Hospitals are growing through acquisitions, digital health partnerships are increasing, and care is moving beyond physical locations into large virtual networks. However, this growth has a weak foundation. Disconnected systems hurt revenue cycles, raise administrative costs, and add risk to both clinical and financial decisions. Executives feel this impact through delays in reimbursements, rising denial rates, compliance risks, and limited visibility within their networks.
A healthcare interoperability solution tackles these issues by establishing a secure, real-time data exchange that allows patient, clinical, and operational information to move easily across hospitals, labs, payers, and third-party systems.
At Intellivon, we create these platforms for large healthcare organizations facing these exact challenges. Our work focuses on compliance, system integration, and data architecture ready for AI. We design solutions that can handle regulatory scrutiny, support large-scale data exchange, and prepare organizations for advanced analytics and automation. In this guide, we will explain how we develop healthcare interoperability solutions from the ground up.
Key Takeaways of the Healthcare Interoperability Solutions Market
According to Grand View Research, the global healthcare interoperability solutions market was valued at approximately USD 3.4 billion in 2023 and is expected to grow to around USD 8.57 billion by 2030, reflecting a strong CAGR of about 14.15% through the decade.
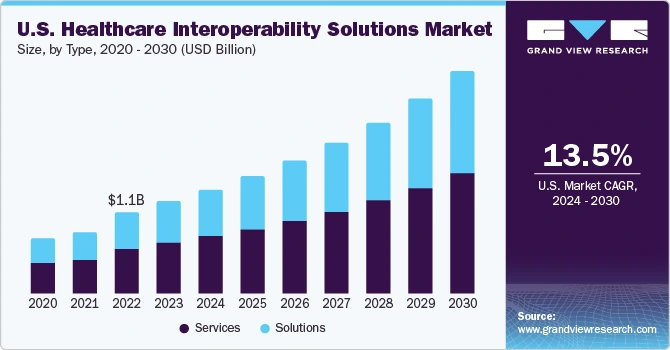
Key Growth Drivers:
- Widespread EHR adoption, along with regulatory mandates such as HIPAA, GDPR, and the 21st Century Cures Act, continues to push healthcare organizations toward standardized, interoperable data exchange.
- The industry shift toward value-based care is intensifying the need for longitudinal patient records and coordinated data flow across providers, payers, and care settings.
- Advances in cloud infrastructure, AI, FHIR-based APIs, blockchain, and big data platforms are expanding what interoperability solutions can achieve, particularly in secure, real-time data movement.
- North America currently leads adoption due to regulatory enforcement and mature healthcare IT systems, while Europe is scaling rapidly through cloud-first policies. Asia-Pacific shows strong growth as national digital health programs expand.
- Market deployments span on-premises, cloud, and hybrid models. Hospitals still favor on-premises for tighter control, although cloud adoption is accelerating due to scalability and cost efficiencies.
- Patient-centric interoperability is gaining momentum as FHIR adoption enables patients to access and manage their health data through mobile apps and wearables.
- Strategic partnerships between providers, payers, technology vendors, and governments are becoming a dominant approach to overcoming integration complexity and improving care workflows.
Interoperability has become a core infrastructure requirement for sustainable growth, risk control, and digital transformation. Enterprises that move early gain operational visibility, financial velocity, and clinical coordination advantages that compound over time.
What Is a Healthcare Interoperability Solution?
A healthcare interoperability solution is an enterprise-grade platform that enables secure, real-time exchange of clinical, operational, and financial data across disconnected healthcare systems.
It connects EHRs, imaging systems, billing platforms, and third-party applications into one coordinated data environment. The goal is to ensure that the right information reaches the right system at the right time.
Basic system integration moves data from one application to another. Interoperability goes further. It standardizes, validates, governs, and secures that data so it can be trusted and reused across the enterprise. This distinction matters at scale.
How Does a Healthcare Interoperability Solution Work?
A healthcare interoperability solution works by ingesting data from multiple clinical and financial systems, standardizing it using global healthcare standards, governing access through consent policies, and securely routing it in real time across the enterprise.
Each stage in this workflow is designed to preserve accuracy, security, and usability while ensuring data moves at the speed healthcare operations demand.
1. Data Ingestion from EHR, LIS, RIS, PACS, and RCM
Data enters the interoperability layer from clinical, diagnostic, imaging, and revenue systems. This includes patient records, lab results, imaging files, and claims data. In large networks, this ingestion must support both real-time streams and bulk data movement.
2. Standards-Based Normalization
Incoming data is translated into common formats using healthcare standards. This ensures that a lab result, discharge summary, or billing event is interpreted consistently across different vendor systems.
3. Identity Resolution and Patient Matching
The platform links records belonging to the same individual across disparate systems. It applies deterministic and probabilistic matching to eliminate duplication and ensure longitudinal patient views remain accurate.
4. Consent Verification and Policy Enforcement
Before data is shared, access is checked against patient consent, organizational policies, and regulatory rules. This layer controls who can see what, where, and under which conditions.
5. Real-Time Routing Across Systems
Once validated, data is routed instantly to downstream systems that require it. This may include care coordination platforms, analytics engines, payer systems, or national exchanges.
6. Secure API-Based Distribution to Applications
Standardized APIs make interoperable data available to clinical apps, population health tools, patient platforms, and AI models without exposing core systems directly.
7. Continuous Monitoring and Audit Logging
Every transaction is logged for traceability. Performance, security events, and data integrity are constantly monitored to meet enterprise governance and compliance requirements.
Interoperability works as a living infrastructure layer, and not a one-time integration project. When built correctly, this workflow creates a secure, real-time data backbone that supports clinical coordination, financial accuracy, and strategic decision-making across the entire healthcare enterprise.
What Problems Do Healthcare Interoperability Solutions Solve?
Healthcare interoperability solutions eliminate data silos, clinical–financial disconnects, and workflow delays by creating a unified, real-time data exchange backbone across enterprise healthcare ecosystems.
Healthcare interoperability solutions are built to remove these structural barriers at their root.
1. EHR-to-EHR Data Silos
In large health systems, different hospitals often operate on different EHR platforms or customized versions of the same system. Without interoperability, patient records remain isolated within facility boundaries. Clinicians see only fragments of a patient’s medical history, which increases clinical risk and forces conservative, redundant decision-making.
For example, when a patient is transferred between two hospitals within the same network, prior imaging, lab trends, and discharge summaries may not be available immediately. As a result, tests are repeated, treatment is delayed, and both cost and exposure rise.
2. Claims, Clinical, and Billing Disconnect
Clinical documentation and revenue operations frequently function as parallel worlds. When coding, billing, and utilization management operate without real-time access to complete clinical data, claim accuracy suffers. This leads to higher denial rates, delayed reimbursements, and manual rework across revenue cycle teams.
In large payer–provider ecosystems, finance leaders often discover unresolved gaps only after denials spike, when tracing a claim back to its originating encounter becomes a manual, time-consuming investigation across multiple systems.
3. Manual Reconciliation Across Facilities
When systems cannot exchange data directly, people become the integration layer. Staff rely on spreadsheets, phone calls, document uploads, and duplicate data entry to keep records aligned. This manual compensation increases operating costs and introduces persistent accuracy risks.
Across multi-facility health systems, entire operational teams are often dedicated to reconciling admissions, lab results, referrals, and discharge information between hospitals and ancillary providers.
4. Delayed Clinical Decision-Making
When critical data arrives late, decisions slow down. This is especially damaging in emergency care, oncology, and chronic disease management, where timely intervention directly affects outcomes. Without interoperability, clinicians wait for faxed reports, external imaging, or portal-based document uploads.
Emergency physicians regularly face situations where external imaging or prior clinical notes are unavailable at the point of care, leading to delayed diagnosis or precautionary over-treatment.
5. Incomplete Longitudinal Patient Records
Without a unified data backbone, healthcare organizations struggle to maintain continuous, multi-year patient histories across care settings. Gaps in data weaken risk stratification, disrupt care coordination, and reduce the accuracy of population health models.
Chronic disease programs frequently fail to identify early deterioration because key signals are spread across outpatient EHRs, hospital systems, labs, and specialized care platforms.
Interoperability solutions resolve deep structural problems that drive inefficiency, inflate operating costs, delay clinical action, and weaken analytics at scale. Eliminating them creates immediate operational stability and unlocks a foundation for long-term digital and financial performance.
How Interoperability Solutions Help Achieve 21–29% Reduction in Emergency Readmissions
Healthcare interoperability solutions using real-time ADT alerts enable care teams to intervene faster after discharge, directly reducing emergency readmissions and avoidable hospitalizations.
Primary data from California-based care networks shows how powerful this shift can be when interoperability is embedded directly into daily workflows, not isolated in portals.
1. Real-Time ADT Alerts
When an admission, discharge, or transfer occurs, ADT-enabled interoperability platforms notify connected care teams instantly. This includes primary care providers, care managers, and specialty teams responsible for follow-up.
In California, a primary-care network using HIE-driven ADT alerts achieved a 21–29% reduction in emergency readmissions. The system ensured that no discharge went unnoticed and no high-risk patient was lost between settings.
2. Interoperability Enables Proactive Follow-Up
ADT alerts work best when they trigger defined actions. These include outreach within 24–48 hours, medication reconciliation, and rapid appointments for unstable patients.
At a Federally Qualified Health Center in Los Angeles, integrating ADT alerts directly into care workflows led to an 85% reduction in emergency visits and a 68% drop in hospitalizations among patients with diabetes within six months. The improvement came from earlier intervention, not new clinical programs.
3. Financial Impact
Lower emergency utilization immediately improves bed availability and emergency throughput. It also reduces avoidable costs tied to penalties, uncompensated care, and downstream complications.
The same California primary-care network recorded an estimated USD 4.2 million in annual savings from better care transitions driven by ADT-enabled interoperability. These savings came from fewer readmissions, shorter lengths of stay, and more efficient post-discharge coordination.
The primary evidence shows that when interoperability is wired into operational workflows through real-time ADT alerts, it directly reshapes emergency utilization, readmission risk, and total cost of care.
What Are the Core Features of an Enterprise Healthcare Interoperability Platform?
Enterprise healthcare interoperability platforms combine multi-EHR data exchange, standards-based normalization, identity resolution, consent governance, real-time routing, and secure APIs to enable trusted data flow at scale.
The following features form the backbone of any scalable healthcare interoperability platform.
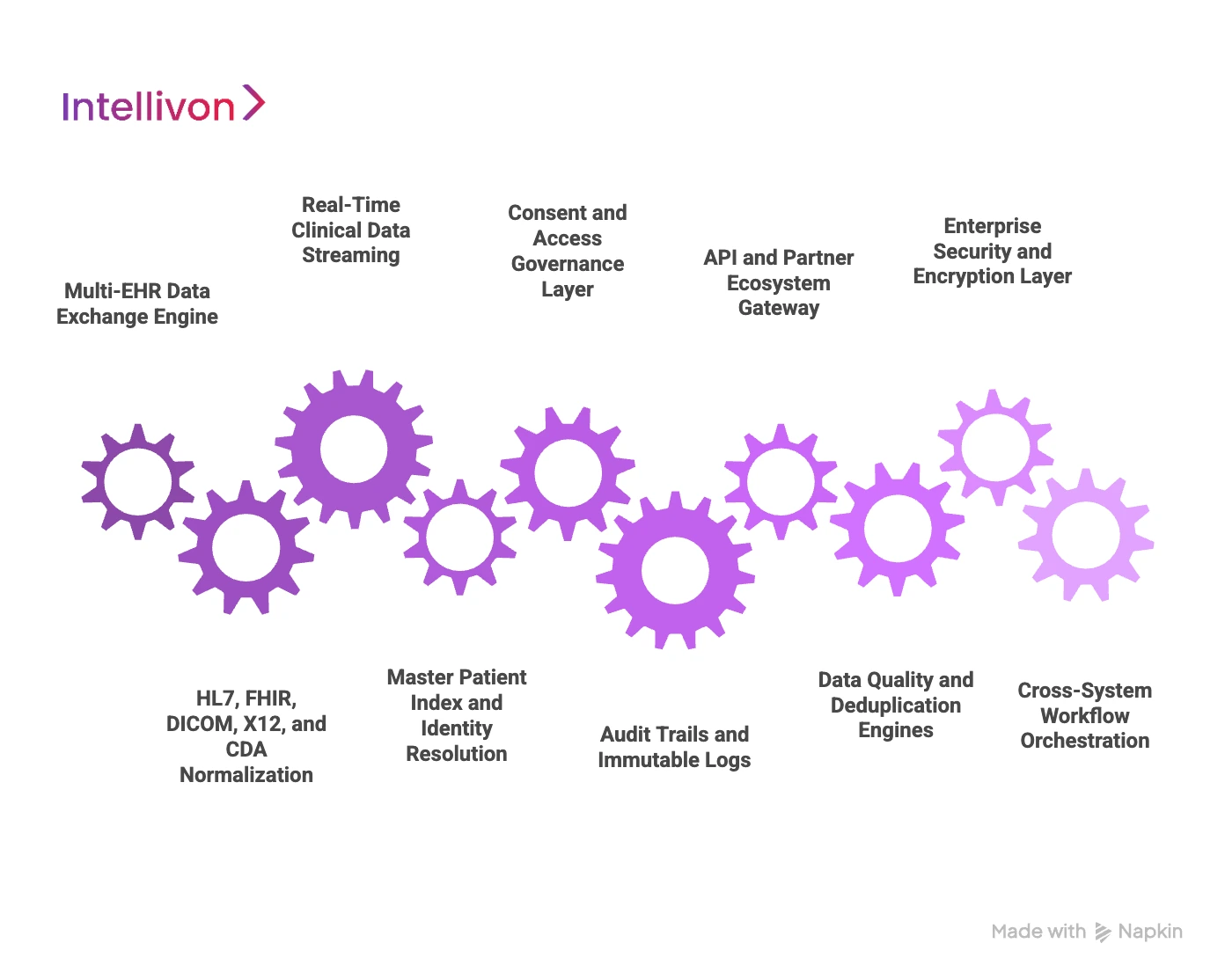
1. Multi-EHR Data Exchange Engine
This engine enables continuous data exchange between different EHR systems across hospitals, clinics, and partner networks. It supports both real-time messages and bulk data transfers.
For large enterprises, this feature ensures that patient records move with the patient, even when care spans multiple facilities and vendors.
2. HL7, FHIR, DICOM, X12, and CDA Normalization
Healthcare data arrives in different formats like HL7, FHIR, DICOM, X12, and CDA, depending on the source system. Normalization converts this data into unified structures that downstream systems can reliably interpret.
This prevents misaligned lab values, incomplete discharge summaries, and inconsistent billing data from disrupting care and revenue workflows.
3. Real-Time Clinical Data Streaming
Streaming capabilities allow vital signs, lab updates, imaging results, and care events to flow instantly across systems. This removes delays between documentation and clinical action.
In time-sensitive environments such as emergency care and intensive care units, real-time data exchange directly supports faster clinical decisions.
4. Master Patient Index and Identity Resolution
The platform continuously matches patient identities across disparate systems using deterministic and probabilistic algorithms. This prevents duplicate records and fragmented histories.
For enterprises managing millions of patient records, accurate identity resolution is what enables safe longitudinal care and trustworthy analytics.
5. Consent and Access Governance Layer
This layer enforces patient consent, provider access rules, and organizational data policies before any information is shared. It aligns daily data operations with regulatory requirements.
Enterprises rely on this feature to protect sensitive data while still enabling legitimate clinical and operational data use.
6. Audit Trails and Immutable Logs
Every data transaction is captured with time-stamped audit records. These logs support compliance reviews, legal defensibility, and internal governance.
In highly regulated environments, immutable auditability is often as critical as data availability itself.
7. API and Partner Ecosystem Gateway
Standardized APIs expose interoperable data to external applications, partners, and digital health platforms without exposing core systems.
This allows enterprises to integrate new tools, payer platforms, and patient apps without rebuilding internal infrastructure.
8. Data Quality and Deduplication Engines
These engines continuously assess data accuracy, detect duplicates, and resolve inconsistencies across systems. They ensure that analytics and clinical decisions are based on clean data.
For large datasets, even small error rates can distort population health insights and financial reporting.
9. Enterprise Security and Encryption Layer
Encryption safeguards data at rest and in motion, while access controls protect systems from unauthorized use. This layer also integrates with enterprise identity and cybersecurity frameworks.
Security at this level ensures that interoperability does not become a new attack surface.
10. Cross-System Workflow Orchestration
Workflow orchestration connects events across systems into automated operational processes. This includes referral routing, discharge follow-up, care coordination, and claims workflows.
Instead of moving data alone, the platform moves work across the enterprise.
These features collectively transform interoperability from a technical connector into a strategic operations platform.
Data Standards That Power Healthcare Interoperability Solutions
Healthcare interoperability standards such as HL7, FHIR, DICOM, X12, and clinical vocabularies like SNOMED and LOINC enable consistent, secure, and machine-readable data exchange across the enterprise.
They establish trust, support automation, and ensure that clinical, financial, and operational systems interpret information in the same way across the entire healthcare ecosystem.
1. HL7 v2 and v3
HL7 remains the backbone of real-time clinical messaging in hospitals. It governs how admissions, discharges, orders, and results move between systems.
In large enterprises, HL7 powers daily operational activity across EHRs, laboratory systems, radiology platforms, and pharmacy systems. It enables event-based workflows such as ADT alerts, order management, and result distribution at scale.
2. FHIR R4 and R5
FHIR modernizes healthcare data exchange through lightweight APIs and web-native structures. It allows applications to retrieve patient data on demand and supports mobile, cloud, and partner ecosystem integrations.
Enterprises rely on FHIR to expose controlled access to clinical data for patient apps, population health platforms, analytics engines, and AI models without creating custom point-to-point integrations.
3. DICOM
DICOM governs how medical imaging data, such as CT scans, MRIs, and X-rays, is stored, exchanged, and displayed across systems.
For large hospital groups, DICOM ensures that imaging studies follow patients between facilities, enabling faster diagnosis, reducing repeat imaging, and supporting cross-site clinical collaboration.
4. X12
X12 standards define administrative and financial data exchange between providers and payers. This includes eligibility checks, claims submission, remittances, and authorization workflows.
At the enterprise level, X12 is critical for automating revenue cycle operations, reducing manual billing effort, and improving claim accuracy across large payer–provider networks.
5. Clinical Document Architecture (CDA)
CDA structures rich clinical documents such as discharge summaries, progress notes, and care plans in a standardized format.
These documents are essential for transitions of care between hospitals, post-acute facilities, and community providers, where narrative clinical context matters as much as structured data.
6. SNOMED, LOINC, and ICD-10
These clinical vocabularies standardize diagnoses, laboratory tests, procedures, and outcomes across systems. They ensure that data retains the same clinical meaning regardless of where it originates.
For enterprises running population health programs and clinical analytics at scale, these terminologies are what allow meaningful aggregation, risk stratification, and outcomes measurement.
7. National and Regional Health Exchange Frameworks
Many countries operate national interoperability frameworks that define security, identity, consent, and exchange protocols at a public infrastructure level.
Enterprises participating in cross-border care, national registries, or government health programs depend on these frameworks to enable compliant, large-scale data exchange.
Data standards are the foundation that turns interoperability into a reliable enterprise capability. When applied correctly, these standards enable automation, analytics, regulatory confidence, and ecosystem-wide collaboration.
Use Cases of Healthcare Interoperability Solutions for Enterprises
Enterprise healthcare interoperability enables real-time data exchange across hospitals, payers, labs, and public health systems to support coordinated care, revenue optimization, and large-scale analytics.
Below are some enterprise-grade scenarios where interoperability creates measurable impact.
1. Multi-Hospital EHR Unification
Large health systems often operate multiple EHR platforms across acquired hospitals and specialty centers. Interoperability unifies these environments into a single clinical data fabric without forcing full system replacement.
A leading U.S. health system running multiple Epic and Cerner installations uses an interoperability layer to allow clinicians at any facility to access complete patient histories in real time across its network.
2. Cross-Network Health Information Exchange (HIE)
Interoperability enables hospitals to participate in regional and national data exchange networks. This allows secure sharing of clinical information with external providers, emergency departments, and specialty clinics.
Statewide exchange programs in California and New York connect hundreds of hospitals and physician networks through centralized HIE platforms built on enterprise interoperability infrastructure.
3. Payer–Provider Real-Time Data Sharing
Interoperability platforms synchronize clinical and financial data between providers and insurance payers. This supports faster prior authorizations, cleaner claims, and reduced denial cycles.
Large national payers use real-time eligibility and utilization feeds to automate claims adjudication with integrated provider networks.
4. AI Clinical Decision Support Enablement
AI models depend on consistent, multi-source data to deliver accurate predictions. Interoperability feeds these models with unified longitudinal patient records across care settings.
Academic medical centers deploying AI for sepsis prediction and readmission risk rely on interoperability layers to aggregate lab, vitals, and EHR data in near real time.
5. Population Health Analytics
Interoperable data enables enterprises to track disease trends, care gaps, and outcomes across millions of patients. This supports value-based care and preventive health programs.
Integrated delivery networks use unified datasets to identify high-risk populations for chronic disease management across outpatient, inpatient, and community settings.
6. Claims Automation and Denial Reduction
By aligning clinical documentation with billing data in real time, interoperability platforms reduce claims errors and downstream denials.
Large hospital revenue cycle operations use interoperable pipelines to validate documentation completeness before claims submission.
7. National Health Data Exchange Programs
Government-led digital health initiatives rely on interoperability to connect public and private providers into national data grids.
Countries running centralized health ID programs use national exchange frameworks to link clinical data across public hospitals and private networks.
8. M&A Hospital System Data Consolidation
After mergers and acquisitions, enterprises must unify patient and operational data across newly added facilities without disrupting ongoing care.
Global healthcare groups use interoperability platforms as a transitional backbone while standardizing IT systems over multi-year integration programs.
These use cases show that healthcare interoperability has become a strategic enterprise capability that supports growth through acquisitions, drives financial performance, enables AI adoption, and strengthens coordinated care across entire health ecosystems.
How We Build Scalable Healthcare Interoperability Solutions
At enterprise scale, interoperability must be engineered as long-term infrastructure, not a short-term integration project. It must support regulatory scrutiny, high transaction volumes, multi-vendor environments, and future AI adoption without degrading performance or security.
At Intellivon, we follow a structured, risk-controlled delivery framework that allows healthcare enterprises to modernize data exchange while keeping clinical and revenue operations stable throughout the transformation.
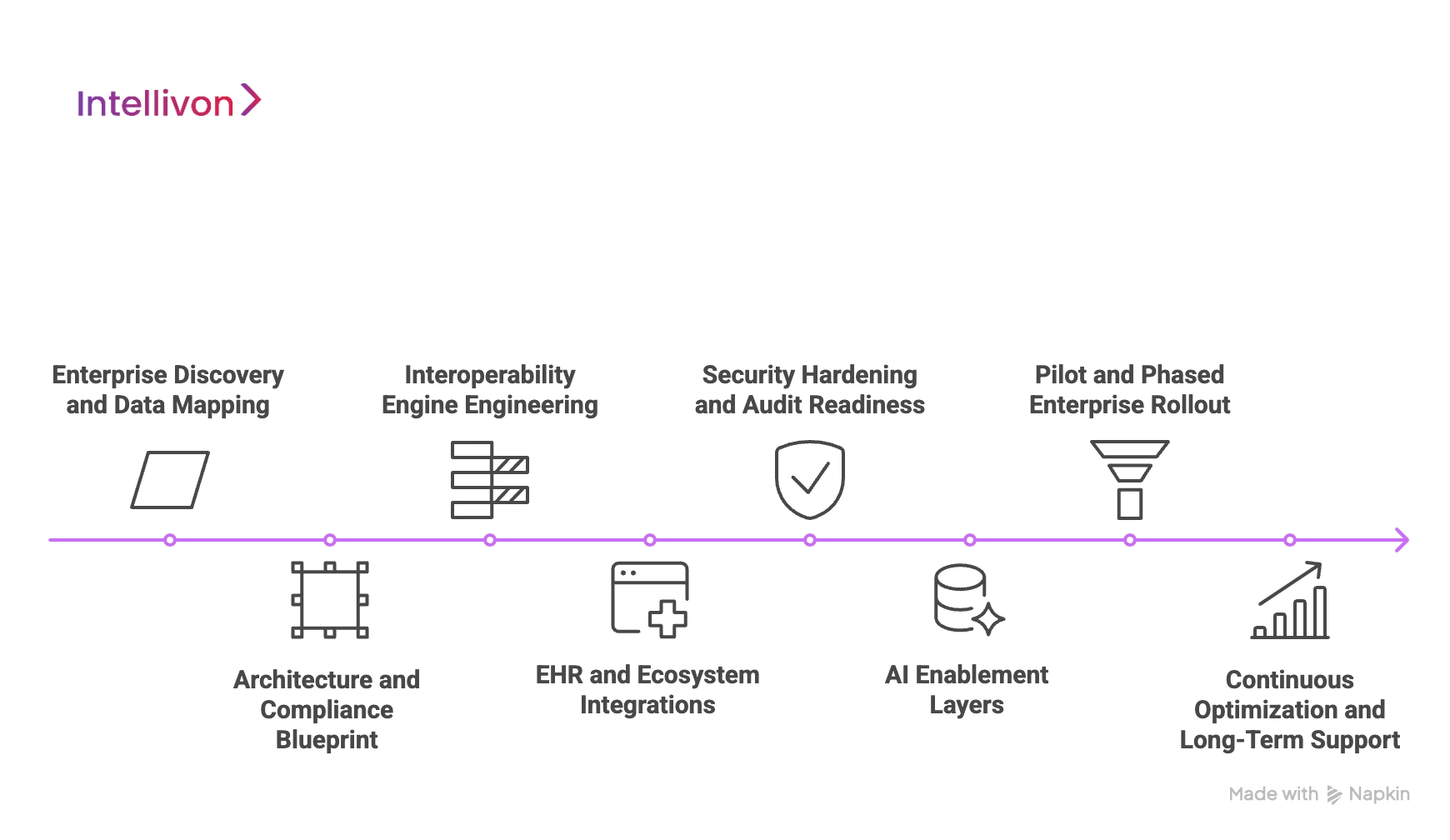
1. Enterprise Discovery and Data Mapping
We start by documenting how data actually moves across the organization today. This includes EHRs, lab systems, imaging platforms, revenue cycle systems, payer connections, and third-party partners. We identify where data originates, where it is consumed, and where delays or manual workarounds exist.
This discovery phase gives leadership a clear, system-level view of integration debt before any technology decisions are finalized. It also ensures future architecture aligns with real operational behavior, not just system diagrams.
2. Architecture and Compliance Blueprint
Once the data landscape is clear, we design a target interoperability architecture with compliance embedded at every layer. Identity management, consent enforcement, encryption, audit controls, and jurisdictional data rules are built into the core design.
This stage prevents the common enterprise failure where platforms scale faster than governance. The resulting blueprint supports long-term regulatory stability while allowing transactional performance to grow.
3. Interoperability Engine Engineering
We then engineer the central interoperability engine responsible for ingestion, normalization, routing, and workflow orchestration. This layer is built for continuous operation under high message volumes, not occasional point-to-point exchange.
At enterprise scale, this engine becomes operational infrastructure, supporting admissions, discharges, lab updates, imaging flows, and claims data without latency spikes or message loss.
4. EHR and Ecosystem Integrations
Next, we connect the platform to core clinical and financial systems across the enterprise and its partner ecosystem. High-impact workflows are prioritized first, such as ADT feeds, lab results, referrals, and claims transactions.
This phased integration strategy allows enterprises to generate value early while minimizing disruption to active hospital operations.
5. Security Hardening and Audit Readiness
Before production expansion, the platform undergoes security hardening, vulnerability testing, and full audit trail validation. Governance policies are operationalized for access control, monitoring, and incident response.
This ensures the platform can withstand cyber threats and regulatory reviews as data volumes and user access expand across facilities and regions.
6. AI Enablement Layers
Once interoperable data is unified and governed, we activate secure data pipelines for analytics and AI workloads. This includes real-time data streaming and structured historical datasets for predictive modeling.
Only at this stage does AI become reliable at the enterprise level, because the underlying data is consistent, complete, and trusted.
7. Pilot and Phased Enterprise Rollout
We deploy the platform through controlled pilots within selected hospitals, departments, or networks. Performance, data integrity, clinician adoption, and operational impact are monitored closely.
Enterprise-wide rollout then proceeds in phases, allowing organizations to scale without disrupting live care delivery or revenue operations.
8. Continuous Optimization and Long-Term Support
Post-deployment, the platform enters a continuous improvement cycle. Data quality, performance, security posture, and workflow utilization are measured against business objectives.
As regulations, partnerships, and care models evolve, the interoperability layer evolves with them. This keeps the platform relevant over multi-year enterprise growth cycles.
Scalable healthcare interoperability is built through disciplined engineering, not ad hoc integration. When delivered through a phased, governance-first approach, it becomes trusted digital infrastructure.
Cost to Build a Healthcare Interoperability Platform
Building an enterprise healthcare interoperability platform is not a typical software project. It is a long-term digital infrastructure investment that sits at the core of clinical operations, revenue cycles, regulatory compliance, and AI enablement. Costs extend far beyond basic integrations into standards management, identity resolution, cybersecurity, governance, audit readiness, and platform reliability at scale.
At Intellivon, we structure phased cost models that align with capital planning, regulatory exposure, and measurable operational ROI. Early phases focus on establishing a compliant, production-ready interoperability core without forcing full ecosystem integration on day one.
Estimated Phase-Wise Cost Breakdown (Enterprise Pilot)
| Phase | Description | Estimated Cost (USD) |
| Clinical & Business Discovery | Enterprise workflow mapping, system inventory, data flow analysis, regulatory scoping, ROI modeling | 15,000 – 25,000 |
| Platform Architecture & Governance Design | Multi-layer interoperability architecture, security blueprint, identity and consent design | 20,000 – 35,000 |
| Core Interoperability Engine Build | Message ingestion, routing, standards processing, workflow orchestration | 45,000 – 80,000 |
| EHR, Lab & Revenue System Integration | Single EHR + LIS/RIS/RCM integration, HL7/FHIR/X12 mapping | 25,000 – 45,000 |
| Identity Resolution & Consent Management | Master patient index, probabilistic matching, consent enforcement | 18,000 – 32,000 |
| Security, IAM & Compliance Controls | Encryption, access control, audit trails, HIPAA/GDPR alignment | 16,000 – 30,000 |
| Testing, QA & Security Validation | Load testing, data integrity validation, penetration testing | 12,000 – 20,000 |
| Pilot Deployment & Enterprise Enablement | Live rollout, stakeholder onboarding, stabilization | 15,000 – 25,000 |
Total Initial Enterprise Pilot Range: USD 166,000 – 292,000
Annual Maintenance and Optimization Costs
Ongoing operations typically require 14–20% of the initial build cost per year, which translates to:
Approx. USD 24,000 – 58,000 annually
Hidden Costs Enterprises Should Plan For
Even with a controlled pilot, several expansion-driven costs should be anticipated early:
- Additional EHR, payer, and partner system integrations
- Growth in data ingestion from labs, imaging, and devices
- Updates to consent and privacy frameworks as regulations evolve
- Cloud compute and storage growth with transaction volume
- Enterprise change management and cross-facility training
- Ongoing patient identity optimization at the national or multi-region scale
Proactive planning prevents budget shocks during enterprise rollout.
Best Practices to Stay Within Budget
Large health systems that scale interoperability successfully follow a disciplined approach:
- Start with one high-impact, high-friction data workflow
- Avoid multi-EHR and multi-region rollouts in phase one
- Enforce security and compliance from the first architecture draft
- Use a modular platform design to add integrations without reengineering
- Track clinical, revenue, and operational impact weekly during the first 90 days
This approach allows leadership to validate measurable ROI before committing broader capital.
Contact us for a free cost estimate and architecture consultation.
Examples of Real-World Healthcare Interoperability Platforms
Leading healthcare interoperability platforms operate as national and enterprise-grade data exchange backbones, enabling real-time clinical, administrative, and payer data sharing across thousands of organizations.
The following five platforms illustrate how interoperability is already reshaping enterprise healthcare operations.
1. CommonWell Health Alliance
CommonWell operates one of the largest vendor-led interoperability networks in the United States. It connects thousands of hospitals, EHR systems, and ambulatory providers through a shared record location and exchange framework.
For enterprises, CommonWell enables automated patient record discovery across participating organizations. This allows clinicians to retrieve external records inside their native EHR workflows, reducing duplication of tests, improving continuity of care, and supporting longitudinal patient histories across competing health systems.
2. Carequality

Carequality is a national interoperability framework governed by a broad coalition of EHR vendors, payers, and healthcare organizations. It establishes trust, legal agreements, and technical standards for nationwide data exchange.
Enterprises use Carequality to securely exchange clinical data with organizations outside their own network. This supports cross-state referrals, emergency care coordination, and payer-provider data sharing without the need for custom legal and technical integrations.
3. Epic Care Everywhere
Epic Care Everywhere is the native interoperability framework within the Epic EHR ecosystem, widely used by large hospital groups and academic medical centers. It enables record sharing across Epic and non-Epic organizations.
For enterprises running Epic across multiple facilities, Care Everywhere supports instant access to outside records at the point of care. This reduces clinical blind spots during referrals, emergency admissions, and multi-site treatment plans.
4. Oracle Health Interoperability
Oracle Health Interoperability, built on the Cerner ecosystem, connects hospitals, laboratories, payers, and health networks through standardized data exchange services. It supports real-time and bulk clinical and administrative data movement.
Large enterprises leverage this platform to unify disparate Cerner deployments after mergers, automate payer data exchange, and enable population-level analytics across regional and national health systems.
These platforms show that healthcare interoperability is already operating as mission-critical infrastructure across national health systems and large enterprise networks. Interoperability delivers the greatest value when it is treated as a long-term strategic backbone, not as a series of isolated integrations.
Conclusion
Healthcare interoperability has moved beyond a technical upgrade. It now functions as foundational infrastructure for clinical coordination, financial accuracy, regulatory confidence, and data-driven growth. As care networks expand and digital health models mature, the ability to exchange trusted data in real time determines how effectively enterprises can scale, control risk, and unlock advanced capabilities such as population health analytics and AI-assisted care.
For large healthcare organizations, interoperability is no longer a cost center. It is a strategic growth enabler. Enterprises that invest with clear governance, phased execution, and measurable ROI position themselves to deliver coordinated care, operate with financial precision, and adapt quickly as care models, regulations, and technologies continue to evolve.
Build a Healthcare Interoperability Solution with Intellivon
At Intellivon, we build enterprise-grade healthcare interoperability platforms that unify clinical, financial, and operational data into one secure, real-time exchange fabric. Our solutions connect EHRs, labs, imaging systems, payer platforms, AI models, and partner ecosystems without disrupting live hospital operations or revenue workflows.
Each platform is engineered for large healthcare enterprises. It is compliant by design, resilient under peak transaction loads, interoperable across multi-vendor environments, and built to deliver measurable operational and financial ROI from the first deployment phase.
Why Partner With Intellivon?
- Compliance-First Architecture: Every deployment aligns with HIPAA, GDPR, data interchange mandates, and regional health regulations with audit-ready governance embedded at every layer.
- Standards-Native Interoperability Engineering: Native support for HL7, FHIR, DICOM, X12, and enterprise APIs enables secure, real-time data exchange across the ecosystem.
- Enterprise-Scale Platform Design: Built for multi-hospital networks, national deployments, and high-volume transaction environments without performance degradation.
- AI-Ready Data Foundations: Unified, governed data pipelines that power advanced analytics, population health intelligence, and predictive care models.
- Zero-Trust Security Framework: Identity-led access controls, end-to-end encryption, and continuous threat monitoring protect PHI at enterprise scale.
- Hybrid Cloud and On-Prem Flexibility: Architectures support regulated hybrid deployments for data residency, latency, and sovereign cloud requirements.
- Proven Enterprise Delivery: Validated architectures, regulatory maturity, and outcomes-driven execution across complex healthcare ecosystems.
Book a strategy consultation with Intellivon to explore how a custom-built healthcare interoperability platform can unify your data infrastructure, strengthen compliance, accelerate AI adoption, and scale safely across your enterprise.
FAQs
Q1. What is the difference between EHR integration and healthcare interoperability?
A1. EHR integration connects systems at a technical level, while healthcare interoperability ensures data is standardized, governed, and usable across enterprises for clinical, financial, analytics, and regulatory workflows.
Q2. How secure are healthcare interoperability platforms for large hospitals?
A2. Enterprise-grade interoperability platforms use zero-trust security, encryption in transit and at rest, identity-based access controls, and continuous audit logging to meet strict regulatory and cybersecurity requirements.
Q3. Can healthcare interoperability platforms support AI and population health analytics?
A3. Yes. Interoperability creates the unified, high-quality data foundation required for AI models, predictive analytics, risk stratification, and large-scale population health management.
Q4. How long does it take to deploy a healthcare interoperability platform in an enterprise environment?
A4. Initial enterprise pilots typically take 4–8 months, depending on system complexity, regulatory scope, number of integrations, and required security validation.
Q5. What regulations govern healthcare data exchange through interoperability platforms?
A5. Key regulations include HIPAA, GDPR, national health data exchange laws, payer interoperability mandates, and emerging AI governance frameworks, all enforced through built-in consent and audit controls.






