Digital chronic care initiatives start with strong intent and promising early engagement. However, as programs grow across clinical teams, outcomes begin to flatten. Engagement rates decline, system failures rise, and operational complexity increases. Chronic care telemedicine fails when platforms aim to replace in-person visits instead of managing ongoing care. Reminders, dashboards, and AI alerts alone do not lead to lasting behavior change or clinical responsibility.
9amHealth avoided this problem by building chronic care around continuity, governance, and controlled clinical workflows. Their model offers a useful perspective for organizations looking to rethink how chronic care telemedicine should work at scale.
At Intellivon, we design chronic care telemedicine platforms to operate within complex enterprise environments, alongside EHRs, identity systems, and clinical governance models. These platforms are created to scale securely without altering legacy data or weakening compliance controls. This blog shares that experience to explain how to build enduring chronic care systems from scratch that can handle scale instead of collapsing under it.
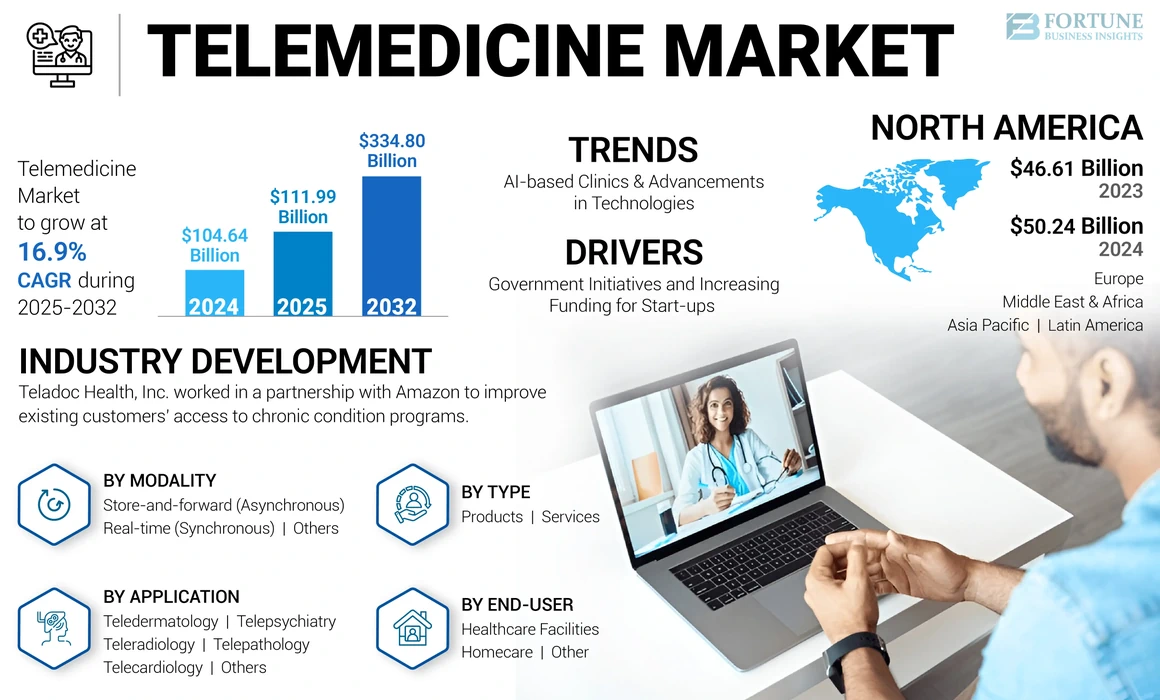
Key Takeaways Of The Telemedicine Platform Market
The telemedicine market has already crossed the USD 100 billion mark and continues to accelerate. Industry estimates show steady growth through 2025, with the market expected to more than triple in size by the early 2030s as adoption expands across care models.
AI in Telemedicine: Growth and Focus Areas
- Investment in AI-enabled telemedicine is accelerating rapidly, with market forecasts indicating expansion from roughly USD 4 billion in the mid-2020s to well over USD 25 billion by the end of the decade.
- This growth reflects sustained adoption of AI across virtual care workflows, particularly in areas that require continuous oversight rather than episodic interaction.
- Among AI use cases, remote patient monitoring stands out as the fastest-scaling function, driven largely by chronic conditions such as diabetes, hypertension, and cardiovascular disease.
Segment and Modality Trends
- Market estimates suggest global telemedicine spending already exceeds USD 140 billion and is expected to grow several-fold by the early 2030s.
- Tele-hospital models currently account for the largest share of deployments, reflecting early enterprise adoption by hospital systems.
- However, mobile health and app-based care models are expanding at a significantly faster pace, with growth rates projected to outstrip traditional tele-hospital platforms.
- While real-time video consultations still represent a large portion of virtual care usage, remote patient monitoring is growing more quickly as care shifts toward continuous management models.
Regional Growth Dynamics
- In the United States, telehealth has transitioned from a niche capability to a core infrastructure investment, with market size expected to increase dramatically over the current decade.
- North America continues to generate the largest share of telehealth revenue, supported by payer reimbursement models and enterprise health-system adoption.
- At the same time, Asia-Pacific is emerging as the fastest-expanding region, fueled by mobile-first healthcare delivery, digital health initiatives, and large underserved populations.
What Is The Chronic Care Telemedicine Platform 9amHealth?
9amHealth is a virtual cardiometabolic care provider focused on preventing and managing chronic conditions such as obesity, type 2 diabetes, hypertension, and high cholesterol. Rather than positioning itself as a general telemedicine tool, it delivers condition-specific care programs designed for long-term outcomes.
At its foundation, the platform combines virtual clinical care with medication management, lifestyle guidance, and at-home diagnostics. As a result, care is continuous instead of episodic. In addition, patients remain connected to the same care model over time, which supports consistency and accountability.
Importantly, 9amHealth follows structured, evidence-based pathways. Therefore, treatment decisions align with established clinical protocols rather than ad-hoc virtual visits. At the same time, technology supports intake, monitoring, and follow-up, while licensed clinicians retain full control over care decisions.
Because of this approach, 9amHealth aligns well with employer and payer models focused on long-term risk reduction. Ultimately, it shows how chronic care telemedicine can function as an outcomes-driven service line rather than a convenience layer.
Features That Set It Apart
9amHealth differentiates itself by how it structures chronic care, not by adding surface-level telemedicine features. Each capability supports continuity, control, and measurable outcomes over time.
1. Condition-Specific Care Programs
The platform is built around cardiometabolic conditions rather than generalized virtual care. As a result, treatment plans, monitoring, and follow-ups align tightly with disease progression. This focus improves clinical consistency and reduces fragmented care experiences.
2. Integrated Medication and Care Management
Care extends beyond consultations into prescription management and adherence support. Therefore, treatment decisions remain connected to outcomes, not isolated visits. This also helps reduce downstream complications and unnecessary escalations.
3. Continuous Monitoring with Clinical Context
Data from labs, self-reported inputs, and ongoing check-ins feed into longitudinal care views. However, information is filtered through clinical protocols, not raw alerts. This prevents noise while keeping care teams informed.
4. Human-Led Care with Technology Support
Technology assists intake, engagement, and follow-up. At the same time, licensed clinicians remain responsible for decisions and accountability. This balance supports trust, safety, and regulatory alignment.
Together, these features show why 9amHealth functions as a chronic care service line rather than a telemedicine tool. The platform prioritizes structure, accountability, and long-term outcomes, which are critical for enterprise-scale chronic care delivery.
Business Model of Telemedicine Platform 9amHealth
9amHealth operates on a business model designed for long-term chronic care rather than transactional virtual visits. The structure aligns clinical delivery, patient engagement, and cost control into a single operating system. As a result, the platform supports predictable outcomes and scalable deployment across enterprise populations.
1. Subscription-Based Chronic Care Delivery
Care is delivered through recurring subscription programs instead of per-visit billing. Therefore, incentives remain aligned with continuity and prevention. This model encourages proactive care while reducing dependence on visit volume for revenue.
2. Employer and Payer-Aligned Distribution
The platform is commonly deployed through employer health benefits and payer partnerships. Consequently, enrollment targets defined populations rather than self-selected individuals. This improves risk pooling and enables systematic outreach to high-risk members.
3. Bundled Clinical and Medication Services
Clinical consultations, prescriptions, and diagnostics are offered as a unified package. As a result, care decisions remain connected to outcomes and costs. This reduces fragmentation across vendors and improves operational clarity.
4. Outcome-Oriented Economic Structure
The business model supports value-based incentives tied to measurable improvement in chronic conditions. Over time, this shifts focus away from utilization and toward sustained health impact.
Overall, 9amHealth’s business model reinforces long-term care ownership. It prioritizes stability, alignment, and outcomes, which are critical for enterprise-grade chronic care telemedicine programs.
From Telemedicine 1.0 Visits to Telemedicine 2.0 Chronic-Care Systems
Telemedicine 2.0 shifts virtual care from isolated video visits to AI-enabled, condition-specific chronic-care service lines governed like enterprise operations.
Many organizations already offer telehealth. However, most still operate at a maturity level designed for access, not outcomes. This gap explains why leaders often see early wins followed by stalled ROI.
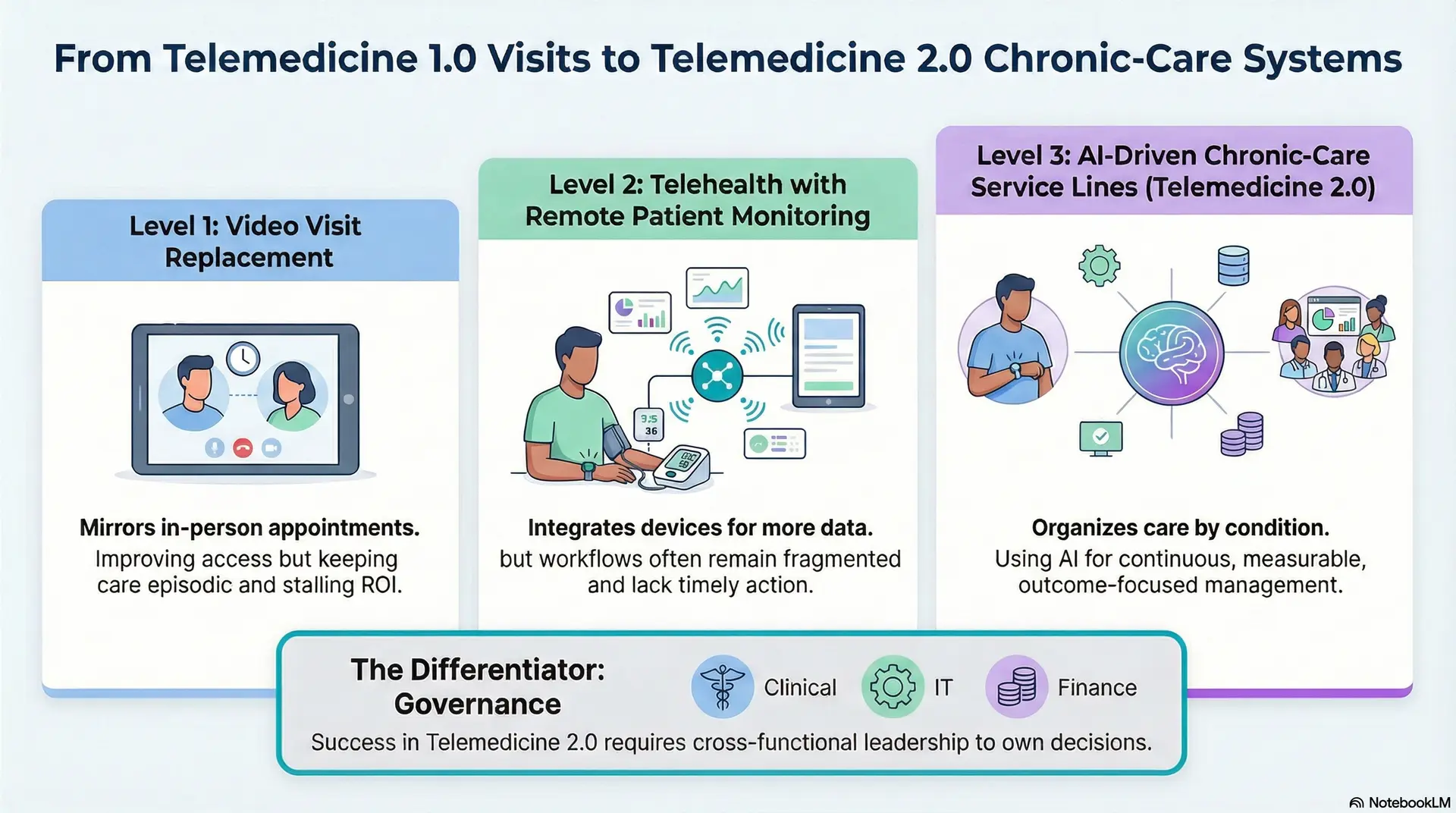
Telemedicine Maturity Model
Level 1: Video Visit Replacement
At this stage, telemedicine mirrors in-person appointments. It improves access and convenience. However, care remains episodic. As a result, outcomes and cost curves change very little over time.
Level 2: Telehealth with Remote Patient Monitoring
Here, platforms integrate devices and basic monitoring. Therefore, clinicians gain more data between visits. Still, workflows often remain fragmented, and insights do not always translate into timely action.
Level 3: AI-Driven Chronic-Care Service Lines
Telemedicine 2.0 organizes care around specific conditions. AI supports intake, risk stratification, and engagement. Consequently, care becomes continuous, measurable, and aligned with long-term outcomes.
Why ROI Plateaus at Visit Replacement
Video visits alone reduce friction, not disease burden. Over time, utilization stabilizes while costs persist. Therefore, financial impact levels off unless care delivery itself changes.
Governance Is the Differentiator
Telemedicine 2.0 requires shared ownership. Cross-functional steering committees bring together clinical, IT, finance, and compliance leaders. This group owns roadmap decisions, budgets, outcomes, and risk management.
Telemedicine 2.0 is not another tool layered onto existing workflows. Instead, it represents a shift toward virtual care as a managed service line. With maturity defined, the next step is deciding what systems must be built to support it.
Telemedicine Platforms Resolve 74% of Patient Concerns in One Visit
Telemedicine outcomes are often discussed in abstract terms. However, primary program data tells a clearer story when platforms are designed for resolution, not volume. In one real-world evaluation of on-demand telemedicine, nearly three out of four patients had their concerns fully addressed in a single virtual encounter. That number matters because it shifts the conversation from access to effectiveness.
For enterprise leaders, this metric signals more than convenience. It points to structural efficiency in care delivery, workload distribution, and cost containment when telemedicine is implemented with clinical intent.
1. Single-Visit Resolution Is an Architectural Outcome
A 74% resolution rate does not happen by chance. It reflects how the platform structures intake, triage, and clinical decision support before a provider ever joins the encounter.
In high-performing telemedicine platforms, patient context is captured early. Symptoms, history, and risk factors are assessed upfront. This allows clinicians to focus on decision-making instead of data gathering. As a result, visits are shorter, more focused, and more likely to conclude with a clear plan of care.
For enterprises, this directly affects clinician capacity. Fewer follow-up visits reduce downstream load while improving patient satisfaction and continuity.
2. Low “New Utilization” Signals Real Substitution
One common concern among decision-makers is whether telemedicine creates unnecessary demand. In the same evaluation, only 16% of patients reported they would have done nothing if telemedicine were unavailable.
This data point is critical. It suggests that telemedicine is primarily substituting for higher-cost or less efficient sites of care rather than generating avoidable utilization. Patients are using virtual care as an alternative, not an add-on.
From an enterprise perspective, this reduces financial risk. Programs that shift care without inflating volume are far more viable under value-based and shared-risk models.
3. Cost Savings Come from Care Redirection
The evaluated program reported net savings ranging from $19 to $121 per telemedicine visit. These savings were driven mainly by diverting patients away from emergency departments, urgent care, and other high-cost settings.
This highlights an important distinction. Cost efficiency in telemedicine does not come solely from AI or automation. It comes from routing patients to the right level of care at the right time.
Platforms that embed clinical decision logic into triage workflows are better positioned to deliver predictable economic outcomes at scale.
4. Telestroke Shows Both the Upside and the Tradeoffs
Registry data from telestroke programs offers a useful counterbalance. Telemedicine evaluation increased the likelihood of patients receiving thrombolytic therapy by 61%. That is a meaningful clinical gain.
At the same time, door-to-needle times increased by just over six minutes, and the likelihood of meeting the 60-minute benchmark dropped by 44%. These findings underline a key enterprise lesson. Telemedicine improves access and decision quality, but workflow design still determines operational performance.
This is where governance matters. Without tight integration into clinical pathways and escalation protocols, even effective telemedicine programs can introduce new bottlenecks.
What This Means for Enterprise Telemedicine Strategy
High-resolution rates, low new utilization, and measurable cost savings all point to one conclusion. Telemedicine platforms succeed when they are designed as clinical systems, not digital front doors.
When telemedicine is architected this way, it becomes a reliable operational lever rather than a variable experiment.
Core Building Blocks of a Chronic Care Telemedicine Platform
Scalable chronic care telemedicine platforms are built as systems, combining enrollment control, care orchestration, data pipelines, and governance rather than isolated virtual visit features.
Building chronic care telemedicine at enterprise scale requires a system-level approach. Individual features matter, but architecture determines whether care remains safe, effective, and governable as volumes grow. The following building blocks define platforms that sustain outcomes over time.
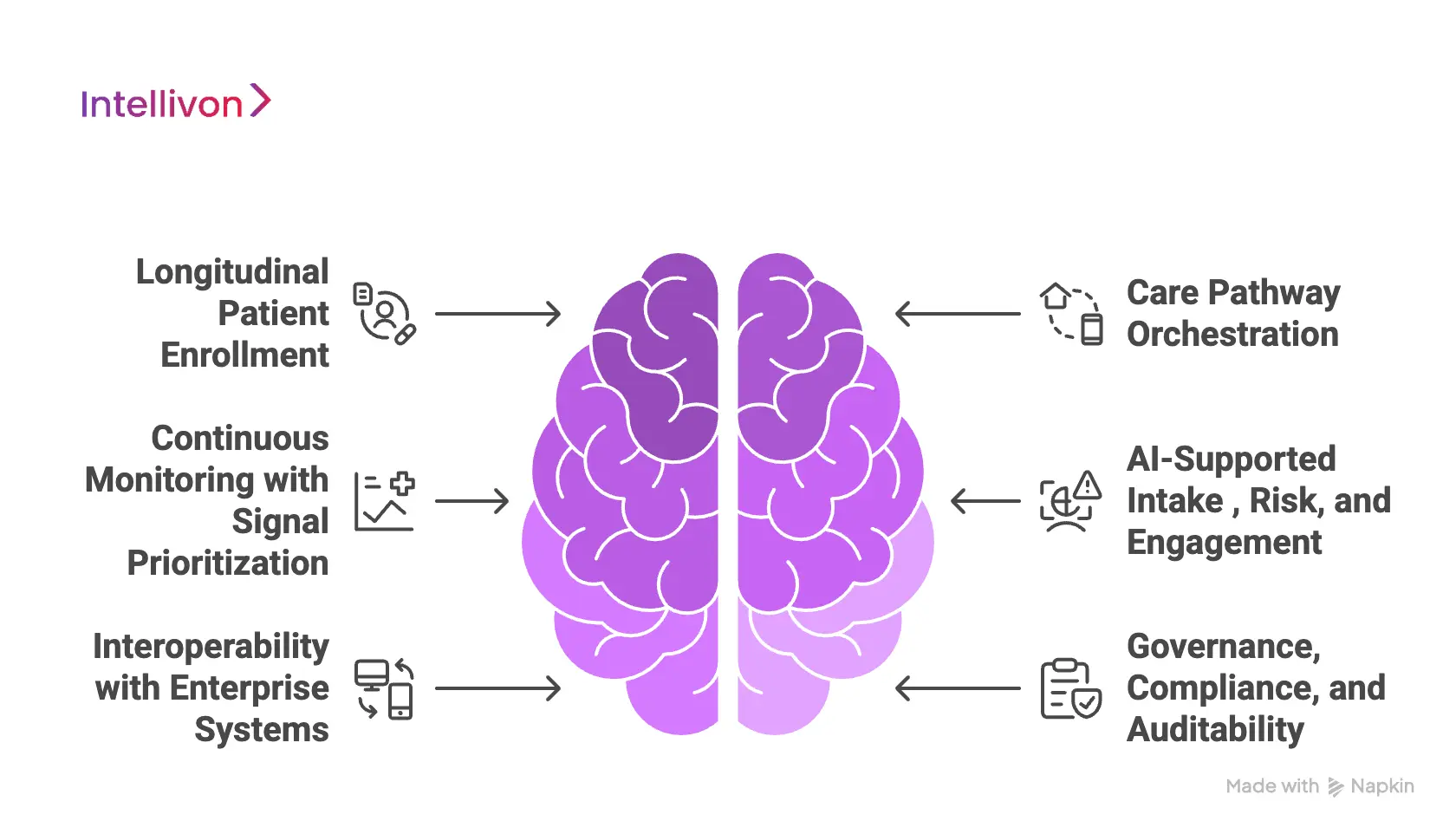
1. Longitudinal Patient Enrollment
Chronic care begins before the first visit. Platforms must support condition-based eligibility, verified identity, and consent that persists across months or years. As a result, care teams work with a stable patient record rather than disconnected encounters.
This layer also determines who enters the program and why. Therefore, it directly impacts risk stratification, equity, and downstream cost control.
2. Care Pathway Orchestration
Effective platforms manage journeys, not calendars. Care pathways define how patients move through education, monitoring, escalation, and follow-up. Consequently, clinical decisions follow a structured approach rather than ad-hoc interactions.
This orchestration layer ensures continuity even when care teams or touchpoints change.
3. Continuous Monitoring with Signal Prioritization
Remote patient monitoring and patient-reported data generate constant input. However, raw data alone creates noise. Platforms must filter signals based on clinical relevance and risk thresholds.
By prioritizing what matters, care teams can intervene earlier without alert fatigue.
4. AI-Supported Intake, Risk, and Engagement
AI plays a supporting role across intake and ongoing engagement. It helps identify risk trends, predict drop-off, and personalize follow-up timing.
At the same time, clinical judgment remains human-led. This balance improves efficiency while preserving accountability.
5. Interoperability with Enterprise Systems
Chronic care platforms must coexist with EHRs, analytics stacks, and identity systems. Clean integration prevents data duplication and protects legacy records. Therefore, scale does not compromise data integrity or compliance.
6. Governance, Compliance, and Auditability
Every action within the platform must be traceable. Role-based access, audit logs, and explainable AI ensure regulatory alignment. This layer protects both patients and enterprises as programs expand.
Chronic care telemedicine succeeds when these building blocks operate as a unified system. With the foundation in place, leaders can then focus on how AI, governance, and economics drive long-term value.
How AI Actually Works Inside a Chronic Care Telemedicine System
AI creates value in chronic care only when it is designed as part of the system, not added as a feature. In enterprise environments, the goal is not automation for speed, but intelligence for control, safety, and scale. When applied correctly, AI reduces cognitive load on care teams and improves consistency across large populations without introducing clinical or regulatory risk.
The sections below explain how AI is practically used inside mature chronic care telemedicine platforms.
1. AI at Intake and Clinical Triage
AI plays its first role before a clinician enters the workflow. Structured intake models organize patient-reported symptoms, medical history, medications, and risk indicators into a coherent clinical summary. Therefore, providers begin visits with context rather than fragmented inputs.
This improves visit efficiency and decision quality. As a result, clinicians spend less time gathering information and more time assessing and guiding care. Over time, this leads to higher single-visit resolution and fewer unnecessary follow-ups.
2. Risk Stratification Across Time
Chronic care depends on understanding patterns, not snapshots. AI continuously evaluates trends across lab results, vitals, adherence behavior, and engagement signals. Consequently, risk is detected earlier, often before patients report worsening symptoms.
This enables proactive outreach and targeted intervention. It also allows care teams to prioritize patients who need attention most, without reviewing every record manually. At scale, this capability is essential to prevent care teams from becoming reactive.
3. Engagement Intelligence and Drop-Off Prevention
Sustained engagement is one of the hardest problems in chronic care. AI monitors behavioral signals such as missed check-ins, delayed refills, or reduced interaction frequency. When disengagement patterns emerge, the system flags the risk.
Importantly, AI does not replace human follow-up. Instead, it guides care teams on when to intervene and how urgently. This improves retention while preserving a human relationship with patients.
4. Operational Forecasting and Capacity Planning
AI also supports the operational side of chronic care delivery. By analyzing historical demand, condition mix, and engagement trends, models forecast future care needs. Therefore, enterprises can align staffing, scheduling, and program expansion more accurately.
This capability becomes critical as programs scale across employers, regions, or payer groups. Without it, growth often leads to clinician burnout or service degradation.
Where AI Is Intentionally Constrained
Enterprise-grade platforms apply clear limits to AI usage. AI does not diagnose, prescribe independently, or make final clinical decisions. Licensed clinicians retain responsibility for care decisions at every stage.
In addition, AI-supported actions are logged, auditable, and explainable. These controls protect patient safety, support compliance, and maintain trust with regulators and internal governance teams.
AI succeeds in chronic care telemedicine when it operates quietly in the background, strengthening continuity and coordination. When designed as infrastructure rather than a decision-maker, AI helps enterprises scale chronic care safely, efficiently, and responsibly.
Key Features Of A Chronic Care Telemedicine Platform Like 9amHealth
High-performing chronic care telemedicine platforms combine continuity, clinical governance, and system integration to deliver measurable outcomes at enterprise scale.
The features below reflect how mature platforms support sustained outcomes rather than short-term engagement.
1. Condition-Specific Care Design
Strong platforms are organized around specific chronic conditions, not generalized telemedicine workflows. Care protocols, monitoring cadence, and escalation rules are aligned to how each condition progresses over time. Therefore, clinical decisions remain consistent even as care teams or touchpoints change.
This design also enables clearer benchmarking. Enterprises can measure outcomes, cost trends, and adherence against condition-level baselines instead of broad utilization metrics.
2. Longitudinal Care Ownership
Patients are enrolled in ongoing care programs rather than single encounters. As a result, responsibility for outcomes remains clear across months and years. This reduces handoffs, missed follow-ups, and care fragmentation.
From an enterprise perspective, longitudinal ownership simplifies governance. Leaders can see who is accountable for care at every stage of the journey.
3. Integrated Medication and Diagnostics Management
Chronic care depends heavily on medication adherence and diagnostic feedback. Mature platforms connect prescribing, refills, lab testing, and follow-up into one coordinated loop. Consequently, treatment decisions reflect real patient responses rather than assumptions.
This integration also reduces operational leakage. Care teams no longer rely on disconnected pharmacy or lab systems to close the loop.
4. Remote Monitoring with Clinical Guardrails
Remote patient monitoring generates continuous streams of data. However, raw signals create noise without structure. Effective platforms apply clinical thresholds and prioritization logic to surface what actually matters.
As a result, care teams can intervene earlier without being overwhelmed. This balance becomes essential as monitoring scales across large populations.
5. AI-Supported Engagement and Risk Prioritization
AI supports intake analysis, engagement timing, and risk detection across large cohorts. It identifies patterns that indicate deterioration or disengagement.
At the same time, final decisions remain clinician-led. This approach improves efficiency while preserving trust, safety, and regulatory alignment.
6. Enterprise-Grade Interoperability
Chronic care platforms must operate alongside existing enterprise systems. Clean integration with EHRs, identity frameworks, and analytics platforms ensures legacy data remains intact.
Therefore, scaling the program does not introduce data inconsistency or compliance gaps. Interoperability also enables longitudinal reporting across virtual and in-person care.
7. Built-In Governance and Auditability
Every interaction within the platform must be traceable. Role-based access, audit logs, and explainable workflows support internal oversight and external compliance.
This governance layer protects both patients and enterprises as programs grow. Without it, scale introduces risk instead of value.
These features work together to transform chronic care telemedicine into a durable service line. When designed as a system, the platform supports growth, accountability, and long-term outcomes rather than short-lived digital adoption.
How Intellivon Builds Enterprise-Grade Chronic Care Telemedicine Platforms
Most telemedicine vendors focus on getting virtual care live. Intellivon focuses on what happens after launch, when volumes grow, regulations tighten, and outcomes come under scrutiny.
Our experience building enterprise AI platforms across regulated healthcare environments shapes how chronic care telemedicine is architected. These platforms operate inside existing EHRs, identity frameworks, and compliance models without altering legacy data or creating parallel systems. As care scales, safety and control scale with it.
The framework below reflects how Intellivon consistently delivers chronic care platforms that endure enterprise complexity.
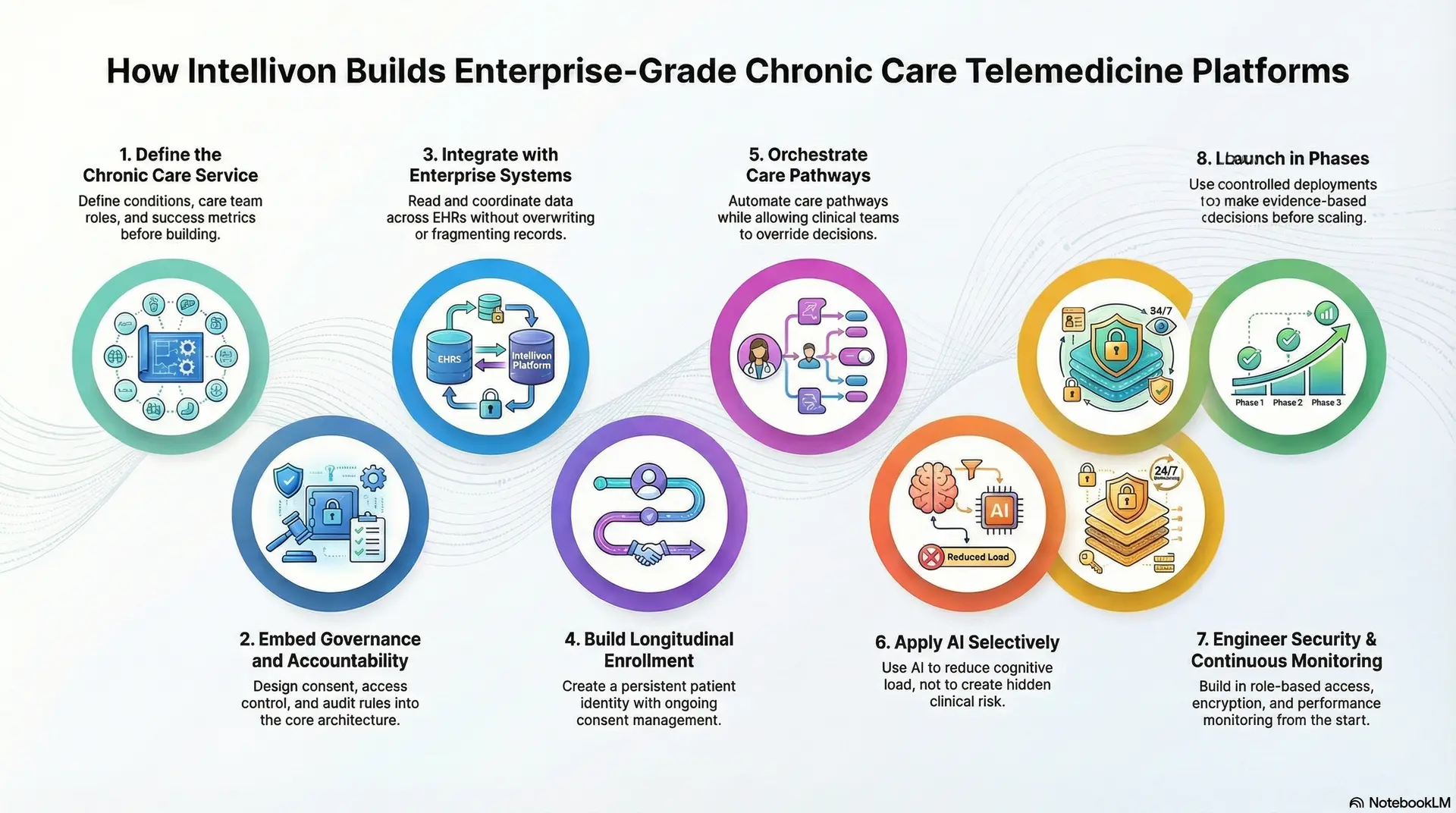
Step 1: Define the Chronic Care Service
Every build begins with service-line clarity. Conditions in scope, care team responsibilities, escalation thresholds, and success metrics are defined first. Therefore, the platform reflects how care is delivered, not how software is imagined.
This step aligns clinical leadership, operations, and technology teams early. As a result, downstream design decisions remain grounded in care reality.
Step 2: Embed Governance and Accountability
Intellivon treats governance as foundational architecture. Clinical accountability, consent logic, access control, and audit requirements are designed before workflows are automated. Consequently, compliance is enforced by system behavior rather than policy documents.
This approach becomes critical when programs expand across employers, regions, or payer contracts.
Step 3: Integrate with Enterprise Systems
Large healthcare organizations cannot afford EHR disruption. Integration architecture defines strict data boundaries across EHRs, labs, PBMs, and analytics platforms. Therefore, the platform reads and coordinates data without overwriting or fragmenting existing records.
This preserves data integrity while enabling real-time coordination across virtual and in-person care.
Step 4: Build Longitudinal Enrollment
Chronic care requires a persistent identity. Enrollment workflows support condition-based eligibility, while consent is managed as an ongoing lifecycle. As a result, patient relationships remain stable across months and care touchpoints.
This foundation simplifies reporting, audit readiness, and continuity at scale.
Step 5: Orchestrate Care Pathways
Condition-specific pathways guide monitoring, follow-ups, and escalation. However, clinical teams retain override authority at every stage. Therefore, automation supports consistency without removing judgment.
This balance protects safety while improving operational efficiency as volumes grow.
Step 6: Apply AI Where It Strengthens Decisions
AI is deployed selectively. Intake summarization, risk stratification, engagement timing, and drop-off detection are prioritized. Models are monitored for drift and bias, and outputs remain explainable.
As a result, AI reduces cognitive load without creating hidden clinical or regulatory risk.
Step 7: Engineer Security and Continuous Monitoring
Enterprise security is not optional. Role-based access, encryption, audit logs, and performance monitoring are built into the platform. Consequently, reliability improves as clinical load increases rather than degrading under pressure.
This ensures the platform remains stable during peak demand.
Step 8: Launch in Phases
Rollout begins with controlled deployments. Clinical outcomes, engagement patterns, and operational signals are validated before expansion. Therefore, scaling decisions are evidence-based rather than assumption-driven.
This phased approach allows enterprises to grow confidently across conditions and populations.
Intellivon does not build chronic care telemedicine as a feature set. We build it as an enterprise operating system designed to survive scale, scrutiny, and long-term use. When architecture, governance, and AI are aligned, chronic care becomes a durable growth engine rather than a fragile digital initiative.
Cost to Build A Chronic Care Telemedicine Platform
Building a chronic care telemedicine platform does not require a single, oversized investment on day one. Most enterprises start with a focused foundation that supports longitudinal care, safe escalation, enterprise integrations, and compliance controls. From there, platforms expand as patient volumes, conditions, and governance requirements grow.
At Intellivon, we structure costs around platform maturity, not feature overload. This phased approach helps enterprises launch faster, validate outcomes early, and scale chronic care with controlled clinical and financial risk.
Estimated Cost Breakdown (USD 85,000–220,000)
| Cost Component | What It Covers | Estimated Range |
| Discovery & Chronic Care Model Design | Condition scope, care pathways, escalation logic, outcome KPIs, and platform architecture | $10,000 – $20,000 |
| Longitudinal Enrollment & Intake Workflows | Condition-based eligibility, structured intake, ongoing assessments, and care continuity logic | $12,000 – $28,000 |
| Care Pathway Orchestration Engine | Protocol-driven journeys, escalation thresholds, follow-ups, and human override controls | $12,000 – $30,000 |
| Remote Patient Monitoring Integration | Device ingestion, patient-reported data, signal prioritization, and alert controls | $10,000 – $25,000 |
| EHR and Enterprise Integrations | HL7/FHIR interfaces, read-only context, scheduling sync, and safe handoffs | $15,000 – $40,000 |
| Identity, Consent, and Access Governance | RBAC, SSO options, consent lifecycle, and audit-ready access control | $8,000 – $18,000 |
| Compliance and Security Controls | HIPAA safeguards, encryption, logging, AI traceability, and audit trails | $8,000 – $16,000 |
| Analytics and Outcomes Reporting | Longitudinal outcomes, utilization trends, risk stratification, and executive dashboards | $6,000 – $15,000 |
| Testing, Pilot, and Stabilization | QA, workflow testing, pilot rollout, clinician feedback, and tuning | $6,000 – $18,000 |
Typical MVP Range: $85,000 – $130,000
Enterprise-Ready Phase 1 Platform: $150,000 – $220,000
The final cost depends on how much governance, integration depth, and outcome measurement are required from the start.
Factors That Influence the Cost of Chronic Care Telemedicine Platforms
Cost in chronic care is driven by system complexity, not screen count. Understanding these drivers early helps enterprises avoid rework and budget overruns later.
1. Depth of Care Pathway Design
Managing one condition with simple follow-ups costs less than orchestrating multi-condition journeys with escalation tiers. Costs increase as protocols require tighter coordination, safety thresholds, and clinician oversight. That added rigor reduces risk at scale.
2. Integration with Existing Clinical Workflows
Light integration may involve read-only access to patient context. Deep integration includes appointment creation, structured notes, and alignment with care teams. Bidirectional workflows cost more, but they prevent fragmented care and data inconsistency.
3. Remote Monitoring and Signal Governance
Basic monitoring is inexpensive. However, enterprise platforms must filter noise, prioritize signals, and prevent alert fatigue. Designing this logic adds effort but protects care teams as monitoring scales.
4. AI Governance and Auditability
AI that supports intake and risk assessment must be explainable and traceable. Costs rise when enterprises require logged AI outputs, confidence thresholds, bias monitoring, and enforced escalation rules. These controls are essential for regulated environments.
5. Identity, Consent, and Multi-Role Access
Single-role systems are simpler. Enterprise platforms require patient, clinician, operations, and admin roles. Consent must also persist, renew, and revoke over time. This governance layer directly impacts cost and long-term safety.
6. Analytics and Executive Visibility
Basic reporting explains what happened. Enterprise analytics explains why outcomes changed and what to adjust next. Costs increase when platforms support real-time dashboards, cohort analysis, and outcome tracking across populations.
How Enterprises Stay Within Budget
Budget discipline comes from phased delivery. Start with enrollment, care pathways, monitoring, EHR context, and compliance controls. Prove outcomes with a focused rollout before expanding into additional conditions or automation.
Equally important, KPIs should be locked early. Most cost overruns occur when the scope expands mid-build. A strong foundation first allows chronic care telemedicine platforms to scale with confidence rather than correction.
How Telemedicine Platforms Like 9amHealth Earn Revenue
Revenue models in chronic care telemedicine look very different from traditional virtual visits. The focus shifts from transaction-based billing to sustained value delivery over time. This structure supports predictable economics while reinforcing better health outcomes.
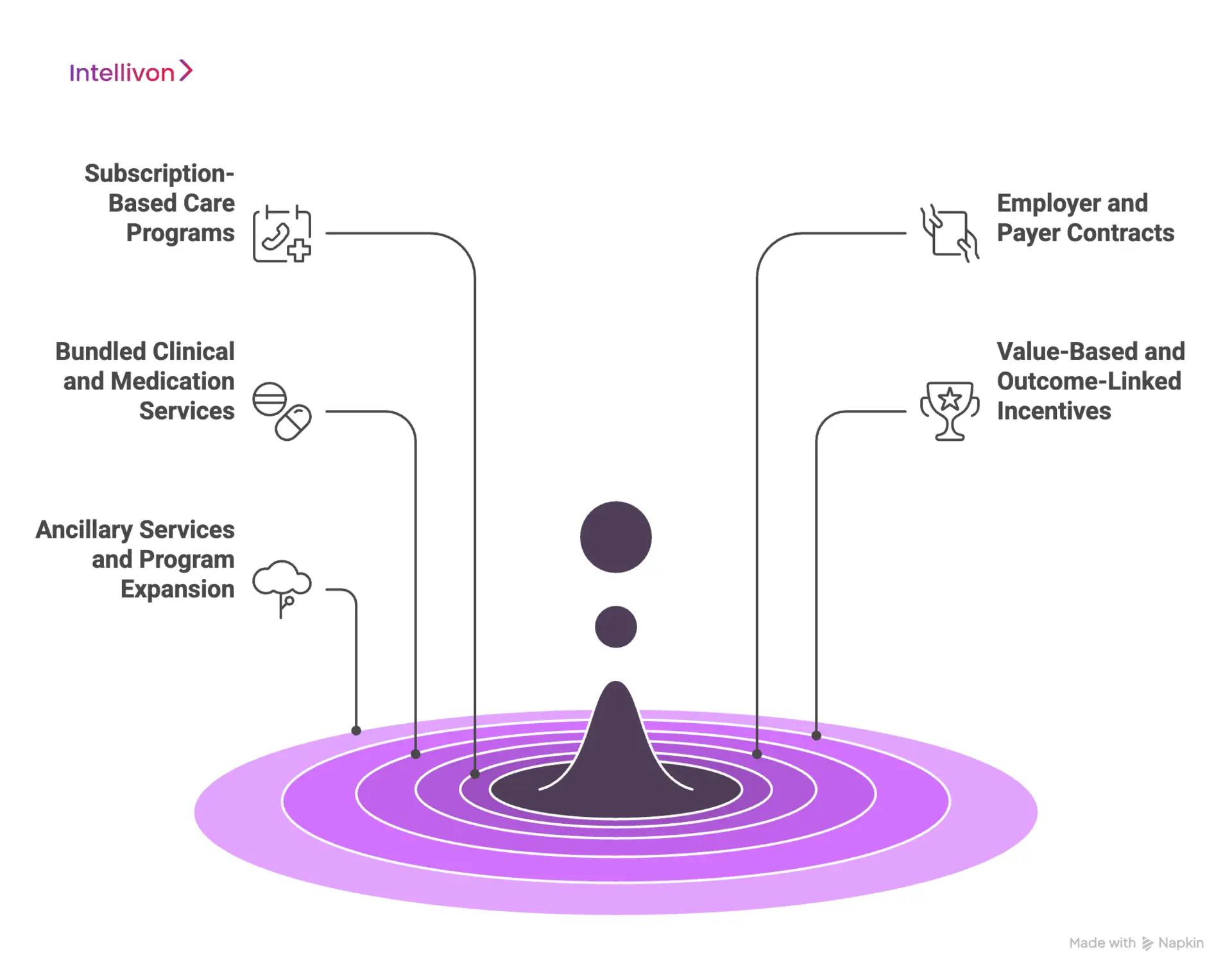
1. Subscription-Based Care Programs
Most chronic care platforms rely on recurring subscription fees. These fees cover ongoing access to care teams, monitoring, and support. Therefore, revenue remains stable even when visit frequency fluctuates.
This model encourages proactive care. It also aligns financial incentives with long-term condition management rather than short-term utilization.
2. Employer and Payer Contracts
Revenue is often driven by enterprise contracts with employers or health plans. Programs are offered as part of employee benefits or covered care pathways.
As a result, enrollment scales at the population level instead of relying only on individual sign-ups. This approach improves risk pooling and lowers customer acquisition costs.
3. Bundled Clinical and Medication Services
Care delivery, prescriptions, and diagnostics are frequently bundled into a single price.
Consequently, platforms capture value across the care continuum instead of isolated touchpoints. Bundling also simplifies billing for enterprises while improving care coordination.
4. Value-Based and Outcome-Linked Incentives
Some platforms participate in performance-based arrangements. Revenue increases when programs demonstrate measurable improvements in chronic outcomes or cost reduction.
Therefore, clinical success directly influences financial upside. This model strengthens trust with enterprise buyers focused on ROI.
5. Ancillary Services and Program Expansion
Additional revenue can come from expanding into new conditions, populations, or service lines. Over time, platforms grow horizontally without redesigning core infrastructure.
Telemedicine platforms like 9amHealth earn revenue by owning long-term care relationships. When economics reward continuity and outcomes, chronic care telemedicine becomes both financially durable and clinically effective.
Conclusion
Chronic care telemedicine has reached a turning point. What once functioned as a digital access layer is now expected to deliver measurable, long-term outcomes across complex populations. That shift demands more than virtual visits, reminders, or standalone AI tools. It requires systems that are designed for continuity, governance, and scale from the outset.
Platforms like 9amHealth illustrate what becomes possible when chronic care is treated as a service line rather than a feature. However, replicating that success inside large enterprises requires a different level of architectural discipline. Integration with existing EHRs, protection of legacy data, clear clinical accountability, and auditable AI are no longer optional. They are foundational.
For enterprise leaders, the real decision is not whether to invest in chronic care telemedicine. It is whether to build something that survives growth, scrutiny, and long-term use. When designed correctly, these platforms do more than reduce costs. They improve outcomes, stabilize operations, and create a scalable foundation for future care models.
Build Your Chronic Care Telemedicine Platform With Intellivon
At Intellivon, we build chronic care telemedicine platforms as enterprise operating systems, not virtual care tools layered on top of existing workflows. Our platforms are designed to govern how patients are enrolled into long-term care, how chronic conditions are managed over time, and how accountability is maintained across AI-assisted workflows, clinical teams, and enterprise infrastructure.
Each solution is engineered for healthcare organizations operating at scale. Platforms are infrastructure-first, compliance-led, and designed to support longitudinal care, remote monitoring, and condition-specific service lines. As programs grow across populations, regions, and benefit models, data integrity, clinical oversight, and operational control remain intact.
Why Partner With Intellivon?
- Chronic-care-first platform architecture aligned with continuity, outcomes, and service-line ownership
- Deep interoperability expertise across EHRs, RPM systems, PBMs, identity platforms, and enterprise analytics stacks
- Compliance-by-design delivery supporting HIPAA, audit readiness, role-based access, and governed AI usage
- AI-assisted orchestration that strengthens care coordination without replacing clinical judgment
- Enterprise delivery model with phased rollout, KPI-led validation, and controlled scale across conditions and populations
Talk to Intellivon’s healthcare platform architects to explore how an enterprise-grade chronic care telemedicine platform can integrate into your existing systems, protect legacy data, improve long-term outcomes, and scale safely without introducing operational or regulatory risk.
FAQs
Q1. What is a chronic care telemedicine platform?
A1. A chronic care telemedicine platform is a system designed to manage long-term conditions through continuous care, monitoring, and coordination. Unlike standard telehealth, it supports longitudinal engagement, integrates with EHRs, and aligns care delivery with outcomes rather than single visits.
Q2. How is chronic care telemedicine different from regular telehealth?
Traditional telehealth focuses on one-off virtual visits. Chronic care telemedicine manages conditions over time using structured care pathways, remote monitoring, and ongoing clinical oversight. The difference lies in continuity, governance, and outcome measurement.
Q3. Can chronic care telemedicine platforms integrate with existing EHR systems?
A3. Yes. Enterprise-grade platforms are built to integrate with EHRs using standards like HL7 and FHIR. They typically read and coordinate data without altering legacy records, ensuring data integrity while supporting virtual and in-person care workflows.
Q4. How does AI improve chronic care telemedicine platforms?
A4. AI supports intake summarization, risk stratification, engagement timing, and early issue detection. It reduces operational load and helps care teams prioritize patients, while clinicians retain full authority over diagnosis and treatment decisions.
Q5. How long does it take to build a chronic care telemedicine platform?
Most enterprises launch a focused MVP within a few months, then expand in phases. Timelines depend on integration depth, governance requirements, and the number of conditions supported. A phased approach helps validate outcomes before scaling.






