Clinical operations today rely on data flowing continuously between EHRs, laboratories, care management systems, payer platforms, and digital health applications. No single system contains the complete clinical or operational context needed to provide care, manage risk, or meet regulatory requirements.
FHIR allows for standardized exchange between these systems. This makes integration a basic necessity rather than an optional feature. As care models, partner ecosystems, and digital services grow, the volume and complexity of integration also rise.
Without a platform approach, FHIR integrations can become disjointed, hard to manage, and increasingly fragile under operational stress. Identity resolution, consent enforcement, data normalization, and auditability need to work consistently across every exchange.
This blog draws from Intellivon’s experience in designing and running FHIR-based healthcare integration platforms as regulated systems. It reflects enterprise deployments where interoperability must scale reliably across systems and partners, without adding operational or compliance risks.
Key Takeaways Of The FHIR Healthcare Market
Recent market data shows the global FHIR solutions market growing from $3.2 billion in 2024 to $13.7 billion by 2033, at a 17.8% CAGR. The rapid growth of the FHIR solutions market reflects a shift from isolated integrations toward enterprise-grade FHIR integration platforms that can scale securely.
Additionally, the healthcare interoperability solutions market is projected to grow from $5.04 billion in 2025 to $9.57 billion by 2031, driven by regulatory mandates, cloud adoption, and demand for AI-ready clinical data exchange.
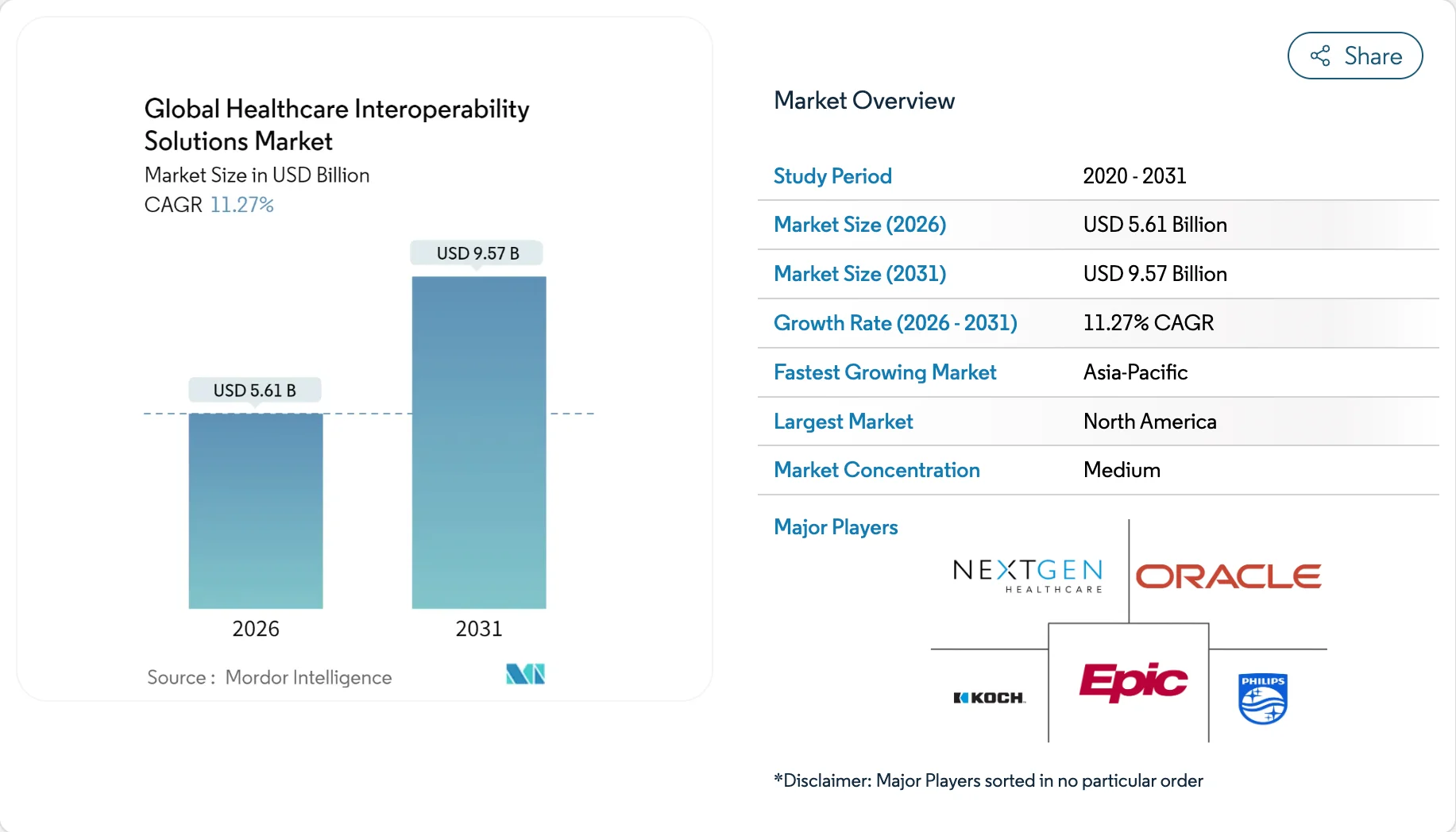
Market Insights:
- Recent data shows 71% of respondents now report active FHIR usage across at least some use cases, up from 66% in 2024, with nearly 90% of health systems expected to adopt FHIR APIs by 2025.
- Within the FHIR ecosystem, software accounts for 62% of total revenue, while services such as implementation and training are expanding rapidly at an 18.6% CAGR through 2033.
- In the broader healthcare interoperability market, revenues are projected to grow from $5.04 billion in 2025 to $5.61 billion in 2026, with software contributing 46% and cloud-based solutions representing 58% of total revenue.
Taken together, these trends point to a clear shift in how healthcare interoperability is being approached. As software platforms account for a larger share of investment and cloud-based deployments become the default, enterprises are prioritizing scalable, governed integration foundations over isolated services.
The continued growth of implementation and training services further reinforces that interoperability success depends not just on adopting standards like FHIR, but on building platforms that can be operationalized, governed, and scaled over time.
This market direction directly shapes how FHIR-based integration platforms must be designed and delivered.
What is an FHIR-Based Healthcare Integration Platform?
An FHIR-based healthcare integration platform is a system that allows healthcare applications to exchange data using the FHIR standard. FHIR defines how clinical data, such as patients, appointments, observations, and medications, are structured and shared. This makes data easier to access, understand, and reuse across systems.
In practice, an FHIR-based platform sits between EHRs, apps, and external services. It pulls data from source systems, applies access rules, and delivers information in a consistent format. As a result, applications do not need custom connections for every system they integrate with.
These platforms also handle security, consent, and identity controls. They ensure that data is shared only with authorized users and systems. In addition, they support versioning and change management as standards evolve.
For enterprises, an FHIR-based integration platform reduces complexity. It improves interoperability, lowers long-term maintenance effort, and supports scalable digital health programs.
How It Works
An FHIR-based healthcare integration platform follows a structured process to move data safely and consistently. Each step focuses on reducing complexity while preserving control.
As a result, applications receive reliable data without custom integrations. At the same time, governance and compliance remain enforced throughout the flow.
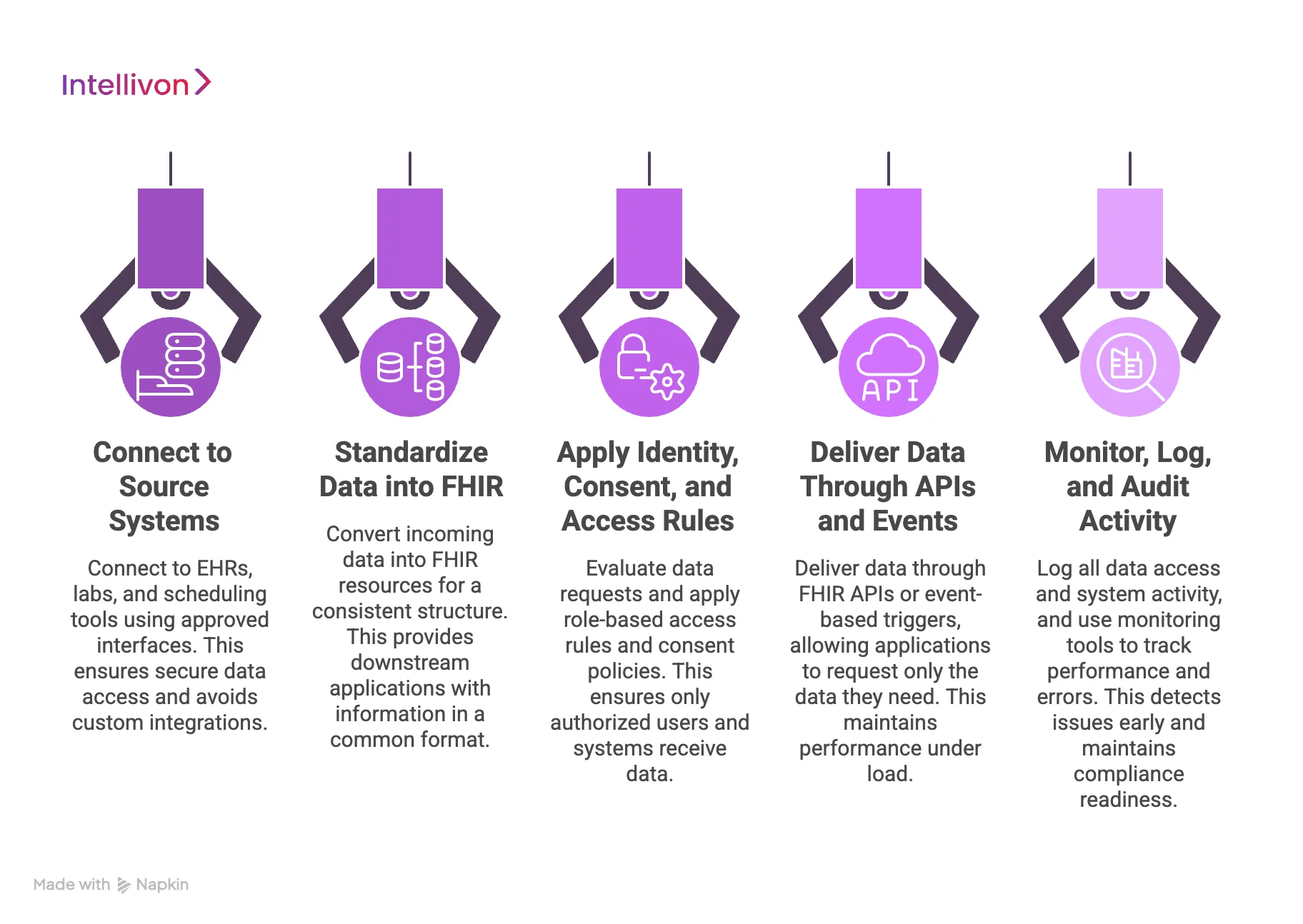
Step 1: Connect to Source Systems
First, the platform connects to source systems such as EHRs, labs, and scheduling tools. These connections use approved interfaces and authentication methods. Therefore, data access remains secure from the start.
At the same time, custom point-to-point integrations are avoided. As a result, onboarding new systems becomes faster and more predictable.
Step 2: Standardize Data into FHIR
Next, the platform converts incoming data into FHIR resources. This step creates a consistent structure for patient, clinical, and operational data. As a result, downstream applications receive information in a common format.
Therefore, teams avoid repeated transformation work. Over time, this reduces integration maintenance effort.
Step 3: Apply Identity, Consent, and Access Rules
Then, the platform evaluates who is requesting the data. It applies role-based access rules and consent policies consistently. As a result, only authorized users and systems receive data.
At the same time, compliance requirements remain enforced automatically. Therefore, security does not depend on application-level logic.
Step 4: Deliver Data Through APIs and Events
After access is approved, the platform delivers data through FHIR APIs or event-based triggers. Applications request only the data they need. As a result, performance remains stable under load.
In addition, real-time workflows can be supported when required. Therefore, both batch and live use cases are covered.
Step 5: Monitor, Log, and Audit Activity
Finally, the platform logs all data access and system activity. Monitoring tools track performance and errors continuously. As a result, teams detect issues early.
At the same time, audit trails remain available for review. Therefore, compliance readiness is maintained over time.
An FHIR-based integration platform works best when every step is planned together. When this happens, data flows stay reliable as scale increases. As a result, enterprises gain interoperability without losing governance or control.
FHIR App Access Reaches 70% of Hospitals, Forcing Platform-First Integration
FHIR app access has moved firmly into mainstream healthcare operations. In 2024, ASTP/ONC analysis reported that 70% of hospitals supported FHIR app access, while 81% enabled some form of app-based access across their systems.
This level of adoption signals a shift from experimentation to production use. FHIR APIs are now actively supporting patient-facing apps, clinical workflows, analytics tools, and third-party services at scale.
As app ecosystems expand, the volume and complexity of integration activity increase. Healthcare systems must manage more connections, more data requests, and more external consumers than earlier integration models were designed to handle.
1. App Access Increases Integration Demand
FHIR apps rely on continuous, real-time access to clinical data. Each new app introduces additional API traffic, authorization checks, and dependency chains across systems.
As the number of connected applications grows, integration patterns quickly move beyond simple request-and-response flows. Systems must coordinate access, enforce policies, and maintain performance across multiple consumers simultaneously.
Without a centralized integration platform, these demands often lead to inconsistent behavior, operational strain, and limited visibility into how data is being accessed and used.
2. Security and Governance Hard To Enforce
FHIR app access expands the attack surface of healthcare systems. Each application requires precise authorization scopes, role-based access controls, and clear boundaries around data usage.
Managing these controls individually across integrations increases the risk of misconfiguration. Inconsistent enforcement of consent, identity, and permissions can lead to compliance gaps and audit challenges.
A platform-first integration approach centralizes security and governance. It ensures that every app interaction follows the same access rules, consent policies, and audit standards.
3. Operational Reliability Is A Platform Concern
As FHIR app usage increases, operational reliability becomes critical. API rate limits, retry storms, and latency issues can impact clinical workflows if not handled correctly.
Point integrations often lack the tooling needed to manage failures gracefully. Teams struggle to detect issues early or recover quickly when problems occur.
An integration platform provides built-in monitoring, throttling, replay, and recovery mechanisms. These capabilities help maintain stable operations even as app usage scales.
4. Platform-first Integration Supports Long-Term Scalability
FHIR adoption continues to grow across healthcare ecosystems. App access will expand further as new care models, analytics initiatives, and AI-driven use cases emerge.
A platform-first integration model allows healthcare enterprises to scale without redesigning integrations repeatedly. It enables consistent onboarding of new applications while preserving governance, security, and performance.
As FHIR app access becomes the norm rather than the exception, integration platforms become the foundation that allows healthcare systems to grow safely and sustainably.
The widespread adoption of FHIR app access marks a turning point for healthcare integration. As app ecosystems expand, integration challenges shift from connectivity to control, reliability, and governance.
A platform-first approach enables healthcare enterprises to manage this shift effectively. It provides the structure needed to support growing app usage while maintaining compliance, operational stability, and long-term scalability.
Healthcare Use Cases That Justify Building FHIR Platforms
FHIR platforms are not needed for every healthcare project. However, certain use cases create enough complexity, scale, and long-term demand that building an FHIR-based platform becomes the most practical choice.
In these cases, direct integrations or one-off connections quickly become difficult to manage. Therefore, organizations turn to FHIR platforms to regain control, consistency, and speed.
1. Multi-EHR and Multi-System Interoperability
Healthcare organizations often operate more than one EHR or clinical system. As systems grow through mergers or partnerships, data fragmentation increases. An FHIR platform provides a common layer that connects systems in a consistent way.
As a result, applications do not need separate integrations for each system. Over time, this reduces maintenance effort. Therefore, interoperability becomes easier to scale.
2. Patient Access and Digital Front Doors
Patient-facing applications rely on timely and accurate data. Scheduling, records access, and messaging often pull information from multiple systems. An FHIR platform centralizes these data flows.
As a result, patient apps remain responsive and consistent. At the same time, access rules and consent are enforced centrally. Therefore, patient experience improves without adding risk.
3. Population Health and Care Coordination
Population health programs depend on data from many sources. Claims, clinical records, and outcomes data must be analyzed together. An FHIR platform standardizes this data before it reaches analytics tools.
As a result, insights become more reliable. In addition, data updates flow continuously. Therefore, care teams can act sooner and plan better.
4. Analytics, AI, and Reporting Pipelines
Advanced analytics and AI require clean and well-structured data. When data arrives in different formats, models perform poorly. An FHIR platform normalizes data before it enters analytics pipelines.
As a result, reporting becomes more accurate. At the same time, governance stays intact. Therefore, AI programs scale with fewer disruptions.
5. Third-Party App Enablement
Healthcare organizations often want to support multiple internal and external applications. Managing direct integrations for each app increases effort and risk. An FHIR platform acts as a controlled gateway for app access.
As a result, onboarding new apps becomes faster. In addition, access policies stay consistent. Therefore, innovation moves forward without losing control.
These use cases share one thing in common. They involve scale, multiple systems, and ongoing change. In such environments, one-off integrations create friction. FHIR platforms replace that friction with structure. As a result, healthcare organizations gain flexibility while maintaining governance and stability.
Architecture for a Secure, Scalable FHIR Integration Platform
A secure FHIR integration platform works best when it is built in clear layers. Each layer handles a specific responsibility and limits how problems spread across the system. As a result, changes in one area do not break the entire platform.
This structure also supports scale as data volume and usage increase. Therefore, layered architecture becomes essential for long-term stability.

1. Source System Layer
This layer connects the platform to EHRs, labs, and operational systems. It controls how data is pulled from each source using approved interfaces. As a result, source systems remain protected from downstream complexity.
In addition, access boundaries are clearly enforced at the entry point. Therefore, data extraction stays predictable and secure over time.
2. Data Standardization Layer
The platform converts incoming data into FHIR resources at this layer. This ensures that all data follows a common structure, regardless of origin. As a result, applications receive consistent and reliable information.
Over time, this reduces repeated transformation work. Therefore, integration maintenance becomes easier as systems grow.
3. Identity and Access Control Layer
This layer manages authentication, authorization, and consent enforcement. It checks who is requesting data and what they are allowed to access. As a result, sensitive information stays protected at all times.
In addition, access decisions remain consistent across applications. Therefore, compliance does not depend on individual app logic.
4. API and Event Delivery Layer
Applications interact with the platform through this layer. Data is delivered using FHIR APIs or event-based triggers. As a result, applications receive information when they need it.
At the same time, request handling remains controlled and efficient. Therefore, performance stays stable even as demand increases.
5. Monitoring and Audit Layer
This layer tracks system activity across the platform. It logs data access, errors, and performance metrics continuously. As a result, teams can identify issues early.
In addition, audit trails remain available for compliance reviews. Therefore, governance remains strong throughout operations.
6. Scalability and Infrastructure Layer
This layer supports growth in users, data volume, and workloads. It manages scaling, redundancy, and availability. As a result, the platform performs reliably under pressure.
Over time, infrastructure adapts without major redesign. Therefore, long-term operational stability is preserved.
Each layer plays a distinct role in maintaining security and scalability. Together, they prevent tight coupling between systems. As a result, changes become easier to manage. This approach allows FHIR platforms to grow while keeping governance intact.
Data Governance and Consent Management in FHIR Platforms
FHIR platforms handle sensitive healthcare data across systems, users, and use cases. Because of this, data governance and consent management cannot be treated as secondary features. They must be built into the platform from the start.
As scale increases, weak governance quickly leads to risk, rework, and compliance gaps. Therefore, strong governance ensures trust, control, and long-term stability.
1. Patient Identity and Matching Strategy
A reliable patient identity strategy is the foundation of any FHIR platform. Data often arrives from multiple systems with inconsistent identifiers. As a result, the platform must resolve identities accurately before data is shared or used. Deterministic matching uses exact identifiers such as medical record numbers.
Probabilistic matching fills gaps by comparing attributes like name, date of birth, and address. When mismatches occur, exception handling workflows allow teams to review and correct records safely.
Key considerations include:
- Deterministic and probabilistic matching methods
- Conflict resolution and exception workflows
- Ongoing identity quality monitoring
2. Consent Capture and Enforcement
Consent must be treated as a first-class object within the FHIR platform. It defines what data can be shared, with whom, and for what purpose. Therefore, consent is captured explicitly and stored alongside patient records.
Enforcement happens at runtime, not after data is delivered. As a result, unauthorized access is blocked automatically. Over time, this approach reduces compliance risk and manual intervention.
Consent handling typically includes:
- Explicit consent capture and updates
- Purpose-based access rules
- Runtime consent enforcement
3. Proxy and Delegated Access Models
Healthcare access often extends beyond the patient. Caregivers, parents, and legal guardians may need controlled access. These scenarios are common in pediatrics and dependent care.
As a result, the platform must support proxy and delegated access models. Each proxy relationship must respect role limits and consent boundaries. Therefore, access remains appropriate even as care situations change.
Common proxy scenarios include:
- Parent or guardian access for minors
- Caregiver access for dependents
- Time-bound or role-based delegation
4. Auditability and Traceability
Every action inside an FHIR platform must be traceable. This includes data access, updates, and sharing events. Audit logs record who accessed data and why. As a result, organizations can answer compliance questions quickly.
In addition, data lineage shows where information came from and how it changed. Therefore, audit readiness becomes continuous rather than reactive.
Audit coverage includes:
- Access logs and user actions
- Data change history
- Source and destination tracking
Governance failures rarely appear immediately. Instead, they surface during audits, incidents, or scale. Strong consent and identity controls prevent these problems early.
As a result, FHIR platforms remain trusted and defensible. When governance is designed properly, innovation can scale without increasing risk.
Security-by-Design Principles for Enterprise FHIR Healthcare Platforms
Enterprise FHIR platforms operate in environments where security failures carry real clinical and regulatory consequences. For that reason, security cannot be added after integrations are built or data flows are live. It must shape architecture, workflows, and operations from the beginning.
As platforms scale across systems and users, security-by-design prevents gaps that are expensive to fix later. Therefore, these principles guide how secure FHIR platforms are built and operated.
1. Least-Privilege Access Control
Every user and system should only access what they truly need. Broad access increases exposure and complicates audits. Instead, permissions are defined narrowly and reviewed regularly.
As roles change, access adjusts automatically rather than relying on manual cleanup. This approach limits blast radius during incidents. As a result, security remains manageable at scale.
2. Defense-in-Depth Architecture
A secure FHIR platform relies on multiple layers of protection rather than a single control. Network security, application security, and data security work together. When one layer fails, others still protect sensitive data.
This reduces reliance on any single safeguard. Over time, layered defenses absorb change more safely. Therefore, resilience improves without slowing delivery.
3. Secure API and Data Exchange
FHIR APIs expose valuable clinical data, so access must be tightly controlled. Authentication, authorization, and rate limits are enforced consistently. Data is encrypted both in transit and at rest.
In addition, requests are validated before processing. This prevents misuse and accidental exposure. As a result, data exchange stays reliable and compliant.
4. Continuous Monitoring and Threat Detection
Security does not stop after deployment. Activity across the platform is monitored continuously. Anomalies and unusual access patterns are flagged early. At the same time, teams respond before issues escalate into incidents.
Over time, monitoring improves platform awareness. Therefore, security posture strengthens as usage grows.
5. Audit-Ready Logging and Visibility
Every action in the platform must be traceable. Here, logs capture access, changes, and system behavior in a consistent way. At the same time, these records support audits without slowing operations.
Visibility also helps teams investigate issues faster. As regulations evolve, audit data remains available. Therefore, compliance becomes part of daily operation rather than a scramble.
6. Secure Change and Upgrade Management
FHIR platforms change frequently as standards, systems, and regulations evolve. Security controls must remain intact during these changes. Updates follow controlled deployment and testing processes.
Regression checks confirm that protections still work as intended. This reduces risk during upgrades. As a result, innovation continues without weakening security.
Security problems in healthcare rarely appear overnight. They grow quietly as systems expand and shortcuts accumulate. Security-by-design prevents that drift by enforcing discipline early. As a result, FHIR platforms scale with confidence rather than caution. This approach protects patients, organizations, and long-term platform value.
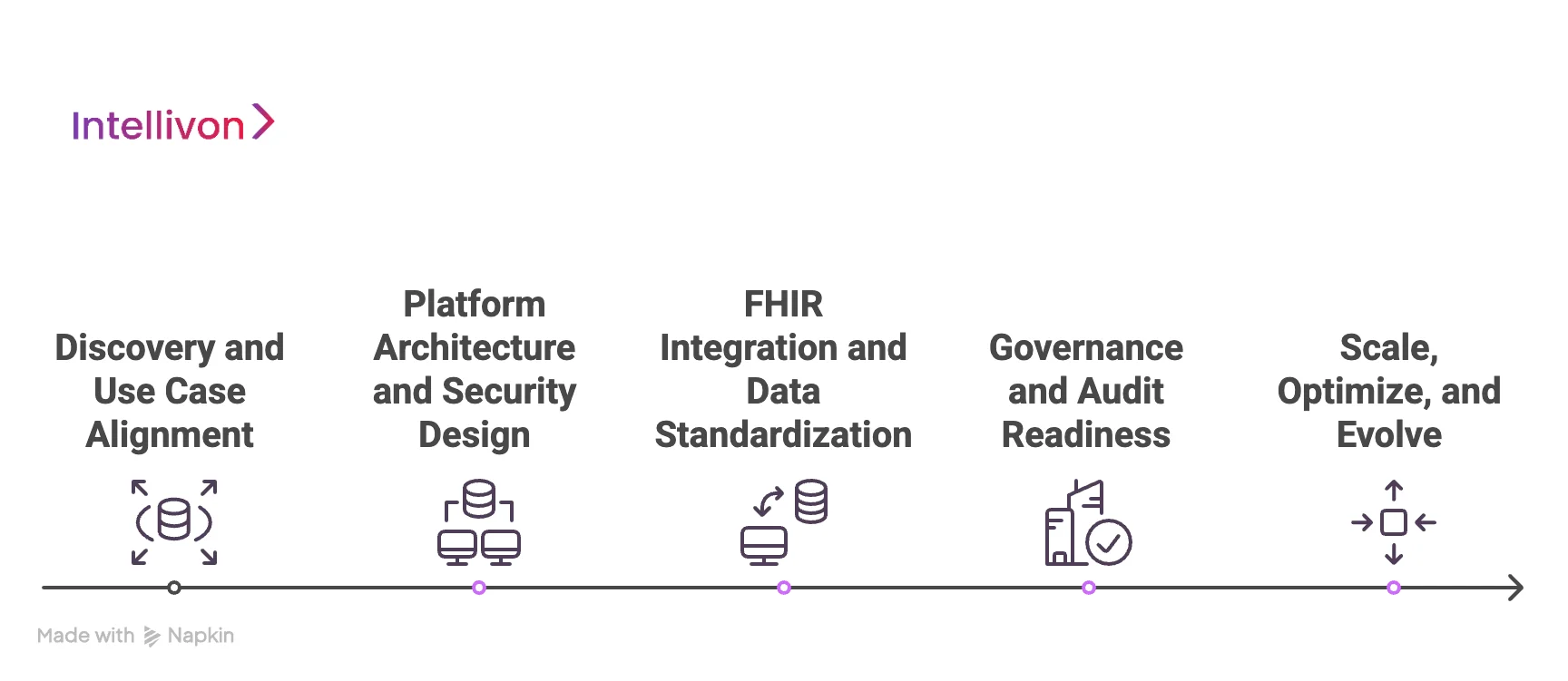
How We Build and Scale FHIR Integration Platforms
At Intellivon, FHIR integration platforms are built through a structured, phase-wise process designed for enterprise healthcare environments. Each phase focuses on reducing risk while preparing the platform for long-term scale. Decisions are made with governance, security, and operational reality in mind.
As requirements evolve, the platform grows without architectural disruption. Therefore, scalability is planned from the beginning rather than added later.
Phase 1: Discovery and Use Case Alignment
Intellivon begins by understanding how data will be used across clinical, operational, and digital workflows. Teams identify source systems, consuming applications, and user groups early.
This clarity helps determine where FHIR provides real value and where it does not. As a result, unnecessary integrations are avoided. Governance, consent, and compliance needs are also identified at this stage. Therefore, later phases move forward with fewer surprises.
Phase 2: Platform Architecture and Security Design
In this phase, Intellivon designs the overall platform architecture. Data flow, access boundaries, and consent handling are planned together. Security controls are embedded into each layer of the platform.
As a result, protection does not rely on individual applications. The architecture also accounts for future growth and change. Therefore, the platform remains stable as demand increases.
Phase 3: FHIR Integration and Data Standardization
Next, Intellivon connects systems using FHIR interfaces and approved access methods. Incoming data is converted into consistent FHIR resources. This step removes format inconsistencies early in the process.
As a result, downstream applications receive reliable data. Reusable integration patterns reduce repeated effort. Therefore, development stays efficient as integrations expand.
Phase 4: Governance and Audit Readiness
Once integrations are active, we apply governance controls across the platform. Identity, consent, and access rules are enforced continuously. Monitoring tools track usage, errors, and performance.
As a result, issues are identified before they escalate. Audit logs capture every action and data exchange. Therefore, compliance remains visible and manageable.
Phase 5: Scale, Optimize, and Evolve
In the final phase, Intellivon prepares the platform for enterprise-scale operation. Performance and cost are reviewed as usage grows. Infrastructure adjusts to handle higher volume without disruption.
As a result, the platform remains reliable under pressure. New systems and applications are onboarded more quickly. Therefore, the platform continues to support a long-term digital strategy.
FHIR integration platforms succeed when they are built with scale, governance, and change in mind. Intellivon’s phase-wise approach ensures that each layer of the platform is ready for real operational use. Early alignment prevents rework, while strong architecture supports growth.
Cost To Build FHIR-Based Healthcare Integration Platforms
At Intellivon, FHIR-based healthcare integration platforms are built as regulated enterprise interoperability infrastructure, not as lightweight data pipes layered onto existing systems. The focus stays on creating platforms that move data safely across EHRs, apps, partners, and regions while maintaining governance and compliance. Every design decision accounts for identity, consent, auditability, and long-term operational stability from the start.
When budget constraints exist, scope is refined with intent. However, security controls, consent enforcement, access governance, and audit readiness are never reduced. As a result, enterprises avoid remediation costs that typically surface after launch. Predictability replaces rework, and long-term ROI remains protected.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Interoperability Alignment | Use-case definition, system mapping, interoperability scope, regulatory assessment | $10,000 – $18,000 |
| Secure Platform Architecture Design | Layered FHIR architecture, identity flows, consent enforcement design | $15,000 – $25,000 |
| Governance & Policy Framework | Access rules, consent models, audit workflows, exception handling | $12,000 – $22,000 |
| Backend & System Integrations | EHRs, labs, payer systems, registries, third-party services | $18,000 – $35,000 |
| API & Integration Layer Development | FHIR APIs, event handling, orchestration logic | $14,000 – $26,000 |
| Security & Data Protection Controls | Encryption, access enforcement, monitoring, logging | $12,000 – $22,000 |
| Testing & Compliance Validation | Functional testing, security testing, audit readiness | $10,000 – $18,000 |
| Deployment & Scale Preparation | Cloud or hybrid deployment, monitoring, performance tuning | $10,000 – $18,000 |
Total initial investment: $110,000 – $210,000
Ongoing maintenance and optimization: ~15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped FHIR platform programs face pressure when indirect cost drivers are ignored. Planning for these early protects budgets, timelines, and compliance posture as data volume and usage grow.
- Integration complexity increases as more systems and partners connect
- Compliance overhead grows with audits, consent reviews, and policy updates
- Governance requires continuous tuning as use cases expand
- Infrastructure costs rise with data volume, analytics, and monitoring workloads
- Change management includes onboarding teams and supporting adoption
- Continuous monitoring becomes essential as reliance on the platform increases
Best Practices to Avoid Budget Overruns
Based on Intellivon’s experience delivering enterprise healthcare interoperability platforms, these practices consistently lead to controlled costs and predictable outcomes.
- Start with clearly defined interoperability use cases before expanding the scope
- Embed governance, consent, and auditability into core platform design
- Use modular integration components that scale without redesign
- Plan multi-system interoperability early to avoid retrofitting
- Maintain visibility across performance, usage, and compliance
- Design for evolving standards rather than one-time certification
Request a tailored proposal from Intellivon’s healthcare integration experts to receive a delivery roadmap aligned with your budget constraints, governance exposure, and long-term FHIR platform strategy.
Conclusion
FHIR-based healthcare integration platforms are no longer optional for organizations managing complex data flows. As systems expand, one-off integrations create risk, delays, and rising maintenance costs. A well-designed FHIR platform brings structure, consistency, and control to interoperability efforts. Therefore, cost planning must account for governance, security, and long-term ownership, not just initial build effort.
At Intellivon, FHIR platforms are treated as enterprise infrastructure built for change. Each platform is designed to scale across systems, partners, and evolving regulations. As a result, organizations gain predictable costs, stronger compliance, and faster innovation. When built with the right architecture and discipline, FHIR integration platforms shift from being a technical expense to a long-term growth enabler.
Build a FHIR-Native Healthcare Integration Platform With Intellivon
At Intellivon, FHIR-native healthcare integration platforms are built as regulated enterprise interoperability infrastructure, not as point-to-point connectors layered onto existing systems. Every architectural and delivery decision prioritizes data governance, security, and standards-based interoperability.
This ensures platforms operate reliably across EHRs, digital health apps, partners, and regions, not just during initial implementation.
As integration programs expand across systems, use cases, and data volumes, stability becomes critical. Governance, performance, and audit readiness remain consistent as data exchange increases.
Organizations retain control over identity, consent, and access without introducing fragmentation, compliance risk, or operational complexity.
Why Partner With Intellivon?
- Enterprise-grade FHIR platform architecture designed for regulated healthcare environments
- Proven delivery across multi-EHR ecosystems, digital health platforms, and enterprise networks
- Compliance-by-design approach with consent enforcement and audit readiness built in
- Secure, modular infrastructure supporting cloud, hybrid, and on-prem deployments
- AI-ready foundations for analytics, automation, and insights with governance controls
Book a strategy call to explore how Intellivon can help you build and scale a FHIR-native healthcare integration platform with confidence, control, and long-term enterprise value.
FAQs
Q1. What is a FHIR-native healthcare integration platform?
A1. A FHIR-native healthcare integration platform is built around the FHIR standard from the start. It uses FHIR resources and APIs as the core data model. This makes data exchange consistent, secure, and easier to scale across systems.
Q2. How much does it cost to build a FHIR-based healthcare integration platform?
A2. The cost usually ranges from $110,000 to $210,000 for an enterprise-ready platform. Pricing depends on integration scope, governance depth, security requirements, and scale. Ongoing ownership costs typically add 15–20% per year.
Q3. When should healthcare organizations build a FHIR platform instead of direct integrations?
A3. FHIR platforms make sense when multiple systems, apps, or partners need access to data. They are also useful when governance, consent, and auditability are critical. Direct integrations often break down as scale increases.
Q4. What are the main benefits of a FHIR-native approach?
A4. FHIR-native platforms reduce integration complexity and long-term maintenance. They improve interoperability and data consistency. In addition, they support faster onboarding of new applications without redesign.
Q5. What are the biggest risks if a FHIR platform is not designed correctly?
A5. Poor design can lead to security gaps, consent failures, and audit issues. It can also increase long-term costs due to rework and performance problems. Strong architecture and governance help avoid these risks early.