Message volumes in clinical settings are growing, and care teams are having a difficult time keeping up. This is because physicians and care teams still use a mix of pagers, EHR inboxes, secure messaging apps, and manual escalation steps to manage urgent decisions.
This fragmentation causes real problems where response times become inconsistent, tracking clinical context gets harder, and governance teams have limited insight into how coordination actually occurs across facilities. As these enterprises expand their services and partnerships, these gaps become tougher to manage. Physician collaboration platforms bridge this structural gap by creating a continuous coordination layer that connects clinicians, data, and decisions within a controlled enterprise environment.
At Intellivon, our teams design physician collaboration platforms as a regulated clinical coordination infrastructure that supports real consultation and care team workflows. This blog is an in-depth discussion of how we build physician collaboration platforms that support safe and scalable coordination across modern healthcare enterprises.
Why Healthcare Enterprises Are Investing in Physician Collaboration Platforms
Healthcare organizations are adopting physician collaboration platforms to improve how care teams communicate and work together. As coordination demands grow, many teams struggle with silos, delays, and rising operational pressure.
These platforms bring secure messaging, EHR data sharing, and AI-driven workflows into one environment. As a result, they help reduce clinician workload, lower costs, and support better patient outcomes.
The clinical communication and collaboration market was valued at USD 3,595.4 million in 2025. It is projected to reach USD 17,286.25 million by 2034. During this period, the market is expected to grow at a CAGR of 19.07%.
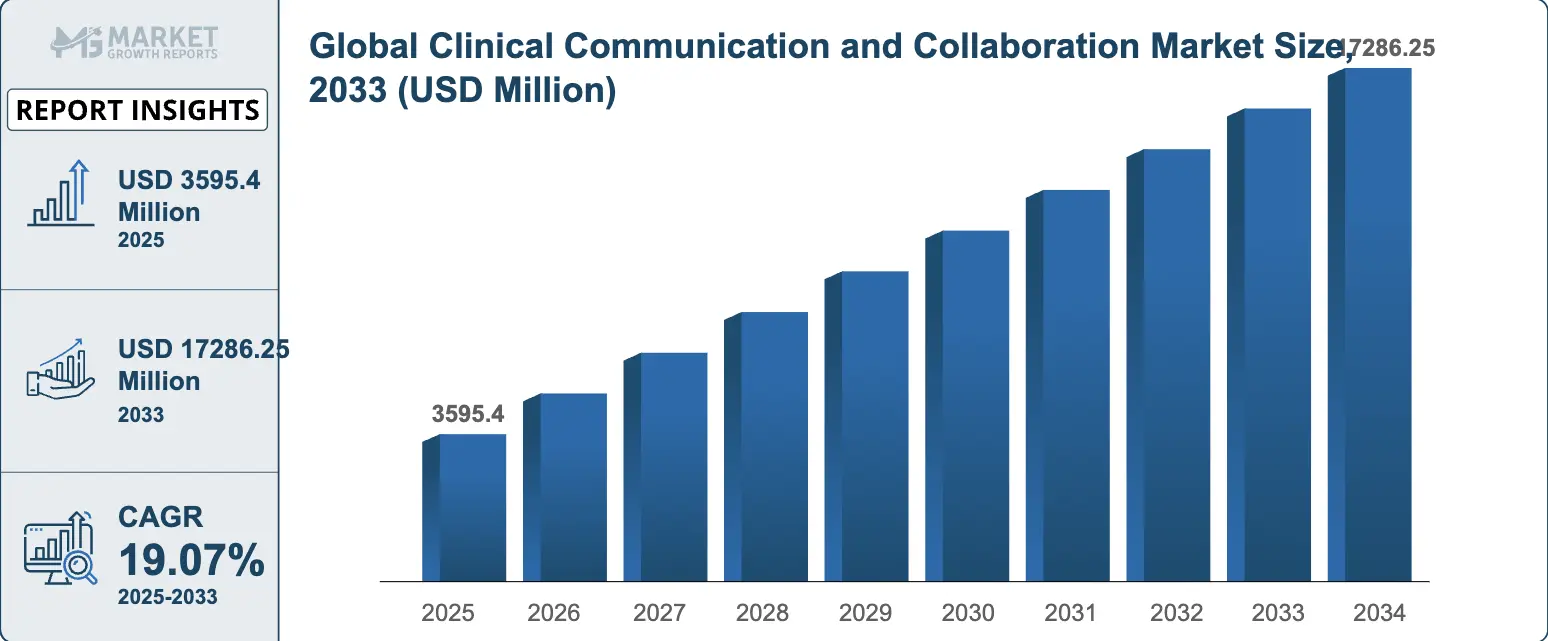
Market Growth Insights:
- Rising chronic disease cases are increasing the need for real-time collaboration across medical specialties.
- Growing telemedicine adoption is pushing providers to coordinate care more efficiently.
- Regulatory pressure around interoperability and value-based care is accelerating enterprise adoption.
- AI-driven diagnostic support is strengthening the case for advanced clinical collaboration tools.
- Post-pandemic care models are shifting toward hybrid and distributed delivery approaches.
- More than 68% of U.S. hospitals now use digital tools to manage cross-specialty coordination.
1. Fragmented Care Delivery Is Increasing Clinical Risk
Care teams now work across departments, facilities, and partner networks. However, communication often remains siloed. As a result, critical context can be lost during handoffs and consults.
Over time, this fragmentation increases the risk of delays, errors, and inconsistent care decisions.
2. Value-Based Care Demands Tighter Coordination
Payment models increasingly reward outcomes instead of volume. Therefore, providers must maintain tighter coordination across the care journey. When collaboration is weak, readmissions often rise and quality metrics decline.
Physician collaboration platforms help teams stay aligned and support performance under value-based contracts.
3. Multi-Hospital Systems Need Unified Communication
Many health systems now operate multiple hospitals and specialty centers. In addition, they often run different EHR environments. Without a unified communication layer, coordination becomes slower and harder to track.
A structured collaboration platform helps standardize workflows across the enterprise network.
4. Physician Burnout and Workflow Friction Are Rising
Clinicians face constant alerts, manual follow-ups, and fragmented inboxes. Consequently, administrative pressure continues to grow. Poorly structured communication tools often add to this burden instead of reducing it.
Purpose-built collaboration platforms streamline interactions and remove unnecessary workflow friction.
5. Compliance and Audit Requirements Are Intensifying
Healthcare organizations must maintain strict control over data access and clinical accountability. At the same time, informal messaging channels create visibility and compliance gaps.
Enterprise collaboration platforms introduce audit trails, role-based access, and governed communication. As a result, organizations stay better prepared for regulatory scrutiny.
Healthcare leaders are prioritizing physician collaboration platforms because coordinated care increasingly depends on a structured, secure, and enterprise-ready communication infrastructure.
What Is a Physician Collaboration Platform?
A physician collaboration platform is a secure digital environment that helps care teams communicate and coordinate patient care in real time. It brings messaging, clinical context, alerts, and workflow routing into one governed system. As a result, physicians can consult faster, track decisions clearly, and reduce manual follow-ups.
Unlike basic chat tools, these platforms connect with EHR systems and support audit-ready communication. Healthcare organizations use them to improve care coordination, reduce delays, and maintain compliance at scale.
Core Capabilities of Physician Collaboration Platforms
Enterprise adoption depends on how well the platform supports real clinical work. Therefore, leaders evaluate capabilities that improve coordination without adding workflow friction.
The most effective physician collaboration platforms combine secure communication, intelligent routing, and deep system integration. Below are the core functions that drive measurable value.
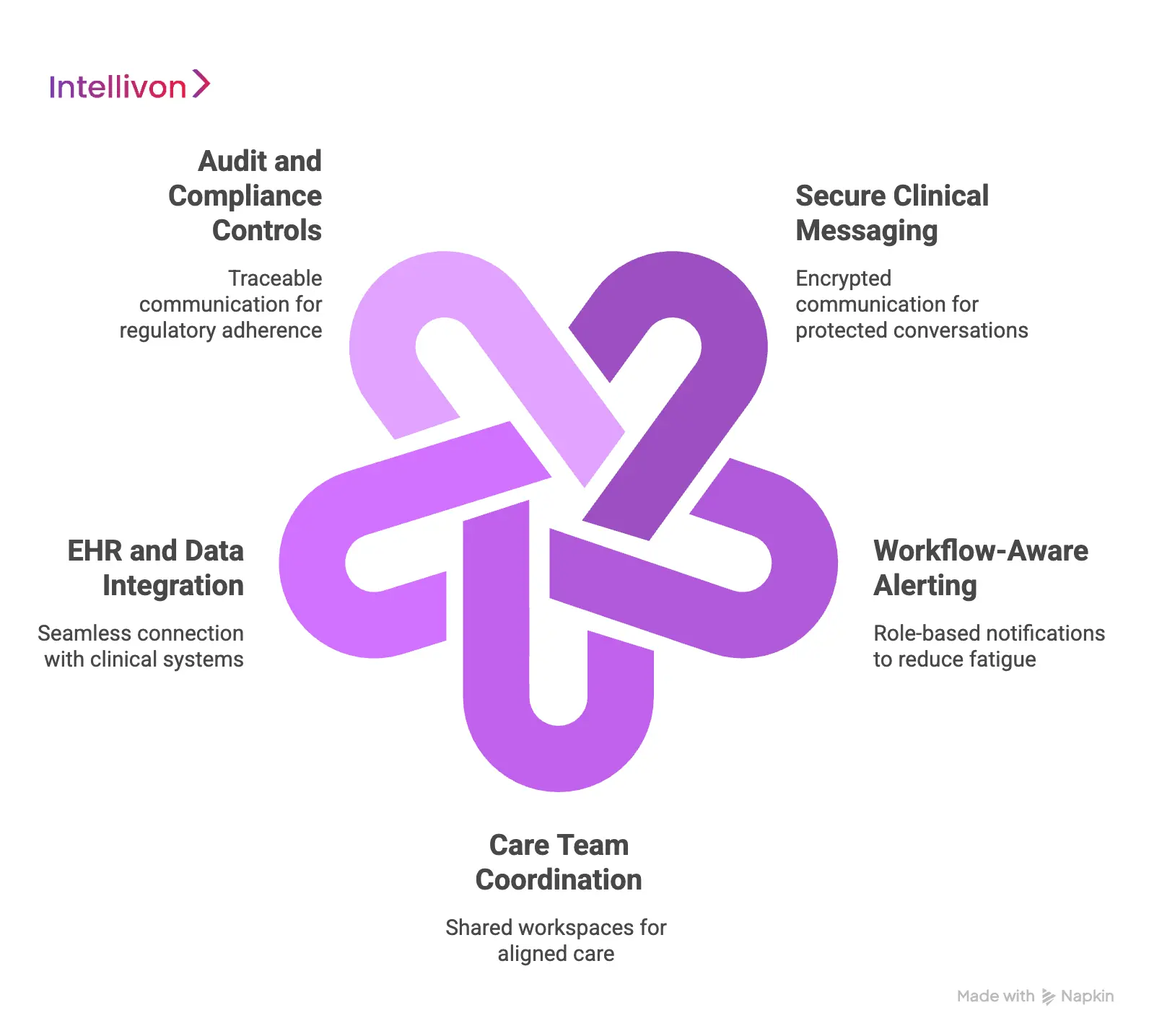
1. Secure Clinical Messaging
Care teams need fast and protected communication. A physician collaboration platform provides encrypted messaging that keeps clinical conversations within a governed environment.
As a result, teams avoid informal channels and maintain full traceability of decisions.
2. Workflow-Aware Alerting
Not every alert should reach every clinician. Therefore, modern platforms use role-based routing to send notifications to the right person at the right time.
This reduces alert fatigue and helps teams respond faster to critical events.
3. Care Team Coordination
Patient care often involves multiple specialists. The platform creates shared workspaces where physicians, nurses, and care managers stay aligned.
Consequently, handoffs become smoother, and accountability becomes clearer across the care journey.
4. EHR and Data Integration
Standalone tools create more silos. In contrast, strong platforms connect directly with EHR systems and clinical data sources.
This allows physicians to view relevant patient context without switching between systems.
5. Audit and Compliance Controls
Healthcare communication must remain fully traceable. Therefore, enterprise platforms include audit logs, role-based access, and policy enforcement.
These controls help organizations maintain compliance and prepare for regulatory reviews.
The true value of physician collaboration platforms comes from how well these capabilities work together. When messaging, workflows, and data integration operate in one governed environment, healthcare organizations can coordinate care more reliably and scale with confidence.
Physician Collaboration Platforms Deliver ROI Within 12 Months
Physician collaboration platforms often show measurable returns within 12 months by reducing errors, cutting wait times, consolidating tools, and improving administrative efficiency.
Most gains come from workflow consolidation, faster clinical coordination, and reduced operational waste. Below is how organizations are seeing returns in real environments.
1. Consolidating Point Solutions
Many hospitals still run multiple communication and coordination tools in parallel. As a result, costs increase while visibility decreases. Unified physician collaboration platforms replace fragmented tools with a single governed environment.
In several enterprise deployments, organizations consolidated up to fourteen point solutions into one platform. Consequently, some health systems reported annual savings of about $1.3 million and recovered implementation costs within the first year. In addition, IT teams benefit from lower maintenance overhead and simpler vendor management.
2. Reducing Clinical Errors
Fragmented communication often contributes to missed context and delayed responses. Therefore, structured collaboration workflows can directly improve clinical reliability.
Recent implementations show error reductions between 29% and 34% after deploying coordinated communication platforms. Because messages, alerts, and decisions remain traceable in one environment, care teams can act faster and with greater confidence. Over time, this improves both patient safety metrics and internal quality reporting.
3. Shortening Wait Times
Response delays frequently occur when consults depend on manual paging or inbox monitoring. However, automated routing and real-time alerts can significantly accelerate decision cycles.
Some health systems have reported wait time reductions of up to 63% after introducing workflow-aware collaboration tools. Faster specialist engagement helps improve throughput in emergency, inpatient, and high acuity settings. As a result, organizations can move patients through care pathways more efficiently.
4. Lowering Support Burden
Disconnected tools often generate high volumes of support tickets and user confusion. Therefore, consolidation into a single collaboration environment tends to reduce help desk pressure.
In practice, some enterprises have seen support calls drop by roughly 43% following platform unification. At the same time, clinician satisfaction scores in certain deployments have climbed to nearly 89%. Simpler workflows and fewer logins play a major role in these gains.
5. Driving Administrative Efficiency
Beyond clinical communication, AI-enabled coordination features are improving back-office productivity. Intelligent routing, automated task assignment, and context-aware alerts remove many manual steps.
Organizations using broader AI-integrated collaboration tools have reported ROI in under 12 months. Much of this value comes from administrative efficiency improvements of about 75% and productivity gains near 74%. These improvements compound as adoption spreads across service lines.
The financial case for physician collaboration platforms is becoming clearer with each large-scale deployment. When implemented as enterprise infrastructure rather than basic messaging, these platforms reduce waste, improve care flow, and strengthen operational visibility.
For organizations under pressure to improve both margins and outcomes, early ROI is no longer the exception. It is increasingly the expectation.
Advanced Features of a Physician Collaboration Platform
Advanced physician collaboration platforms use AI routing, cross-hospital consult workflows, and governed clinical communication to improve specialist response time and enterprise oversight.
Below are the enterprise-grade capabilities that matter most.
1. AI-Driven Consult Routing
High-volume clinical environments cannot depend on manual paging. Modern physician collaboration platforms use AI to route consult requests and on-call alerts automatically. The system evaluates specialty, availability, workload, and escalation rules in real time.
Therefore, the right physician receives the request without manual intervention. As a result, response times become more predictable across departments. Over time, this reduces delays in time-sensitive care decisions.
2. Real-Time Specialist Escalation
Critical cases often require immediate physician attention. Advanced platforms include structured escalation paths for stroke alerts, cardiac events, and urgent lab abnormalities. If the primary physician does not respond within the defined window, the system escalates automatically.
Consequently, care teams avoid gaps caused by missed pages or inbox delays. This closed-loop process improves reliability in high acuity environments. It also strengthens enterprise-level accountability.
3. Cross Hospital Physician Collaboration
Many health systems operate across multiple hospitals, specialty centers, and partner networks. However, specialist access often remains uneven between facilities. Advanced physician collaboration platforms allow physicians to consult across locations while maintaining full clinical context.
Shared case views, imaging summaries, and structured recommendations remain visible to all stakeholders. Therefore, expertise can move across the network without unnecessary patient transfers. This improves both access and operational efficiency.
4. Multidisciplinary Care Workspaces
Complex cases rarely involve a single physician. Oncology, cardiac, and surgical pathways often require coordinated input from multiple specialists. Physician collaboration platforms create shared workspaces where care teams review cases together.
Each update, comment, and decision remains time-stamped and visible. As a result, teams reduce fragmented communication and improve care alignment. This structure is especially valuable during tumor boards and complex treatment planning.
5. Embedded Clinical Context
Physicians lose time when they must switch between multiple systems. Advanced platforms integrate directly with EHR environments to surface relevant patient context within the conversation. Clinicians can view lab trends, imaging summaries, medications, and problem lists in one place.
Therefore, decision-making becomes faster and more informed. This also reduces cognitive load during high-pressure clinical situations. Over time, workflow efficiency improves across the care team.
6. Governance and Audit Visibility
Enterprise collaboration must remain fully traceable. Advanced physician collaboration platforms capture consult timelines, response intervals, and escalation history automatically.
In addition, leaders gain dashboards that show how coordination performs across service lines. This visibility supports compliance reviews, quality programs, and operational audits. As organizations scale, governance remains consistent rather than reactive. Consequently, communication stays controlled even as message volume grows.
Advanced capabilities turn physician collaboration platforms into a true clinical coordination infrastructure. When routing, escalation, and cross-hospital workflows operate together, enterprises gain faster consult cycles and clearer accountability.
How AI Enhances Physician Collaboration Platforms
AI enhances physician collaboration platforms by automating consult routing, predicting clinical risk, reducing alert noise, and improving enterprise visibility across care teams.
As care coordination grows more complex, manual workflows struggle to keep pace. Therefore, many enterprises are adding AI capabilities to physician collaboration platforms to improve speed and decision support. When implemented carefully, AI removes routine friction while keeping physicians in control. Below are the areas where AI is creating the most measurable impact.
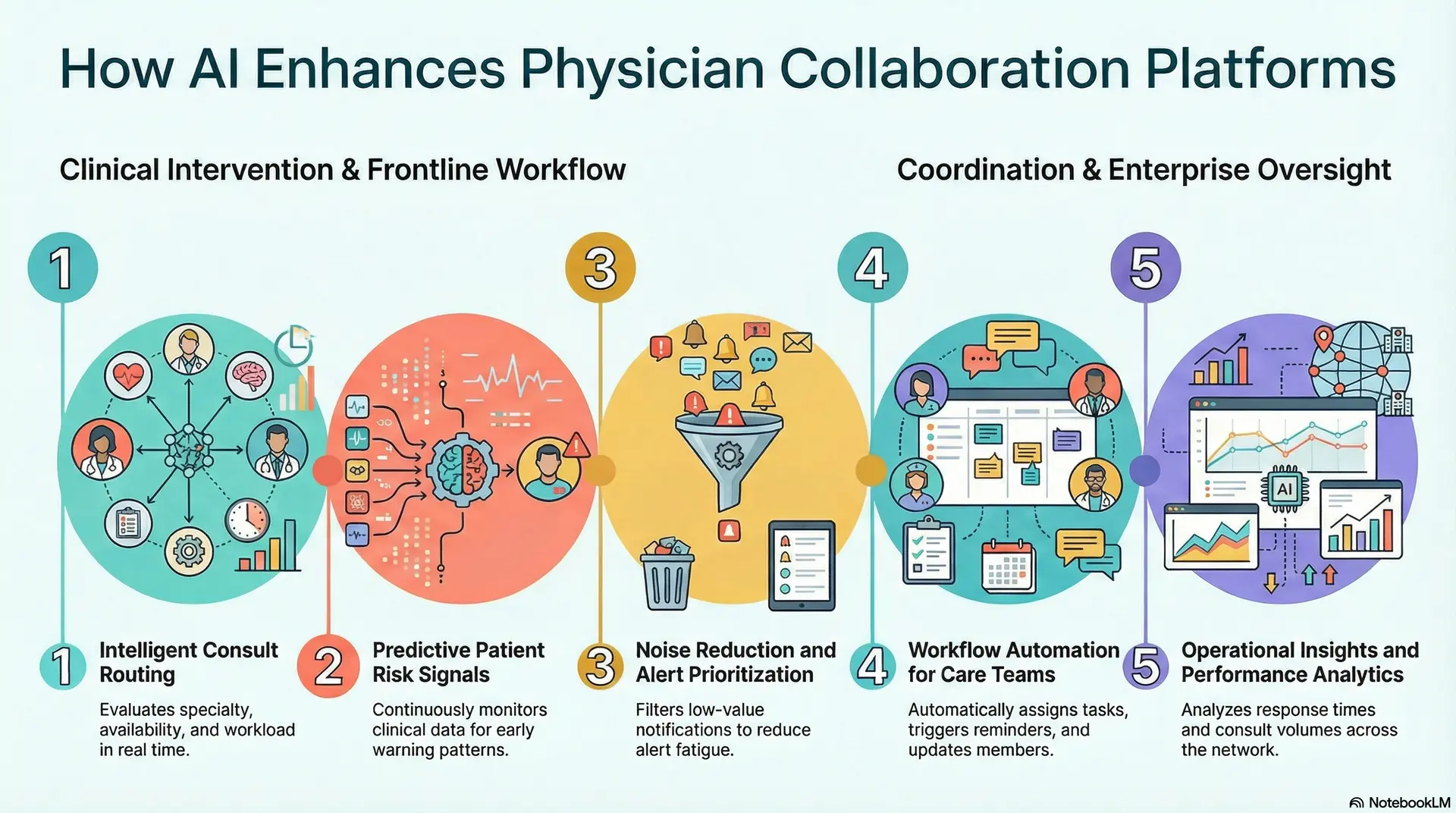
1. Intelligent Consult Routing
AI improves how consult requests move across the care team. Instead of relying on static on-call lists, the platform evaluates specialty, availability, and workload in real time.
Consequently, requests reach the most appropriate physician faster. This reduces manual triage work and improves response consistency. Over time, organizations see smoother consult flow across departments and facilities.
2. Predictive Patient Risk Signals
AI models can continuously monitor clinical data streams for early warning patterns. For example, the system can flag potential sepsis risk, patient deterioration, or abnormal lab trends.
Therefore, physicians receive timely alerts before conditions worsen. Earlier visibility supports faster intervention and better care outcomes. It also helps teams prioritize the patients who need attention most.
3. Noise Reduction and Alert Prioritization
One major challenge in clinical environments is alert fatigue. AI helps by filtering low-value notifications and prioritizing critical events. As a result, physicians see fewer unnecessary interruptions during busy shifts.
Important alerts surface more clearly within the collaboration workflow. This improves focus and reduces the risk of missed signals.
4. Workflow Automation for Care Teams
AI can automate routine coordination steps that previously required manual follow-up. For instance, the platform can assign tasks, trigger reminders, and update care team members automatically.
Consequently, clinicians spend less time managing logistics. Administrative overhead decreases while coordination becomes more reliable. This is especially valuable in high-volume inpatient settings.
5. Operational Insights and Performance Analytics
Beyond frontline workflows, AI also strengthens enterprise visibility. Advanced platforms analyze response times, escalation patterns, and consult volumes across the network.
Leaders can identify bottlenecks and optimize staffing decisions. In addition, predictive analytics help forecast demand across service lines. This supports better planning as organizations expand.
AI is rapidly becoming a core layer within physician collaboration platforms. When used thoughtfully, it improves consult speed, reduces alert fatigue, and strengthens enterprise oversight. Organizations that combine AI intelligence with governed clinical workflows are better positioned to scale coordination safely and efficiently.
How Physician Collaboration Platforms Fit Into Real Clinical Workflows
Physician collaboration platforms are embedded into consults, tumor boards, discharges, and cross-hospital referrals to improve response time, care alignment, and clinical visibility.
When designed correctly, they remove coordination friction without disrupting physician routines. Below are high-impact workflows where enterprises see measurable value.
1. Emergency Department to Specialist Escalation
Emergency teams often need rapid specialist input. Delays usually occur during paging and manual follow-up.
Workflow
- ED physician flags a complex case in the platform
- System routes the consult to the on-call specialist
- Vitals, labs, and imaging attach automatically
- Specialist responds inside the same thread
- Care team receives real-time guidance
- Full consult timeline remains audit-ready
Enterprise impact
- Faster specialist response
- Fewer paging delays
- Closed-loop communication
- Improved time to treatment
2. Multidisciplinary Tumor Board Coordination
Cancer care depends on tight coordination across specialties. However, preparation is often manual and fragmented.
Workflow
- Oncology case created in shared workspace
- Radiology, surgery, and oncology teams are auto-notified
- Imaging and reports aggregated in one view
- Specialists add recommendations asynchronously
- MDT meeting occurs with full clinical context
- Treatment plan documented and distributed
Enterprise impact
- Better case readiness
- Shorter MDT meetings
- Stronger treatment alignment
- Improved documentation quality
3. Inpatient Discharge and Care Transition
Discharge delays typically occur when teams work in silos. Coordination gaps slow bed turnover and increase readmission risk.
Workflow
- Attending physician initiates discharge workflow
- Case management and pharmacy auto-alerted
- Medication reconciliation completed collaboratively
- Follow-up appointments scheduled
- Post-acute providers receive structured handoff
- Transition status is tracked end-to-end
Enterprise impact
- Faster bed availability
- Lower readmission exposure
- Clear task ownership
- Improved transition visibility
4. Cross Hospital Specialist Consults
Community facilities often need tertiary expertise, and phone consults rarely provide full context or traceability.
Workflow
- Referring physician submits structured consult
- Patient summary shared securely
- Specialist reviews asynchronously
- Recommendations returned in the platform
- Local team executes care plan
- Full interaction remains audit visible
Enterprise impact
- Fewer unnecessary transfers
- Expanded specialty reach
- Better network coordination
- Stronger referral retention
Physician collaboration platforms deliver the most value when they align directly with clinical workflows. Organizations that embed structured consults, escalations, and transitions into one governed environment gain faster decisions and clearer accountability.
Security Architecture That Enables Safe Collaboration
Secure physician collaboration requires encryption, role-based access, audit trails, consent controls, and protected APIs to keep clinical communication safe at enterprise scale.
Security is the foundation of any physician collaboration platform. Clinical conversations often include sensitive patient data, consult decisions, and care instructions.
Therefore, enterprises need an architecture that protects information without slowing clinical workflows. When security is built into the platform design, organizations can scale collaboration with confidence. Below are the security layers that matter most.
1. End-to-End Encryption
Clinical communication must remain protected at every step. Modern platforms encrypt data both in transit and at rest. As a result, messages, images, and attachments stay secure even across mobile devices and external networks. Strong encryption also helps replace informal messaging channels that create compliance risk.
Key protections
- Encryption in transit
- Encryption at rest
- Secure media handling
- Protected mobile messaging
2. Role-Based Access Controls
Not every clinician should see the same data. Therefore, physician collaboration platforms enforce role-based and context-aware access.
The system grants visibility based on specialty, care team membership, and clinical responsibility. This ensures users only see the minimum necessary information.
Key protections
- Least privilege access
- Dynamic care team roles
- Break glass controls
- Context-aware permissions
3. Audit Trails and Communication Traceability
Enterprises must track who accessed what information and when. Advanced platforms automatically log consult timelines, message views, and escalation history.
Consequently, governance teams gain full visibility into clinical communication patterns. These records also support compliance audits and quality reviews.
Key protections
- Message-level audit logs
- Access tracking
- Consult timeline visibility
- Escalation history records
4. Consent and Data Governance Controls
Patient consent requirements continue to grow across regions and care models. Therefore, collaboration platforms must enforce policy-driven data sharing.
The system respects consent directives before allowing information to move between clinicians or facilities. This helps organizations maintain regulatory alignment.
Key protections
- Consent-aware data sharing
- Policy-based access rules
- Data segmentation controls
- Cross-region governance support
5. Secure Interoperability and API Protection
Physician collaboration platforms rarely operate in isolation. They connect with EHR systems, imaging platforms, and external partners.
For this reason, strong API security is essential. Modern platforms use token-based authentication, gateway controls, and threat monitoring to protect data exchange.
Key protections
- FHIR security layers
- API gateway controls
- Token-based authentication
- Rate limiting and threat detection
Safe physician collaboration depends on security that works quietly in the background. When encryption, access controls, and governance operate together, organizations can share clinical context without increasing risk.
Enterprises that invest in strong security architecture are better prepared to scale collaboration across complex care networks.
How We Create a Physician Collaboration Platform
Intellivon builds physician collaboration platforms through a structured approach that combines workflow analysis, secure architecture, AI routing, and enterprise-scale deployment.
At Intellivon, we approach physician collaboration platforms as core clinical infrastructure, not as messaging add-ons. Our focus stays on real workflows, enterprise governance, and long-term scalability.
Therefore, every implementation follows a structured path that reduces risk while accelerating adoption. Below is the framework our teams use.
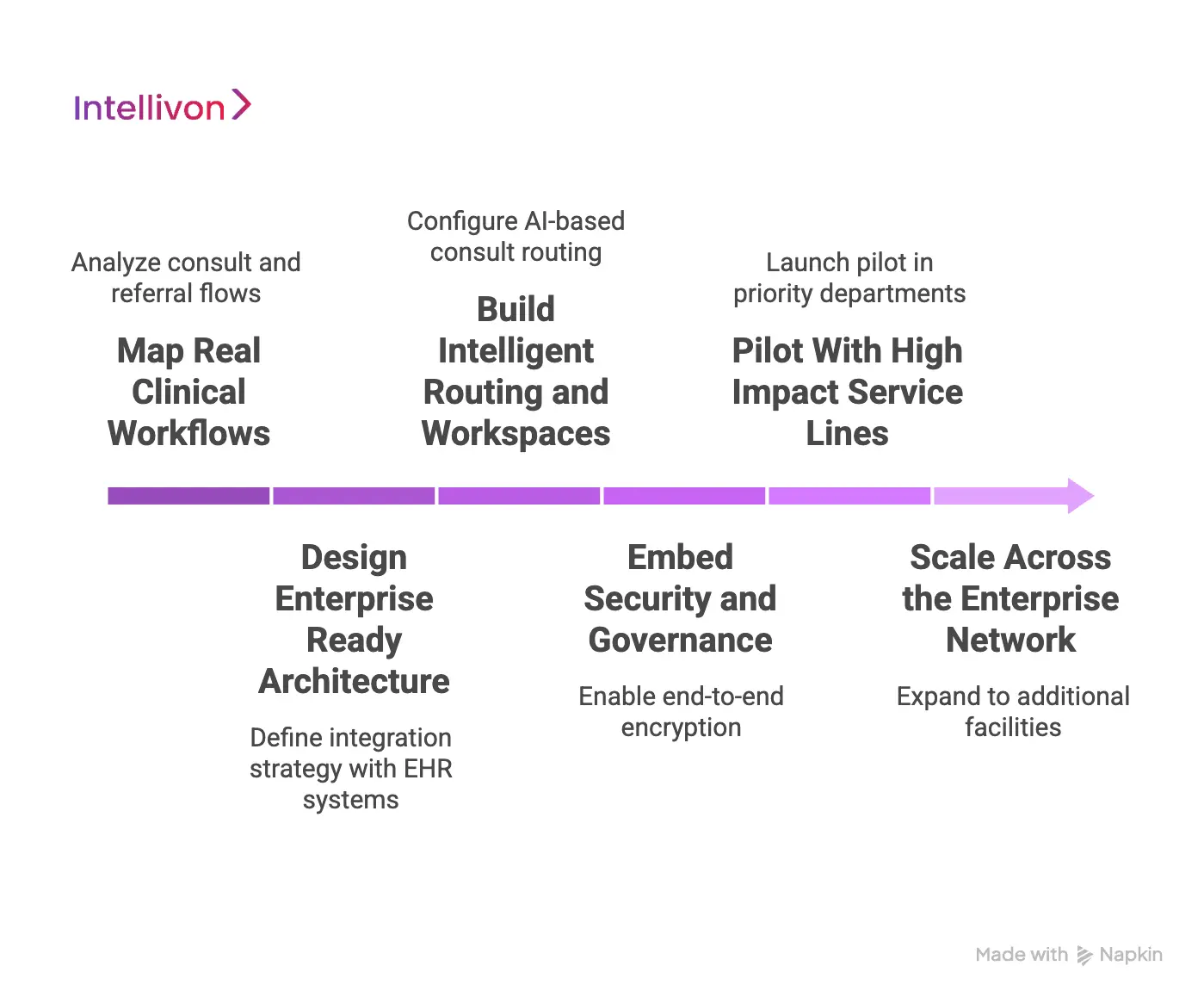
Step 1: Map Real Clinical Workflows
Every successful platform begins with workflow clarity. Our teams work with clinical and operational leaders to understand how consults, escalations, and handoffs actually occur today. This helps identify delays, manual steps, and visibility gaps.
What we do
- Analyze consult and referral flows
- Review escalation patterns
- Identify communication bottlenecks
- Document care team roles
Outcome
- Clear baseline of coordination gaps
- Prioritized use cases for rollout
Step 2: Design Enterprise Ready Architecture
Once workflows are clear, we design the technical foundation. Intellivon architects physician collaboration platforms to support high message volume, multi-facility environments, and strict compliance needs.
What we do
- Define an integration strategy with EHR systems
- Design a secure messaging framework
- Plan identity and access controls
- Establish a scalability model
Outcome
- Future-ready platform blueprint
- Reduced integration risk
Step 3: Build Intelligent Routing and Workspaces
Next, we implement the collaboration engine. This includes AI-driven consult routing, shared care workspaces, and structured escalation paths. The goal is to remove manual coordination wherever possible.
What we do
- Configure AI-based consult routing
- Build multidisciplinary workspaces
- Implement escalation logic
- Embed clinical context views
Outcome
- Faster specialist response
- Cleaner care team alignment
Step 4: Embed Security and Governance
Security is integrated from the start, not added later. Intellivon platforms include encryption, audit visibility, and policy-driven access controls to support enterprise compliance.
What we do
- Enable end-to-end encryption
- Configure role-based access
- Activate audit logging
- Apply consent policies
Outcome
- Audit-ready collaboration
- Controlled data sharing
Step 5: Pilot With High Impact Service Lines
Before enterprise rollout, we validate the platform in targeted environments. This helps prove value quickly and refine workflows with real user feedback.
What we do
- Launch pilot in priority departments
- Track consult response metrics
- Gather clinician feedback
- Optimize routing and alerts
Outcome
- Measurable early ROI
- Stronger clinician adoption
Step 6: Scale Across the Enterprise Network
After validation, the platform expands across hospitals and care settings. Our teams focus on performance monitoring, adoption support, and continuous optimization.
What we do
- Expand to additional facilities
- Monitor usage and response trends
- Provide adoption support
- Continuously refine workflows
Outcome
- Network-wide coordination
- Sustainable enterprise scale
Creating a physician collaboration platform requires more than deploying secure messaging. It demands deep workflow understanding, strong architecture, and disciplined rollout.
Intellivon brings these elements together to help healthcare organizations build a collaboration infrastructure that performs reliably as care networks grow.
Examples of Physician Collaboration Platforms in the Market
Leading physician collaboration platforms combine secure messaging, intelligent routing, voice workflows, and EHR integration to improve real-time clinical coordination.
The physician collaboration market includes several mature platforms that focus on clinical communication and care team alignment. However, each solution approaches collaboration differently. Some focus on messaging, while others emphasize routing, voice workflows, or EHR embedded communication.
Understanding how these platforms operate helps enterprise leaders evaluate architectural depth, workflow fit, and long-term scalability.
1. TigerConnect — Clinical Communication Platform
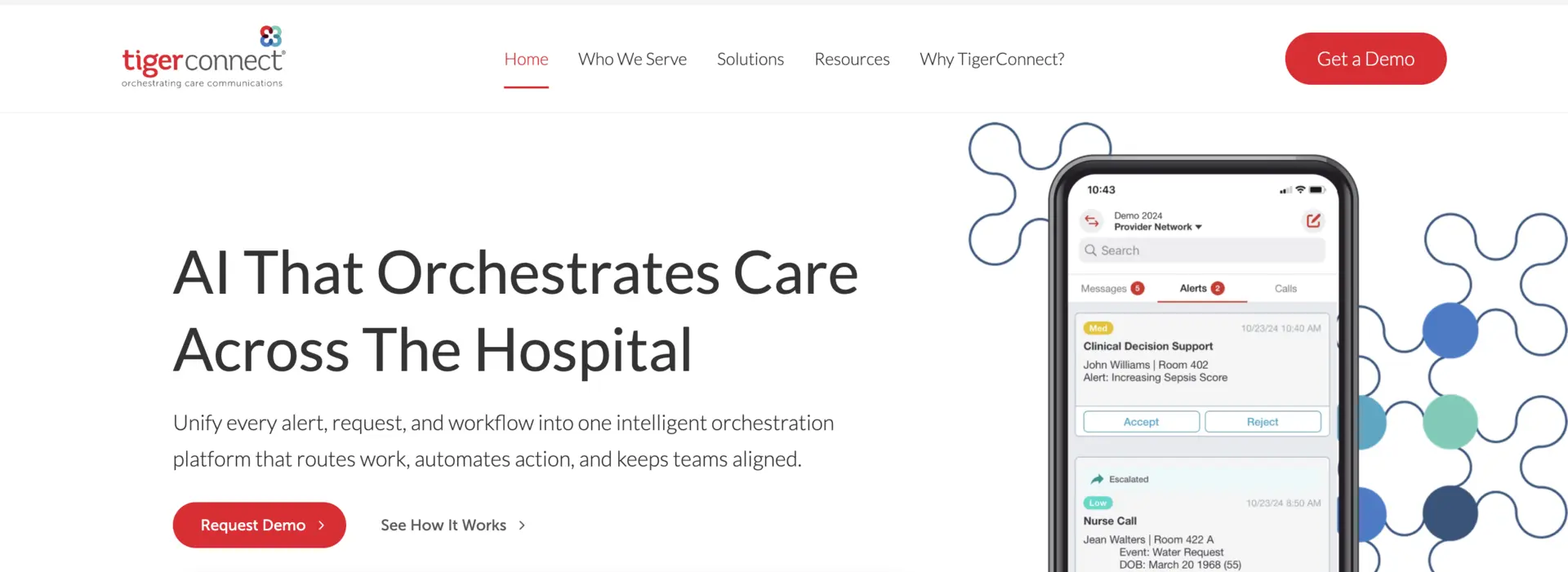
TigerConnect is a purpose-built clinical communication platform widely used in large health systems. The platform combines secure messaging, alert routing, and care team coordination in one environment.
How physician collaboration works
- Physicians receive context-aware alerts from the EHR
- Consult requests route automatically to the right role
- Care teams communicate through secure mobile messaging
- Patient context attaches directly to conversations
- Escalation workflows support time-sensitive events
The platform uses AI to interpret signals from clinical systems and route the next best action across care teams.
How they monetize
- Enterprise subscription licensing
- Module-based pricing for workflow add-ons
- Implementation and support services
- Custom enterprise contracts
TigerConnect is strong in real-time messaging and alert orchestration, especially for large hospitals that want to replace pagers and fragmented tools.
2. PerfectServe — Communication and Scheduling Intelligence
PerfectServe focuses heavily on intelligent routing and on call schedule management. It evolved from secure messaging into a broader clinical communication platform.
How physician collaboration works
- Messages are routed based on call schedules
- The platform integrates with EHR and nurse call systems
- Providers receive role-based notifications
- Care teams coordinate through secure messaging
- Escalation rules manage missed responses
The system routes messages to the appropriate clinician using availability and assignment data, which helps reduce delays.
How they monetize
- Subscription licensing
- Scheduling and routing modules
- Integration services
- Enterprise support packages
PerfectServe is particularly strong for organizations that struggle with on-call complexity and manual consult routing.
3. Vocera Engage — Voice First Clinical Collaboration
Vocera Engage, now part of Stryker, is known for its voice-driven clinical communication model. It is widely used in inpatient and acute care environments.
How physician collaboration works
- Hands-free voice communication between clinicians
- Secure messaging and alerts in one platform
- Integration with clinical and operational systems
- Rapid response team activation
- Role-based communication workflows
The platform blends voice, text, and alarm notifications to support real-time clinical interaction across care teams.
How they monetize
- Hardware plus software bundles
- Enterprise licensing
- Device ecosystem revenue
- Implementation services
Vocera is well-suited for hospitals that prioritize hands-free communication in high acuity environments.
Each platform approaches physician collaboration differently, with strengths in messaging, routing, voice, or EHR integration. Enterprises should focus on workflow fit and scalability to choose a solution that supports long-term clinical coordination.
Conclusion
Physician collaboration platforms are quickly becoming essential infrastructure for modern healthcare organizations. As care teams spread across departments and facilities, structured and secure coordination is no longer optional.
Enterprises that invest early often see faster consult cycles, clearer accountability, and better operational visibility. However, success depends on choosing a platform that fits real clinical workflows and integrates cleanly with existing systems.
When implemented thoughtfully, physician collaboration platforms do more than improve communication. Organizations that treat collaboration as a strategic capability will be better prepared for the next phase of digital healthcare.
Build a Physician Collaboration Platform With Intellivon
At Intellivon, physician collaboration platforms are built as a regulated clinical coordination infrastructure, not secure messaging layered onto disconnected tools. Every architectural and delivery decision prioritizes consult workflow integrity, governance controls, and long-term operational stability.
As collaboration programs scale across hospitals, specialty groups, and partner ecosystems, consistency becomes critical. Governance, performance, and audit readiness remain steady as message volume, specialist engagement, and workflow complexity increase.
Why Partner With Intellivon?
- Enterprise-grade collaboration architecture built for regulated healthcare environments
- Proven delivery across multi-hospital systems and complex care networks
- Compliance by design with audit visibility and access governance embedded
- Secure, modular platform supporting cloud, hybrid, and on-prem deployments
- AI-ready foundation for intelligent routing, analytics, and workflow automation
Book a strategy call to explore how Intellivon can help you design and scale a physician collaboration platform with confidence, control, and long-term enterprise value.
FAQs
Q1. What is a physician collaboration platform?
A1. A physician collaboration platform is a secure digital system that helps care teams communicate and coordinate patient care in real time. It connects messaging, consult routing, clinical context, and audit controls in one governed environment. Healthcare organizations use it to reduce delays, improve specialist alignment, and maintain compliance across the enterprise.
Q2. How is a physician collaboration platform different from secure messaging?
A2. Secure messaging focuses mainly on encrypted communication. In contrast, physician collaboration platforms add workflow routing, consult management, and clinical context. Therefore, they support structured care coordination rather than simple chat. Enterprises prefer these platforms because they improve accountability and scale better across complex care networks.
Q3. Do physician collaboration platforms need EHR integration?
A3. Yes, deep EHR integration is critical for enterprise success. Without it, clinicians must switch between systems, which slows decisions and increases friction. Modern physician collaboration platforms connect with HL7 and FHIR data sources to surface relevant patient context inside the workflow. This keeps communication fast and clinically meaningful.
Q4. How long does it take to implement a physician collaboration platform?
A4. Most enterprise implementations take three to six months for an initial rollout. However, timelines vary based on integration complexity, the number of facilities, and workflow customization needs. Many organizations begin with a focused pilot in high-impact departments before scaling across the network. This approach reduces risk and improves adoption.
Q5. What ROI can enterprises expect from physician collaboration platforms?
A5. Enterprises often see value within the first year when platforms are implemented correctly. Common gains include faster consult response, fewer communication errors, and improved operational visibility. Over time, organizations also benefit from lower coordination costs and better clinician satisfaction. The strongest ROI comes when collaboration is embedded directly into clinical workflows.






