Running a big healthcare network comes with a lot of responsibility for patients, staff, and the entire enterprise as a whole. As these networks grow, keeping care consistent everywhere gets tougher. What works well in one hospital might not work in another, leading to differences in patient results. And often, by the time leaders spot these problems, it’s already too late to fix them quickly.
This is not for a lack of effort because doctors and staff work hard every day. The real issue is the systems and tools in place. They just weren’t built to handle so much information or to work across such a large organization.
That is where clinical intelligence really makes a difference. Instead of just adding another dashboard or report, clinical intelligence connects data, context, and clinical expertise across every site of care. It helps all the parties involved make better decisions, no matter where they work in the hospital environment.
At Intellivon, we build these platforms specifically for large healthcare provider networks. Our tools stay up to date with the latest medical knowledge, integrate smoothly with hospital systems, and deliver the right information to the right people at the right time. In this blog, we will share what we have learned from building and deploying these healthcare platforms, and show you how we make them work in real hospital environments.
Why Large Enterprises Need Clinical Intelligence Systems Now
Large healthcare organizations are turning to clinical intelligence systems to make better use of their growing data. These platforms analyze EHR data, identify patient risks early, and improve clinical and operational workflows.
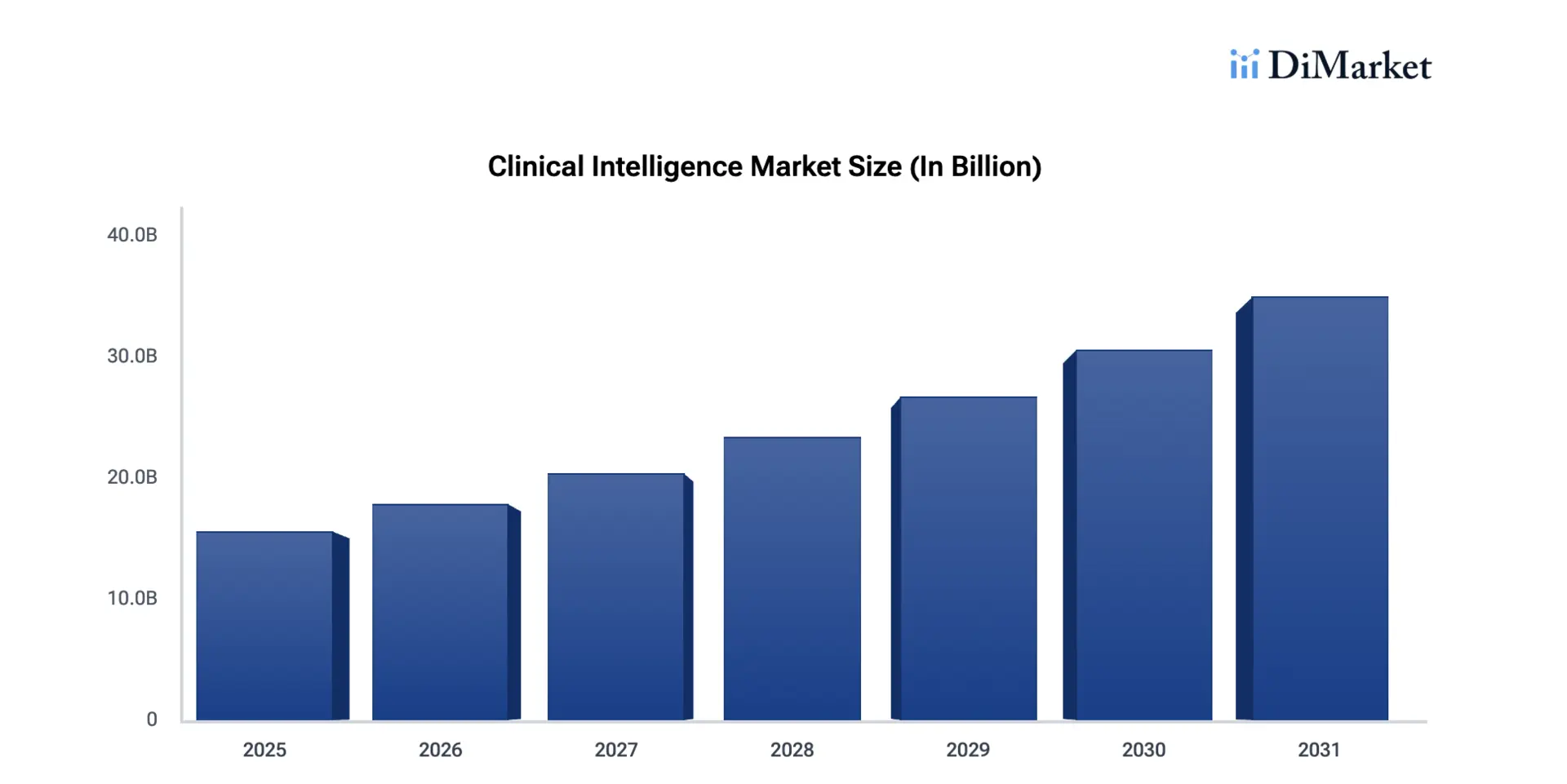
As chronic disease cases rise and value-based care expands, many providers are investing in smarter, data-driven decision support. Current industry trends show strong growth ahead. The market is expected to expand at a 14.4% compound annual growth rate, reaching about $15.61 billion by 2025.
- Rapid growth in healthcare data from EHRs, labs, and diagnostic systems is pushing providers to adopt smarter intelligence tools.
- Advances in AI and machine learning are making predictive analytics more practical and clinically useful at scale.
- Large health systems are under pressure to reduce costs while improving patient outcomes and operational efficiency.
- Rising rates of chronic diseases are increasing the need for proactive, data-driven clinical decision support.
- Regulatory requirements such as HIPAA are encouraging hospitals and provider networks to strengthen data governance and oversight.
Clinical intelligence systems help large enterprises turn raw data into timely, actionable insight. As care models become more complex, the need for real-time visibility and coordinated decision support is becoming urgent.
1. Managing Data Volume Across Complex Care Networks
Large health systems operate across multiple hospitals, clinics, and partner organizations. Each location generates valuable clinical and operational data. However, this information often sits in disconnected systems.
Clinical intelligence platforms aggregate data from EHRs, labs, imaging, and other sources into a unified view. As a result, leaders gain consistent visibility across the network. This improves coordination, reduces blind spots, and supports more confident decision-making at scale.
2. Supporting Value-Based Care and Risk Management
Payment models are shifting toward value-based care. Therefore, provider networks must monitor quality metrics, patient risk levels, and care outcomes more closely than before.
Clinical intelligence systems help identify high-risk patients earlier. They also track performance against quality benchmarks in near real time. With better insight, organizations can intervene sooner, manage risk more effectively, and protect reimbursement under value-based contracts.
3. Improving Clinical and Operational Efficiency
Many large providers still rely on manual reporting and fragmented dashboards. These approaches slow down decision-making and increase administrative burden.
This software automates data analysis and surfaces relevant insights directly within workflows. For example, care teams can receive early warnings for patient deterioration or discharge delays. Consequently, staff spend less time searching for information and more time acting on it.
4. Strengthening Enterprise-Wide Visibility and Governance
As provider networks grow, maintaining consistent oversight becomes more difficult. Leaders need clear visibility into performance, compliance, and resource utilization across facilities.
These systems provide standardized dashboards, audit trails, and performance monitoring tools. In addition, they support data governance and regulatory readiness. This level of transparency helps organizations scale operations without losing control.
5. Preparing for AI-Driven Healthcare Delivery
Healthcare is steadily moving toward predictive and AI-assisted care models. However, AI initiatives struggle when data remains fragmented or poorly normalized.
Clinical intelligence platforms create the structured, governed data foundation that advanced analytics requires. Therefore, enterprises that invest early are better positioned to deploy predictive models safely and effectively in the future.
Clinical intelligence systems provide the real-time visibility, risk awareness, and operational clarity that modern healthcare demands. Organizations that adopt these platforms now are better equipped to manage complexity, support value-based care, and scale with confidence.
What Is A Clinical Intelligence System?
A clinical intelligence system is a healthcare platform that turns clinical and operational data into actionable insights. It collects information from EHRs, labs, imaging systems, and other sources. The system then analyzes this data to identify risks, track performance, and support faster decisions.
In large provider networks, these platforms help care teams spot patient deterioration early, monitor quality metrics, and improve workflow efficiency. In addition, leadership teams gain a clear, real-time view of performance across facilities.
Unlike traditional reporting tools, clinical intelligence systems operate continuously and support proactive care management. As healthcare becomes more data-driven, these platforms are becoming essential infrastructure for modern provider organizations.
How It Works
Clinical intelligence systems follow a structured process that turns raw healthcare data into useful insight. Each stage builds on the previous one to support timely, informed decisions.
- Data sources are connected: The platform integrates with EHRs, laboratory systems, imaging platforms, pharmacy tools, and claims systems across the enterprise.
- Data is ingested and standardized: Information flows into the platform in real time or batches. It is then normalized using standards such as HL7 and FHIR.
- Data quality is validated: The system checks for missing values, duplicates, and coding inconsistencies. This step improves trust in downstream analytics.
- Patient records are unified: Identity matching links data across facilities and encounters. As a result, teams gain a longitudinal patient view.
- Analytics and risk models are applied: The platform runs rules, dashboards, and predictive models to detect clinical risks and operational trends.
- Insights are delivered into workflows: Alerts, summaries, and dashboards reach care teams and operational leaders at the right time.
- Performance is continuously monitored: Organizations track outcomes, audit decisions, and refine models to improve accuracy and impact over time.
Types of Clinical Intelligence Platforms
Clinical intelligence is not a single product category. Large provider networks deploy different platform types based on the decisions they need to support. Some focus on forecasting patient risk, while others improve workflow visibility or enterprise performance tracking.
Therefore, understanding the major platform categories helps organizations choose the right investment path and avoid capability gaps as they scale.
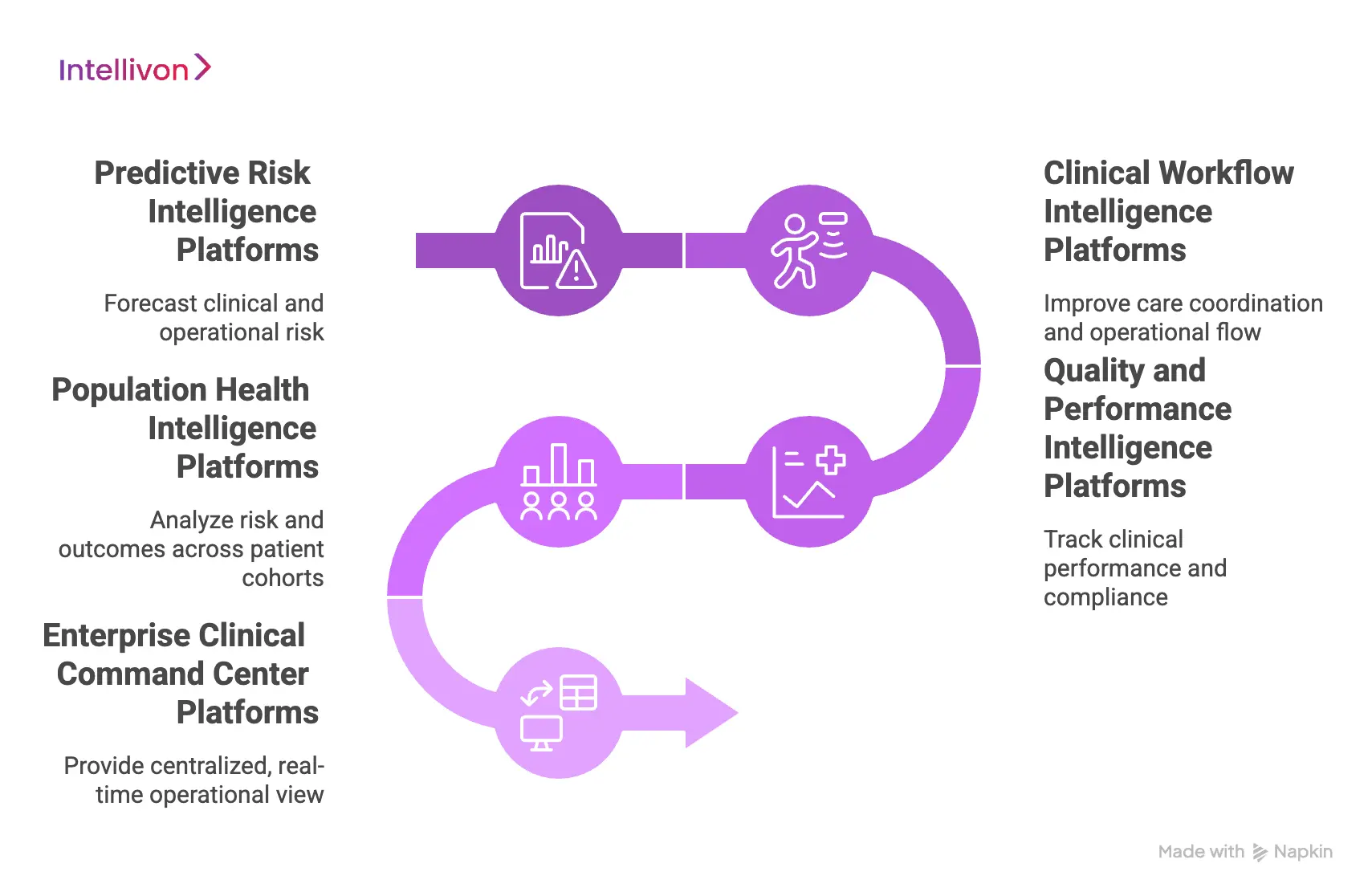
1. Predictive Risk Intelligence Platforms
Predictive risk intelligence platforms use statistical models and AI to forecast clinical and operational risk. They analyze historical and real-time data to identify patients or workflows that may require early intervention.
These systems help teams move from reactive care to proactive management. As a result, organizations can prioritize high-risk patients earlier.
What they do:
- Use statistical modeling and machine learning to forecast patient and operational risk
- Continuously analyze EHR, claims, and utilization data for early warning signals
Common capabilities:
- Readmission prediction
- Deterioration risk detection
- No-show prediction
- Length of stay forecasting
- Population risk scoring
Best fit for:
- Value-based care programs
- Care management prioritization
- Early warning initiatives
2. Clinical Workflow Intelligence Platforms
Clinical workflow intelligence platforms focus on improving care coordination and operational flow inside hospitals and health systems. Instead of predicting risk alone, they monitor how work moves across departments.
These systems surface bottlenecks, delays, and handoff gaps that affect patient flow and staff efficiency. Consequently, leaders gain better control over day-to-day operations.
What they do:
- Monitor patient movement and care progression in real time
- Identify workflow delays and coordination gaps
- Support discharge planning and throughput optimization
Common capabilities:
- Bed management visibility
- Discharge readiness tracking
- Care team task coordination
- Order and turnaround monitoring
- Throughput analytics
Best fit for:
- Patient flow optimization programs
- Hospital operations teams
- Throughput improvement initiatives
3. Quality and Performance Intelligence Platforms
Quality intelligence platforms help organizations track clinical performance, compliance, and outcome metrics across facilities. They are especially important in value-based and regulated care environments.
These systems provide standardized scorecards and performance dashboards. In addition, they support audit readiness and quality reporting requirements.
What they do:
- Monitor quality measures and compliance indicators
- Track provider and service line performance
- Support regulatory and accreditation reporting
Common capabilities:
- HEDIS and quality metric tracking
- Core measure monitoring
- Provider performance dashboards
- Variation analysis
- Regulatory reporting support
Best fit for:
- Quality improvement programs
- Value-based reimbursement environments
- Enterprise performance oversight
4. Population Health Intelligence Platforms
Population health intelligence platforms analyze risk and outcomes across large patient cohorts. They help provider networks manage chronic conditions and value-based populations more effectively.
These systems aggregate clinical, claims, and social data to identify care gaps and high-risk groups. Therefore, care management teams can intervene earlier at scale.
What they do:
- Stratify populations by risk and utilization
- Identify care gaps across cohorts
- Support preventive and longitudinal care planning
Common capabilities:
- Chronic disease risk stratification
- Care gap identification
- Cohort segmentation
- Preventive care tracking
- Utilization trend analysis
Best fit for:
- ACOs and value-based care programs
- Chronic disease management initiatives
- Large multi-facility provider networks
5. Enterprise Clinical Command Center Platforms
Clinical command center platforms provide a centralized, real-time operational view across the health system. They combine multiple intelligence streams into a single control layer.
These environments support system-wide decision-making during both routine operations and capacity stress events. As a result, leadership teams gain faster situational awareness.
What they do:
- Provide real-time enterprise-wide visibility
- Combine clinical, operational, and capacity signals
- Support rapid escalation and coordination
Common capabilities:
- System-wide patient flow monitoring
- Capacity and demand forecasting
- Cross-facility dashboards
- Escalation alerts
- Command center visualization
Best fit for:
- Large integrated delivery networks
- Multi-hospital systems
- Centralized operations teams
Clinical intelligence platforms serve different but complementary roles across large provider networks. Organizations that align the right platform type with their strategic priorities typically achieve faster operational and clinical impact.
Why Traditional Analytics Fail at The Enterprise-Level
Traditional healthcare analytics fails at enterprise scale because it relies on static reports, delayed data, and fragmented views that cannot support real-time clinical and operational decisions.
Many large provider networks still rely on legacy analytics tools and static reporting. These systems worked when data volumes were smaller, and care delivery was less complex. However, enterprise healthcare environments now operate in real time and across multiple facilities. Traditional analytics struggles to keep pace with this scale and speed.
As a result, leadership teams often receive delayed insights, fragmented reports, and limited predictive visibility. Clinical intelligence systems address these gaps by delivering continuous, workflow-aware intelligence rather than retrospective summaries.
1. Delayed and Retrospective Reporting
Traditional analytics platforms typically produce scheduled reports. These reports often reflect what already happened rather than what is about to happen.
In fast-moving care environments, delayed insight limits the ability to intervene early. For example, a deterioration risk report delivered days later offers little clinical value. Enterprise teams need continuous monitoring, not monthly or weekly summaries.
2. Fragmented Data Across Systems
Large provider networks operate dozens of clinical and operational systems. Legacy analytics tools often pull from limited data sources or require heavy manual integration.
Because of this, decision-makers rarely see a complete patient or operational picture. Data silos create blind spots across facilities and departments. Over time, these gaps reduce confidence in analytics outputs.
3. Limited Support for Real-Time Workflows
Traditional business intelligence tools were designed for reporting, not for live clinical workflows. They generate dashboards but rarely deliver insights directly into care or operations.
However, modern healthcare requires intelligence that reaches the right team at the right moment. Without workflow integration, even accurate analytics may go unused.
4. Weak Predictive and Risk Capabilities
Many legacy analytics environments rely on historical trend analysis alone. While useful for reporting, this approach does not provide forward-looking risk visibility.
Enterprise provider networks now need early warning signals for readmissions, deterioration, and capacity strain. Clinical intelligence systems apply advanced models that move beyond descriptive analytics into predictive support.
5. Scalability and Performance Constraints
As data volume grows, traditional analytics platforms often struggle with performance and refresh speed. Batch processing pipelines can become slow and difficult to maintain.
In large health systems, this creates delays exactly when real-time insight is most valuable. Modern intelligence platforms are designed for high-volume, continuously updating environments.
Traditional analytics tools were built for a slower, more centralized healthcare model. Today’s large provider networks require continuous, real-time intelligence that supports both clinical and operational decisions.
Organizations that move beyond static reporting are better positioned to manage complexity and respond faster to emerging risks.
Core Capabilities of an Enterprise Clinical Intelligence System
An enterprise clinical intelligence system combines real-time data aggregation, predictive analytics, workflow integration, and governance controls to support system-wide clinical and operational decisions.
Enterprise provider networks operate across multiple hospitals, clinics, and partner systems. Therefore, a clinical intelligence system must do far more than generate reports. It must continuously process data, surface risk early, and support coordinated action across the organization.
The most effective platforms combine real-time analytics, strong data governance, and workflow-aware delivery. When these capabilities work together, healthcare leaders gain the visibility and control required at scale.
1. Real-Time Data Aggregation and Normalization
Enterprise environments generate data from many sources every minute. A strong clinical intelligence system must ingest and standardize this information continuously.
The platform connects to EHRs, labs, imaging systems, pharmacy tools, and claims platforms. It then normalizes the data using standards such as HL7 and FHIR. As a result, teams work from a consistent and trusted data foundation.
Why it matters at scale:
- Eliminates data silos across facilities
- Supports near real-time visibility
- Improves data consistency for analytics and AI
2. Unified Longitudinal Patient View
Large networks often struggle with fragmented patient records across facilities. Identity mismatches and duplicate records can weaken clinical insight.
Enterprise intelligence platforms resolve identities and link encounters over time. This creates a longitudinal patient view that follows individuals across care settings. Consequently, clinicians and care managers gain a better context for decision-making.
Enterprise impact:
- Improves care continuity
- Strengthens risk detection
- Supports population health programs
3. Advanced Predictive and Risk Analytics
Descriptive dashboards are no longer sufficient for large health systems. Enterprises need forward-looking insight that highlights emerging risk.
Clinical intelligence systems apply statistical models and machine learning to identify patterns early. These may include deterioration risk, readmission likelihood, or capacity strain. Therefore, teams can intervene before issues escalate.
Typical predictive capabilities:
- Readmission risk scoring
- Clinical deterioration alerts
- Length of stay forecasting
- No-show prediction
- Population risk stratification
4. Workflow-Aware Intelligence Delivery
Insight has limited value if it sits in a dashboard. Enterprise platforms must deliver intelligence directly into clinical and operational workflows.
Modern systems push alerts, task prompts, and summaries to the appropriate teams at the right moment. In addition, role-based dashboards help different users focus on what matters most. This approach increases adoption and speeds response times.
Where this creates value:
- Care coordination
- Discharge planning
- Capacity management
- Utilization review
5. Enterprise Performance and Quality Monitoring
Large provider networks must track quality metrics, utilization patterns, and financial performance across facilities. Manual reporting cannot keep up with this demand.
Clinical intelligence systems provide standardized scorecards and near real-time performance dashboards. Leaders can monitor trends, identify variation, and act quickly when performance drifts.
Key monitoring areas:
- Quality and safety metrics
- Value-based performance indicators
- Service line efficiency
- Provider utilization patterns
6. Strong Data Governance and Compliance Controls
Healthcare enterprises operate under strict regulatory oversight. Therefore, intelligence platforms must include built-in governance.
Enterprise-grade systems enforce role-based access, audit logging, and consent controls. They also support HIPAA-aligned data protection and monitoring. This ensures that insight delivery does not create compliance risk.
Governance capabilities include:
- Role-based access control
- Audit trail visibility
- Data lineage tracking
- PHI protection safeguards
7. Scalable, High-Availability Architecture
Large provider networks cannot tolerate downtime or performance bottlenecks. Clinical intelligence platforms must scale as data volume and user demand grow.
Enterprise systems use cloud-native or hybrid architectures that support high throughput and resilience. As a result, organizations maintain stable performance even during peak usage.
Scalability benefits:
- Supports multi-facility expansion
- Handles real-time data streams
- Maintains consistent performance under load
An enterprise clinical intelligence system must do more than analyze data. It must unify information, predict risk, support workflows, and maintain strong governance at scale. Organizations that invest in these core capabilities gain faster insight, tighter operational control, and a stronger foundation for AI-driven care.
Operating Models for Clinical Intelligence in Large Provider Networks
Large provider networks rarely succeed with a one-size approach to clinical intelligence. The operating model determines how insight flows, who acts on it, and how quickly value appears. Therefore, choosing the right model is as important as selecting the platform itself.
Most enterprises adopt one of several proven models based on their scale, governance maturity, and care delivery structure. In many cases, organizations evolve from one model to another as their data and coordination capabilities improve.
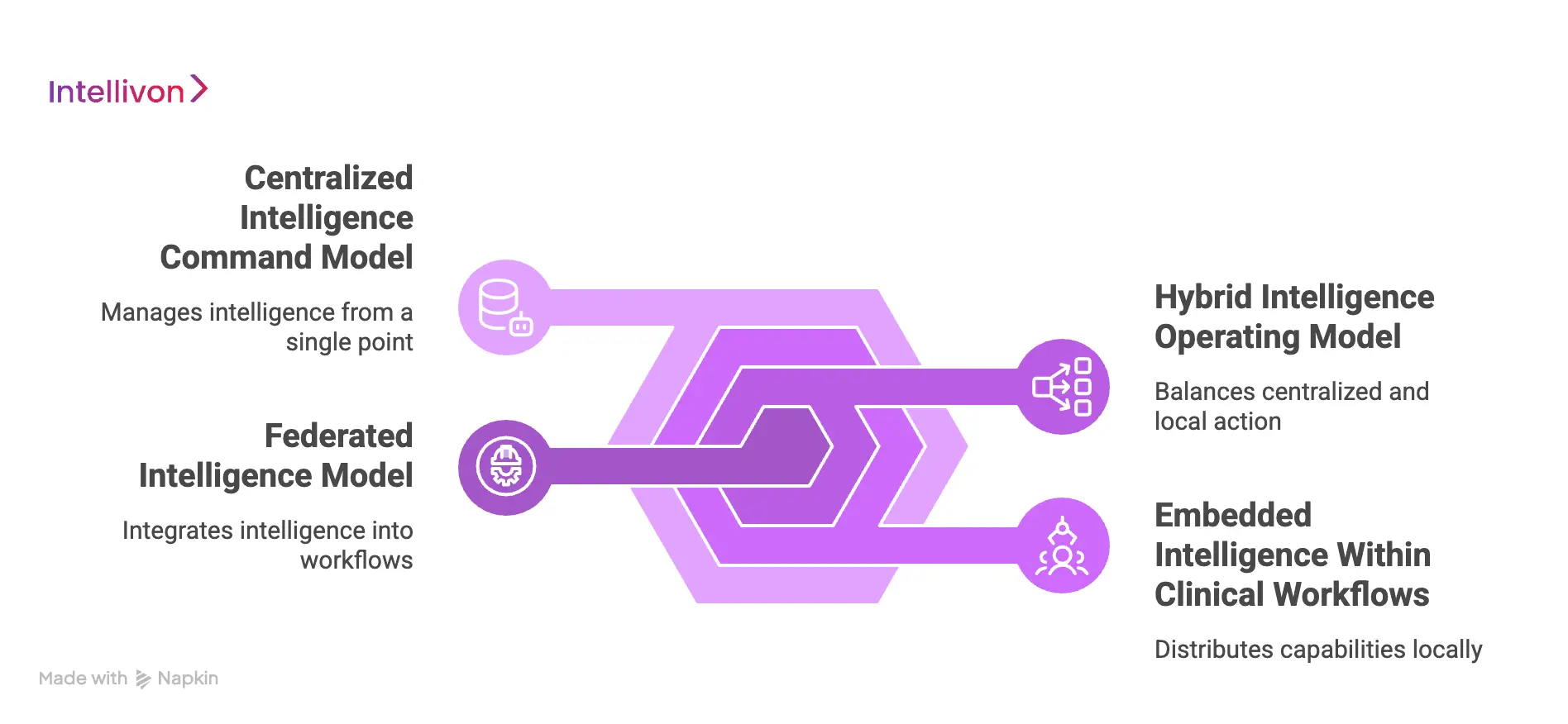
1. Centralized Intelligence Command Model
In this model, a central analytics or operations team manages the clinical intelligence platform. The team monitors system-wide dashboards, risk signals, and performance metrics from a single control point.
This approach works well when leadership wants strong oversight and standardized processes. In addition, it helps multi-hospital systems maintain consistent quality and reporting practices.
How it typically operates:
- A central command center monitors enterprise-wide data
- Alerts and insights flow outward to hospitals and care teams
- Governance and model management remain tightly controlled
Best suited for:
- Large integrated delivery networks
- Health systems with centralized governance
- Organizations building enterprise command centers
2. Federated Intelligence Model
The federated model distributes intelligence capabilities closer to the point of care. Individual hospitals or service lines access shared data but act locally on insights.
This model supports flexibility and faster local decision-making. However, it requires strong data standards to maintain consistency across the network.
How it typically operates:
- Shared data platform across the enterprise
- Local teams manage workflows and interventions
- Governance standards remain centrally defined
Best suited for:
- Multi-hospital systems with semi-independent facilities
- Academic medical networks
- Organizations prioritizing local clinical autonomy
3. Hybrid Intelligence Operating Model
Many large provider networks ultimately move toward a hybrid model. This approach combines centralized oversight with local execution.
A central team manages data pipelines, models, and governance. Meanwhile, hospitals and care teams act on insights within their workflows. As a result, organizations gain both consistency and responsiveness.
How it typically operates:
- Centralized data and model management
- Distributed clinical and operational action
- Shared performance monitoring across the network
Best suited for:
- Mature enterprise health systems
- Organizations scaling value-based care
- Networks balancing control with agility
4. Embedded Intelligence Within Clinical Workflows
Some organizations focus on embedding intelligence directly into EHR workflows rather than building a visible command layer. In this model, clinicians receive alerts and recommendations within the tools they already use.
This approach drives strong adoption because it minimizes disruption. However, it still depends on a robust intelligence backbone behind the scenes.
How it typically operates:
- Risk signals appear inside the EHR or care management tools
- Minimal need for separate dashboards
- Workflow integration drives usage
Best suited for:
- Clinician-driven environments
- Organizations focused on point-of-care decisions
- Networks early in their intelligence journey
The operating model shapes how clinical intelligence delivers real value across large provider networks. Organizations that align governance, workflows, and technology under the right model typically see faster adoption and stronger outcomes.
As networks mature, many evolve toward hybrid approaches that balance centralized control with local clinical action.
Use Cases Of Clinical Intelligence Systems for Large Provider Networks
Large provider networks generate constant streams of clinical and operational data. However, value appears only when that data drives timely action. Clinical intelligence systems help organizations move from passive reporting to proactive intervention across the care continuum.
Below are high-impact use cases where large health systems typically see measurable improvement in quality, efficiency, and financial performance.
1. Early Patient Deterioration Detection
Care teams often struggle to spot subtle signs of patient decline. Traditional monitoring may miss early warning signals until the condition worsens.
Clinical intelligence platforms continuously analyze vitals, labs, and clinical notes. When risk patterns appear, the system alerts the care team quickly. As a result, clinicians can intervene earlier and reduce adverse events.
Typical impact areas:
- Sepsis and clinical deterioration monitoring
- Rapid response activation
- ICU transfer prevention
- Patient safety improvement
2. Readmission Risk Management
Avoidable readmissions remain a major financial and quality concern. Large networks need better visibility into which patients require follow-up support.
These systems score readmission risk before discharge. Care managers can then prioritize outreach and post-discharge planning. Therefore, organizations improve continuity of care and protect value-based reimbursement.
Where it helps most:
- High-risk discharge planning
- Transitional care programs
- Value-based contracts
- Care management prioritization
3. Length of Stay and Throughput Optimization
Bed capacity and patient flow directly affect both revenue and patient experience. However, delays often remain hidden inside complex workflows.
Clinical intelligence platforms monitor discharge readiness, bottlenecks, and unit capacity in near real time. Operations teams can act sooner to remove barriers. Consequently, hospitals improve bed turnover and reduce unnecessary days.
Operational benefits:
- Faster discharge planning
- Improved bed utilization
- Reduced ED boarding
- Better capacity forecasting
4. No-Show and Schedule Optimization
Missed appointments create revenue loss and disrupt care continuity. Large networks need better ways to predict and prevent no-shows.
These systems analyze scheduling history, patient behavior, and access patterns. The platform flags high-risk appointments and supports targeted reminders or overbooking strategies. As a result, clinics improve utilization and reduce schedule gaps.
Common improvements:
- Lower no-show rates
- Better clinic utilization
- Improved access management
- Stronger revenue capture
5. Population Health and Chronic Disease Management
Managing chronic conditions across large populations requires continuous risk visibility. Manual tracking cannot scale effectively.
Clinical intelligence platforms stratify populations by risk and identify care gaps. Care teams can then focus outreach on patients who need attention first. In addition, leadership gains clearer insight into cohort performance.
Best-fit programs:
- Diabetes and heart failure management
- Value-based population programs
- Preventive care outreach
- Risk-based care management
6. Enterprise Command Center Visibility
Large provider networks often lack a unified operational view. This makes it difficult to coordinate resources during demand surges.
These systems power enterprise command centers with real-time dashboards. Leaders can monitor patient flow, capacity, and risk signals across facilities. Therefore, the organization responds faster during both routine operations and peak demand periods.
Enterprise advantages:
- System-wide situational awareness
- Faster escalation decisions
- Improved cross-facility coordination
- Stronger operational control
Clinical intelligence systems create value across clinical care, operations, and population health. Large provider networks that deploy these platforms strategically often see earlier risk detection, smoother patient flow, and stronger financial performance.
How We Build Clinical Intelligence Systems For Large Enterprises
Intellivon builds clinical intelligence systems through a step-by-step approach that starts with governance and data readiness, then delivers interoperable, workflow-integrated intelligence at enterprise scale.
Large provider networks do not need another dashboard. They need a clinical intelligence layer that works across facilities, workflows, and data sources. That requires disciplined architecture, strong governance, and a delivery model built for real hospital conditions.
At Intellivon, we build clinical intelligence systems as enterprise-grade healthcare infrastructure. We focus on interoperability, data trust, and workflow impact from the start. Therefore, the platform supports both clinical action and operational control at scale.
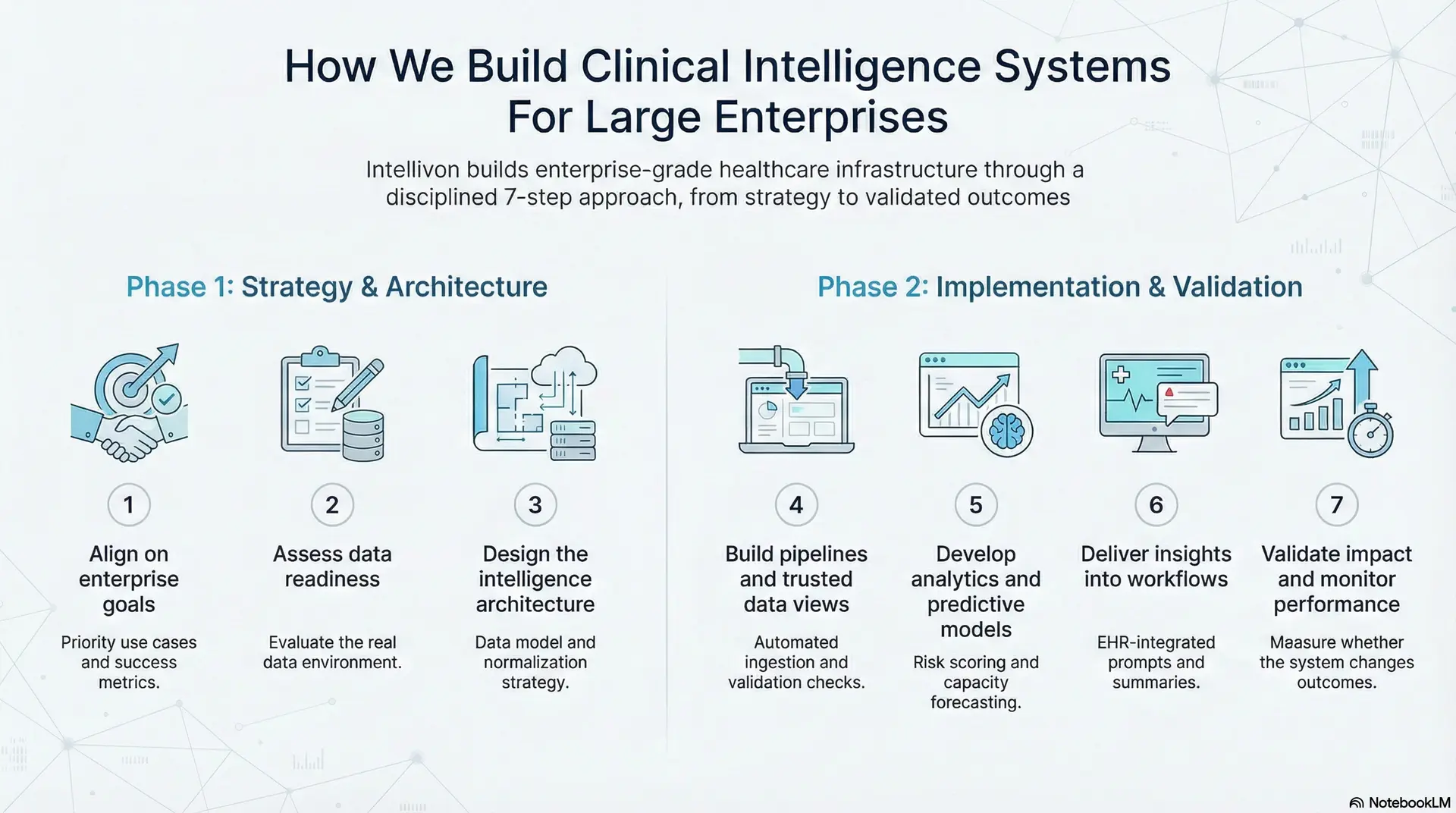
Step 1: Align on enterprise goals
We start by clarifying what decisions the system must improve. This prevents teams from building reports that do not drive action. We map who needs insight, when they need it, and how they will respond.
What we define in this step:
- Priority use cases and success metrics
- Clinical and operational workflows were affected
- Facilities, service lines, and rollout scope
- Stakeholders and ownership for action
Step 2: Assess data readiness
Next, we evaluate the real data environment. Large networks often have multiple EHR instances, varied documentation habits, and inconsistent coding. Therefore, we identify gaps before engineering begins.
What we assess:
- EHR, lab, imaging, pharmacy, claims, and scheduling sources
- Data quality issues and missing fields
- Identity matching and duplicate record risk
- HL7 and FHIR integration approach
Step 3: Design the intelligence architecture
We design the platform for long-term stability. This includes ingestion pipelines, a normalized data layer, and rules for access and audit control. In addition, we define governance so the system remains safe and trusted as it scales.
What we establish:
- Data model and normalization strategy
- Role-based access and audit logging
- Consent and PHI handling controls
- Reliability, uptime, and performance targets
Step 4: Build pipelines and trusted data views
We then build the data layer that powers the intelligence outputs. This is where we ingest, clean, and standardize data. We also create unified patient views across encounters and facilities.
What we deliver:
- Automated ingestion and validation checks
- Standardized terminology mapping
- Identity resolution and longitudinal records
- Trusted datasets for analytics and reporting
Step 5: Develop analytics and predictive models
Once the data foundation is stable, we build the intelligence layer. This includes dashboards, risk scoring, and workflow triggers. However, we only deploy models that can be validated and monitored properly.
Typical intelligence components:
- Deterioration and readmission risk scoring
- Length of stay and capacity forecasting
- No-show prediction and access insights
- Quality and performance monitoring
Step 6: Deliver insights into workflows
Adoption depends on delivery. Therefore, we embed insights into the tools teams already use. We also route alerts based on role and urgency to reduce alert fatigue.
How we drive real usage:
- Role-based dashboards and worklists
- EHR-integrated prompts and summaries
- Escalation pathways for high-risk signals
- Alert tuning and threshold governance
Step 7: Validate impact and monitor performance
Finally, we measure whether the system changes outcomes. We track both clinical and operational impact, then expand in controlled phases. This keeps cost and risk predictable while the platform grows.
What we monitor:
- Model accuracy and false alert rates
- Response time and workflow adoption
- Quality, throughput, and revenue impact
- Data drift and integration stability
Intellivon builds clinical intelligence systems with a structured enterprise approach. We start with governance and data trust, then deliver workflow-integrated intelligence that scales across facilities. As a result, large provider networks gain faster insight, stronger operational control, and a clear path to measurable outcomes.
Managing Alert Fatigue in Clinical Intelligence Systems
Clinical intelligence systems can surface valuable risk signals. However, too many alerts can overwhelm care teams and reduce trust in the platform. When clinicians receive constant notifications, important warnings may be ignored or delayed.
Large provider networks must treat alert design as a clinical safety issue, not just a technical setting. The goal is to deliver the right signal to the right person at the right time. When managed well, intelligence platforms improve response speed without increasing noise.
1. Prioritize High-Value Alerts First
Not every risk signal requires immediate action. Therefore, organizations should classify alerts based on clinical urgency and expected impact.
High-severity alerts must stand out clearly. Lower-priority signals can appear in dashboards or summary views instead of interrupting workflows. This approach helps teams focus on what truly requires attention.
Practical steps:
- Define severity tiers for alerts
- Reserve interruptive alerts for critical events
- Route informational signals to passive views
2. Use Role-Based Alert Routing
Different teams need different types of intelligence. A one-size alert strategy often creates unnecessary noise across the enterprise.
Clinical intelligence systems should route alerts based on role, specialty, and workflow context. For example, bedside clinicians may receive deterioration warnings, while operations teams see capacity risks. As a result, each group receives fewer but more relevant signals.
Key benefits:
- Reduces alert overload
- Improves response accuracy
- Increases user trust
3. Embed Intelligence Into Existing Workflows
Alerts that sit outside daily workflows are more likely to be ignored. Therefore, delivery should occur inside the tools teams already use.
When intelligence appears within the EHR or care management workflow, teams can act immediately without switching systems. In addition, this reduces the need for duplicate notifications.
Where to embed alerts:
- EHR patient views
- Care management worklists
- Bed management dashboards
- Discharge planning screens
4. Continuously Tune and Govern Alert Logic
Alert fatigue often grows slowly over time. New rules are added, thresholds drift, and signal quality declines.
Enterprise teams should regularly review alert performance. This includes monitoring override rates, response times, and clinical outcomes. Based on these insights, thresholds and rules can be refined.
Governance best practices:
- Track alert acceptance and dismissal rates
- Review high-volume alerts quarterly
- Retire low-value rules
- Validate clinical impact regularly
5. Apply AI Carefully to Reduce Noise
AI and predictive models can improve alert precision. However, poorly tuned models may increase false positives.
Organizations should use explainable models and validate them in real clinical settings. In addition, confidence thresholds should be calibrated to balance sensitivity and specificity. When implemented carefully, AI can reduce unnecessary alerts while preserving early warning capability.
Alert fatigue is a real risk in large-scale clinical intelligence programs. However, disciplined alert design, role-based routing, and ongoing governance can keep signal quality high. Provider networks that manage alert noise effectively see stronger adoption, faster response times, and safer clinical operations.
Conclusion
Clinical intelligence systems are quickly becoming core infrastructure for large provider networks. As data volumes grow and care models become more complex, delayed reporting is no longer enough. Organizations need real-time insight that supports clinical decisions, operational flow, and financial performance.
Enterprises that invest early in governed, workflow-aware intelligence platforms position themselves to respond faster and scale with confidence. However, success depends on strong architecture, clean data foundations, and disciplined execution.
Intellivon helps healthcare enterprises design and deploy clinical intelligence systems that deliver measurable impact. If your organization is planning the next phase of digital transformation, now is the right time to build an intelligence layer that drives both efficiency and long-term growth.
Build A Clinical Intelligence System With Intellivon
At Intellivon, clinical intelligence systems are engineered as governed healthcare intelligence infrastructure, not as analytics layered onto fragmented reporting environments. Every architectural and delivery decision focuses on data trust, workflow integration, and real-time operational visibility.
As enterprise provider networks grow more complex, consistency becomes critical. Governance, performance, and audit readiness remain stable even as data volume, predictive models, and system integrations expand. Therefore, organizations retain control over clinical and operational decisions while continuing to improve performance at scale.
Why Partner With Intellivon?
- Enterprise-grade clinical intelligence architecture designed for regulated healthcare ecosystems
- Proven delivery across hospitals, multi-facility health systems, and digital care environments
- Compliance-by-design approach with embedded data governance and audit visibility
- Secure modular infrastructure supporting cloud, hybrid, and on-prem deployments
- AI-enabled monitoring, risk stratification, and performance intelligence with strong governance controls
Book a strategy call to explore how Intellivon can help you build and scale clinical intelligence systems with confidence, control, and long-term enterprise value.
FAQs
Q1. What is a clinical intelligence system in healthcare?
A1. A clinical intelligence system is a platform that analyzes clinical and operational data to support faster, better decisions. It aggregates data from EHRs, labs, and other sources. As a result, care teams and leaders gain real-time visibility into risk, performance, and workflow efficiency.
Q2. How do large provider networks benefit from clinical intelligence systems?
A2. Large provider networks use clinical intelligence systems to detect patient risk earlier, improve care coordination, and optimize operations. In addition, these platforms help organizations manage value-based care programs and monitor performance across multiple facilities.
Q3. How long does it take to implement a clinical intelligence platform?
A3. Implementation timelines usually range from 4 to 12 months, depending on data complexity, integration scope, and rollout scale. However, many enterprises launch high-priority use cases first and then expand in phases to reduce risk and accelerate early value.
Q4. What data sources are required for clinical intelligence systems?
A4. Most platforms integrate with EHRs, laboratory systems, imaging platforms, pharmacy tools, claims data, and scheduling systems. In addition, some organizations include remote monitoring and social determinants data to strengthen predictive accuracy.
Q5. What are the biggest challenges when deploying clinical intelligence at scale?
A5. The most common challenges include fragmented data, inconsistent data quality, alert fatigue, and workflow adoption barriers. However, organizations that prioritize governance, interoperability, and phased rollout typically overcome these risks and achieve stronger outcomes.