Wearable devices have become essential for patients tracking their health. Millions of people now monitor heart rate, sleep, activity, glucose, and oxygen levels through platforms like Apple Health and connected consumer or clinical-grade devices. At the same time, leading virtual care platforms, such as Teladoc Health, show how wearable data can enhance remote care programs and clinician workflows when integrated properly.
What sets these successful models apart from most implementations is orchestration, which determines when wearable signals trigger care workflows and who is responsible for acting on them. This is because care improves when wearable signals are filtered, contextualized, and routed into the correct workflows at the right time, with clear clinical responsibility. Simply sending data to an EHR or dashboard is not enough. Instead, structured summaries, event-driven triggers, and governed decision pathways make a significant difference.
At Intellivon, we view wearable integration as a care orchestration challenge rather than just a connectivity task. In this blog, we will explain how to connect wearable devices to EHR and telehealth data streams using proven strategies, API architecture, AI signal intelligence, and workflow design.
The Rise Of Wearable Data Creates Demand For EHR-Led Integration
The global wearable technology market is estimated at USD 203.38 billion in 2025. It is expected to grow to USD 231.45 billion in 2026 and reach nearly USD 703.32 billion by 2035, reflecting a CAGR of 13.21% between 2026 and 2035. Much of this growth is now coming from healthcare use cases, where wearables are increasingly embedded into remote monitoring, virtual care, and longitudinal treatment models.
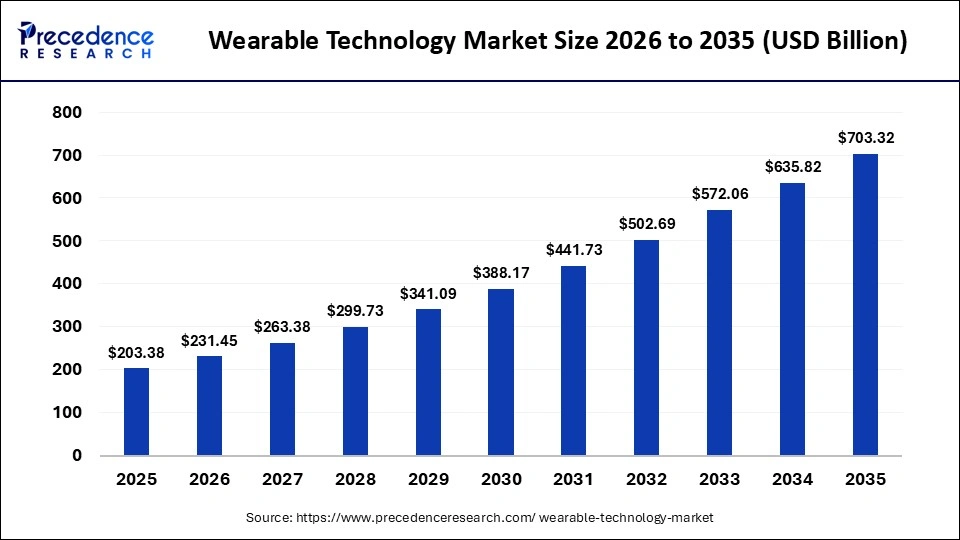
Market Insights:
- Wrist-worn devices are expected to account for nearly 49% of the total market share in 2025, driven by advanced health monitoring features.
- North America is projected to lead global adoption with around 39% market share in 2025, supported by strong IoT and consumer electronics penetration
- Wearable usage among US adults increased to over 36% in 2022, up from approximately 28–30% in 2019, largely influenced by COVID-era health awareness.
- Around 30% of US adults now use wearable devices specifically for health and wellness monitoring.
- Nearly 47% of wearable users engage with their devices daily, indicating consistent and ongoing usage.
- More than 80% of users report willingness to share wearable data with healthcare providers.
- An estimated 142 million Americans actively use health-tracking wearables, generating roughly 2.8 petabytes of data each year.
Demand for EHR–wearable integration is increasing as clinical systems adapt to patient-generated health data. Around 67% of major EHR platforms now support direct wearable connections through APIs such as Apple HealthKit, Google Fit, and Fitbit.
Patient behavior is accelerating this shift. Roughly one in three US adults uses health wearables, and more than 80% are willing to share their data with clinicians. This is pushing EHRs beyond documentation toward active roles in remote and longitudinal care.
Reimbursement trends reinforce this demand. Remote patient monitoring claims grew by nearly 1,294% between 2019 and 2022, driven by wearable data integrated into chronic care workflows. The healthcare data integration market, including wearables, is projected to expand from USD 28.5 billion in 2025 to USD 100.7 billion by 2034, at a 15% CAGR.
Why Is It Essential To Integrate Wearable Devices Into Telehealth and EHR
As wearable adoption grows, enterprises face a new operational reality. Health data is being generated continuously, while clinical systems are designed for structured, accountable decisions. However, integration is what enables organizations to manage this gap at scale.
For enterprises, wearable integration reflects control, efficiency, and sustainability across modern care models.
1. Enables Scalable Remote Care Models
Remote and hybrid care programs rely on continuous health signals. Without integration, teams must manually review data across multiple tools.
Integrated wearables allow enterprises to support larger patient populations without increasing clinical workload at the same rate. Data flows directly into telehealth workflows and EHR systems, where it can be acted on efficiently.
2. Reduces Clinical And Operational Risk
Unintegrated wearable data creates ambiguity. This is where dignals may be seen but not owned. However, integration establishes clear pathways for review, escalation, and documentation.
It defines who is responsible for acting on data and ensures decisions are recorded within governed systems. This reduces liability and improves audit readiness.
3. Improves Care Team Efficiency
High-volume wearable data can overwhelm care teams, and not every signal requires action.
Integration allows systems to filter noise and surface only clinically relevant information. As a result, clinicians receive fewer alerts and make decisions at the right moment, not after the fact.
4. Supports Reimbursement And Program Viability
Many reimbursement models depend on documented monitoring and follow-up. Wearable data must be tied to clinical actions.
Integration ensures that data supporting RPM and chronic care programs is captured within EHR workflows. This strengthens billing integrity and long-term program sustainability.
5. Creates Foundation For AI Applications
AI and analytics depend on clean, structured data. However, wearables generate volume, but integration provides context.
When wearable data is integrated into telehealth and EHR systems, enterprises can safely apply AI for trend analysis, risk detection, and population insights. Without integration, advanced intelligence remains unreliable.
Wearable devices are increasing data volume across healthcare, and integration is what makes that data usable at scale.
For enterprises, integrating wearables into telehealth and EHR systems is essential to reduce risk, improve efficiency, and sustain modern care models. Without it, wearable programs struggle to deliver lasting operational value.
Types Of Wearable Data Enterprises Must Handle
Wearable devices generate far more than simple health readings. For enterprises, the challenge is not collecting this data. It is determining how each data type should be validated, routed, and acted on within clinical systems.
Different categories of wearable data carry different levels of risk, urgency, and operational impact. Treating them the same creates noise and inefficiency.
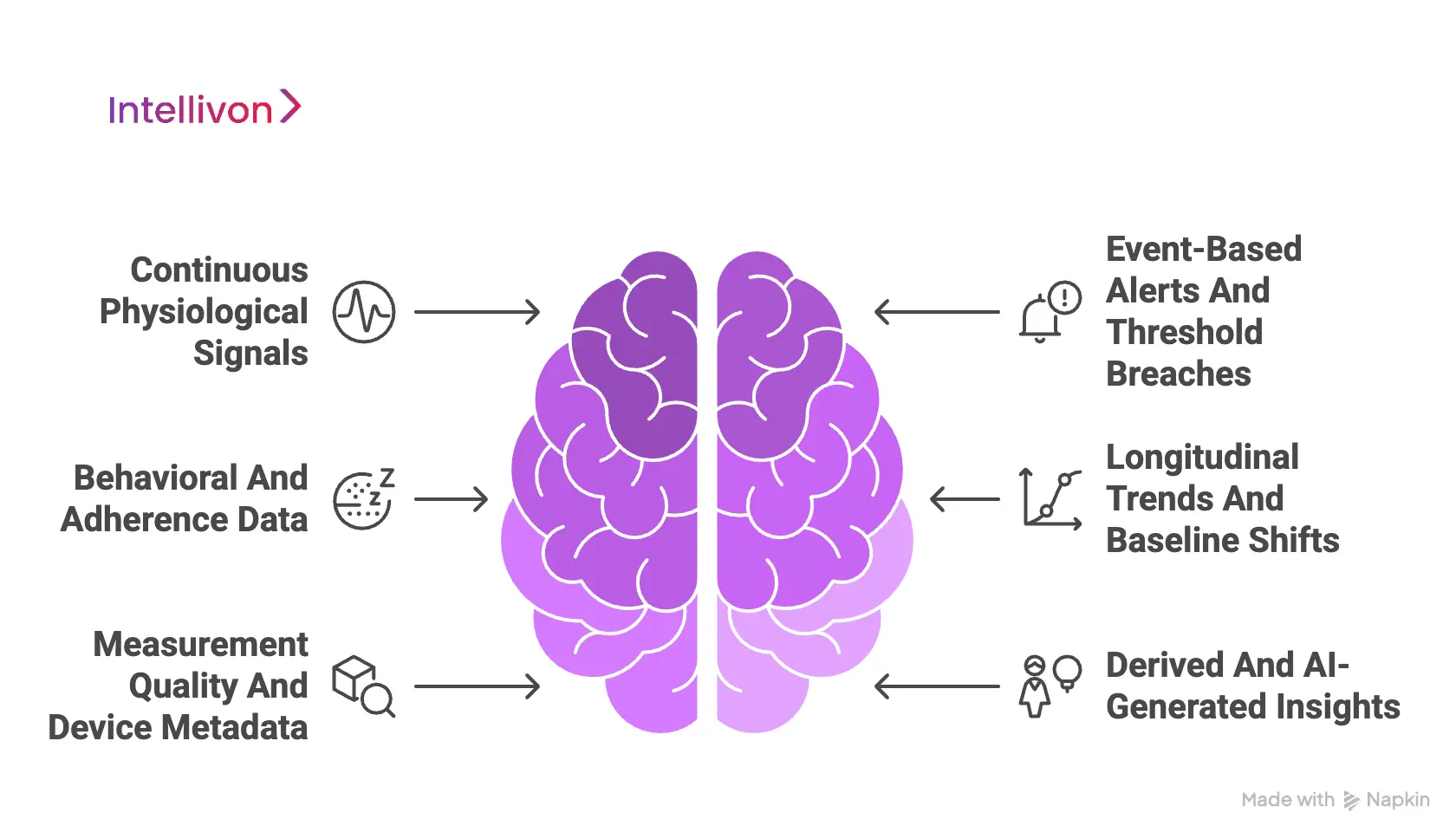
1. Continuous Physiological Signals
Physiological signals such as heart rate, HRV, SpO₂, glucose, respiration, and temperature are generated continuously. These signals form the backbone of remote monitoring and chronic care programs.
At an enterprise level, raw streams must be normalized and contextualized. Without this step, high-frequency data overwhelms telehealth workflows and EHR systems.
2. Event-Based Alerts And Threshold Breaches
Event-based data represents meaningful changes rather than constant measurement. Examples include sustained blood pressure elevation or hypoglycemia events.
Enterprises act on events, not streams. Properly defined triggers allow care teams to respond quickly while limiting unnecessary alerts.
3. Behavioral And Adherence Data
Behavioral data captures activity levels, sleep patterns, and adherence signals over time. This data influences outcomes but rarely requires immediate clinical action.
When routed correctly, it supports care plans and coaching workflows without adding clinical burden.
4. Longitudinal Trends And Baseline Shifts
Trend data highlights gradual changes across days or weeks. A single reading may appear normal, while the pattern signals deterioration.
Healthcare enterprises rely on this data to support preventive care and value-based models. Longitudinal analysis requires systems designed to store and interpret data over time.
5. Measurement Quality And Device Metadata
Not all wearable data is equally reliable. Signal confidence, wear time, and device state affect data accuracy.
Enterprises must account for data quality to reduce false alerts and defend clinical decisions. This layer is critical for risk management and audit readiness.
6. Derived And AI-Generated Insights
Derived insights summarize large data volumes into actionable outputs. These include risk scores, trend summaries, and prioritization flags.
For enterprises, these outputs guide workflows rather than replace clinicians. They must remain explainable and governed within clinical systems.
Wearable integration is not a single technical task. Each data type demands a different handling strategy. Enterprises that classify wearable data correctly can reduce noise, improve decision timing, and scale care delivery safely.
Where Wearable Data Fits Inside Telehealth And EHR Workflows
Wearable data only improves care when it aligns with how clinical work actually happens. Telehealth platforms and EHR systems play distinct roles, and wearable signals must be routed based on those roles. Telehealth supports monitoring, triage, and near-real-time action, while EHRs exist to document decisions and preserve longitudinal records.
Effective integration respects this separation instead of treating both systems as interchangeable endpoints.
1. Telehealth As The Action Layer
Telehealth platforms are the operational layer for wearable data. This is where signals are reviewed, filtered, and translated into actions such as outreach, follow-ups, or escalations. Continuous data feeds are best handled here, where workflows can adapt quickly without disrupting core clinical systems.
By placing wearable data in telehealth first, enterprises maintain responsiveness while controlling clinician workload.
2. EHR As The Record Layer
The EHR is not designed to manage high-frequency data streams. Its role is to store clinically relevant summaries, decisions, and outcomes.
Wearable data should reach the EHR only after it has been interpreted and acted upon. This keeps medical records concise, defensible, and aligned with clinical accountability.
3. Separating Action From Documentation
Routing wearable data through telehealth before EHR entry creates a clean separation between care delivery and documentation. Telehealth workflows drive action, while the EHR captures what was decided and why.
This structure prevents data overload and supports audit readiness. It also allows enterprises to scale wearable programs without compromising clarity.
Wearable integration succeeds when data is placed where it adds the most value. Telehealth systems handle monitoring and response, while EHRs reflect final clinical decisions. Enterprises that respect this division gain efficiency, clarity, and control.
Integration Strategies For Wearables, Telehealth, And EHR Systems
There is no single way to integrate wearable data into healthcare systems. The right strategy depends on scale, care delivery models, and risk exposure. Most failures occur when enterprises adopt an approach that does not align with how care is actually delivered.
Integration strategies should support today’s needs while allowing room to evolve. In practice, organizations rarely stay with one strategy forever.
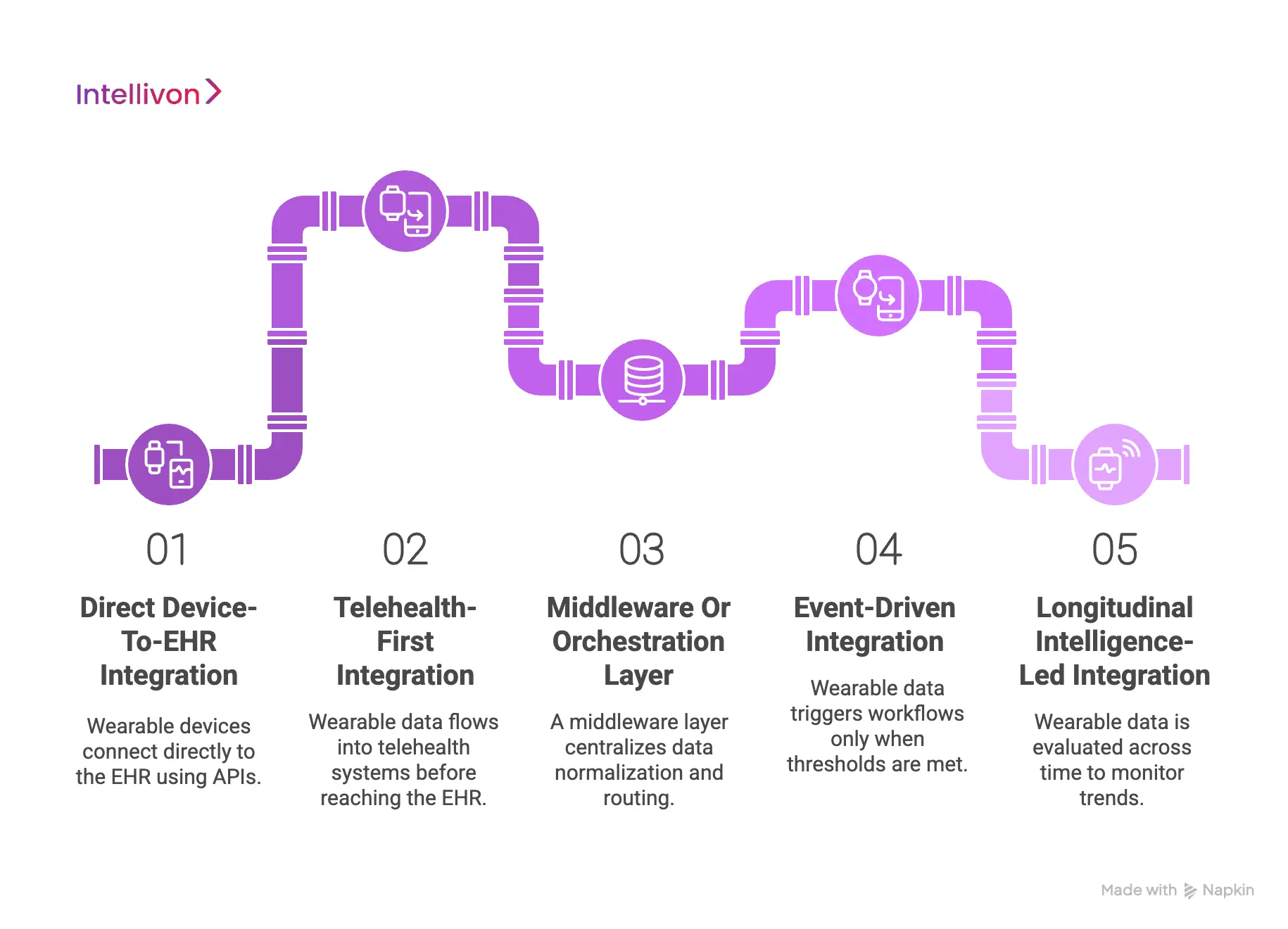
1. Direct Device-To-EHR Integration
This strategy connects wearable devices directly to the EHR using device and EHR APIs. Data flows into the medical record with little to no filtering or workflow logic. It can work for small pilots or low-frequency data use cases.
However, EHRs are not designed to handle continuous data streams. As volume grows, clinicians face information overload and unclear ownership. Most enterprises outgrow this approach once programs scale.
2. Telehealth-First Integration
In a telehealth-first model, wearable data flows into telehealth systems before reaching the EHR. Telehealth workflows handle review, triage, and follow-up actions. This allows care teams to respond in near real time without disrupting core clinical systems.
Only relevant summaries and outcomes are written to the EHR. The approach improves responsiveness while maintaining documentation discipline. It is well-suited for remote monitoring and virtual-first care models.
3. Middleware Or Orchestration Layer
A middleware layer sits between wearable devices, telehealth platforms, and EHRs. It centralizes data normalization, consent enforcement, and routing logic. Devices and clinical systems remain loosely coupled.
This allows enterprises to add or replace devices without redesigning workflows. The model supports multi-device and multi-EHR environments. It is commonly used in enterprise-scale and long-term platform strategies.
4. Event-Driven Integration
Event-driven integration focuses on meaningful changes rather than constant data flow. Wearable data triggers workflows only when thresholds or patterns are met. This prevents clinicians from being overwhelmed by routine readings.
Alerts are routed based on urgency and responsibility. Care teams act on events, not dashboards. This approach improves efficiency while preserving clinical sensitivity.
5. Longitudinal Intelligence-Led Integration
This strategy evaluates wearable data across time instead of in isolation. Systems establish patient-specific baselines and monitor gradual change. Trends matter more than single readings.
This supports chronic care, preventive programs, and value-based models. The approach relies on clean, structured integration upstream. Without proper integration, longitudinal insights lose reliability.
Integration strategy determines whether wearable programs succeed or fail. Simple approaches may work early, but break under growth.
Mature enterprises often combine strategies to balance responsiveness, control, and intelligence. The goal is not technical elegance. It is sustainable, accountable care delivery at scale.
Wearable Device Integration in Healthcare Has Reached 36% From 28% Within 3 Years
Wearable device usage in healthcare has moved beyond early adoption. In just three years, usage among US adults increased from roughly 28–30% in 2019 to over 36% by 2022. This shift reflects more than consumer interest. It signals growing demand to connect wearable data with clinical systems and care delivery workflows.
As wearable adoption rises, healthcare organizations are under pressure to turn patient-generated data into usable clinical inputs. Integration is no longer optional. It is becoming foundational.
1. Wearable Adoption Is Driving Integration Expectations
The increase in wearable usage has changed patient expectations. Many users now assume that the data they collect daily can inform medical decisions.
This expectation pushes healthcare systems to support the ingestion of wearable data into telehealth platforms and EHRs. Without integration, data remains isolated and underutilized.
2. Healthcare Demand Has Shifted From Tracking To Action
Early wearable use focused on self-tracking. Today, healthcare demand centers on action.
Providers are increasingly asked to review trends, respond to alerts, and incorporate wearable insights into care plans. This shift requires systems that can filter, contextualize, and route wearable data into real workflows.
3. Integration Pressure Increased After COVID
Remote and hybrid care models accelerated wearable relevance. During and after the COVID period, continuous monitoring became more valuable than episodic visits.
As a result, healthcare teams now rely on integrated wearable data to support remote patient monitoring, chronic care, and virtual follow-ups. Integration enables continuity when in-person care is limited.
4. Higher Adoption Exposes Gaps
As wearable usage crosses one-third of the adult population, gaps become more visible. Many systems can ingest data, but cannot act on it.
This gap highlights the need for orchestration layers that connect wearable signals to telehealth workflows and EHR documentation, with clear ownership and timing.
The rise from 28% to 36% wearable usage marks a structural shift in healthcare demand. Patients are generating more data and more often.
To keep pace, healthcare platforms must integrate wearables in ways that support clinical action, not just visibility. Integration has become the bridge between growing wearable adoption and effective, accountable care delivery.
How AI Enhances Wearable–Telehealth–EHR Integrations
Wearable data introduces scale and complexity that manual workflows cannot manage. Continuous signals, multiple devices, and varying data quality create noise before value.
AI helps bridge this gap when used correctly. Its role is not to replace clinicians, but to refine data before it enters care workflows and EHR records. When placed thoughtfully, AI improves timing, relevance, and safety across integrated systems.
1. AI As A Signal Filtering Layer
Wearable devices generate high-frequency data that can overwhelm care teams. AI helps filter routine or low-confidence signals before they reach clinicians. This reduces alert fatigue and protects workflow capacity.
Only signals that meet relevance thresholds move forward. As a result, teams focus on meaningful changes rather than constant monitoring. This filtering step is essential for scale.
2. AI For Contextual Interpretation
Raw metrics rarely tell the full story. AI adds context by interpreting signals alongside patient history, conditions, and baselines. It correlates multiple data points instead of relying on single readings.
This reduces false positives and improves clinical relevance. Contextual interpretation ensures that signals align with real care needs. It also supports safer decision-making.
3. AI For Event Prioritization And Routing
Not all events require the same response. AI helps rank urgency based on severity, trend direction, and patient risk. It then routes events to the appropriate role, such as a nurse, care manager, or clinician.
This ensures timely action without unnecessary escalation. Clear routing also reinforces accountability. Decisions happen faster and with less friction.
4. AI Supporting Longitudinal Care Models
Many care models depend on trends, not isolated readings. AI establishes patient-specific baselines and monitors gradual change over time. This supports chronic care, preventive programs, and value-based initiatives.
Early signals of deterioration can be identified before symptoms escalate. Longitudinal analysis requires clean, integrated data. Without proper integration, these insights lose reliability.
5. AI Governance And Clinical Control
AI must operate within clear boundaries. It should support decisions, not make them independently. Clinicians remain responsible for diagnosis and treatment. AI outputs must be explainable and traceable within workflows.
This preserves trust, compliance, and audit readiness. Governance ensures AI strengthens care without increasing risk.
How AI Refines Wearable Signals Before EHR Integration
| Wearable Category | Common Devices (Examples) | Typical EHR Integration Targets | How AI Enhances The Data Before EHR Entry |
| Smartwatches | Apple Watch, Samsung Galaxy Watch, Fitbit, Garmin | Epic, Cerner, Athenahealth | Filters high-frequency HR and activity data, detects rhythm irregularities, summarizes trends, and flags only sustained or clinically relevant changes for review. |
| Smart Rings | Oura Ring, Galaxy Ring | Epic, Cerner | Correlates HRV, temperature deviation, and sleep quality to detect early illness patterns, reduces noise from lifestyle variation, and generates recovery or risk summaries. |
| Cardiac Patches | iRhythm Zio, VitalPatch, BioButton | Epic, Cerner, Meditech | Identifies true arrhythmias, removes motion artifacts, prioritizes abnormal rhythm events, and delivers clinician-ready diagnostic summaries instead of raw waveform data. |
| Continuous Glucose Monitors (CGM) | Dexcom G7, Abbott Libre 3 | Epic, Cerner | Predicts glucose excursions, detects sensor anomalies, highlights time-in-range trends, and surfaces actionable insights for titration or intervention decisions. |
| Home Vital Devices | BP cuffs, weight scales, pulse oximeters | Epic, Athenahealth | Combines readings across devices, detects inconsistent measurements, flags fluid retention or deterioration patterns, and prioritizes outreach lists for care teams. |
| Clinical Sensor Platforms | Masimo Radius PPG, bedside wearables | Epic, Cerner | Monitors continuous SpO₂ and respiration, predicts deterioration risk, reduces false alarms, and supports early escalation in inpatient or step-down settings. |
AI enhances wearable–telehealth–EHR integrations by improving signal quality, timing, and relevance. Its value depends on proper placement and governance. When integrated thoughtfully, AI reduces noise and supports scalable care delivery.
When misused, it adds risk and complexity. Enterprises succeed by treating AI as an enabler, not the centerpiece.
Architecture Needed For Integrating Wearable Devices into Telehealth EHR
Integrating wearable devices into healthcare systems requires more than APIs and data sync. Enterprises need a layered architecture that separates signal capture, intelligence, workflows, and clinical records. Each layer serves a distinct purpose and protects the system from overload, risk, and fragmentation. When these layers are clearly defined, wearable data can scale safely across telehealth and EHR environments.
Below is an eight-layer architecture designed for enterprise-grade wearable integration.
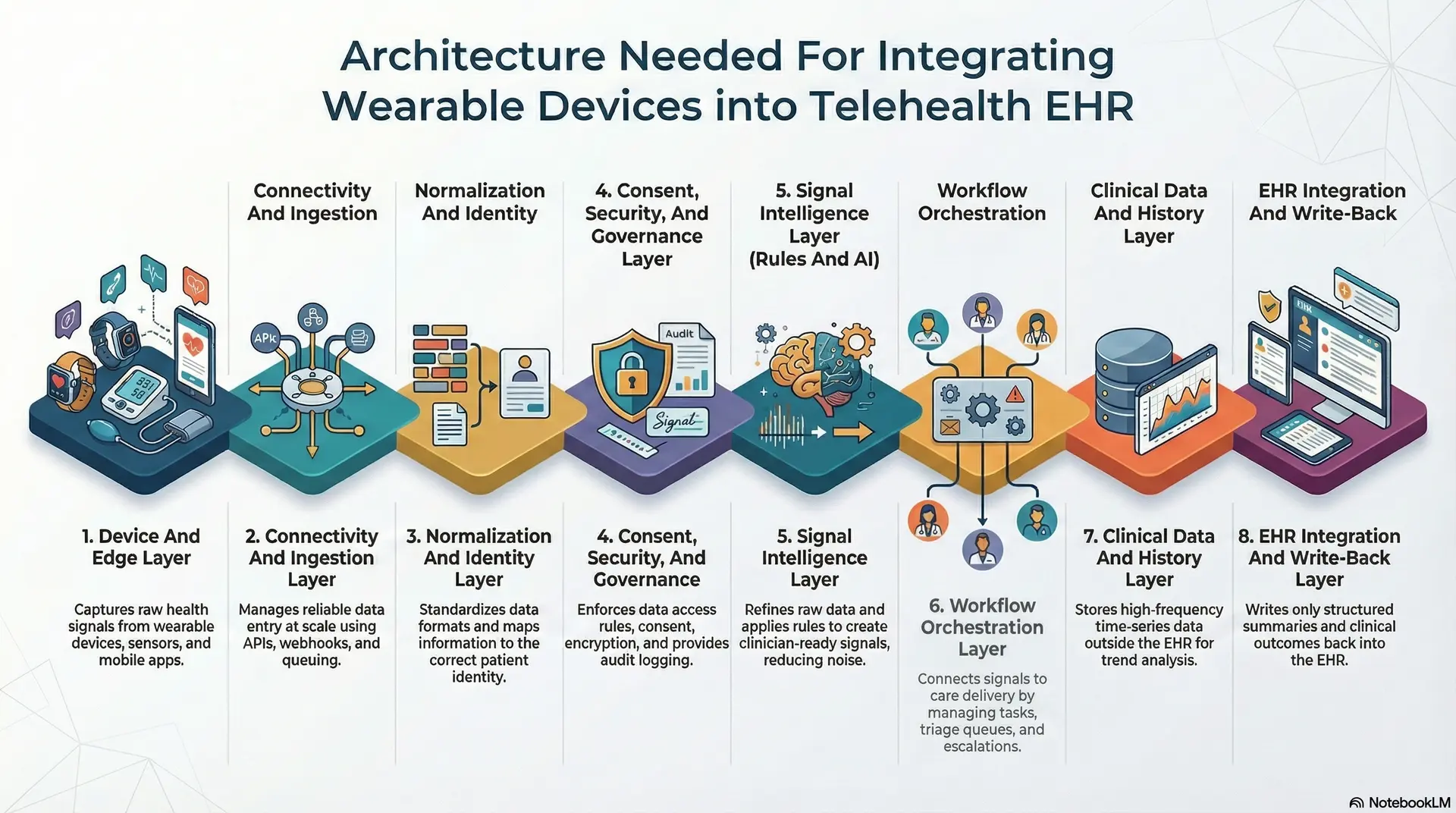
1. Device And Edge Layer
This layer includes wearable devices, sensors, and companion mobile applications. It is where raw health signals are captured and transmitted. Data quality, sampling frequency, and device reliability start here.
Enterprises must account for device variability and intermittent connectivity at this layer. Weak controls here amplify issues downstream.
2. Connectivity And Ingestion Layer
The ingestion layer handles how data enters the platform. It manages APIs, webhooks, retries, rate limits, and queuing. This layer ensures data arrives reliably and at scale.
Without proper ingestion controls, enterprises face data loss, duplication, or system instability. Reliability at this layer is non-negotiable.
3. Normalization And Identity Layer
Wearable data arrives in different formats, units, and timestamps. This layer standardizes data and maps it to the correct patient identity. Accurate patient matching is critical for clinical safety.
Errors here can lead to misattribution and serious risk. This is why enterprises must treat identity resolution as a core architectural concern.
4. Consent, Security, And Governance Layer
This layer enforces who can access data and for what purpose. It manages consent propagation, role-based access, encryption, and audit logging. Governance must be enforced by system logic, not policy documents.
Without this layer, integration quickly becomes a compliance liability. Enterprises rely on it to maintain trust and audit readiness.
5. Signal Intelligence Layer (Rules And AI)
The signal intelligence layer refines raw data before action. It applies thresholds, trend detection, anomaly checks, and quality scoring. AI operates here as a support mechanism, not a decision-maker.
This layer reduces noise and prepares clinician-ready signals. It determines what deserves attention and what does not.
6. Workflow Orchestration Layer
This layer connects signals to care delivery. It manages triage queues, task creation, escalation paths, and clinician attribution. Wearable data becomes actionable only at this stage.
Clear workflows define who acts, when they act, and how outcomes are tracked. This layer is where accountability is established.
7. Clinical Data And History Layer
High-frequency wearable data should not live inside the EHR. This layer stores time-series data and longitudinal history outside core clinical systems. It supports analytics, trend analysis, and population insights.
Enterprises use this layer to preserve context without overloading medical records. It also enables future intelligence safely.
8. EHR Integration And Write-Back Layer
The final layer controls what enters the EHR. Only structured summaries, decisions, and outcomes are written back. Data is mapped to standard clinical objects and documentation workflows.
This keeps the EHR concise, defensible, and audit-ready. The EHR remains the system of record, not the system of streaming data.
Wearable integration succeeds when architecture enforces separation of concerns. Each layer protects the next from unnecessary complexity. Together, they allow enterprises to scale wearable programs without overwhelming clinicians or clinical systems.
Where APIs Fit In The Integration Architecture
APIs enable communication between systems, but they are not the integration strategy by themselves. In wearable healthcare platforms, APIs support each architectural layer with a specific role. When APIs are placed correctly, data flows reliably and safely. When they are overused or misused, integration becomes fragile and hard to govern.
Understanding where APIs belong helps enterprises avoid treating integration as a simple connectivity task.
1. Device And Wearable APIs
Device APIs connect wearables and mobile apps to the platform. They are used to collect raw signals such as heart rate, activity, glucose, or SpO₂. These APIs often operate at high frequency and variable quality.
Enterprises should treat them as signal sources, not clinical interfaces. Data from this layer always requires validation downstream.
2. Ingestion And Data Gateway APIs
Ingestion APIs handle how wearable data enters the system at scale. They manage authentication, retries, rate limits, and message ordering. This layer protects core systems from spikes, failures, and duplication.
Reliable ingestion ensures no data is lost or misattributed. It also creates a stable foundation for downstream processing.
3. Normalization And Identity APIs
Normalization APIs standardize incoming data formats and units. Identity APIs map data to the correct patient record across systems. These APIs are critical for clinical safety and compliance.
Errors here can lead to incorrect attribution or data leakage. Enterprises must prioritize accuracy over speed at this stage.
4. Telehealth And Workflow APIs
Workflow APIs connect refined signals to care delivery actions. They create tasks, trigger reviews, and route alerts to the right care teams. These APIs ensure wearable data results in action, not just visibility.
Clear API contracts define ownership and response expectations. This layer directly supports operational efficiency.
5. EHR Integration APIs
EHR APIs control what information is written into the medical record. They are used to store summaries, trends, and clinical decisions. Raw wearable streams should not pass through these APIs.
Proper use keeps EHRs concise, defensible, and audit-ready. This protects both clinicians and enterprises.
APIs are essential, but they are only as effective as the architecture around them. Each API layer serves a distinct purpose within the integration stack. Enterprises succeed when APIs are used to support governance, workflows, and accountability. Integration fails when APIs are treated as the solution instead of the enabler.
How We Approach Wearable–EHR–Telehealth Integration
Enterprises do not need another device sync or data feed. They need a repeatable way to convert wearable signals into accountable care actions and audit-ready records. Our approach is workflow-first, compliance-enforced, and built to scale across devices, telehealth programs, and EHR environments.
Below is the step-by-step process we follow.

Step 1: Define The Care Model
We start by mapping the care model that the integration must support. This includes RPM, chronic care, post-discharge follow-ups, or virtual-first programs. We then define ownership for each signal type and escalation path.
This clarifies who reviews, who acts, and what timelines apply. Clear ownership prevents data from becoming “seen but unmanaged.”
Step 2: Identify Signals That Matter
Next, we classify wearable data into streams, events, and summaries. We separate urgent clinical signals from coaching and behavioral signals.
This reduces noise before it reaches care teams. It also protects EHR documentation from unnecessary volume. Signal classification shapes every downstream decision.
Step 3: Design The Integration Architecture
We then design a layered architecture that matches your operating model. Wearable data enters through a controlled ingestion layer and passes through normalization and identity mapping.
Governance controls are enforced at each step. This ensures data arrives securely and is attributed correctly. It also keeps systems stable as volumes grow.
Step 4: Add Rules And AI
Our experts apply rules and AI where they add real operational value. This includes quality checks, trend detection, anomaly flags, and event prioritization. The goal is to turn continuous data into clinician-ready signals.
AI supports decision-making but never replaces clinical ownership. Every output remains explainable and traceable.
Step 5: Orchestrate Telehealth Actions
We connect refined signals to telehealth workflows that drive action. This includes triage queues, task assignment, follow-ups, and escalation to clinicians.
At the same time, we also capture outcomes and response timing. This step is where integration becomes care delivery. It ensures signals lead to consistent actions.
Step 6: Write Back Only What Belongs In The EHR
Finally, we define what the EHR should store and what it should not. We write back structured summaries, decisions, and outcomes.
We avoid pushing raw wearable streams into the medical record. This keeps documentation clean and audit-ready. It also preserves clinical clarity for providers.
At Intellivon, our experts approach wearable integration as an operating layer, not a connectivity task. Each step is designed to reduce noise, strengthen accountability, and protect clinical systems. This allows enterprises to scale wearable programs without compromising safety or workflow efficiency. The result is a durable integration that supports real care delivery.
How We Solve Common Wearable-EHR-Telehealth Integration Mistakes
Many wearable integration initiatives fail for the same reasons. The technology works, but the system around it does not. Data moves, yet care delivery does not improve. We see these patterns repeatedly across enterprise healthcare programs.
Below are the most common integration mistakes and how we address them in practice.
1. Treating Integration As An API Task
Many teams focus on connecting devices to systems through APIs and stop there. Data flows into dashboards or EHR fields without clear workflows or ownership. This creates visibility without action.
How we solve it:
We design integration around care workflows first. APIs support ingestion and routing, but actions, escalation paths, and documentation rules are defined upfront. Data only moves when it has a clear purpose.
2. Streaming Raw Wearable Data Into The EHR
EHRs are often used as data sinks for high-frequency wearable streams. This overwhelms clinicians and clutters the medical record.
How we solve it:
We separate operational data from clinical records. Telehealth workflows handle streams and events, while the EHR receives structured summaries and decisions only. This keeps records concise and defensible.
3. Lacking Clear Clinical Ownership
Wearable alerts are generated, but responsibility is unclear. Signals are seen but not acted on consistently.
How we solve it:
We define ownership at the signal level. Every alert has a responsible role, response window, and escalation rule. Accountability is enforced through workflows, not assumptions.
4. Ignoring Data Quality And Device Context
Not all wearable data is reliable. Poor signal quality and device misuse lead to false alerts and wasted effort.
How we solve it:
Our experts incorporate quality checks and device context into the signal layer. Low-confidence data is filtered early. Care teams see only signals that meet reliability thresholds.
5. Applying AI Without Governance
AI is added without clear boundaries. Outputs are hard to explain and difficult to trust.
How we solve it:
At Intellivon, we use AI to refine signals, not replace decisions. Every insight is explainable, traceable, and routed through governed workflows. Clinicians remain decision owners.
Wearable integration fails when it is treated as a technical shortcut. It succeeds when it is designed as a care operating layer. Our approach addresses the root causes that derail most programs. This allows enterprises to scale wearable, telehealth, and EHR integrations with control, clarity, and confidence.
Conclusion
Wearable devices are generating more health data than ever before. However, data volume alone does not improve care delivery. Value emerges only when signals are integrated into telehealth workflows, refined through governance and intelligence, and recorded responsibly within EHR systems. Enterprises that treat integration as a workflow and accountability challenge gain clarity, efficiency, and scale.
As wearable adoption continues to grow, integration can no longer remain an afterthought. Platforms must be designed to manage timing, ownership, and clinical relevance from the start. When wearable data moves through the right architecture, organizations can deliver modern care models without overwhelming clinicians or compromising compliance.
What Intellivon Can Do For You
At Intellivon, we build wearable-integrated telehealth platforms as enterprise operating systems, not device connectors or data aggregation layers. Our platforms are designed to govern how wearable signals are ingested, how insights flow into clinical decision-making, and how accountability and compliance are preserved as care scales across programs and populations.
Each solution is engineered for healthcare organizations operating at scale. Platforms are architecture-first and compliance-led, with wearable workflows embedded across telehealth operations, EHR documentation, identity controls, data governance, and audit layers. As programs expand across devices, care models, and regions, clinical oversight, data integrity, and operational predictability remain intact.
Why Partner With Intellivon?
- Enterprise-grade platform architecture aligned with wearable-driven remote, chronic, and hybrid care models
- Deep interoperability expertise across EHRs, wearable ecosystems, telehealth platforms, identity frameworks, and analytics infrastructure
- Compliance-by-design delivery supporting HIPAA, GDPR, clinical accountability, consent enforcement, and audit readiness
- AI-assisted orchestration that refines wearable signals into actionable workflows without removing clinician control
- Proven enterprise delivery model with phased rollout, workflow validation, and long-term platform scalability
Talk to Intellivon’s healthcare experts to explore how a wearable-integrated telehealth platform can fit into your existing ecosystem, reduce operational friction, and deliver accountable, scalable care powered by real-world health data.
FAQs
Q1. How is wearable data integrated into telehealth and EHR systems?
A1. Wearable data is first ingested through secure APIs and normalized for accuracy. It is then routed into telehealth workflows for review and action. Only clinically relevant summaries and decisions are written back to the EHR. This approach prevents data overload and preserves clinical accountability.
Q2. Should wearable data be stored directly in the EHR?
A2. No, raw wearable data should not be stored directly in the EHR. EHRs are designed for documentation, not high-frequency data streams. Wearable signals should be processed and summarized before EHR entry. This keeps medical records concise, defensible, and audit-ready.
Q3. What role does AI play in wearable EHR integration?
A3. AI helps refine wearable data before it reaches clinicians or EHR systems. It filters noise, detects trends, and prioritizes events that require action. AI supports decision-making but does not replace clinicians. All outputs remain governed and explainable.
Q4. What are the biggest challenges in integrating wearables with healthcare systems?
A4. Common challenges include data overload, unclear clinical ownership, poor data quality, and lack of workflow alignment. Many integrations focus only on APIs and ignore care delivery processes. These gaps limit clinical value and increase operational risk.
Q5. How do enterprises ensure compliance when integrating wearable data?
A5. Compliance is enforced through architecture, not policy alone. This includes consent management, role-based access, audit logs, and controlled EHR write-back. Wearable data must move through governed workflows with clear accountability. This approach supports HIPAA, GDPR, and clinical audit requirements.





