When a healthcare provider uses Epic, they do not want to switch to another system. Epic acts as the clinical backbone, holding patient records, managing workflows, and keeping operations running across the entire organization. Hence, this foundation is secure. However, as enterprises grow by adding facilities, launching new services, and expanding to different areas, challenges arise. Specialized clinics require workflows that Epic wasn’t designed to support. Meanwhile, data science teams struggle to get analytics quickly. In these cases, patient-facing apps seem outdated compared to consumer expectations in 2025.
These are complexities that arise in enterprise environments, not failures of Epic. When IT leaders hear about “Epic customization,” they often think of risky, costly changes that make upgrades harder and invalidate vendor support agreements. At Intellivon, Epic customization means building software that works with Epic, not within it.
Our specialized approach enhances Epic’s capabilities through governed integrations and custom applications that run alongside the EHR. This delivers flexibility and speed without interfering with Epic’s core or compromising compliance. This blog explains how our experts approach Epic-compatible customization in practice.
Key Takeaways Of The Healthcare Software Market
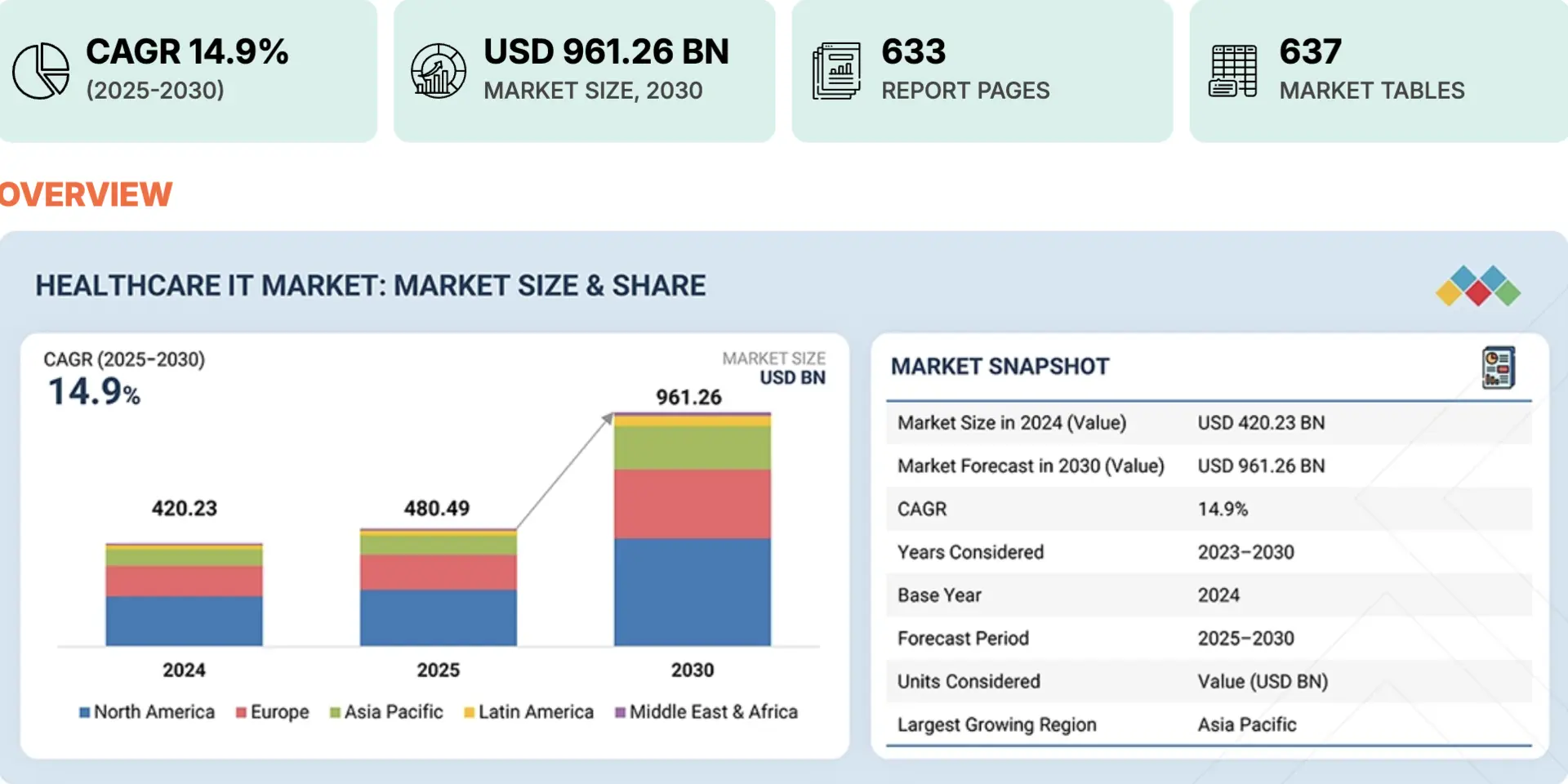
The global healthcare information technology market is expanding rapidly as providers invest in digital systems for clinical, operational, and patient engagement use cases.
According to recent forecasts, the healthcare IT market is projected to grow from roughly USD 420 billion in 2024 to nearly USD 961 billion by 2030, at a compound annual growth rate of about 14.9 %.
Market Insights:
- Enterprise healthcare software is outpacing core EHR growth. Healthcare enterprise software is expected to reach $110B+ by 2032, growing at 13.5% CAGR, as providers invest in custom workflows, analytics, and integrations around EHRs.
- EHR adoption is mature, shifting focus to optimization. The global EHR market will grow from $34B (2023) to $64B by 2032, signaling saturation and a shift toward extending existing platforms like Epic rather than replacing them.
- Many enterprise EHR integration projects see positive ROI within 12–24 months, driven by reduced admin costs, fewer billing errors, faster reimbursements, and improved operational workflow efficiency.
- Cloud integration initiatives report strong financial returns, with some enterprises achieving up to 295% ROI over three years and payback in six months through improved efficiency and reduced silos.
Epic has become the digital backbone for many large healthcare organizations. As care models expand and operational complexity increases, the ability to extend Epic safely and intelligently becomes a strategic necessity.
Epic-compatible software customization offers a controlled path to scale, innovation, and measurable return without compromising stability or compliance.
Why Epic-Based Enterprises Still Require Custom Software
Epic provides a reliable foundation for clinical and administrative operations. However, enterprise healthcare environments evolve continuously. As organizations expand across facilities, regions, and care models, operational complexity increases.
Consequently, new requirements emerge that extend beyond what any single EHR platform is designed to handle alone. Custom software becomes the practical way to adapt without destabilizing Epic.
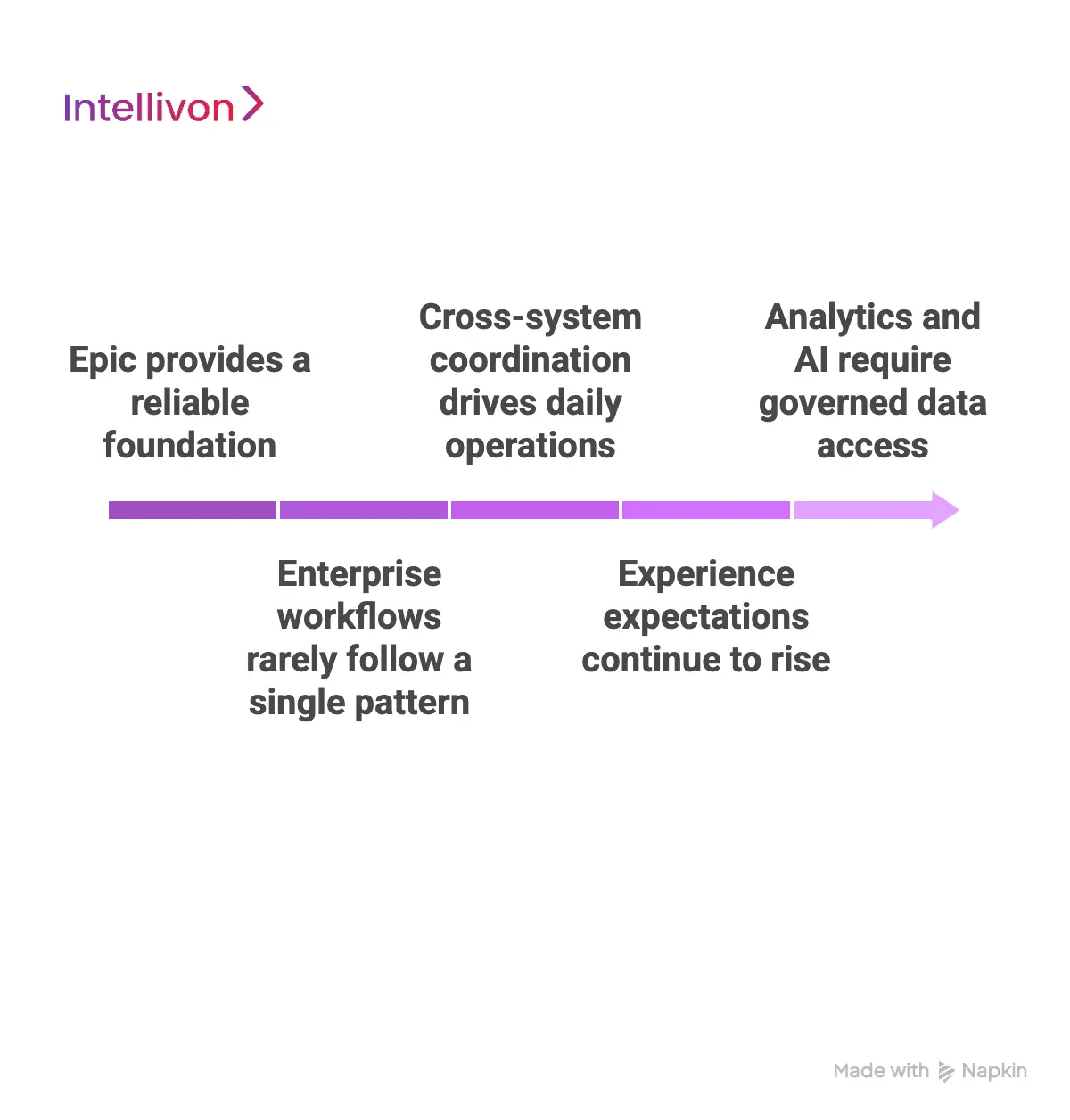
1. Enterprise workflows rarely follow a single pattern
Epic supports standardized workflows by design. However, large healthcare enterprises operate across specialties, geographies, and regulatory frameworks. As a result, approval paths, documentation flows, and operational handoffs vary significantly.
Custom software allows enterprises to reflect these realities accurately. Therefore, teams avoid workarounds that slow execution and introduce risk.
2. Cross-system coordination drives daily operations
Modern healthcare delivery depends on multiple systems working together. Imaging platforms, labs, billing tools, and partner networks must remain aligned. While Epic anchors clinical data, it cannot orchestrate every external dependency alone.
For this reason, enterprises rely on custom software to coordinate workflows across systems. In addition, this approach preserves Epic’s role as the system of record.
3. Experience expectations continue to rise
Patients and providers expect simple, responsive digital experiences. However, native interfaces often struggle to support differentiated needs at scale. As care models diversify, experience gaps become more visible.
Custom software enables enterprises to design experiences aligned with their brand and workflows. Meanwhile, Epic continues to manage core data and transactions.
4. Analytics and AI require governed data access
Enterprise decision-making increasingly depends on analytics and AI. These capabilities require structured, reliable access to operational and clinical data. However, analytics workloads should not sit inside the EHR interface.
Therefore, custom software creates governed data pipelines that support insights, automation, and forecasting. At the same time, data integrity and compliance remain intact.
Epic remains central to enterprise healthcare operations. However, custom software supports everything that surrounds it. When designed correctly, it enables scale, integration, and innovation while keeping Epic stable, trusted, and in control.
What “Epic-Compatible Customization” Really Means
Epic-compatible customization is frequently misunderstood in enterprise healthcare discussions. Many assume it involves altering Epic or forcing nonstandard behavior into the EHR. In reality, it follows a disciplined architectural approach.
It focuses on extending enterprise capabilities while leaving Epic untouched and authoritative. This distinction defines whether customization becomes an asset or a long-term risk.
1. Epic-compatible vs Epic-modifying customization
Epic-compatible customization and Epic-modifying approaches differ fundamentally in intent, risk, and sustainability.
| Aspect | Epic-Compatible Customization | Epic-Modifying Approach |
| Interaction with Epic | Uses approved APIs and standards | Alters internal workflows or logic |
| Impact on upgrades | Remains stable across upgrades | High risk of breakage |
| Compliance posture | Governance-first and auditable | Difficult to audit consistently |
| Data ownership | Epic remains the system of record | Risk of duplicate or conflicting data |
| Enterprise scalability | Designed to scale independently | Becomes brittle at scale |
| Long-term viability | Sustainable and supportable | Operationally risky |
As a result, enterprises consistently choose compatibility over modification to protect stability and control.
2. What can be built, integrated, and extended
Epic-compatible customization enables enterprises to address needs that sit beyond the EHR interface. These solutions operate externally but remain tightly aligned with Epic data and workflows. Therefore, flexibility increases without increasing operational risk.
Common examples include:
- Patient engagement platforms connected to Epic schedules and records
- Provider workflow tools triggered by Epic events
- Care coordination and referral management systems
- Analytics and AI platforms are consuming Epic clinical data
- Integration layers connecting Epic with finance, labs, and partners
Each solution extends Epic’s value while preserving its role.
3. Where custom software sits architecturally
Custom software operates as an enterprise layer outside Epic. It communicates through governed interfaces and event-driven connections. This separation is intentional and strategic. It allows systems to evolve without destabilizing the EHR.
Typically, this layer:
- Reads and writes data through approved interfaces
- Applies business logic outside Epic
- Orchestrates workflows across multiple systems
- Scales independently of Epic performance
As a result, agility and reliability coexist.
4. Why Epic remains authoritative at all times
Epic continues to serve as the system of record. Clinical truth, encounters, and orders originate and resolve within Epic. Custom software never overrides this authority. Instead, it acts on Epic data under strict governance.
This approach ensures:
- No conflicting patient records
- Clear audit trails
- Predictable upgrade behavior
- Strong regulatory alignment
Epic-compatible customization is not about changing Epic. It is about building enterprise software that complements it, respects its boundaries, and enables healthcare organizations to scale safely and intelligently.
Epic at Enterprise Scale: 325M Records and 45B Monthly Exchanges
Epic operates at a scale few healthcare platforms reach. With hundreds of millions of patient records and billions of data exchanges every month, Epic functions as the digital backbone of large healthcare ecosystems.
At this level, extension and interoperability stop being optional. Instead, they become structural requirements for operating efficiently across complex enterprises.
1. Epic’s footprint makes extension unavoidable
Epic supports 325 million active patient records across providers, payers, and care networks. At this scale, no single platform can address every workflow, reporting need, or experience expectation.
Enterprises rely on Epic-compatible software to support specialized operations while preserving Epic as the system of record.
2. Interoperability now outweighs core UI usage
Epic processes 45+ billion data messages each month across 60,000+ active interfaces. This volume shows where enterprise value is concentrated.
Data constantly moves between Epic and external platforms for analytics, coordination, billing, and automation. Custom Epic-compatible systems provide governance and control over this exchange.
Epic’s scale reinforces a clear reality. Enterprise performance depends on how effectively Epic is extended and governed across the broader healthcare ecosystem.
Common Enterprise Use Cases for Epic-Integrated Custom Software
As healthcare organizations grow, Epic continues to anchor clinical data and core workflows. However, many enterprise needs sit outside the EHR interface. These needs involve coordination, experience, and intelligence across systems.
Epic-integrated custom software fills this gap by extending Epic’s value without disrupting its role as the system of record.
1. Patient engagement beyond native portals
Epic provides strong foundational patient access. However, enterprises often require experiences tailored to specific populations, service lines, or care programs.
Custom engagement platforms integrate with Epic schedules, records, and messaging while offering flexibility in design and functionality. As a result, organizations improve access and satisfaction without fragmenting patient data.
2. Provider workflow acceleration tools
Clinicians and staff face an increasing administrative load. While Epic manages core clinical tasks, many operational steps happen before or after EHR interaction.
Custom tools help automate intake, approvals, handoffs, and follow-ups. Therefore, providers spend less time navigating systems and more time delivering care.
3. Care coordination and referral management
Enterprise care delivery spans hospitals, clinics, partners, and post-acute services. Coordination across these entities is complex and often manual. Epic-integrated coordination platforms track referrals, transitions, and care plans across systems.
Consequently, enterprises reduce delays, close gaps in care, and maintain visibility without duplicating records.
4. Enterprise analytics and reporting platforms
Leadership teams rely on timely insights to guide decisions. However, advanced analytics should not run inside the EHR interface.
Custom analytics platforms consume Epic data through governed pipelines. In addition, they combine it with operational and financial data. This approach supports forecasting, performance tracking, and population health initiatives.
5. AI and automation layers
AI initiatives require structured, reliable data access. Epic supplies trusted clinical data, but AI execution often lives outside the EHR.
Custom software enables automation, decision support, and predictive models that operate alongside Epic. Meanwhile, governance ensures compliance and transparency remain intact.
Epic-integrated custom software supports the work that happens around the EHR. These use cases allow enterprises to scale operations, improve experience, and unlock intelligence while keeping Epic stable and authoritative.
Real-World Examples of Epic-Compatible Custom Software
Epic-compatible customization becomes clearer when viewed through real deployments. Large healthcare enterprises already rely on external applications that integrate tightly with Epic while keeping its core untouched.
These platforms solve specific operational and clinical problems that sit outside the EHR interface. Together, they show how extension works safely at enterprise scale.
1. Kyruus ProviderMatch
Kyruus ProviderMatch integrates with Epic scheduling, provider, and location data. It helps patients find the right provider based on specialty, availability, and care needs. As a result, enterprises improve access and reduce leakage without changing Epic scheduling logic.
2. Twistle (Health Loop)
Twistle, formerly Health Loop, connects to Epic encounters and care plans. It automates follow-ups, reminders, and education after visits or procedures. Therefore, care teams stay connected with patients while Epic continues to manage clinical records.
3. CarePort
CarePort integrates with Epic to manage referrals and post-acute transitions. It tracks patient movement across hospitals, skilled nursing facilities, and home care providers. Consequently, enterprises gain visibility into outcomes and reduce delays without duplicating data.
4. Voalte One
Voalte One integrates with Epic patient context to support secure messaging and alerts. Care teams communicate faster while remaining aligned to patient records. Meanwhile, Epic remains the system of record for clinical activity.
5. PatientPing
PatientPing connects Epic data with real-time admission, discharge, and transfer events. Care teams receive timely notifications across facilities and partners. As a result, coordination improves without altering Epic workflows.
6. Redox
Redox acts as a governed integration layer between Epic and custom enterprise applications. It normalizes data exchange and manages connectivity at scale. Therefore, enterprises reduce integration complexity while keeping Epic stable.
These real-world examples show how Epic-compatible custom software operates in practice. Each platform extends Epic’s reach, supports specialized enterprise needs, and preserves Epic’s authority. Together, they demonstrate how customization succeeds when guided by architecture, governance, and clear boundaries.
Epic Integration Models Used in Enterprise Custom Development
Enterprise healthcare systems integrate with Epic in different ways, depending on risk tolerance, scale, and use case. There is no single integration model that fits every need.
Instead, successful organizations choose models that balance flexibility with governance. Epic-compatible integration focuses on stability, auditability, and long-term sustainability.
1. FHIR and SMART on FHIR applications
FHIR-based integrations are widely used for modern Epic extensions. These applications read and write structured data using standardized APIs. SMART on FHIR apps also run inside Epic workflows with proper authorization.
As a result, enterprises enable real-time interactions while keeping data access governed and predictable.
2. Epic App Orchard applications
Epic App Orchard provides a controlled environment for third-party and custom apps. Applications listed here meet Epic’s security and interoperability standards.
Therefore, enterprises gain confidence that integrations will remain stable through upgrades. App Orchard is often used for patient engagement, scheduling, and care coordination tools.
3. Backend API and data feed integrations
Some enterprise use cases require backend connectivity rather than user-facing apps. These integrations pull data from Epic using approved APIs or data feeds. They support analytics, reporting, and operational workflows. In addition, they reduce UI complexity for clinicians and staff.
4. Event-based and real-time data synchronization
Event-driven integrations react to changes inside Epic, such as admissions or orders. Custom systems respond automatically when these events occur.
Consequently, enterprises improve responsiveness across care coordination and operations. This model supports real-time decision-making without manual intervention.
5. Read and write boundaries with governance controls
Not all integrations require full write access. Enterprises carefully define when external systems can read from Epic and when they can write back. Governance policies control these boundaries. Therefore, data integrity and compliance remain intact across systems.
Epic integration models vary, but the goal remains consistent. Enterprises extend Epic’s capabilities while protecting its stability. When integration choices are made deliberately, custom development supports scale, compliance, and long-term success.
Compliance, Security, and Epic Governance Considerations
Compliance and security are not secondary concerns in Epic-integrated development. They shape every architectural and delivery decision. Enterprise healthcare organizations operate under strict regulatory scrutiny.
Therefore, Epic-compatible customization must be designed with governance in mind from the start and not added later.
1. Regulatory compliance sets the baseline
Healthcare systems must comply with HIPAA and related privacy regulations. Data access, storage, and transmission require clear controls. Custom software must align with these requirements at all times. As a result, compliance considerations influence integration methods, data flows, and system boundaries.
2. Epic API governance defines what is allowed
Epic enforces clear rules around how its APIs can be used. These rules protect data integrity and system stability. Enterprises must design integrations that follow Epic’s approved patterns. Therefore, customization succeeds only when it respects Epic’s governance framework.
3. Auditability and traceability are mandatory
Enterprise environments require full visibility into data movement. Every access, update, and transaction must be traceable. Custom software must maintain logs and audit trails aligned with Epic activity. Consequently, organizations can respond confidently to audits and internal reviews.
4. Security controls extend beyond the EHR
Security does not stop at Epic’s boundary. External platforms must implement role-based access, identity controls, and encryption. In addition, security reviews and risk assessments are often required before deployment. This ensures consistent protection across the ecosystem.
Compliance and governance define whether Epic-compatible customization succeeds or fails. When security, auditability, and policy alignment are built in from the beginning, enterprises gain flexibility without increasing risk.
How We Build Epic-Compatible Custom Software
Epic-compatible custom software cannot be built in fragments. It requires a structured, compliance-led process that respects Epic’s role while enabling enterprise flexibility.
Our approach focuses on clarity first, execution second, and long-term stability throughout. This ensures solutions scale without creating technical or regulatory debt.

Step 1: Define goals and boundaries
Every engagement starts with understanding what the organization is trying to achieve. We work with business and operational teams to identify outcomes tied to access, efficiency, coordination, or intelligence. At the same time, we define clear boundaries around Epic’s role as the system of record.
This includes identifying which data stays authoritative in Epic and which workflows operate externally. Security, compliance, and governance constraints are established early. As a result, the project begins with shared alignment rather than assumptions.
Step 2: Map workflows and data flows
Next, we map how work actually happens across teams and systems. This includes clinical steps, operational handoffs, and decision points that sit before or after Epic interaction. We also trace how data moves in and out of Epic today.
Therefore, gaps, delays, and duplication become visible. This step ensures custom software supports real workflows instead of idealized ones. It also prevents building features that conflict with existing processes.
Step 3: Choose the right integration model
Not every use case needs the same type of integration. We evaluate whether the solution requires FHIR APIs, App Orchard apps, backend integrations, or event-driven triggers. Read and write access is carefully assessed.
In addition, the governance requirements guide which model is safest. This prevents over-engineering while maintaining control. As a result, integration choices remain purposeful and compliant.
Step 4: Design the enterprise software layer
Custom software is designed as an external enterprise layer that connects to Epic through approved interfaces. Business logic, orchestration, and user experience live outside the EHR. This separation protects Epic’s stability.
Meanwhile, the custom layer can evolve independently as needs change. Scalability, performance, and fault tolerance are built in from the start. Therefore, growth does not introduce fragility.
Step 5: Build with compliance and security built in
Development follows healthcare security and compliance standards throughout. Access controls, identity management, and encryption are applied consistently. Audit trails are designed to align with Epic activity.
Testing includes security validation and governance checks, not just functionality. As a result, solutions are ready for enterprise scrutiny from day one. Compliance is treated as a foundation, not a final step.
Step 6: Test, deploy, and govern continuously
Before launch, integrations are tested against real workflows and Epic upgrade scenarios. Deployment follows controlled rollout plans to minimize disruption. After go-live, governance processes manage updates, monitoring, and change.
Feedback loops help refine workflows without breaking integrations. Therefore, the solution remains stable as Epic and enterprise needs evolve.
Epic-compatible custom software succeeds when built with structure and intent. A step-by-step, governance-led approach ensures flexibility without sacrificing control. This allows healthcare enterprises to innovate confidently while keeping Epic stable, authoritative, and secure.
Cost of Building Epic-Compatible Custom Software
Epic-compatible patient engagement platforms require a very different cost lens than basic engagement tools. The platform must operate reliably within Epic workflows while supporting scale across hospitals, regions, and care models. Therefore, architecture decisions account for workflow integrity, identity governance, consent enforcement, compliance controls, and long-term interoperability risk from the start.
At Intellivon, budget flexibility is handled deliberately. The scope can be adjusted when constraints exist. However, core foundations are never compromised. These include Epic workflow alignment, identity and proxy access, auditability, and operational reliability.
Estimated phase-wise cost breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Epic workflow mapping | Engagement use cases, Epic workflow alignment, operational, and compliance assessment | $7,000 – $12,000 |
| Platform architecture design | Layered platform design, Epic integration approach, scalability planning | $9,000 – $16,000 |
| Identity, consent & governance | Proxy access, role-based access, consent logic, audit workflows | $9,000 – $15,000 |
| Core engagement platform development | Scheduling flows, messaging, portals, and care plan engagement logic | $18,000 – $30,000 |
| Epic integrations | Scheduling, encounters, messaging, results, and billing touchpoints | $16,000 – $28,000 |
| Role-based interfaces | Patient, caregiver, admin, operations, support interfaces | $9,000 – $15,000 |
| Security & compliance controls | Encryption, access control, audit trails, and monitoring | $10,000 – $16,000 |
| Testing & validation | Workflow testing, security validation, and enterprise readiness | $7,000 – $11,000 |
| Deployment & scale readiness | Cloud or hybrid setup, performance tuning, and monitoring | $8,000 – $14,000 |
Total initial investment: $93,000 – $187,000
Ongoing maintenance and optimization: 15–20% of the initial build per year
Hidden costs enterprises should plan for
Even well-scoped Epic-compatible programs face pressure when indirect costs are ignored. Planning for these early protects both the budget and the timelines.
- Integration complexity grows as new Epic modules, sites, or workflows are added
- Compliance overhead increases with audits, privacy reviews, and policy updates
- Governance requires continuous tuning of consent and proxy access models
- Infrastructure costs rise with analytics, real-time engagement, and AI usage
- Change management includes onboarding clinical, IT, and operations teams
- Continuous monitoring becomes critical as engagement volume increases
Best practices to avoid budget overruns
Based on experience delivering enterprise healthcare platforms, several practices consistently lead to controlled costs and predictable outcomes.
- Define Epic workflows and engagement triggers before expanding features
- Embed governance, identity, and auditability into the core platform design
- Use modular components that scale without redesign
- Plan Epic integrations early to avoid costly retrofitting
- Maintain visibility across performance, security, and compliance metrics
- Design for ongoing Epic updates, not one-time alignment
Request a tailored proposal from Intellivon’s healthcare platform experts to receive a delivery roadmap aligned with your budget, Epic environment, and long-term patient engagement strategy.
Conclusion
Epic has become the backbone of enterprise healthcare operations. However, long-term success depends on how effectively it is extended, not replaced. Epic-compatible custom software allows organizations to adapt workflows, improve engagement, and unlock data without compromising stability or compliance. When customization is approached with clear boundaries and governance, it reduces risk instead of creating it.
This is not a short-term technology decision. It is an enterprise strategy that affects operations, experience, and growth. Platforms built with intent scale across regions, support evolving care models, and remain stable through Epic upgrades. With the right partner and a disciplined approach, Epic-compatible customization becomes a foundation for sustainable innovation and measurable return.
Build Epic-Compatible Enterprise Software With Intellivon
At Intellivon, Epic-compatible enterprise software is built as a regulated healthcare infrastructure, not as custom layers bolted onto Epic. Every architectural and delivery decision prioritizes workflow integrity, data authority, identity governance, and compliance from day one. This ensures enterprise platforms operate reliably within Epic environments, not just during initial deployment.
As enterprise programs expand across hospitals, regions, and care models, stability becomes non-negotiable. Governance, performance, and audit readiness remain consistent as integration volume, data access, and operational complexity increase. Organizations retain control over workflows, data flows, and compliance obligations without introducing fragmentation, upgrade risk, or long-term rework.
Why Partner With Intellivon?
- Enterprise-grade platform architecture designed for Epic-governed healthcare environments
- Proven delivery across Epic-connected health systems, multi-site networks, and regulated enterprises
- Compliance-by-design approach covering identity, consent, auditability, and access control
- Secure, modular architecture supporting cloud, hybrid, and on-prem deployments
- AI-ready foundations enabling analytics, automation, and intelligent workflows with governance and oversight
Book a strategy call to explore how Intellivon can help you build and scale Epic-compatible enterprise software with confidence, control, and long-term operational value.
FAQs
Q1. What does Epic-compatible software customization mean?
A1. Epic-compatible software customization refers to building external enterprise applications that integrate with Epic using approved interfaces. These solutions extend workflows and capabilities without modifying Epic’s core system or data model.
Q2. Does Epic-compatible customization require changing Epic itself?
A2. No. Epic-compatible customization does not involve altering Epic’s internal code or workflows. Epic remains the system of record, while custom software operates alongside it using governed APIs and integration standards.
Q3. What types of enterprise software can integrate with Epic?
A3. Enterprises commonly build patient engagement platforms, care coordination systems, analytics layers, AI automation tools, and integration hubs. All of these can integrate with Epic while preserving compliance and operational stability.
Q4. How do Epic upgrades affect custom integrated software?
A4. When built correctly, Epic-compatible software remains stable through upgrades. Because integrations rely on approved APIs and governance models, enterprises avoid rework or disruption during Epic version changes.
Q5. Is Epic-compatible custom software secure and compliant?
A5. Yes. When designed with identity management, consent enforcement, audit trails, and access controls, Epic-compatible software meets enterprise security and regulatory requirements, including HIPAA and internal governance standards.