An AI healthcare app serves as essential operational infrastructure for enterprise healthcare organizations. It shapes how care is delivered, managed, and expanded. However, most discussions still center around features, algorithms, or interfaces. This viewpoint is becoming outdated.
The real challenge today is not around how capable an AI healthcare app is. Instead, it focuses on keeping those capabilities clinically sound, approved by regulators, financially responsible, and able to work seamlessly across complex healthcare systems. This challenge becomes even greater as healthcare and financial systems start to merge. AI healthcare apps are now crucial to both clinical workflows and financial operations, covering areas from claims automation to consent enforcement. Therefore, developing such an app also involves the proper platform and governance choices.
At Intellivon, we design AI healthcare apps as enterprise-grade healthcare platforms. Here, AI, compliance, interoperability, and financial governance come together. In this blog, we will draw from our experience to discuss how to build such an app from the ground up and scale it in enterprise-level environments.
Why Businesses Are Investing In AI Healthcare Apps
The growing emphasis on compliance is shaping how AI healthcare apps are being designed at the enterprise level.
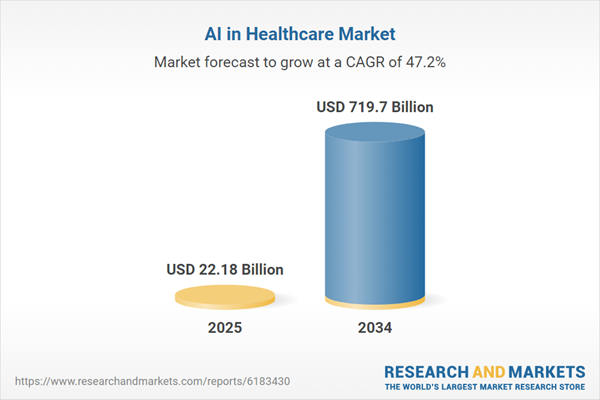
According to Research and Markets, the AI in healthcare market is entering a phase of exponential growth. In 2025, it is valued at USD 22.18 billion. By 2034, it is expected to reach USD 719.7 billion, expanding at a CAGR of 47.2%.
This reflects a deeper shift in how healthcare organizations view digital platforms. Enterprises now expect AI-powered systems to manage privacy, automate governance, and reduce operational exposure by design.
Market Growth Drivers:
- Emerging frameworks such as the 2025 HIPAA Security Rule are accelerating this shift. As digital health ecosystems become more interconnected, compliance can no longer be treated as a layer added after deployment.
- Enterprises are adopting AI to manage data growth, clinician shortages, and rising costs, enabled by advances in diagnostics, ambient documentation, and virtual care integration.
- Early pilots show 30–50% reductions in documentation workload and 10–20% cost savings, especially in high-friction areas like prior authorization and imaging.
The ROI case for AI healthcare apps is becoming increasingly concrete for enterprises. Organizations now report 15–25% faster revenue cycle processing and 20–35% improvements in claims accuracy, which directly strengthens financial performance.
In parallel, AI-led care coordination and predictive interventions are driving 10–18% reductions in avoidable readmissions, improving both outcomes and cost efficiency.
At the same time, large-scale investments indicate where the market is heading. Leaders such as IBM, Oracle (Cerner), and Philips now hold major positions across AI healthcare platforms. Moreover, around 78% of organizations already use AI across core functions, while healthcare itself is growing at a 36.8% adoption CAGR.
What Is An Enterprise AI Healthcare App?
An enterprise AI healthcare app is a regulated digital platform that uses AI to support clinical and operational workflows while ensuring compliance, security, and scalability.
An enterprise AI healthcare app is a core business system used by healthcare organizations to deliver, manage, and govern care at scale. These platforms support real clinical and administrative workflows. For example, they assist with diagnosis, automate documentation, manage claims, and coordinate care across departments.
However, what truly defines them is not intelligence alone. It is their ability to operate reliably under strict regulatory, security, and performance requirements. They integrate with existing hospital systems, protect sensitive patient data, and generate audit-ready records by design.
As a result, enterprise AI healthcare apps function as long-term infrastructure. They are built to scale across regions, teams, and use cases without increasing compliance or operational risk.
Consumer AI apps vs enterprise AI healthcare platforms
To understand why enterprise AI healthcare apps require a different design approach, it helps to compare them with consumer health apps. While both may use AI, they serve very different purposes and operate under very different constraints.
| Aspect | Enterprise AI Healthcare App | Consumer Health App |
| Primary purpose | Supports core clinical and operational workflows | Supports personal health tracking or wellness |
| Users | Clinicians, administrators, payers, care teams | Individual patients or consumers |
| Regulatory scope | Must comply with HIPAA, GDPR, audit, and reporting standards | Limited or no regulatory obligations |
| Data sensitivity | Handles protected health and financial data | Handles mostly personal or non-clinical data |
| Integration needs | Deep integration with EHRs, labs, and billing systems | Minimal or no enterprise integration |
| AI accountability | Requires explainability, traceability, and oversight | Rarely requires formal AI governance |
| Scalability expectations | Designed for multi-region and multi-system deployment | Designed for individual or small user bases |
| Risk tolerance | Very low tolerance for failure or downtime | Higher tolerance for feature or service issues |
Enterprise AI healthcare apps carry legal, clinical, and financial responsibility. Therefore, they must be engineered as long-term platforms, not short-lived products.
As a result, organizations that treat enterprise AI healthcare apps like consumer software often face compliance gaps, scaling failures, and operational risk. Building with the enterprise context in mind is what enables sustainable and defensible digital healthcare growth.
Which AI Healthcare App Use Cases Deliver Measurable ROI?
AI healthcare apps deliver measurable ROI when embedded into high-friction workflows tied directly to revenue protection, labor efficiency, and compliance performance.
Therefore, enterprises must prioritize use cases that intersect with revenue, cost, and regulatory outcomes. This shift moves AI from experimentation into defensible business value.
1. Claims and Billing Automation
Revenue leakage remains one of the most persistent problems in healthcare operations. AI healthcare apps that automate claims processing, document extraction, and coding validation directly reduce manual errors and administrative load.
Research on AI-driven claims processing shows reductions of up to 30–40% in manual handling time and meaningful improvements in first-pass claim accuracy
As a result, organizations shorten billing cycles and stabilize cash flow. Over time, this strengthens financial resilience without increasing operational overhead.
2. Clinical Documentation and Ambient Scribing
Physician time is one of the most constrained and expensive resources in healthcare. AI-assisted documentation has demonstrated measurable productivity gains in real environments. Studies linked to Stanford show ambient AI scribes can save 11–20 minutes per clinician per day, which compounds into thousands of hours annually.
Moreover, The Permanente Medical Group reported over 15,000 clinician hours saved in one year using AI scribing. Therefore, these systems directly improve throughput while reducing burnout-related attrition.
3. Prior Authorization and Utilization Review
Prior authorization continues to be a major source of delay and administrative friction. AI healthcare apps can analyze historical approvals, payer rules, and clinical context to streamline this process.
In mature deployments, organizations report 40–60% faster authorization turnaround times through AI-assisted workflows. Consequently, treatment delays drop while administrative workload decreases. This improves both operational efficiency and patient experience.
4. Imaging and Diagnostic Decision Support
AI applied to imaging improves detection speed and diagnostic consistency. Its financial impact becomes visible through lower repeat scan rates and faster downstream care. Enterprise deployments have shown 10–20% reductions in repeat imaging and measurable improvements in radiology throughput
As a result, organizations improve asset utilization without expanding equipment or staffing. This allows imaging operations to scale sustainably.
5. Fraud, Waste, and Compliance Monitoring
Fraud and compliance failures carry both financial and reputational risk. AI healthcare apps continuously monitor transactions and records for anomalies across clinical and financial systems.
Large healthcare networks using AI-based monitoring report millions in annual cost avoidance through earlier detection of irregularities. Moreover, compliance teams gain audit-ready visibility without relying on manual controls. Over time, this lowers the cost of governance while improving regulatory defensibility.
AI healthcare apps deliver ROI when applied to workflows that already carry financial, operational, or regulatory friction. However, success depends less on model sophistication and more on how deeply AI integrates into enterprise operations.
What $10M-Plus Breaches Reveal About the Future of AI Healthcare Apps
$10M-plus healthcare breaches show that AI health platforms must treat compliance as engineering infrastructure, not documentation, to remain financially and operationally viable.
1. Why HIPAA Has Become an Engineering Problem
HIPAA compliance now shapes how AI health platforms are designed from the ground up. According to IBM’s 2025 Cost of a Data Breach Report, the average U.S. healthcare breach costs $10.22 million. Therefore, every architectural decision directly influences financial exposure and platform stability.
As a result, compliance has become a core enterprise design constraint rather than a legal afterthought.
2. How Breaches Now Disrupt Care
Breaches today interrupt care delivery and not just data access. They delay clinical services, strain operations, and weaken patient trust. Consequently, cybersecurity is now inseparable from patient safety.
The Change Healthcare attack demonstrated this clearly, as one missing control disrupted EHRs, imaging, and payments across hundreds of hospitals.
3. Why Regulatory Expectations Are Tightening
Regulators are removing flexibility in compliance interpretation. The proposed 2025 HIPAA Security Rule makes safeguards such as encryption and MFA mandatory. At the same time, FDA AI guidance now requires threat modeling before AI enters production.
Therefore, AI platforms must demonstrate regulatory readiness alongside innovation.
4. Where Privacy and Performance Must Be Designed Together
AI platforms must protect sensitive data while enabling real-time intelligence. This balance is only possible when security is embedded directly into data pipelines.
When security is added later, performance often suffers. But when it is built in, compliant intelligence scales reliably.
5. Why Continuous Governance Is Now the Enterprise Baseline
Compliance now evolves with the platform. Regulators expect governance to move at the pace of DevOps. As a result, compliance has become an ongoing operational discipline, not static documentation.
Downtime now creates clinical risk. During outages, hospitals lose thousands per minute. Consequently, AI healthcare apps must be designed for rapid recovery through redundancy and restoration.
What Is The Architecture Of An AI Healthcare App?
An AI healthcare app requires a layered architecture that connects data, workflows, AI services, and governance so insights remain compliant, reliable, and scalable in enterprise environments.
Therefore, architecture must be designed to handle compliance, scale, interoperability, and safety together. It must support real clinical and financial workflows, not just analytics. As a result, enterprise architecture is less about tools and more about how systems behave under stress.
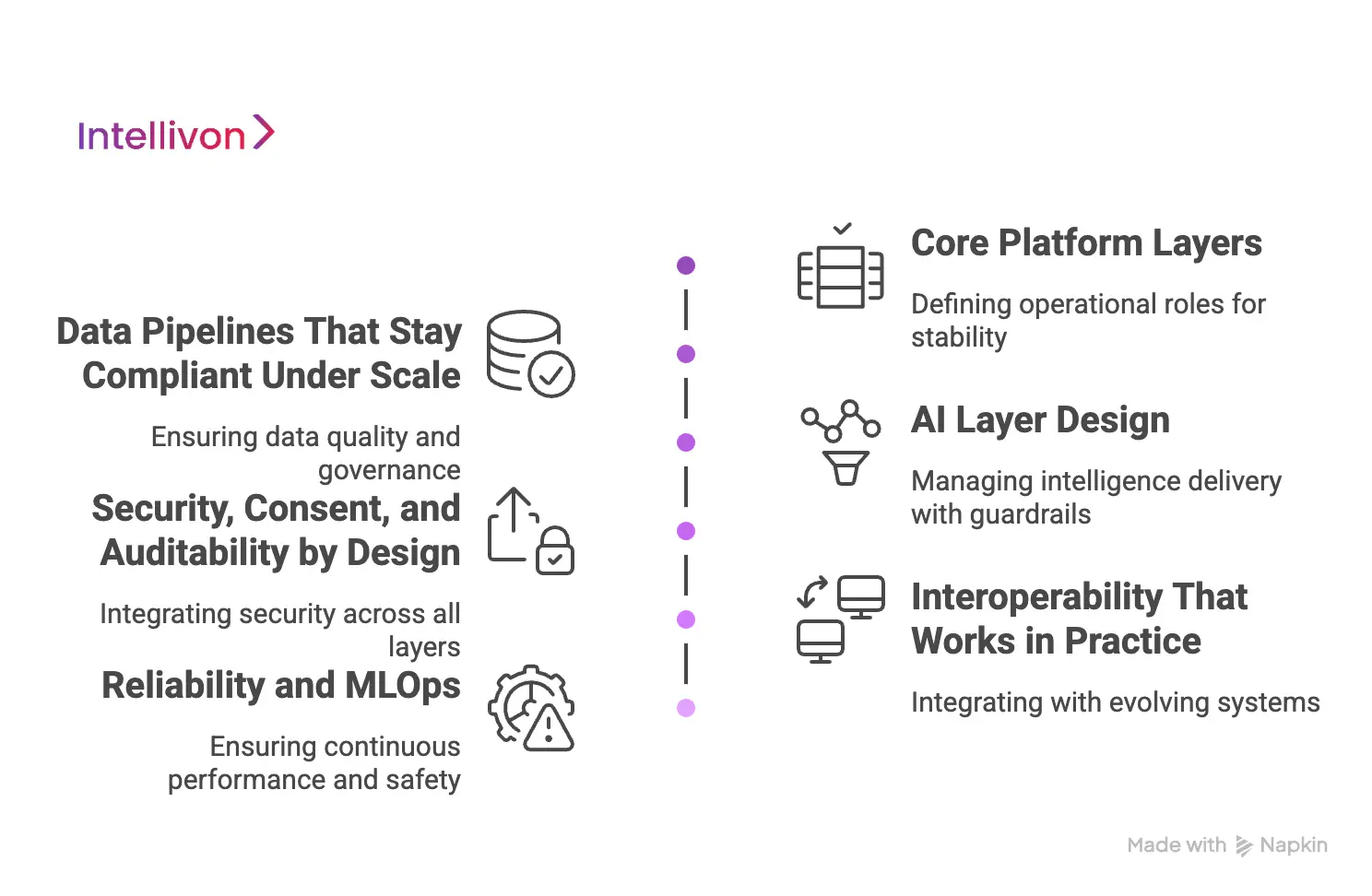
1. Core Platform Layers
An enterprise AI healthcare app is built as a set of clearly defined layers, each serving a distinct operational role. These layers ensure the system remains usable, governable, and resilient as complexity grows. In practice, this layered structure allows teams to scale parts of the platform independently without breaking compliance or performance.
Therefore, it becomes the backbone of long-term enterprise stability. The core layers typically include:
- Experience layer: Interfaces for clinicians, operations, and administrators
- Workflow layer: Task routing, approvals, escalation, and orchestration
- Integration layer: Secure connectivity with EHRs, labs, imaging, and payers
- Operations layer: Monitoring, uptime management, and incident response
Together, these layers define how the platform behaves in real-world healthcare environments.
2. Data Pipelines That Stay Compliant Under Scale
Data architecture determines whether AI remains trustworthy as volume and variety increase. In healthcare, data must pass through quality and governance checks before reaching any AI service. Therefore, ingestion pipelines are designed to normalize formats, resolve identities, and enforce patient-level access controls.
In addition, every transformation must generate a traceable lineage for audits. Without this, AI outputs cannot remain defensible in enterprise environments. Key components of compliant data pipelines include:
- Structured ingestion from clinical and financial systems
- Identity resolution and patient record matching
- Data normalization using FHIR-aligned models
- End-to-end lineage and audit trails
This ensures that data supports both intelligence and compliance simultaneously.
3. AI Layer Design
The AI layer is not a single model running in isolation. Instead, it operates as a set of services that manage how intelligence is delivered into workflows. In healthcare, AI must be constrained by clinical context and regulatory rules. Therefore, outputs must pass through guardrails and, in high-risk cases, human review.
This ensures intelligence does not override accountability. A production-ready AI layer typically includes:
- Model serving and version management
- Retrieval and context orchestration
- Output guardrails and policy enforcement
- Human-in-the-loop review points
These controls turn AI from a capability into a governed system.
4. Security, Consent, and Auditability by Design
Security in AI healthcare apps is inseparable from architecture. Identity management, encryption, and access policies must operate across every layer, not as a separate module.
Moreover, consent enforcement must follow the data and the decision, not just the record. When audit trails are embedded into workflows, compliance becomes operational rather than administrative. This reduces regulatory exposure while preserving system performance. Core architectural controls include:
- Role-based access and least privilege
- Encryption in transit and at rest
- Consent enforcement across systems
- Immutable audit logging
These ensure that trust is built into system behavior, not added later.
5. Interoperability That Works in Practice
Enterprise AI healthcare apps must integrate across systems that evolve independently. Therefore, interoperability cannot rely on static APIs alone. Instead, platforms must use canonical data models, event-driven updates, and version control across integrations.
This prevents silent failures when upstream systems change. As a result, AI outputs remain consistent even as ecosystems grow. Practical interoperability relies on:
- Canonical data models with adapters
- Event-driven updates from source systems
- Integration testing and change control
- Versioned API and data contracts
This makes the platform resilient to ecosystem change.
6. Reliability and MLOps
An AI healthcare app must remain safe after deployment. Model drift, data shifts, and usage changes are inevitable in real environments. Therefore, platforms must monitor performance continuously and trigger fallback mechanisms when thresholds are breached.
In addition, version control and release approvals ensure changes do not introduce new risk. This is how AI remains reliable over time, not just accurate at launch. Operational reliability is supported through:
- Continuous model and data monitoring
- Drift detection and alerting
- Controlled releases and rollbacks
- Incident response for AI failures
This ensures AI behaves predictably under enterprise conditions.
AI healthcare apps succeed when architecture anticipates enterprise reality. Models alone cannot carry compliance, scale, and operational safety. Therefore, organizations that invest in layered, governed architecture build platforms that regulators, clinicians, and partners can trust.
How To Make An AI Healthcare App HIPAA and GDPR Ready?
An AI healthcare app becomes HIPAA and GDPR ready when privacy, security, consent, and auditability are built into its architecture and daily operations from the start.
Compliance in healthcare can no longer be treated as a legal exercise handled after deployment. This is especially true for AI-driven platforms that process sensitive clinical and financial data.
1. Build Compliance Into Architecture
Many organizations attempt to add compliance controls after an AI healthcare app is already live. However, this approach often creates gaps that are expensive and risky to fix later.
Therefore, enterprises must embed privacy, security, and governance directly into the system architecture. This includes designing data flows that minimize exposure and enforce access control by default. When compliance is built in early, it supports scale rather than slowing it down.
2. Enforce Data Minimization and Purpose Limitation
HIPAA and GDPR both require that organizations collect and process only what is necessary. In AI healthcare apps, this principle must extend to training data, inference pipelines, and analytics workflows. Therefore, systems should actively restrict data usage to approved clinical and operational purposes.
In addition, automated checks should prevent secondary use without authorization. This ensures AI remains aligned with regulatory intent, not just technical capability.
3. Implement Strong Identity and Access
Who can access data is just as important as how data is processed. AI healthcare apps must enforce role-based access and least privilege across every layer. Moreover, consent must travel with the data, not remain locked in static records.
When identity and consent are enforced dynamically, organizations can confidently scale across teams and regions. This reduces regulatory exposure while preserving operational agility.
4. Maintain Auditability and Explainability
Regulators increasingly expect enterprises to explain not only what data was used, but also how decisions were made. Therefore, AI healthcare apps must maintain detailed audit logs tied to both data access and AI outputs.
In addition, explainability mechanisms should make AI decisions interpretable to clinicians and compliance teams. When auditability is built into workflows, compliance becomes verifiable rather than assumed.
4. Secure Data Across Borders and Lifecycles
GDPR introduces additional complexity for cross-border data handling. AI healthcare apps must account for data residency, encryption, and lawful transfer mechanisms from the outset.
Moreover, data must remain protected across its entire lifecycle, from ingestion to archival and deletion. This ensures privacy obligations are met without disrupting care delivery or analytics.
HIPAA and GDPR readiness is no longer a barrier to innovation. When implemented correctly, it becomes a foundation for scalable and trustworthy AI healthcare apps. Therefore, enterprises that treat compliance as an architectural and operational discipline gain a strategic advantage.
How Will The AI Healthcare App Integrate With EHRs via FHIR?
An AI healthcare app integrates with EHRs via FHIR when clinical data is normalized, governed, and delivered into AI workflows with traceability, consent, and reliability built in.
When integration is done correctly, it enables AI to operate inside real clinical workflows rather than alongside them. As a result, interoperability becomes a strategic enabler, not just a technical requirement.
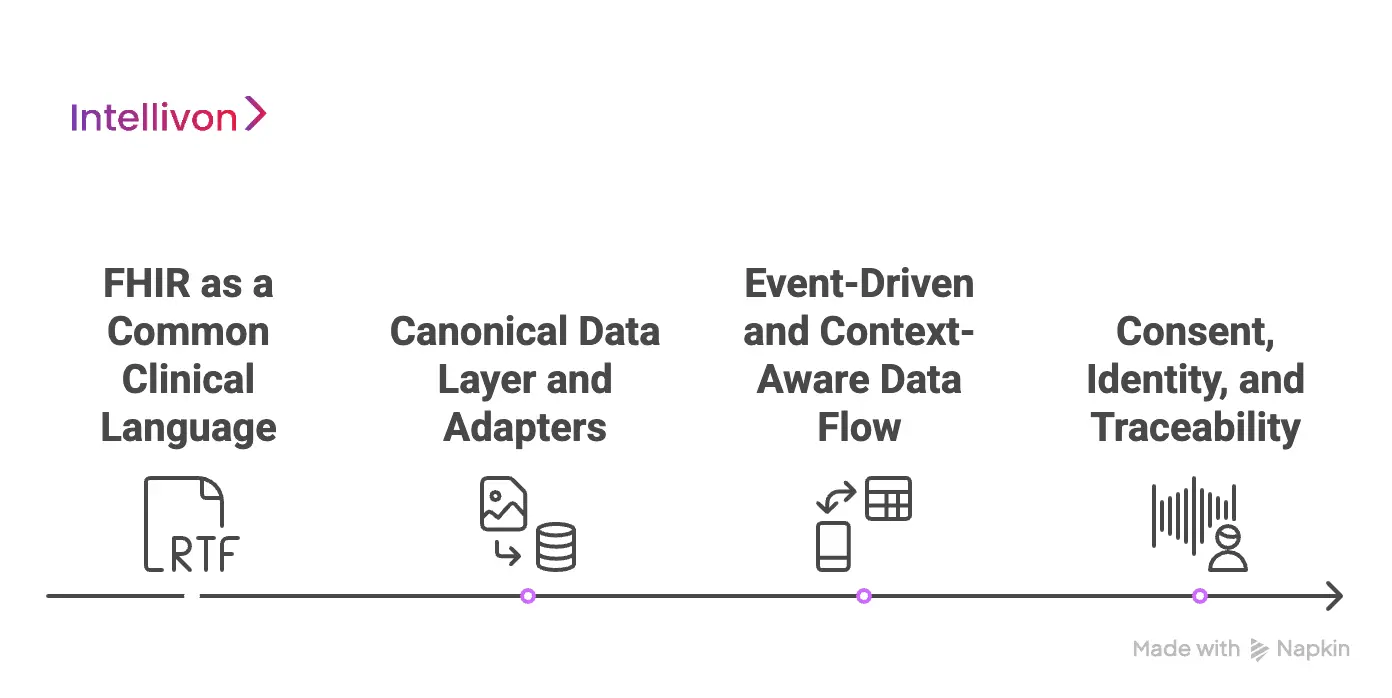
1. FHIR as a Common Clinical Language
FHIR provides a structured way to represent clinical data so systems can exchange it consistently. However, using FHIR does not automatically make integration enterprise-ready. Each EHR still implements standards differently.
Therefore, AI healthcare apps must treat FHIR as a shared language, not a plug-and-play interface. This mindset prevents oversimplified assumptions that often break at scale.
2. Canonical Data Layer and Adapters
Enterprise AI platforms cannot rely on raw EHR feeds alone. Instead, they normalize incoming data into a canonical model that remains consistent across sources. Adapters then translate each EHR’s structure into this shared format.
As a result, AI services receive predictable inputs regardless of where data originates. This layer also absorbs upstream changes without destabilizing downstream systems.
3. Event-Driven and Context-Aware Data Flow
Clinical data is not static. Therefore, AI healthcare apps must support event-driven updates using subscriptions or triggers. This ensures that AI operates on current and relevant information.
At the same time, context packaging delivers only the data required for a specific task. This limits unnecessary exposure while improving performance.
4. Consent, Identity, and Traceability
FHIR integration must respect who the data belongs to and how it can be used. Identity resolution ensures patient records remain accurate across systems. Moreover, consent must be enforced dynamically, not assumed once access is granted.
Every AI output should also reference its source data. This makes decisions auditable and defensible.
5. What Production-Ready Integration Looks Like
Enterprise integration must work under real-world conditions. A production-ready setup typically includes:
- Data completeness and quality checks
- Latency and availability monitoring
- Fallbacks when EHR access fails
- Version control for interfaces
- Continuous integration testing
These controls prevent silent failures that undermine trust in AI outputs.
FHIR integration determines whether an AI healthcare app can scale responsibly and deliver reliable outcomes. Therefore, organizations that invest in governed, production-grade interoperability unlock both clinical value and enterprise ROI. This is what transforms AI from a promising capability into a trusted operational system.
How We Build An Enterprise-Grade AI Healthcare App
Intellivon builds AI healthcare apps through a structured delivery model that aligns business outcomes, governance, and scalable engineering from day one.
Each phase reduces uncertainty while strengthening operational readiness. In addition, this approach keeps clinical, technical, and business teams aligned throughout execution. As a result, the AI healthcare app evolves as an enterprise platform, not an experimental product.
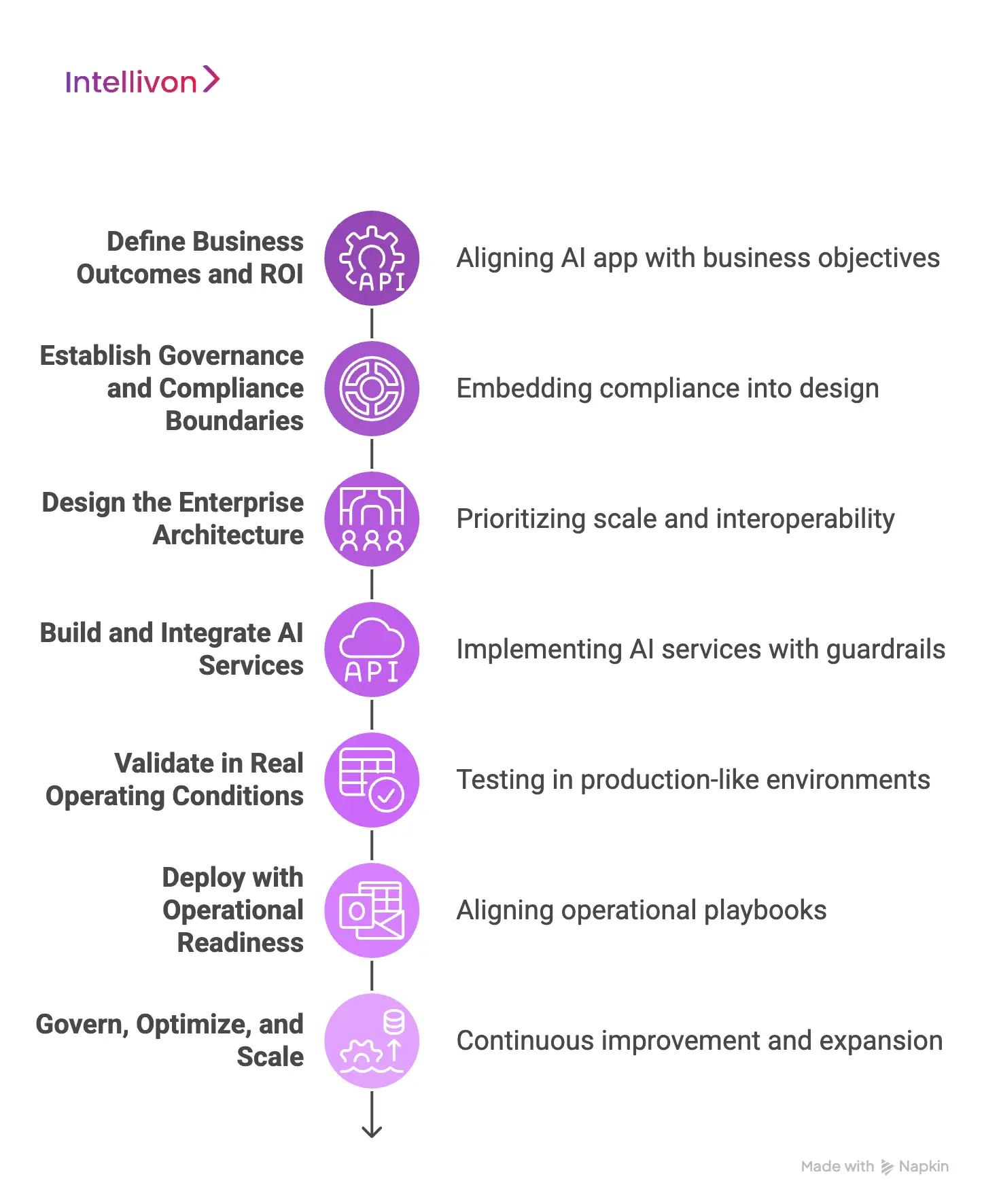
Step 1: Define Business Outcomes and ROI
We begin by aligning the AI healthcare app with concrete business objectives. This includes revenue protection, cost reduction, throughput improvement, and compliance performance.
Therefore, we map high-friction workflows before selecting any technology. In addition, we identify which stakeholders will own outcomes post-launch. This ensures the solution is funded and measured as a business initiative, not an innovation experiment.
Step 2: Establish Governance and Compliance Boundaries
Next, we define how data, AI, and users will be governed across the platform. This includes access control, consent enforcement, audit requirements, and model accountability.
Therefore, compliance is embedded into the design rather than validated later. In addition, risk thresholds are agreed upon before development begins. This prevents rework while strengthening regulatory defensibility.
Step 3: Design the Enterprise Architecture
Once governance is clear, we design the reference architecture around scale and interoperability. This includes data pipelines, AI services, security layers, and operational controls.
Moreover, we prioritize integration with EHRs, labs, imaging, and financial systems. As a result, the AI healthcare app becomes part of real workflows rather than an isolated tool. This step ensures the platform remains viable beyond pilot deployments.
Step 4: Build and Integrate AI Services
We then implement AI services aligned with the defined use cases. This includes model selection, retrieval pipelines, guardrails, and human review points.
Therefore, intelligence is introduced in a controlled and auditable manner. In addition, every AI output remains traceable to its data and logic. This preserves trust across clinical and operational teams.
Step 5: Validate in Real Operating Conditions
Before scale, we validate the AI healthcare app in production-like environments. This includes performance testing, compliance verification, and failure scenario simulations.
Therefore, risks are surfaced early, not after enterprise rollout. In addition, we refine workflows based on real user behavior. This ensures the system performs reliably under operational pressure.
Step 6: Deploy with Operational Readiness
Deployment is not treated as a handover event. Instead, we align operational playbooks, monitoring systems, and incident response before launch. Therefore, the platform enters production with clear ownership and accountability.
In addition, we establish KPIs tied to business and clinical outcomes. This ensures value realization continues after go-live.
Step 7: Govern, Optimize, and Scale
After deployment, we continuously govern and optimize the AI healthcare app. This includes monitoring model performance, workflow adoption, and regulatory alignment.
Therefore, the platform evolves safely as volumes, use cases, and regions expand. In addition, we support phased scaling without disrupting operations. This final step transforms delivery into long-term platform stewardship.
At Intellivon, building an AI healthcare app is a long-term partnership focused on sustainable enterprise value. Therefore, our delivery model prioritizes governance, scalability, and operational confidence from the outset.
Where Do Payments, Reimbursements, And Wallets Fit In The App?
Payments, reimbursements, and wallets become core infrastructure inside an AI healthcare app when financial workflows are embedded directly into care delivery and governance layers.
As healthcare becomes digital-first, financial transactions now occur inside the same workflows as clinical decisions. Therefore, AI healthcare apps must treat finance as core infrastructure, not a supporting feature.
1. Payments as Part of the Care Workflow
In enterprise healthcare, payments are part of how access, authorization, and service delivery are coordinated. Therefore, AI healthcare apps must support payment logic within scheduling, treatment, and discharge workflows.
This allows organizations to reduce billing delays and improve transparency. In addition, embedding payments improves patient trust by eliminating fragmented financial journeys.
2. Reimbursements and Claims Automation
Reimbursements are where operational complexity and financial risk converge. AI healthcare apps can automate claims generation, validation, and submission directly from clinical data. As a result, errors decrease while processing speed improves.
Moreover, organizations gain better visibility into revenue cycle performance without relying on manual reconciliation. This strengthens both cash flow predictability and compliance readiness.
3. Digital Wallets for Patient and Provider Ecosystems
Digital wallets extend financial capability beyond simple payments. In AI healthcare apps, wallets can support co-pays, benefits management, and cross-provider transactions. Therefore, they become tools for financial continuity across fragmented healthcare networks.
In addition, wallets enable new care models such as subscription-based services or employer-funded benefits. This expands how healthcare platforms engage patients and partners.
4. Financial Governance and Auditability
Financial workflows in healthcare are tightly regulated. Therefore, AI healthcare apps must enforce role-based access, transaction traceability, and audit logging across every financial action.
In addition, financial data must remain aligned with clinical records and consent rules. When governance is embedded into financial layers, compliance becomes operational rather than administrative. This reduces both regulatory risk and financial exposure.
Payments, reimbursements, and wallets now form a strategic layer inside AI healthcare apps. When built correctly, they transform digital care platforms into enterprise-grade healthcare-fintech infrastructure.
How AI Healthcare Apps Make Money
AI healthcare apps generate revenue by embedding financial logic into real care and operational workflows. Therefore, monetization aligns with how healthcare organizations deliver and pay for care rather than consumer-style growth tactics.
Revenue Models for AI Healthcare Apps
| Revenue Model | How It Works | Why Enterprises Use It |
| Platform Licensing & Subscription | Organizations pay recurring fees for access to core platform modules and upgrades | Provides predictable costs and supports long-term financial planning |
| Transaction-Based Pricing | Charges per claim processed, payment handled, or verification completed | Scales with operational volume and ties revenue to real usage |
| Value-Based Pricing | Fees linked to performance outcomes like reduced denials or faster reimbursements | Aligns vendor success directly with enterprise results |
| Ecosystem & Marketplace Revenue | Revenue from third-party modules, integrations, and partner services | Expands platform capability without full in-house development |
| Insights as a Service | Monetizes anonymized benchmarks and analytics, not raw data | Enables strategic decisions while maintaining regulatory compliance |
AI healthcare apps make money when monetization is built into operational value rather than isolated features. When revenue aligns with enterprise performance and compliance, financial sustainability follows naturally. This is what allows AI healthcare apps to scale responsibly while remaining commercially viable.
What Does An Enterprise AI Healthcare App Cost To Build
At Intellivon, AI healthcare apps are built as a regulated digital healthcare infrastructure, not as isolated AI features layered onto existing products. The focus stays on creating platforms that operate reliably across providers, payers, regions, and evolving regulatory frameworks. Every architectural and delivery decision accounts for governance, interoperability, and long-term operational risk from the start.
When budget constraints exist, scope is refined with intent. However, AI governance, data security, consent enforcement, and auditability are never compromised. Therefore, enterprises avoid remediation costs that typically surface after launch. Predictability replaces rework, and long-term ROI remains protected.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Regulatory Alignment | Use case prioritization, compliance mapping, and AI risk classification | $9,000 – $15,000 |
| Secure Architecture Design | Layered AI platform design, data flows, identity, and consent logic | $12,000 – $20,000 |
| Governance & AI Policy Framework | Model oversight, approval workflows, audit logic, and exception handling | $10,000 – $17,000 |
| AI Model Development & Orchestration | Model selection, training, RAG pipelines, output guardrails | $18,000 – $32,000 |
| Backend & Enterprise Integrations | EHRs, imaging systems, claims engines, payer platforms | $16,000 – $30,000 |
| Frontend & Role-Based Interfaces | Clinician, admin, ops dashboards with access controls | $11,000 – $19,000 |
| Security & Compliance Controls | Encryption, access enforcement, monitoring, anomaly detection | $10,000 – $18,000 |
| Testing & Compliance Validation | Functional testing, security testing, AI audits, readiness reviews | $7,000 – $12,000 |
| Deployment & Scale Readiness | Cloud/hybrid setup, performance tuning, reliability testing | $8,000 – $14,000 |
Total initial investment: $101,000 – $197,000
Ongoing maintenance and optimization: ~15–20% of the initial build per year
Request a tailored proposal from Intellivon’s AI healthcare experts to receive a delivery roadmap aligned with your budget constraints, compliance exposure, and long-term enterprise AI strategy.
Top Examples of AI Healthcare Apps
AI healthcare apps today operate inside real care, diagnostic, and operational workflows across healthcare systems.
Therefore, looking at how leading platforms apply AI in practice helps enterprises separate usable models from theoretical ones. The examples below show how AI is embedded, governed, and monetized in real-world healthcare environments.
1. Ada Health
A global symptom assessment and health guidance platform used by consumers and healthcare organizations.
How AI works:
- Uses machine learning and clinical knowledge graphs
- Interprets symptoms and risk factors to suggest next steps
- Continuously improves through real-world data patterns
How they monetize:
- Free consumer app
- Enterprise licensing for insurers and healthcare providers
2. K Health
A virtual primary care platform combining AI with clinician-led consultations.
How AI works:
- Analyzes large anonymized clinical datasets
- Suggests likely diagnoses for clinician review
- Supports triage and care routing
How they monetize:
- Subscriptions
- Contracts with payers and healthcare systems
3. Lark Health
A digital health coach focused on chronic condition management.
How AI works:
- Conversational AI delivers coaching and nudges
- Personalizes interventions using behavioral data
How they monetize:
- B2B contracts with employers and health plans
- Population health management programs
4. Buoy Health
An AI-powered symptom checker used in patient intake and triage.
How AI works:
- Uses NLP to understand user-reported symptoms
- Maps symptoms to likely conditions and next actions
How they monetize:
- Licensing to hospitals, insurers, and digital health platforms
5. Qure.ai
A medical imaging AI platform supporting radiology workflows.
How AI works:
- Deep learning models detect abnormalities in X-rays and CT scans
- Prioritizes urgent cases and reduces radiologist workload
How they monetize:
- Enterprise licensing
- Volume-based diagnostic contracts
These AI healthcare apps show how intelligence becomes valuable only when embedded into real workflows and governed at scale. More importantly, they demonstrate that sustainable monetization follows operational value, not just technical capability.
Conclusion
AI healthcare apps are becoming core enterprise platforms that shape how care, compliance, and financial operations converge.
Organizations that treat AI as governed infrastructure rather than isolated innovation unlock sustainable value at scale. With the right architecture, governance, and delivery approach, AI becomes a growth enabler, not a risk multiplier. Intellivon helps enterprises build AI healthcare platforms designed for real-world complexity and long-term leadership.
Build An AI Healthcare App With Intellivon
At Intellivon, AI healthcare apps are built as regulated enterprise platforms, not as AI features layered onto care systems. Every architectural and delivery decision prioritizes compliance, interoperability, and long-term operational reliability. This ensures platforms perform across providers, payers, and regions, not just during pilot deployments.
As AI programs scale across use cases and populations, stability becomes critical. Governance, performance, and audit readiness remain consistent as volumes grow. Organizations retain control over data, models, and workflows without introducing fragmentation or regulatory risk.
Why Partner With Intellivon?
- Enterprise-grade AI healthcare architecture designed for regulated care environments
- Proven delivery across providers, insurers, and healthcare technology platforms
- Compliance-by-design approach with audit readiness and policy enforcement
- Secure, modular infrastructure supporting cloud, hybrid, and on-prem deployments
- Governed AI enablement for insights, automation, and decision support
- Deep interoperability expertise across EHRs, imaging, and claims systems
- ROI-focused delivery model aligned to enterprise performance metrics
- Scalable delivery frameworks for multi-region and multi-entity healthcare networks
Book a strategy call to explore how Intellivon can help you build and scale an AI healthcare app with confidence, control, and long-term enterprise value.
FAQs
Q1. What is an AI healthcare app, and how is it different from traditional healthcare software?
A1. An AI healthcare app uses machine learning and data intelligence to automate, predict, and optimize clinical and operational workflows. Unlike traditional healthcare software that only digitizes processes, AI healthcare apps actively analyze data to support decisions, reduce friction, and improve outcomes across care, finance, and compliance.
Q2. How much does it cost to build an enterprise AI healthcare app?
A2. The cost to build an enterprise AI healthcare app typically ranges from $100,000 to $200,000 for an initial platform. Final cost depends on compliance scope, AI complexity, EHR integrations, security requirements, and scalability expectations. Ongoing maintenance usually adds 15–20% annually.
Q3. Are AI healthcare apps compliant with HIPAA and GDPR by default?
A3. No, AI healthcare apps are not compliant by default. Compliance depends on how privacy, security, consent, and auditability are built into the system architecture. Enterprise-grade AI healthcare apps must enforce role-based access, data minimization, audit trails, and cross-border data controls to meet HIPAA and GDPR standards.
Q4. How do AI healthcare apps integrate with EHR systems like Epic or Cerner?
A4. AI healthcare apps integrate with EHRs using standards such as FHIR to securely access and update clinical data. However, production-ready integration also requires identity resolution, consent enforcement, data normalization, and continuous monitoring to ensure AI outputs remain reliable and auditable.
Q5. What business value do AI healthcare apps deliver for enterprises?
A5. AI healthcare apps deliver business value by reducing operational costs, protecting revenue, improving clinical efficiency, and strengthening compliance. Enterprises commonly use them to automate claims, accelerate documentation, streamline prior authorization, enhance diagnostics, and support scalable digital care models.