Most hospital operations face challenges because daily work relies on numerous handoffs between systems that do not communicate or respond in real time. Tasks move through EHRs, emails, spreadsheets, phone calls, and manual approvals. Over time, delays in decisions and gaps in coordination become a normal part of operations. What once seemed like a manageable inefficiency evolves into operational risk, compliance issues, and loss of revenue on a large scale.
This is where workflow automation requires a fresh perspective. Hospitals need a workflow automation platform that coordinates work among people, systems, and decisions in a controlled manner.
At Intellivon, we lead in building enterprise-grade healthcare platforms that operate inside live hospital environments. Our decades of experience shape how we approach hospital workflow automation as a platform problem, not a tooling exercise. In this guide, we explain how to design a hospital workflow automation platform that unifies work across systems, teams, and decisions without disrupting care delivery.
Key Takeaways of the Healthcare Automation Market
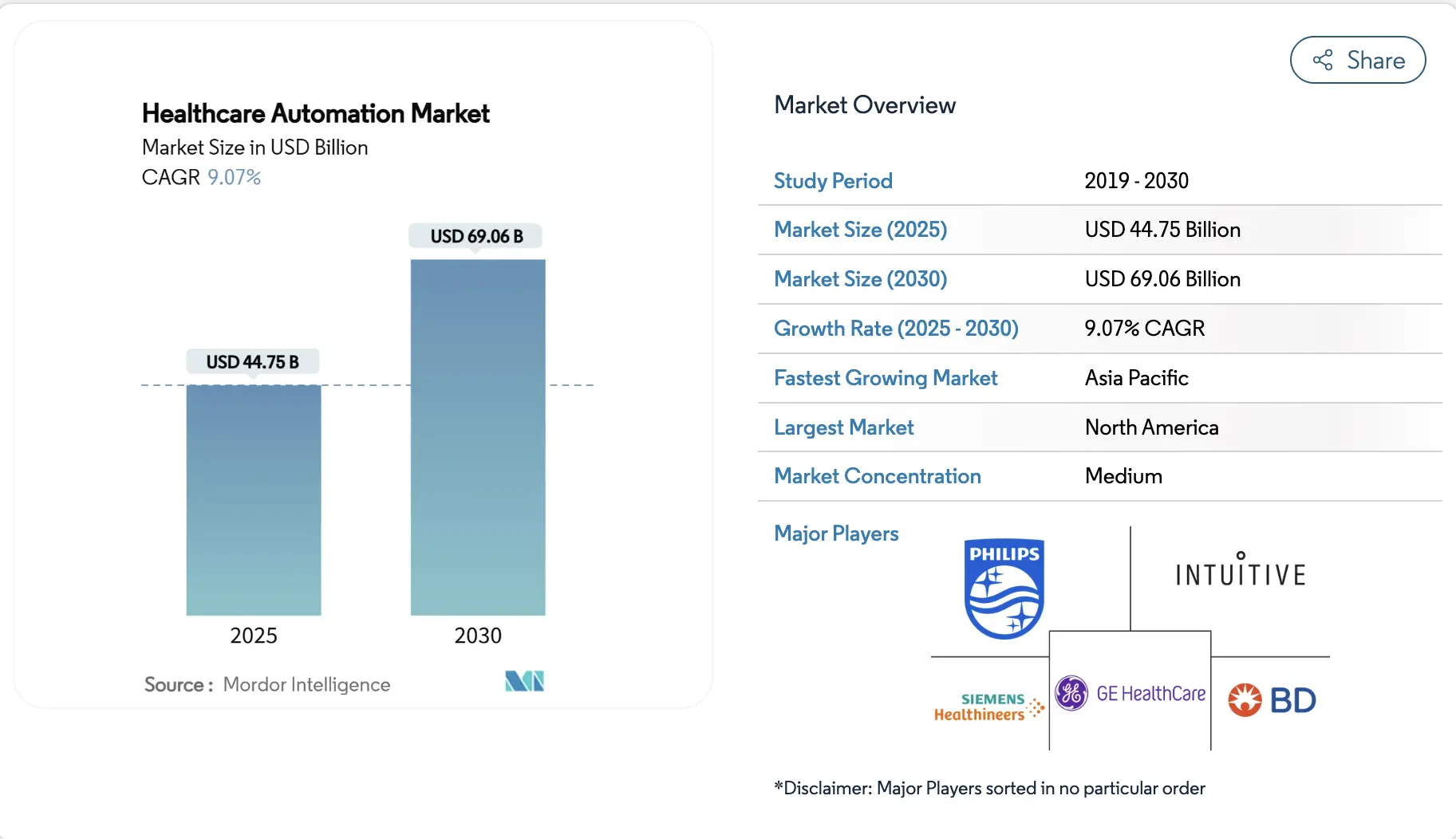
Adoption Rates
Adoption continues to rise, led by large hospitals and systems integrating automation with enterprise AI platforms.
- 71% of U.S. non-federal acute-care hospitals used predictive AI integrated with EHRs in 2024, up from 66% in 2023.
- AI adoption across hospital workflows reached 18.7% by 2022, rising sharply to 90–96% among hospitals with over 400 beds and 81–86% within multi-hospital systems.
- 2025 RPA adoption is expected to exceed 35% of healthcare organizations, while 63% of healthcare leaders already use AI in operational workflows.
Success Rates and ROI
Enterprise deployments show consistent financial returns through efficiency, accuracy, and workforce improvements.
- One 500-bed hospital generated USD 800K in annual savings from a USD 200K AI investment, delivering a 4× ROI or USD 3.20 for every dollar spent.
- A large healthcare organization achieved 2.6× ROI by automating 105 workflows, resulting in USD 14 million in annual cost savings.
- Additional outcomes reported include a 60% reduction in medication errors, an 18% increase in staff satisfaction, and 171% ROI within the first year for skilled nursing facilities.
Together, these figures reinforce a clear pattern. Hospitals that adopt automation at the platform level see faster adoption, stronger clinician acceptance, and measurable financial returns. As automation becomes embedded across core workflows in larger and multi-hospital systems, it is increasingly viewed as an operational necessity rather than a discretionary investment.
What Is a Hospital Workflow Automation Platform?
A hospital workflow automation platform is a centralized system that orchestrates clinical, operational, and administrative workflows across a hospital by coordinating people, systems, and decisions in real time.
Hospitals run on thousands of interconnected actions every day. These actions span clinicians, administrators, systems, and approvals. When coordination breaks down, work slows even if teams perform well. A hospital workflow automation platform exists to close this coordination gap.
At its core, the platform provides a shared execution layer for hospital workflows. It replaces manual follow-ups and siloed task management with structured, real-time orchestration. Instead of relying on people to chase the next step, the platform ensures work moves forward automatically.
How This Platform Differs From Traditional Automation Tools
Hospitals often start their automation journey with individual tools. These tools solve specific problems, but they do not change how work flows across the organization. Understanding the difference between task-level automation and a workflow automation platform helps clarify why many enterprise initiatives stall after early gains.
Below is a simple comparison to illustrate how a hospital workflow automation platform differs from traditional automation tools.
| Area of Comparison | Traditional Automation Tools | Hospital Workflow Automation Platform |
| Scope of automation | Automates individual tasks or steps within a single department | Orchestrates complete workflows across multiple departments and systems |
| System visibility | Limited to the tool or application where automation runs | Provides end-to-end visibility across the entire workflow lifecycle |
| Integration approach | Point-to-point integrations tied to one system | Acts as a coordination layer across EHRs, clinical systems, and enterprise applications |
| Handling exceptions | Breaks or requires manual intervention when workflows deviate | Manages exceptions, escalations, and approvals through defined logic |
| Scalability | Scales within departments, but struggles at the hospital-wide level | Designed to scale across hospitals, service lines, and health systems |
| Governance and control | Minimal oversight beyond local teams | Central governance with role-based execution and auditability |
| Adaptability | Requires rework when workflows or policies change | Allows workflows to evolve through configuration rather than reengineering |
| Strategic value | Improves efficiency in isolated areas | Enables predictable, enterprise-wide execution of hospital operations |
A hospital workflow automation platform provides a higher level of control by coordinating workflows across systems, teams, and locations. This platform-based approach transforms automation from a series of tactical fixes into a strategic capability that supports scale, governance, and long-term operational resilience.
How A Hospital Workflow Automation Platform Works
A hospital workflow automation platform works by monitoring clinical and operational events, applying predefined logic and intelligence, and coordinating tasks across systems and teams in real time.
At a high level, the platform functions as a continuous loop. It listens for events, decides what should happen next, executes actions, and monitors outcomes. This cycle repeats across every workflow the hospital runs.
1. Event Detection and Workflow Triggers
Every workflow begins with an event. This could be a physician order, a lab result, a discharge approval, or a missed task deadline. The platform connects to source systems and monitors these events as they occur.
Once an event is detected, the platform identifies the relevant workflow and triggers the next steps automatically. Teams no longer rely on manual handoffs or delayed notifications. Work moves forward based on system signals rather than memory.
2. Decision Logic and Intelligence Layer
After a workflow is triggered, the platform applies decision logic to determine the correct path. This logic can include clinical rules, operational policies, scheduling constraints, or AI-driven predictions.
For example, the platform may prioritize tasks based on patient acuity, staff availability, or capacity thresholds. Decisions remain transparent and configurable, allowing hospitals to define guardrails while still benefiting from intelligent automation. This balance keeps humans in control.
3. Task Coordination Across Teams
Once decisions are made, the platform coordinates execution. Tasks are assigned to the right roles, system updates are triggered automatically, and interdependent steps run in parallel when possible.
Because the platform understands task dependencies, it prevents downstream delays. Pharmacy, billing, transport, and nursing workflows stay aligned. Everyone works from the same execution logic, even across departments.
4. Monitoring, Escalation, and Exception Handling
Workflows rarely follow a perfect path. When tasks stall or conditions change, the platform detects deviations in real time. It then escalates issues based on predefined thresholds.
This approach prevents silent failures. Instead of discovering delays hours later, teams receive timely alerts. Leaders gain visibility into where intervention is required, allowing corrective action before patient care or throughput is affected.
5. Continuous Optimization
Over time, the platform captures execution data across workflows. This data highlights where delays occur, which steps consume the most time, and how frequently exceptions arise.
Hospitals use these insights to refine rules, adjust staffing models, or redesign workflows. As a result, automation improves continuously rather than becoming static. The platform evolves alongside operational needs.
A hospital workflow automation platform works by coordinating people, systems, and decisions through a shared execution layer. It listens for events, applies intelligence, orchestrates tasks, and enforces accountability in real time. By transforming how work flows across the hospital, the platform delivers control and scalability without disrupting care delivery.
Hospital Workflows Orchestrated at Enterprise Scale
An enterprise hospital workflow automation platform orchestrates clinical, operational, and administrative workflows across departments and facilities using shared rules, real-time coordination, and centralized governance. At enterprise scale, orchestration must span multiple hospitals, facilities, and service lines while still allowing local teams to execute workflows in context.
A workflow automation platform enables hospitals to manage this scale deliberately. At this level, isolated automation creates fragmentation. Orchestration replaces it with coordinated execution across the entire hospital system. It ensures that work moves consistently, regardless of where it starts or who performs it.
1. Clinical Workflows
Clinical workflows demand precision. Delays or missed steps directly affect care quality and safety. At enterprise scale, manual coordination struggles to keep up with patient volume, acuity variation, and cross-facility care delivery.
The platform orchestrates clinical workflows by aligning orders, tasks, and handoffs in real time. Care teams receive actions in sequence, supported by clear accountability. When conditions change, the workflow adapts without breaking continuity. This coordination reduces variability while preserving clinical judgment across units and locations.
2. Operational Workflows
Operational workflows determine how smoothly a hospital runs. Bed management, staffing coordination, transport, and housekeeping all influence patient flow. When these processes fall out of sync, bottlenecks surface quickly.
With platform orchestration, operational workflows respond to real demand signals. Discharges trigger cleaning and transport automatically. Admissions align with bed availability and staffing levels across facilities. Leaders gain near real-time insight into throughput, allowing capacity adjustments before congestion affects care delivery.
3. Administrative Workflows
Administrative workflows often operate behind clinical care but have an equal impact. Documentation delays, authorization hold-ups, and billing gaps can stall downstream processes and revenue cycles.
A workflow automation platform synchronizes these administrative steps with clinical activity. Documentation completion, approvals, and submissions follow governed paths tied to care events. This alignment reduces rework, shortens cycle times, and improves financial predictability without adding operational burden.
4. Standardization Without Sacrificing Local Flexibility
Enterprise hospitals require consistency, but no two departments or facilities operate identically. The platform supports standardized workflows while allowing local configuration. Policies govern how workflows behave, not how clinicians practice.
Shared rules enforce safety, compliance, and reporting. Local adjustments account for specialty-specific or facility-level realities. This balance enables system-wide reliability without forcing rigid uniformity.
Enterprise-scale orchestration transforms hospitals from loosely connected units into coordinated systems. A hospital workflow automation platform enables this shift by aligning clinical, operational, and administrative workflows under shared execution logic. The result is consistent performance, informed decision-making, and resilient operations across the health system.
Workflow Automation Showed 57% Improvement in Patient Discharge Rates
Patient discharge often looks simple on paper. In practice, it is one of the most fragmented workflows inside a hospital. Clinical decisions, documentation, pharmacy clearance, transport, billing, and housekeeping all move on different timelines. When even one step stalls, beds stay occupied longer than necessary.
A Six Sigma–led hospital study illustrates how powerful workflow automation can be when applied at the platform level. After redesigning the discharge process and introducing automated workflow coordination, the hospital achieved a 57% improvement in the proportion of patients discharged in under 50 minutes.
This gain did not come from faster clinicians. It came from removing coordination friction.
1. Why Discharge Delays Become Enterprise Problems
Discharge is the final step in care delivery, but it directly affects the first step for the next patient. When discharge slows down, emergency departments back up. Elective procedures get delayed. Bed utilization metrics start slipping, even when clinical capacity exists.
At the single-hospital scale, teams absorb these delays manually. At the multi-hospital scale, the same inefficiencies multiply. Leaders lose visibility into where discharge slows down and why. As a result, hospitals often invest in new beds or facilities when the real constraint lies in workflow execution.
Workflow automation addresses this by treating discharge as a coordinated, end-to-end process rather than a series of disconnected tasks.
2. What Changed in the Six Sigma Workflow Redesign
The Six Sigma project examined the full discharge journey, from physician clearance to patient exit. Instead of speeding up individual steps, the team focused on handoffs, waiting points, and task dependencies. Automation was introduced to sequence tasks automatically and eliminate unnecessary waiting.
After implementation, average discharge time dropped from over seven hours to just over four hours in intervention wards. Some waiting steps were reduced to zero. Importantly, these improvements were sustained, not one-time fixes, indicating a structural change in how work flowed.
This highlights a critical lesson for enterprises. The value of automation lies in orchestration, not isolated efficiency gains.
What This Metric Signals About Workflow Automation Platforms
A 57% improvement in discharge speed reflects more than faster execution. It signals tighter coordination across departments. Clinical staff no longer wait for downstream tasks to complete in silence. Administrative teams receive automated triggers instead of chasing updates. Leaders gain real-time insight into discharge status across units.
When this capability sits inside a hospital workflow automation platform, the impact extends beyond discharge. The same orchestration logic can apply to admissions, transfers, care coordination, and post-acute handoffs. One platform governs multiple workflows, using shared rules, visibility, and accountability.
This is where enterprise ROI begins to compound.
Features of a Hospital Workflow Automation Platform
A hospital workflow automation platform combines orchestration, intelligence, visibility, and governance to coordinate clinical, operational, and administrative workflows at enterprise scale.
The capabilities below form the foundation of such a platform. Together, they enable reliability without disrupting care delivery.
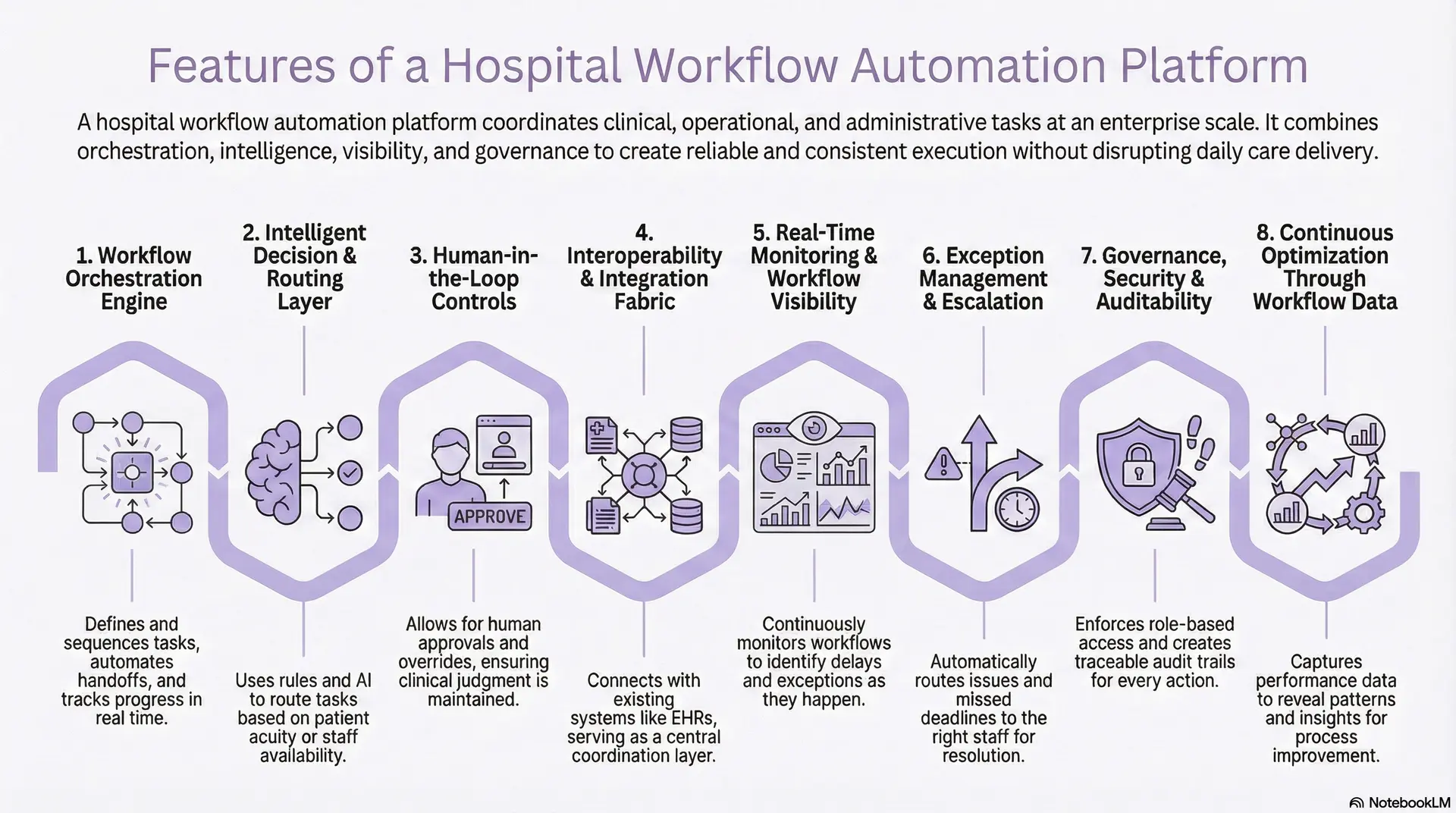
1. Workflow Orchestration Engine
The orchestration engine is the backbone of the platform. It defines how tasks are sequenced, which steps run in parallel, and how handoffs occur across departments. Workflows are modeled end-to-end rather than as isolated steps.
This engine tracks progress in real time. When a step completes, the next action triggers automatically. When a step stalls, delays surface immediately. This structure replaces manual chasing with predictable execution.
2. Intelligent Decision and Routing Layer
Hospitals operate on constant prioritization. A workflow automation platform embeds decision logic directly into execution. Rules, thresholds, and AI models help determine what happens next and who should act.
For example, the platform can route tasks based on patient acuity, staff availability, or operational load. Decisions remain transparent and adjustable. This allows hospitals to use intelligence without giving up control.
3. Human-in-the-Loop Controls
Not every decision should be automated. Clinical judgment and oversight remain essential, especially in complex or high-risk workflows.
The platform supports human checkpoints within workflows. Approvals, overrides, and acknowledgments appear where they matter most. Automation accelerates execution, while people retain authority over outcomes.
4. Interoperability and Integration Fabric
A hospital workflow automation platform does not replace existing systems. It connects them. The integration layer allows the platform to listen for events and trigger actions across EHRs, clinical systems, and enterprise applications.
By serving as a coordination layer, the platform avoids disrupting daily operations. Hospitals preserve existing investments while gaining cross-system visibility and control.
5. Real-Time Monitoring and Workflow Visibility
Execution without visibility creates blind spots. The platform continuously monitors workflows as they run. Leaders can see delays, exceptions, and workload distribution across teams and facilities.
This visibility shifts operations from reactive to proactive. Problems surface early, allowing intervention before patient care or throughput is affected.
6. Exception Management and Escalation
Hospital workflows rarely follow a perfect path. When tasks miss deadlines or conditions change, the platform responds automatically.
Escalation rules route issues to the right roles. Notifications replace guesswork. Instead of relying on after-the-fact reporting, teams address risks as they emerge.
7. Governance, Security, and Auditability
At enterprise scale, automation must be governed. The platform enforces role-based access, policy controls, and audit trails across all workflows.
Every action is traceable. Decisions are reviewable. Compliance becomes part of execution rather than a separate layer. This governance framework protects patient safety and organizational integrity.
8. Continuous Optimization Through Workflow Data
Every workflow generates data. The platform captures this information to reveal patterns in delays, rework, and resource utilization.
Hospitals use these insights to refine workflows over time. Adjustments happen through configuration rather than reimplementation. As operations evolve, the platform evolves with them.
The core capabilities of a hospital workflow automation platform work together to create controlled execution across the enterprise. By orchestrating tasks, embedding intelligence, maintaining oversight, and enforcing governance, the platform enables hospitals to operate with consistency, visibility, and scalability in complex care environments.
AI’s Role Within a Hospital Workflow Automation Platform
Within a hospital workflow automation platform, AI supports decision-making, prioritization, and prediction while the platform retains control over execution, governance, and accountability.
This distinction matters at enterprise scale. AI informs decisions, and the platform ensures those decisions translate into consistent action.
1. From Reactive Workflows to Predictive Coordination
Traditional hospital workflows react after something happens. A platform-enabled approach allows workflows to anticipate what is likely to occur next. AI models analyze patterns across admissions, diagnostics, staffing, and discharges to surface early signals.
For example, AI can predict discharge readiness, identify patients likely to face delays, or flag rising operational load. The platform then uses these signals to trigger preparatory steps in advance. As a result, work moves earlier rather than faster under pressure.
2. Intelligent Prioritization Without Loss of Control
Hospitals constantly juggle competing priorities. AI helps rank tasks based on context such as urgency, risk, and resource availability. What changes inside a workflow automation platform is how these priorities are applied.
The platform uses AI insights to recommend sequencing and routing. Final execution still follows defined rules and approvals. Leaders set boundaries, and AI works within them. This keeps prioritization consistent across teams and facilities.
3. Decision Support That Stays Inside the Workflow
AI delivers the most value when insights appear where work already happens. A workflow automation platform embeds AI-driven recommendations directly into task execution.
Instead of separate dashboards, clinicians and operations teams receive prompts within workflows they already use. This reduces cognitive load and improves adoption. AI becomes part of daily operations rather than an additional layer to manage.
4. Exception Detection and Risk Awareness
Many enterprise failures occur at the edges. AI helps identify anomalies that rules alone cannot catch. Unusual delays, repeated escalations, or abnormal workflow patterns surface earlier through machine learning.
When AI flags these conditions, the platform initiates escalation paths automatically. Human oversight remains central. AI highlights risk. The platform ensures accountability.
5. Learning From Execution, Not Just Data
AI models improve when grounded in real execution data. A workflow automation platform captures rich signals about how work actually flows, not how it was designed to flow.
This feedback loop allows models to refine predictions over time. Workflow rules evolve based on evidence. Automation becomes smarter because it learns from operations, not assumptions.
6. Guardrails That Preserve Trust and Compliance
Enterprise hospitals require transparency. AI decisions cannot be black boxes. A workflow automation platform enforces guardrails around AI use.
Models operate within defined scopes, and outputs are explainable. Decisions are logged, and overrides remain available. These controls protect patient safety and reinforce trust among clinicians and administrators.
AI strengthens a hospital workflow automation platform when it acts as an intelligence layer, not an autonomous operator. By predicting, prioritizing, and detecting risk within governed workflows, AI improves coordination without introducing uncertainty. When intelligence and execution work together, hospitals gain insight, control, and scalability in equal measure.
Compliance, Risk & Governance as Platform Foundations
A hospital workflow automation platform embeds compliance, risk controls, and governance directly into workflow execution to ensure safe, auditable, and regulation-aligned operations at enterprise scale.
This foundation allows hospitals to scale automation without increasing clinical, legal, or financial risk.
1. Regulatory Compliance Embedded Into Workflows
A hospital workflow automation platform must align with healthcare regulations by design. These include HIPAA and HITECH for patient data protection, GDPR where applicable, and regional healthcare privacy mandates.
Instead of enforcing compliance after work is done, the platform enforces it while work happens. Access controls, data handling rules, and approval paths are built directly into workflows. This reduces reliance on manual checks and post-hoc audits.
2. Auditability and End-to-End Traceability
Enterprise hospitals require defensible audit trails. Every action, decision, and handoff must be traceable.
The platform automatically records who initiated a task, when it was moved, how decisions were made, and what systems were involved. This level of traceability supports internal reviews, regulatory audits, and incident investigations without operational disruption.
Audit readiness becomes continuous rather than episodic.
3. Role-Based Access and Accountability
Risk increases when workflows lack clear ownership. A workflow automation platform assigns responsibilities explicitly through role-based execution.
Permissions control who can initiate, approve, modify, or override workflows. Escalation paths are predefined. Accountability remains visible at every step. This clarity reduces operational risk and protects clinical integrity.
4. Controls for Clinical and Operational Risk
Not all workflows should run fully autonomously. The platform enforces guardrails through human-in-the-loop checkpoints, thresholds, and exception rules.
High-risk steps trigger additional review. Deviations prompt escalation. This approach balances automation speed with patient safety and regulatory expectations.
Risk management becomes proactive rather than reactive.
5. Security and Data Protection
A platform-level approach strengthens security. Data encryption, secure integrations, and segregation of sensitive information are applied consistently across workflows.
Because the platform coordinates rather than stores unnecessary data, exposure is minimized, security policies apply uniformly, regardless of department or facility, reducing variation and attack surfaces.
6. Governance That Scales
As hospitals grow, governance complexity increases. The platform provides centralized policy definition with local execution. Enterprise leaders define standards for compliance, security, and reporting. Departments configure workflows within those boundaries. This model supports expansion without losing control.
Compliance, risk, and governance are not constraints on automation. They are what make enterprise-scale automation possible. By embedding regulatory alignment, a hospital workflow automation platform enables hospitals to innovate safely, scale confidently, and operate with control in highly regulated environments.
How a Workflow Automation Platform Sits Inside the Tech Stack
A hospital workflow automation platform sits above core clinical and business systems, coordinating workflows across applications without replacing existing hospital technology.
Rather than replacing EHRs, departmental systems, or financial platforms, the platform works alongside them. It listens to events, applies logic, and orchestrates actions across systems that already power daily hospital operations.
1. Positioned Above Core Clinical and Business Systems
At the foundation of the hospital tech stack sit systems such as EHR, HIS, LIS, RIS, PACS, pharmacy platforms, billing systems, and ERP tools. These systems remain the source of truth for clinical and operational data.
The workflow automation platform connects to these systems using secure APIs, HL7 and FHIR interfaces, and event streams. It does not replicate data models or duplicate workflows. Instead, it consumes system events and coordinates what should happen next. This preserves system stability while adding orchestration on top.
2. Integrated Through Existing Integration Layers
Most hospitals already rely on interface engines or integration platforms to move data between systems. A workflow automation platform uses this same layer rather than creating new point-to-point connections.
When an admission occurs or a discharge order is placed, the platform receives those signals through the integration layer. It then triggers downstream workflows across nursing, pharmacy, transport, and administration. This approach keeps integrations clean and scalable as the enterprise grows.
3. Connected to Data, Analytics, and AI Services
The platform also connects to analytics and AI services that support decision-making. Predictive models, document processing tools, and clinical decision support can be invoked at specific workflow steps.
For example, AI may assess discharge readiness or flag process delays. The workflow automation platform uses that insight to route tasks or escalate issues. Execution remains governed by workflow logic, while intelligence enhances timing and prioritization.
At the same time, workflow execution data feeds back into analytics systems. Hospitals gain visibility into cycle times, variation, and bottlenecks across facilities and service lines.
4. Delivered Through Familiar User Interfaces
Users do not need a new application for every workflow. The platform surfaces work where teams already operate. This includes embedded views inside EHRs, role-based dashboards for operations teams, and mobile-friendly task lists for frontline staff.
Tasks appear in clear queues with context and next steps. Status updates flow automatically. The platform adapts to existing workflows rather than forcing staff to adapt to yet another system.
5. Surrounded by Governance Controls
Around the entire stack sit identity and security services. The workflow automation platform integrates with single sign-on, role-based access controls, audit logging, and compliance frameworks.
Every action, escalation, and decision is logged. Permissions determine who can initiate or approve steps. This alignment ensures automation operates safely within enterprise governance requirements.
When a workflow automation platform sits correctly inside the tech stack, it avoids becoming another silo. It enhances coordination without disrupting existing systems. Hospitals gain orchestration without large-scale replacement projects.
How We Build Hospital Workflow Automation Platforms
At Intellivon, we use a structured, repeatable method so large enterprises know what will happen at every stage. Below is how we typically build a workflow automation platform for multi-hospital systems and high-volume facilities.
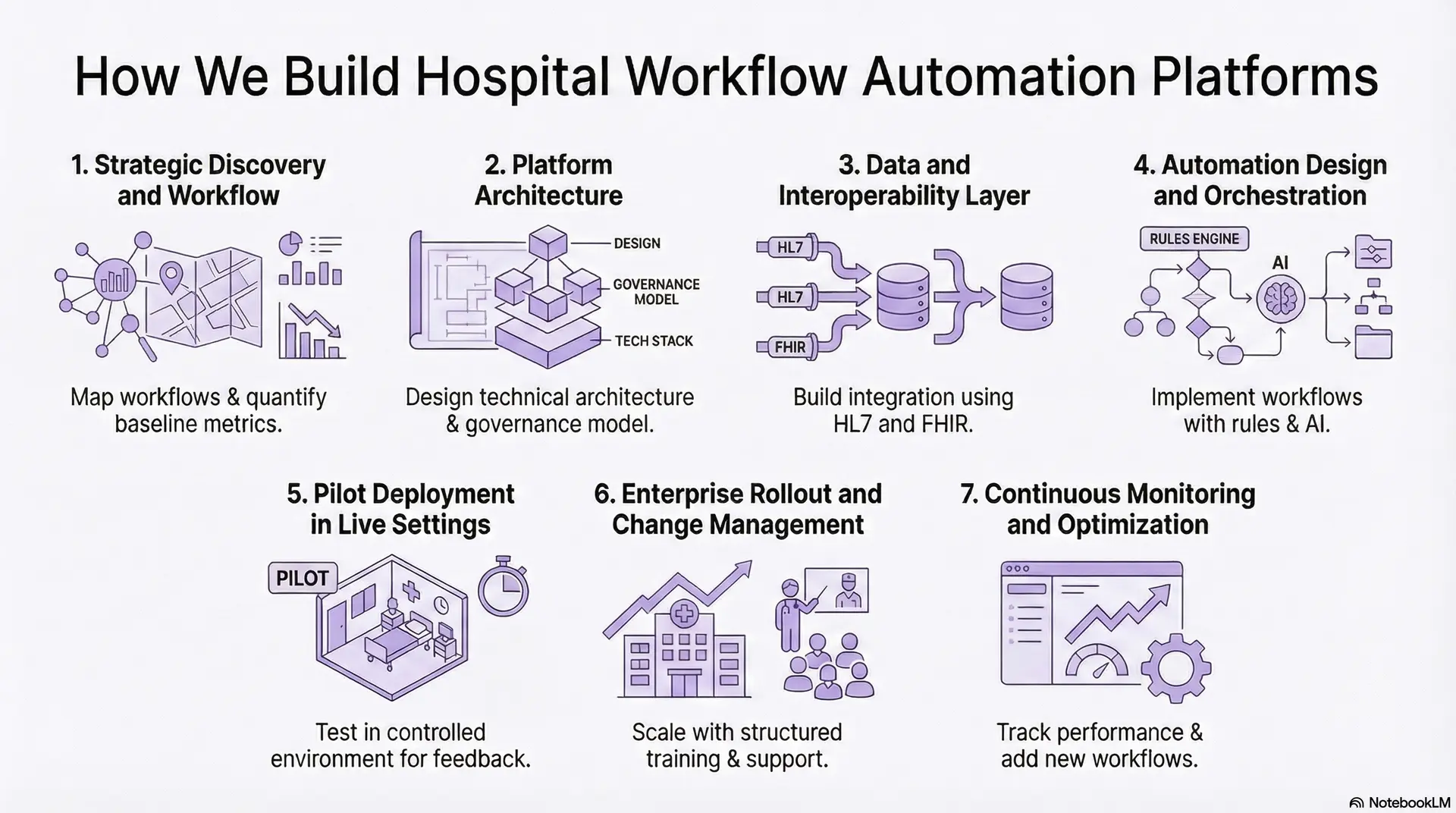
Step 1: Strategic Discovery and Workflow
We begin with a discovery phase focused on reality, not assumptions. Our team maps your current workflows across key domains, like admissions, discharge, bed management, surgery scheduling, diagnostics, billing, and administrative approvals. We sit with clinical, operational, and finance leaders to understand their constraints, delays, and risks.
We then quantify the baseline. Typical metrics include average discharge time, appointment lead time, claim denial rates, bed turnover, and task completion time for high-friction processes. This gives us a measurable “before” view that future automation can be judged against.
Step 2: Platform Architecture
Next, we move from problems to platform design. Intellivon’s architects define how the workflow automation platform will sit inside your environment. This includes event buses, orchestration engines, API gateways, data pipelines, and monitoring layers. We also define how the platform will co-exist with EHR, HIS, LIS, RIS, PACS, RCM, ERP, and existing automation tools.
In parallel, we design a governance model. This covers role-based access, approval hierarchies, audit trails, exception handling, and ownership of each process. The result is an architecture and governance blueprint your leadership can evaluate in plain language.
Step 3: Data and Interoperability Layer
Without clean, connected data, no automation platform works. Our engineers build the integration layer that allows the platform to “listen” and “act” across systems. We use standards such as HL7, FHIR, DICOM, X12, and secure APIs to consume events, trigger actions, and keep records in sync.
During this stage, we also address data quality, master data management, and identity mapping. For example, the same patient and encounter must be consistently recognized across EHR, billing, and scheduling. This makes every downstream workflow reliable and traceable.
Step 4: Automation Design and Orchestration
Once the platform backbone is ready, we design workflows that run on top of it. For each high-value use case, we break the process into discrete steps, like event triggers, decisions, tasks, approvals, and notifications. Our team defines which steps stay human-led and which can be automated by AI.
We then implement orchestration using rules engines and AI models. These models may predict no-shows, prioritize tasks, flag missing documentation, or recommend next best actions. The platform coordinates everything so the right task reaches the right person at the right time.
Step 5: Pilot Deployment in Live Settings
We never roll out a new platform across the entire hospital on day one. Instead, we select controlled environments such as one ward, one service line, or a defined process group. The platform runs in production, but within clear boundaries. We closely track operational metrics, staff feedback, and exception patterns.
During pilots, our team sits close to clinical and operational users. We refine rules, thresholds, notifications, and user interfaces based on real working days, not theoretical journeys. This de-risks full-scale deployment and builds internal champions.
Step 6: Enterprise Rollout and Change Management
Once the pilot proves value and stability, we scale. Intellivon manages a structured rollout plan across departments, sites, or the entire group. We align timelines with your internal initiatives, seasonal patient volumes, and regulatory windows.
Change management is handled with the same seriousness as technology. We design training journeys for clinical teams, back-office staff, and leadership. Playbooks, SOPs, and visual workflow guides help teams understand what has changed and why it matters.
Step 7: Continuous Monitoring and Optimization
A workflow automation platform is never “finished.” It should evolve with your hospital. We set up performance dashboards that track discharge times, task completion rates, exception frequency, escalation volume, and user adoption. Alerts highlight where automation is working and where friction remains.
Over time, we introduce new workflows onto the same platform. For example, a hospital might start with discharge, then add prior authorization, imaging order routing, or operating room scheduling. Because the foundation is already in place, each additional use case is faster and less risky to implement.
This step-by-step approach gives leaders a clear path from concept to measurable impact. It reduces transformation risk, avoids “big bang” failures, and creates an asset your organization can keep building on. With Intellivon, you are partnering to build a hospital workflow automation platform that becomes part of your long-term digital and clinical strategy.
Cost of Building Hospital Workflow Automation Platforms
The cost of building a hospital workflow automation platform depends on scope, integration depth, and phased rollout strategy rather than the number of automated workflows alone.
For large hospitals and multi-hospital systems, the cost of building a workflow automation platform is rarely driven by features in isolation. Costs typically increase when organizations attempt to automate too many workflows at once or treat the platform as a one-time deployment instead of a scalable foundation.
At Intellivon, we approach hospital workflow automation as a phased, use-case–driven investment. We align platform build decisions with operational priorities, compliance readiness, and near-term ROI. This approach controls capital risk while ensuring the platform remains extensible, governed, and enterprise-ready from the start.
Estimated Phase-Wise Cost Breakdown
Enterprise Hospital Workflow Automation Platform
| Phase | Description | Estimated Cost (USD) |
| Discovery & Workflow Blueprint | Enterprise workflow mapping, bottleneck analysis, stakeholder alignment, and regulatory scoping | 20,000 – 30,000 |
| Platform Architecture & Orchestration Design | Workflow engine design, scalability planning, governance, and control model | 25,000 – 40,000 |
| Integration & Interoperability Setup | EHR, LIS, RIS, PACS, RCM, ERP integrations using FHIR, HL7, APIs | 30,000 – 50,000 |
| Workflow Configuration & Orchestration | Clinical, operational, and administrative workflow modeling and sequencing | 30,000 – 45,000 |
| AI Enablement & Decision Logic | Predictive prioritization, exception detection, rule engines, and explainability | 25,000 – 40,000 |
| Security, IAM & Compliance Controls | Role-based access, audit logging, encryption, and compliance configuration | 18,000 – 30,000 |
| Testing, QA & Operational Validation | Workflow simulation, performance testing, compliance verification | 15,000 – 25,000 |
| Pilot Deployment & Training | Phased rollout, staff onboarding, workflow optimization | 18,000 – 30,000 |
Total Initial Investment Range: USD 100,000 – 150,000
This investment typically supports an enterprise-grade platform tailored to one or two high-impact workflows, such as discharge orchestration, patient flow management, or revenue-cycle task coordination.
Annual Maintenance and Platform Optimization Costs
Once live, ongoing costs focus on keeping the platform reliable, secure, and optimized as volumes and workflows expand.
These typically include infrastructure operations, integration support, security updates, AI model monitoring, and workflow performance tuning.
Estimated Annual Cost: 12–18% of the initial build
Approximate Range: USD 22,000 – 55,000 per year
When built with modular services and governed orchestration, these costs scale predictably as additional workflows are added.
Hidden Costs Enterprises Should Plan For
Even with strong upfront scoping, hospital workflow automation platforms introduce additional costs as adoption expands across the enterprise.
Common cost drivers include:
- Expanding automation into new clinical or operational workflows
- Supporting additional hospitals, facilities, or service lines
- Higher data, event, and messaging volumes as usage grows
- New compliance, audit, or reporting requirements tied to regulations
- Ongoing staff training as workflows and teams evolve
Planning for these early allows leadership to scale the platform deliberately without unexpected budget pressure.
Best Practices to Control Platform Costs
Healthcare enterprises that manage workflow automation investment effectively tend to follow a few consistent practices.
They typically:
- Start with one high-impact workflow before broad expansion
- Roll out additional workflows in phases aligned with budget cycles
- Use a modular, platform-based architecture rather than point solutions
- Embed security, compliance, and governance at the foundation
- Track operational and financial ROI within the first six months
This disciplined approach ensures the platform proves value early while keeping long-term costs predictable.
Top Hospital Workflow Automation Platforms Enterprises Use
Leading hospital workflow automation platforms combine orchestration engines, AI-driven decision support, and deep system integrations to coordinate workflows across clinical and operational environments.
Below are widely adopted, AI-powered platforms that enterprises use today. The goal is not to promote tools, but to illustrate how workflow automation platforms are being designed and deployed across hospitals.
1. Qventus
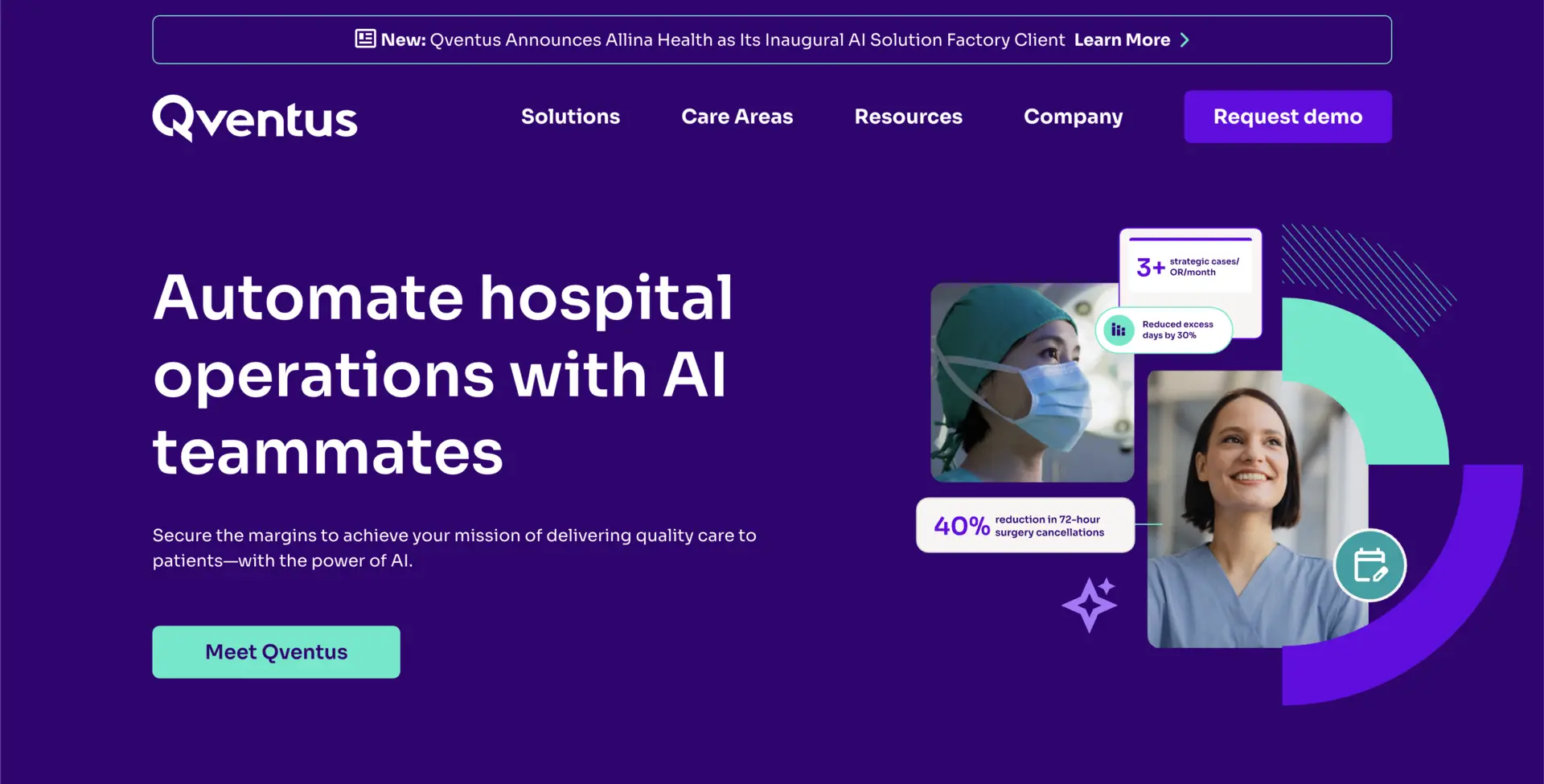
Qventus focuses strongly on hospital operations. Its platform uses AI models to monitor capacity, patient flow, and staffing signals. Based on real-time data, it recommends actions to reduce bottlenecks and improve throughput.
The platform works by ingesting events from EHRs and operational systems. AI analyzes patterns such as discharge delays or bed constraints, then pushes prioritized tasks to staff. Execution remains human-led, but guided through structured workflows. This approach shows how AI supports orchestration without replacing decision authority.
2. Notable
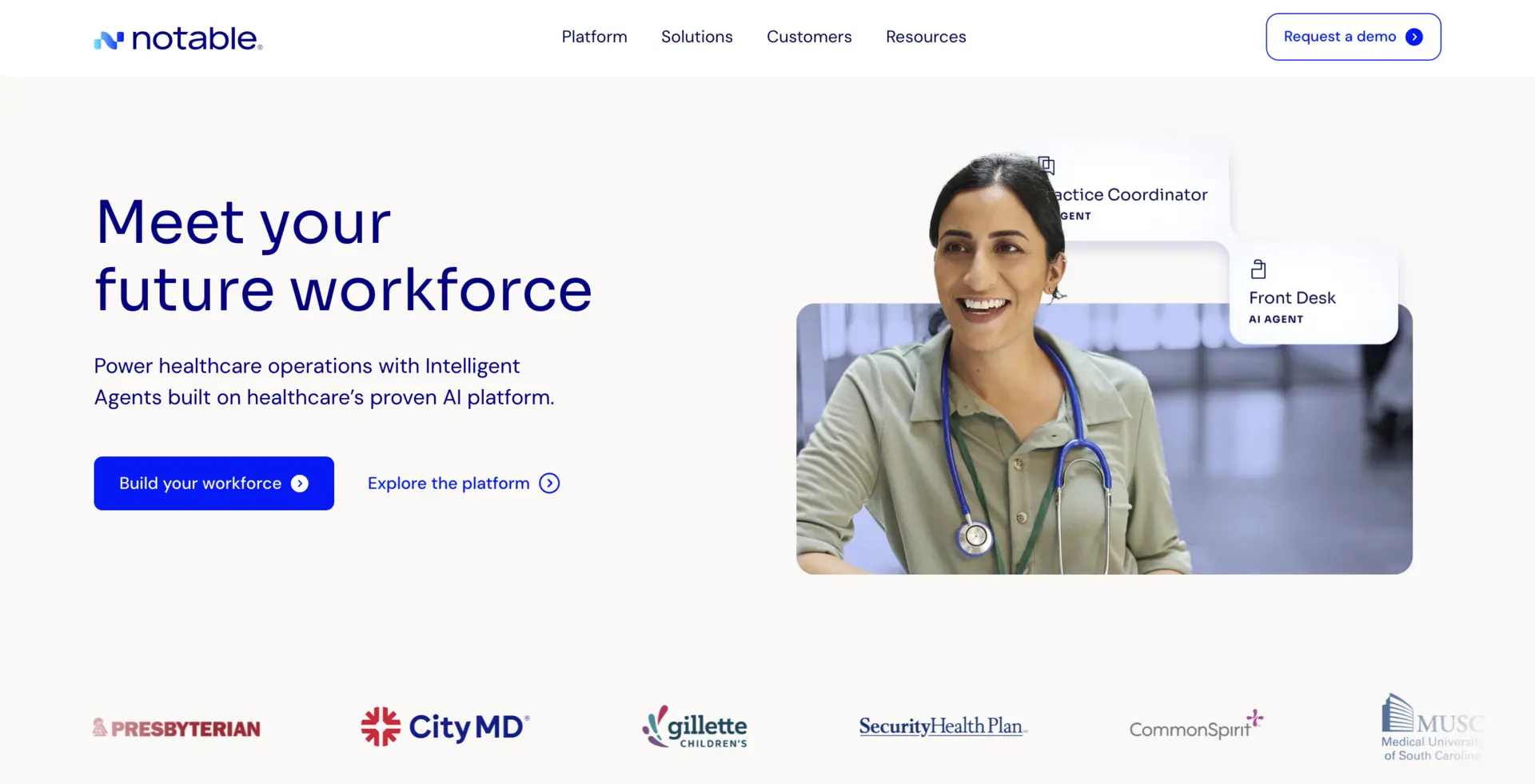
Notable positions itself as an enterprise automation platform for hospitals, with a strong focus on administrative and patient-facing workflows. It uses AI to automate scheduling, prior authorizations, documentation routing, and patient communications.
The platform operates through configurable workflows that connect intake, clinical documentation, and revenue operations. AI helps classify documents, extract key data, and route tasks faster. What makes it relevant is its platform design rather than isolated automation, allowing hospitals to expand use cases over time.
3. UiPath Healthcare
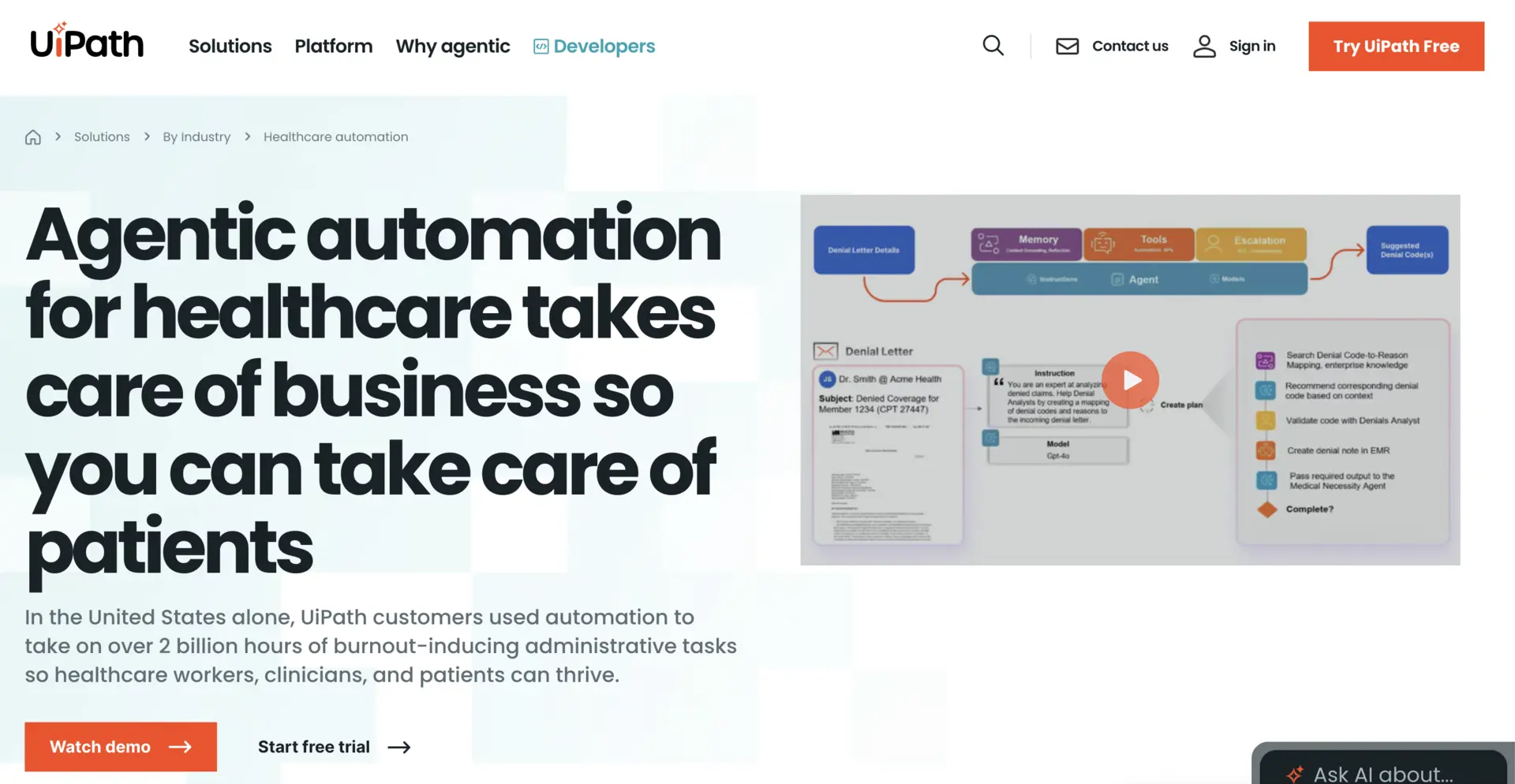
UiPath is often adopted by large health systems to automate high-volume administrative workflows. While not healthcare-exclusive, its AI-enabled RPA capabilities are used across billing, claims processing, prior authorization, and reporting.
The platform works by combining task automation with AI models that understand documents and unstructured data. Hospitals use UiPath to reduce manual effort, then layer governance and analytics on top. This illustrates how enterprises often start with RPA and later realize the need for higher-level orchestration.
4. ServiceNow Healthcare
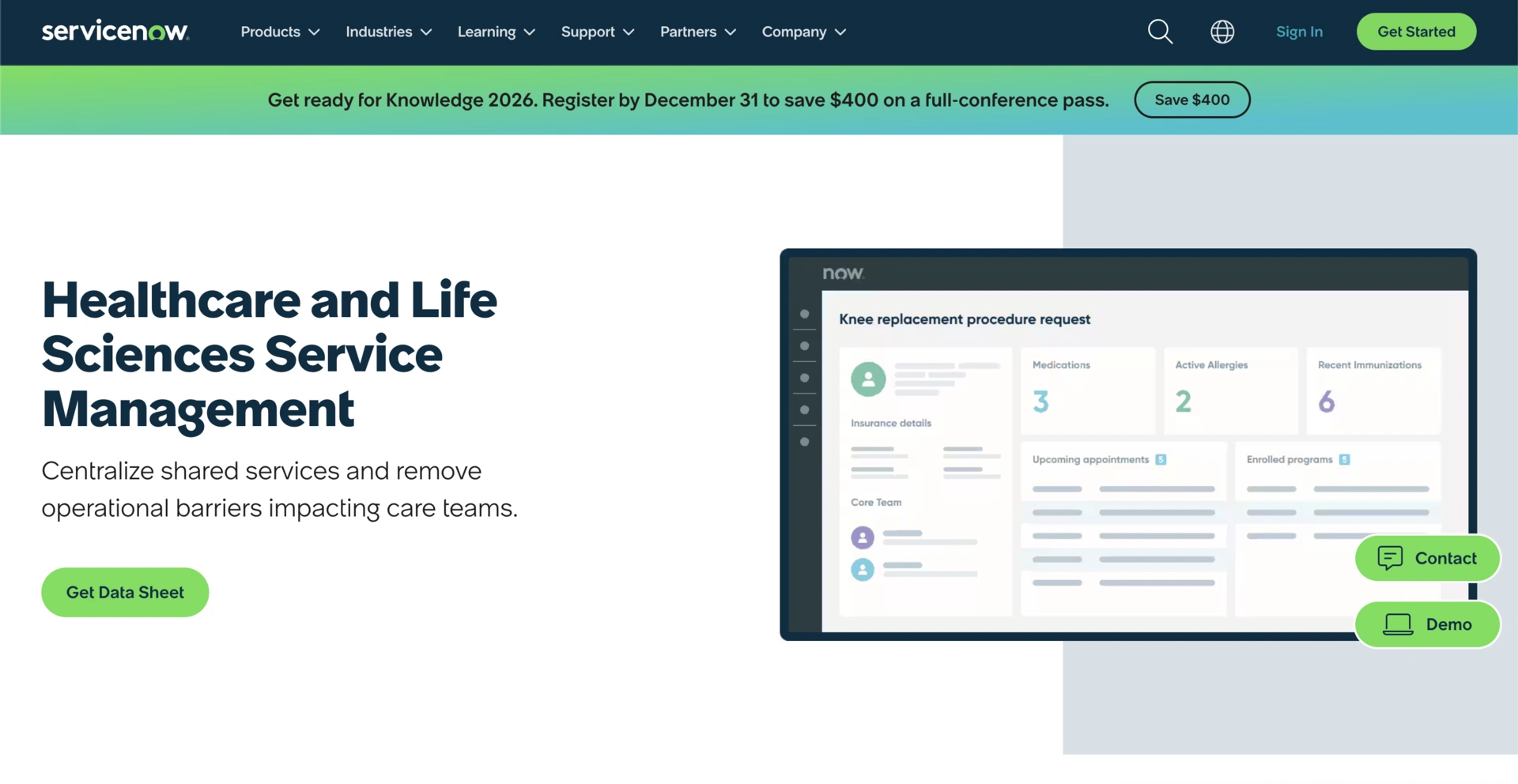
ServiceNow is used by some large healthcare enterprises as a workflow backbone for IT, compliance, and operational coordination. Its healthcare workflows integrate AI-based case routing, service management, and request orchestration.
The platform acts as a central workflow system that coordinates tasks across departments. AI assists by prioritizing incidents and predicting resolution needs. While not purpose-built for clinical workflows, it demonstrates how enterprise platforms can unify governance and execution across complex organizations.
Most platforms succeed when they coordinate workflows, not just automate steps. Where platforms struggle is when orchestration, governance, or cross-system visibility is limited. This gap is often what drives enterprises toward custom, platform-first solutions.
Conclusion
Hospital workflow automation is no longer about making individual tasks faster. It has become a foundational capability for how large healthcare enterprises operate, scale, and maintain control across increasingly complex environments. At the platform level, automation shifts hospitals from reactive coordination to predictable execution across clinical, operational, and administrative domains.
A well-designed hospital workflow automation platform creates clarity where fragmentation once existed. It aligns people, systems, and decisions through a shared orchestration layer. Over time, this improves throughput, reduces operational risk, strengthens compliance posture, and frees teams to focus on higher-value clinical and strategic work.
Build a Hospital Workflow Automation Platform With Intellivon
At Intellivon, we build enterprise-grade hospital workflow automation platforms that orchestrate clinical, operational, and administrative workflows through a single governed execution layer. Our platforms connect EHRs, HIS, LIS, RIS, PACS, staffing, billing, and AI services without disrupting live clinical, operational, or revenue workflows.
Each platform is engineered for modern healthcare enterprises. Solutions are compliant by design, resilient under real-world hospital volumes, interoperable across vendors, and built to deliver measurable operational, clinical, and financial ROI from the earliest deployment phases.
Why Partner With Intellivon?
- Compliance-First Workflow Architecture: Every platform aligns with HIPAA, HITECH, GDPR, where applicable, and CMS requirements.
- Orchestration-Native Automation: Workflows coordinate tasks, handoffs, approvals, and escalations across departments instead of automating isolated steps, ensuring predictable execution at enterprise scale.
- Workflow-Native User Experience: Tasks, alerts, and approvals surface directly inside existing EHRs, operational dashboards, and role-based interfaces, so teams do not need to change their daily systems.
- AI-Guided, Human-Controlled Execution: Embedded AI models support prioritization, risk detection, and exception handling while humans retain oversight, approvals, and accountability where it matters most.
- Vendor-Agnostic, Multi-Hospital Design: Our platforms integrate across heterogeneous EHRs, clinical systems, operational tools, and legacy infrastructure without locking enterprises into closed ecosystems.
- Scalable Across Enterprise Workflows: The same platform supports discharge orchestration, patient flow, staffing coordination, revenue-cycle workflows, and compliance operations without duplicating tooling.
- Zero-Trust Security and Workflow Governance: Identity-first access control, end-to-end encryption, data minimization, and continuous monitoring protect PHI and operational data across every workflow.
Book a strategy call with Intellivon to explore how a custom-built hospital workflow automation platform can improve throughput, reduce operational risk, and bring controlled, enterprise-scale execution across your health system.
FAQs
Q1. What is a hospital workflow automation platform?
A1. A hospital workflow automation platform is an enterprise system that coordinates clinical, operational, and administrative workflows across departments and facilities. It orchestrates tasks, decisions, and handoffs in real time while integrating with existing hospital systems and enforcing governance.
Q2. How does workflow automation improve hospital operations?
A2. Workflow automation improves hospital operations by reducing manual coordination, removing delays in handoffs, and making execution predictable. Hospitals see faster discharge times, improved throughput, clearer accountability, and better visibility into where workflows slow down.
Q3. Is hospital workflow automation compliant with healthcare regulations?
A3. Yes. When built correctly, hospital workflow automation platforms embed HIPAA, HITECH, and regional regulatory requirements directly into workflow execution. Role-based access, audit trails, and human-in-the-loop controls help ensure compliance as processes scale.
Q4. How long does it take to implement a hospital workflow automation platform?
A4. Implementation timelines vary by scope, but most enterprises launch their first high-impact workflow within 12 to 16 weeks. Broader rollout across departments and facilities typically follows a phased approach aligned with operational priorities.
Q5. How is a workflow automation platform different from RPA in hospitals?
A5. RPA automates individual tasks inside specific systems. A workflow automation platform goes further by orchestrating end-to-end workflows across multiple systems, managing exceptions, enforcing governance, and providing enterprise-wide visibility and control.