Virtual clinics are now a standard part of healthcare. Organizations treating them as essential infrastructure now face a key question on whether they should build a custom platform or use existing solutions. Making the wrong choice can waste money on systems that don’t integrate well, frustrate medical staff, or create compliance issues later.
The challenge of building a new platform is significant. A functioning virtual clinic app must communicate with existing electronic health records without causing problems. It also needs to handle patient scheduling and provider availability in real-time, manage prescriptions and legally binding documentation, and work for both clinic staff handling appointments and patients looking to see a doctor. When you add multiple locations, different specialties, various insurance providers, and strict data protection requirements, the technical demands quickly increase.
Our experts create virtual clinic apps that fit how healthcare organizations operate. The focus is on connecting easily with whatever EMR system is already in place. They ensure compliance as regulations change and make sure both clinical teams and patients can use the system smoothly. This blog will focus on how our experts design and scale virtual clinic apps while managing clinical risk and compliance.
Key Takeaways Of The Virtual Care Market
This growth represents a 32.20% CAGR between 2025 and 2034. The acceleration reflects sustained enterprise investment in virtual-first care models. It also signals that virtual care is becoming a core healthcare growth channel, not a temporary shift.
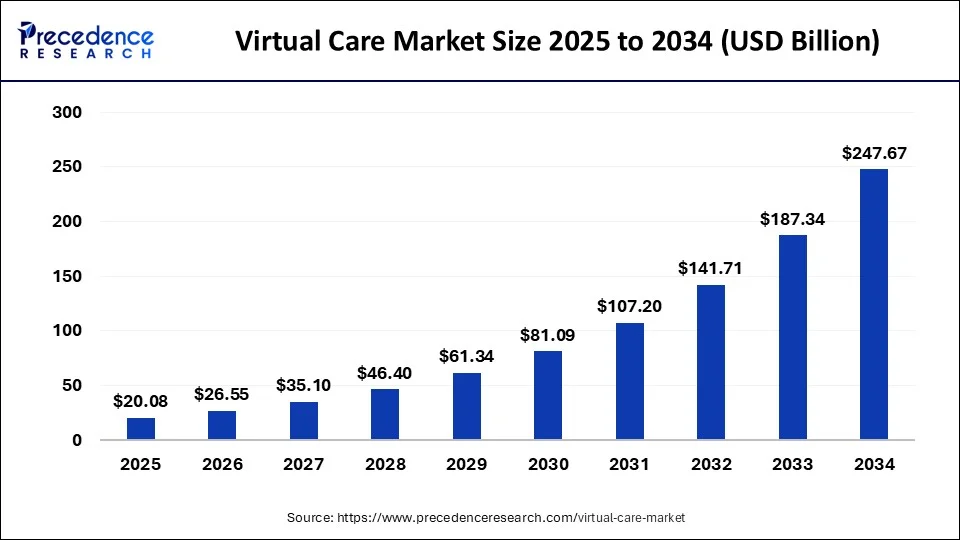
Market Insights:
- 44% of patients used virtual visits in 2024, with 94% willing to repeat, driving continued enterprise expansion despite reimbursement hurdles.
- Uneven broadband access shapes delivery in emerging markets, with 78% rural APAC smartphone ownership favoring audio and async care over video.
- Chronic care platforms manage diabetes and heart disease through RPM, reducing hospital visits and enabling home-based care.
- Hybrid care models combine in-person and virtual visits to improve flexibility and optimize provider capacity amid aging populations.
- AI and RPM integration uses real-time ECG and glucose data to trigger alerts, improving outcomes in underserved regions.
- Reimbursement parity could accelerate adoption, with 82% of executives willing to expand, while usage remains 18% urban vs 14% rural.
Investing in virtual care apps is a strategic move toward scalable, resilient care delivery. Virtual platforms expand access, stabilize operating costs, and support continuous care beyond physical facilities. In addition, they align with reimbursement trends, consumer expectations, and workforce constraints. For healthcare enterprises, virtual care apps create a foundation for long-term growth by turning care delivery into a repeatable, data-driven operating model rather than a location-bound service.
What Is a Virtual Clinic App?
A virtual clinic app is an enterprise care delivery platform that coordinates intake, consultations, follow-ups, monitoring, and care teams through governed workflows. Unlike basic telemedicine tools, it manages longitudinal care, data continuity, and accountability across services. This structure enables scalable virtual and hybrid care without fragmenting clinical ownership or compliance.
A virtual clinic app is a digital care platform that delivers coordinated clinical services through a single, governed system. It supports patient intake, consultations, follow-ups, and ongoing monitoring across multiple specialties. Unlike basic telehealth tools, it manages workflows, data, and care teams together.
Patients access care through structured journeys rather than isolated visits. Clinicians work within defined protocols that support safety and accountability. For healthcare organizations, a virtual clinic app enables scalable care delivery, consistent patient experiences, and better operational control across virtual and hybrid models.
Virtual Clinic vs Telemedicine App
The difference between telemedicine and virtual clinic apps lies in scope and governance. Telemedicine supports individual remote visits, while virtual clinics orchestrate ongoing care across teams, services, and time. At enterprise scale, this distinction determines whether virtual care remains manageable or becomes fragmented, risky, and operationally inefficient.
Although the terms are often used interchangeably, they solve very different problems. A telemedicine app focuses on enabling remote consultations. A virtual clinic app supports end-to-end care delivery across services, teams, and time. Understanding this difference matters when planning for scale, compliance, and long-term ROI.
| Aspect | Telemedicine App | Virtual Clinic App |
| Core purpose | Enable remote consultations | Deliver coordinated, ongoing care |
| Scope of care | Single visit or episodic interaction | Multi-visit, longitudinal care journeys |
| Clinical workflows | Minimal, visit-based | Structured, protocol-driven workflows |
| Care team involvement | Individual clinician | Multi-role care teams |
| Data handling | Visit-level data | Unified, longitudinal patient records |
| Integration depth | Limited EHR or scheduling | Deep EHR, RPM, labs, and pharmacy integration |
| Scalability | Suitable for low-complexity use cases | Designed for enterprise-scale operations |
| Compliance governance | Basic safeguards | Embedded governance, auditability, and controls |
In practice, telemedicine apps work well for simple access needs. However, as services expand, their limits become visible. A virtual clinic app provides the structure required to manage complexity, maintain accountability, and deliver consistent care at scale.
Key Use Cases Virtual Clinic Apps Support Today
Building on the coordinated care and workflow foundations outlined earlier, virtual clinic apps are adopted by enterprises to operationalize specific care models at scale.
Enterprises adopt virtual clinic apps to manage access, continuity, and scale without expanding physical infrastructure. These platforms support primary, chronic, behavioral, and specialty care through structured workflows. By centralizing coordination and data, virtual clinics reduce operational strain while maintaining clinical consistency across large and distributed populations.
Virtual clinic apps succeed when they are built around real care delivery models. Enterprises adopt them to solve access gaps, manage chronic demand, and scale services without expanding physical infrastructure.
Each use case below reflects where virtual clinics deliver measurable impact today.
1. Primary and Preventive Care
Virtual clinics support first-contact care, routine consultations, and preventive check-ins. Structured intake and triage reduce unnecessary in-person visits. Clinicians focus on higher-value interactions, while patients receive faster access and continuity. This model works well for large populations and recurring care needs.
2. Chronic Care Management
Virtual clinic apps play a central role in managing long-term conditions. Remote monitoring supports conditions such as diabetes and heart disease. Care teams track trends, intervene early, and reduce avoidable hospitalizations. Over time, this approach improves outcomes while stabilizing operational costs.
3. Behavioral and Mental Health
Virtual delivery improves access to behavioral health services. Patients engage through scheduled sessions and asynchronous follow-ups. Care plans remain consistent across visits, which supports adherence. For organizations, this model expands capacity without increasing physical clinic load.
4. Specialty and Follow-Up Care
Specialty consultations and post-procedure follow-ups adapt well to virtual clinics. Care pathways guide patients through evaluations, results, and next steps. This reduces delays and improves coordination between specialists and primary teams. As a result, care feels connected rather than fragmented.
5. Employer and Insurer-Led Programs
Virtual clinics support population-level programs for employers and payers. These programs focus on preventive care, triage, and chronic condition oversight. Utilization shifts away from high-cost settings. Enterprises gain better visibility into outcomes and engagement.
Virtual clinic apps create value when they align with clear use cases. They reduce access friction, improve continuity, and support scalable care delivery. For healthcare enterprises, these use cases form the foundation for long-term virtual care strategies.
Hospital APIs Expanded Patient Access to 80%, Unlocking Scalable Virtual Clinics
Once care coordination is established at the workflow level, integration maturity becomes the primary enabler of scale.
API maturity and reimbursement expansion have shifted virtual care from isolated tools to enterprise platforms. As hospitals expose scheduling, documentation, and clinical data through governed interfaces, virtual clinics can coordinate multiple services within a single system. This enables scale without replacing core infrastructure or increasing administrative complexity.
Telehealth operates as a reimbursable clinical service layer across multiple specialties and care moments. This shift changes how hospitals must think about structure, governance, and scale.
Federal data now lists more than 250 reimbursable Medicare telehealth codes. That growth reflects how virtual care has moved into routine clinical delivery. As the scope widens, hospitals face a new challenge. They must coordinate more services without increasing operational friction.
1. Telehealth Now Functions as a Multi-Service Clinical Layer
The expansion of reimbursable services signals a structural change in care delivery. Hospitals now provide behavioral health, chronic care, diagnostics, post-discharge follow-ups, and specialty consultations through virtual channels.
Each service brings different workflows, clinical ownership, and reporting obligations. When teams manage these services independently, fragmentation builds over time. Coordination slows, accountability blurs, and patient journeys lose consistency.
Therefore, virtual clinic design must begin with orchestration. A shared care model aligns services, roles, and outcomes across the enterprise. This alignment becomes essential as service volume increases.
2. Hospital APIs Already Enable Platform-Level Access
Most hospitals have already invested in the technical foundation required for virtual clinics. In inpatient settings, API enablement for patient-facing applications rose from 68% in 2021 to 83% in 2023.
In 2024, adoption stabilized at 80%. This plateau reflects maturity rather than stalled progress. Hospitals now expose data and workflows through controlled interfaces instead of closed systems.
These APIs support access to scheduling, documentation, patient data, and care coordination. As a result, hospitals can support integrated virtual clinic platforms without replacing core clinical systems.
3. Bulk Data Capabilities Support Cross-Service Care Intelligence
Data consolidation has progressed quietly across health systems. By 2021, 74% of hospitals had adopted bulk data export capabilities.
Among those organizations, 84% used bulk data for analytics and reporting. In addition, 47% applied it to population health management. These capabilities matter because virtual care depends on shared visibility.
Risk stratification, follow-up planning, and outcome tracking rely on unified data access. Without it, services operate in isolation and insights remain incomplete.
Why This Matters When Building a Virtual Clinic App
As telehealth services multiply, access stops being the bottleneck. Coordination becomes the constraint. A virtual clinic app must operate as a unifying layer that connects services, data, and care teams through governed workflows.
Instead of scaling virtual care tool by tool, hospitals can structure growth through a single virtual clinic architecture. This approach supports consistency across patient journeys, maintains clinical accountability, and protects data integrity as complexity increases.
When designed correctly, a virtual clinic becomes an operating system for modern care delivery rather than another digital channel.
Core Components of a Virtual Clinic App
To support the enterprise care model described earlier, virtual clinic platforms require a tightly integrated set of functional components.
A virtual clinic app functions as a unified enterprise platform rather than a collection of features. Patient access, clinician workspaces, AI-assisted intake, workflow orchestration, interoperability, security, and analytics must operate together. This integration keeps care predictable, compliant, and scalable as services and patient volumes grow.
A virtual clinic app must function as an enterprise care platform rather than a collection of digital tools. Each component should support scale, compliance, and operational clarity from day one. The features below reflect what mature healthcare organizations prioritize when building for long-term impact.
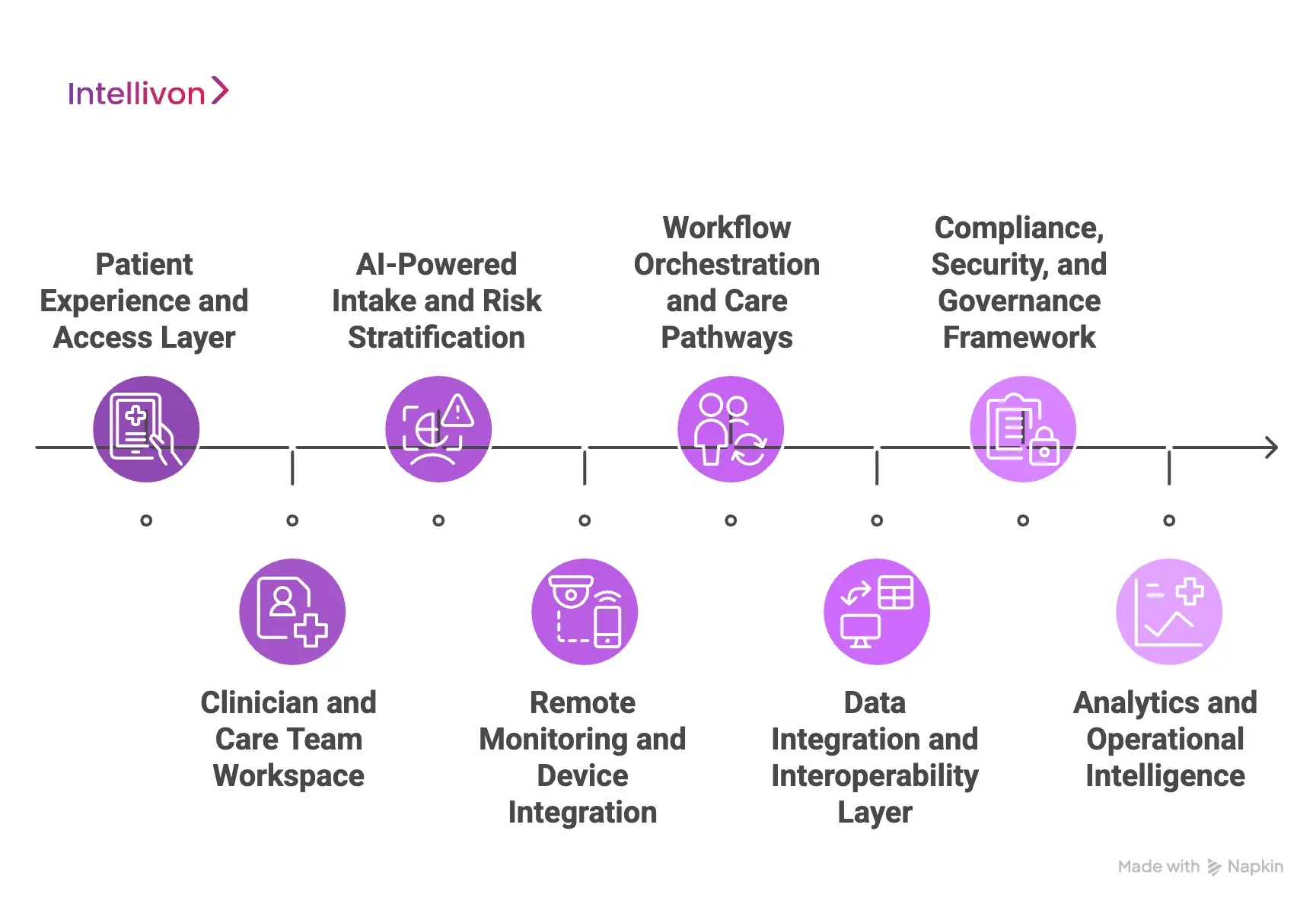
1. Patient Experience and Access Layer
The patient experience layer defines how care begins and progresses. Structured digital intake captures symptoms, medical history, and consent in a guided flow that feels simple but remains clinically complete. Scheduling routes patients to the appropriate service or care team without manual intervention.
Messaging, virtual visits, and follow-ups remain connected within the same care journey. This continuity reduces drop-offs and repeat data entry. As patient volumes grow, access stays predictable and governed.
2. Clinician and Care Team Workspace
Clinicians require a workspace designed for speed and clarity. The platform presents patient summaries, tasks, and alerts in a single, consistent view. Care teams collaborate across roles without switching between systems. AI-assisted summaries reduce documentation burden while preserving clinical context.
Workflow visibility improves accountability across handoffs and follow-ups. As service complexity increases, clinician efficiency remains stable.
3. AI-Powered Intake and Risk Stratification
AI-driven intake reviews patient inputs as they are submitted. Rules and models identify risk signals before the clinician review begins. High-risk cases escalate automatically to the appropriate care pathway.
Lower-risk cases route efficiently without unnecessary clinical effort. This approach improves safety while protecting clinician time. Over time, the system adapts to changing patient populations.
4. Remote Monitoring and Device Integration
Remote monitoring enables continuous insight beyond scheduled visits. The platform ingests data from devices such as glucose monitors and ECGs securely. AI analyzes trends rather than isolated readings.
Alerts trigger when thresholds or patterns indicate risk. Care teams intervene earlier with a clearer context. This reduces avoidable hospital visits and improves outcomes.
5. Workflow Orchestration and Care Pathways
Workflow orchestration keeps care consistent across services. Clinical pathways define tasks, escalation rules, and follow-up timelines. Automation ensures actions trigger at the right moment without manual tracking.
Care delivery remains aligned with protocols even as teams scale. This structure prevents fragmentation across specialties. Operational predictability improves as complexity grows.
6. Data Integration and Interoperability Layer
Virtual clinics rely on seamless data exchange. The platform integrates with EHRs, labs, pharmacies, and imaging systems. Data flows securely through standardized interfaces. Longitudinal records remain complete across encounters.
This shared visibility supports better clinical decisions. Reporting and analytics improve without manual reconciliation.
7. Compliance, Security, and Governance Framework
Enterprise adoption depends on trust and control. The platform enforces role-based access and auditability by design. Consent management aligns with regulatory requirements across regions. Data remains encrypted in transit and at rest.
Governance controls support oversight without slowing care delivery. Compliance scales alongside service expansion.
8. Analytics and Operational Intelligence
Analytics converts care activity into actionable insight. Dashboards track utilization, outcomes, and operational performance. Leaders gain visibility into service efficiency and patient engagement. AI highlights trends that require intervention. Decisions become data-driven rather than reactive. This intelligence supports sustainable growth.
A virtual clinic app works only when its components operate as one system. Connected workflows, data, and governance keep complexity under control. When built this way, virtual care scales with confidence rather than friction.
Clinical Workflow Design Inside A Virtual Clinic App
With platform components in place, the effectiveness of a virtual clinic depends on how clinical workflows are structured and executed over time.
Effective virtual clinic workflows shift care from visit-based execution to pathway-based coordination. Structured intake, intelligent routing, and continuous follow-up reduce manual handoffs and missed actions. This design protects clinical quality while allowing care teams to scale without proportional increases in workload or risk.
Virtual care operates under different constraints and opportunities. Therefore, workflows must shift from visit-based thinking to pathway-based execution. This section explains how effective virtual clinics design clinical workflows that scale safely. Each step reduces friction while protecting clinical quality.
1. Digital Intake and Risk Stratification
Digital intake sets the tone for the entire care journey. Protocol-driven questionnaires collect structured, decision-ready information before any clinician time is used. These protocols adapt based on symptoms, history, and context rather than static forms.
Red flag detection runs in the background to surface safety risks early. High-risk cases move forward with urgency, while routine cases stay streamlined. As a result, clinicians start with clarity instead of raw data.
2. Care Routing and Clinical Decision Paths
Care routing determines who handles a case and when. The system automatically directs patients to a general provider, specialist, or care coordinator based on predefined rules. Decision paths reflect clinical protocols rather than availability alone. Escalation triggers activate when risk thresholds or response delays appear.
This prevents bottlenecks and missed handoffs. Over time, routing consistency improves outcomes and accountability.
3. Follow-Ups, Monitoring, and Continuity
Continuity defines whether virtual care delivers long-term value. Virtual clinics rely on asynchronous care loops rather than repeated appointments. Task-based follow-ups replace manual reminders and memory-based tracking.
Monitoring data and patient responses feed back into the care plan automatically. Clinicians intervene when signals change, not on fixed schedules. This approach keeps care active between visits.
Strong workflow design turns virtual clinics into scalable care systems. Structured intake, intelligent routing, and continuous follow-up reduce clinical load while improving safety. When workflows align with virtual-first realities, care delivery becomes predictable and sustainable.
Where AI Adds Value In Virtual Clinic Apps
After workflows and care pathways are defined, AI becomes a force multiplier rather than a risk surface.
AI adds value in virtual clinic apps when embedded within governed workflows. It improves intake quality, prioritization, documentation, and monitoring without replacing clinical judgment. Used with human oversight and auditability, AI increases consistency and efficiency while preserving safety and regulatory trust at enterprise scale.
AI creates impact in virtual clinics only when applied to the right problems. It should reduce cognitive load, not introduce uncertainty. For enterprise teams, the value lies in speed, consistency, and better use of scarce clinical time.
When positioned correctly, AI strengthens workflows rather than sitting on top of them. This section outlines where AI delivers measurable value today. It also clarifies where restraint remains essential.
1. AI-Powered Intake, Triage, and Prioritization
AI improves care quality when it operates before clinicians engage. Intelligent intake reviews patient inputs in real time and structures them into usable clinical summaries. Risk signals surface early through pattern recognition rather than manual review.
As a result, urgent cases move faster through the system. Lower-risk cases remain streamlined without unnecessary escalation. This balance protects safety while preserving clinician capacity.
2. Clinical Decision Support
AI supports clinicians best when it augments, not replaces, judgment. Decision support tools surface relevant guidelines, history, and context during care delivery. Documentation assistance generates visit summaries and notes from structured inputs and interactions.
Clinicians spend less time on administrative work and more time on care decisions. Consistency improves across teams and services. Over time, this support stabilizes quality as volumes grow.
3. Monitoring, Alerts, and Care Continuity
AI plays a critical role in continuous care models. Monitoring systems analyze data streams from devices and patient interactions. Alerts trigger only when patterns indicate meaningful change, not noise.
Care teams focus on intervention rather than constant review. This approach supports early action without alert fatigue. Continuity improves because care responds to signals, not schedules.
AI delivers value in virtual clinic apps when it operates within governed workflows. It improves prioritization, reduces administrative load, and strengthens continuity. Used with discipline, AI becomes a force multiplier rather than a risk surface.
How We Build Enterprise-Grade Virtual Clinic Apps
Translating virtual clinic strategy into a production system requires disciplined execution across care design, architecture, and governance.
Building enterprise-grade virtual clinics requires aligning care models, architecture, compliance, and AI governance from the outset. Platforms must be designed for long-term ownership, not rapid launch. A structured, phased approach reduces downstream rework and ensures virtual care systems remain stable as services and regulations evolve.
At Intellivon, virtual clinic apps are designed as long-term operating systems for care delivery. The focus remains on how healthcare organizations actually scale services, manage risk, and sustain outcomes. Every engagement balances clinical safety, operational clarity, and enterprise growth.
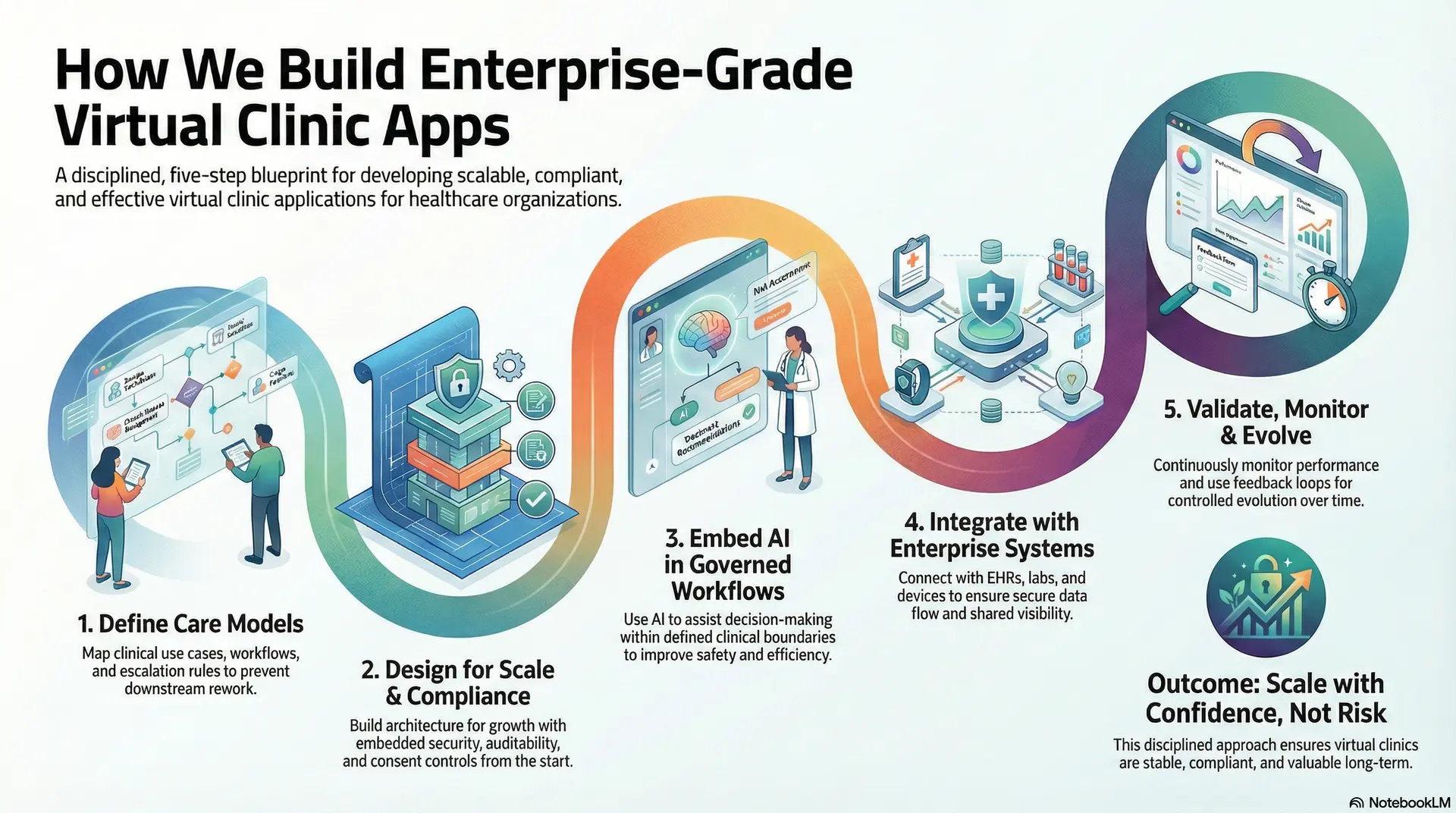
Step 1: Define Care Models
The process starts by defining how care should flow across services. Clinical use cases, ownership models, and escalation rules are mapped upfront. This ensures the platform reflects operational reality instead of assumptions. Service boundaries clarify where automation applies and where human judgment remains critical.
As a result, workflows stay consistent as services expand. This foundation prevents downstream rework.
Step 2: Design Architecture for Scale and Compliance
Enterprise platforms must assume growth from the beginning. Intellivon designs architecture with clear separation between access, workflows, data, and intelligence layers.
Compliance requirements shape system design rather than being added later. Security, auditability, and consent controls remain embedded throughout.
This structure supports expansion across regions and services. Stability improves as complexity increases.
Step 3: Embed AI Inside Governed Workflows
AI is introduced only where it improves safety and efficiency. Intake automation, risk stratification, and documentation support operate within defined clinical boundaries.
Models assist decision-making without overriding clinical authority. This approach reduces cognitive load while preserving accountability. Over time, AI adapts to real usage patterns. Value compounds without increasing risk.
Step 4: Integrate With Enterprise Systems and Data Sources
Virtual clinics cannot operate in isolation. Intellivon integrates platforms with EHRs, labs, devices, and pharmacy systems using standardized interfaces. Data flows securely and remains longitudinal across encounters.
Teams gain shared visibility without manual reconciliation. This integration supports better decisions and cleaner reporting. Operational silos are reduced.
Step 5: Validate, Monitor, and Evolve Continuously
Enterprise deployment does not end at launch. Clinical workflows, AI performance, and operational metrics are monitored continuously. Feedback loops inform refinements without disrupting care delivery.
Governance frameworks support controlled evolution over time. This ensures the platform remains aligned with changing regulations and care models. Long-term value stays intact.
Enterprise-grade virtual clinics require more than technical execution. They demand discipline across care design, architecture, and governance. When built with this approach, virtual clinics scale with confidence rather than risk.
Cost to Build a Virtual Clinic App
Cost planning reflects the clinical complexity, integration depth, and governance requirements established earlier in the virtual clinic design process.
The cost of building a virtual clinic app depends on care complexity, compliance exposure, integration depth, and scale requirements. Enterprise platforms typically require phased investment to support governance, interoperability, and resilience. Predictable budgeting focuses on long-term operation rather than short-term feature delivery.
At Intellivon, virtual clinic apps are built as enterprise-grade care delivery platforms, not as extensions of basic telemedicine tools. Cost planning is tied directly to clinical complexity, compliance exposure, and long-term operating scale.
When budget constraints exist, scope is refined collaboratively and strategically. However, clinical safety, data protection, and governance controls are never compromised. This approach balances cost discipline with scalability and defensible ROI. Enterprises gain predictability rather than hidden rework.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Clinical Alignment | Care model definition, use case prioritization, workflow mapping, compliance scope, KPI alignment | $7,000 – $14,000 |
| Architecture & Secure Platform Design | Scalable system design, data flows, identity controls, resilience planning | $9,000 – $16,000 |
| Workflow & Governance Design | Clinical pathways, escalation logic, consent rules, and role-based accountability | $8,000 – $15,000 |
| Backend & Integration Development | EHR, RPM devices, labs, pharmacy, identity, insurer, or employer systems | $14,000 – $26,000 |
| Frontend & Role-Based Interfaces | Patient, clinician, and admin experiences with accessibility controls | $11,000 – $20,000 |
| AI & Automation Layer | Intake intelligence, risk stratification, summaries, alerts, and monitoring logic | $10,000 – $18,000 |
| Security & Privacy Engineering | Encryption, access control, audit logs, monitoring, zero-trust enforcement | $9,000 – $16,000 |
| Testing & Clinical Validation | Workflow testing, security testing, compliance checks, and audit readiness | $7,000 – $12,000 |
| Deployment & Scale Readiness | Cloud deployment, observability, performance tuning, and failover planning | $8,000 – $14,000 |
Total initial investment: $80,000 – $170,000
Ongoing maintenance and optimization: 15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped virtual clinic programs face pressure when hidden cost drivers are ignored. Planning for these early protects timelines, budgets, and clinical integrity as scale increases.
- Integration complexity increases with fragmented EHRs, devices, and third-party systems
- Compliance overhead grows due to audits, reporting, and evolving healthcare regulations
- Data governance requires continuous validation, mapping, and consent enforcement
- Cloud costs rise with real-time monitoring, routing logic, and analytics workloads
- Change management includes clinician onboarding, workflow adoption, and training
- Continuous monitoring and optimization remain necessary as volume and risk evolve
Best Practices to Avoid Budget Overruns
Based on Intellivon’s enterprise healthcare delivery experience, these practices consistently lead to predictable costs and controlled growth.
- Start with a focused care scope before expanding services
- Embed clinical and compliance rules directly into workflows and architecture
- Use modular components that can be reused across programs and populations
- Balance real-time interactions with asynchronous care to control cloud spend
- Maintain continuous observability across performance, security, and compliance
- Plan for regulatory evolution rather than one-time certification
Request a tailored proposal from Intellivon’s healthcare team to receive a delivery roadmap aligned with your budget, clinical priorities, and long-term virtual care growth strategy.
Top Enterprise-Grade Virtual Clinic Apps
Enterprise leaders often evaluate real platforms to understand what scalable virtual care looks like in practice. The examples below illustrate how mature virtual clinic apps operate at scale and how they generate revenue. Each follows a consistent structure for clarity and comparison.
1. Teladoc Health
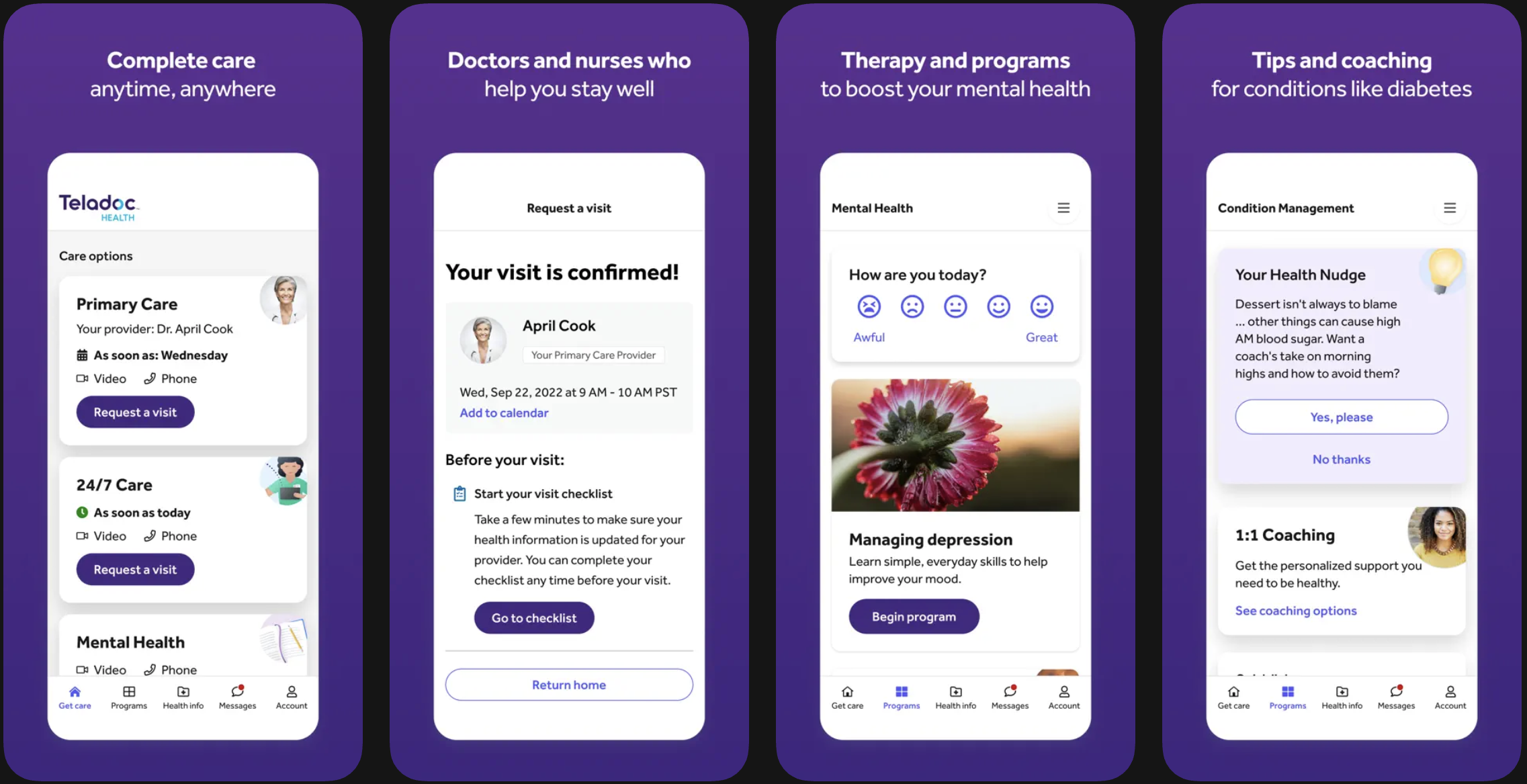
Teladoc Health operates as a multi-service virtual care platform covering primary care, mental health, and chronic condition management. Patients access care through scheduled or on-demand visits that connect to longitudinal care programs. Clinical teams coordinate across services rather than handling isolated encounters.
This structure supports continuity for high-volume populations. Monetization relies mainly on enterprise contracts with employers and payers. Revenue flows through subscription and per-member pricing models.
2. Amwell

Amwell enables health systems to deliver branded virtual care experiences. Patients interact with clinicians through integrated video visits and follow-ups embedded into existing care programs. The platform emphasizes interoperability with hospital systems and payer networks.
This allows organizations to extend services without disrupting core workflows. Amwell monetizes through platform licensing and usage-based fees. Health systems pay to operate virtual clinics under their own brand.
3. Pager
Pager focuses on care navigation rather than standalone visits. Patients begin with chat-based triage and progress to virtual or in-person care as needed. The platform coordinates nurses, physicians, and scheduling within one flow. This reduces unnecessary utilization and improves routing accuracy.
Monetization typically follows per-member per-month pricing. Insurers and health systems fund the platform as a care coordination layer.
4. K Health
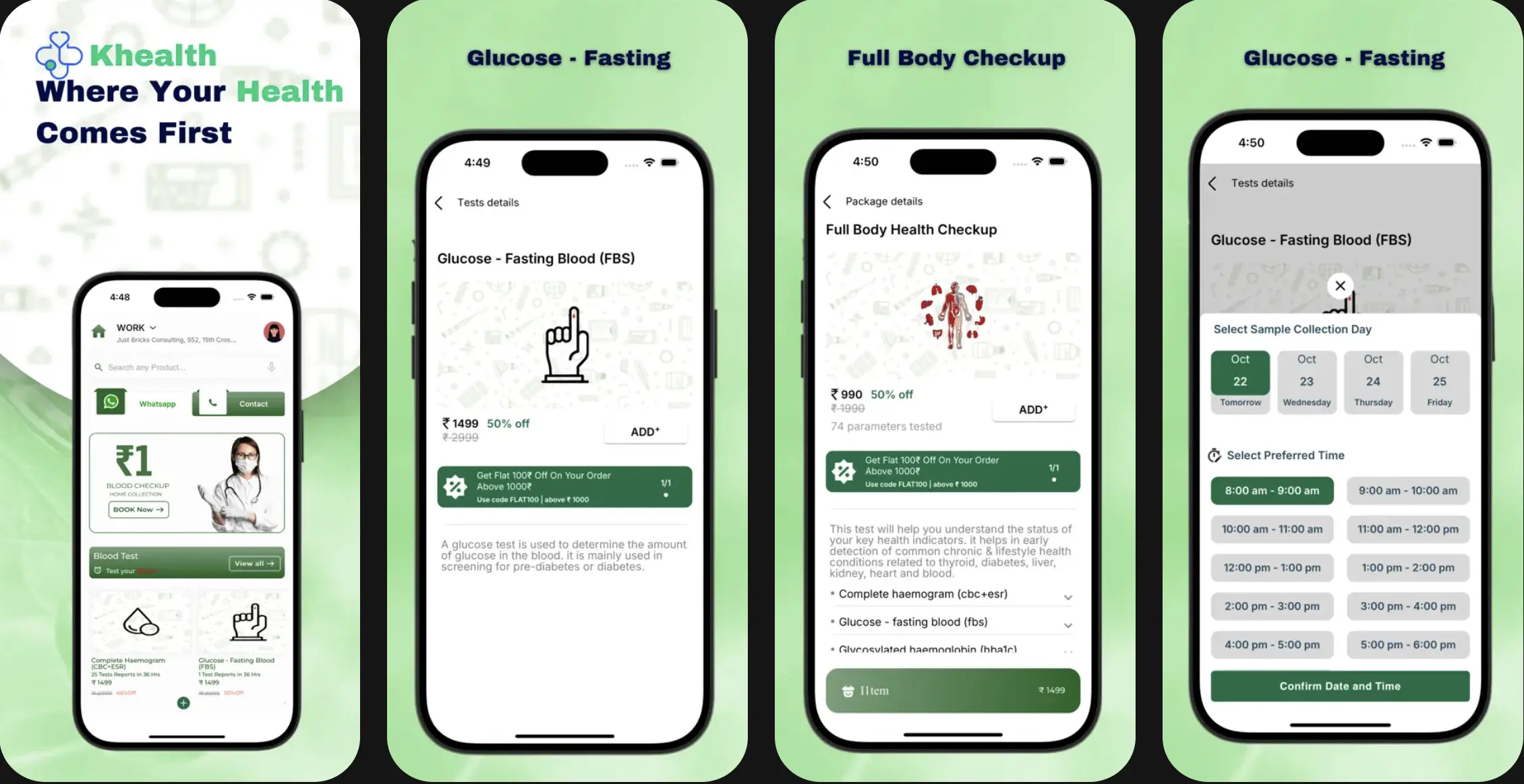
K Health combines AI-assisted intake with clinician-led primary care. Patients receive structured guidance before engaging with a provider. Clinicians review AI-generated context during consultations. This shortens visit time and standardizes intake quality.
The platform monetizes through subscriptions and per-visit fees. Partnerships with insurers extend reach and reduce per-patient costs.
These platforms show that enterprise-grade virtual clinics go beyond video visits. They integrate workflows, data, and monetization into sustainable operating models. For healthcare organizations, these examples clarify how virtual care scales when designed for real-world complexity.
Conclusion
Virtual clinic apps are best suited for hospitals, healthcare enterprises, insurers, and employer health programs responsible for sustained care delivery. These organizations benefit from coordinated workflows, longitudinal data, and governed AI. For them, virtual clinics function as operating systems that support growth without increasing operational risk.
Virtual clinic apps are no longer optional for healthcare enterprises planning long-term growth. They reshape how care is delivered, coordinated, and scaled across services.
When built with the right workflows, governance, and AI support, they improve access without increasing operational strain. More importantly, they create a foundation for continuous, data-driven care. Organizations that invest now gain flexibility as reimbursement, demand, and care models evolve.
With the right partner, virtual clinics become growth enablers rather than cost centers. Intellivon helps healthcare enterprises design and build virtual clinic platforms that scale safely, perform reliably, and deliver measurable impact.
Why Choose Intellivon As Your Virtual Clinic App Development Partner
At Intellivon, virtual clinic apps are built as enterprise care platforms, not standalone digital tools. Architecture and delivery decisions prioritize clinical reliability, regulatory alignment, and long-term scalability. This ensures platforms perform under real operational pressure, not just at launch.
As virtual clinics expand across services and populations, governance, performance, and compliance remain stable. Organizations scale care without introducing operational risk or workflow fragmentation.
Why Partner With Intellivon?
- Enterprise-grade virtual clinic architecture built for complex, multi-service care
- Proven delivery across hospital, employer, insurer, and hybrid care models
- Compliance-by-design with audit readiness and consent management
- Secure role-based access and end-to-end traceability
- AI-assisted workflows with mandatory human oversight
- Modular, cloud-native infrastructure for phased scaling
Book a strategy call to explore how Intellivon can help you build and scale a virtual clinic platform with confidence.
FAQs
Q1. What is a virtual clinic app?
A1. A virtual clinic app is a digital care platform that delivers coordinated healthcare services through structured workflows. It supports intake, consultations, follow-ups, monitoring, and care continuity across specialties. Unlike basic telemedicine apps, it operates as a governed care delivery system.
Q2. How is a virtual clinic app different from a telemedicine app?
A2. A telemedicine app focuses on individual virtual visits. A virtual clinic app manages end-to-end care journeys, workflows, and data across multiple services. It is designed for scale, compliance, and long-term care delivery rather than episodic interactions.
Q3. How much does it cost to build a virtual clinic app?
A3. Building an enterprise-grade virtual clinic app typically costs between $80,000 and $170,000. Costs depend on care complexity, compliance scope, integrations, and AI features. Ongoing maintenance usually adds 15–20% annually.
Q4. Where does AI add value in virtual clinic apps?
A4. AI adds value by improving intake quality, risk prioritization, documentation, and monitoring. It reduces clinician workload and supports faster decision-making. However, it works best when embedded within governed clinical workflows with human oversight.
Q5. Who should invest in building a virtual clinic app?
A5. Hospitals, healthcare enterprises, insurers, and employer health programs benefit most from virtual clinic apps. These platforms help scale care delivery, reduce operational strain, and support long-term digital health strategies.