Most healthcare organizations do not struggle due to poor clinical decisions. They face challenges because care often breaks down between those decisions, where transitions are missed, follow-ups fall through the cracks, and responsibility spreads across teams and systems. Over time, these issues lead to readmissions, delayed interventions, frustrated clinicians, and higher operational costs.
A care coordination software platform addresses this specific failure point. It operates above core clinical systems and connects people, data, and workflows into a single working layer. When designed for large-scale operations, it provides visibility into care transitions, automates routine handoffs, identifies at-risk patients before issues worsen, and ensures that accountability does not fade between departments. The result is fewer readmissions, quicker discharge planning, improved clinician satisfaction, and clear ROI on value-based care contracts.
At Intellivon, we have spent over a decade creating enterprise healthcare platforms where interoperability, automation, and AI-driven intelligence work alongside clinical realities and regulatory demands. This blog is an extension of our experience and explains how we build care coordination software platforms from scratch.
Key Takeaways of the Care Coordination Software Market
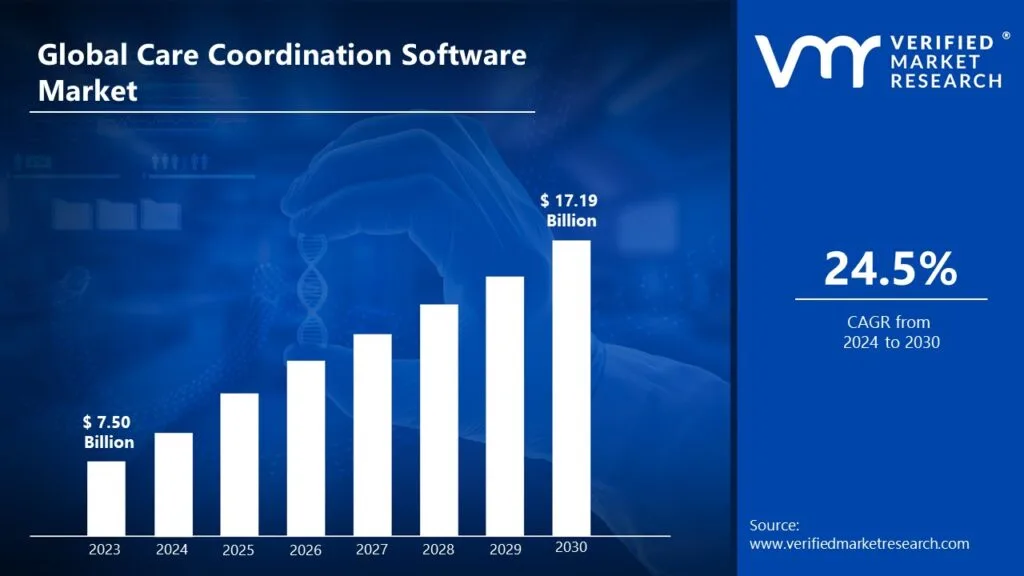
Valued at roughly USD 7.5 billion in 2023, the care coordination software market is on a strong upward curve. By 2030, it is forecasted to reach close to USD 17.2 billion, driven by a projected CAGR of 24.5% between 2024 and 2030.
Key Growth Drivers and Market Trends
Structural and Policy Drivers
- The rising burden of chronic diseases such as diabetes, heart failure, COPD, and multimorbidity is driving demand for longitudinal, coordinated care rather than episodic interventions.
- Value-based and risk-sharing care models now tie roughly 10–50% or more of provider and payer revenue to outcomes, readmissions, and total cost of care, making structured care coordination a financial necessity.
- Regulatory frameworks and payer mandates increasingly emphasize integrated, patient-centric care delivery, accelerating the adoption of dedicated care coordination and care management platforms.
Technology and Deployment Trends
- Cloud-based and SaaS deployments represent nearly two-thirds of care coordination and care management implementations, accounting for approximately 67.7% of the market in 2024.
- Cloud solutions are projected to grow at over 15% CAGR as enterprises prioritize scalability, remote access, and subscription-based operating models over capital-intensive on-premise systems.
- Demand for cloud-native platforms continues to dominate due to lower upfront costs, easier integration with telehealth and remote care, and faster enterprise rollout timelines.
- AI, machine learning, and advanced analytics are increasingly embedded to power risk stratification, proactive outreach, and real-time care alerts, strengthening the ROI case for coordinated care platforms.
Adoption Patterns and Enterprise Focus
- Care coordination has become a foundational capability within population health and care management programs for hospitals, integrated delivery networks, payers, and ACOs.
- Software platforms anchor an estimated 72% of the care management solutions segment in 2024, reflecting a strong enterprise preference for configurable, interoperable digital systems.
- Within the broader care management systems market, software holds roughly a 56.4% share, driven by the need to unify engagement, coordination, outcomes tracking, and compliance reporting.
Fastest-Growing Care Settings
- Care coordination platforms are widely deployed across hospitals, outpatient clinics, and post-acute environments, with home and community-based care emerging as one of the fastest-growing segments.
- Growth in home-based coordination is closely linked to remote patient monitoring, virtual care models, and the expansion of chronic care outside traditional facility walls.
- Population health management platforms with embedded care coordination are increasingly used to aggregate data, identify at-risk cohorts, and orchestrate interventions across large care networks.
Taken together, these trends show that care coordination software is becoming a core enterprise capability. Growth is being driven not only by technology advancement but by structural shifts in healthcare economics, regulatory expectations, and care delivery models.
What Is a Care Coordination Software Platform?
A care coordination software platform is an enterprise system designed to organize, track, and manage care activities across teams, settings, and time. It connects clinicians, care managers, and support staff around a shared care plan, ensuring that responsibilities, transitions, and follow-ups are clearly owned and executed.
Unlike EHRs, which document clinical events, care coordination platforms govern what happens next. They unify workflows, surface risks early, and maintain continuity across hospitals, outpatient clinics, post-acute providers, and home-based care to prevent patients from falling through operational gaps.
How They Work
Care coordination platforms follow a clear, repeatable workflow. They connect fragmented systems, surface the right insights, and guide teams through timely actions.
Step 1: Ingest and Normalize Multi-Source Data
The platform pulls data from EHRs, claims, labs, RPM devices, and CRMs. It standardizes formats, maps patient identities, and resolves duplicates to create a single, longitudinal patient record.
Step 2: Stratify Patients and Segment Cohorts
Risk models and rule engines score patients for readmission risk, disease progression, and care gaps. The platform segments cohorts, such as high-risk heart failure or uncontrolled diabetes, for targeted interventions.
Step 3: Generate Evidence-Based Care Plans
Templates, guidelines, and embedded clinical content support plan creation. Care teams configure goals, tasks, and timelines for each patient, aligned with pathways and contracts.
Step 4: Orchestrate Multidisciplinary Workflows
The system routes tasks to nurses, physicians, social workers, and call-center teams. Each role sees a clean work queue with priorities, due dates, and context.
Step 5: Engage Patients Across Channels
Patients receive reminders, education, and check-ins through SMS, apps, phone, or portals. The platform logs every interaction, updates adherence status, and flags non-responsive patients.
Step 6: Monitor Signals and Trigger Alerts
The platform watches vitals, utilization events, and self-reported symptoms in near real time. It triggers alerts for deterioration, missed follow-ups, or emerging care gaps.
Step 7: Measure Outcomes and Feed Back Insights
Quality, utilization, and cost metrics roll into dashboards at program and contract levels. Leaders track impact against value-based metrics and refine pathways based on real performance.
In practice, these steps run continuously in the background.
The platform stitches them into one loop, so care teams focus less on chasing information and more on coordinated action.
Key Use Cases of Care Coordination Software in Enterprise Healthcare
Care coordination platforms deliver value only when they solve real operational problems. At the enterprise level, these problems surface across care transitions, chronic care programs, risk contracts, and virtual delivery models.
Below are the most critical use cases where coordination platforms create a measurable impact.
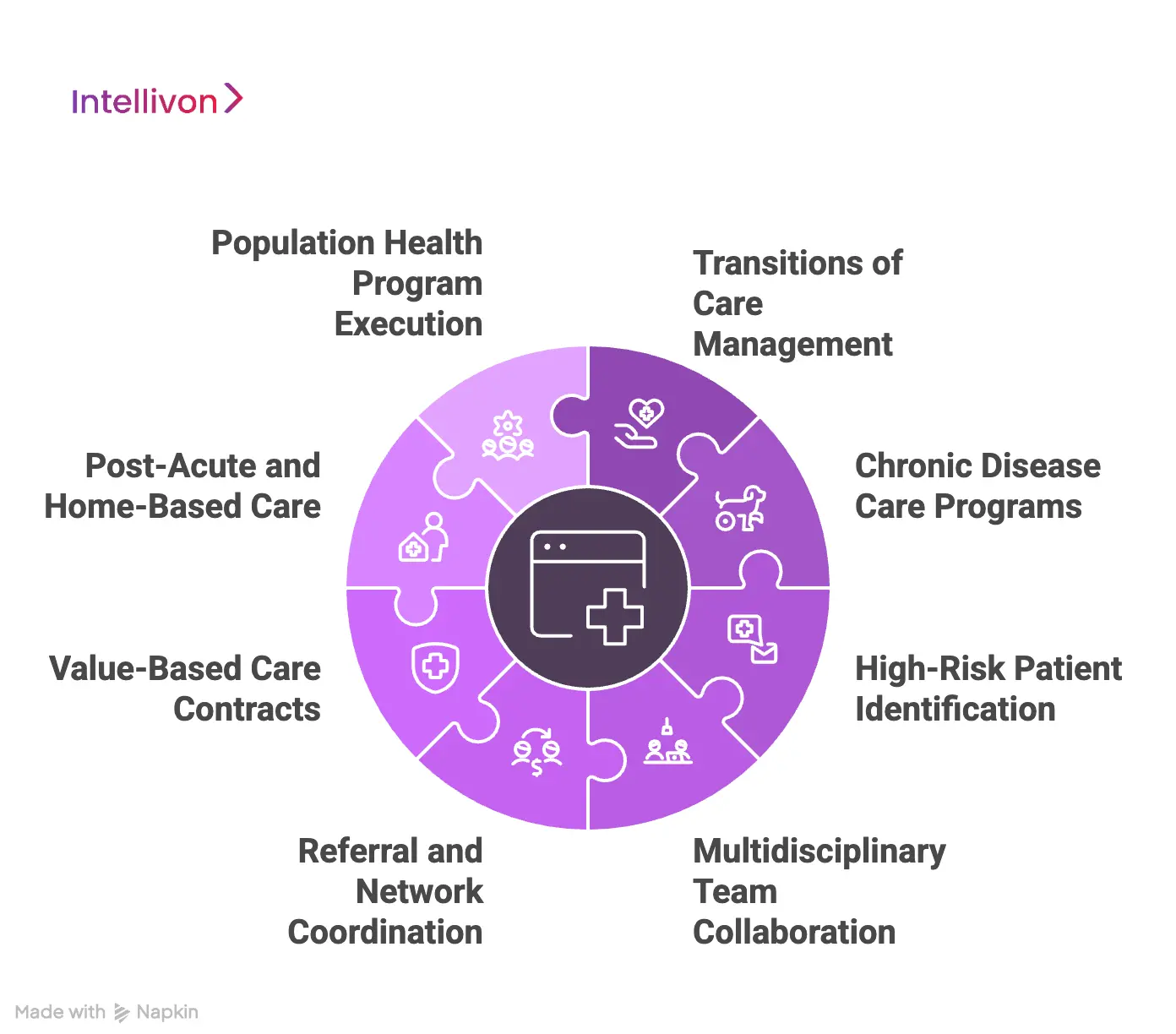
1. Transitions of Care Management
Transitions from hospital to home, rehab, or post-acute care remain one of the highest risk points in healthcare delivery. Discharge instructions often fragment across teams, and follow-ups rely on manual tracking.
Care coordination platforms standardize discharge workflows by assigning ownership for follow-ups, medication reconciliation, and post-discharge outreach. This reduces missed appointments, improves continuity, and lowers avoidable readmissions across large patient volumes.
2. Chronic Disease Care Programs
Patients with diabetes, heart failure, COPD, and multimorbidity require long-term, coordinated management rather than episodic visits.
These platforms support longitudinal care plans, ongoing monitoring, and proactive outreach. Teams can track adherence, intervene early when risks rise, and adjust care plans over time. This approach improves outcomes while preventing reactive, high-cost utilization.
3. High-Risk Patient Identification
Enterprises managing large populations need to identify which patients need attention now. Care coordination platforms use rules and analytics to flag rising risk based on clinical events, utilization patterns, or engagement gaps.
These signals guide care managers toward targeted interventions rather than broad, inefficient outreach. The result is better use of limited care management capacity.
4. Multidisciplinary Team Collaboration
Modern care delivery involves physicians, nurses, care coordinators, pharmacists, and social workers working across different systems. Without coordination, tasks overlap or fall through the gaps.
These platforms centralize task management and role-based workflows, ensuring each team member understands responsibilities and timelines. This improves accountability while reducing communication friction.
5. Referral and Network Coordination
Referrals often break when information does not flow between providers. Care coordination platforms track referrals end-to-end, from initiation through appointment completion.
They ensure supporting documents follow the patient and alert teams when delays occur. This protects network integrity, reduces leakage, and improves patient experience within enterprise care networks.
6. Value-Based Care Contracts
Under shared savings and downside risk models, enterprises must track outcomes across months or years. The software provides longitudinal visibility into utilization, quality measures, and intervention effectiveness.
They support documentation, reporting, and continuous optimization of care programs tied to financial performance.
7. Post-Acute And Home-Based Care
As care shifts into the home, coordination becomes harder. Care coordination platforms connect home health teams, remote monitoring data, and virtual care workflows into the broader care plan.
They ensure patients discharged from facilities remain supported and visible, preventing deterioration outside traditional care settings.
8. Population Health Program Execution
Population health initiatives require identifying cohorts, enrolling patients, and tracking outcomes at scale. Care coordination platforms operationalize these programs by linking data, workflows, and reporting.
Teams can align outreach strategies with risk profiles and monitor performance across entire populations instead of isolated programs.
Across these use cases, the platforms turn fragmented activities into structured, repeatable processes.
Care Coordination Platforms Reduced Readmissions by 17%
Reducing readmissions is not a documentation problem. It is a coordination problem. Patients leave the hospital with instructions, medications, and follow-ups that span multiple teams and systems.
A large 2025 JAMA Network Open meta-analysis brings clarity here. Across 116 randomized trials covering more than 204,000 patients, EHR-connected coordination interventions reduced 30-day all-cause readmissions by 17% and 90-day readmissions by 28% compared to usual care.
Why Readmissions Persist Despite Modern EHRs
Most enterprises already run advanced EHR environments. Yet readmissions remain stubbornly high.
That is because EHRs record what happened. They do not ensure what should happen next. Discharge summaries, follow-up appointments, medication changes, and home care instructions often live in separate workflows with limited accountability.
Care coordination platforms fill this gap by acting as an operational layer. They track ownership, timing, and execution of post-discharge steps across teams and settings, not just inside hospital walls.
Types of Interventions That Drove the 17% Reduction
The meta-analysis highlights a consistent pattern across high-performing programs.
Readmission reductions were largest when enterprises combined multiple coordination capabilities instead of relying on a single tool.
These included:
- Telemonitoring to detect post-discharge deterioration early
- Structured care management programs with defined follow-up ownership
- Discharge alerts routed to care teams outside the hospital
- Medication reconciliation workflows that closed gaps between inpatient and outpatient care
Each element reinforced the others. Platforms that unified these workflows delivered stronger, more sustained outcomes than point solutions operating in isolation.
How Care Coordination Platforms Enable These Outcomes
At enterprise scale, success depends on repeatability. Manual processes do not hold when patient volume grows.
A well-designed care coordination platform centralizes post-discharge workflows into a single system of record for action. Tasks are assigned, monitored, and escalated when timelines slip. Care teams see the same patient context, regardless of location or system.
Most importantly, coordination happens longitudinally. The platform tracks the patient beyond 30 days, which explains the even stronger 90-day readmission reduction seen in the data.
What This Means for Enterprise Leaders
A 17% reduction in 30-day readmissions is not a marginal gain. For large systems, it translates into:
- Fewer penalty exposures
- Lower utilization pressure
- Improved capacity planning
- Better performance under value-based contracts
The data also sends a clear message. Readmission improvement comes from orchestration, not documentation upgrades. Enterprises that treat care coordination as a core operational capability outperform those that rely on disconnected workflows.
Core Features of an Enterprise-Grade Care Coordination Platform
An enterprise-grade care coordination platform combines longitudinal care management, workflow orchestration, interoperability, patient engagement, analytics, and compliance controls to support coordinated care at scale.
Enterprise care coordination platforms are built to manage complexity across teams, systems, and settings. They operate as foundational infrastructure that aligns clinical activity with operational accountability while supporting regulatory and financial performance.
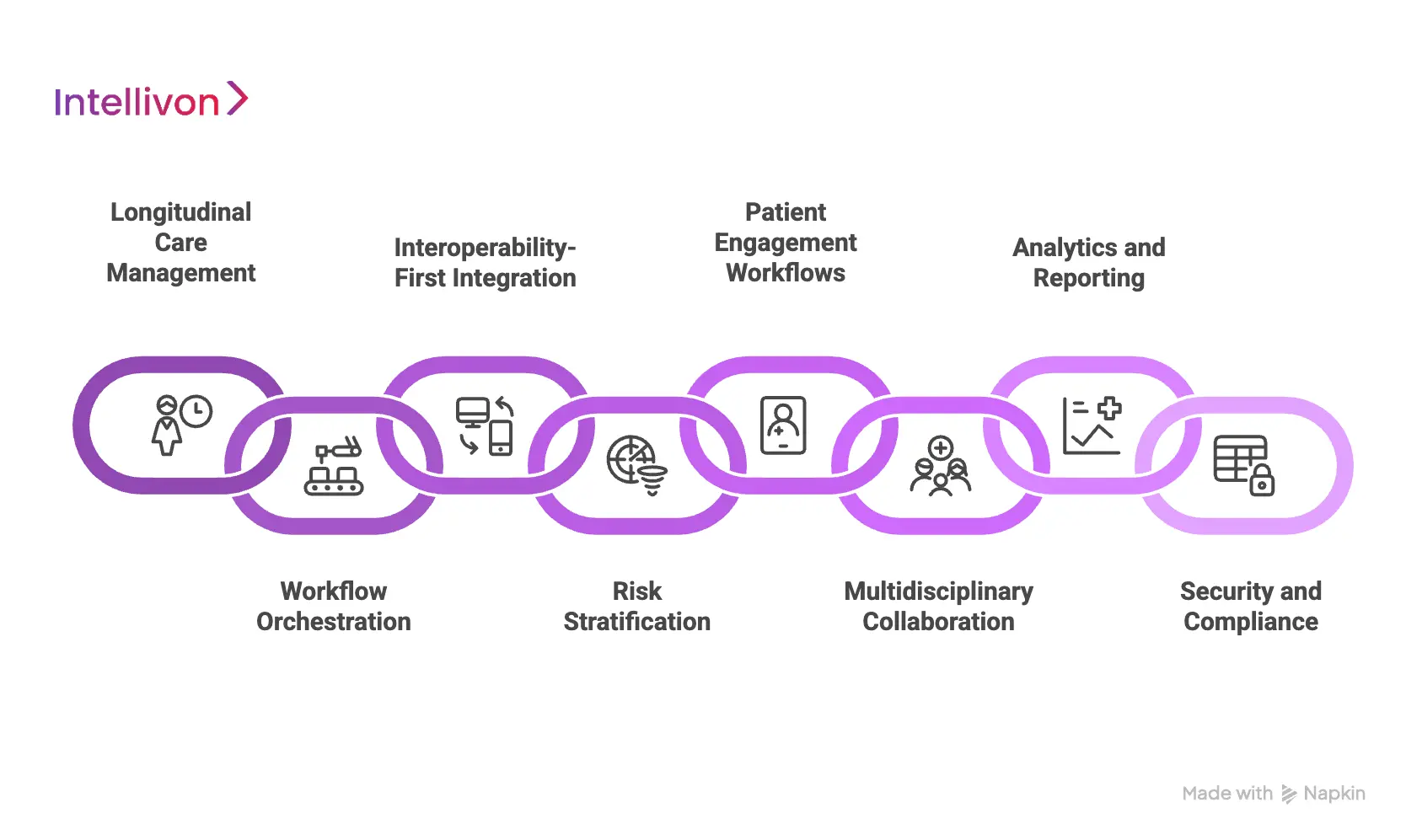
1. Longitudinal Care Management
The platform maintains a continuous care record across encounters, programs, and settings.
Care plans, tasks, and outcomes remain connected over time, allowing teams to manage patients longitudinally rather than resetting context at each visit. This continuity is critical for chronic conditions, post-acute care, and value-based programs.
2. Workflow Orchestration
Enterprise platforms translate care pathways into executable workflows. Tasks are routed to the right roles with clear ownership, deadlines, and escalation rules.
This replaces manual tracking and informal handoffs with structured, repeatable processes that scale across facilities.
3. Interoperability-First Integration
Care coordination relies on seamless data exchange. Platforms integrate with EHRs, labs, claims systems, telehealth tools, and remote monitoring without disrupting live operations.
Standards-based APIs support bidirectional data flow so teams always work from current information.
4. Risk Stratification
Rules engines and analytics continuously evaluate patient data to identify rising risk and missed care opportunities.
Instead of broad alerts, teams receive prioritized signals that guide timely intervention. This allows limited care management capacity to be used effectively.
5. Patient Engagement Workflows
Coordinated outreach is central to continuity. Platforms support communication across calls, messages, portals, and apps while tracking preferences, consent, and responses.
Engagement data feeds back into care plans, closing the loop between outreach and outcomes.
6. Multidisciplinary Collaboration
Complex care requires multiple roles. Platforms support role-based access, shared task views, and secure communication within a unified patient context.
This alignment reduces miscommunication and reinforces accountability across teams.
7. Analytics And Reporting
Operational and clinical dashboards provide visibility into readmissions, utilization, adherence, and quality performance.
Leaders can monitor program impact, identify bottlenecks, and adjust strategy based on real data rather than assumptions.
8. Security and compliance
Enterprise platforms embed security and governance from the start. Role-based access, audit trails, and consent management support regulatory requirements while enabling controlled data sharing across the care ecosystem.
Together, these features define a platform built for real enterprise demands. Care coordination shifts from an operational burden to a strategic capability that supports scale, accountability, and measurable outcomes.
Architecture of a Care Coordination Software Platform
An enterprise care coordination platform uses layered architecture, which includes data integration, longitudinal records, workflow engines, engagement tools, analytics, and compliance controls to orchestrate multi-team care across hospitals, clinics, and home settings.
A strong architecture is what separates a point solution from an enterprise platform. It decides how easily you integrate new programs, scale to new regions, and add AI without breaking compliance. Below is a practical view of how a real care coordination platform should be structured if you want it to work across complex health systems.
1. Data Integration Layer
The first layer pulls information from EHRs, claims platforms, lab systems, RPM devices, and telehealth tools. It normalizes these feeds using standards such as FHIR, HL7, X12, and sometimes custom APIs, where legacy systems demand it.
Incoming data is cleaned, mapped, and de-duplicated so teams do not chase conflicting records. Event streams, like new discharges or abnormal vitals, are published into queues to trigger coordination workflows in near real time.
When this layer is engineered well, your coordinators see a single, stable view of the patient journey instead of toggling through multiple systems.
2. Longitudinal Patient Record
Above integration, the platform maintains a longitudinal care record. This record aggregates encounters, problems, medications, social factors, risk scores, and communication logs into one timeline.
Care teams can see what happened in the hospital, clinic, pharmacy, and home in a single view. For population programs, cohorts can be formed based on conditions, utilization, risk level, or gaps in care.
This becomes the backbone for every outreach, task, and intervention decision. Without it, coordination remains manual and fragmented.
3. Workflow and Rules Engine
The workflow engine translates care pathways and contracts into practical tasks. It assigns responsibilities, sets due dates, and defines escalation paths when activities are delayed or skipped.
Rules can fire when there is a discharge, a high ED utilization pattern, or a missed appointment. Each rule generates a task list that aligns the work of nurses, social workers, pharmacists, and call center staff.
Over time, these workflows are tuned based on results, allowing your programs to move from ad-hoc coordination to repeatable, measurable processes.
4. Communication and Engagement Hub
This layer manages communication across patients, caregivers, and clinical teams. It supports outbound calls, secure messaging, email, SMS, and patient portal engagement from one place.
Scripts, education content, and care plans can be embedded in the outreach workflow. All touchpoints are logged back into the longitudinal record, so no one calls a patient blind.
When designed well, this hub reduces duplication, prevents conflicting messages, and gives leaders a clear view of contact effectiveness.
5. Analytics and AI Layer
Analytics and AI sit across the platform rather than in a separate silo. Predictive models score patients for readmission risk, care gaps, medication non-adherence, or rising-risk patterns.
The platform surfaces these insights directly into worklists so coordinators do not need to read reports in a different system. AI models can also prioritize which tasks matter most today based on risk and regulatory commitments.
This layer turns raw data into action, helping teams focus on interventions that move financial and clinical metrics instead of spreading effort thinly.
6. Security, Privacy, and Compliance Layer
Security and compliance must be baked into every layer, not added at the end. Role-based access ensures each user sees only what they need for their role.
All data in transit and at rest remains encrypted. Detailed audit trails capture who accessed what, when, and why. The architecture supports HIPAA, GDPR, where relevant, and local data residency rules for different regions.
For enterprise leaders, this layer is what makes regulators comfortable and boards confident to scale programs across larger populations.
7. Platform and Deployment Layer
Finally, the deployment layer supports cloud-native, containerized, and often microservices-based components. This enables independent scaling of analytics, messaging, and workflow services as program volumes grow.
Multi-tenant or logically separated environments can be created for different hospitals, regions, or strategic partners on the same core platform. APIs allow new apps, AI tools, and partner services to plug in without major rewrites.
This layer makes the platform sustainable. It ensures that adding a new line of business, payer contract, or care model is an incremental change, not a multi-year rebuild.
In combination, these layers define whether your care coordination initiative becomes a scalable enterprise capability or remains a patchwork of tools and spreadsheets. A well-architected platform gives you the foundation to layer new AI models, programs, and partnerships without destabilizing operations.
How AI Enhances Care Coordination at Scale
AI strengthens care coordination platforms by prioritizing risk, predicting care gaps, automating outreach, and guiding teams toward timely interventions across large patient populations.
AI helps coordination platforms decide what matters now, who needs action, and where intervention will change outcomes.
1. Risk Stratification and Prioritization
AI models continuously analyze clinical events, utilization patterns, vitals, and engagement history to identify patients whose risk is rising. Instead of static risk scores, prioritization adjusts in near real time.
Care teams see who needs attention today, not who needed it last month. This prevents limited care management resources from being spread too thin.
2. Early Detection of Care Gaps
AI identifies patterns humans often miss. Missed follow-ups, overdue labs, medication lapses, or declining engagement trends surface before outcomes deteriorate.
By flagging these gaps early, coordination platforms shift care from reactive to preventive. Small interventions happen sooner, reducing downstream cost and complexity.
3. Intelligent Task Routing
At scale, routing work manually becomes inefficient. AI-driven logic assigns tasks based on urgency, patient context, workload balance, and role capability.
High-risk cases escalate automatically, while lower-risk follow-ups remain streamlined. This ensures the right team acts at the right moment without constant manual triage.
4. Personalized Patient Engagement
AI tailors outreach based on response history, language preferences, and behavior patterns. Some patients respond to messages. Others need calls or caregiver involvement.
AI-driven personalization improves engagement rates while reducing repeated, ineffective outreach that frustrates patients and staff.
5. Predictive Impact Modeling
AI helps enterprises understand which interventions actually move outcomes. By analyzing historical coordination data, platforms learn which actions reduce readmissions, improve adherence, or close care gaps for specific populations.
Leaders can refine programs based on evidence, not assumptions.
6. Human-in-the-Loop Governance
Enterprise-grade AI does not replace clinical judgment. It supports it. Care coordination platforms embed review checkpoints where clinicians validate recommendations, override actions, and provide feedback.
This keeps AI transparent, auditable, and aligned with regulatory expectations.
7. Continuous Learning at Scale
As programs grow, AI models improve. Each interaction, outcome, and override feeds back into model refinement. Over time, coordination becomes smarter across the system, not just for individual patients or pilots.
At scale, AI turns coordination from an exercise in effort into an exercise in focus. It helps healthcare enterprises deliver timely, consistent care across thousands of patients without overwhelming teams or sacrificing accountability.
How We Build Enterprise-Grade Care Coordination Platforms
Intellivon follows an eight-step lifecycle, from discovery and architecture to integration, AI enablement, compliance, rollout, and optimisation, to build scalable, secure care coordination platforms for large healthcare enterprises.
Below is how we typically build enterprise-grade care coordination platforms for hospitals, IDNs, payers, ACOs, and population health programs. You should be able to see your organisation’s reality reflected in each step.
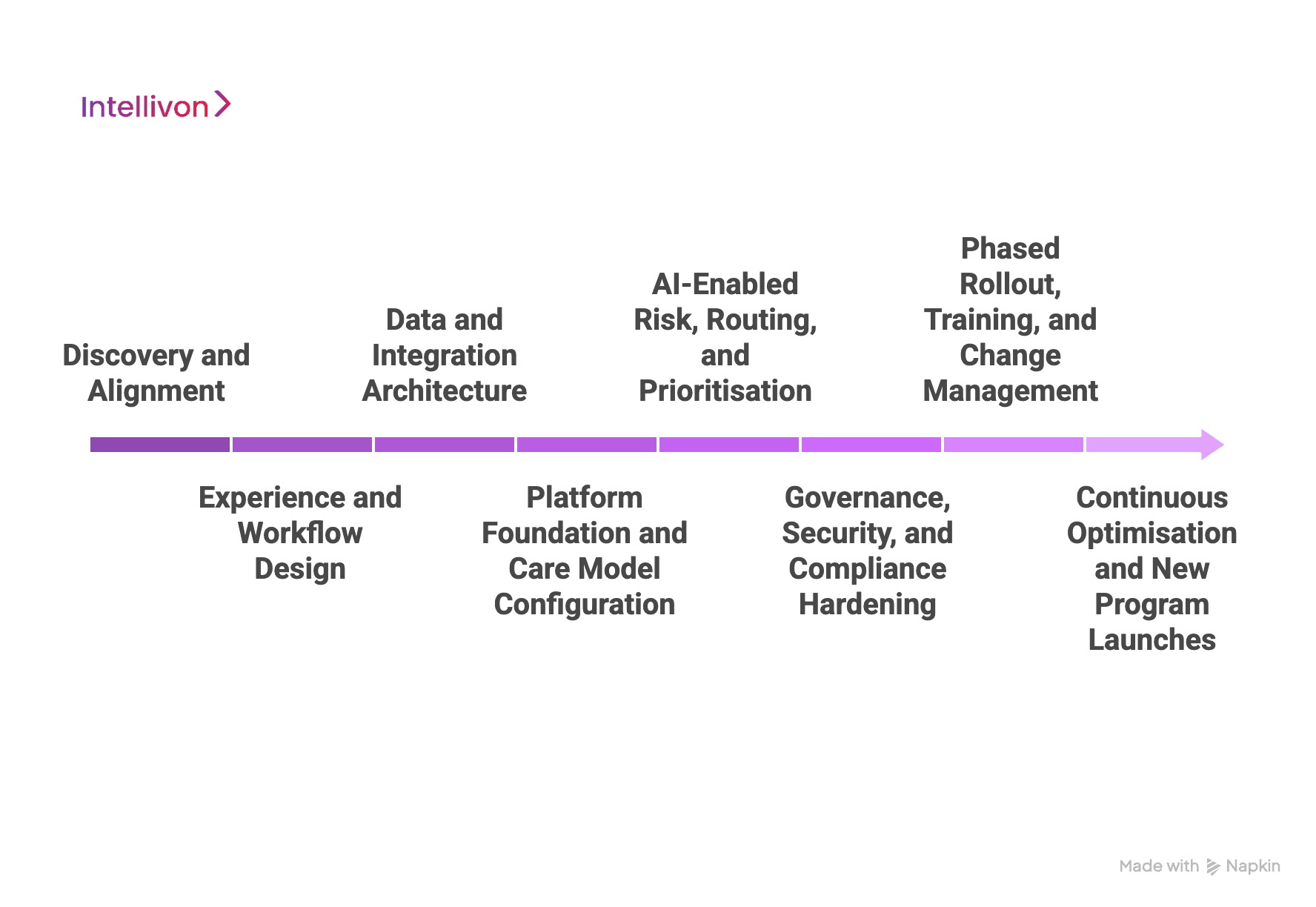
Step 1: Discovery and Alignment
We begin by understanding where coordination actually breaks down in your network today. That means looking at referral leakages, discharge handoffs, chronic care programs, call centre escalations, and gaps between clinical and non-clinical teams.
Our team works with your stakeholders to map current-state workflows, major contracts, value-based arrangements, and technology constraints. We document what “good coordination” means in your context: fewer readmissions, better quality scores, smoother handoffs, or stronger patient engagement.
By the end of this phase, we have a clear problem statement, a prioritised roadmap, and an agreed definition of success tied directly to enterprise metrics.
Step 2: Experience and Workflow Design
Next, we design how the platform should actually feel for care teams and patients. If the coordination tool adds clicks or friction, it will never scale, no matter how advanced the technology is.
We create role-based journey maps for care managers, physicians, nurses, social workers, call centre staff, and care coordinators. These journeys define who sees which tasks, which alerts matter, and how information should appear during a busy day.
From there, we translate these journeys into concrete workflows: referral routing, enrolment into programs, care plan updates, outreach tasks, escalation rules, and handoff checklists. The goal is simple: the platform should give each team member only what they need, at the time they need it.
Step 3: Data and Integration Architecture
A care coordination platform is only as strong as the data feeding it. At this stage, we define how data moves from your ecosystem into the coordination layer and back.
We design an integration architecture that usually spans EHR systems, claims data, telehealth tools, RPM devices, call centre platforms, CRM, and existing PHM or analytics stacks. Our engineers use standards such as HL7, FHIR, X12, and DICOM along with secure APIs to keep data flowing in real time.
We also agree with your teams on which data elements are “source of truth” for decisions: problem lists, risk scores, utilization flags, social determinants, and program enrolment status. That prevents conflicting signals and duplicate work later.
Step 4: Platform Foundation and Care Model Configuration
Once the data backbone is defined, we configure the core platform capabilities. This is where your care models become living, executable workflows instead of static protocols in PDFs.
We build and configure modules for patient enrolment, care plans, task management, risk views, communication, documentation, and reporting. Care pathways for heart failure, diabetes, COPD, post-discharge, oncology, or maternity can be configured as templates and then tailored for your organisation.
At this stage, we also enable multi-entity support if you operate across locations, networks, or partner organisations. Each site can follow standardised models while still preserving local nuances where they truly matter.
Step 5: AI-Enabled Risk, Routing, and Prioritisation
After the foundations are stable, we layer in AI where it adds clear value. The goal is to help teams focus on the right patients, at the right time, with the right actions.
We work with your clinical and operational leaders to design AI models for risk stratification, readmission prediction, deterioration risk, no-show prediction, and outreach prioritisation. These models use your historical data patterns while respecting regulatory and ethical boundaries.
The outputs do not replace clinical judgement. They surface smarter queues, highlight rising-risk patients, and suggest next-best actions so that human teams can intervene earlier and more effectively. All recommendations remain auditable and explainable for governance.
Step 6: Governance, Security, and Compliance Hardening
Enterprise healthcare platforms must be safe before they are smart. Here, we formalise governance and make security decisions that allow you to scale without regulatory surprises.
We align the platform with HIPAA, HITECH, GDPR (where applicable), and regional privacy and security regulations. Access controls, role-based permissions, audit logs, encryption, and data residency are engineered into the design, not patched at the end.
We also define governance processes: who approves new workflows, who validates AI models, how patient consent is handled, and how external partners access data. This step ensures your compliance team remains comfortable as adoption grows.
Step 7: Phased Rollout, Training, and Change Management
A care coordination platform fails if it launches as a “big bang” without behavioural adoption. That is why we roll out in phases and support teams closely.
We start with high-value pilot programs or specific regions, measure impact, and collect feedback. Training is role-specific, scenario-based, and aligned with real tasks rather than “feature tours.” Our teams sit with your coordinators, nurses, and physicians to refine workflows as they use the platform.
Leadership receives clear dashboards on adoption, case volume, program performance, and operational impact. This allows them to steer the rollout and adjust incentives, policies, or staffing where needed.
Step 8: Continuous Optimisation and New Program Launches
Finally, we treat the care coordination platform as a living asset, not a one-time project. Your operating environment, contracts, and patient population will keep changing. The platform must evolve with them.
Our team works with you to monitor KPIs such as readmissions, avoidable ED visits, program enrolment, task completion, outreach success, and staff productivity. When patterns emerge, we refine rules, pathways, and AI models to improve performance.
We also help you launch new programs on top of the same platform: new chronic disease bundles, post-acute networks, high-risk maternity, value-based contracts, or community-based coordination initiatives. Each new use case benefits from the same data, governance, and workflow foundation.
This build process is designed to give your organisation a care coordination platform that is aligned to your strategy, grounded in your data, and usable by real teams under pressure.
With Intellivon as your partner, you are not buying another point solution. You are building a coordination backbone that can support today’s contracts and tomorrow’s models of care, while keeping compliance, AI governance, and enterprise scale at the centre.
Cost To Create A Care Coordination Software Platform
For healthcare enterprises, hospital networks, payers, and population health organizations, the cost of building a care coordination software platform depends far more on scope control and phased execution than on feature volume alone. Platforms become expensive when organizations attempt to support every care program, condition, and line of business in the first release.
At Intellivon, we structure care coordination initiatives around phased, use-case–driven rollouts aligned with enterprise budget cycles, compliance readiness, and near-term operational ROI. This approach reduces capital risk while ensuring the platform remains scalable, governed, and enterprise-ready from day one.
Estimated Phase-Wise Cost Breakdown
Enterprise Care Coordination Software Platform
| Phase | Description | Estimated Cost (USD) |
| Discovery & Care Model Blueprint | Care coordination use-case definition, workflow mapping, stakeholder alignment, and regulatory scoping | 15,000 – 25,000 |
| Platform Architecture & Data Design | Longitudinal patient model, integration architecture, scalability planning | 20,000 – 35,000 |
| Integration & Data Ingestion Setup | EHR, claims, lab, telehealth, RPM integrations using FHIR/HL7/APIs | 25,000 – 45,000 |
| Workflow & Care Pathway Configuration | Task orchestration, care plans, transitions, escalation logic | 25,000 – 40,000 |
| AI Enablement & Risk Stratification | Risk models, prioritization logic, and explainability setup | 20,000 – 35,000 |
| Security, IAM & Compliance Controls | Role-based access, audit trails, consent management, encryption | 15,000 – 25,000 |
| Testing, QA & Operational Validation | Workflow testing, performance validation, compliance checks | 12,000 – 20,000 |
| Pilot Deployment & Training | Phased rollout, care team onboarding, feedback-driven optimization | 15,000 – 25,000 |
Total Initial Investment Range:
USD 145,000 – 250,000
This range supports a secure, compliant, enterprise-grade care coordination platform for a single high-impact program, such as transitions of care, chronic disease management, or high-risk population coordination.
Annual Maintenance and Optimization Costs
Ongoing costs cover infrastructure, integration support, security updates, AI model monitoring, and workflow optimization as volumes grow.
- Estimated Annual Cost: 12–20% of initial build
- Approximate Range: USD 18,000 – 50,000 per year
When built on modular services and governed workflows, these costs scale predictably as programs and populations expand.
Hidden Costs Enterprises Should Plan For
Even well-scoped care coordination platforms introduce additional cost factors over time:
- Expansion into new care programs or specialties
- Supporting additional facilities, regions, or partner networks
- Increased data and messaging volumes as populations scale
- New value-based contracts with additional reporting requirements
- Regulatory updates impacting consent, privacy, or audit expectations
- Ongoing training as workflows evolve and teams grow
Planning for these early helps avoid budget overruns during system-wide rollout.
Best Practices to Stay Within Budget
Healthcare enterprises that control care coordination costs most effectively tend to:
- Start with one high-impact coordination use case
- Roll out programs sequentially instead of all at once
- Use modular, platform-based architecture
- Embed security and compliance at the foundation
- Track operational and financial ROI within the first six months
This phased approach ensures the platform proves value before broader capital investment.
Build Your Care Coordination Platform with Intellivon. Our teams help healthcare enterprises define a tailored cost model and phased rollout strategy aligned with care priorities, regulatory requirements, and long-term growth goals.
Top Care Coordination Healthcare Platforms
Leading care coordination healthcare platforms combine workflow orchestration, interoperability, analytics, and AI-driven risk insights to manage patients across settings, teams, and time.
As care delivery becomes distributed across hospitals, clinics, post-acute facilities, and home settings, several care coordination platforms have emerged as enterprise standards. These platforms are not patient-facing apps alone. They function as operational systems that help health systems manage transitions, chronic care, risk contracts, and team-based workflows at scale.
Below are four widely adopted care coordination platforms, along with how they work, what they are known for, and how AI is applied within each.
1. Epic Care Everywhere
Epic’s care coordination capabilities are embedded within its broader EHR ecosystem. They focus on transitions of care, referrals, and longitudinal care plans across Epic-connected organizations.
The platform works by sharing patient records, care plans, and alerts across hospitals, clinics, and post-acute partners using interoperable data exchange. Care teams can see external encounters, discharge summaries, and follow-up requirements without separate logins.
Epic’s strength lies in scale and adoption. Large IDNs use it to reduce duplicate testing, improve handoffs, and manage care for complex patients already on Epic infrastructure.
AI is used primarily for risk scoring and clinical decision support. Models assist with identifying high-risk patients for readmission, missed follow-ups, or care gaps, with recommendations surfaced directly inside clinician workflows.
2. WellSky Care Coordination
WellSky focuses strongly on post-acute, home health, and community-based coordination. It is widely used by health systems managing transitions beyond the hospital and into long-term care settings.
The platform tracks patients from discharge through home health, hospice, and community services. Care managers monitor status, coordinate providers, and ensure continuity as patients move across care settings.
WellSky is recognized for improving discharge efficiency and reducing breakdowns between acute and post-acute providers. Health systems use it to gain visibility into care beyond hospital walls.
AI capabilities support risk identification, visit prioritization, and utilization trends. Analytics help teams spot patients at risk of deterioration or delayed services and intervene sooner.
3. Health Catalyst Care Management
Health Catalyst combines care coordination with population health analytics. It is commonly used by health systems focused on value-based care and large-scale population programs.
The platform aggregates clinical, claims, and operational data into longitudinal patient profiles. Care teams use these profiles to coordinate outreach, manage chronic programs, and track adherence to care pathways.
Its strength lies in measurable outcomes. Organizations use Health Catalyst to demonstrate improvements in quality metrics, cost of care, and utilization performance under risk contracts.
AI and advanced analytics play a central role. Predictive models stratify populations by risk, identify care gaps, and highlight interventions most likely to reduce cost and improve outcomes for specific cohorts.
4. ThoroughCare
ThoroughCare is purpose-built for care management and coordination programs, particularly for chronic care, transitional care, and remote patient monitoring.
The platform supports team-based care planning, task management, and patient engagement across conditions such as heart failure, diabetes, and COPD. Care coordinators track interactions, monitor adherence, and escalate issues through structured workflows.
It has gained traction among organizations focused on CMS programs and chronic care reimbursement, helping providers operationalize complex care management requirements efficiently.
AI supports prioritization and monitoring by highlighting changes in patient status, engagement patterns, and care plan adherence. These insights help teams focus on patients needing immediate outreach rather than relying on manual review.
These platforms illustrate how care coordination has evolved from manual tracking into enterprise-grade infrastructure. While each system differs in scope and focus, they share a common foundation, which includes interoperability, workflow orchestration, analytics, and increasing use of AI to guide action.
Conclusion
Care coordination has moved from a clinical support function to a core enterprise capability. As care delivery spans hospitals, virtual programs, and the home, health systems need platforms that coordinate people, data, and workflows in real time. When built correctly, care coordination software reduces fragmentation, supports value-based performance, and strengthens patient trust while easing operational strain on care teams.
The organizations that succeed will treat care coordination as long-term infrastructure, not a short-term tool. Partnering with an experienced technology provider makes the difference between limited pilots and scalable impact. With the right platform and execution strategy, care coordination becomes a growth enabler that supports better outcomes, financial resilience, and enterprise-wide innovation.
Build a Care Coordination Software Platform With Intellivon
At Intellivon, we build enterprise-grade care coordination platforms that unify care teams, data flows, and patient journeys into a single governed coordination fabric. Our platforms connect EHRs, care management tools, telehealth, RPM devices, pharmacies, payers, and community partners without disrupting live clinical or revenue workflows.
Each solution is engineered for modern healthcare enterprises. Platforms are compliant by design, resilient under real-world volumes, interoperable across vendors, and built to deliver measurable clinical, operational, and financial ROI from the earliest deployment phases.
Why Partner With Intellivon?
- Compliance-First Care Architecture: Every deployment aligns with HIPAA, GDPR, CMS interoperability rules, and regional regulations, with audit-ready governance embedded into every interaction.
- Workflow-Native Coordination: Task lists, care plans, and alerts surface directly inside existing EHR, care management, and telehealth systems, so teams do not need to change their daily tools.
- Omnichannel Patient and Care Team Connectivity: Our platforms support secure messaging, telehealth, reminders, and caregiver collaboration across web, mobile, and portal experiences without fragmenting communication.
- AI-Enhanced Risk and Outreach: Embedded analytics and AI models prioritize high-risk patients, trigger outreach, and recommend next best actions that fit enterprise care pathways and policies.
- Vendor-Agnostic, Network-Wide Design: We integrate across heterogeneous EHRs, RPM vendors, payers, and community organizations without locking you into a closed ecosystem.
- Scalable Orchestration Across Programs: The same platform can support chronic care, transitional care, behavioral health, population health, and value-based programs without duplicating tooling.
- Zero-Trust Security and PHI Protection: End-to-end encryption, identity-first access control, data minimization, and continuous monitoring protect sensitive information across the entire coordination lifecycle.
Book a strategy call with Intellivon to explore how a custom-built care coordination platform can reduce avoidable utilization, close care gaps, and scale team-based, patient-centered care across your healthcare enterprise.
FAQs
Q1. What is a care coordination software platform in healthcare?
A1. A care coordination platform is a centralized system that connects care teams, patients, and workflows across settings. It helps track care plans, tasks, referrals, and follow-ups in one place. The goal is to reduce fragmentation, close care gaps, and support team-based, longitudinal care for complex and chronic patients.
Q2. How do care coordination platforms improve outcomes and reduce readmissions?
A2. These platforms surface risk signals early, standardize transitions of care, and make it easier to follow evidence-based pathways. Teams see who is responsible for each task, which gaps remain open, and which patients need outreach today. This reduces missed follow-ups, duplicate tests, and avoidable emergency visits, which in turn lowers readmissions and total cost of care.
Q3. What are the key features of an enterprise-grade care coordination platform?
A3. Enterprise care coordination platforms typically include shared care plans, task and workflow management, referrals, secure messaging, and patient engagement tools. They integrate with EHRs, claims, labs, RPM feeds, and telehealth systems to avoid double documentation. Advanced platforms add AI-driven risk stratification, triage queues, real-time alerts, and analytics for quality, capacity, and financial performance.
Q4. How does AI enhance care coordination in large health systems?
A4. AI helps prioritize worklists by predicting who is likely to deteriorate, disengage, or be readmitted. It flags rising risk cohorts, recommends next best actions, and routes patients to the right program or team. When used with strong governance, AI turns raw clinical and operational data into practical, daily workflows for nurses, care managers, and virtual care teams.
Q5. How long does it take to implement a care coordination platform in an enterprise environment?
Timeline depends on scope, integrations, and regulatory expectations, but most large organizations see a first phase live in three to nine months. Faster projects start with a specific population or program, such as heart failure, oncology, or post-discharge follow-up. Partnering with an experienced vendor like Intellivon helps align architecture, integrations, and change management so the platform delivers measurable value from the first rollout.