260 physicians, which is a labor savings worth $2.8M–$3.45M annually. Hospitals pay the subscription because the return is measurable.
2. Encounter-Based Pricing
Some vendors price based on volume, which includes the number of documented visits, minutes of audio, or hours of transcription processed. This model appeals to urgent care chains, telehealth providers, and practices with fluctuating scheduling patterns.
Typical Pricing:
- $0.50–$2.00 per documented encounter for post-visit transcription.
- $2.50–$8.00 per encounter for full ambient scribe automation with AI-generated notes.
Market Example: Abridge, which has raised over $200M in funding, uses usage-based pricing within several health systems. Telehealth networks prefer this model because they scale up and down month-to-month without fixed seat fees.
3. Tiered Enterprise Licensing
Large hospital groups negotiate bundled contracts that cover thousands of clinicians and multiple sites. This structure locks in long-term value and simplifies budgeting.
Typical Pricing:
- $150,000–$1.2M per year, depending on the number of seats, sites, and EHR integrations.
- Multi-year contracts often include discounted per-clinician rates.
Market Example: When DAX Copilot rolled out inside UNC Health and CoxHealth, these platforms were deployed as enterprise solutions rather than small pilots. Hospitals paid for scalability, uptime, clinical accuracy, and support for specialty workflows.
4. White-Labeled EHR Integrations
Some platforms partner directly with EHR vendors and sell ambient scribing as an integrated add-on. Hospitals prefer this because workflows stay within Epic, Cerner, Meditech, or athenahealth, with no extra screens or toggling.
Typical Pricing:
- $50–$75 per provider per month as an EHR add-on.
- Premium versions with care plans and auto-coded documentation run $100–$200 per month.
Market Example: Several mid-market EHRs bundle clinical dictation and AI note automation into their platforms and charge hospitals a monthly fee. In these settings, the EHR vendor collects revenue and shares a portion with the AI provider.
5. Hybrid Licensing
Some enterprises negotiate a base platform license with additional usage-based billing. This keeps costs predictable while still offering flexibility.
Typical Pricing Structure:
- Flat $5,000–$25,000 annual platform license.
- $1–$3 per encounter on top.
Hybrid models are gaining traction among digital health companies and hospital innovation teams because they can start small and scale as adoption grows.
When a platform can return 500–1,000 physician hours per year, the subscription cost becomes small compared to the regained clinical capacity. For example, if a physician’s time is valued at $200/hour, reclaiming 100 hours per year equals $20,000 in value. Many clinicians save far more than that.
How We Develop Ambient AI Scribe Platforms for Doctors
Hospitals need technology that fits into their daily workflow, and not tools that add extra clicks or change how clinicians document care. At Intellivon, we build ambient scribe platforms that understand clinical language, maintain regulatory trust, and integrate directly into existing EHR ecosystems. Our development process is structured to deliver accuracy, safety, and measurable operational impact.

1. Analyze Existing Workflows
Every hospital has its own documentation style. Some clinicians dictate after the visit, others type in real time, and specialty groups often use unique templates.
We begin by observing how notes are created today, which includes metrics like how long they take, where errors appear, and what slows clinicians down. This ensures the platform automates the right parts of the workflow while preserving clinical autonomy.
2. Build Secure Architecture
Security cannot be added later. The system is engineered for protected PHI flows, encryption at every checkpoint, strict identity access, and full audit trails.
We map data residency rules, retention schedules, and compliance controls during architecture, and not after deployment. This protects legal defensibility and makes IT teams confident from the first build.
3. Clinical ASR Tuning
General-purpose ASR struggles in hospitals where alarms beep, multiple speakers talk at once, and terms change mid-sentence. We train speech models on medical vocabulary, drug names, acronyms, and accents found across specialties.
The platform learns to ignore non-clinical noise and capture medically relevant information without forcing clinicians to speak unnaturally.
4. Built NLP Pipelines
Ambient scribes are only valuable when they understand context, not just words. Our NLP pipelines detect diagnoses, medications, symptoms, vital mentions, and follow-up instructions.
They also identify negations, for example, “no chest pain” should never be recorded as a symptom. This creates structured clinical data instead of raw transcription.
5. Template-Aware Note Generation
Clinicians write SOAP notes, HPI, H&P, consults, discharge summaries, and specialty-specific formats. We design the platform to understand these structures and produce clear, billing-ready notes.
Orthopedics, pediatrics, cardiology, and behavioral health all require different documentation styles, so the model adapts instead of forcing a one-size-fits-all output.
6. FHIR/HL7 Interoperability
A true ambient scribe does not live outside the EHR. We connect through FHIR, HL7, or SMART on FHIR to route documents to the correct patient, encounter, and timestamp. Notes appear where clinicians expect them, ready for review and signature. This avoids copy-paste workflows and reduces coding friction.
7. Review and Editing Dashboards
Clinicians need transparency, not black-box automation. We build dashboards where providers can quickly review drafts, correct details, and sign notes. Coding teams get their own view for billing elements and missing fields.
At the same time, administrators can see usage logs, system performance, and audit trails. This keeps the platform safe, traceable, and easy to manage.
8. Testing, Sandbox, and Silent Mode Rollout
Before a single note goes live, the platform runs in silent mode. It listens, drafts notes, and measures accuracy without changing clinician behavior.
Departments can compare system outputs against real notes, giving confidence before full production rollout. Training, onboarding, and feedback loops ensure adoption is smooth.
9. Continuous Learning and Model Improvement
Medicine evolves every day. New treatments, drug names, diagnostic patterns, and abbreviations constantly appear in real-world practice.
We keep models calibrated with ongoing optimization, specialty tuning, and edge-case learning. This prevents model drift and keeps documentation accuracy high year after year.
Conclusion
Ambient AI scribes are reshaping clinical documentation by removing manual typing, reducing after-hours charting, and supporting billing accuracy. Hospitals that once struggled with overloaded clinicians and shrinking appointment capacity are now seeing faster note turnaround, clearer records, and higher-quality patient interactions. As adoption grows, the technology is proving that automation can strengthen, and not replace, clinical judgment.
The cost to build a fully compliant, EHR-integrated ambient scribe is significant, but the return shows up quickly in reclaimed physician time and operational efficiency. Health systems ready to modernize documentation are treating ambient scribes as a long-term investment in workflow performance, clinical quality, and financial resilience.
Build an Ambient AI Scribe Platform With Intellivon
At Intellivon, we build ambient AI scribe platforms that combine medical-grade accuracy, clinical compliance, and enterprise-scale reliability. Each deployment is engineered for hospitals that require security, uptime, and measurable ROI from day one.
Why Partner With Intellivon?
- Compliance-First Architecture: Every platform aligns with HIPAA, GDPR, FDA SaMD, and EU AI Act frameworks. PHI encryption, immutable audit logs, and access control keep documentation legally defensible across regions.
- Healthcare-Tuned AI Models: Our ASR, NLP, and note-generation engines are trained on clinical speech, specialty terminology, and real-world usage. Notes are accurate, structured, and ready for provider approval in seconds.
- Seamless EHR Interoperability: We integrate through FHIR, HL7, and SMART on FHIR. Notes post directly to the correct patient, encounter, and timestamp, and no manual data entry.
- Scalable Cloud-Native Infrastructure: Low-latency inference, high availability, elastic scaling, monitoring, and automated failover support enterprise workloads without slowdown.
- Continuous Model Optimization: MLOps pipelines detect drift, retrain models, and improve accuracy over time as the system learns from real clinical workflows.
- Zero-Trust Security: End-to-end encryption, identity management, segmentation, and threat detection safeguard PHI without interrupting care delivery.
- Human-Centered Product Design: Clinician review screens, coder dashboards, and admin controls make adoption effortless, with no workflow disruption and no steep learning curve.
Book a strategy call with Intellivon to explore how a custom ambient scribe platform can reduce documentation time, strengthen billing accuracy, and scale across your hospital network.
FAQs
Q1. How much does it cost to build an ambient AI scribe platform for hospitals?
A1. A production-grade ambient scribe platform costs $100,000–$200,000. This includes medical ASR tuning, NLP pipelines, EHR integration, HIPAA security, and cloud infrastructure. Costs scale with clinical complexity, specialty support, and real-time performance requirements.
Q2. What features make an ambient scribe “enterprise-grade”?
A2. Hospitals look for medical-tuned speech recognition, structured note generation, FHIR/HL7 interoperability, audit trails, encryption, uptime monitoring, and accuracy in noisy environments. Platforms that support billing and coding intelligence typically deliver higher ROI.
Q3. Can ambient scribes integrate with Epic, Cerner, or Meditech?
A3. Yes. Enterprise platforms connect through FHIR, HL7, and SMART on FHIR. Notes attach directly to the right patient, encounter, and timestamp, so clinicians do not need to copy or re-enter text.
Q4. How long does it take to deploy an ambient AI scribe?
A4. A typical rollout takes 12–20 weeks, including workflow analysis, ASR/NLP tuning, EHR integration, testing, silent-mode validation, and phased go-live across departments.
Q5. What is the ROI of using ambient AI scribes in hospitals?
A5. ROI appears through reduced after-hours charting, faster note turnaround, lower burnout, and increased appointment capacity. Many deployments report 30–50% time savings per note and significant improvement in billing accuracy due to structured documentation.