If you’re building a healthcare app that needs to connect with Epic, you understand the high stakes involved. You must handle protected health information in live clinical settings, where one mistake can disrupt patient care, lead to compliance issues, or waste months of development work.
Epic makes this process challenging, and understandably so. Hospitals face strict regulatory requirements, and their EHR systems are vital for operations. Every API call must pass authentication checks, respect patient consent, maintain audit trails, and protect PHI. This all has to work smoothly through Epic’s upgrades that happen twice a year. Most integration projects fail not due to technical challenges, but because security and compliance processes are added too late.
When Epic’s governance requirements are treated as mere checkboxes instead of essential guidelines, the result is fragile integrations that can fail in real-world situations or create risks that can’t be tolerated.
At Intellivon, we handle Epic integrations differently. Instead of just linking systems and hoping for the best outcome, we design integrations as crucial infrastructure from the start. We focus on security, auditability, and long-term stability before we write any code. In this blog, we will explain how we create Epic API integrations that succeed in real healthcare settings, ensuring your integration stands the test of time.
Key Takeaways Of The Global Healthcare API Market
The global healthcare API market continues to grow as healthcare organizations push for interoperability, real-time data access, and platform-led digital transformation. APIs now sit at the center of how healthcare apps connect with EHRs, care networks, and external partners.
This shift makes secure, governed API integrations essential, especially when operating within enterprise systems like Epic, where compliance, reliability, and long-term scalability directly shape business outcomes.
The global healthcare API market is projected to grow steadily from an estimated USD 242.7 million in 2025 to about USD 372.5 million by 2032, with a 6.3% compound annual growth rate (CAGR) over the forecast period. This reflects rising demand for interoperable digital health solutions and real-time data exchange across clinical systems.
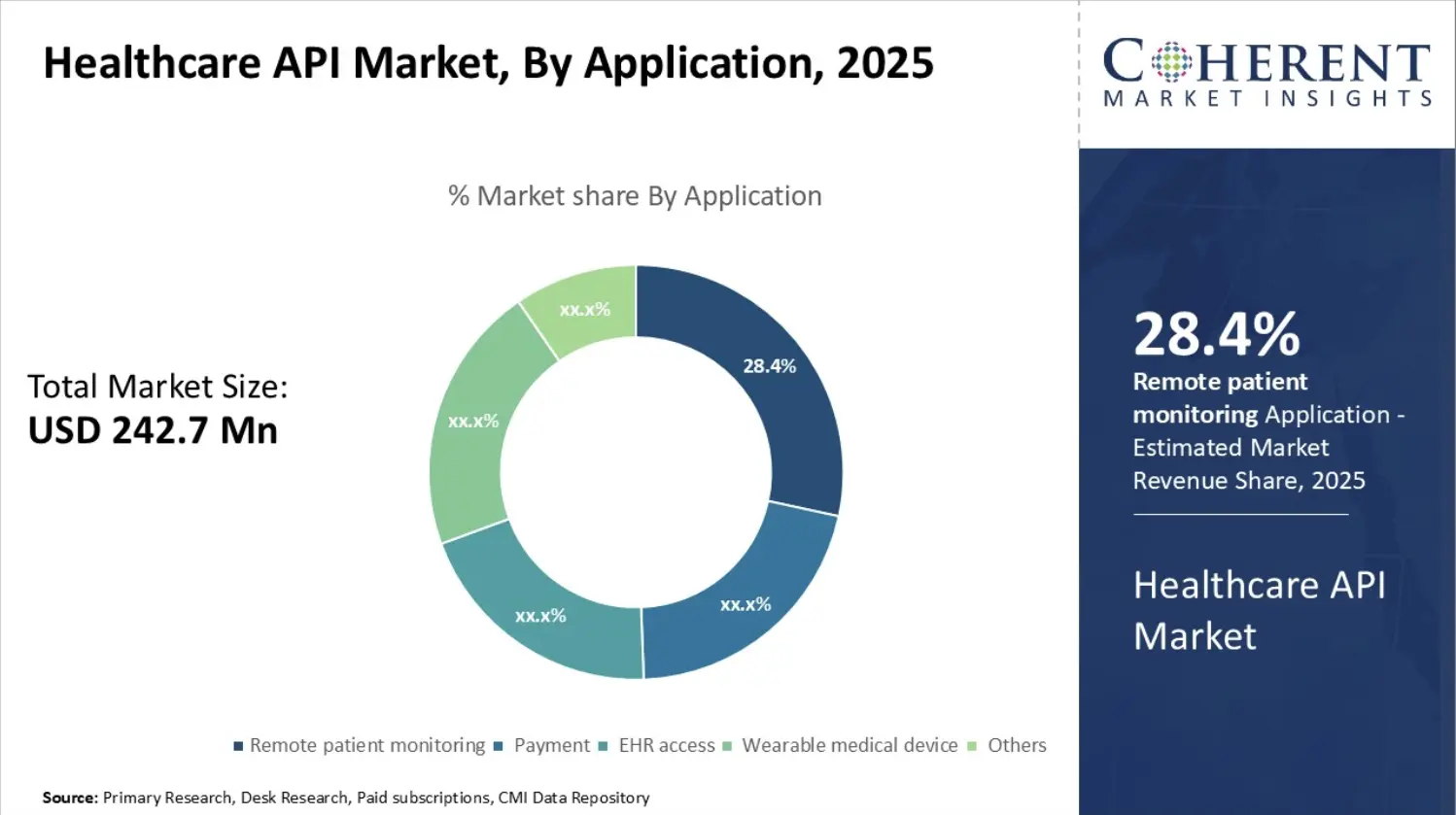
Market Insights:
- Application Trends: APIs for remote patient monitoring, EHR access, and clinical workflows are among the fastest-growing segments, driven by digital health adoption and connected care models.
- Deployment: Cloud-based deployments dominate (77.4% share in 2025) as healthcare organizations prioritize scalable and flexible integration platforms over traditional on-premise systems.
- End Users: Healthcare providers account for the largest share (44.4%) in 2025, indicating strong institutional investment in API-driven integration for operational efficiency and patient engagement.
FHIR adoption is accelerating across healthcare, with nearly 90% of health systems expected to use FHIR APIs by 2025, and 84% of industry leaders forecasting steady long-term growth. This momentum is driven by regulatory pressure and operational need. Mandates such as TEFCA and USCDI v3, with compliance timelines extending into 2026, are forcing organizations to standardize API-based data exchange.
At the same time, cloud-based healthcare APIs now account for over 81% of deployments, while payers represent nearly 50% of API end-use, signaling a shift toward ecosystem-wide interoperability.
These trends converge around Epic’s market dominance. With Epic securing roughly 70–79% of hospital EHR contracts and generating $4.9 billion in revenue in 2023, enterprises increasingly rely on Epic-connected APIs to support AI, telehealth, analytics, and real-time clinical workflows.
As adoption scales, secure API design becomes a strategic requirement and not a technical preference.
Understanding the Epic API Ecosystem
Epic runs as a tightly governed clinical system where data access is controlled by design. Any healthcare app integrating with Epic Systems must operate within this ecosystem, not around it.
Understanding how Epic exposes data is essential before discussing security, performance, or scale. Without this context, integrations often fail during approval, upgrades, or real-world use.
1. What the Epic API Ecosystem Really Is
Epic’s API ecosystem is a controlled layer that sits between external applications and the EHR. It exists to protect patient data, preserve workflow integrity, and maintain regulatory compliance.
Epic does not allow direct database access. Instead, all integrations flow through approved APIs with strict rules.
At a high level, the ecosystem is built to:
- Limit what data an app can access
- Control how and when that access occurs
- Ensure every interaction is auditable
This structure protects both healthcare organizations and patients.
2. The Role of Epic App Orchard
Epic App Orchard is the official gateway for third-party integrations. Any external app that wants to connect to Epic must go through this program.
App Orchard governs:
- API access approval
- Security and compliance review
- Ongoing version and upgrade compatibility
This process ensures apps behave predictably inside clinical environments. As a result, shortcuts are not tolerated, even for internal enterprise apps.
3. Core API Types Used in Epic Integrations
Epic offers multiple API types, each serving a different purpose. Understanding these categories helps enterprises choose the right integration approach.
Common Epic API categories include:
- FHIR APIs for standardized data exchange
- SMART on FHIR APIs for context-aware app launches
- Epic proprietary APIs for scheduling and workflows
- Authentication APIs for secure access control
Each category comes with different governance and approval requirements.
4. Why FHIR APIs Are Central to Epic Integrations
FHIR APIs form the backbone of most modern Epic integrations. They allow structured access to patient data using widely accepted standards.
FHIR APIs are commonly used for:
- Patient demographics
- Appointments and encounters
- Observations and clinical results
- Medications and care plans
Because they are standardized, FHIR APIs support interoperability across systems. However, they still operate under Epic’s strict security controls.
5. How Access Is Controlled Across the Ecosystem
Epic enforces access through layered controls. These controls ensure apps only see what they are allowed to see.
Key control mechanisms include:
- OAuth-based authentication
- Scoped permissions
- Role-based access rules
- Patient consent enforcement
Together, these mechanisms prevent data overreach and unauthorized use.
Why This Ecosystem Matters for Enterprises
For enterprises, the Epic API ecosystem shapes more than integration design. It influences timelines, costs, and long-term reliability.
Organizations that understand this ecosystem early:
- Avoid rework during approval
- Reduce integration failures during upgrades
- Build apps clinicians actually trust
In contrast, teams that underestimate Epic’s governance often face delays and operational risk.
The Epic API ecosystem is designed to protect care delivery at scale. It prioritizes security, stability, and compliance over speed or flexibility. Enterprises that respect this structure build integrations that last, perform reliably, and scale with confidence. Understanding this ecosystem is the foundation for everything that follows.
How Epic’s 1.5-Second API Response Time Impacts Clinician Productivity
Epic-integrated applications run inside active clinical workflows. Clinicians rely on them while reviewing patient data, documenting care, or making time-sensitive decisions. Because of this, even small delays become visible immediately. Epic’s 1.5-second response expectation sets a clear operational boundary for any app that wants to work reliably at scale.
1. Why Response Time Matters Inside Epic Workflows
Clinicians move quickly between screens and tasks. When an app responds slowly, users are forced to wait, switch context, or abandon the workflow. Over time, these interruptions reduce efficiency and confidence in digital tools.
Therefore, response time directly affects how often an app is used. Apps that feel slow are bypassed, even if they offer valuable functionality.
2. How Seconds Add Up at Enterprise Scale
A one-second delay may seem minor in isolation. However, across hundreds of clinicians and thousands of daily interactions, the impact grows fast. Those seconds turn into lost minutes per shift and hours across departments.
At scale, this loss shows up as reduced throughput, longer documentation cycles, and increased clinician fatigue. As a result, API performance becomes an operational concern, not a technical detail.
3. The Hidden Role of Secure API Design
Security decisions influence response time more than many teams expect. Over-scoped tokens, unnecessary data calls, and repeated authentication flows add latency. In addition, poorly designed integration layers slow down every request.
Secure API design must be intentional. When security is embedded correctly, apps protect patient data without slowing clinical work.
4. Where Productivity and ROI Connect
Faster response times improve task completion speed and reduce workflow friction. Clinicians spend less time waiting and more time delivering care. Over months, this leads to better adoption, higher satisfaction, and measurable operational gains.
This is where return on investment becomes clear. Productivity improvements come from design discipline, not added features.
Epic’s 1.5-second API response expectation reflects real clinical behavior. It marks the point where technology either supports care or disrupts it. Organizations that design secure, high-performance integrations respect this boundary and see stronger adoption at scale. In the long run, productivity follows performance.
Common Healthcare App Use Cases That Require Epic Integration
Healthcare apps now depend on real-time access to EHR data to deliver value. When an organization runs on Epic Systems, these apps must integrate with Epic to stay relevant, usable, and compliant.
Epic integration becomes necessary whenever an app touches patient data, clinician workflows, or revenue operations. In these cases, secure API access is not optional. It is foundational.
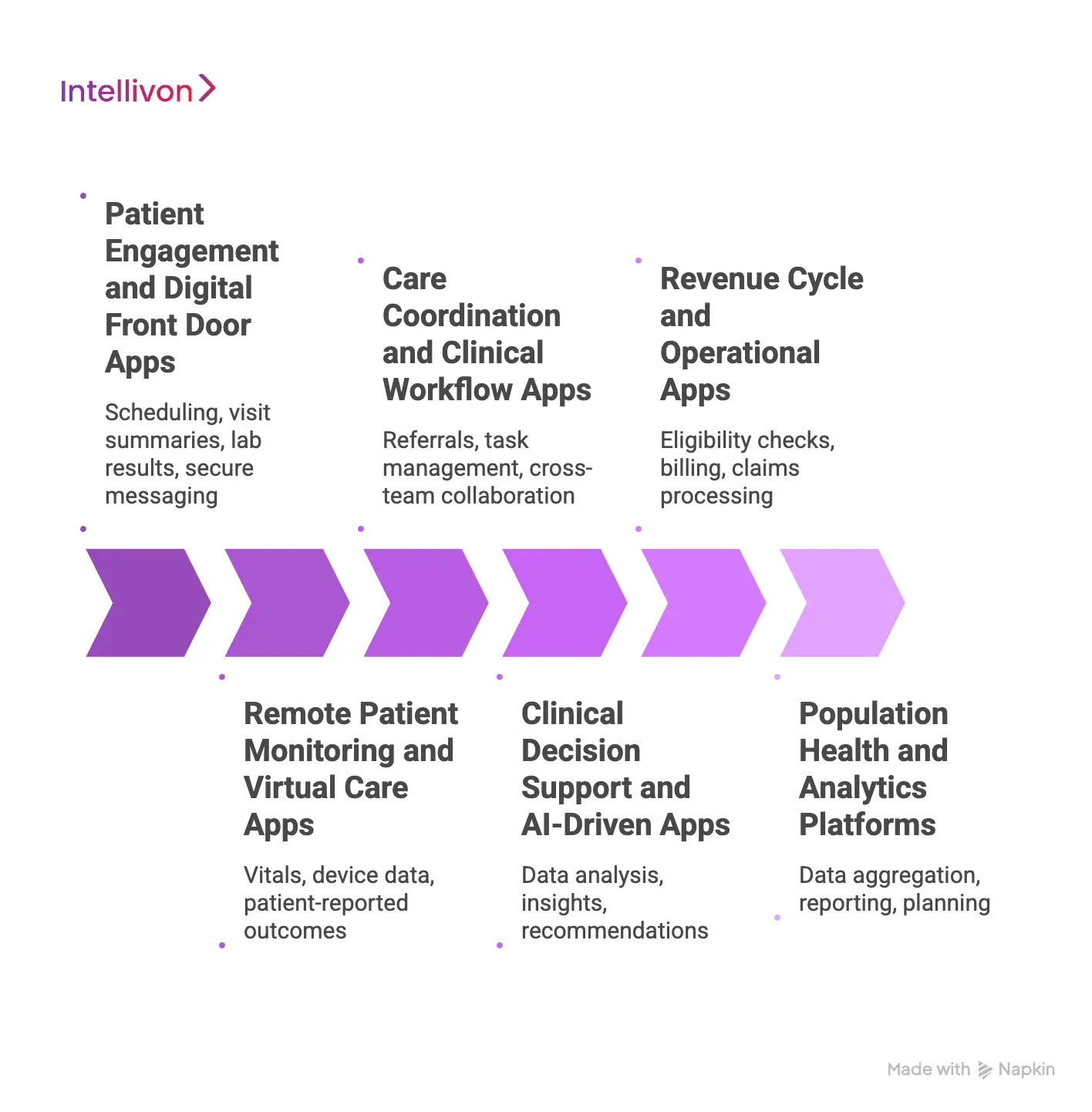
1. Patient Engagement and Digital Front Door Apps
These apps support scheduling, visit summaries, lab results, and secure messaging. Patients expect information to be current and accurate.
Epic integration ensures:
- Appointments stay in sync
- Results reflect the clinical record
- Messages reach the right care teams
Without secure integration, data becomes outdated. Trust erodes quickly, and adoption drops.
2. Remote Patient Monitoring and Virtual Care Apps
Remote monitoring apps collect vitals, device data, and patient-reported outcomes. Virtual care platforms rely on the same data for continuity.
Epic integration allows these apps to:
- Push observations into clinical workflows
- Trigger alerts for care teams
- Maintain a single source of truth
Because data flows continuously, security and reliability matter even more here.
3. Care Coordination and Clinical Workflow Apps
These apps support referrals, task management, and cross-team collaboration. Many run directly inside clinician workflows.
Epic integration provides:
- Patient and encounter context
- Role-based access for staff
- Workflow continuity across departments
If performance or access fails, clinicians stop using the app.
4. Clinical Decision Support and AI-Driven Apps
Decision support tools analyze patient data and surface insights during care delivery. Many operate in read-only mode but still influence outcomes.
Epic integration enables:
- Access to current patient data
- Context-aware recommendations
- Audit-ready clinical decisions
Even without write access, these apps require strong governance.
5. Revenue Cycle and Operational Apps
Operational apps support eligibility checks, billing workflows, and claims processing. They often combine clinical and financial data.
Epic integration ensures:
- Accurate data exchange
- Consistent workflow automation
- Clear audit trails
Failures here directly impact revenue and compliance.
6. Population Health and Analytics Platforms
Analytics platforms aggregate Epic data for reporting, planning, and performance tracking. They often span departments or organizations.
Epic integration allows:
- Standardized data access
- Scalable data pipelines
- Governed long-term analysis
Security and access control become critical at this scale.
These use cases share one requirement. They must integrate with Epic to deliver real value. Each touches sensitive workflows where performance, security, and reliability matter.
Understanding these use cases helps enterprises design integrations that support growth without introducing risk.
Real-World Healthcare Apps Built on Secure Epic API Integrations
Epic API integrations power healthcare apps that operate inside daily workflows across hospitals and health systems. These apps touch patient data, clinician actions, and operational processes, which means failures show up quickly and visibly. Looking at real examples helps clarify why secure API design is essential, not optional.
Each app category relies on Epic APIs in different ways. As a result, the security and performance requirements also vary.
1. Patient Engagement and Digital Front Door Apps
Patient engagement apps support scheduling, lab results, visit summaries, and secure communication. Patients expect these apps to reflect the same information their care teams see. When data falls out of sync, trust drops immediately.
Epic integration keeps patient-facing data accurate and timely while enforcing consent and access controls.
Real examples
MyChart: Many health systems build custom patient apps using Epic APIs similar to those behind MyChart. These apps retrieve appointments, results, and medication data directly from Epic. Security is critical because patients access sensitive health information without clinical mediation.
Xealth: Xealth embeds approved digital health tools into Epic-driven care journeys. Epic APIs provide patient context while access controls ensure only authorized tools receive data. This balance protects privacy without slowing engagement.
2. Remote Patient Monitoring Apps
Remote patient monitoring apps collect vitals and patient-reported data on an ongoing basis. Care teams depend on this data to identify risk and intervene early. Delays or errors reduce clinical confidence quickly.
Epic integration allows monitoring data to flow into clinical workflows in a structured way. Security prevents over-collection and ensures alerts remain actionable.
Real examples
Validic: Validic aggregates data from wearables and home devices, then routes validated observations into Epic-connected systems. Epic APIs support consistent data intake while governance controls protect system performance.
Livongo: Livongo supported chronic condition management through connected monitoring. Epic integration ensured clinicians received timely patient data inside their workflows. Strong security reduced clinical and operational risk.
3. Care Coordination and Provider Workflow Apps
Care coordination apps help clinicians manage referrals, tasks, and cross-team communication. Many run directly inside Epic sessions, which makes speed and reliability essential. Even small delays interrupt care delivery.
Epic integration provides patient context and workflow continuity across departments. Security ensures clinicians only access data relevant to their role.
Real examples
Notable: Notable automates administrative and clinical workflows using Epic integrations. Epic APIs support scheduling and task data while access controls prevent unauthorized use. Performance directly affects clinician adoption.
CarePort Health: CarePort connects hospitals with post-acute providers using Epic data. Epic APIs enable secure data sharing across organizations. Strong governance is required because data crosses legal boundaries.
4. Clinical Decision Support Apps
Clinical decision support apps analyze patient data and surface insights during care delivery. These tools influence clinical decisions even when they operate in read-only mode.
Epic integration ensures insights are based on current patient data. Security supports auditability and accountability.
Real examples
VisualDx: VisualDx integrates with Epic to provide diagnostic guidance during clinician sessions. Epic APIs supply patient context while session-based access limits data exposure.
Sepsis Watch: Sepsis Watch analyzes real-time clinical data to identify risk patterns. Epic integration enables timely insights while governance controls support clinical accountability.
5. Revenue Cycle and Operational Apps
Revenue cycle apps support eligibility checks, billing workflows, and claims processing. These apps often combine clinical and financial data, which increases exposure. Errors here affect both revenue and compliance.
Epic integration ensures accurate data exchange across operational systems. Security protects sensitive information at scale.
Real examples
R1 RCM: R1 integrates deeply with Epic to manage billing and revenue operations. Epic APIs support claims and coverage workflows while audit controls protect financial integrity.
Olive AI: Olive automated administrative workflows using Epic integrations. Secure API access enabled automation without compromising data protection.
These examples show how Epic API integrations support real healthcare operations at scale. Each app category introduces different data flows, risks, and performance needs. Secure API design ensures these apps remain reliable, trusted, and ready for long-term growth.
Epic APIs Used to Build These Healthcare Apps
Healthcare apps do not connect to Epic in one universal way. Epic offers different APIs based on how an app works, who uses it, and what data it needs. Choosing the right APIs early shapes security, performance, and long-term stability.
Understanding these API types helps enterprises design integrations that scale without creating operational risk inside Epic Systems environments.
1. Epic FHIR APIs
FHIR APIs form the foundation of most modern Epic integrations. They provide standardized access to clinical and patient data using widely accepted formats. Because of this, they support interoperability across systems.
These APIs are commonly used for:
- Patient demographics
- Appointments and encounters
- Observations and lab results
- Medications and care plans
FHIR APIs work well for patient-facing apps, analytics platforms, and read-heavy workflows. Security is enforced through scoped access and consent controls.
2. SMART on FHIR APIs
SMART on FHIR APIs support apps that launch directly inside Epic workflows. They allow apps to understand who the user is and which patient record is open.
These APIs are often used in:
- Clinician workflow tools
- Decision support apps
- Embedded care coordination tools
Because these apps run during live care, access is session-based and tightly controlled. Performance and permission accuracy are critical here.
3. Epic Proprietary APIs
Epic also provides proprietary APIs for workflows not fully covered by FHIR. These APIs support deeper operational and scheduling use cases.
They are commonly used for:
- Scheduling and referrals
- Revenue cycle workflows
- Administrative automation
Access to these APIs requires additional approval and governance. Security is stricter because these workflows often affect operations and revenue directly.
4. Authentication and Authorization APIs
All Epic integrations rely on strong authentication and authorization layers. Epic uses OAuth-based flows to control access across apps and systems.
These APIs manage:
- User and system authentication
- Token scopes and lifecycles
- Role-based access rules
Good security design here prevents over-permissioning and reduces exposure if credentials are compromised.
5. Event, Notification, and Data Sync APIs
Some healthcare apps rely on real-time or near-real-time updates. Epic supports this through event-driven and data sync mechanisms.
These APIs help apps:
- React to clinical changes
- Trigger alerts or workflows
- Keep systems aligned over time
Because data moves continuously, monitoring and rate controls are essential to protect system performance.
Epic APIs are designed to balance access with control. Each API type serves a specific purpose and comes with different security expectations. Enterprises that understand these distinctions build integrations that perform well, pass governance checks, and remain stable as usage grows. This clarity sets the stage for secure and scalable healthcare applications.
Security-First Architecture for Epic API Integrations
Epic API integrations must be designed as an enterprise healthcare infrastructure. This means using clear architectural layers, not direct connections between apps and Epic. Each layer has a specific role in protecting data, performance, and compliance.
Without this structure, integrations become fragile and risky. With it, security becomes predictable and scalable.
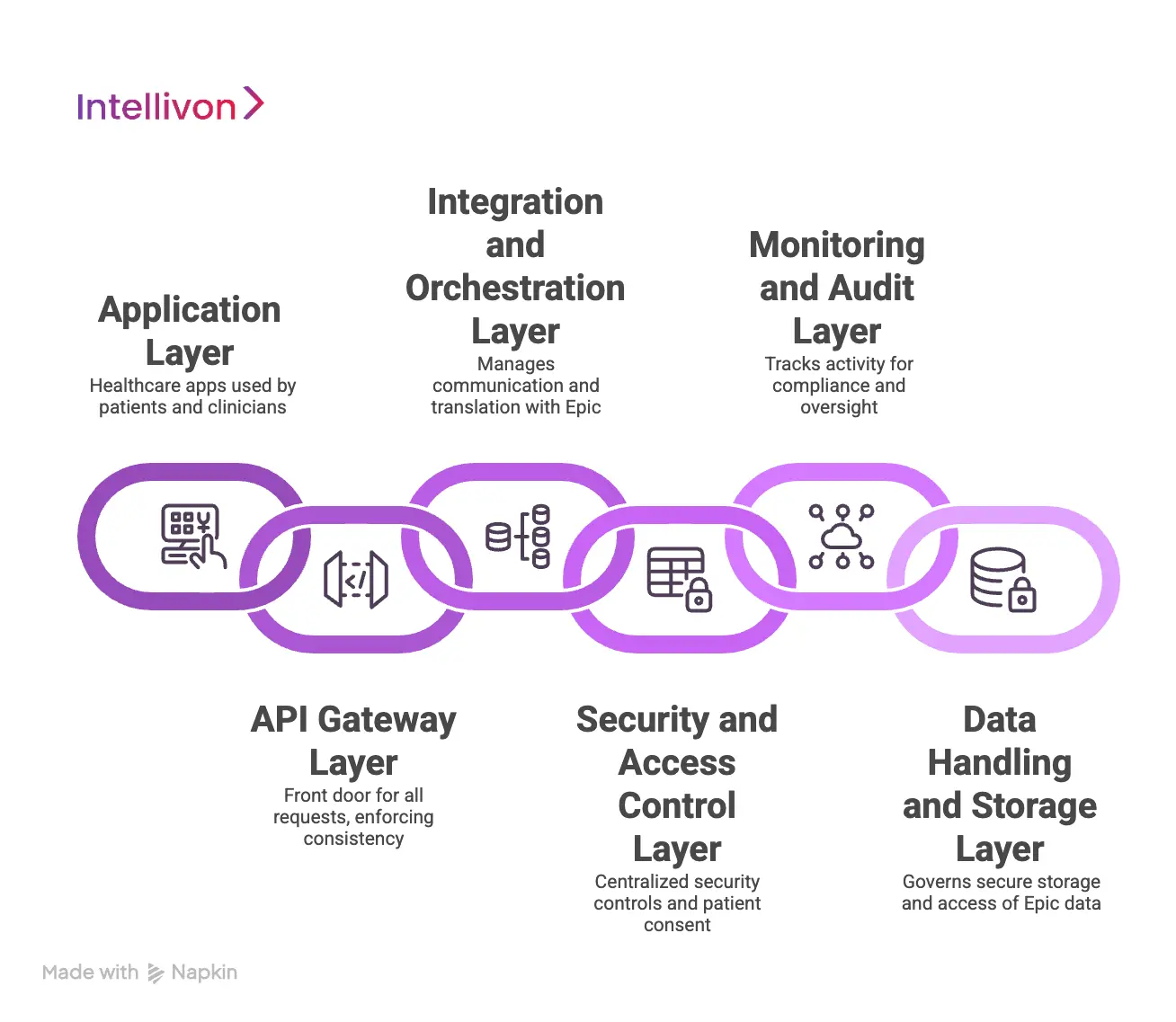
Layer 1: Application Layer
This is the healthcare app used by patients, clinicians, or operations teams. It handles user interactions and business logic. It should never connect directly to Epic APIs.
The application layer:
- Displays data and workflows
- Sends requests to backend services
- Never stores Epic credentials
Keeping this layer separate limits exposure if the app is compromised.
Layer 2: API Gateway Layer
The API gateway acts as the front door for all requests. It validates traffic before anything reaches Epic-connected services. This layer enforces consistency and control.
The gateway layer:
- Validates authentication tokens
- Applies rate limits
- Blocks unauthorized requests
This layer prevents abuse and protects downstream systems.
Layer 3: Integration and Orchestration Layer
This layer manages all communication with Epic. It translates app requests into approved Epic API calls. It also handles retries, errors, and response formatting.
The integration layer:
- Calls Epic FHIR and proprietary APIs
- Enforces scope and consent rules
- Controls data volume and timing
This is where most Epic-specific logic belongs.
Layer 4: Security and Access Control Layer
Security controls should not be scattered across the system. They belong in a dedicated layer that applies rules consistently.
This layer:
- Manages OAuth tokens and lifecycles
- Applies role-based access rules
- Enforces patient consent
Centralizing security reduces mistakes and audit risk.
Layer 5: Monitoring and Audit Layer
Every Epic integration must be observable. This layer tracks activity across all other layers. It supports compliance and operational oversight.
The monitoring layer:
- Logs all API calls
- Tracks user and system actions
- Flags unusual access patterns
This layer is critical for audits and incident response.
Layer 6: Data Handling and Storage Layer
Some apps store limited Epic-derived data. When they do, storage must be tightly controlled. This layer governs how data is stored and accessed.
This layer:
- Encrypts data at rest
- Applies retention policies
- Limits secondary use
Poor design here creates long-term compliance risk.
Why Layered Architecture Matters in Epic Environments
Epic environments, including Epic Systems, are built for stability and control. Layered architecture aligns with this model. It limits blast radius, simplifies audits, and protects workflows. Enterprises that skip layers often face rework, delays, and failures during scale or upgrades.
Security-first architecture for Epic integrations is about structure, not tools. Clear layers separate concerns, reduce risk, and support long-term growth. When architecture is designed this way, security becomes part of normal operations rather than a constant firefight.
Ensuring HIPAA Compliance and PHI Protection
HIPAA compliance is not a checklist item for Epic integrations. It is an ongoing operational responsibility. Every API call that touches patient data carries compliance risk if not handled correctly.
When apps integrate with Epic Systems, they inherit the same expectations around privacy, security, and accountability. This makes PHI protection a core design requirement, not a legal afterthought.
1. Understanding Where PHI Exposure Actually Occurs
Most PHI exposure does not happen through dramatic breaches. It happens through everyday interactions such as over-fetching data, logging sensitive fields, or sharing access too broadly.
Epic API integrations amplify this risk because they operate continuously. Data moves between systems, users, and workflows throughout the day. Without strong controls, small gaps become persistent exposure points.
2. Controlling Data Access at the Source
HIPAA compliance begins with limiting what data an app can access. Epic APIs support scoped access, but scopes alone are not enough. Enterprises must design integrations to request only the minimum data required for each workflow.
When apps retrieve unnecessary patient data, they increase liability without adding value. Keeping access narrow reduces exposure and simplifies audits.
3. Protecting PHI in Transit and Processing
PHI must remain protected while it moves between systems. This includes data traveling from Epic APIs into backend services and through internal processing layers.
Encryption in transit is mandatory, but processing safeguards matter just as much. Data should be handled in memory carefully, avoided in logs, and cleared when no longer needed. These controls prevent accidental leakage during normal operations.
4. Ensuring Auditability and Traceability
HIPAA requires organizations to know who accessed PHI, when it was accessed, and why. Epic integrations must support this level of traceability at all times.
Every API interaction should be tied back to a user or system identity. Clear records allow compliance teams to respond quickly to audits, investigations, or patient inquiries.
5. Managing Third-Party and Downstream Risk
Many Epic-integrated apps rely on third-party services for analytics, messaging, or automation. Each additional dependency introduces a new compliance risk.
HIPAA responsibility does not end at the API boundary. Enterprises must ensure downstream systems handle PHI with the same level of protection. Contracts alone are not enough without technical enforcement.
Ensuring HIPAA compliance and PHI protection requires discipline across architecture, access control, and operations. Epic API integrations make this responsibility more visible because they operate at the center of care delivery. Enterprises that embed compliance into daily system behavior reduce risk, simplify audits, and protect patient trust over time.
Real-World Integration Pitfalls and Risks
Epic API integrations rarely fail at launch. Issues usually appear later, when usage grows, audits begin, or workflows change. At that point, fixing problems becomes expensive and disruptive.
Knowing where integrations break in real environments helps enterprises design them correctly from the start.
1. Seeing Epic Integration as a Short-Term Project
Epic integration is often treated as a task with a clear finish line. Once the app goes live, long-term ownership weakens. Over time, platform updates and increased usage expose gaps in the original design.
At Intellivon, Epic integrations are planned as long-running infrastructure. Architecture decisions account for scale, governance, and change cycles early. This keeps integrations stable well beyond launch.
2. Asking for Broad Data Access Too Early
Wide data access often feels convenient during development. Teams request broad permissions to avoid repeated approvals. Over time, this creates compliance risk and performance overhead.
Access is designed around real workflows at Intellivon. Each integration request only includes what the app truly needs. This keeps exposure low and makes audits easier to manage.
3. Letting Performance Issues Emerge at Scale
Pilot environments rarely reveal performance problems. Once clinicians depend on an app daily, even small delays disrupt care delivery. Trust in the app fades quickly.
Performance is treated as a design requirement, not a tuning step. Intellivon optimizes API usage early, removes unnecessary calls, and monitors response times continuously. This protects clinician productivity as adoption grows.
4. Reusing Tokens and Sessions Across Workflows
Security shortcuts often appear in token management. Long-lived or shared access increases risk quietly. When an issue occurs, the impact spreads quickly.
Access is structured around short-lived, scoped sessions. Tokens are isolated by workflow, and ownership remains clear. This limits blast radius without slowing users down.
5. Operating Without Clear Visibility
Some integrations go live without strong monitoring. Teams lack insight into access patterns, failures, or unusual behavior. Problems surface late, often through audits or operational complaints.
Visibility is built in from day one. Intellivon ensures Epic API activity remains observable and traceable. This allows issues to be addressed early, before they escalate.
6. Ignoring Epic Governance and Change Cycles
Epic environments evolve constantly. API updates, policy changes, and platform upgrades are routine. Integrations that ignore this reality break without warning.
Governance-aware planning avoids these disruptions. Intellivon aligns integration design with Epic change cycles and validation requirements. This prevents delays and protects operational continuity.
Real-world Epic integration risks are predictable. They come from shortcuts in architecture, access control, and governance. Enterprises that address these challenges early build integrations that remain secure, reliable, and trusted over time. Careful design turns potential risk into long-term resilience.
How Intellivon Approaches Secure Epic API Integrations
Building secure Epic API integrations is not about speed or shortcuts. It requires a deep understanding of healthcare workflows, regulatory pressure, and how systems behave under real operational load. This work is approached as enterprise infrastructure, where early decisions shape long-term stability.
The steps below reflect how secure Epic integrations are delivered in real healthcare environments. Each step reduces risk before it appears and keeps the system reliable as usage grows.
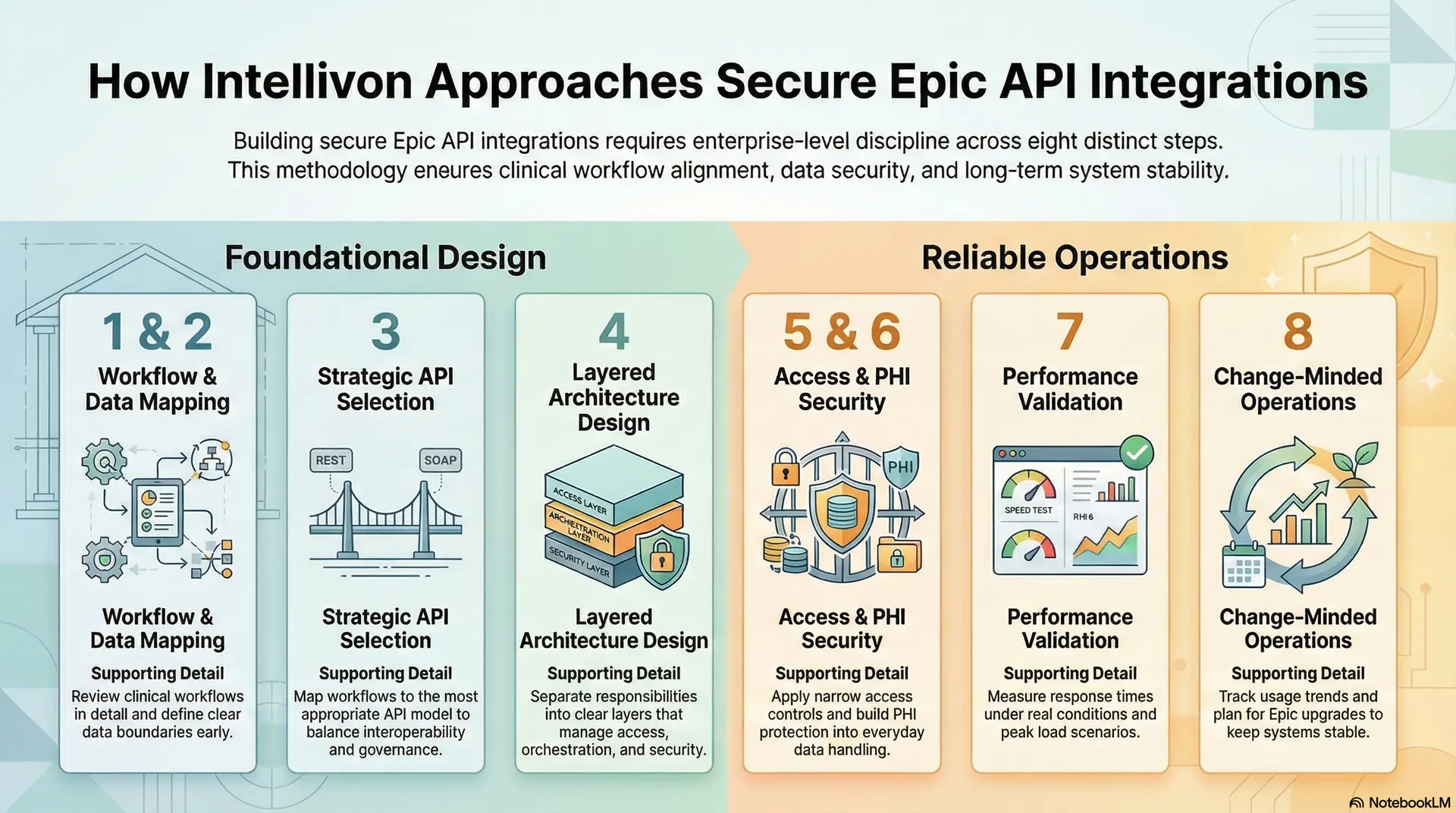
Step 1: Start with how work actually flows
Every integration begins with understanding how people really work, not how systems are assumed to work. Clinical, operational, and administrative workflows are reviewed in detail, including where decisions are made and where delays already exist.
This step prevents building integrations that technically function but fail in practice. When workflows are understood early, integration design supports daily operations instead of disrupting them.
Clear outcomes are also defined at this stage, which keeps later technical decisions grounded in business reality.
Step 2: Define clear data boundaries early
Before any API access is requested, the data required for each workflow is clearly identified. Only what is necessary is included, and everything else is deliberately excluded.
This discipline reduces compliance exposure and avoids future rework. It also makes conversations with security and compliance teams far more straightforward.
When data boundaries are clear from the start, integrations remain easier to manage, audit, and explain over time.
Step 3: Choose the right Epic API approach
Epic provides multiple API options, each designed for specific use cases. Selecting the wrong path often leads to approval delays or redesigns later.
Each workflow is mapped carefully to the most appropriate API model, balancing interoperability needs with governance expectations. This prevents overengineering while still supporting future scale.
Making this decision early saves time and avoids friction during certification and expansion.
Step 4: Design the architecture in clear layers
Secure Epic integrations never rely on direct connections between apps and the EHR. Instead, responsibilities are separated into clear layers that manage access, orchestration, and security.
Layered architecture limits blast radius when issues occur and makes change easier to manage. It also allows security controls to remain consistent across workflows.
This structure creates stability, especially as integrations grow more complex.
Step 5: Apply access controls as a default behavior
Access control is treated as a baseline expectation, not an optional feature. Permissions remain narrow, session-based, and tied to clear identities.
This approach prevents silent data overreach and keeps exposure predictable. It also simplifies audit conversations because access patterns are intentional and explainable.
When access is controlled by design, security becomes part of normal operations rather than a constant concern.
Step 6: Build PHI protection into everyday handling
Protecting patient data goes beyond encryption. Data handling avoids unnecessary storage and prevents sensitive information from appearing in logs or secondary systems.
Processing paths are kept clean and intentional, which reduces accidental exposure during normal operations. These safeguards operate quietly but consistently.
As a result, PHI remains protected without slowing down workflows or users.
Step 7: Validate performance where it matters most
Performance is tested under real conditions, not just in isolated environments. Response times are measured during realistic usage patterns and peak load scenarios.
This helps identify bottlenecks early, before clinicians or staff feel the impact. Optimizations focus on reducing unnecessary calls and limiting payload size.
When performance is treated seriously, adoption remains strong as usage increases.
Step 8: Operate with change in mind
After launch, integrations are monitored continuously. Usage trends, failures, and unusual access patterns are tracked so issues are addressed early.
Epic upgrades and policy changes are expected and planned for, not treated as surprises. This mindset keeps systems stable as environments evolve.
Ongoing operation is viewed as part of delivery, not something handed off and forgotten.
Secure Epic API integrations succeed through structure, discipline, and experience. A step-by-step approach keeps risk contained and systems reliable as scale increases. When integrations are delivered this way, they continue to support care delivery long after launch.
Conclusion
Secure Epic API integration has become a strategic capability for healthcare organizations operating at scale. As digital initiatives expand across patient engagement, clinical workflows, analytics, and operations, the quality of integration decisions determines long-term success.
When integrations are designed as regulated infrastructure, they remain stable through growth, audits, and platform change. Performance stays predictable, security remains enforceable, and teams retain confidence in daily use.
Organizations that invest in disciplined architecture, intentional access control, and continuous governance reduce risk while enabling faster innovation.
This approach turns Epic integrations into growth enablers rather than operational constraints. With the right expertise guiding design and execution, secure Epic API integrations support better care delivery, stronger compliance posture, and sustainable enterprise value over time.
Build Secure Epic API Integrations With Intellivon
At Intellivon, secure Epic API integrations are built as a regulated enterprise healthcare infrastructure, not as point-to-point connections layered onto Epic environments.
Here, every architectural and delivery decision prioritizes security boundaries, identity governance, compliance enforcement, and long-term operational stability. This ensures integrations operate reliably inside Epic workflows, not just during initial certification or rollout.
As Epic-connected ecosystems expand across providers, partners, and digital services, stability becomes critical. Here, governance, performance, and audit readiness remain consistent as data volume, access complexity, and integration scope increase.
At the same time, organizations retain control over API access, data flows, and compliance obligations without introducing fragmentation, hidden risk, or recurring rework.
Why Partner With Intellivon?
- Enterprise-grade Epic API integration architecture designed for regulated healthcare environments
- Proven delivery across Epic-connected health systems, multi-entity networks, and enterprise platforms
- Compliance-by-design approach covering HIPAA, consent enforcement, access control, and audit readiness
- Secure, layered integration architecture supporting cloud, hybrid, and on-prem deployments
- AI-ready integration foundations enabling analytics, automation, and intelligent workflows with governance and oversight
Book a strategy call to explore how Intellivon can help you build and scale secure Epic API integrations with confidence, control, and long-term enterprise value.
FAQs
Q1. What are Epic APIs, and how do healthcare apps use them?
A1. Epic APIs allow healthcare apps to securely access EHR data without touching Epic’s database directly. Apps use these APIs to read or write patient, clinical, and operational data while following Epic’s governance, security, and compliance requirements.
Q2. How do you build secure Epic API integrations for healthcare apps?
A2. Secure Epic API integrations are built by limiting data access, enforcing identity and consent controls, and using a layered architecture. This approach protects PHI while ensuring integrations perform reliably inside live Epic workflows.
Q3. Which Epic APIs are commonly used for healthcare app integrations?
A3. Most healthcare apps use Epic FHIR APIs for standardized data access and SMART on FHIR for workflow-embedded experiences. Some operational and revenue workflows also rely on Epic’s proprietary APIs, depending on the use case.
Q4. Why is security critical when integrating apps with Epic?
A4. Epic integrations operate inside regulated clinical systems where small security gaps can expose PHI or disrupt care delivery. Strong security design protects patient data, supports audits, and prevents operational instability as usage scales.
Q5. How long does it take to build a secure Epic API integration?
A5. Timelines vary based on use case, governance scope, and approval requirements. Most secure Epic API integrations take several months when designed for enterprise scale, compliance readiness, and long-term stability rather than quick pilots.