There is a rapid rise in wearable and remote monitoring data in the healthcare industry. However, only a small fraction can use it effectively. This is because device feeds come in different formats, signals lack clinical context, and teams spend hours trying to interpret patterns that should show up automatically. Continuous data exists throughout the organization, but useful insights rarely emerge.
A wearable health data intelligence platform can change this situation. It combines device data, real-time signals, historical records, and behavioral inputs into a structured analytical layer that makes sense to clinical and operational teams. Instead of scattered measurements, organizations receive structured intelligence that highlights risks, detects anomalies, and aids timely intervention. This change improves decision-making and eases the operational challenges that slow down modern care programs.
At Intellivon, we have spent more than a decade building enterprise healthcare platforms that manage continuous physiological data, integrate with complex device ecosystems, and uphold strict compliance across large clinical environments. Drawing from this experience, we are using this blog to discuss how wearable health data intelligence platforms should be designed from the ground up.
Key Takeaways of the Wearable Health Data Market
The wearable medical devices sector was valued at about USD 42.68 billion in 2024. It is expected to reach roughly USD 53.73 billion in 2025 and accelerate toward nearly USD 427.05 billion by 2034, reflecting a strong projected CAGR of 25.90% during 2025–2034.
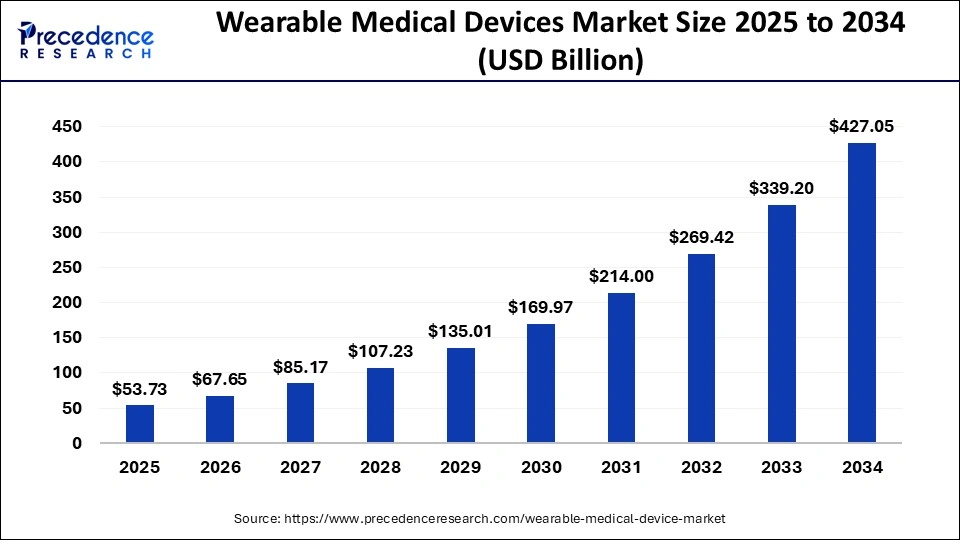
Market Insights:
- An estimated 44–45% of Americans now use health-tracking wearables, and more than 80% are open to sharing this data with their care teams. National adoption among adults generally ranges between 35–50%.
- Worldwide, the number of wearable users surpassed 1.1 billion by 2024, with device shipments rising 9.6% year-over-year to 136.5 million units in Q2 2025.
- Healthcare-focused wearables saw steady momentum, climbing from roughly 28–30% adoption in 2019 to about 36% by 2022 as AI tools and telehealth programs became more common.
Performance and Clinical Reliability
- Clinical studies show strong reliability across many devices, including low heart rate measurement bias, around 86% rhythm interpretation accuracy, and satisfaction scores averaging 3.7–3.8 compared with 2.6 for traditional monitors.
- Sustained wear and data transfer rates remain high, with adherence ranging between 85–93.5% and data transmission success above 90%. Predictive performance for arrhythmia detection often reaches 76–90% positive predictive value.
- Among 310 reviewed consumer wearables, only about 11% met formal biometric validation criteria. However, the validated subset supported meaningful clinical actions, enabling intervention in roughly 10–35% of detected events.
Right Time to Build a Wearable Intelligence Platform
Enterprises now operate in a market where adoption is widespread, clinical reliability is improving, and patients are willing to share continuous health data. At the same time, organizations need structured intelligence rather than raw device feeds. This convergence of maturity, scale, and patient readiness creates an ideal window for healthcare systems to invest in a wearable data intelligence platform that strengthens risk management, supports proactive care, and builds new digital operating models for the decade ahead.
What Is a Wearable Health Data Intelligence Platform?
A wearable health data intelligence platform is a governed system that collects, standardizes, and analyzes continuous signals from wearable devices and remote monitoring tools. It transforms raw measurements into structured insights that clinical and operational teams can use.
Instead of isolated data points, the platform builds a unified view of patient patterns, risk factors, and recovery trajectories. It integrates with EHRs, telehealth systems, care management tools, and enterprise analytics so insights move directly into existing workflows.
Enterprises use this platform to improve oversight, detect early deterioration, support chronic care programs, and strengthen value-based care performance. The goal is to turn continuous data into actionable intelligence that fits the scale and complexity of modern healthcare.
How It Differs from Basic Wearable Tracking Apps
Most consumer tracking apps were designed for personal wellness, not clinical decision-making. They capture activity trends or heart rate snapshots but offer little context or interoperability. A wearable intelligence platform takes a different role. It connects continuous signals with clinical meaning, governs sensitive data, and embeds insights into enterprise workflows. The table below highlights the core differences in a clear, scannable format.
Consumer Tracking Apps vs. Wearable Health Data Intelligence Platforms
| Capability | Basic Wearable Tracking Apps | Wearable Health Data Intelligence Platforms |
| Purpose | Personal wellness tracking | Clinical and operational intelligence |
| Data Interpretation | Shows raw numbers | Detects patterns, trends, anomalies, and risk |
| Clinical Context | None; user-driven | Links data to diagnoses, recovery paths, and care plans |
| Integration | Limited to mobile apps | Connects with EHRs, care management tools, telehealth, analytics |
| Governance & Compliance | Minimal; not PHI-ready | HIPAA-grade controls, audit trails, encryption, role-based access |
| Scalability | One user at a time | Thousands of patients with automated processing |
| AI Capabilities | Basic activity stats | Predictive models, early-warning alerts, risk scoring |
| Operational Use | Individual insights only | Supports population health, chronic care, RPM, and workflows |
| Data Quality Controls | Inconsistent | Continuous validation, signal cleaning, and reliability checks |
The distinction goes far beyond tracking features. A wearable intelligence platform offers the architecture, governance, and analytical depth needed for enterprise healthcare. It transforms continuous data into insights that care teams can trust and operationalize, enabling clinical-grade monitoring at a real-world scale.
How does it work?
A wearable intelligence platform follows a structured flow. It ingests data, enriches it with context, applies analytics, and drives insights into care workflows. The strength lies in how these layers operate together.
1. Data Ingestion and Standardization
The platform collects signals from multiple wearables and normalizes them into consistent formats that clinical systems can understand.
2. Intelligence Layer and AI Models
Machine learning models analyze patterns, detect anomalies, and forecast risk using continuous activity, heart rate, sleep, and recovery markers.
3. Interoperability and Workflow Integration
Insights flow into EHRs, telehealth tools, and care management platforms so teams can act without switching systems.
4. Continuous Governance and Quality Controls
The system monitors data quality, model behavior, and access permissions to maintain trust and compliance at scale.
When these layers function together, continuous data becomes more than a stream. It becomes a reliable intelligence engine that supports timely intervention and enterprise-level decision-making.
Real-World Use Cases Of Wearable Intelligence Platform
A wearable intelligence platform becomes valuable when it solves real clinical and operational challenges. The most impactful deployments focus on early detection, proactive outreach, and continuous oversight.
These use cases show how enterprises can turn raw device signals into measurable outcomes across different care environments.
1. Postoperative Recovery Monitoring
Wearable signals help teams track recovery patterns between discharge and follow-up visits. Subtle shifts in heart rate trends, mobility, or sleep often surface several days before symptoms appear. A platform can route these insights to care teams, allowing timely checks or medication adjustments.
This leads to fewer avoidable readmissions and smoother recovery paths for high-risk patients.
2. Chronic Disease Management at Scale
Patients with heart failure, COPD, diabetes, and hypertension generate meaningful physiological patterns that change over time. The platform detects deviations that may indicate worsening control or early deterioration.
Teams gain a continuous view of risk, enabling proactive interventions rather than reactive escalations.
3. Virtual Wards and Hospital-at-Home Programs
Enterprises can move selected patients out of inpatient settings while still maintaining clinical oversight. The platform provides real-time alerts on instability, supports vital trend reviews, and integrates with telehealth workflows.
This increases bed capacity while preserving safety and efficiency.
4. Population Health Programs and Value-Based Care
Wearable intelligence strengthens care models where outcomes and utilization matter. It helps identify rising-risk populations earlier and supports ongoing monitoring without manual workload increases.
Enterprises gain the ability to target interventions, reduce acute events, and improve program performance.
5. Behavioral Health and Stress Monitoring
Continuous data provides early visibility into changes in activity, sleep, or physiological stress markers. When connected to a governed intelligence layer, these insights support behavioral health teams in detecting early signals of decline.
It enhances patient engagement and helps teams intervene before issues escalate.
6. Clinical Trials and Real-World Evidence Generation
Trials benefit from continuous, objective measurements rather than episodic site visits. The platform standardizes data across devices, improves adherence tracking, and provides near real-time insights into participant well-being.
This improves data completeness and accelerates study timelines.
These use cases show that wearable intelligence is not limited to wellness or basic tracking. When built on an enterprise platform, continuous signals become a strategic asset. They reduce risk, strengthen operational performance, and support care models that depend on early insight and timely action.
Wearable Data Platforms Can Predict Complications With 74% Accuracy
Real-world clinical research shows that wearable data combined with machine learning can detect postoperative complications days before traditional diagnosis, offering sensitivity near 91% and accuracy around 74%. The Science Advances study by Hua et al. demonstrated this clearly.
A wearable intelligence platform takes these research insights and operationalizes them at enterprise scale. Instead of treating such models as isolated experiments, the platform embeds them into care pathways, escalation rules, and coordinated outreach. This allows early-warning signals to reach the right teams in time to change outcomes.
1. How Early Detection Enhances Postoperative Care
Machine learning models built on wearable signals identify deviations from a patient’s expected recovery curve. When paired with a governed data platform, these deviations can trigger early reviews, symptom checks, or care team outreach. This prevents deterioration from going unnoticed and reduces the reliance on patient self-reporting, which often arrives late.
2. Transforming Recovery Monitoring at Scale
Enterprises gain the ability to track thousands of recovery journeys simultaneously. The intelligence layer learns from each case, refining its understanding of what “normal recovery” looks like across demographics, surgeries, comorbidities, and activity patterns. This helps organizations move from episodic monitoring to continuous oversight without increasing staff burden.
3. Reducing Avoidable Readmissions
Many readmissions begin with small physiological changes. A platform that surfaces risk several days earlier gives teams time to intervene. Even a simple teleconsultation or medication adjustment can prevent escalation. This early window, made possible by wearable intelligence, directly affects readmission rates, LOS, and downstream costs.
4. Closing Clinical Blind Spots
Traditional recovery assessments rely on scheduled visits or patient complaints, which means complications may progress unnoticed. Wearable data fills this gap. Continuous signals offer visibility during the days when most issues emerge but care teams have the least contact. A structured intelligence platform ensures these insights are not lost in raw data streams.
Why This Matters for Enterprise Leaders
Research like Hua et al.’s is more than an academic milestone. It shows what becomes possible when continuous data is transformed into governed clinical intelligence. Predicting complications three days before diagnosis is a meaningful operational advantage.
For enterprises, the opportunity lies in building a wearable intelligence platform that brings this capability into real workflows, improves outcomes, and reduces the cost of postoperative care at scale.
Core Features of a Wearable Health Data Intelligence Platform
A wearable health intelligence platform converts continuous sensor streams into governed, clinically relevant insights through real-time ingestion, AI analytics, interoperability, longitudinal modeling, and enterprise-grade compliance.
When these capabilities align, enterprises gain real-time visibility into patient status, clearer risk signals, and actionable insights that improve efficiency and outcomes.
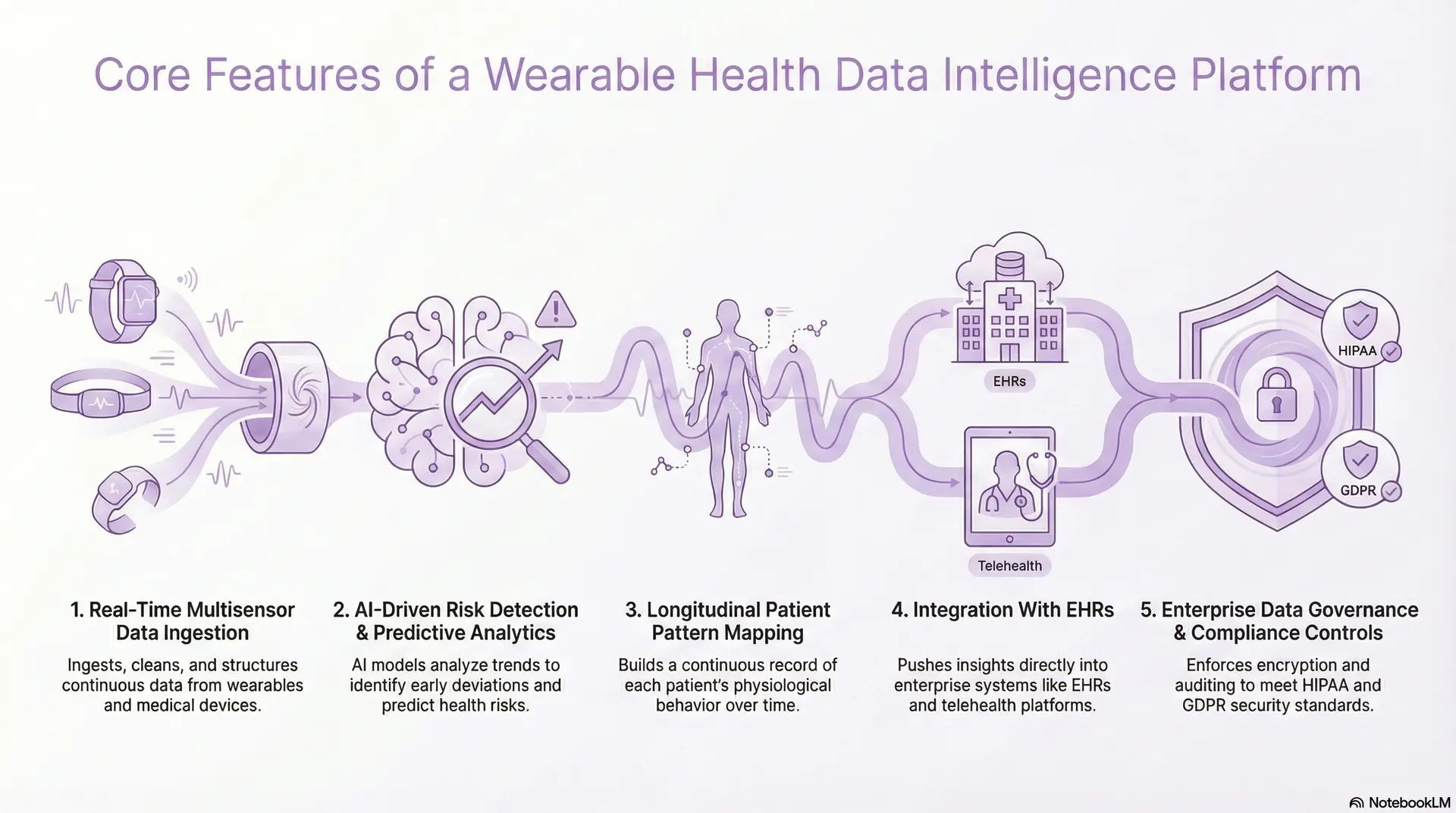
1. Real-Time Multisensor Data Ingestion
The platform ingests continuous data from wearables, medical-grade devices, and remote monitoring tools. It cleans each stream, removes noise, and converts irregular signals into structured formats that downstream systems can understand.
This process covers heart rate variability, sleep cycles, step patterns, oxygen saturation, temperature, and more. It ensures every incoming signal is consistent and ready for intelligence processing.
2. AI-Driven Risk Detection and Predictive Analytics
Machine learning models analyze fluctuations in daily activity, heart rate trends, sleep quality, movement patterns, and physiological stress markers. They identify early deviations that often precede deterioration, complications, or poor disease control.
These models detect subtle shifts that manual review would miss. They support early alerts, targeted outreach, and more efficient care pathways. Over time, the system learns from outcomes and refines its predictions to improve reliability.
3. Longitudinal Patient Pattern Mapping
The platform builds a continuous record of each patient’s physiological behavior over time. It maps recovery patterns, chronic condition trajectories, and daily variations in activity or sleep.
This longitudinal perspective provides context that episodic clinical visits cannot offer. Changes become visible across weeks rather than hours, helping teams spot slow declines or incomplete recoveries.
4. Integration With EHRs
The platform pushes insights directly into enterprise systems through secure, standards-based APIs. It integrates with EHRs, telehealth platforms, care management tools, and clinician dashboards, ensuring teams do not need to switch applications.
This reduces workflow friction and prevents insight gaps that occur when data lives in isolated apps. Clinicians receive alerts, risk scores, and summaries alongside existing patient records.
5. Enterprise Data Governance and Compliance Controls
A wearable intelligence platform must operate with strict governance. It enforces encryption, role-based access, data isolation, logging, and auditing to meet HIPAA, GDPR, and organizational security standards.
It validates data quality continuously, monitors model behavior, and ensures that sensitive information is used appropriately. These controls build trust. They allow enterprises to scale continuous monitoring programs without increasing regulatory exposure or operational risk.
These core capabilities form the backbone of a true wearable health data intelligence platform. When implemented together, they help enterprises move beyond raw wearable data and build a governed, reliable intelligence layer that supports early detection, workflow efficiency, and better patient outcomes.
Architecture Blueprint for a Wearable Health Intelligence Platform
A wearable health intelligence platform typically spans six layers, which includes devices, connectivity, data lakehouse, AI services, applications, and a cross-cutting security and governance fabric.
The goal is to get a structure that accepts noisy signals at scale, converts them into intelligence, and pushes insights into real workflows without compromising security or performance.
1. Device and Edge Layer
This layer covers smartwatches, patches, medical wearables, home monitoring kits, and clinical devices. It also includes any edge components that preprocess signals before they reach the cloud.
Typical responsibilities include:
- Capturing raw physiological and activity data.
- Applying basic quality checks or smoothing.
- Handling offline buffering and secure transmission.
Enterprises should prioritize devices with reliable data quality, clear regulatory status, and stable SDK or API support.
2. Ingestion and Connectivity Layer
Here, the platform connects to multiple device ecosystems and funnels data into a single entry point. It manages streaming, batching, and protocol differences across vendors.
Key capabilities:
- Supporting APIs, SDKs, BLE, MQTT, and integration with device clouds.
- Normalizing timestamps, identifiers, and basic units.
- Handling retries, error queues, and throughput spikes.
This layer must stay resilient. If ingestion fails, every downstream layer loses trust in the data.
3. Data Lakehouse and Storage Layer
All standardized data lands in a governed lakehouse or equivalent architecture. This combines the flexibility of a data lake with the structure of a warehouse.
Typical features include:
- Raw, curated, and feature-ready zones.
- Support for time-series storage and partitioning by patient, cohort, and program.
- Versioning of datasets for audit and model reproducibility.
This layer creates the analytical backbone. It ensures that historical, real-time, and derived data can coexist and remain traceable.
4. Intelligence and AI Services Layer
This is the analytical engine. Models consume cleaned data and produce risk scores, predictions, and recommendations.
Core functions:
- Running anomaly detection, forecasting, and classification models.
- Managing model lifecycles, retraining, and performance monitoring.
- Exposing intelligence through APIs and event streams for other services.
Enterprises should treat this as a modular layer. It should be easy to plug in new models, update existing ones, and test performance across different populations.
5. Clinical and Operational Applications Layer
This layer delivers insights to the people who act on them. It includes clinician dashboards, population health views, care management consoles, and patient-facing applications.
Examples:
- Recovery monitoring dashboards for surgical teams.
- Risk lists and task queues for care coordinators.
- Population-level views for strategy, finance, and quality leaders.
The design principle is straightforward. Insights must appear in a form that is simple to interpret and easy to act on.
6. Security, Compliance, and Governance Fabric
Security and governance sit across every layer instead of living in a single box. They manage how data enters, moves, and leaves the platform.
Core elements:
- Identity and access management with least-privilege principles.
- Encryption in transit and at rest, plus secrets management.
- Audit logs, consent tracking, and policy enforcement.
This fabric protects the organization while still allowing innovation. It reassures boards, regulators, and clinical leaders that continuous monitoring does not create uncontrolled risk.
This blueprint offers a practical way to think about a wearable health intelligence platform. It separates concerns without fragmenting responsibility. When these layers work together, enterprises gain a stable foundation where wearable data flows from devices to decisions in a controlled, predictable, and scalable manner.
How We Built a Wearable Health Data Intelligence Platform
Building a wearable health intelligence platform requires a structured process, which includes clarifying use cases, designing architecture, setting up data pipelines, deploying AI models, integrating workflows, and governing everything with strong compliance.
Below is a step-by-step view of how a partner like Intellivon typically approaches these builds for large healthcare organizations.
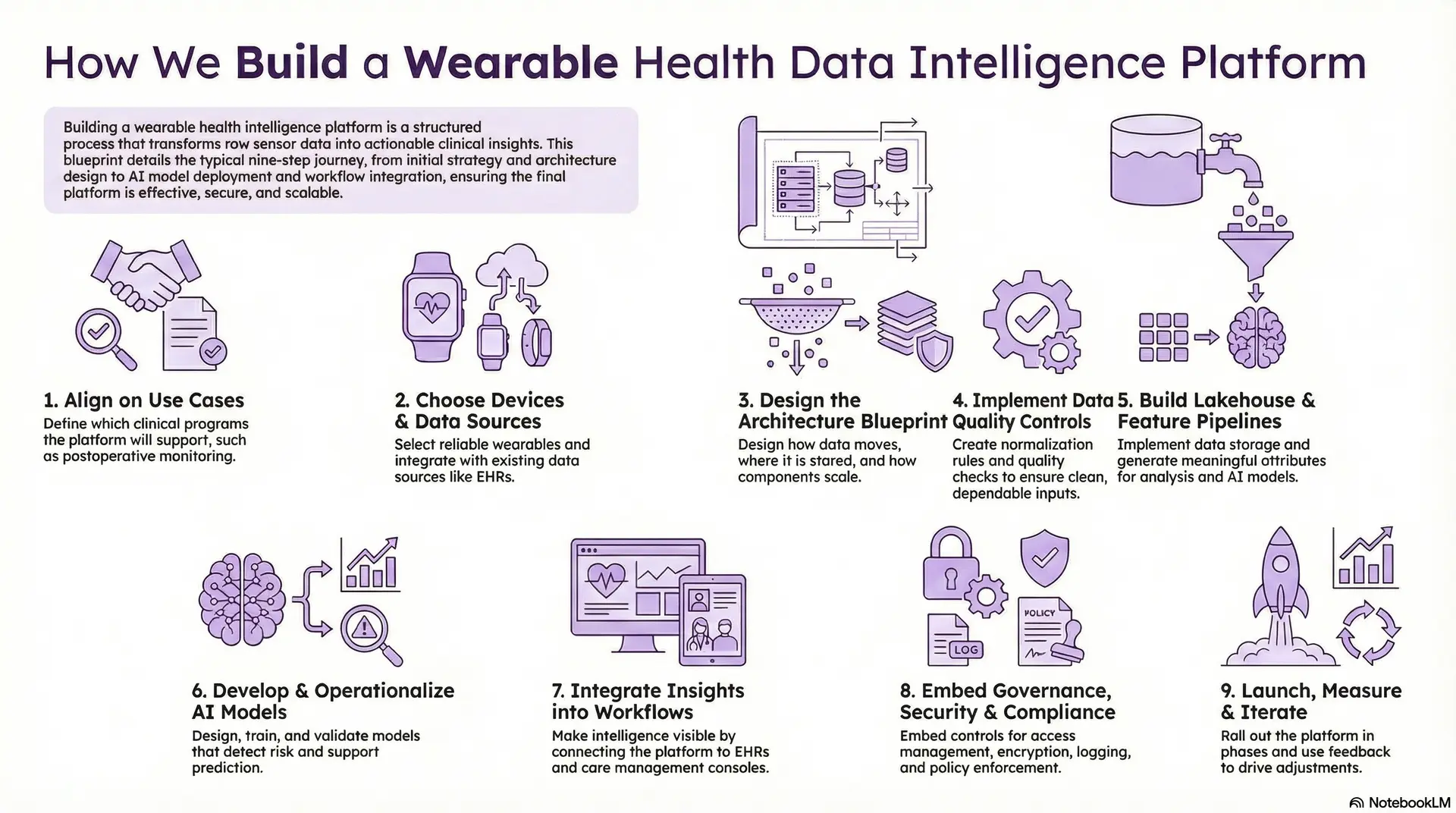
Step 1: Align on Use Cases
We begin with outcomes, and not devices. The first step is to clarify which programs the platform should support. Common starting points include postoperative monitoring, heart failure management, COPD, diabetes, or hospital-at-home. We identify the clinical owners, operational sponsors, and technical teams.
This alignment prevents “pilot sprawl” and keeps every technical decision tied to measurable impact.
Step 2: Choose Devices and Data Sources
Next, we define which wearables, sensors, and existing data sources the platform will support. Device selection focuses on reliability, comfort, regulatory status, and integration options.
We also look at EHR feeds, claims data, telehealth tools, and existing RPM platforms. This helps us understand what context the wearable signals will sit beside.
The goal is a realistic ecosystem, not a lab environment that works only on paper.
Step 3: Design the Architecture Blueprint
Once the ecosystem is clear, we design the architecture that connects it. This includes device and edge components, ingestion pipelines, a data lakehouse, AI services, and application layers.
We define how data moves, where it is stored, and how each component scales. We also map which layers need low latency and which can be batch-based.
This blueprint becomes the reference point for engineering, security, and clinical teams.
Step 4: Implement Data Quality Controls
With architecture approved, we build the ingestion layer. It handles APIs, SDKs, and streaming protocols from different device vendors.
We create normalization rules so heart rate, steps, sleep stages, and other metrics arrive in consistent formats. We also build data quality checks that flag gaps, outliers, and corrupted records.
This step ensures that the intelligence layer receives clean, dependable inputs.
Step 5: Build the Lakehouse and Feature Pipelines
We then implement the lakehouse that holds raw, curated, and feature-ready datasets. Time-series storage and partitioning strategies are selected to match clinical and analytical needs.
On top of this, we design feature pipelines. These pipelines generate meaningful attributes such as recovery slopes, variability metrics, adherence indicators, and composite risk features.
These features become the building blocks for current and future models.
Step 6: Develop and Operationalize AI Models
With features in place, we design the models that detect risk and support prediction. These may include anomaly detection, classification, forecasting, and segmentation models.
We train, validate, and benchmark them against real-world outcomes. We also define thresholds, alert rules, and clear “what happens next” pathways.
Every model is treated as a product. It has monitoring, retraining plans, and clear ownership.
Step 7: Integrate Insights Into Workflows
The next step is to make intelligence visible where it matters. We connect the platform to EHRs, telehealth tools, care management consoles, and population health systems.
Risk scores, trend summaries, and alerts appear alongside existing clinical data. We design views for different roles, such as clinicians, coordinators, and program managers.
The purpose is simple. Insights must be easy to understand and even easier to act on.
Step 8: Embed Governance, Security, and Compliance
In parallel, we work with security and compliance teams to embed controls across the platform. This covers access management, encryption, logging, and policy enforcement.
We document data flows, model usage, and consent handling so auditors and regulators have a clear view. We also agree on escalation paths for any security or data quality events.
These safeguards allow the platform to scale without increasing risk exposure.
Step 9: Launch, Measure, and Iterate
Finally, we roll out the platform in defined phases. We often begin with a focused cohort or program, then expand as results prove value.
We track operational metrics, clinical outcomes, user experience, and financial impact. Feedback drives adjustments to thresholds, workflows, and models.
Over time, the platform becomes a core part of how the organization monitors patients, controls risk, and designs new care models.
This step-by-step approach ensures that a wearable health data intelligence platform is not just deployed, but adopted and trusted. It connects strategy, technology, and frontline workflows into a single, governed system that can grow with the enterprise.
Cost to Build a Wearable Health Data Intelligence Platform
The cost to build a wearable health intelligence platform ranges from $50,000 to $150,000, depending on scope, data pipelines, AI depth, compliance needs, and integration complexity.
The investment required to build a wearable intelligence platform depends heavily on how focused the initial scope is. Costs rise when enterprises attempt multi-condition monitoring, hospital-wide deployment, or complex analytics in the first phase.
At Intellivon, we design these platforms around one high-impact clinical use case, delivered through a phased, governance-first approach. This keeps early investment predictable while ensuring the platform is scalable for future expansion.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost (USD) |
| Clinical & Business Discovery | Define use cases, patient cohorts, clinical risks, KPIs, care pathways | 8,000 – 15,000 |
| Architecture & Data Blueprint | Data pipeline design, sensor ecosystem planning, scalability and latency mapping | 10,000 – 20,000 |
| Device Integration & Ingestion Setup | APIs/SDKs, BLE/MQTT setup, normalization rules, data quality checks | 12,000 – 25,000 |
| AI Models & Risk Analytics | Early-warning models, anomaly detection, adherence scoring, feature engineering | 15,000 – 30,000 |
| Workflow Integration & UX | EHR/telehealth integration, dashboards, alert routing, clinician workflows | 8,000 – 15,000 |
| Governance, Security & Compliance | HIPAA controls, audit logging, access rules, consent handling | 6,000 – 10,000 |
| Testing & Clinical Validation | Model validation, safety checks, cross-functional review | 5,000 – 10,000 |
| Pilot Deployment & Training | Limited rollout, team onboarding, iteration cycles | 6,000 – 10,000 |
Total Initial Investment Range
USD 50,000 – 150,000
This supports a full wearable intelligence platform deployed for a focused program such as postoperative recovery monitoring, chronic disease management, or virtual ward enablement.
Annual Maintenance and Optimization Costs
Ongoing platform costs remain predictable when built on modular services and governed AI pipelines.
| Estimated Annual Cost | 12–18% of the initial build |
| Approx. USD 6,000 – 25,000 per year |
This covers infrastructure, device integration support, model recalibration, compliance updates, monitoring, and workflow optimization as usage grows.
Hidden Costs Enterprises Should Plan For
Even well-designed platforms introduce secondary costs as they scale across sites or programs. Enterprises should anticipate:
- Expanding into new monitoring use cases (CHF, COPD, diabetes, behavioral health)
- Supporting more hospitals, clinics, or home-based care networks
- Higher data volumes from long-term monitoring programs
- Additional model retraining as population behaviors evolve
- Compliance updates tied to HIPAA, FDA guidance, or algorithmic transparency
- Ongoing training for clinical teams as workflows mature
Planning for these early prevents unplanned budget surprises.
Best Practices to Stay Within Budget
Healthcare enterprises that control costs most effectively tend to:
- Start with one high-value, clinically validated use case
- Launch a controlled pilot before enterprise-wide expansion
- Use a modular architecture that supports plug-and-play model updates
- Embed compliance and governance from day one
- Track ROI within the first 60–120 days
- Align technology decisions with measurable clinical and financial outcomes
This approach ensures value is proven early, reducing financial and operational risk.
At Intellivon, we help healthcare enterprises build cost-controlled wearable intelligence platforms aligned with clinical priorities, regulatory expectations, and long-term scalability. Our phased approach minimizes upfront risk while creating a durable foundation for enterprise-wide continuous monitoring and AI-driven insight.
Overcoming Challenges in Building a Wearable Intelligence Platform
Enterprises face several barriers when building a wearable intelligence platform, like data noise, device fragmentation, workflow adoption, AI reliability, and compliance. Each challenge requires a structured, enterprise-first solution.
Building a wearable intelligence platform is not only a technical effort. Enterprises must address issues that affect clinical accuracy, operational flow, and long-term scalability. Below are the most common challenges and how a strategic partner can help overcome them.
1. Data Noise, Inconsistency, and Signal Gaps
Wearable data can be unreliable. Heart rate streams fluctuate, devices drop connections, and timestamps drift across vendors. These inconsistencies make it difficult for clinical teams to trust insights derived from raw signals.
Our team solves this by engineering strong ingestion rules, quality checks, and normalization pipelines that clean and structure every feed. Signals are corrected, aligned, and validated before they reach any analytical model. This gives enterprises dependable inputs and reduces the risk of misleading alerts.
2. Device Fragmentation
Healthcare environments often deal with multiple devices. Each one uses different APIs, data formats, and reliability profiles. Fragmentation creates integration overhead and increases operational complexity.
We address this by unifying all devices under a single ingestion framework. The platform supports diverse vendors while applying standardized rules, so organizations are not locked into one ecosystem. This flexibility reduces cost, simplifies onboarding, and strengthens long-term sustainability.
3. Limited Clinical Workflow Adoption
Even the best insights are useless if they do not reach the right teams in a usable format. Many platforms fail because clinicians must check separate dashboards or adapt to unfamiliar tools. This disrupts workflows and slows adoption.
We prevent this by integrating intelligence directly into existing systems, like EHRs, care coordination tools, and telehealth platforms. Alerts, summaries, and risk indicators appear naturally within daily workflows. This reduces cognitive load and increases trust among clinical teams.
4. AI Model Drift, Bias, and Reliability Concerns
Models fed by continuous signals face drift as patient behaviors, device usage, and environmental patterns shift over time. Enterprises also worry about bias, explainability, and inconsistent performance across populations.
We implement governed AI pipelines that monitor model behavior, track drift, and trigger retraining cycles when thresholds are exceeded. Documentation, lineage tracking, and transparent logic help teams understand why the model produced a particular output. This builds confidence and ensures regulatory readiness.
5. Compliance, PHI Protection, and Regulatory Alignment
Wearable signals flow through multiple systems and vendors, increasing exposure risk. Enterprises must protect PHI, enforce access controls, and meet HIPAA, GDPR, and evolving AI governance guidelines.
Our approach embeds compliance into each stage of the platform, from ingestion to storage to model outputs. Encryption, audit trails, consent controls, and role-based access ensure data remains secure and fully traceable. This reduces regulatory risk and supports long-term growth.
These challenges are real, but each one is solvable with the right architecture, workflow design, and governance. With a structured approach, enterprises can build a wearable intelligence platform that is accurate, scalable, trusted by clinicians, and ready for long-term expansion.
Conclusion
A wearable health intelligence platform strengthens early detection, improves care coordination, and empowers enterprises to operate with data-driven precision at a clinical scale.
Wearable data is only valuable when it becomes intelligence that teams can trust and act on. When enterprises bring together real-time ingestion, AI-driven insight, workflow integration, and strong governance, they create a foundation capable of transforming care delivery. Programs that once relied on episodic assessments gain continuous visibility. Clinical teams identify deterioration sooner. Organizations operate with clearer signals, fewer blind spots, and stronger outcomes.
Building this platform requires thoughtful decisions across architecture, compliance, and workflow design. However, the payoff is meaningful. A well-designed system improves quality measures, reduces unnecessary utilization, and supports modern care models such as hospital-at-home, virtual wards, and chronic disease programs.
Build A Wearable Health Data Intelligence Platform With Intellivon
At Intellivon, we build enterprise-grade wearable health intelligence platforms that transform continuous sensor data into reliable clinical insight. Our systems unify data from wearables, medical-grade sensors, remote monitoring tools, EHRs, care management systems, and AI models into a single governed intelligence layer that strengthens early detection, proactive outreach, and clinical decision-making without disrupting existing workflows.
Each platform is engineered for modern healthcare enterprises. Solutions are compliant by design, resilient under real-time data load, interoperable across device ecosystems, and built to deliver measurable improvements in patient outcomes, operational efficiency, and value-based performance from the earliest deployment phases.
Why Partner With Us?
- Compliance-First Continuous Monitoring: Every deployment aligns with HIPAA, GDPR, where applicable, FDA guidance on device data and clinical decision support, and emerging AI governance standards, with full auditability across data pipelines and model outputs.
- Workflow-Native Clinical Intelligence: Risk scores, adherence indicators, anomaly alerts, and recovery trends surface directly inside existing EHR, telehealth, and care coordination environments, allowing teams to act without switching systems or adding operational friction.
- Predictive and Context-Aware AI Models: Our models analyze heart rate variability, sleep cycles, mobility patterns, and recovery trajectories to flag early deterioration, forecast instability, and highlight rising-risk cohorts with strong clinical context and transparency.
- Device-Agnostic Architecture: We integrate across consumer wearables, clinical-grade devices, remote monitoring kits, and vendor-specific clouds, ensuring flexibility without forcing enterprises into a single ecosystem or hardware standard.
- Scalable Monitoring Across Programs: The same platform supports postoperative care, chronic disease management, virtual wards, and population health initiatives without duplicating infrastructure, data pipelines, or governance layers.
- Zero-Trust Security and PHI Protection: End-to-end encryption, identity-first access, continuous audits, and real-time monitoring protect sensitive physiological signals and ensure the platform remains secure as it scales across teams and regions.
Book a strategy call to explore how a wearable health data intelligence platform can enhance early detection, reduce avoidable utilization, and power the next generation of continuous, AI-enabled care across your healthcare enterprise.
FAQs
Q1. What is a wearable health data intelligence platform?
A1. It is an enterprise system that collects, standardizes, and analyzes continuous signals from wearables and medical sensors. The platform converts raw physiological data into actionable insights that support early detection, proactive outreach, and large-scale care delivery. It integrates with EHRs, telehealth tools, and care management systems so teams can use insights inside their existing workflows.
Q2. How do wearable intelligence platforms help in early risk detection?
A2. These platforms use machine learning to analyze heart rate, activity, sleep, and recovery trends. They identify subtle deviations that often appear days before symptoms surface. This allows clinical teams to intervene earlier, reduce avoidable deterioration, and improve patient safety across inpatient, outpatient, and home-based care programs.
Q3. What are the key technical components needed to build this platform?
A3. A mature solution includes real-time ingestion pipelines, a governed data lakehouse, AI analytics, interoperability layers, clinical dashboards, and strong security controls. Together, these components allow enterprises to process data at scale, deliver reliable insights, and maintain full compliance with HIPAA and other regulations.
Q4. How much does it cost to develop a wearable health data intelligence platform?
A4. The initial investment typically ranges from $50,000 to $150,000, depending on scope, device integrations, workflow complexity, and AI depth. Costs remain predictable when the platform is built with modular architecture, phased deployment, and governance-first engineering.
Q5. How do healthcare organizations integrate wearable insights into clinical workflows?
A5. Integration happens through secure APIs that push risk scores, alerts, and summaries into EHRs, care management platforms, and telehealth systems. This ensures insights appear where clinicians already work, reducing workflow friction and improving adoption. The platform supports role-based views so each care team member receives actionable information without switching tools.