Most health systems still operate as isolated entities, even though care delivery already happens across networks. Patients move between providers for referrals, transfers, and specialist care, but their clinical data doesn’t follow them. This structural mismatch creates business pressures enterprise leaders cannot ignore.
Cross-provider HIE exists to fix this mismatch. But the challenge is about building shared infrastructure between organizations that compete and collaborate simultaneously. Most HIE initiatives fail because they underestimate the governance complexity, can’t align participant incentives, or never resolve the trust issues that keep organizations from opening their data.
Intellivon builds cross-provider HIE platforms and helps enterprises connect to existing exchanges. This guide shows how we develop HIEs that actually reach sustainable operation. We will cover how to structure governance across independent organizations, design participation models that work economically, and build technical architecture that handles the reality of cross-organizational accountability at enterprise scale.
Why Should You Invest In Cross-Privider HIE Platform Now
Cross-provider Health Information Exchange (HIE) platforms let hospitals, clinics, labs, and payers share patient data securely. This reduces data silos and helps care teams see a complete patient history.
As a result, referrals improve, transfers become safer, and care coordination gets easier. Standards like FHIR make this possible across different software systems. For enterprises, this creates both urgency and opportunity.
Market trends now show rapid enterprise adoption, driven by both compliance pressure and the need for scalable digital infrastructure. In fact, according to a Grand View Research report, the global health information exchange (HIE) market was valued at about USD 2 billion in 2023 and is expected to grow to nearly USD 4 billion by 2030.
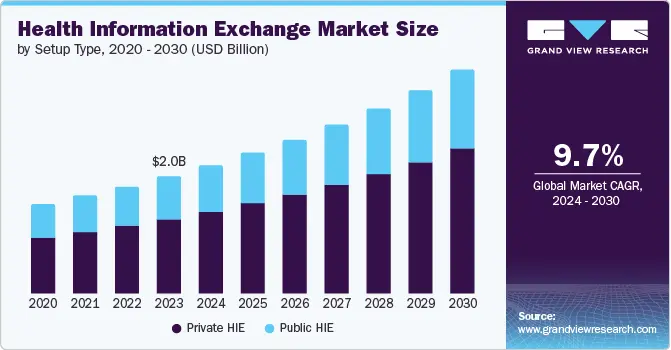
Market Insights:
- Regulations now require systems to share data, not just store it, which is driving strong enterprise demand for interoperable platforms.
- Growing data volumes and the need to connect EHRs across providers are accelerating HIE adoption across large healthcare networks.
- Despite security and legacy system challenges, widespread FHIR adoption is making cross-provider exchange more practical and investment-ready.
- Private HIEs lead the market with 63.6% share, driven by the need for internal efficiency and secure connections with public health networks.
- Centralized HIE models account for 55%, as enterprises prefer simpler control and governance in large deployments.
- North America holds 46% market dominance, while Asia-Pacific is growing fastest due to aggressive digital health programs and regulatory support.
Several established vendors shape today’s cross-provider HIE landscape. Companies such as McKesson, Optum, InterSystems, CommonWell Health Alliance, and Epic Systems play a central role in building and operating large exchange networks across healthcare systems.
In addition, firms like Allscripts, Orion Health, and IBM focus strongly on clinical data exchange and interoperability platforms. Increasingly, these vendors are forming partnerships and consolidating capabilities to scale faster and offer more integrated solutions to enterprise buyers.
What Is A Cross-Provider Healthcare Information Exchange Platform?
A cross-provider Healthcare Information Exchange (HIE) platform is a system that allows different healthcare organizations to share patient data securely and in real time. This includes hospitals, clinics, labs, pharmacies, and payers that normally operate on separate systems.
Instead of keeping patient information locked inside one hospital or network, an HIE creates a shared layer for data exchange. As a result, care teams can access a more complete view of a patient’s history, even when treatment happens across multiple providers.
This matters because modern healthcare rarely stays within one organization. Patients move between specialists, diagnostic centers, and care settings. Without an HIE, this movement often breaks the flow of information.
A cross-provider HIE does not replace existing hospital systems. Instead, it connects them. It works in the background, ensuring data moves safely, follows regulatory rules, and stays usable for clinical decisions. For enterprises, this means better coordination, fewer errors, and stronger operational control across the care network.
Cross-Provider HIE Vs Traditional Health Data Exchange
Not all health data exchange is the same. Many organizations already move data internally between their own systems. However, cross-provider HIEs operate at a very different level and solve a much broader problem.
Traditional health data exchange usually connects systems inside one organization. It helps a hospital move information between its EHR, billing, and clinical tools. While useful, it does not address how data flows between independent hospitals, labs, insurers, and public health bodies.
A cross-provider HIE platform exists precisely for that purpose. It creates a neutral layer where multiple organizations can share data safely, even when they do not belong to the same group or follow the same internal rules.
Here is how the two models differ in practice:
| Aspect | Traditional Health Data Exchange | Cross-Provider HIE Platform |
| Scope | Within one organization | Across multiple independent organizations |
| Ownership | A single entity controls the system | Neutral or shared governance model |
| Trust Model | Internal trust | Engineered trust across parties |
| Compliance | Managed centrally | Shared accountability across participants |
| Data Access | Limited to internal users | Controlled access for external providers |
| Scalability | Designed for local growth | Built for regional or national scale |
In simple terms, traditional exchange improves internal efficiency. A cross-provider HIE enables healthcare networks to function as coordinated systems.
For enterprise leaders, this difference matters. Internal integration supports today’s operations. Cross-provider HIEs shape tomorrow’s care delivery model. They require more planning, stronger governance, and deeper trust, but they unlock far greater clinical and business value in return.
Core Features of a Cross-Provider HIE Platform
A cross-provider HIE platform is not a single piece of software. It is a set of connected capabilities that work together to make data exchange safe, reliable, and useful across organizations. Each feature plays a specific role in ensuring that the platform functions smoothly in real healthcare environments.
Below are the core features enterprise leaders should expect from a production-grade HIE platform.
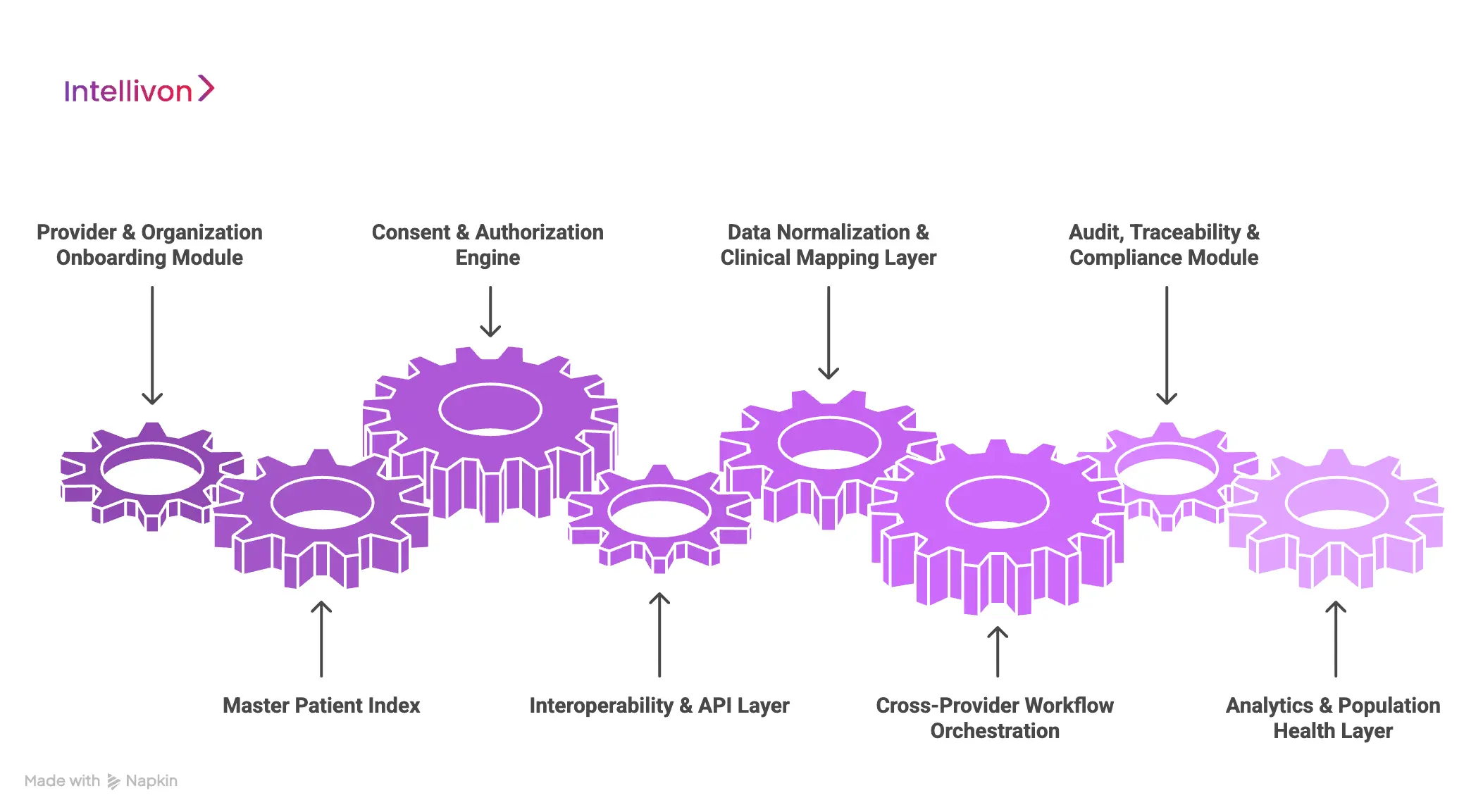
1. Provider & Organization Onboarding Module
Before any data can move, the platform must know who is allowed to participate. This module manages how hospitals, clinics, labs, and payers join the network.
It verifies credentials, confirms regulatory compliance, and establishes trust between participants. In addition, it defines each organization’s role and access boundaries. As a result, data sharing begins on a foundation of accountability rather than assumptions.
This step is critical because cross-provider HIEs depend on shared responsibility, not just technical access.
2. Master Patient Index
Patients often appear differently across systems. Names vary, identifiers change, and records get duplicated.
The identity engine resolves this by linking records that belong to the same person across hospitals and clinics. It reduces mismatches and ensures care teams are viewing the correct patient history.
Without this capability, even the most advanced HIE becomes unreliable. Therefore, patient identity resolution sits at the heart of any cross-provider exchange.
3. Consent & Authorization Engine
Data sharing only works when it respects patient choice and legal boundaries. This engine manages patient consent in a portable way, meaning preferences follow the patient across providers. It also enforces who can access what data and under which circumstances.
Emergency access rules are handled here as well, ensuring clinicians can act when needed while maintaining auditability. As a result, trust is preserved without slowing down care delivery.
4. Interoperability & API Layer
Healthcare systems speak different technical languages. The interoperability layer translates between them.
Using standards like FHIR, this layer enables both real-time and batch data exchange between EHRs, lab systems, and imaging platforms.
It allows organizations to connect without replacing their existing software. In practice, this is what makes cross-provider exchange technically possible at scale.
5. Data Normalization & Clinical Mapping Layer
Raw data alone is not enough. It must be consistent and clinically meaningful. This layer maps data to common standards such as SNOMED, LOINC, and ICD. As a result, information coming from different providers becomes comparable and usable.
This ensures that clinicians and analysts can rely on the data, rather than questioning its structure or meaning.
6. Cross-Provider Workflow Orchestration
Beyond moving data, an HIE must support real clinical workflows. This includes managing referrals, sharing discharge summaries, and enabling joint care plans across organizations.
Therefore, the platform becomes part of how care is delivered, not just how information travels. This is where HIEs move from being technical tools to operational enablers.
7. Audit, Traceability & Compliance Module
Every access and action must be visible and defensible. This module tracks who accessed what data, when, and under what authority. It supports audits, regulatory reporting, and internal governance.
For enterprises, this creates confidence that sharing data does not mean losing control.
8. Analytics & Population Health Layer
Finally, a mature HIE supports decision-making at scale. It enables cross-provider reporting, utilization tracking, and outcome analysis. This helps leaders identify gaps in care, inefficiencies, and improvement opportunities.
In addition, it supports value-based care and population health initiatives that depend on unified data views.
These features define whether an HIE remains a connector or becomes a real healthcare infrastructure. At enterprise scale, that distinction determines trust, compliance, and long-term value.
How a Cross-Provider HIE Platform Is Architected
A cross-provider HIE platform must be built as a layered infrastructure, not as a single application. Each layer solves a specific problem while supporting the layers above it. This approach makes the platform easier to scale, secure, and govern across independent organizations.
It also ensures that technical decisions align with regulatory and operational realities. Below is how a production-grade HIE platform is typically structured.
1. Data Layer
The data layer is responsible for how information is stored, retrieved, and protected. It handles both clinical and administrative data coming from multiple providers. Because this data originates from different systems, the layer must support varied formats and volumes.
In addition, it must ensure that records remain accurate and tamper-proof over time. This layer also enforces basic data security controls, such as encryption and backups. Without a reliable data layer, every other part of the platform becomes fragile.
2. Interoperability Layer
This layer enables different systems to communicate with each other. It translates data between EHRs, lab systems, imaging platforms, and payer systems. Standards like FHIR and HL7 are used here to reduce friction between technologies.
However, real-world interoperability also requires handling exceptions and custom formats.
Therefore, this layer must remain flexible while still enforcing structure. In practice, it is what makes cross-provider exchange technically possible.
3. Identity and Consent Layer
Sharing data across organizations requires clarity on who the patient is and what data can be accessed. This layer resolves patient identities across hospitals and clinics that use different identifiers.
It also enforces patient consent and access permissions in real time. As a result, data moves only when it is legally and ethically allowed. This layer protects trust between providers and patients alike. Without it, even secure platforms fail to gain adoption.
4. Workflow and Orchestration Layer
Healthcare is driven by processes, not just data. This layer manages how information flows through referrals, discharges, and shared care plans. It ensures that data appears at the right time, in the right place, for the right user.
In addition, it connects technical exchange with real operational workflows. This is where the HIE becomes part of daily care delivery. Without this layer, the platform remains a passive data pipeline.
5. Governance and Compliance Layer
Cross-provider platforms must operate under shared rules. This layer defines how access is granted, monitored, and reviewed across organizations. It also supports audits, reporting, and regulatory compliance.
Importantly, it enforces accountability when multiple providers share responsibility. This creates a defensible operating model for the HIE. For enterprise leaders, this layer determines whether the platform can survive regulatory scrutiny.
6. Application and Analytics Layer
This is the layer users interact with most directly. It includes dashboards, reporting tools, and population health views built on top of shared data.
It allows leaders to see trends, gaps in care, and operational inefficiencies across providers. In addition, it supports value-based care and performance monitoring.
This layer turns exchanged data into business and clinical insight. Without it, the HIE delivers connectivity but not intelligence.
A cross-provider HIE succeeds only when these layers work together as a single system. If one layer is weak, the entire platform becomes unstable. Therefore, architecture is not a technical detail but a strategic decision.
For enterprises, getting this right determines whether the HIE becomes a long-term asset or a recurring operational burden.
How Cross-Provider Data Exchange Works: End-to-End Flow
Understanding how data actually moves across providers helps leaders assess both feasibility and risk. While the technology may feel abstract, the process itself is structured and predictable. Below is a simplified walkthrough of how a typical cross-provider exchange happens in practice.
Step 1: Data Is Generated at the Source
A patient visits a hospital, clinic, or lab, where new medical data is created. This could include test results, prescriptions, or discharge notes. The local system records this information in its own format.
However, at this stage, the data remains locked inside that organization. Therefore, the HIE platform must first detect that new information is available for sharing.
Step 2: Patient Identity Is Matched Across Providers
Before any data moves, the platform checks whether this patient already exists in the shared network. It compares identifiers such as name, date of birth, and medical numbers. This process links records that belong to the same person across different systems.
As a result, the platform avoids duplicate or fragmented patient profiles. This step ensures that data is attached to the correct individual.
Step 3: Consent and Access Rules Are Verified
Next, the system confirms whether the data can legally be shared. It checks patient consent preferences and organizational access policies. Only providers with proper authorization can view or use the information.
In emergency cases, special access rules may apply, but they are always logged. Therefore, compliance is maintained without delaying care.
Step 4: Data Is Standardized and Prepared for Exchange
The data is then converted into standardized formats so other systems can understand it. Clinical codes and terms are aligned to common medical standards. This makes the information usable across different software environments.
Without this step, shared data would be difficult to interpret or trust. Standardization is what makes cross-provider exchange practical.
Step 5: Data Is Delivered to the Receiving Provider
Once cleared and prepared, the data is securely transmitted to the requesting provider. It appears inside their local system or HIE interface, depending on the setup. Clinicians can now view and use the information as part of their workflow.
This allows faster decisions and better coordination. Importantly, this happens without manual data chasing.
Step 6: Every Action Is Logged and Audited
Finally, the platform records who accessed the data, when, and for what purpose. These logs support audits, compliance reviews, and internal governance.
They also provide accountability across organizations. As a result, sharing data does not mean losing control over it.
This flow shows that cross-provider exchange is not chaotic or informal. It follows a controlled, rule-driven process designed for scale and accountability. For enterprise leaders, this means HIEs can support growth without compromising trust or compliance. When implemented correctly, data moves freely, but never loosely.
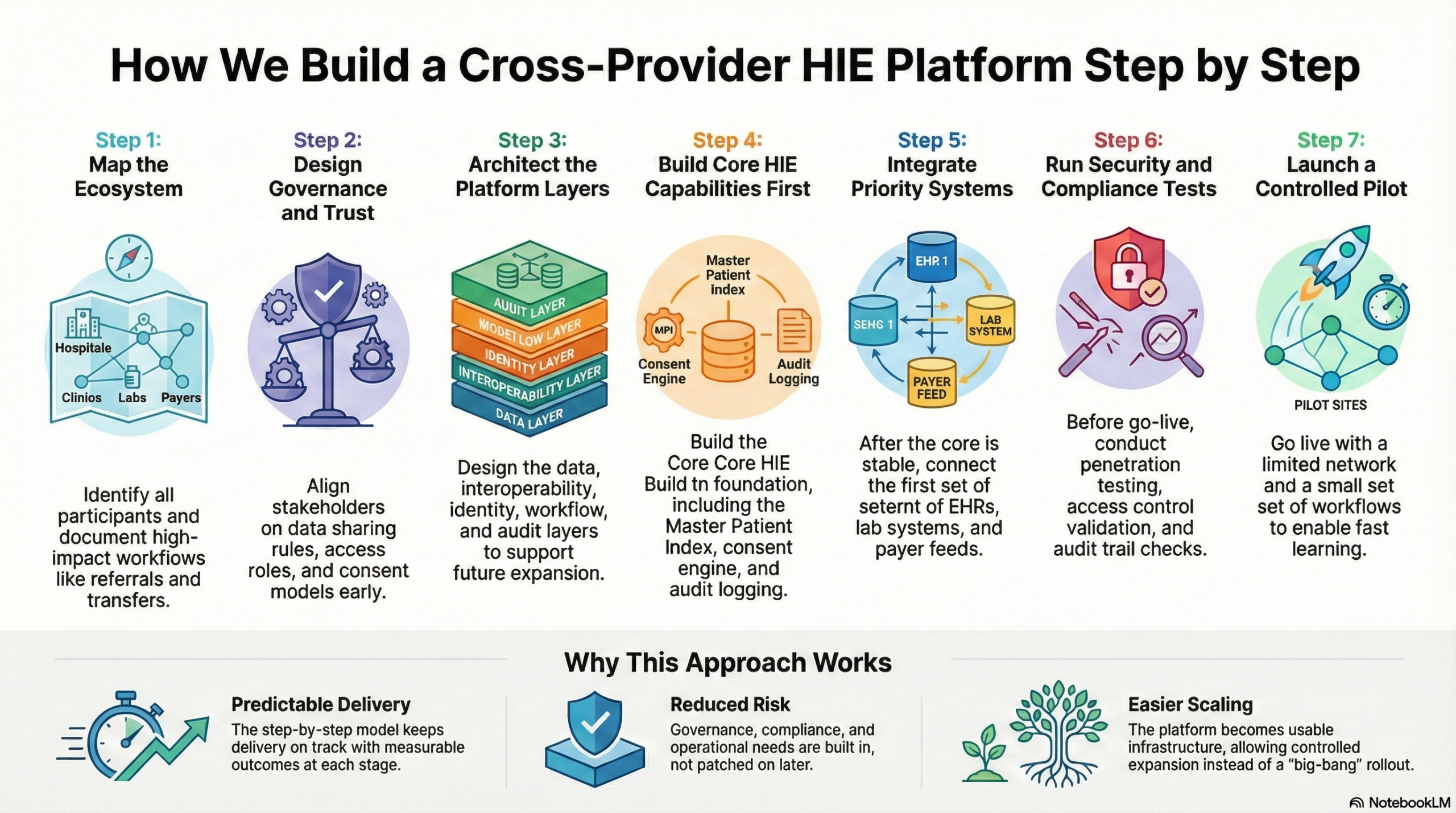
How We Built a Cross-Provider HIE Platform Step by Step
When enterprises invest in HIE software, they want predictable delivery. They also want control over risk, compliance, and long-term scalability. That is why we build in clear phases, with measurable outcomes at each stage.
In addition, we design for cross-provider realities from day one, not after integrations start. This approach reduces rework and prevents governance gaps later.
Step 1: Map the ecosystem
We start by identifying who will participate and how data should move between them. This includes hospitals, clinics, labs, payers, and any public health connections. We also document the high-impact workflows, such as referrals, transfers, and discharge sharing.
Therefore, the platform scope is based on real care journeys, not assumptions. We define what “good” looks like in accuracy, speed, and availability.
Step 2: Design governance and trust boundaries
Cross-provider exchange fails when policies are unclear. So we align stakeholders on data sharing rules early. We define access roles, consent models, and emergency override policies. In addition, we establish audit expectations and shared accountability. This becomes the governance blueprint for the platform. As a result, teams avoid policy debates during build and rollout.
Step 3: Architect the platform layers
Next, we design the architecture as a layered infrastructure. We plan the data layer, interoperability layer, identity and consent layer, workflow layer, and audit layer. We also choose the right deployment model, such as cloud, hybrid, or on-prem.
Therefore, the architecture supports both current needs and future expansion. This is where we remove hidden scale risks early.
Step 4: Build the core HIE capabilities first
We then build the foundation before adding integrations. This includes the Master Patient Index, consent and authorization engine, and audit logging. We also implement the interoperability layer using standards like FHIR where possible.
In addition, we built data normalization so shared records remain clinically usable. As a result, the platform can handle real-world data variation from the start.
Step 5: Integrate priority systems
After the core is stable, we connect the first set of EHRs, lab systems, imaging systems, and payer feeds. We validate patient matching accuracy, field mapping, and code consistency.
We also test real workflows, such as referral handoffs and discharge summaries. Therefore, integration testing focuses on clinical usability, not just successful API calls. This reduces downstream operational friction.
Step 6: Run Security And Compliance Tests
Before go-live, we test the system as if it were already under scrutiny. This includes penetration testing, access control validation, and audit trail checks. We also verify consent behavior across edge cases, including revocation and emergency access.
In addition, we confirm that logging and reporting meet compliance requirements. As a result, the platform is defensible, not just functional.
Step 7: Launch a controlled pilot
We launch with a limited network and a small set of high-value workflows. This allows fast learning without putting the full ecosystem at risk. We track adoption, performance, and exception handling during real usage.
Therefore, scaling becomes a controlled expansion, not a big-bang rollout. We then onboard new providers in waves with clear readiness criteria.
Why this approach works for enterprise leaders
This step-by-step model keeps delivery predictable and reduces risk across multiple organizations. It also ensures governance, compliance, and operational workflows are built in, not patched later.
As a result, HIE software becomes a usable infrastructure rather than a recurring integration project. For enterprises, that translates into faster coordination, stronger control, and easier scaling.
Cost of Developing a Cross-Provider HIE Platform
At Intellivon, cross-provider HIE platforms are built as a regulated healthcare data infrastructure, not as simple data connectors layered onto existing systems. The focus remains on creating platforms that operate reliably across hospitals, clinics, labs, payers, and public health networks. Every design decision accounts for governance, interoperability, and long-term regulatory exposure from the start.
When budget constraints exist, scope is refined with intent. However, security controls, identity resolution, consent enforcement, auditability, and compliance logic are never reduced. Therefore, enterprises avoid remediation costs that typically surface after launch. Predictability replaces rework, and long-term ROI remains protected.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Regulatory Alignment | HIE model definition, participant mapping, jurisdiction analysis, compliance assessment | $5,000 – $10,000 |
| Secure Architecture Design | Layered HIE architecture, identity flows, consent logic, governance design | $6,000 – $12,000 |
| Governance & Policy Framework | Access rules, audit workflows, data-sharing policies, and exception handling | $5,000 – $10,000 |
| Backend & Enterprise Integrations | EHRs, LIS/RIS, payer systems, identity registries, APIs | $10,000 – $20,000 |
| Frontend & Role-Based Interfaces | Clinician, admin, auditor, and partner dashboards | $6,000 – $12,000 |
| Master Patient Index & Data Normalization | Identity resolution, clinical code harmonization | $5,000 – $10,000 |
| Security & Compliance Controls | Encryption, access enforcement, monitoring, breach safeguards | $5,000 – $10,000 |
| Testing & Compliance Validation | Functional testing, security testing, and audit readiness | $4,000 – $8,000 |
| Deployment & Scale Readiness | Cloud or hybrid setup, performance tuning, and monitoring | $4,000 – $8,000 |
Total initial investment: $50,000 – $150,000
Ongoing maintenance and optimization: ~15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-scoped HIE programs face pressure when indirect cost drivers are ignored. Planning for these early protects budgets, timelines, and compliance posture as participation scales.
- Integration complexity increases as more provider systems and data types are added
- Compliance overhead grows with audits, reporting, and regulation updates
- Governance requires continuous policy tuning and exception handling
- Infrastructure costs rise with data volume, analytics, and monitoring workloads
- Change management includes onboarding IT, clinical, and operations teams
- Continuous monitoring becomes critical as regulatory scrutiny increases
Best Practices to Avoid Budget Overruns
Based on Intellivon’s experience delivering enterprise healthcare platforms, these practices consistently lead to controlled costs and predictable outcomes.
- Start with a clearly defined HIE operating model before expanding regions or participants
- Embed governance, auditability, and consent into the core architecture
- Use modular components that scale without redesign
- Plan interoperability early to avoid expensive retrofitting
- Maintain observability across performance, security, and compliance
- Design for regulatory evolution rather than one-time certification
Request a tailored proposal from Intellivon’s healthcare and AI platform experts to receive a delivery roadmap aligned with your budget constraints, compliance exposure, and long-term cross-provider interoperability strategy.
Best Practices to Maintain Compliance in Cross-Provider HIE Platforms
Designing a compliant HIE platform is only the first step. Maintaining compliance over time is where most enterprises struggle. Regulations evolve, participants change, and data volumes grow.
Therefore, compliance must be treated as an ongoing operational discipline, not a one-time milestone. Below are the practices that help enterprises sustain compliance at scale.
1. Monitor compliance continuously, not periodically
Annual audits alone are no longer sufficient. Instead, compliance must be monitored in real time across the platform.
This includes tracking access patterns, policy violations, and unusual data activity. Automated alerts allow teams to respond before issues escalate. As a result, risks are contained early rather than discovered late.
Continuous monitoring also builds confidence with regulators and partners alike.
2. Enforce role-based and context-aware access
Not everyone should see everything, even within trusted networks. Access must depend on who the user is and why they need the data.
This includes the provider role, the care context, and the patient’s consent status. Emergency access should be allowed, but always logged and reviewed. This ensures care delivery stays flexible while remaining legally defensible.
3. Centralize consent and policy management
Fragmented consent management is one of the fastest ways to lose compliance control. A cross-provider HIE must manage consent and policies from a central point. This ensures that patient preferences apply consistently across all participating organizations.
It also allows quick updates when regulations change. As a result, enterprises avoid conflicting rules and accidental violations.
4. Conduct regular cross-provider audits
Auditing one hospital or clinic at a time is not enough. Compliance must be reviewed at the network level, not just locally. This includes shared reports, provider-level scorecards, and joint remediation processes.
These audits reinforce accountability across the ecosystem. They also help align participants around common standards and expectations.
5. Keep regulatory logic adaptable
Healthcare regulations rarely remain static. HIE platforms must support configurable compliance rules rather than hard-coded policies. This allows enterprises to respond quickly to new mandates without rebuilding core systems.
Therefore, regulatory change becomes manageable instead of disruptive. This flexibility protects long-term platform viability.
6. Train operators and providers continuously
Many compliance failures are operational, not technical. Staff must understand how consent works, how access is granted, and how incidents are reported.
Training should occur during onboarding and whenever workflows change. This ensures compliance remains embedded in daily operations. A well-trained network is as important as a well-built platform.
7. Align AI and analytics with compliance policies
As analytics and AI become part of HIE platforms, compliance must extend to how insights are generated and used.
Data minimization, explainability, and auditability must apply to algorithms as well. Without this alignment, AI can quickly become a compliance risk. With it, AI becomes a safe and powerful extension of the platform.
Compliance failures in cross-provider HIEs rarely stay isolated. They affect every participant and undermine trust across the network.
By treating compliance as a continuous system rather than a checklist, enterprises protect both their reputation and their ability to scale. In the long run, this discipline becomes a competitive advantage, not just a legal necessity.
Conclusion
Cross-provider HIE platforms are no longer optional systems. They are becoming core infrastructure for modern healthcare enterprises. As care delivery expands across organizations, data must move with the same speed and reliability. When built correctly, HIEs reduce operational friction, strengthen compliance, and improve clinical outcomes at scale.
However, success depends on more than technology. It requires the right architecture, governance, and long-term discipline. This is where many initiatives succeed or fail. At Intellivon, we build HIE platforms as enterprise-grade, AI-ready healthcare infrastructure. If you are planning to connect providers, scale safely, and lead in digital health, we are ready to partner with you.
Build A Cross-Provider HIE Software With Intellivon
At Intellivon, cross-provider HIE platforms are built as regulated healthcare data infrastructure, not as data-sharing features layered onto existing systems. Every architectural and delivery decision prioritizes compliance, interoperability, and long-term operational resilience. This ensures HIE platforms operate reliably across hospitals, clinics, labs, payers, and public health networks, not just during pilot deployments.
As HIE programs expand across regions, provider groups, and care models, stability becomes critical. Governance, performance, and audit readiness remain consistent as participation and data volume grow. Organizations retain control over identity, consent, and data access without introducing fragmentation, regulatory risk, or operational complexity.
Why Partner With Intellivon?
- Enterprise-grade HIE architecture designed for regulated, multi-provider healthcare ecosystems
- Proven delivery across hospital networks, insurers, digital health platforms, and public health programs
- Compliance-by-design approach with audit readiness and policy enforcement built into the core
- Secure, modular infrastructure supporting cloud, hybrid, and on-prem deployments
- AI enablement for analytics, automation, and decision support with governance and oversight
Book a strategy call to explore how Intellivon can help you build and scale a cross-provider HIE platform with confidence, control, and long-term enterprise value.
FAQs
Q1. What is cross-provider HIE software in healthcare?
A1. Cross-provider HIE software is a platform that enables secure data exchange between independent healthcare organizations such as hospitals, clinics, labs, and payers. It allows patient information to move across care settings while enforcing consent, compliance, and audit controls.
Q2. How is a cross-provider HIE different from EHR integration?
A2. EHR integration connects systems within a single organization. In contrast, a cross-provider HIE operates across multiple independent organizations, requiring neutral governance, shared accountability, and compliance across different regulatory and operational boundaries.
Q3. How long does it take to build a cross-provider HIE platform?
A3. Most enterprise-grade cross-provider HIE platforms take between 6 to 12 months to build and launch, depending on the number of participants, regulatory scope, and integration complexity. Phased rollouts often reduce risk and speed early value delivery.
Q4. What are the biggest challenges in implementing a cross-provider HIE?
A4. The main challenges include patient identity matching across systems, aligning governance between organizations, managing consent consistently, integrating legacy systems, and maintaining compliance as the network scales.
Q5. Is cross-provider HIE software compliant with healthcare regulations by default?
A5. No HIE platform is compliant by default. Compliance depends on how the software is designed, configured, and operated. Enterprise-grade HIE platforms embed consent management, auditability, and security controls to support HIPAA, GDPR, and other regulatory requirements.