Many care organizations are reevaluating how patients transition between virtual visits, in-clinic appointments, remote monitoring, and follow-up services. They want each interaction to feel connected, predictable, and safe, no matter where it starts. However, most current systems were never made to support this combined model.
A hybrid virtual and in-clinic platform changes this dynamic. It provides a single space where a patient’s journey can move between channels without interrupting documentation, care plans, or the workloads of clinical teams. This change is increasingly viewed as crucial for organizations managing access, costs, and coordination.
Intellivon has spent over a decade developing healthcare platforms that bring together clinical workflows, integrate separate systems, and use AI where it adds real value. This blog shares that experience to explain how a hybrid virtual and in-clinic care platform is designed, built, and deployed at a large scale.
Key Market Insights of The Virtual Care Market
The global market for virtual hybrid care platforms is expanding rapidly. Estimates place the sector at roughly USD 18.64 billion in 2025, with projections reaching USD 50.28 billion by 2029 at a 28.2% growth rate.

Market Growth Drivers:
- Growth is driven by rising chronic conditions and increasing demand for convenient access, supported by stronger telecom networks and AI-enabled remote monitoring.
- Expanded reimbursement, hybrid triage workflows, and reduced clinician fatigue are encouraging broader system-wide adoption.
- Employers are pushing for integrated care models, while scalable SaaS platforms continue gaining traction across North America and fast-growing emerging markets.
Adoption Rates
- Surveys indicate that 82% of patients and 83% of clinicians now prefer the flexibility of hybrid care over single-channel models.
- About 70% of healthcare organizations have already connected these systems with their EHR environments.
- More than 775 provider groups are using AI-enhanced hybrid platforms in daily operations.
- Roughly 80% of ACOs rely on similar tools to track and improve value-based care performance.
Success Rates & Metrics
- Hybrid models achieve close to 90% patient satisfaction and engagement, far outperforming fragmented setups that average around 48%.
- Hybrid hospital-at-home programs report responsiveness ratings near 87%, with some achieving full recommendation scores in pilot surveys.
- AI-driven triage now manages approximately one-third of inbound inquiries and has contributed to measurable reductions in chronic care readmissions.
What is a Hybrid Virtual + In-Clinic Care Platform?
A hybrid virtual and in-clinic care platform is a coordinated environment that connects virtual visits, in-person appointments, remote monitoring, and follow-up services into one unified workflow. It acts as the operational layer that brings every touchpoint together, so patients never feel like they are entering a different system when switching channels.
The platform routes each patient to the right setting, supports shared clinical documentation, and keeps teams aligned across locations. It also manages scheduling, communication, and data flow in real time. Instead of treating virtual and physical care as separate tracks, it organizes them as parts of the same journey.
For organizations working to expand access, reduce fragmentation, and manage rising care demands, this type of integrated platform becomes the foundation for a scalable hybrid model.
How the Platform Works
A hybrid virtual and in-clinic care platform runs like a coordinated engine behind the scenes. It receives patient demand, applies routing rules, activates workflows, and keeps every interaction tied to a single record. Here is how that process typically unfolds.
1. Capture Demand Through a Single Front Door
Patients enter through one entry point. This could be a portal, app, call center, referral, or kiosk. The platform collects symptoms, intent, preferences, and key clinical details.
2. Run Triage and Channel Selection
Triage rules and AI models assess risk, urgency, and eligibility. The platform decides whether the next step should be virtual, in-clinic, home-based, or a combination.
3. Match to the Right Clinician and Location
The system checks provider skills, licenses, availability, and site capacity. It then schedules the patient into a virtual slot, clinic appointment, or hybrid pathway.
4. Orchestrate Workflows Across Teams
Tasks, forms, and care plans appear in clinician tools. Staff see one worklist for each patient, not separate lists for virtual and in-person activity.
5. Sync Documentation and Data in Real Time
Notes, orders, vitals, and remote monitoring data feed into one longitudinal record. Everyone works from the same information, regardless of channel.
6. Trigger Follow-Ups and Hybrid Journeys
The platform schedules follow-up visits, pushes reminders, and can move the patient between virtual and in-clinic care when needed.
7. Monitor Performance and Refine Rules
Analytics track access, utilization, outcomes, and costs. Leaders use these insights to adjust triage logic, capacity, and hybrid pathways over time.
Hybrid Virtual Clinic Platforms Have 87% High Responsiveness
A Mayo Clinic hybrid hospital-at-home evaluation reported 87% high responsiveness ratings and 100% recommendation scores, demonstrating strong patient trust in coordinated virtual and in-person care models.
Responsiveness matters because it reflects how quickly care teams act, how consistently they communicate, and how effectively they coordinate across settings. When hybrid systems are well-designed, patients feel supported rather than left to navigate different channels alone.
1. Why Responsiveness Scores Reach 87% in Hybrid Models
High responsiveness emerges from the way these models structure their teams. In the Mayo Clinic program:
- Care teams were reachable at any time during the care period.
- Patients consistently received timely updates throughout their recovery.
- Virtual clinicians and on-site staff worked as a single coordinated team.
This level of coordination reduces the chances of delays, unanswered questions, or disjointed instructions. It reflects a workflow design where communication tools, task routing, and escalation rules are all integrated into one platform rather than spread across separate systems.
2. Integrated Touchpoints Drive 100% Recommendation Rates
A major reason the program achieved a 100% recommendation score is the seamless transition between virtual and in-person care. Patients were not asked to repeat information, reintroduce their symptoms, or navigate different systems.
Instead:
- Virtual check-ins are fed directly into in-home clinical visits.
- Remote monitoring data triggered timely outreach and follow-ups.
- Care tasks stayed synchronized across both care environments.
Patients experienced the care journey as one continuous pathway, not a series of disconnected steps. That continuity is what makes hybrid models feel safe, coordinated, and support-ready.
What These Metrics Mean for Enterprise Strategy
For leaders evaluating hybrid platforms, the responsiveness and recommendation scores are more than impressive statistics. They point to deeper architectural strengths:
- Aligned workflows reduce clinical risk.
- Real-time communication lowers avoidable escalations.
- Unified teams improve trust and adherence.
- Integrated data flows eliminate fragmentation.
These outcomes also influence operational performance by reducing readmissions, improving satisfaction metrics, and supporting value-based care benchmarks.
The 87% responsiveness score and 100% recommendation rate from the Mayo Clinic hybrid hospital-at-home study demonstrate that hybrid models can outperform traditional setups when built with coordinated workflows. They show that patients value not just convenience, but consistency and reliability across every interaction.
Use Cases of Hybrid Virtual + In-Clinic Care Platforms
Hybrid virtual clinic platforms support virtual-first care, chronic disease programs, behavioral health, specialty diagnostics, urgent routing, and post-acute recovery.
Hybrid models add the most value when they support full care journeys instead of isolated visits. The following use cases show how blended pathways improve access, efficiency, and clinical consistency.
1. Virtual-First Care
Many journeys now begin with a virtual consult. The platform handles intake, symptom review, and early assessment. When a physical exam, imaging, or procedure is needed, it shifts the patient to an in-clinic visit without repeating information.
This approach reduces unnecessary clinic volume, improves appointment availability, and gives patients a smoother experience. It also helps organizations manage demand without adding infrastructure.
2. Chronic Care Programs
Patients managing long-term conditions benefit from continuous digital oversight. Remote monitoring devices capture daily readings, while virtual touchpoints allow quick intervention when symptoms change.
In-clinic visits are reserved for moments that genuinely require hands-on evaluation. This reduces travel, improves disease stability, and enables teams to manage larger populations with fewer disruptions.
3. Behavioral and Maternal Health
Specialties like behavioral health and maternal care fit naturally into hybrid workflows. Therapy sessions, prenatal education, and routine check-ins happen virtually. More detailed assessments take place in person when needed.
The platform keeps notes, reminders, and care plans unified, allowing clinicians to maintain continuity across settings. This consistency strengthens trust and reduces missed steps during high-touch care journeys.
4. Specialty Care and Recovery
Hybrid pathways support specialty consults, diagnostics, and post-surgical recovery. A specialist may begin with a virtual consult, send the patient for imaging, and review results online.
Post-surgical programs also rely on virtual monitoring for daily progress updates, with clinic visits reserved for complications or wound checks. Urgent care triage further benefits from hybrid routing, sending low-risk cases to virtual care and high-risk cases to the appropriate site.
5. High-Coordination and Multi-Team Care
Patients with complex needs often require input from several teams. Hybrid platforms give clinicians, nurses, social workers, and specialists a unified view of tasks, notes, and care plans. Virtual and in-person interactions contribute to the same record, so nothing gets lost during transitions.
This model is particularly effective for transitions of care after hospital discharge. Daily virtual check-ins provide close oversight during early recovery, while in-clinic milestones ensure safe progression. Multi-team coordination reduces duplication, avoids missed steps, and improves outcomes for high-risk populations.
Hybrid use cases succeed when every interaction feels connected. When the platform coordinates care across digital and physical environments, organizations gain efficiency, patients experience smoother journeys, and teams work with greater clarity.
Key Features of a Hybrid Virtual + In-Clinic Care Platform
Core features include a digital front door, omnichannel communication, virtual care tools, in-clinic workflow integration, full EHR interoperability, unified care plans, and a compliant billing layer.
These features form the foundation that allows patients, clinicians, and operations teams to work within one coordinated environment instead of toggling between disconnected systems.
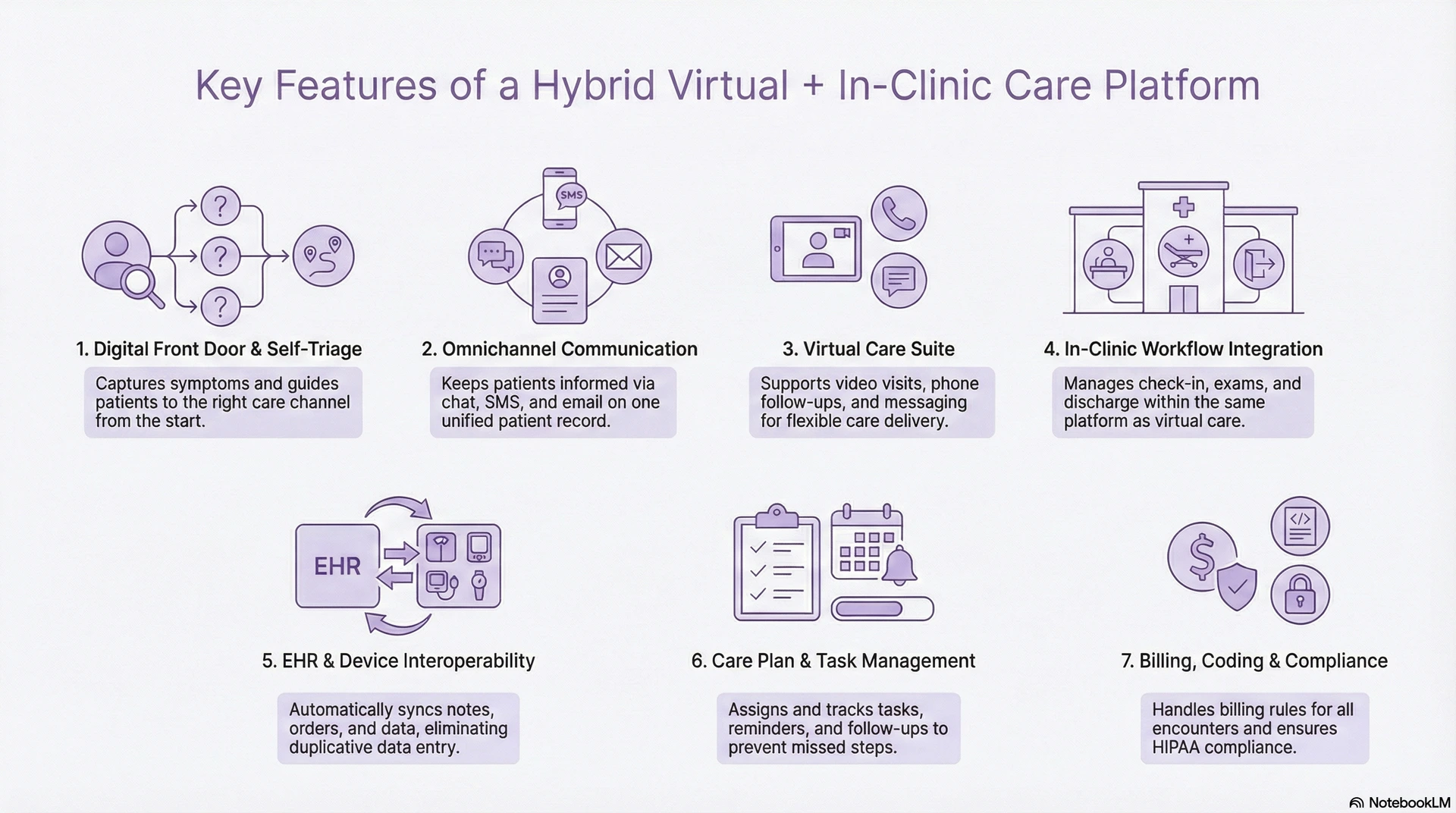
1. Digital Front Door + Self-Triage
The digital front door captures symptoms, intent, and patient preferences through guided forms, chat, voice, or app-based flows. Self-triage tools, supported by rules and AI, assess risk and determine whether the patient should enter a virtual consult, schedule a clinic visit, or move into remote monitoring.
This creates a structured entry point that improves access, reduces uncertainty for patients, and ensures the right channel is chosen from the start.
2. Omnichannel Communication Layer
A hybrid platform needs consistent communication across every stage of the journey. Secure chat, SMS reminders, email notifications, voice calls, and app alerts all connect to the same patient record.
This keeps patients informed, reduces no-shows, and creates reliable handoffs between virtual care teams and in-clinic staff without adding manual work.
3. Virtual Care Suite
The virtual care suite supports synchronous and asynchronous interactions. Patients can meet clinicians over video, receive follow-ups by phone, send messages for quick questions, or complete store-and-forward consultations for non-urgent needs.
These flexible touchpoints reduce clinic load, improve convenience, and allow clinicians to manage more patients without compromising care quality.
4. In-Clinic Workflow Integration
Hybrid platforms must support all in-clinic tasks, including check-in, vitals, room assignment, nurse intake, provider exams, orders, and discharge steps. These workflows appear inside the same platform that manages virtual visits.
This eliminates the usual fragmentation between digital and physical care, giving teams a consistent view of tasks, documentation, and patient status across both settings.
5. Interoperability With EHR and Devices
The platform integrates with EHR systems using FHIR, HL7, and secure APIs. Orders, notes, labs, diagnoses, billing codes, and visit summaries flow automatically. It also connects with remote monitoring devices and wearables, feeding real-time data into care workflows.
This interoperability keeps clinicians informed and eliminates duplicative data entry that often slows operations.
6. Care Plan + Task Management
Every patient journey generates tasks, reminders, education steps, and follow-up actions. The platform assigns these tasks automatically, routes them to the right team, and tracks completion across virtual and in-person interactions.
This prevents missed steps, improves handoffs, and ensures that chronic care, behavioral health, maternal programs, and specialty pathways stay organized.
7. Billing, Coding, and Compliance Layer
Hybrid platforms handle billing rules for virtual visits, in-clinic encounters, diagnostics, and remote monitoring. Coding prompts help clinicians document accurately, while compliance tools align with HIPAA, GDPR, and payer requirements.
This reduces administrative burden and protects revenue integrity as organizations scale hybrid care models.
These features work together to create a unified, predictable, and scalable hybrid care environment. When digital and physical workflows operate through the same coordinated platform, organizations gain efficiency, clinicians experience less friction, and patients receive a smoother, more connected care journey.
Advanced AI-Powered Features
AI gives a Hybrid Virtual + In-Clinic Care Platform the intelligence it needs to operate at scale. It strengthens decision-making, automates clinical and operational tasks, and keeps virtual and in-person workflows tightly coordinated.
These capabilities allow organizations to deliver consistent care without increasing workload across teams.
1. AI Triage and Routing
AI analyzes symptoms, patient history, and urgency markers to guide individuals to the right care setting. The Hybrid Virtual + In-Clinic Care Platform then routes them to a virtual visit, an in-clinic appointment, or urgent escalation.
This improves safety, reduces unnecessary clinic traffic, and ensures patients reach the appropriate channel quickly.
2. Demand and Capacity Forecasting
Machine learning models forecast appointment demand, staffing needs, and peak load across both virtual and physical sites. The platform helps leaders rebalance resources and avoid bottlenecks before they disrupt care.
This allows the Hybrid Virtual + In-Clinic Care Platform to run smoothly even during periods of high volume or fluctuating demand.
3. Risk Stratification for High-Risk Patients
AI reviews vital trends, adherence patterns, and historical data to flag early signs of deterioration. These insights guide virtual follow-ups or in-clinic assessments before conditions worsen.
For chronic care programs, this capability makes the Hybrid Virtual + In-Clinic Care Platform a proactive tool rather than a reactive one.
4. No-Show and Cancellation Prediction
Predictive models identify patients likely to miss appointments. The platform then triggers reminders, alternative slots, or a virtual-first pathway when appropriate.
This improves operational flow and enhances the efficiency of both virtual and in-clinic schedules.
5. Ambient Clinical Documentation
AI-powered speech and text tools capture clinical conversations and generate structured summaries. Documentation from both virtual and in-clinic visits flows into a unified record.
This reduces administrative workload and strengthens the accuracy of the Hybrid Virtual + In-Clinic Care Platform’s clinical data.
6. Continuous Monitoring Insights From Devices
AI analyzes data from wearables, sensors, and remote monitoring devices, identifying risks or abnormal trends. It can recommend virtual outreach or an immediate in-clinic evaluation.
This continuous insight helps the Hybrid Virtual + In-Clinic Care Platform support high-risk populations with timely intervention.
AI transforms the Hybrid Virtual + In-Clinic Care Platform from a coordination tool into an adaptive, learning system. When applied thoughtfully, AI enhances patient safety, improves clinical decision-making, and creates stronger operational resilience across all care settings.
Technical Architecture of a Hybrid Virtual + In-Clinic Care Platform
The technical architecture of a Hybrid Virtual + In-Clinic Care Platform spans experience, workflow, integration, data, and security layers built on interoperable, cloud-native services.
1. Experience Layer
The experience layer includes patient apps, portals, kiosks, clinician workstations, and dashboards for operations teams.
Patients use this layer to book visits, join virtual sessions, complete forms, and receive instructions. Clinicians see worklists, documentation screens, and decision support. Operations teams view capacity, performance metrics, and alerts.
Everything in this layer connects back to shared services and data, so users see consistent information regardless of channel.
2. Orchestration and Workflow Layer
This layer is the “brain” of the Hybrid Virtual + In-Clinic Care Platform. It manages triage, routing, scheduling logic, task creation, and care pathways. Rules engines and workflow services decide when a patient should stay virtual, move to a clinic, or enter a post-acute or monitoring program.
Workflows trigger events such as notifications, task assignments, or data updates. This keeps teams aligned and ensures each journey follows a predictable, governed path.
3. Integration Layer
The integration layer connects the platform to EHRs, remote monitoring tools, telehealth vendors, call centers, labs, and other enterprise systems. It relies on standards such as FHIR, HL7, DICOM, and secure APIs.
This layer handles data mapping, transformation, and message routing. It allows the Hybrid Virtual + In-Clinic Care Platform to sit alongside existing investments rather than replacing them, which is critical for large health systems.
4. Data and Intelligence Layer
Here, the platform collects clinical data, operational metrics, event logs, and device streams. It usually combines an operational data store for real-time workflows with an analytics warehouse or lake for deeper insights.
AI models for triage, forecasting, risk scoring, and documentation run within this layer. Their outputs flow back into workflows and user interfaces, turning raw data into actions that matter for clinical and operational decisions.
5. Security and Compliance Layer
The final layer enforces access control, encryption, auditing, and monitoring. It ensures the Hybrid Virtual + In-Clinic Care Platform complies with HIPAA, GDPR, where relevant, and internal governance policies.
Capabilities here include identity and role management, key and secret management, logging, intrusion detection, and performance monitoring. This layer also supports incident response and ongoing risk assessment.
When these layers are designed to work together, the technical architecture becomes a stable foundation for hybrid care. Virtual and in-clinic services can evolve, but the core platform still delivers a single, coordinated experience for patients, clinicians, and leaders.
How We Build Hybrid Virtual + In-Clinic Care Platforms
Building a Hybrid Virtual + In-Clinic Care Platform requires structured discovery, workflow design, interoperability planning, engineering, AI integration, piloting, and enterprise-scale optimization.
The steps below outline how we approach these implementations at enterprise scale.

1. Discovery and Ecosystem Mapping
Every engagement begins with a clear understanding of the current ecosystem. We review patient journeys, virtual care tools, clinic workflows, existing EHR integrations, and operational bottlenecks.
This helps identify where fragmentation occurs and which pathways offer the highest ROI for hybrid deployment.
2. Define Hybrid Care Pathways
We work with clinical, operational, and digital teams to design the hybrid pathways that matter most, which are virtual-first care, chronic care programs, diagnostics flows, or post-acute recovery.
Each pathway includes routing rules, triage logic, capacity settings, clinical guardrails, and escalation structures.
3. Architecture and Interoperability Planning
Next, we design the technical blueprint. This includes the workflow engine, data pipelines, integration patterns, AI services, and observability tools.
We map EHR, RPM, telehealth, scheduling, and analytics integrations using HL7, FHIR, and secure APIs, ensuring the platform fits cleanly into the enterprise environment.
4. Platform Engineering
We build the orchestration layer, communication tools, clinician consoles, patient experiences, and real-time data services.
This stage emphasizes modular, cloud-native engineering so each component can evolve without destabilizing the broader platform.
5. AI and Decision Support Integration
Once the core platform is stable, we integrate AI for triage, routing, risk scoring, demand forecasting, and documentation support.
AI outputs are embedded within clinical workflows so they enhance decision-making without adding complexity.
6. Pilot Deployment and Clinician Adoption
We launch controlled pilots with specific service lines, often primary care, behavioral health, or post-acute programs.
Clinicians receive tooling, training, and workflow support. Feedback loops help refine routing rules, tasks, and user flows before scaling.
7. Scale, Optimize, and Govern
When the platform proves stable and effective, we expand to more clinics, departments, or markets.
We establish ongoing governance for quality, compliance, and model performance, ensuring the Hybrid Virtual + In-Clinic Care Platform remains reliable as demand and service lines grow.
This structured approach ensures the platform is not just technically sound but also clinically intuitive, operationally efficient, and ready to support enterprise-wide hybrid care models.
Cost to Build a Hybrid Virtual + In-Clinic Care Platform
The cost of building a Hybrid Virtual + In-Clinic Care Platform varies widely based on scope, integration needs, and whether the platform is designed for a single service line or enterprise-wide deployment. Expenses increase when organizations attempt to support multiple specialties, advanced AI triage, and deep EHR interoperability in the first release.
At Intellivon, we design hybrid care platforms around one well-defined, high-impact pathway, such as virtual-first primary care, chronic care, or post-acute recovery. This phased approach reduces upfront investment, keeps clinical risk low, and ensures the platform can scale cleanly across departments, markets, or population segments.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost (USD) |
| Clinical & Operational Discovery | Define hybrid pathways, triage rules, care models, staffing flows, and KPIs | 10,000 – 20,000 |
| Architecture & Workflow Blueprint | Platform modules, orchestration layer, routing logic, interoperability mapping | 12,000 – 25,000 |
| EHR & Third-Party Integrations | FHIR/HL7 setup, telehealth, scheduling, RPM devices, identity systems | 15,000 – 40,000 |
| Hybrid Workflow Engine Development | Triage engine, capacity logic, task routing, clinician dashboards | 18,000 – 45,000 |
| Virtual Care Modules | Video, phone, chat, async consults, documentation tools | 10,000 – 30,000 |
| In-Clinic Workflow Integration | Check-in, vitals, nurse intake, orders, discharge workflows | 12,000 – 35,000 |
| AI Models & Intelligence Layer | AI triage, capacity forecasting, risk scoring, and documentation support | 15,000 – 40,000 |
| Governance, Security & Compliance | HIPAA, GDPR, audit logging, RBAC, encryption, consent flows | 8,000 – 15,000 |
| Testing & Clinical Validation | Workflow tests, safety checks, documentation review, simulation runs | 6,000 – 12,000 |
| Pilot Deployment & Training | Rollout, clinician onboarding, refinement cycles | 7,000 – 15,000 |
Total Initial Investment Range: USD 80,000 – 300,000
This supports a full Hybrid Virtual + In-Clinic Care Platform designed for one high-value care program, ready for expansion across additional specialties.
Annual Maintenance and Optimization Costs
Annual costs remain stable when the platform uses modular services and a governed architecture.
| Estimated Annual Cost | % of Initial Cost |
| USD 12,000 – 45,000 per year | 12–18% |
These costs cover infrastructure, integration updates, workflow refinements, AI model recalibration, compliance updates, and performance monitoring.
Factors Affecting The Cost Of Building A Hybrid Virtual+In-Clinic Care Platform
The investment required to build a Hybrid Virtual + In-Clinic Care Platform depends on how ambitious the first release is and how deeply the platform needs to integrate into a health system’s digital ecosystem. These factors determine both engineering effort and long-term operational cost.
Below are the major elements that shape the total cost.
1. Scope of Clinical Workflows
Platforms designed for a single care program, such as virtual-first primary care or post-acute recovery, cost far less than those spanning multiple service lines.
More specialties mean additional triage rules, routing patterns, forms, documentation templates, and clinical logic.
2. Level of EHR and System Integration
Lightweight integrations (e.g., scheduling or patient demographics) cost significantly less than deep, bidirectional EHR workflows.
FHIR/HL7 connectivity, CCD/CCDA exchanges, clinical note syncing, order entry, and billing integration all increase the engineering footprint.
3. AI Depth and Intelligence Requirements
Basic rule-based triage is inexpensive. Complex AI, such as risk scoring, deterioration prediction, capacity forecasting, or ambient documentation, requires advanced pipelines, model training, monitoring, and governance.
4. Virtual Care Capabilities Needed
Simple video visits are low-cost. Adding phone workflows, secure messaging, async consults, automated routing, and consolidated clinical worklists increases development and integration complexity.
5. In-Clinic Workflow Integration
Platforms that support check-in, vitals capture, intake, orders, and discharge generate additional UX, integration, and orchestration needs. The deeper the clinic workflow support, the higher the engineering effort.
6. Compliance and Security Expectations
Costs rise when enterprises require:
- Full HIPAA and GDPR readiness
- Zero-trust architecture
- Audit logging across all modules
- Consent and data governance flows
- PHI encryption and key rotation
These controls add design, implementation, and testing requirements.
7. Device Ecosystem Integration
If the hybrid platform includes home-based monitoring, device integration costs increase. APIs, SDKs, data ingestion rules, and signal normalization pipelines often require additional engineering.
The cost of building a Hybrid Virtual + In-Clinic Care Platform hinges on how many workflows you include, how deeply it must integrate with existing systems, and how much intelligence and automation your organization expects.
At Intellivon, we help organizations design cost-controlled Hybrid Virtual + In-Clinic Care Platforms built around measurable outcomes, scalable workflows, and compliance-first engineering. Our phased builds deliver predictable investment and create a foundation ready for enterprise-wide hybrid care transformation.
Challenges in Building a Hybrid Virtual + In-Clinic Platform
Key challenges include fragmented systems, workflow misalignment, data inconsistency, clinician adoption, interoperability gaps, and the need for strong governance, each of which is solvable through unified platform design.
Below are the major challenges organizations encounter, with clarity on how Intellivon addresses each through platform design and implementation.
1. Fragmented Legacy Systems
Many organizations run telehealth tools, clinic systems, scheduling applications, and analytics platforms that don’t communicate smoothly. This fragmentation makes it difficult to maintain a unified patient journey.
Intellivon’s Solution
We create an orchestration layer that sits above existing systems. It unifies routing, documentation, tasks, and data flow so virtual and in-clinic interactions feel connected without forcing a system replacement.
2. Misaligned Clinical and Operational Workflows
Virtual teams and in-clinic teams often follow different routines, documentation habits, and escalation practices. When these workflows remain siloed, hybrid models struggle to scale.
Intellivon’s Solution
We map end-to-end pathways with clinical, operational, and digital stakeholders. This ensures workflows are synchronized, predictable, and supported by a platform designed around real-world behaviors, and not theoretical diagrams.
3. Inconsistent Data Across Care Settings
Virtual visits, device data, clinic documentation, and administrative updates often end up stored in separate locations. This creates gaps that affect decision-making and care quality.
Intellivon’s Solution
Our data fabric combines inputs from EHRs, RPM devices, telehealth tools, and scheduling systems into one longitudinal record. Clinicians always see accurate, up-to-date information, no matter where the visit took place.
4. Clinician Adoption and Workflow Change
Even the best technology fails without clinician support. If hybrid tools add extra clicks or disrupt established routines, adoption drops quickly.
Intellivon’s Solution
We design interfaces and workflows that fit into existing habits. Virtual notes, in-clinic tasks, and messaging tools all appear in one view. We also run guided pilots and provide training that emphasizes ease rather than complexity.
5. Interoperability and Vendor Limitations
Hybrid platforms must integrate with multiple EHRs, telehealth vendors, RPM devices, and identity systems. Each has its own standards, constraints, and compliance expectations.
Intellivon’s Solution
We use HL7, FHIR, secure APIs, and event-driven architectures to bridge these systems. The platform becomes vendor-agnostic, ensuring enterprises can grow without being restricted by a single tool.
6. Scaling Beyond the Pilot Phase
Many organizations succeed with small hybrid pilots but struggle to expand across departments or regions. Scaling introduces gaps in consistency, user training, and workflow coordination.
Intellivon’s Solution
We design hybrid platforms using modular, cloud-native components. This allows organizations to scale horizontally, so that new care programs, clinics, or service lines can be added without rebuilding foundational elements.
Hybrid care succeeds only when technology, workflows, and governance operate as a single system. These challenges are real, but each one is solvable through a platform built with orchestration, interoperability, and clinician-centered design at its core.
With Intellivon’s structured approach, organizations move from fragmented digital tools to a coordinated Hybrid Virtual + In-Clinic Platform capable of supporting modern care delivery at enterprise scale.
Conclusion
Hybrid care is no longer a future concept. It is a practical operating model that blends virtual access, in-clinic services, remote monitoring, and coordinated follow-ups into one continuous system. The organizations that move early are already seeing the benefits—stronger patient experience, better clinical oversight, improved resource utilization, and measurable cost reductions.
The real advantage comes from the platform itself. When triage, routing, scheduling, documentation, analytics, and communication run through one unified layer, the entire care journey becomes clearer and more predictable. Virtual and in-clinic teams stop working in parallel and start working as one. Patients feel supported, clinicians experience less friction, and leadership gains visibility into how care is delivered at every step.
Build A Hybrid Virtual + In-Clinic Care Platform With Us
At Intellivon, we build enterprise-grade hybrid care platforms that connect virtual visits, in-clinic workflows, remote monitoring, and EHR-integrated documentation into one coordinated system. Our platforms remove fragmentation by unifying triage, scheduling, clinical tasks, and follow-ups across both care settings. This creates a consistent experience for patients and an efficient workflow for clinicians.
Each solution is engineered for modern healthcare enterprises. Platforms are compliant by design, resilient under real clinical load, interoperable across systems, and built to improve access, continuity, and operational performance from day one.
Why Partner With Us?
- Compliance-First Hybrid Architecture: We embed HIPAA, GDPR where applicable, audit trails, and strong identity controls into every layer. Security and governance come built-in, not added later.
- Workflow-Native Orchestration: Triage, routing, tasks, and documentation flow into existing EHR and telehealth tools. Clinicians move between virtual and in-clinic care without switching systems.
- AI for Routing, Risk, and Efficiency: AI supports triage, risk scoring, capacity forecasting, and documentation. Teams gain earlier insights, fewer bottlenecks, and better resource utilization.
- Interoperable and Vendor-Agnostic: We integrate with EHRs, scheduling systems, telehealth platforms, and devices using FHIR, HL7, and secure APIs. No vendor lock-in and no workflow disruption.
- Scalable Across Programs and Locations: One foundation supports primary care, behavioral health, chronic care, specialty services, urgent care, and post-acute programs. Expansion is modular and predictable.
- Zero-Trust Security and PHI Protection: End-to-end encryption, real-time monitoring, and identity-first access protect sensitive data across virtual and in-clinic workflows.
Book a strategy call with Intellivon to explore how a Hybrid Virtual + In-Clinic Care Platform can improve access, reduce operational friction, and create a connected care experience across your enterprise.
FAQs
Q1. What is a Hybrid Virtual + In-Clinic Care Platform?
A1. A Hybrid Virtual + In-Clinic Care Platform connects virtual visits, in-person services, remote monitoring, and follow-up workflows into one unified system. It ensures patients move smoothly between care settings while clinicians work from shared records and coordinated tasks.
Q2. How does a hybrid care platform improve patient experience?
A2. Hybrid platforms reduce friction by offering virtual access for low-acuity needs and in-clinic care when hands-on evaluation is required. Patients avoid repeat intake steps, receive consistent communication, and stay connected through one guided pathway.
Q3. What technologies power Hybrid Virtual + In-Clinic Care Platforms?
A3. Most platforms rely on orchestration engines, EHR integrations, AI triage tools, scheduling services, remote monitoring, and secure communication channels. Together, these components support real-time coordination across all care settings.
Q4. How do hybrid care workflows help clinicians?
A4. Clinicians benefit from consolidated worklists, streamlined documentation, and fewer repetitive steps. The platform also reduces administrative work by automating follow-ups, surfacing relevant data, and syncing notes across virtual and in-clinic encounters.
Q5. What are the biggest challenges in implementing hybrid care?
A5. Common challenges include integrating legacy systems, aligning workflows, ensuring data consistency, managing clinician adoption, and meeting compliance requirements. These can be solved through strong governance, modular architecture, and partner-led implementation support.








