Healthcare’s interoperability problem is expensive. Hospitals repeat tests because they can’t access patient records, and administrative work eats up a quarter of healthcare spending. Fora large health system, their current integration setup blocks new partnerships and care models.
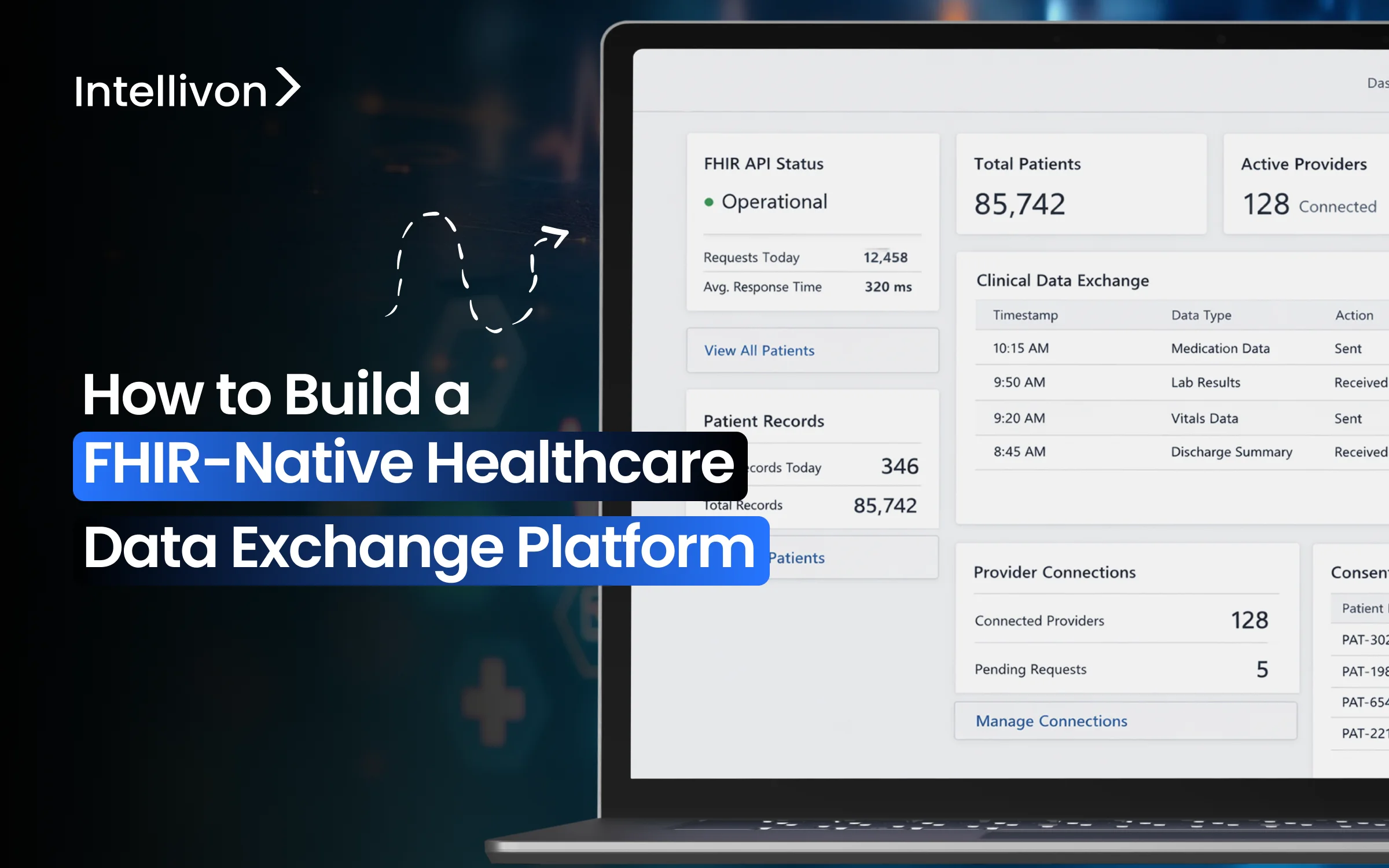
We at Intellivon have built FHIR-native data exchange platforms for large healthcare organizations. The mistake that we keep seeing is that they treat FHIR as just a technical standard instead of an enterprise-wide system that needs to work across your entire organization.
The platforms that work do more than move data around. They have security models that your CISO will approve, governance frameworks that your clinical teams trust, and performance that supports patient care when seconds matter.
In our experience, we have learned what makes FHIR platforms succeed in production versus fail after millions spent. This guide explains those decisions, where we touch upon what separates functional systems from expensive proofs-of-concept, and understand exactly what your organization needs to build a FHIR platform that delivers real interoperability without creating new risks or bottlenecks.
Why You Should Invest In FHIR-Native HIE Platforms Now
FHIR-native healthcare data exchange platforms make it easier for healthcare organizations to share clinical data across systems. As data-sharing regulations tighten, these platforms are becoming essential for large enterprises.
By using a common data standard, they remove long-standing data silos and improve coordination across hospitals, labs, and insurers. Therefore, many enterprises are now adopting them as a core part of their digital strategy.
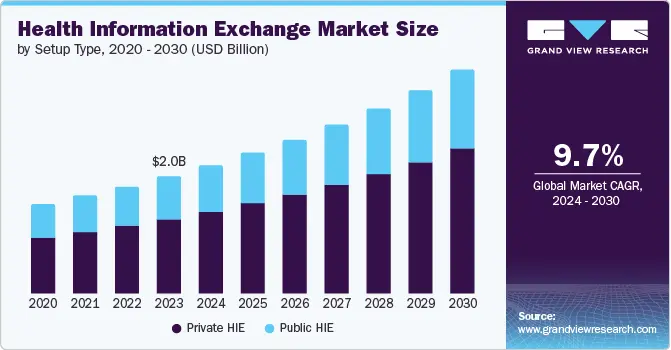
Market trends now show rapid enterprise adoption, driven by both compliance pressure and the need for scalable digital infrastructure. In fact, according to a Grand View Research report, the global health information exchange (HIE) market was valued at about USD 2 billion in 2023 and is expected to grow to nearly USD 4 billion by 2030.
Must-Read Market Insights:
- New regulations such as the 21st Century Cures Act are pushing healthcare organizations to move from older data formats to FHIR-based data sharing.
- FHIR-based platforms are enabling much faster system integrations, often reducing integration timelines by 50–60%, while also supporting new care coordination apps.
- Growing demand for value-based care and AI-driven analytics is driving steady enterprise investment in hybrid FHIR deployments across healthcare systems.
1. FHIR Adoption Is Now Mainstream
FHIR usage continues to grow steadily across global healthcare systems. In 2025, FHIR was used in about 71% of key healthcare data exchange use cases, up from 66% the year before.
In addition, nearly 90% of health systems are expected to support FHIR APIs by the end of the year. This clearly shows that FHIR is becoming standard healthcare infrastructure.
2. Regulations Are Accelerating FHIR-Based Exchange
Regulatory support is strongly reinforcing this shift. Today, around 73% of countries with national e-health exchange policies either mandate or actively recommend FHIR. As a result, healthcare organizations are are adopting FHIR to remain compliant and future-ready in a tightening regulatory environment.
3. Vendors and Platforms Shaping the FHIR Ecosystem
Several technology providers are shaping today’s interoperability landscape. Established vendors such as Epic Systems, Oracle Cerner, InterSystems, Veradigm, Orion Health, and MEDITECH hold a major share of health information exchange deployments.
In addition, cloud platforms like Microsoft Azure Health Data Services and integration layers such as Redox are enabling scalable, enterprise-grade FHIR integration.
FHIR Standards Are Maturing Alongside Enterprise Needs
From a standards perspective, FHIR R4 remains the most widely used version today. However, R4B and R5 are gaining traction for more advanced workflows. These include real-time subscriptions, bulk data access, and complex care coordination.
This evolution shows that FHIR is maturing in parallel with enterprise platform requirements.
What is an Enterprise Healthcare Data Exchange Platform?
An enterprise healthcare data exchange platform is the system that allows health information to move securely and consistently across different parts of a healthcare organization and its external partners.
Instead of keeping data locked inside individual systems, this platform creates a shared layer where information can flow between hospitals, clinics, labs, insurers, and digital health applications.
For example, when a patient moves from a clinic to a hospital, their medical history, lab results, and medications can follow them without manual intervention. This reduces delays and avoids errors.
In addition, enterprise data exchange platforms enforce security, consent, and audit rules at scale. As a result, organizations can expand their digital services without increasing compliance risk or operational complexity.
What Makes a Healthcare Data Exchange Platform FHIR-Native?
A FHIR-native healthcare data exchange platform is built with FHIR at its core, not added later as a connector or translation layer.
Instead of moving documents or files, it shares structured health data through standard APIs. This allows systems to request only the information they need, when they need it. As a result, data becomes easier to use across clinical, financial, and operational workflows.
Because FHIR defines a common way to represent healthcare data, different systems can understand each other without heavy customization. Therefore, new partners and applications can connect faster and with fewer integration issues.
Mandatory FHIR Rules and Requirements Enterprises Must Account For
FHIR-native platforms must operate within a clear regulatory and technical framework. These rules are no longer optional. They directly shape how healthcare data exchange platforms are designed and deployed across large enterprises.
Understanding these requirements early helps avoid costly redesigns and compliance failures later.
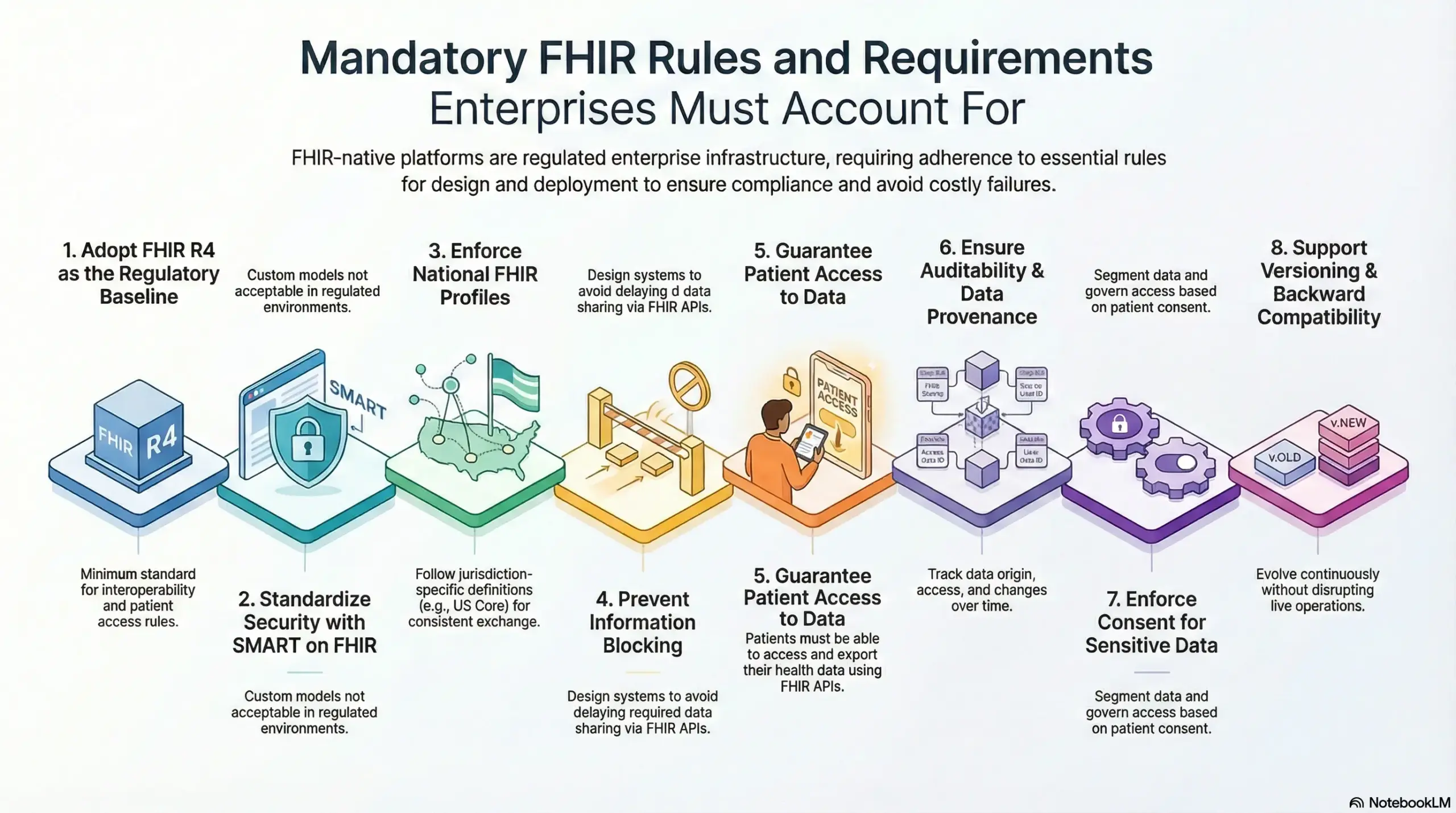
1. FHIR R4 as the Regulatory Baseline
Today, most healthcare regulations require platforms to support FHIR R4 as a minimum standard. This applies across US interoperability rules, CMS patient access requirements, and many national digital health programs worldwide.
Therefore, any platform that does not support FHIR R4 already faces compliance and integration risk.
2. Standardized Security Through SMART on FHIR
FHIR APIs must now follow the SMART on FHIR security model, which is built on OAuth2 authorization. This applies to patient-facing apps, third-party integrations, and enterprise API ecosystems.
As a result, custom or proprietary security models are no longer acceptable in regulated environments.
3. National FHIR Profiles Must Be Enforced
FHIR implementations must align with national core profiles such as US Core, UK Core, AU Base, and Canada Health Infoway profiles. This means enterprises cannot freely design their own data structures.
They must follow jurisdiction-specific definitions to ensure consistent and interoperable data exchange.
4. Preventing Information Blocking Under the Cures Act
The 21st Century Cures Act requires organizations to avoid delaying or restricting access to data that should be shared via FHIR APIs. This applies to providers, health IT vendors, and HIE operators.
Therefore, FHIR platforms must be designed to prevent unintentional data blocking caused by system limitations or access constraints.
5. Patient Access to Data via FHIR APIs
Patients must be able to access and export their health data using standardized FHIR APIs. This is now required under US CMS rules and many global digital health policies.
Consequently, data exchange platforms must support patient-mediated access, not only internal enterprise workflows.
6. Auditability and Data Provenance
FHIR platforms must track where data comes from, who accessed it, and how it changed over time. These requirements apply under HIPAA, GDPR, and national health data protection laws.
Without built-in audit trails, enterprises face serious legal and operational exposure.
7. Consent Enforcement for Sensitive Data
Sensitive data such as mental health records, HIV status, substance use, and genetic information must be segmented and governed by consent. This applies under HIPAA Part 2, GDPR, and country-specific privacy laws.
Therefore, FHIR-native platforms must enforce access at the data level, not only at the user level.
8. Versioning and Backward Compatibility
Certified health IT platforms must support version upgrades while maintaining backward compatibility. FHIR implementations cannot remain static. They must evolve continuously without disrupting live enterprise operations.
These requirements make it clear that FHIR-native platforms are regulated enterprise infrastructure rather than just technical systems. Therefore, compliance must shape architecture from the start, not be added later.
What Enterprise Outcomes a FHIR-Native Exchange Platform Unlocks
A FHIR-native healthcare data exchange platform changes how a healthcare enterprise runs, scales, and delivers value.
When data moves easily and consistently across systems, many long-standing operational and strategic challenges begin to ease. Below are the key outcomes enterprises see when this foundation is in place.
1. Faster System and Partner Integration
With FHIR-native APIs, new systems and partners can connect without heavy custom work. Therefore, enterprises spend less time building interfaces and more time delivering services. This shortens project timelines and reduces integration costs.
2. Clearer Business and Clinical Visibility
When data is standardized across platforms, leaders get a more reliable view of operations and care delivery. As a result, reports improve, decisions become faster, and planning is based on real-time insights rather than delayed information.
3. Smoother Day-to-Day Operations
FHIR-native exchange reduces the need to search across disconnected systems. Teams spend less time reconciling data and more time acting on it. Consequently, workflows become faster and less error-prone across departments.
4. Stronger Compliance and Risk Control
Because access, consent, and audit rules are enforced at the data level, enterprises can scale digital services without increasing regulatory risk. This creates confidence when expanding into new markets or launching new applications.
5. A Platform for Future Growth
AI, advanced analytics, patient apps, and new care models all depend on accessible and well-governed data. A FHIR-native exchange platform supports these initiatives without requiring core system replacements each time.
In practice, a FHIR-native exchange platform turns data sharing from an operational burden into a strategic advantage. Therefore, it becomes a foundation not only for efficiency, but also for long-term growth.
16 Minutes Per Visit on EHRs Highlights Workflow Inefficiencies
Clinical studies show that physicians spend around 16 minutes per patient visit interacting with electronic health records. This number comes from observational research published on PubMed and reinforced by broader health IT time-motion studies. On the surface, this may appear like a usability issue. However, when viewed through an enterprise lens, it reveals a deeper data workflow problem.
This time is largely consumed by searching for information, navigating fragmented records, and reconciling data from multiple systems.
1. Why Clinicians Are Spending So Much Time on EHRs
Most EHR platforms were designed to store data, not move it efficiently across care environments. As a result:
- Patient information often sits across multiple systems
- Data must be manually pieced together during each encounter
- Clinicians spend time locating and validating information instead of acting on it
Therefore, the issue is not simply interface design. It is how data is structured, accessed, and shared across the enterprise.
2. What This Means for Healthcare Enterprises
When clinicians spend 16 minutes per visit on EHR tasks, the impact goes far beyond productivity loss.
It directly affects:
- Appointment throughput
- Care quality and responsiveness
- Provider burnout and turnover
- Operational costs tied to inefficiency
In addition, this time burden scales with volume. As patient loads increase, so does the cost of fragmented data access.
3.FHIR-Native Data Exchange Changes This Dynamic
A FHIR-native healthcare data exchange platform addresses this problem at its root. By enabling standardized, API-driven access to clinical data across systems, it allows:
- Faster retrieval of complete patient records
- Reduced manual searching and reconciliation
- Real-time access to labs, medications, and history
- Consistent data views across care teams
As a result, clinicians spend less time navigating systems and more time delivering care.
Why This Matters Strategically
For enterprise leaders, the 16-minute statistic is a signal that data architecture is directly shaping workforce efficiency, cost structures, and care delivery outcomes.
Fixing workflows at the application layer alone will not solve this. The solution lies in rethinking how healthcare data moves across the organization.
That is precisely where FHIR-native healthcare data exchange platforms become a strategic investment rather than a technical upgrade.
Reference Architecture of a FHIR-Native Healthcare Data Exchange Platform
A FHIR-native healthcare data exchange platform is not a single system. It is a layered architecture where each part plays a clear role in making data flow safely, reliably, and at scale.
Understanding these layers helps enterprises see how interoperability becomes an operational capability, not just a technical feature.
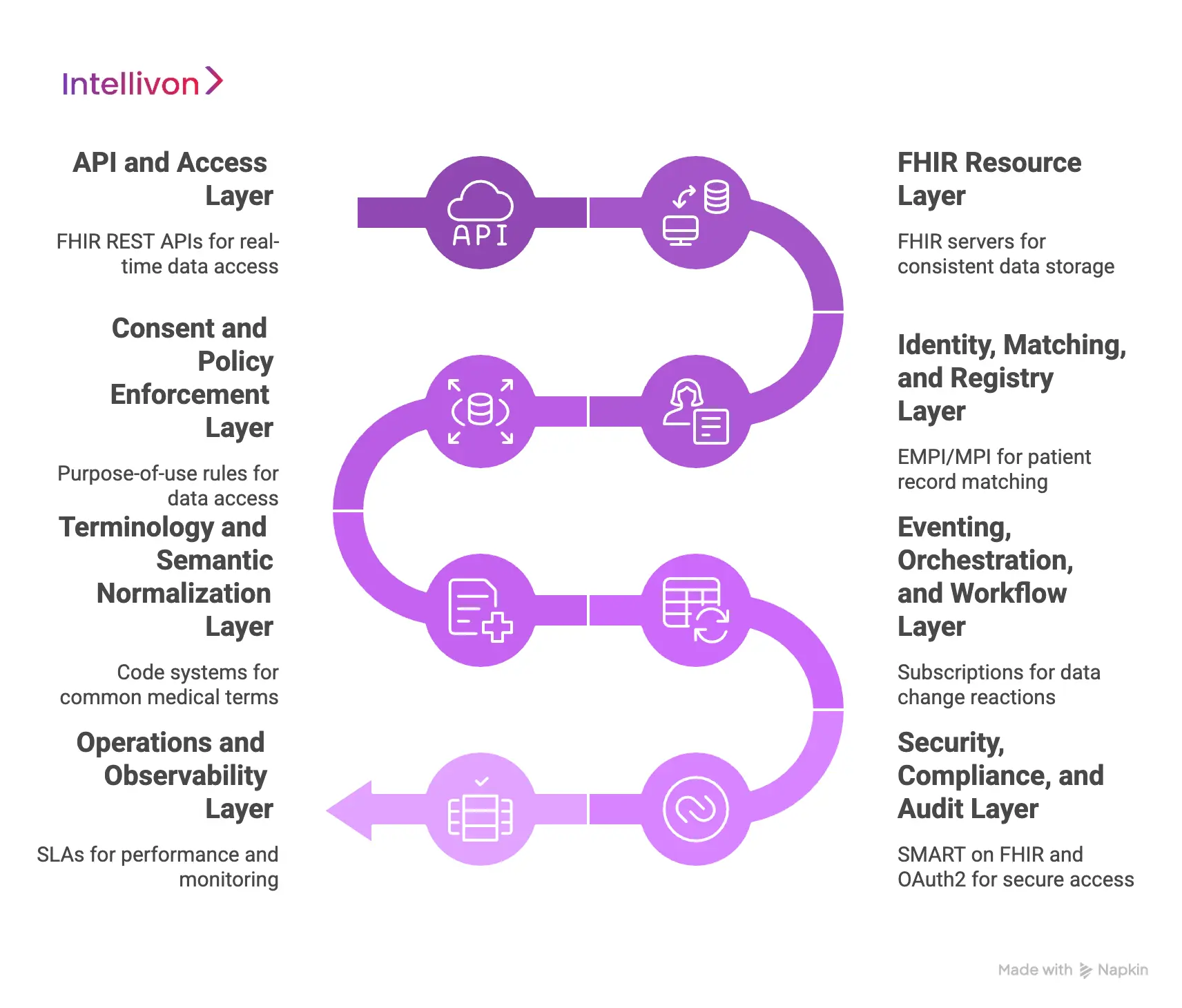
1. API and Access Layer
This is how systems and applications connect to the platform.
FHIR REST APIs allow applications to request and update specific pieces of health data in real time. In addition, subscription and event APIs enable systems to receive updates when data changes. Bulk data APIs support analytics, population health, and AI pipelines.
Alongside these, identity, registry, consent, and policy APIs ensure that access is controlled and traceable.
Hybrid integration APIs also allow the platform to connect with older systems using HL7 v2, CDA, or DICOM, which is essential in large enterprises.
2. FHIR Resource Layer
This layer stores and manages healthcare data using FHIR structures. FHIR servers hold the data in a consistent format. Profiles and validation rules ensure that incoming data meets enterprise and regulatory requirements.
A versioning strategy allows the platform to evolve without breaking existing integrations. Resource lifecycle governance controls how data is created, updated, and retired over time.
3. Identity, Matching, and Registry Layer
This layer ensures that the platform knows who and what the data refers to.
EMPI or MPI systems match patient records across different sources. Record locator services track where a patient’s data exists across the network. Provider and organization registries define trusted participants in the exchange.
Without this layer, data exchange becomes unreliable, even if the APIs work perfectly.
4. Consent and Policy Enforcement Layer
This layer decides who can access what data and why. Purpose-of-use rules ensure data is used only for approved reasons. Resource-level access decisions allow fine control over what data is shared.
Sensitive data segmentation ensures that highly confidential information is handled with additional care. Therefore, compliance becomes part of the platform, not an external control.
5. Terminology and Semantic Normalization Layer
This layer ensures that data means the same thing everywhere. Code systems and value sets define common medical terms. Mapping and normalization align different vocabularies across systems.
As a result, analytics and AI can work on consistent data rather than conflicting definitions.
6. Eventing, Orchestration, and Workflow Layer
This layer connects data movement to real workflows. Subscriptions allow systems to react when data changes.
Routing and retries ensure data reaches the right place even during failures. Workflow triggers connect data events to operational actions such as alerts or care coordination tasks. This is where data exchange becomes operational, not just technical.
7. Security, Compliance, and Audit Layer
This layer protects the platform and builds trust. SMART on FHIR and OAuth2 manage secure access. Audit trails record who accessed what and when. Data residency controls ensure information stays in approved regions.
Breach traceability enables rapid response to incidents. Together, these elements make the platform defensible in audits and investigations.
8. Operations and Observability Layer
This layer ensures the platform runs reliably day after day. SLAs define expected performance. Monitoring provides visibility into system health. Incident response processes handle failures quickly.
Partner certification and onboarding ensure new participants meet platform standards before going live. Without this layer, even well-designed platforms struggle at enterprise scale.
Data Flows A FHIR-Native Exchange Platform Supports
A FHIR-native healthcare data exchange platform becomes valuable only when it supports real, day-to-day data movement across the enterprise.
These data flows are not theoretical. They directly shape how care is delivered, managed, and scaled across healthcare systems.
Below are the core data flows such platforms are built to handle.
1. Core Clinical Data Exchange
This includes patient details, encounters, medications, allergies, and clinical observations.
With FHIR-native exchange, this information moves easily between systems such as EHRs, specialist platforms, and care management tools. As a result, clinicians work with a complete and up-to-date patient record instead of fragmented views.
2. Care Coordination and Referrals
This flow supports referrals, care plans, and discharge summaries. When these move across organizations without manual effort, transitions of care become smoother.
Therefore, patients face fewer delays and providers avoid unnecessary follow-ups caused by missing information.
3. Diagnostics and Results
This covers lab results, imaging reports, and pathology findings. FHIR-native exchange ensures that results reach the right system and care team quickly.
Consequently, repeat tests reduce and treatment decisions happen faster.
4. Patient-Mediated Data Sharing
This enables patients to access and share their longitudinal records across providers.
Because sharing is driven by consent, patients remain in control of their data. In addition, this supports portability when patients move between regions or care networks.
5. Payer and Administrative Workflows
This includes eligibility checks, prior authorizations, and clinical attachments linked to claims.
When this data flows smoothly between providers and payers, billing cycles shorten and disputes reduce. As a result, revenue operations become more predictable.
6. Population Health and Public Health
This flow supports disease registries, public health reporting, and surveillance programs.
FHIR-native exchange allows health systems to report accurately and in near real time. Therefore, organizations can respond faster to public health needs and regulatory reporting requirements.
7. AI, Analytics, and Secondary Data Use
This covers de-identified data pipelines, research-ready datasets, and real-time feeds for AI models.
When data is standardized and governed, advanced analytics becomes possible without complex data preparation. Consequently, enterprises can innovate while maintaining compliance and data integrity.
Together, these data flows turn a FHIR-native exchange platform into a core operational system rather than a background integration layer. Therefore, data exchange becomes an enabler of care, efficiency, and innovation across the enterprise.
How We Build A FHIR-Native Healthcare Data Exchange Platform
At Intellivon, we build FHIR-native healthcare data exchange platforms as regulated enterprise infrastructure. The work is structured, measurable, and designed for real operating conditions, so enterprises can scale interoperability without creating new risk.
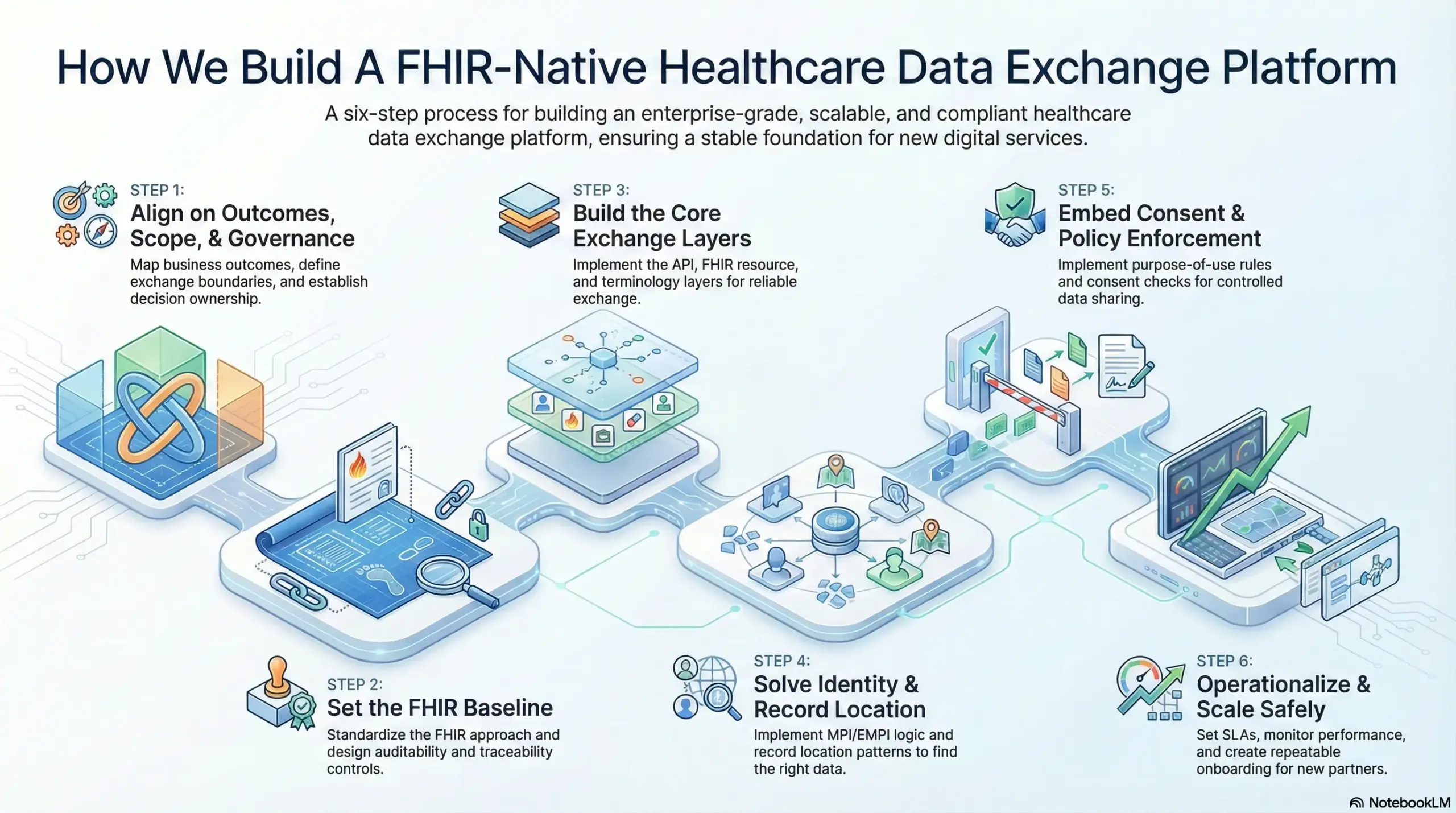
Step 1: Align on outcomes, scope, and governance
We start by mapping the business outcomes the platform must deliver, such as faster partner onboarding, safer data access, or better reporting. In addition, we define the exchange boundaries early so the build stays controlled.
We establish decision ownership across IT, compliance, and operations, therefore the platform does not become an “IT-only” project. Our experts also lock initial success metrics, so progress stays visible and practical.
Step 2: Set the FHIR Baseline
Next, we standardize the FHIR approach using FHIR R4 and the right jurisdiction profiles, so the platform stays aligned with policy requirements. We define validation rules, versioning strategy, and the minimum dataset needed for priority workflows.
In parallel, we design auditability, traceability, and data residency controls, because these are hard to bolt on later. This ensures the platform stays audit-ready as it scales.
Step 3: Build the Core Exchange Layers
We then implement the core architecture layers that make exchange reliable in production. This includes the API and access layer, the FHIR resource layer, and the terminology and normalization layer.
In addition, we set up eventing patterns so systems can receive updates without manual polling. The goal is simple: data should move consistently, and systems should understand it the same way every time.
Step 4: Solve Identity and Record Location
Identity is where many exchange programs break, so we treat it as a primary workstream. We implement MPI or EMPI logic, matching thresholds, and workflows for exceptions, so teams can resolve mismatches fast.
At the same time, we also establish record location patterns so the platform can find where data lives across participants. As a result, clinicians and systems receive the right record, not just a record.
Step 5: Embed Consent and Policy Enforcement
Once data starts flowing, governance must scale with it. We implement purpose-of-use rules, consent checks, and resource-level access decisions, so sharing stays controlled across partners and apps.
Sensitive data segmentation is handled explicitly, therefore privacy requirements do not become operational blockers. This approach keeps data exchange flexible while staying compliant.
Step 6: Operationalize and Scale Safely
Finally, we treat the platform like a product that must run every day, not a one-time delivery. We set SLAs, monitoring, and incident response practices, so reliability is measurable and managed.
At the same time, we also create repeatable onboarding and certification steps for new partners, which reduces integration time and surprises. Over time, the platform becomes a stable foundation for new digital services, analytics, and AI programs.
This step-by-step approach helps enterprises move from fragmented integrations to a governed, FHIR-native healthcare data exchange platform that can grow with the organization. Therefore, interoperability becomes a long-term capability that supports both operational efficiency and new digital growth.
Cost Of Building A FHIR-Native Healthcare Data Exchange Platform
At Intellivon, FHIR-native healthcare data exchange platforms are built as regulated enterprise data infrastructure, not as integration layers added on top of existing systems. The focus remains on creating platforms that operate reliably across providers, payers, regions, and evolving healthcare regulations. Every architectural decision accounts for governance, identity resolution, security, and long-term interoperability risk from the start.
When budget constraints exist, scope is refined with intent. However, core elements such as compliance controls, consent enforcement, identity services, auditability, and data provenance are never reduced. Therefore, enterprises avoid expensive remediation and redesign cycles after launch. Predictability replaces rework, and long-term ROI remains protected.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Regulatory Alignment | Use case definition, data exchange scope, jurisdiction mapping, compliance assessment | $8,000 – $14,000 |
| FHIR-Native Architecture Design | Layered platform design, FHIR R4 modeling, API and security patterns | $10,000 – $18,000 |
| Governance & Policy Framework | Consent logic, access policies, audit workflows, exception handling | $9,000 – $16,000 |
| Core Platform Development | FHIR servers, terminology services, eventing, normalization layers | $18,000 – $32,000 |
| Enterprise Integrations | EHRs, LIS, RIS, payer systems, registries, legacy HL7/CDA | $16,000 – $30,000 |
| Role-Based Interfaces & Access | Admin, compliance, operations, and partner interfaces | $10,000 – $18,000 |
| Security & Compliance Controls | Encryption, authorization, audit trails, breach traceability | $10,000 – $18,000 |
| Testing & Compliance Validation | Functional testing, security testing, regulatory readiness | $7,000 – $12,000 |
| Deployment & Scale Readiness | Cloud or hybrid setup, monitoring, performance tuning | $8,000 – $14,000 |
Total initial investment: $96,000 – $192,000
Ongoing maintenance and optimization: ~15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped FHIR-native exchange programs face pressure when indirect cost drivers are ignored. Planning for these early protects budgets, timelines, and compliance posture as data volume grows.
- Integration complexity increases as new EHRs, labs, and partner systems are added
- Compliance overhead grows due to audits, regulatory updates, and reporting needs
- Governance requires continuous policy tuning and consent model adjustments
- Infrastructure costs rise with analytics, AI workloads, and real-time data flows
- Change management includes onboarding clinical, IT, compliance, and operations teams
- Continuous monitoring becomes critical as data sensitivity and access expands
Best Practices to Avoid Budget Overruns
Based on Intellivon’s experience delivering enterprise healthcare platforms, these practices consistently lead to controlled costs and predictable outcomes.
- Define the data exchange model and priority workflows before expanding scope
- Embed governance, consent, and auditability into the core architecture
- Use modular components that scale without platform redesign
- Plan interoperability early to avoid expensive retrofitting
- Maintain observability across performance, security, and compliance
- Design for regulatory evolution rather than one-time certification
Request a tailored proposal from Intellivon’s healthcare platform experts to receive a delivery roadmap aligned with your budget constraints, regulatory exposure, and long-term FHIR-native interoperability strategy.
What Most FHIR-Based HIE Projects Get Wrong (and How to Avoid It)
Many healthcare organizations invest in FHIR-based HIE projects with the right intent but still struggle to see enterprise-level impact. The issue is rarely with FHIR itself. It usually comes from how the platform is designed, governed, and scaled across real operating environments.
Below are some of the most common challenges we see and how Intellivon helps enterprises avoid them.
1. Treating FHIR as a Data Format Instead of a Platform
A frequent mistake is using FHIR only as a way to convert data between systems while keeping the underlying architecture unchanged. In these cases, the enterprise still operates on disconnected systems, only with a modern interface layered on top. This limits scalability and makes future expansion expensive and slow.
At Intellivon, we treat FHIR as the core platform model rather than a translation layer. APIs, governance, and security are structured around FHIR from the beginning so interoperability becomes a foundation instead of a temporary solution. As a result, enterprises build systems that are easier to grow and adapt over time.
2. Delaying Identity Resolution Until After Integration
Many projects focus first on connecting systems and only address patient identity once problems appear. This approach leads to duplicate records, mismatches, and declining trust in exchanged data. Once these issues surface, fixing them becomes disruptive and costly. Intellivon treats identity as a primary design layer, not something to be handled later.
We implement matching logic, resolution workflows, and data quality controls early in the build. Therefore, the platform maintains data reliability as the network expands.
3. Treating Consent and Governance as Application-Level Concerns
Some FHIR platforms push consent management and access control into individual applications instead of handling them at the exchange level. This works briefly but breaks down as more partners and systems connect. Sensitive data then becomes difficult to control consistently across the enterprise.
At Intellivon, governance is embedded into the data exchange platform itself. Consent rules, purpose-of-use controls, and access decisions operate directly on the data layer. Consequently, compliance scales naturally as the platform grows.
4. Underestimating Operational Ownership After Go-Live
Another common issue is assuming the platform will run smoothly once it is deployed. In reality, enterprise data exchange requires continuous monitoring, onboarding, and incident management. Without this, performance degrades and trust in the platform drops.
Intellivon designs platforms with operational ownership in mind from day one. We define SLAs, observability, and partner onboarding processes as part of the core delivery. This ensures the platform remains reliable long after launch.
Most failures in FHIR-based HIE projects are architectural and operational in nature. By addressing these challenges upfront, enterprises can turn FHIR-native platforms into long-term assets rather than recurring problems.
Top Examples Of Enterprises Using FHIR-Native HIE
Looking at how leading healthcare enterprises approach FHIR-based interoperability helps clarify what a FHIR-native exchange platform looks like in practice. These examples are not meant as product comparisons.
They demonstrate architectural patterns that large enterprises are already using to make healthcare data exchange reliable, scalable, and operational.
1. Epic Care Everywhere
Epic Care Everywhere operates as a large-scale clinical data exchange network across healthcare organizations. Architecturally, it shows how interoperability must work beyond single systems and into multi-organization networks.
It relies on standardized data exchange patterns, patient identity matching, and trust frameworks that allow hospitals on different Epic instances to share patient records securely. What this demonstrates is that a true healthcare data exchange platform must be designed to operate across organizational boundaries, not just within one enterprise.
It also highlights the importance of governance and routing logic when data moves across regional or national networks.
2. CommonWell Health Alliance
CommonWell functions as a shared interoperability infrastructure rather than a single enterprise product. It provides services such as record location, identity resolution, and trusted data routing across multiple EHR vendors.
Architecturally, this demonstrates that large-scale exchange requires platform-level services that every participant can rely on, not just APIs between two systems. The key lesson here is that identity services, registries, and network-level governance must exist independently of any single application.
This aligns closely with how FHIR-native exchange platforms must be built for multi-partner ecosystems.
3. Oracle Health (Cerner) Interoperability APIs
Oracle Health exposes FHIR-based APIs that allow external systems and applications to access clinical data in a standardized way. This shows how interoperability is shifting from document-based sharing to API-driven data access.
Architecturally, it demonstrates that modern healthcare platforms must behave like digital platforms rather than closed systems. External apps, analytics tools, and patient-facing services can connect through APIs instead of custom integrations.
For enterprises, this reinforces the need for an API-first exchange layer that supports extensibility without breaking core systems.
4. Cloud FHIR Platforms (Azure Health Data Services and Google Healthcare API)
Cloud-native FHIR platforms illustrate how FHIR is becoming a data infrastructure model, not just a data format. These platforms store healthcare data directly as FHIR resources and expose it through standardized APIs, while also supporting analytics, AI pipelines, and security controls.
Architecturally, this shows how FHIR-native exchange can be combined with scalable cloud services to support both real-time operations and advanced data use.
The key takeaway is that FHIR-native exchange is increasingly embedded into enterprise data platforms rather than sitting at the edges.
Together, these examples show that enterprises are already adopting platform-based, API-driven, and identity-aware models to make healthcare data move reliably at scale. The architectural patterns behind these implementations are what modern FHIR-native healthcare data exchange platforms must replicate and extend.
Conclusion
FHIR-native healthcare data exchange platforms are no longer future concepts. They are becoming the foundation for how healthcare enterprises operate, comply, and grow. When data flows safely and consistently across systems, organizations move faster, reduce risk, and unlock new digital capabilities.
However, success depends on building these platforms as regulated infrastructure, not as isolated integrations. This is where execution matters as much as vision.
At Intellivon, we help enterprises design and deliver FHIR-native platforms that scale with care models, regulatory change, and AI-driven transformation. The result is not just better interoperability, but a stronger, more resilient digital health ecosystem.
Build A FHIR-Native Healthcare Date Exchange Platform With Intellivon
At Intellivon, FHIR-native healthcare data exchange platforms are built as regulated enterprise data infrastructure, not as integration layers added onto fragmented systems. Every architectural and delivery decision prioritizes compliance, interoperability, and long-term platform stability. This ensures exchange platforms operate reliably across providers, payers, partners, and regions, not just during early deployment.
As data exchange programs expand across organizations, care networks, and digital services, stability becomes critical. Governance, performance, and audit readiness remain consistent as data volume and access complexity increase. Organizations retain control over identity, consent, and data flows without introducing fragmentation, regulatory exposure, or operational drag.
Why Partner With Intellivon?
- Enterprise-grade interoperability architecture designed for regulated healthcare ecosystems
- Proven delivery across multi-provider networks, digital health platforms, and payer-integrated systems
- Compliance-by-design approach with audit readiness and policy enforcement built i
- Secure, modular infrastructure supporting cloud, hybrid, and on-prem deployment
- AI-ready data foundations enabling analytics, automation, and intelligent care workflows with governance and oversight
Book a strategy call to explore how Intellivon can help you build and scale a FHIR-native healthcare data exchange platform with confidence, control, and long-term enterprise value.
FAQs
Q1. What is a FHIR-native healthcare data exchange platform?
A1. A FHIR-native healthcare data exchange platform is built with FHIR as its core data model and access layer. It enables real-time, API-driven sharing of clinical data across systems while enforcing security, consent, and audit controls at scale.
Q2. How is a FHIR-native exchange different from traditional HIE systems?
A2. Traditional HIEs focus on document transfer and batch workflows. A FHIR-native exchange supports structured, real-time data access through APIs, making it more suitable for modern care delivery, AI, and digital health ecosystems.
Q3. Is FHIR-native data exchange required for regulatory compliance?
A3. In many regions, yes. Regulations increasingly mandate standardized, API-based access to healthcare data. FHIR-native platforms help enterprises meet interoperability, patient access, and information-sharing requirements more reliably.
Q4. How long does it take to build a FHIR-native healthcare data exchange platform?
A4. Timelines vary by scope and maturity. Enterprises typically begin with a governed foundation in 8–12 weeks, followed by phased expansion across systems, partners, and workflows over several months.
Q5. Can a FHIR-native platform support AI and advanced analytics?
A5. Yes. Because data is structured, standardized, and governed, FHIR-native platforms provide a strong foundation for AI models, population health analytics, and real-time decision support without complex data rework.