Hospitals deal with documentation burdens that never seem to end. Clinicians spend hours typing notes, correcting charts, and filling in missing details after their shifts, which slows down care delivery and causes billing gaps. Ambient AI scribe platforms solve this by capturing natural doctor–patient conversations and turning them into structured clinical notes inside the EHR. At the same time, they remove manual data entry, reduce after-hours charting, and improve documentation accuracy without changing how clinicians interact with patients.
At Intellivon, we build enterprise-grade ambient AI scribe platforms for hospital environments, like noisy rooms, telehealth sessions, specialty-specific terminology, and strict compliance requirements. Our systems understand clinical language, maintain accuracy at scale, and fit smoothly into existing EHR workflows. In this blog, we will cover how we develop these healthcare platforms from the ground up and make them ready for enterprise-level deployment.
Key Takeaways of the AI Scribe Market
This growth reflects higher demand for accurate clinical documentation, wider telemedicine adoption, and increasing reliance on AI-powered speech recognition and NLP to improve speed and accuracy. Hospitals are shifting from manual or outsourced transcription to automated scribing because the economics and operational outcomes are stronger.
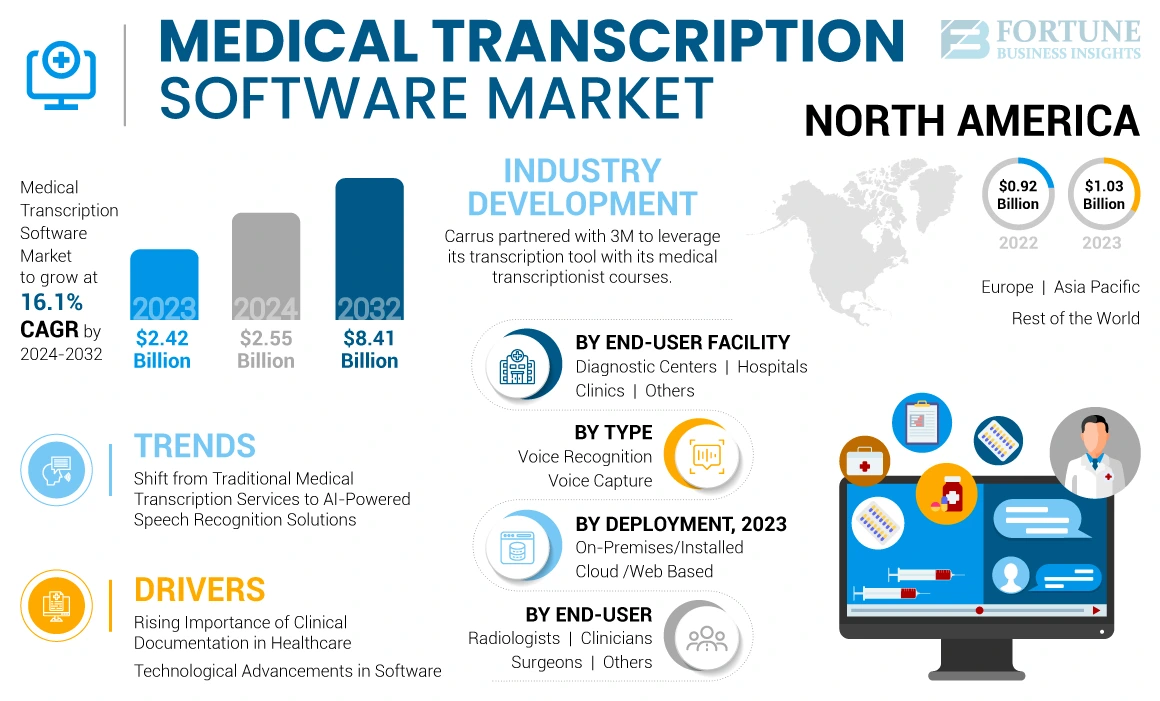
Market Insights:
- The ambient AI scribe platform market was valued at approximately $600 million in 2025, with adoption expected to reach 40% of large hospital systems by 2028.
- Ambient AI scribes save physicians up to two hours per day and reduce documentation errors by 30%.
- Emergency medicine, psychiatry, and outpatient care show the highest adoption due to burnout reduction and workflow efficiency.
- ROI payback periods fall between 18 and 24 months, driven by faster chart closures, higher coding accuracy, and a 25% gain in patient throughput.
- More than 80% of clinicians report better patient interactions and improved satisfaction due to reduced “pajama time.”
- Cloud deployments now account for over 50% of implementations, enabling faster onboarding and smooth EHR integration with Epic and Cerner.
- Fewer than 10 vendors hold more than 75% market share, and many are expanding into real-time clinical decision support.
- Compliance remains a top adoption driver, with platforms adding audit trails and encryption to meet strict healthcare regulations.
Ambient AI scribing has shifted from early adoption to enterprise scaling. Hospitals now treat it as core infrastructure for efficiency, patient experience, and financial performance.
What Is an Ambient AI Scribe Platform?
An ambient AI scribe platform listens to clinical conversations and turns them into structured notes. It captures physician–patient dialogue, understands medical terminology, and drafts documentation that syncs with the EHR.
The result is accurate, compliant clinical notes without typing or workflow disruption. Hospitals use it to cut charting time, improve billing completeness, and strengthen audit readiness.
How Are They Different from Traditional AI Scribe Platforms?
Most hospitals have seen or tested basic AI scribe tools. They speed up dictation, but they still require extra steps. A clinician needs to start the recorder, speak in a structured format, and review dictated text before pushing it into the EHR. It saves time, but it still feels like documentation work.
Ambient scribing works differently. The system listens in real time during a natural conversation, separates voices, understands clinical language, and drafts the note without clinicians changing how they speak. There is no special script to follow and no “dictation mode” to remember. When technology adapts to clinical behavior instead of forcing behavior to adapt to technology, adoption happens faster, and the operational impact is much larger.
How They Work
These platforms follow a clear workflow from recording the consultation to generating final notes. Each layer plays a specific role, so hospitals get accurate documentation without extra effort from clinicians.
1) Audio Capture at the Point of Care
The platform securely records consultations in rooms or telehealth sessions. It handles background noise and identifies speakers. Recording activates only within approved workflows.
2) Real-Time Speech Recognition (ASR)
A medical ASR engine converts speech to text as the visit unfolds. It handles accents, interruptions, and specialty vocabulary. Healthcare-trained models improve accuracy over time.
3) Medical NLP for Structure and Context
NLP detects symptoms, medications, allergies, and procedures. It maps terms to clinical ontologies to avoid ambiguity, and these entities feed downstream note creation and coding.
4) Draft Note Generation in Clinical Formats
The system prepares a structured SOAP or specialty-specific template. It captures clinical reasoning, orders, assessments, and plans. On the other hand, confidence scores flag items for review.
5) AI-Assisted Coding Suggestions
ICD and CPT suggestions align with the documented exam and plan. The platform shows supporting evidence for billing teams. This improves revenue integrity and reduces denials.
6) Clinician Review and Sign-Off
Physicians review, edit, and approve with minimal clicks. Inline controls make corrections fast and traceable. Every change is logged for audits.
7) EHR Integration and Interoperability
Approved notes post to the EHR via FHIR, HL7, or SMART on FHIR. The platform supports Epic, Cerner, Meditech, and other systems. It keeps routing and departmental workflows unchanged.
8) Security, Compliance, and Monitoring
Encryption, PHI redaction, and RBAC protect data at every stage. Continuous monitoring tracks drift and system health. Detailed logs support HIPAA, GDPR, and internal reviews.
In short, ambient scribing removes manual typing without changing how clinicians work. Hospitals get faster documentation, cleaner notes, and stronger revenue capture with less operational friction.
How AI Powers Ambient Scribe Platforms
Ambient scribe platforms are more than transcription tools. They combine multiple layers of artificial intelligence that work together to understand conversations, extract clinical meaning, and generate structured notes that fit hospital documentation standards.
When each layer performs well, the platform feels invisible inside the clinical workflow. Physicians talk, the system listens, and the EHR receives a complete record without manual typing.
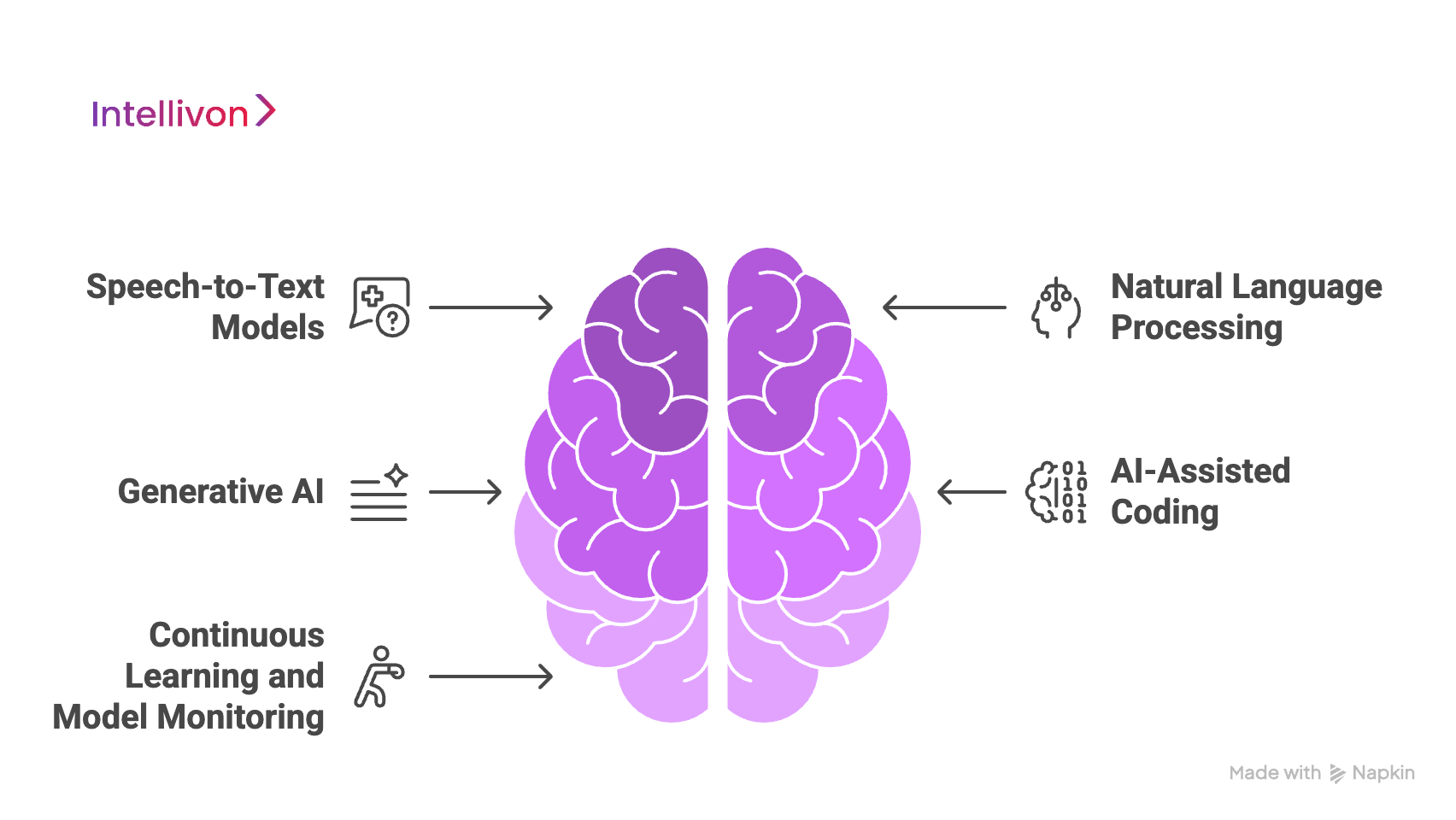
1. Speech-to-Text Models
The process starts with Automatic Speech Recognition, but not the consumer-grade engines used in call centers or mobile apps. Ambient scribe platforms use healthcare-trained ASR models that recognize medical terminology, drug names, symptoms, and complex sentence structures.
These models reduce errors by learning from clinical data, not general speech. As a result, they maintain accuracy even with accents, interruptions, or background noise.
2. Natural Language Processing
Once speech becomes text, NLP models process the transcript and identify clinical meaning. The system detects diagnoses, treatments, allergies, vitals, review-of-systems entries, and assessment details.
Instead of treating language as plain text, it maps each element to the correct medical concept. This is what turns a spoken conversation into structured data that billing and compliance teams can trust.
3. Generative AI
A generative model assembles the documentation into SOAP or specialty-specific templates. It keeps clinical reasoning intact and organizes findings into the right sections.
The goal is to create a usable medical note that reads like something the physician would write themselves. This step eliminates the bulk of post-visit typing.
4. AI-Assisted Coding
Some platforms use machine learning to suggest ICD and CPT codes based on the documented findings. Instead of guessing or relying on memory, clinicians see suggested codes with supporting evidence from the encounter.
This improves billing accuracy and reduces the risk of denials. The physician then reviews the draft, makes edits, and signs off. Every change is tracked for audit purposes.
5. Continuous Learning and Model Monitoring
Hospitals operate in constantly changing clinical environments. Ambient systems monitor model performance, track drift, and retrain when accuracy drops.
Over time, the platform becomes more familiar with accents, specialties, and documentation patterns unique to each organization. This learning cycle is what keeps long-term accuracy stable.
AI makes the scribing process effortless by handling language, structure, and medical reasoning in the background. Instead of typing, clinicians speak naturally. Instead of missing details, documentation stays complete. And instead of losing hours to charting, hospitals regain time that can be spent on care.
Why Ambient AI Scribe Platforms Have Become a Hospital Priority
Hospitals are re-evaluating how clinical data moves through their systems. Manual documentation slows care delivery, increases billing risk, and pushes clinicians into after-hours charting.
Ambient AI scribing changes that by capturing conversations in real time and converting them into structured notes that flow back into the EHR. The shift is not about convenience. It is about fixing the most expensive inefficiencies in modern healthcare.
1. Clinical Documentation Consumes Physician Capacity
JAMA reports that physicians spend 35%–55% of their working hours documenting care instead of treating patients. The Annals of Internal Medicine found nearly two hours of charting for every hour of patient interaction.
For mid-sized hospitals, this leads to more than a million dollars in annual productivity loss. Ambient scribing removes the typing burden and keeps clinicians focused on clinical tasks.
2. Documentation Gaps Trigger Revenue Loss
Incomplete notes directly impact reimbursement. HIMSS estimates hospitals lose $25–$40 per patient visit in missed billable details.
The AMA confirms that 37% of claim denials happen because documentation is missing or inaccurate. When details are captured automatically during the visit, hospitals protect revenue already earned.
3. Burnout and Turnover Create Hidden Costs
The AMA reports that 63% of physicians cite documentation as a driver of burnout.
Replacing a physician can cost $500,000–$1M, according to Mayo Clinic Proceedings. Ambient scribe platforms reduce after-hours charting and support workforce retention.
4. Accuracy Improves With Medical-Tuned AI
Generic speech engines struggle with accents and terminology. Stanford research shows medical-tuned ASR improves accuracy by 18%–22%.
With physician review, Nature Digital Medicine reports accuracy above 95% for structured notes.
Hospitals adopting ambient scribing recover time, protect reimbursements, and strengthen compliance. It is becoming a core layer of digital care delivery, not an optional upgrade.
Architecture of an Ambient AI Scribe Platform
A production-ready ambient scribe platform has to do more than turn speech into notes. It must run in noisy clinical settings, protect PHI, integrate with EHRs, scale across departments, and remain accurate over time. To achieve that, the architecture operates in several coordinated layers, each responsible for a specific part of the workflow.
1. Audio Capture and Edge Layer
The system begins by capturing live conversations through mobile apps, telehealth integrations, or clinical room microphones. Edge components handle noise filtering, speaker separation, and consent controls before data leaves the device.
Hospitals use this layer to avoid unapproved recordings and ensure compliance from the first interaction.
2. AI Processing Pipeline
Once audio is captured, the AI pipeline takes over. Medical-grade ASR models convert speech into text while maintaining clinical vocabulary and abbreviations.
NLP and entity extraction models identify diagnoses, medications, orders, and assessment details. Some architectures add a generative model to assemble SOAP notes or specialty templates, reducing manual edits.
3. Clinical Validation and Feedback Layer
Human-in-the-loop validation happens here. Physicians review drafts, make corrections, and approve the final note.
Every edit becomes training feedback, so accuracy improves over time. This layer ensures AI supports clinical decision-making rather than replacing oversight.
4. Model Management and Drift Monitoring
Accuracy changes as accents, departments, and documentation patterns shift. Model monitoring tracks confidence scores, error rates, and edge-case failures.
When drift occurs, the platform re-trains or updates models without interrupting hospital workflows. This is what keeps long-term performance stable.
5. Data Governance and Compliance Layer
Security sits at the heart of deployment. PHI is encrypted in transit and at rest. Tokenization and redaction limit exposure.
RBAC ensures only authorized users see sensitive data. Immutable audit logs track every user action and every AI-generated change to maintain regulatory defensibility.
6. Integration and Interoperability Layer
The final documentation goes into the EHR through FHIR, HL7, or SMART on FHIR connectors. The platform adapts to Epic, Cerner, Meditech, athenahealth, and other systems without altering existing clinical workflows.
Routing rules place notes in the correct chart, visit type, and timestamp.
7. Cloud, On-Prem, or Hybrid Deployment
Hospitals choose where models run, and cloud deployments offer faster scaling and lower infrastructure overhead.
On-prem or VPC cloud deployments keep all PHI inside the hospital network. Hybrid models process speech at the edge while NLP and note generation take place in the cloud.
8. Observability and DevOps Layer
To stay reliable, the platform needs real-time monitoring of latency, uptime, and integration health. Automated alerts flag failed uploads, EHR sync errors, or API slowdowns. This DevOps layer gives IT teams the transparency they expect from enterprise systems.
A complete architecture allows hospitals to deploy ambient scribing with confidence. It is secure, compliant, upgradeable, and capable of supporting thousands of clinical encounters each day without slowing down care delivery.
How To Ensure Compliance in Ambient AI Scribe Platforms
Any platform that handles clinical conversations must meet strict compliance expectations. Hospitals cannot afford uncertainty around privacy, auditability, or regulatory alignment.
A compliant ambient scribe platform protects PHI from the moment audio is captured to the moment the final note lands inside the EHR. The strongest deployments treat compliance as an architectural requirement, not a feature added later.
1. PHI Protection and Data Minimization
Security begins with how the system captures data. Audio is encrypted in transit and at rest, and hospitals control when recording starts and stops.
Modern ambient scribe platforms also reduce exposure by redacting identifiers and storing only what is needed for documentation. This limits risk and keeps sensitive data from moving through unnecessary systems.
2. HIPAA and GDPR Alignment
Hospitals need proof that every interaction is traceable. Role-based access restricts who can view or edit documentation. Immutable audit logs capture every action, such as who recorded the encounter, who edited the draft, and when the note was entered into the EHR.
If a patient requests data removal or export, the system supports it. This gives compliance teams a clear chain of custody.
3. Secure EHR Integrations
Most breaches do not happen inside the AI model. Instead, they happen during data movement. A compliant platform uses secure FHIR, HL7, or SMART on FHIR connections with identity validation before any note reaches the EHR.
Failed syncs, unauthorized requests, and connection interruptions are logged in real time so IT teams know exactly what happened.
4. FDA and EU AI Act Readiness
Some regions treat AI-generated medical documentation like a regulated medical system. To prepare for this, the platform stores versioned model outputs, confidence scores, and metadata that show how a note was generated.
Human review remains part of the workflow, making audit defense stronger and reducing clinical risk.
5. Auditability and Chain of Custody
From audio capture to sign-off, every stage needs a paper trail. Clinician edits, AI suggestions, and coding recommendations are version-controlled. Final notes carry digital signatures.
If a payer or regulator asks for validation, hospitals can produce a complete history in minutes rather than days.
6. Secure Deployment Models
Hospitals vary in how they handle PHI. Some prefer full cloud for fast scaling, others require on-prem or VPC. A compliant platform supports all three and isolates tenant data in multi-hospital deployments.
Continuous penetration testing, vulnerability scans, and SOC-aligned DevOps practices reduce operational risk without slowing clinical use.
Compliance is not a checkbox for ambient scribing. It is the foundation that allows hospitals to trust the system, keep regulators satisfied, and protect patients. When security, auditability, and regulatory alignment are baked into the architecture, adoption becomes easier and leaders gain confidence that automation is working in their favor.
How We Build Ambient AI Scribe Platforms for Hospitals
Building an ambient scribe platform is not just a data science exercise. It is a full-scale healthcare engineering process that must respect clinical workflows, compliance obligations, and enterprise IT requirements. At Intellivon, we use an eight-step approach that delivers accuracy, security, and long-term reliability.
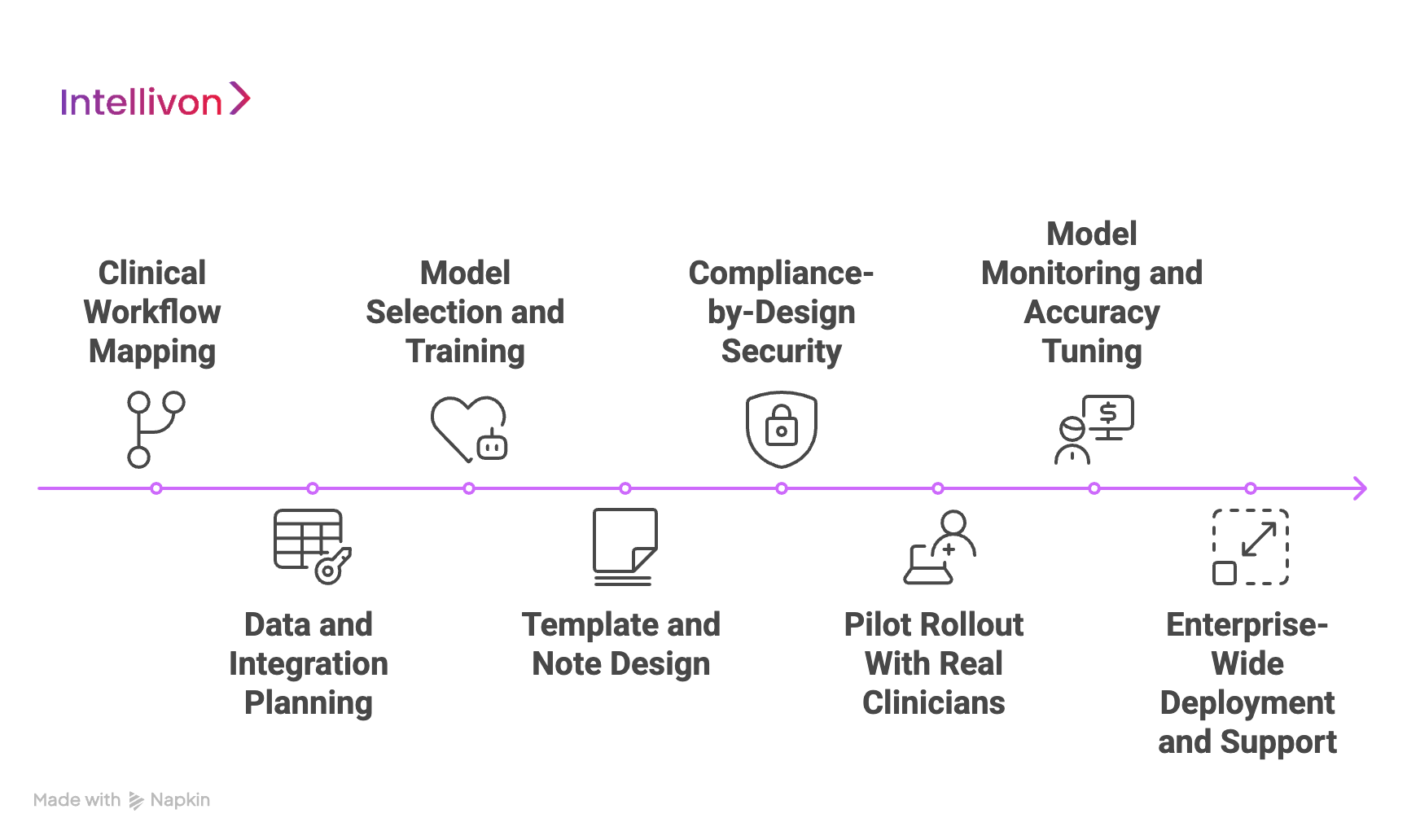
1. Clinical Workflow Mapping
Every hospital documents care differently. We begin by studying how physicians move through their day, how departments chart encounters, and where notes break down. This helps us design a system that fits naturally into existing routines instead of forcing new behavior.
2. Data and Integration Planning
The platform needs access to encounter data, scheduling systems, telehealth sessions, and the EHR. Our team maps the data landscape and defines how information will flow securely across systems. This removes uncertainty later in deployment.
3. Model Selection and Training
We train ASR and NLP models on domain-specific language, accents, and specialty terminology. The platform learns clinical phrasing, drug names, and abbreviations, so accuracy stays high even in noisy environments.
4. Template and Note Design
Each department has its own documentation style. We build structured SOAP notes and specialty-specific templates that reflect how clinicians actually write. This reduces editing time and makes adoption easier.
5. Compliance-by-Design Security
Security is engineered into the core. PHI encryption, RBAC, audit logging, and data minimization are defined before a single line of code is deployed. This ensures HIPAA and GDPR alignment from the first test environment.
6. Pilot Rollout With Real Clinicians
We launch in a controlled environment with selected physicians and nurses. Feedback in this phase helps adjust accuracy, templates, and EHR routing. Adoption grows because the system improves before full deployment.
7. Model Monitoring and Accuracy Tuning
The platform learns how each department speaks and documents care. Drift monitoring, retraining, and confidence metrics keep performance stable as usage expands. Over time, accuracy rises rather than declines.
8. Enterprise-Wide Deployment and Support
Once the system is validated, we scale to other departments and locations. Our team monitors uptime, latency, and integration health. When regulations change or new workflows are introduced, the platform adapts without disruption.
By following a structured build process, hospitals get a platform that delivers measurable value, stays compliant, and fits into daily clinical life without adding friction.
Cost Breakdown for Building an Ambient AI Scribe Platform
At Intellivon, the priority is to help healthcare enterprises build ambient scribe platforms that are compliant, resilient, and enterprise-ready. Pricing aligns with business goals, regulatory scope, and scale. Every dollar aims to drive measurable gains in patient safety, operational efficiency, and trusted data workflows.
When budgets are tight, we refine the scope with stakeholders. We never compromise HIPAA or GDPR alignment. We prepare for FDA and EU AI Act readiness. Every build balances cost efficiency with sustainable compliance and clear ROI visibility.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Compliance Alignment | Requirements, risk mapping, HIPAA controls, EU AI Act scoping, KPI definition | $6,000 – $12,000 |
| Architecture & Secure Design | Multi-layer design for PHI handling, encryption, resilience, IAM | $8,000 – $15,000 |
| Audio Capture & Edge Setup | Room mics, telehealth hooks, consent flows, noise filtering, speaker ID | $6,000 – $12,000 |
| ASR, NLP & Note Generation | Medical ASR tuning, entity extraction, SOAP templates, confidence scoring | $12,000 – $25,000 |
| EHR Integration & Interoperability | FHIR, HL7, SMART on FHIR, routing rules for Epic, Cerner, Meditech | $10,000 – $20,000 |
| Security & Privacy Engineering | RBAC, MFA, tokenization, redaction, keys, continuous monitoring | $8,000 – $15,000 |
| Platform UX & Interfaces | Clinician review UI, coder view, audit console, admin controls | $10,000 – $20,000 |
| Testing & Validation | HIPAA checks, penetration tests, safety tests, and model validation | $6,000 – $10,000 |
| Pilot & Training | Limited rollout, feedback loops, template refinements, playbooks | $6,000 – $10,000 |
| Deployment & Scaling | Cloud rollout, HA setup, observability, elastic scaling | $6,000 – $12,000 |
Total Initial Investment Range: $50,000 – $150,000
Ongoing Maintenance & Optimization (Annual): 15–20% of initial build
Hidden Costs Enterprises Should Plan For
- Integration complexity: Legacy EHR variants can require extra middleware and mapping.
- Compliance overhead: Audits, risk assessments, and documentation need recurring effort.
- Data governance: Normalizing mixed formats across departments takes steady resources.
- Cloud spend: Real-time pipelines and storage need cost controls to protect ROI.
- Change management: Training clinicians and coders carries measurable transition costs.
- Model drift: Periodic retraining preserves accuracy, fairness, and certification posture.
Best Practices to Avoid Budget Overruns
- Start with a focused scope: Pilot one department, prove impact, then scale.
- Embed compliance from day one: Avoid expensive rework later.
- Adopt modular design: Reuse AI pipelines and templates across service lines.
- Optimize cloud usage: Mix batch and real-time to control compute.
- Ensure observability: Track uptime, latency, and integration health continuously.
- Iterate for longevity: Update controls, recalibrate models, and refine workflows.
Request a tailored proposal from Intellivon’s healthcare AI experts. We will align your roadmap with budget, compliance obligations, and scalability goals.
Overcoming Challenges to Building An Ambient AI Scribe Platform
Deploying an ambient scribe system is not as simple as adding speech recognition. Hospitals operate in noisy, regulated, and highly integrated environments. To succeed, the platform must deliver accurate notes, protect PHI, and fit into existing workflows without creating extra work.
1. Clinical Accuracy Gaps
Many speech engines are trained on everyday conversations. They struggle with rapid clinical dialogue, drug names, acronyms, and multi-speaker environments. When accuracy drops, physicians end up correcting the transcript, which defeats the purpose of automation.
We use healthcare-trained ASR models built on clinical speech patterns. They understand specialty jargon, abbreviations, and fast-paced discussions. Accuracy improves as the platform learns real physician interactions, reducing the time clinicians spend reviewing AI output.
2. Notes Without Clinician Oversight
Fully automated documentation sounds appealing, but skipping physician review introduces compliance and medico-legal risk. If the AI misinterprets a symptom or adds unsupported content, hospitals become responsible for the error.
Every note passes through a human-in-the-loop review. Physicians can edit and sign off in seconds. The system stores version history, timestamps, and reviewer details. This keeps documentation defensible during audits, payer reviews, or legal disputes.
3. Weak EHR Integration
Some platforms generate notes, but clinicians still need to copy, paste, or manually attach documents. When that happens, the “automation” becomes another administrative task, not a time saver.
The platform connects to existing clinical systems through secure interoperability layers that follow FHIR, HL7, and SMART on FHIR standards. Documentation is posted to the appropriate patient record, visit type, and timestamp in real time. Clinicians never copy or paste, and administrators avoid duplicate work. The technology becomes invisible inside routine workflows.
4. Unsafe PHI Handling
Live audio and transcripts contain sensitive details. If a platform stores unencrypted data or lacks proper access controls, hospitals face unnecessary exposure and regulatory scrutiny.
Security is engineered into the core. PHI is encrypted in transit and at rest. Tokenization and redaction limit what stays in the system. Role-based access ensures only authorized users can interact with documentation, and every action is logged.
5. Limited Audit Visibility
Healthcare teams need proof of what happened and when. Without traceability, hospitals cannot defend documentation during payer disputes or compliance reviews.
Intellivon maintains immutable audit logs that track audio capture, ASR output, clinician edits, and EHR submission. Compliance teams can produce a complete history in minutes, not days.
6. Long-Term Model Drift
Language changes. New treatments and medications appear. Different departments use different phrasing. Without monitoring, accuracy drops and physician trust fades.
We monitor model drift and retrain on approved datasets without pausing operations. The platform learns how each department speaks, improving accuracy month after month instead of degrading.
7. High IT Overhead
Hospitals already manage many mission-critical systems. If a new platform is hard to deploy or maintain, it becomes a burden on IT teams.
We offer cloud, on-prem, or hybrid deployments. Observability dashboards track uptime, latency, and integration health. Automated scaling, backups, and failover keep the platform reliable with minimal IT involvement.
Hospitals succeed with ambient scribing when accuracy, compliance, and workflow fit come first. Intellivon designs with these realities in mind, so documentation becomes faster, safer, and easier at enterprise scale.
Top Examples of AI Scribe Platforms
Hospitals exploring ambient scribing often look at how existing platforms operate in real clinical settings. The examples below show how different vendors are applying speech recognition, NLP, and generative AI to reduce manual charting and support accurate, audit-ready notes.
1. Ambience Healthcare
Ambience Healthcare offers a fully ambient documentation platform used across multiple specialties. The system listens during the clinical encounter and converts natural conversation into structured notes ready for clinician review.
Its core engine uses medical-trained speech recognition combined with NLP to identify symptoms, diagnoses, medications, plans, and relevant clinical details.
The draft note is generated in real time and aligned to specialty-specific templates, which reduces editing for physicians. Ambience also supports coding workflows by suggesting ICD and CPT codes based on what was said in the consultation, making it attractive for billing teams that want cleaner documentation and fewer denials.
2. Tali AI Ambient Scribe
Tali offers an AI scribe that works across browser and desktop environments, making it accessible for outpatient practices and telehealth visits. Clinicians speak naturally during their consultations or record a short summary afterward, and Tali generates the full clinical note automatically.
Its AI models identify medical entities, format SOAP documentation, and structure assessments, plans, and orders. Because it is EHR-agnostic and cloud-based, clinicians can adopt it without changing existing workflows. The platform also learns from physician corrections, so accuracy improves over time.
3. Heidi Health
Heidi Health focuses on fully automated clinical note generation for hospitals and medical practices across different countries. The platform transcribes conversations, extracts clinical meaning, and prepares notes, letters, and summaries for physician sign-off.
It uses LLM-driven engines tuned for clinical language, enabling it to recognize contextual details such as presenting complaints, treatment plans, and follow-up instructions. Heidi emphasizes reducing after-hours charting and supports multilingual environments, making it useful for diverse patient populations and global deployments.
4. Aura — Insight Health
Aura is built for practices that want mobile or browser-based scribing without extra hardware. It records the consultation, transcribes it, and generates a structured note that clinicians can edit and approve.
Its AI models map clinical findings into SOAP or specialty templates and offer code suggestions for billing accuracy. The platform supports specialty customization, enabling departments like dermatology, cardiology, or pediatrics to receive notes that reflect their clinical documentation style. Aura’s design focuses on quick onboarding and minimal workflow disruption.
These platforms demonstrate how ambient scribing is moving from pilot projects to everyday clinical use. Each takes a different path, but the goal remains consistent, which is faster charting, cleaner documentation, and less administrative pressure on clinicians.
Conclusion
Ambient scribe systems are moving from experimental pilots to core infrastructure in modern healthcare. When documentation becomes automatic, physicians spend more time with patients and less time completing charts after hours. Hospitals see faster chart closures, stronger billing accuracy, and fewer compliance gaps. The impact improves staff morale, retention, and capacity without adding extra clinicians to the workforce.
However, building and deploying a secure platform is not a simple engineering task. It demands medical-grade AI, EHR interoperability, audit trails, and long-term model monitoring. Working with a healthcare-focused solution provider ensures the platform aligns with regulatory expectations, integrates smoothly with existing systems, and remains reliable as clinical environments evolve. For hospitals, that stability matters as much as the technology itself.
Build An Ambient AI Scribe Platform With Intellivon
At Intellivon, we build ambient AI scribe platforms that combine medical-grade accuracy, clinical compliance, and enterprise-scale reliability. Our systems remove manual documentation burden, reduce after-hours charting, and protect revenue integrity, all while integrating seamlessly with existing EHR and telehealth workflows.
Each platform is engineered to meet the demands of modern hospitals: secure, scalable, and designed for measurable ROI from day one.
Why Partner With Intellivon?
- Compliance-First Architecture: Every deployment aligns with HIPAA, GDPR, FDA SaMD, and EU AI Act frameworks. PHI encryption, immutable audit logs, and access controls ensure trust, traceability, and legal defensibility across regions.
- Healthcare-Tuned AI Models: Our ASR, NLP, and generative note systems are trained on clinical speech patterns, specialty-specific terminology, and real-world usage. The result: accurate notes that clinicians approve in seconds.
- Seamless EHR Interoperability: We connect directly with custom systems using FHIR, HL7, and SMART on FHIR. Notes post automatically to the correct chart and timestamp without manual effort.
- Scalable Cloud-Native Infrastructure: Multi-hospital deployments, low-latency inference, high availability, and elastic scaling keep the platform reliable during peak usage. IT teams get dashboards, monitoring, and automated failover.
- Continuous Model Optimization: Integrated MLOps pipelines detect drift, retrain models, and improve accuracy over time. The system learns from real workflows and becomes more precise with ongoing usage.
- Zero-Trust Security Framework: Encryption at every layer, identity management, segmentation, and continuous threat detection keep PHI safe without slowing down clinical operations.
- Human-Centered Design: Clinician review screens, coder dashboards, and admin controls make AI-generated notes easy to verify and sign. Adoption rises because the platform fits naturally into clinical routines.
- Proven Healthcare Expertise: With years of experience delivering enterprise healthcare AI systems, we bring validated reference architectures, compliance maturity, and outcomes-driven delivery.
Book a strategy call with Intellivon to explore how a custom-built ambient scribe platform can reduce documentation time, strengthen billing accuracy, and scale seamlessly across your hospital network.
FAQs
Q1. How accurate are ambient AI scribe systems in real clinical use?
A1. Accuracy depends on the quality of the speech engine and how well it is trained on medical language. Enterprise-grade platforms use clinical ASR and NLP models that understand terminology, abbreviations, and specialty-specific dialogue. In real deployments, accuracy improves over time as the system learns physician phrasing and department workflows. Clinicians typically review and sign notes in seconds because the majority of documentation is already complete.
Q2. Can ambient AI scribes integrate with custom platforms?
A2. Yes. Modern platforms connect through FHIR, HL7, and SMART on FHIR. A well-built scribe system routes notes directly into the correct patient chart, encounter, and timestamp without copy-paste work. Hospitals see the most value when integration is designed as part of the architecture instead of an afterthought.
Q3. What is the cost of deploying an AI scribe at enterprise scale?
A3. Costs vary based on deployment model, number of clinicians, EHR integrations, and compliance scope. Most enterprise builds fall between $50,000 and $150,000, with annual maintenance in the 15–20% range. Hospitals often start with a department-level pilot and scale as results become measurable.
Q4. Is ambient AI scribing HIPAA and GDPR compliant?
A4. It can be, but only if the platform was engineered for healthcare. Compliance requires encryption end-to-end, strict access controls, audit trails, redaction, and support for data deletion or export. Hospitals should evaluate how the system handles PHI before approving deployment.
Q5. Do clinicians still review notes generated by AI?
A5. Yes. Human review remains essential. The AI prepares the draft, but the physician verifies accuracy and finalizes the note. This keeps documentation legally defensible and prevents incorrect information from entering the EHR. Review and approval usually take seconds instead of minutes, which is where time savings are realized.





