As digital health programs expand, data rarely stays where it was originally created. It needs to move across EHRs, care settings, partner systems, analytics platforms, and patient-facing applications. Over time, this movement becomes harder to manage, especially when interoperability is built around a single EHR or tied too closely to vendor-specific workflows.
As ecosystems grow more complex, the limits of EHR-centric integration become visible. Data paths multiply, governance becomes harder to enforce, and small changes carry outsized operational risk. At this stage, interoperability is no longer an IT concern. It becomes a question of control, resilience, and long-term scalability. An EHR-agnostic interoperability layer addresses this challenge by creating a neutral foundation for data exchange across systems, vendors, and use cases.
Informed by Intellivon’s work building interoperability platforms that enterprises actually adopt and scale, this blog explains the design choices that determine whether an EHR-agnostic layer becomes foundational infrastructure or another fragile integration. It walks through how such a layer is designed, the types of clinical and operational data it manages, the safety mechanisms required to prevent downstream risk, and the architectural choices that matter at enterprise scale.
Key Takeaways Of The EHR-Agnostic Market
What matters for enterprises is why this market is growing. Healthcare systems are no longer integrating one EHR or one application at a time.
They are operating across multiple EHRs, digital platforms, partners, and regulatory environments. As integration volume increases, point-to-point connections become expensive, fragile, and risky.
This is where the conversation moves beyond integrations to EHR-agnostic interoperability layers. Market growth signals a demand for centralized control, vendor independence, and scalable data exchange.
Enterprises are investing not just to connect systems, but to create stable interoperability foundations that can support long-term digital, clinical, and regulatory requirements.
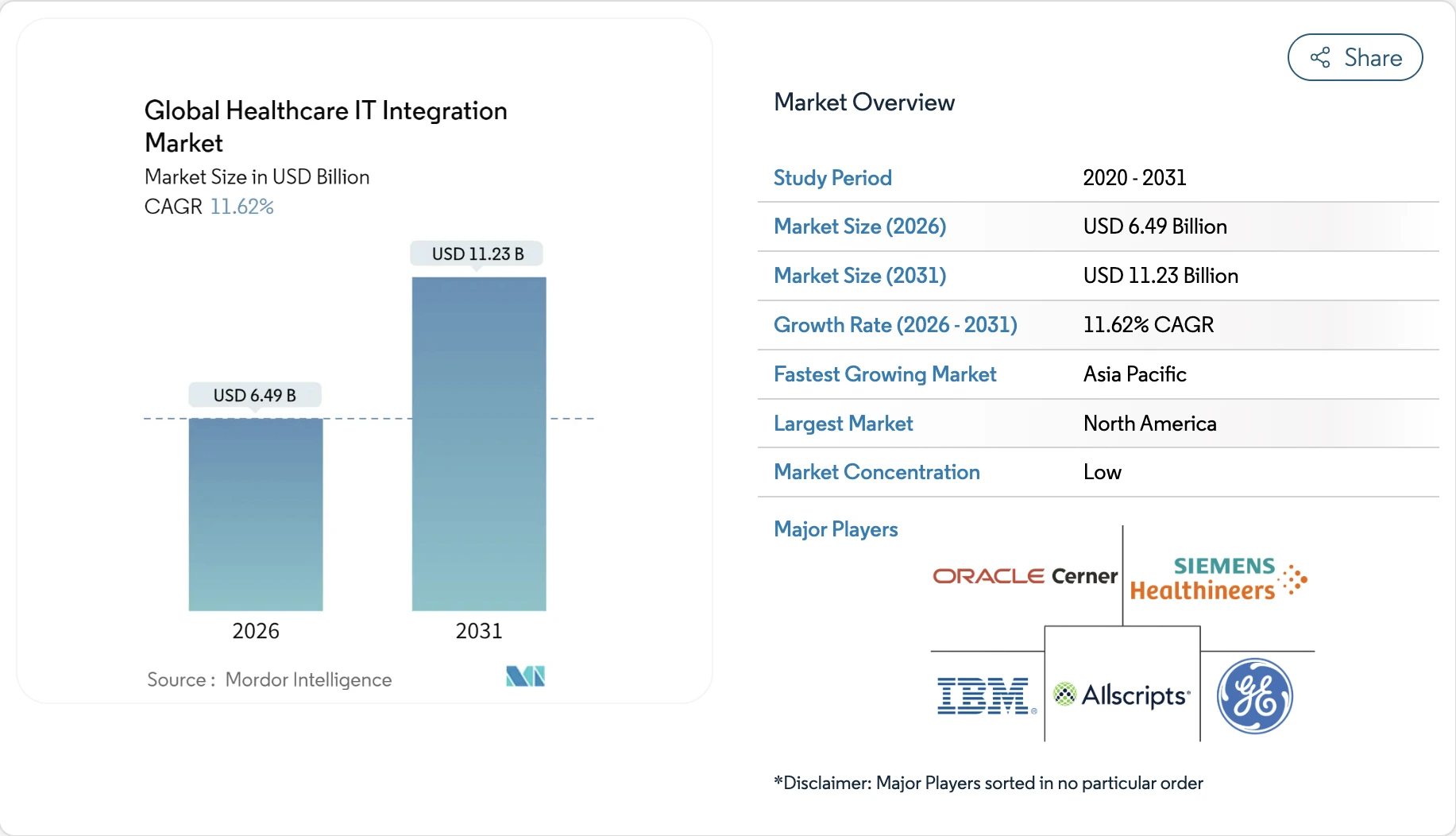
Market Insights:
- Component mix: Services generated nearly 57% of market revenue in 2025, reflecting continued reliance on implementation and integration expertise. However, product-led platforms are accelerating faster, with a projected 13.05% CAGR through 2031.
- Deployment model: On-premise integration solutions accounted for about 62% of market adoption in 2025, driven by legacy infrastructure and regulatory comfort. At the same time, cloud-based integration is gaining momentum, growing at an estimated 12.22% CAGR as enterprises modernize.
- Application focus: Hospital interface and EHR integration represented roughly 40% of total market demand in 2025, underscoring ongoing core system integration needs. In contrast, medical device integration is expanding steadily, with an expected 11.76% CAGR through 2031.
- End-user adoption: Hospitals and clinics remained the primary buyers, contributing nearly 64% of market revenue in 2025. Diagnostic and imaging centers, however, are emerging as the fastest-growing adopters, with growth projected at 11.88% CAGR.
- Regional dynamics: North America led the market in 2025 with close to 43% share, supported by mature digital health ecosystems. Asia-Pacific is showing the fastest expansion, forecast to grow at a 14.12% CAGR as healthcare digitization accelerates.
These trends show that healthcare integration is moving beyond isolated EHR connections. While services and on-premise models still dominate, faster growth in products, cloud adoption, and new use cases signals rising complexity. As systems, regions, and partners expand, point integrations become harder to sustain. This is why enterprises are shifting toward EHR-agnostic interoperability layers that provide long-term control, scalability, and stability.
What “EHR-Agnostic” Actually Means in Enterprise Architecture
EHR-agnostic means your systems do not depend on one EHR to function. Applications and data flows are built once and work with multiple EHRs. When an EHR changes, the rest of the platform does not need to change.
Access rules, security, and data handling stay the same across systems. This gives organizations control over their technology instead of inheriting limits from EHR vendors.
An EHR-agnostic interoperability layer follows a clear, repeatable process. Each step is designed to isolate EHR complexity from the rest of the enterprise. As a result, systems stay stable even as integrations grow.
How It Works
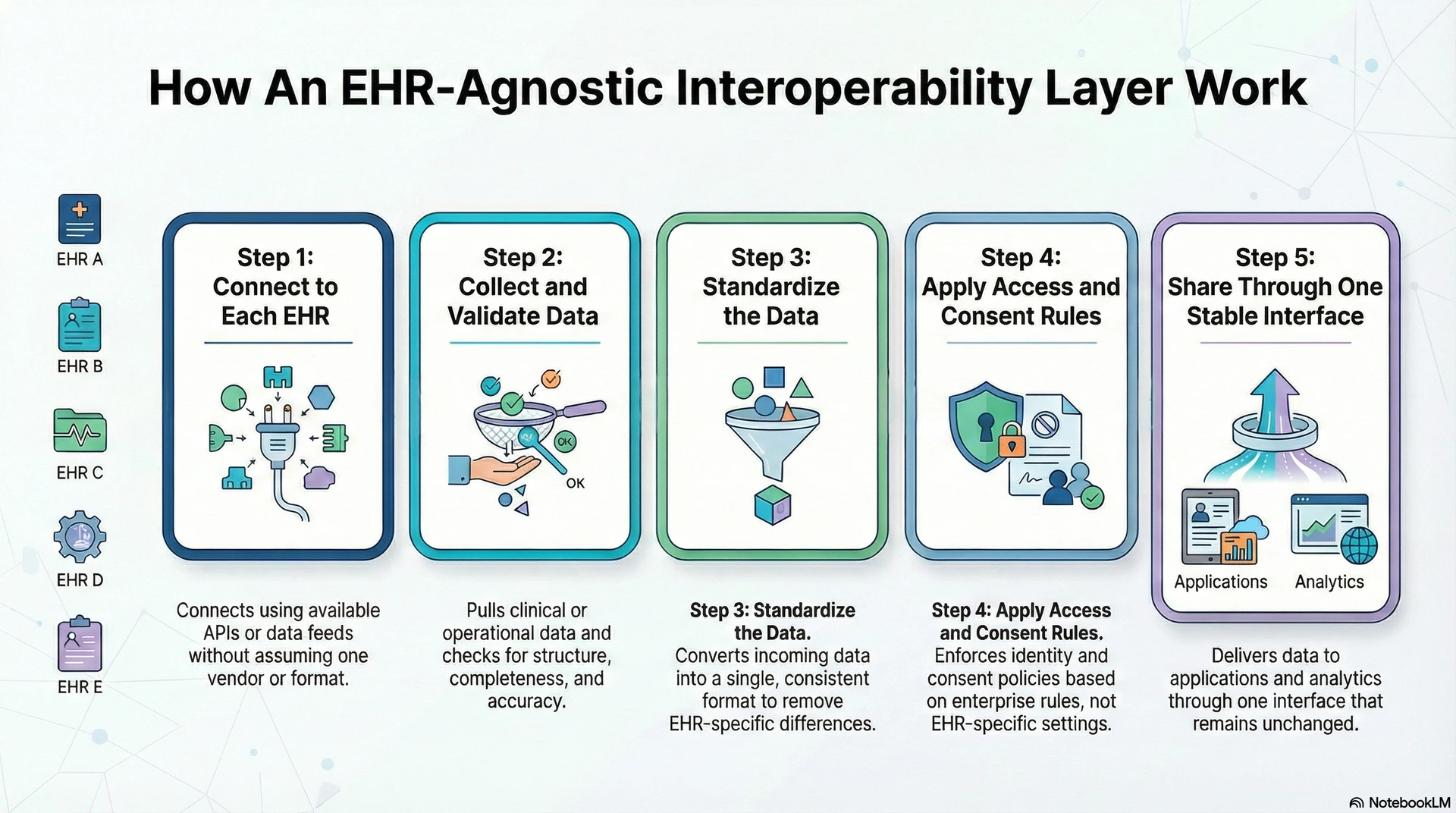
Step 1: Connect to Each EHR
The layer connects to different EHRs using available APIs or data feeds. It does not assume one vendor or format. This allows multiple EHRs to plug into the same platform without custom logic.
Step 2: Collect and Validate Data
Next, the layer pulls required clinical or operational data. It checks structure, completeness, and basic accuracy. Invalid or incomplete data is handled before moving forward.
Step 3: Standardize the Data
Then, incoming data is converted into a single, consistent format. This removes EHR-specific differences. Downstream systems always receive data in the same structure.
Step 4: Apply Access and Consent Rules
After standardization, identity and consent rules are enforced. Access is granted based on enterprise policies, not EHR-specific settings. Every action is tracked.
Step 5: Share Through One Stable Interface
Finally, data is delivered to applications, analytics, or partners through one interface. These systems remain unchanged even when EHRs evolve.
In conclusion, this step-by-step flow removes EHR dependency. It keeps integrations controlled, predictable, and scalable over time.
Enterprise Problems an EHR-Agnostic Interoperability Layer Solves
As healthcare organizations scale, integration issues shift from technical friction to business risk. Multiple EHRs, partners, and digital products increase data movement every day. However, traditional integrations struggle to keep up with this growth.
As a result, teams face rising costs, delays, and governance gaps. This is where an EHR-agnostic interoperability layer directly addresses enterprise-level problems.
1. Too Many Fragile Integrations
Enterprises often rely on many point-to-point EHR integrations. However, each new connection increases maintenance and failure risk. As systems change, fixes must be repeated across integrations. Therefore, teams spend more time repairing than improving systems.
An interoperability layer replaces many connections with one controlled platform. As a result, complexity and rework drop significantly.
2. Lack of Control Over Data and Access
EHR-native integrations apply rules inside each system. However, governance differs across vendors and sites. As a result, access, consent, and audit controls become inconsistent.
Therefore, enterprises struggle to enforce policies uniformly. An EHR-agnostic layer centralizes these controls. This ensures data access follows enterprise rules everywhere.
3. Digital Products Break When EHRs Change
Apps and analytics often depend directly on EHR-specific logic. However, vendor updates or expansions can break these dependencies.
As a result, innovation slows and risk increases. An interoperability layer shields digital products from EHR changes. Therefore, platforms remain stable while EHRs evolve.
In conclusion, these problems are not isolated integration issues. They are structural challenges caused by EHR-centric design. An EHR-agnostic interoperability layer solves them by restoring control, stability, and scalability.
Core Capabilities Required for a True EHR-Agnostic Layer
A true EHR-agnostic layer is defined by how well it controls complexity at scale. It must work consistently across EHRs, regions, and partners. Otherwise, interoperability becomes another fragile integration effort.
Therefore, enterprises must look beyond connectivity and focus on capabilities that reduce long-term risk. The following features explain what makes an EHR-agnostic layer reliable in real environments.

1. Data Standardization Across EHRs
First, the layer standardizes data coming from different EHR systems. Each EHR records similar information in different formats and structures. Therefore, without standardization, data cannot be reused safely.
As a result, the layer converts incoming data into one consistent enterprise format. This ensures downstream systems always receive predictable data. Over time, this reduces repeated cleanup and rework.
2. Centralized Identity and Consent Control
Next, the layer enforces identity and consent rules centrally. EHR-native controls vary by vendor and site. As a result, governance becomes fragmented across systems. Therefore, the interoperability layer applies access rules before data is shared.
This ensures the same policies are enforced everywhere. In addition, audit readiness improves without manual effort.
3. Vendor-Independent Interfaces for Applications
The layer exposes one stable interface to applications and platforms. Applications do not connect directly to EHR-specific APIs. As a result, EHR upgrades or vendor changes do not break downstream systems.
Therefore, digital products remain stable as environments evolve. This decoupling protects long-term platform investments. It also limits vendor lock-in.
4. Data Orchestration and Flow Control
The layer controls how data moves between systems. It decides when data should be routed, validated, or delayed. Therefore, integrations follow consistent business rules. As a result, errors and manual intervention decrease.
In addition, complex workflows remain manageable as scale increases. This keeps operations predictable.
5. Monitoring, Logging, and Audit Visibility
Every data movement is tracked by the platform. Teams can see where data came from, where it went, and who accessed it. Therefore, issues are detected early. As a result, troubleshooting becomes faster and more accurate.
In addition, audit trails are always available. This reduces compliance risk.
6. Performance and Scalability Management
The layer is designed to handle growing data volumes. As hospitals, devices, and partners are added, performance remains stable. Therefore, growth does not require redesigning integrations.
In addition, throughput and reliability are actively managed. This ensures the platform remains usable under pressure. Scalability becomes predictable instead of risky.
In conclusion, these capabilities focus on control rather than connectivity. Without them, EHR-agnostic claims collapse at scale. However, when implemented correctly, they reduce cost, risk, and operational friction.
As a result, interoperability becomes a stable infrastructure. This is what enterprises actually need.
98% of EHR Data Is Not Ready for Enterprise Use
EHR systems capture large volumes of clinical data every day. However, this data is primarily created to support documentation and billing workflows. As a result, it is not structured for reuse across enterprise systems.
Therefore, when organizations scale integrations, data issues surface quickly. This challenge becomes more visible as data moves beyond a single EHR. Consequently, interoperability problems persist despite widespread EHR adoption.
1. Data Is Designed for Internal EHR Use
EHR data is optimized to function inside the system where it is created. However, different EHRs record the same clinical information in different ways. As a result, fields, formats, and context often do not align.
Therefore, when this data is shared externally, it requires correction or rework. In addition, clinical meaning can be lost during exchange. This limits the reliability of downstream systems.
2. Integrations Pass Problems Forward
Most EHR-native integrations move data without fixing underlying issues. As a result, inconsistencies travel downstream into applications and analytics platforms. Therefore, each consuming system must clean and validate data again.
Over time, this duplication increases cost and operational risk. In addition, governance rules are applied unevenly. Consequently, enterprises lose control as integration volume grows.
3. Why an Interoperability Layer Is Required
An EHR-agnostic interoperability layer prepares data before it is shared. First, it standardizes structure and terminology across systems.
Then, it applies validation, consent, and access rules consistently. As a result, downstream systems receive reliable data. Therefore, teams spend less time fixing issues and more time delivering value.
In conclusion, the 98% statistic highlights a structural limitation of EHR-centric architectures. EHRs store data, but they do not govern it at an enterprise scale. As interoperability demands increase, this gap becomes costly.
Therefore, enterprises adopt EHR-agnostic layers to regain control. This approach turns raw EHR data into usable enterprise data.
Reference Architecture for an EHR-Agnostic Interoperability Layer
A reference architecture explains how an EHR-agnostic layer works as enterprise infrastructure. It shows how data moves, where control is enforced, and how scale is handled.
More importantly, it separates EHR complexity from digital platforms. Therefore, each architectural layer has a clear responsibility. Together, these layers create stability as systems, regions, and partners grow.
1. EHR and Source System Connectivity Layer
This layer connects to multiple EHRs and source systems using APIs, feeds, or interfaces. However, it does not expose EHR-specific logic to the rest of the platform. Instead, it isolates vendor differences at the edge.
As a result, adding or changing an EHR does not affect downstream systems. In addition, connectivity changes remain localized. This protects the overall architecture from vendor churn.
2. Data Standardization and Transformation Layer
Next, incoming data is converted into a consistent enterprise format. Different EHRs represent the same information in different ways. Therefore, this layer normalizes structure, terminology, and basic semantics.
As a result, downstream systems always receive predictable data. In addition, transformation logic is managed centrally. This reduces long-term integration debt.
3. Orchestration and Workflow Control Layer
This layer controls how data moves across the ecosystem. It decides routing, sequencing, and validation based on business rules. Therefore, integrations behave consistently across use cases.
As a result, manual intervention is reduced. In addition, complex workflows remain manageable as scale increases. This keeps operations reliable.
4. Governance, Security, and Audit Layer
Governance is enforced before data is shared. Identity, consent, and access rules are applied consistently across all systems. Therefore, enterprises retain control over who can access data and why.
As a result, compliance becomes part of the architecture, not a manual process. In addition, every action is logged. This ensures audit readiness at all times.
5. Application and Consumption Layer
Finally, applications, analytics, and partners consume data through one stable interface. They do not connect directly to EHRs.
As a result, digital products remain unaffected by EHR changes. Therefore, innovation can continue without repeated reintegration. In addition, this layer supports internal and external use cases. Scale becomes predictable.
In conclusion, this reference architecture focuses on the separation of concerns. Each layer absorbs complexity, so the rest of the system stays stable. Without this structure, EHR-agnostic claims break under pressure. With it, interoperability becomes a durable enterprise infrastructure.
Interoperability Standards in an EHR-Agnostic Architecture
Interoperability standards play an important role in healthcare data exchange. However, standards alone do not create enterprise interoperability. Most organizations already use standards and still face integration issues. This happens because standards define format, not control.
Therefore, an EHR-agnostic architecture must use standards carefully. The goal is to enable exchange without creating new dependencies.
1. Where FHIR Fits in an EHR-Agnostic Architecture
FHIR helps standardize how systems request and receive healthcare data. As a result, it simplifies integration for modern applications. However, FHIR implementations differ across EHR vendors and versions.
Therefore, relying on FHIR alone still creates variability. In an EHR-agnostic architecture, FHIR is managed inside the interoperability layer, not exposed directly to apps. This ensures consistency across sources.
- Standardizes how data is accessed
- Simplifies app-level integration
- Varies by vendor and version
- Requires a control layer to stay consistent
2. Supporting Legacy and Mixed Standards
Most enterprises operate with more than one data standard. HL7 v2, CDA, and proprietary formats remain widely used. Therefore, these standards cannot be replaced overnight. An EHR-agnostic layer absorbs this diversity centrally.
As a result, downstream systems do not need to handle multiple formats. This reduces operational complexity over time.
- HL7 v2 remains common in hospital systems
- CDA is still used for document exchange
- Proprietary formats exist across vendors
- Central handling prevents duplication
3. Why Standards Alone Do Not Solve Enterprise Problems
Standards define structure, but they do not enforce governance. They do not manage identity, consent, or access policies. In addition, they do not handle version drift or vendor-specific behavior.
Therefore, standards without a platform layer increase integration work. Over time, this leads to fragmentation instead of simplification. Architecture determines control, not standards.
- No built-in governance or policy enforcement
- No protection from vendor variation
- No control over access and consent
- No solution for long-term scale
In conclusion, interoperability standards are necessary but insufficient. They enable data exchange but do not manage enterprise complexity. An EHR-agnostic architecture uses standards as inputs, not foundations.
As a result, organizations gain flexibility without losing control. This is how interoperability remains stable as systems grow.
Challenges Unique to EHR-Agnostic Interoperability Platforms
Building an EHR-agnostic interoperability platform introduces challenges that do not appear in single-EHR integrations. These challenges emerge as scale, governance, and reuse increase. Therefore, they must be addressed at an architectural level, not through patches.
Otherwise, the platform becomes fragile over time. The sections below explain the most common challenges enterprises face. Each also explains how they are solved in practice.
1. Managing Data Meaning Across Different EHRs
Different EHRs record the same clinical information in different ways. As a result, data can lose meaning when shared across systems. Therefore, values may look correct but behave inconsistently in analytics or applications.
Over time, this creates trust issues across teams. The challenge is not moving data, but preserving context at scale.
How We Solve It
The platform uses a consistent enterprise data model. Therefore, mappings are managed centrally instead of inside applications. In addition, clinical meaning is validated during transformation.
As a result, downstream systems receive predictable data. This keeps reporting and decision-making reliable. Over time, data trust improves.
2. Performance Drops as Integration Volume Grows
As more EHRs, apps, and partners are added, data volume increases rapidly. However, many platforms are not designed for sustained enterprise traffic. As a result, latency, failures, and bottlenecks appear.
Therefore, performance becomes a business risk. This challenge grows silently until scale exposes it.
How We Solve It
The platform is designed for high throughput from the start. Data flows are decoupled and processed asynchronously where needed. As a result, spikes do not break the system. In addition, performance is monitored continuously.
Therefore, capacity is adjusted before issues impact operations. This keeps the platform stable under load.
3. Governance Becomes Fragmented Across Teams
In large organizations, different teams often control different systems. As a result, governance rules become inconsistent. Therefore, access, consent, and audit policies drift over time.
This creates compliance risk and slows approvals. The challenge is maintaining control without slowing innovation.
How We Solve It
Governance is centralized within the interoperability layer. Policies are defined once and enforced everywhere. As a result, teams follow the same rules without added effort. In addition, audit logs are generated automatically.
Therefore, compliance becomes part of normal operations. Control improves without blocking progress.
In conclusion, these challenges are not edge cases. They appear naturally as enterprises scale interoperability. However, when addressed through platform design, they become manageable. An EHR-agnostic layer succeeds only when it anticipates these issues. That is what makes it enterprise-ready.
How We Create An EHR-Agnostic Interoperability Layer For Healthcare Apps
Building an EHR-agnostic layer requires a platform mindset, not an integration mindset. We start by aligning on enterprise outcomes, not just technical connectivity. Then, we design the layer to absorb EHR variation and protect downstream apps.
As a result, applications stay stable even as EHRs change. Therefore, every step prioritizes control, governance, and scalability. This is how we create interoperability that holds up over time.
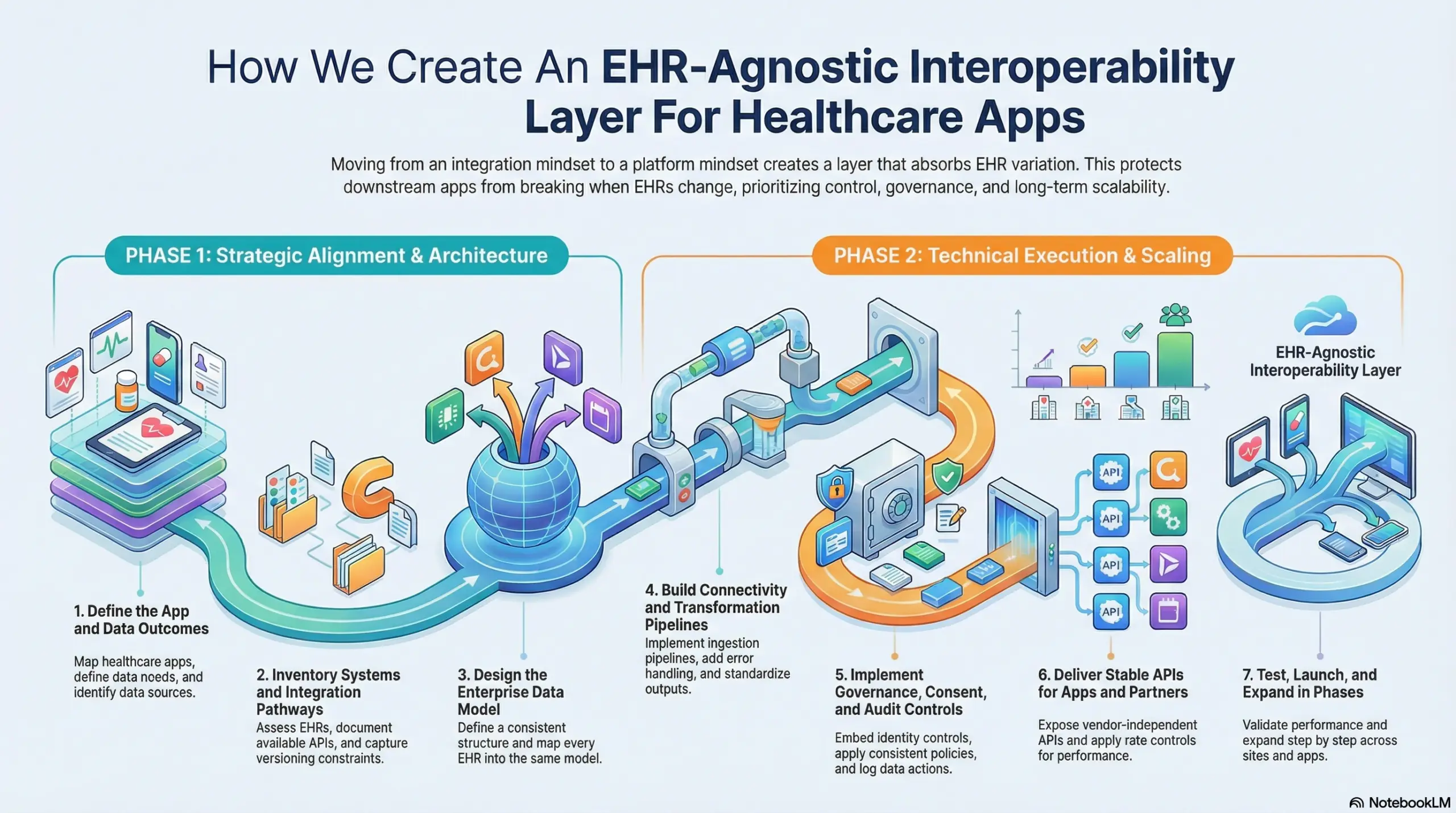
Step 1: Define the App and Data Outcomes
First, we map the healthcare apps that will consume data. We define what each app needs and when it needs it. Therefore, the platform is built around real usage, not assumptions. In addition, we identify the data sources that matter most.
As a result, the scope stays focused and measurable. This reduces rework later.
Step 2: Inventory Systems and Integration Pathways
Next, we assess EHRs, ancillary systems, and partner connections. We document the available APIs, feeds, and interface methods. Therefore, we understand what is possible without disruption.
In addition, we capture constraints like versioning and downtime windows. As a result, integration planning becomes realistic. This prevents fragile designs.
Step 3: Design the Enterprise Data Model
Then, we define a consistent enterprise structure for key data domains. This includes clinical, operational, and identity-related data. Therefore, every EHR maps into the same model.
As a result, downstream apps receive predictable data. In addition, updates stay localized to mappings. This protects applications from change.
Step 4: Build the Connectivity and Transformation Pipelines
After that, we implement pipelines to ingest, validate, and transform data. We add error handling and replay controls for reliability. Therefore, failures do not create manual chaos. In addition, we standardize outputs into stable interfaces.
As a result, apps integrate once and scale across EHRs. This reduces time-to-launch.
Step 5: Implement Governance, Consent, and Audit Controls
Next, we embed identity, access, and consent enforcement in the layer. We ensure policies are applied consistently across sources and consumers. Therefore, compliance does not depend on individual systems. In addition, we log every data action for traceability. As a result, audits become faster and safer. This strengthens enterprise control.
Step 6: Deliver Stable APIs for Apps and Partners
Then, we expose secure, vendor-independent APIs and event streams. Apps consume data through these interfaces, not through EHR-specific endpoints. Therefore, EHR changes do not break applications.
In addition, we apply rate controls and monitoring to protect performance. As a result, access stays stable as usage grows. This supports long-term product scale.
Step 7: Test, Launch, and Expand in Phases
Finally, we validate accuracy, performance, and governance under real workloads. We launch with a focused set of high-value use cases first.
Therefore, teams build confidence without disruption. In addition, we expand step by step across sites, partners, and apps. As a result, scalability is proven, not assumed. This keeps rollouts controlled.
In conclusion, we create EHR-agnostic interoperability by designing for change from day one. Each step reduces dependency on any single EHR and protects downstream apps.
Therefore, enterprises gain stable data exchange without repeated reintegration. As complexity grows, this layer becomes the foundation for digital healthcare products. That is how interoperability turns into durable infrastructure.
Cost Structure of an EHR-Agnostic Interoperability Layer
At Intellivon, EHR-agnostic interoperability layers are built as a regulated healthcare data infrastructure, not as interfaces stitched between systems. The focus stays on creating a durable control layer that operates safely across multiple EHRs, apps, partners, and regions.
When budget constraints exist, scope is refined with intent. However, identity controls, consent enforcement, audit trails, and validation rules are never reduced. Therefore, enterprises avoid remediation costs that surface after rollout.
In addition, predictable architecture limits rework as EHR APIs and environments change. As a result, cost remains controlled as scale increases. Over time, ROI stays protected.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Interoperability Alignment | Use case definition, system inventory, data domains, success metrics | $5,000 – $10,000 |
| Governance & Compliance Baseline | Identity model, consent rules, audit requirements, policy ownership | $6,000 – $12,000 |
| Reference Architecture & Data Model | Platform design, canonical model, mapping strategy | $7,000 – $14,000 |
| Connectivity & Ingestion Setup | EHR/source connectors, routing, API integrations | $8,000 – $18,000 |
| Transformation & Standardization Pipelines | Validation, normalization, error handling | $7,000 – $15,000 |
| Secure API / Event Delivery for Apps | Vendor-neutral APIs, access controls, and throttling | $6,000 – $12,000 |
| Observability, Audit, and Monitoring | Logging, traceability, dashboards | $4,000 – $9,000 |
| Testing & Compliance Validation | Functional, security, and performance testing | $3,000 – $7,000 |
| Deployment & Scale Readiness | Cloud or hybrid deployment, tuning | $4,000 – $8,000 |
Total initial investment: $50,000 – $150,000
Ongoing maintenance and optimization: ~15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped interoperability programs face pressure when indirect cost drivers are ignored. Therefore, planning for these early protects budgets and timelines. In addition, these costs rise faster with point-to-point integrations.
As a result, they must be treated as platform considerations. Common hidden cost areas include:
- Integration complexity as new EHRs, apps, and partners are added
- Compliance overhead from audits and regulatory updates
- Governance effort for consent rules and exceptions
- Infrastructure growth from transaction volume and monitoring
- Change management across IT, clinical, and operations teams
- Continuous monitoring as dependency and risk increase
Best Practices to Avoid Budget Overruns
Cost control depends on architectural discipline from the start. Therefore, decisions must reduce future rework. In addition, platforms should be designed for change, not one-time delivery. As a result, expansion remains predictable. Proven practices include:
- Start with a clear enterprise use case map
- Embed governance and auditability into core design
- Use modular connectors and pipelines
- Standardize data early to avoid repeated cleanup
- Maintain observability across performance and policy enforcement
- Design for vendor and version change
In conclusion, the cost of an EHR-agnostic interoperability layer depends on governance depth, integration diversity, and scale expectations. However, the right structure prevents repeated reintegration costs.
Conclusion
In conclusion, EHR-agnostic interoperability is no longer a technical preference. Instead, it is a strategic requirement for enterprise healthcare systems. As EHR environments grow more complex, point integrations fail to scale safely.
Therefore, organizations need a control layer that standardizes data, enforces governance, and protects digital products. Over time, this approach reduces risk, lowers rework, and enables sustainable growth. Ultimately, interoperability becomes a stable infrastructure, not an ongoing problem.
Build An EHR-Agnostic Interoperability Layer With Intellivon
At Intellivon, EHR-agnostic interoperability layers are built as a regulated healthcare data infrastructure, not as integration tooling layered onto existing EHR systems. Every architectural and delivery decision prioritizes governance, security, and long-term control.
This ensures interoperability platforms operate reliably across multiple EHRs, applications, partners, and regions. As a result, enterprises gain stability that extends beyond initial deployment.
As interoperability programs expand across hospitals, digital products, and external ecosystems, consistency becomes critical. Organizations retain control over data access, consent, and workflows without introducing fragmentation or vendor dependency. This allows healthcare teams to scale confidently without repeated reintegration or compliance risk.
Why Partner With Intellivon?
- Enterprise-grade interoperability architecture designed for regulated healthcare environments
- Proven delivery across multi-EHR systems, digital health platforms, and enterprise care networks
- Compliance-by-design approach with centralized governance and audit readiness
- Secure, modular infrastructure supporting cloud, hybrid, and on-prem deployments
- AI-ready data foundations with monitoring, automation, and human oversight
Book a strategy call to explore how Intellivon can help you build and scale an EHR-agnostic interoperability layer with confidence, control, and long-term enterprise value.
FAQs
Q1. What does EHR-agnostic interoperability mean in healthcare?
A1. EHR-agnostic interoperability means systems are not tied to one EHR vendor. Instead, data flows through a neutral layer that works across multiple EHRs. As a result, applications stay stable even when EHRs change. This reduces vendor lock-in and long-term integration risk.
Q2. Why is FHIR alone not enough for enterprise interoperability?
A2. FHIR helps standardize data exchange, but it does not manage governance or scale. Different EHRs implement FHIR differently. Therefore, relying on FHIR alone still creates inconsistency. An EHR-agnostic layer controls how FHIR is used across systems.
Q3. When does an organization need an EHR-agnostic interoperability layer?
A3. Organizations typically need it once they operate more than one EHR. It also becomes necessary when multiple apps, partners, or regions access clinical data. As integration volume grows, point-to-point models break down. At that stage, a centralized layer becomes critical.
Q4. How does an EHR-agnostic layer reduce integration costs over time?
A4. The layer replaces many fragile integrations with one controlled platform. Therefore, changes are handled once instead of repeatedly. As EHRs evolve, downstream systems remain unaffected. Over time, this reduces maintenance effort and unexpected rework costs.
Q5. Is an EHR-agnostic interoperability layer compliant with healthcare regulations?
A5. Yes, when designed correctly. The layer enforces identity, consent, and access rules centrally. As a result, compliance is applied consistently across systems. Audit logs and monitoring are built into the platform. This supports regulatory readiness as scale increases.






