Custom hospital software platforms start to incur costs before development begins. In hospitals, teams first define user access, map clinical workflows, review compliance needs, and set security rules while the platform still exists only as an idea. These early decisions quietly shape the total cost of developing custom hospital software platforms.
In 2026, custom hospital software platforms are at the core of daily healthcare operations. Patient access, clinical workflows, revenue cycle performance, and analytics depend on systems that can manage audits, upgrades, and heavy usage. Because of this, compliance strength, architectural stability, and interoperability depth significantly affect how enterprise budgets are organized.
At Intellivon, we create custom hospital software platforms as a regulated healthcare infrastructure. Our teams focus on interoperability, compliance by design, and long-term scalability from the outset. In this blog, we explain how the cost of developing custom hospital software platforms increases, where governance raises spending, and how healthcare enterprises can plan platforms that remain stable as they grow.
Why the Cost to Develop Custom Hospital Software Platforms Is Rising in 2026
In 2026, the cost to develop custom hospital software platforms continues to rise. Demand for advanced integrations, tighter regulations, and skilled talent is pushing budgets upward.
As a result, many healthcare enterprises are seeing development costs grow by 15 to 25% each year. This increase reflects growing platform complexity that often outpaces efficiency gains.
The global hospital information system market reached USD 157.93 billion in 2024. It grew to about USD 185.25 billion in 2025 and is projected to hit nearly USD 778.83 billion by 2034. This steady rise reflects strong demand across healthcare providers. Overall, the market is expected to expand at a CAGR of 17.30 percent between 2025 and 2034.
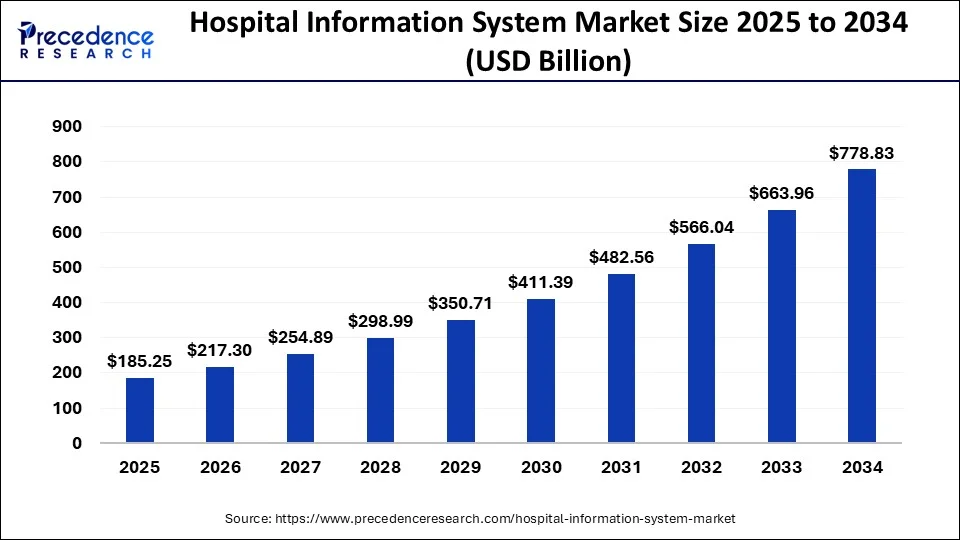
Market Insights:
- Cloud-based solutions lead adoption because they improve scalability and help control infrastructure costs across growing healthcare environments.
- AI and machine learning strengthen diagnostics and enable predictive analytics that support faster, more informed clinical and operational decisions.
- Rising chronic disease rates, higher hospital admissions, and stronger interoperability demands continue to accelerate digital platform adoption across health systems.
- Government digital health initiatives are further encouraging providers to modernize legacy hospital IT environments and invest in connected care infrastructure.
- Interoperability platforms and mobile applications enable real-time data exchange, which helps reduce operational waste, estimated at about 40% by the WHO.
The cost to develop custom hospital software platforms is rising because hospitals now demand enterprise-scale systems that support interoperability, compliance, and long-term operational resilience.
1. From HIS to Enterprise Platforms
Traditional hospital information systems were built to support basic recordkeeping and administrative workflows. However, modern health systems expect far more from their digital infrastructure.
Today’s platforms must coordinate patient access, clinical workflows, revenue operations, and analytics across multiple facilities. As a result, the engineering scope expands beyond simple modules into full enterprise orchestration. This shift is one of the primary reasons the cost to develop custom hospital software platforms continues to rise.
2. Regulatory and Interoperability Pressure
Compliance and interoperability are core architectural requirements that shape platform design from the earliest planning stages.
Healthcare organizations must now support standards such as HL7 and FHIR while maintaining strict security, consent, and audit controls. In addition, integrations with EHRs, labs, imaging systems, and payer networks require rigorous validation and ongoing maintenance.
Consequently, governance and testing overhead significantly increase total development costs.
3. Off-the-Shelf Technical Debt
Many hospitals initially adopt packaged solutions to move quickly. However, these systems often struggle to scale with enterprise needs.
Over time, organizations encounter limitations in workflow flexibility, interoperability depth, and performance under heavy load. When customization layers pile up, technical debt begins to accumulate.
Eventually, health systems invest in custom platforms to regain control, but remediation work adds to the overall cost burden.
4. Platform vs Application Mindset
There is a growing difference between building applications and engineering healthcare platforms. Applications typically solve a narrow problem.
Platforms, on the other hand, must support evolving workflows, new integrations, and regulatory change over many years. Because of this, enterprise teams are prioritizing modular architecture, governance controls, and scalability from day one.
While this approach requires higher upfront investment, it reduces long-term risk and rework. Still, the immediate effect is a higher cost to develop custom hospital software platforms in 2026.
Rising costs reflect a fundamental shift in how hospitals view digital infrastructure. As healthcare organizations move toward enterprise-grade, interoperable platforms, investment levels naturally increase.
Cost to Develop Custom Hospital Software Platforms in 2026
The cost to develop custom hospital software platforms in 2026 typically ranges from $70,000 to $500,000+, depending on platform scope, interoperability depth, and governance requirements.
The cost to develop custom hospital software platforms in 2026 varies widely across healthcare organizations. Most investments fall between $70,000 for focused solutions and more than $500,000 for enterprise-ready platforms. However, this range only becomes meaningful when viewed in the right context.
There is no single price point because hospitals build very different systems under the same label. Some teams implement departmental tools that support a narrow workflow. Others build connected platforms that coordinate clinical, operational, and financial processes across facilities. Each approach carries a different level of responsibility and engineering effort.
As platform scope expands, costs rise steadily. This increase rarely comes from features alone. Instead, spending grows due to interoperability work, compliance validation, testing cycles, and long-term support needs. Therefore, realistic budgeting begins by clearly defining what type of hospital platform the organization plans to operate.
Custom Hospital Software Platform Cost Comparison by Deployment Type (2026)
| Deployment Type | Typical Use Case | Platform Scope | Expected Cost Range |
| Departmental Hospital Solution | Scheduling tools, basic patient management, and reporting | Low | $70,000 – $120,000 |
| Workflow-Connected Hospital Platform | Clinical workflows, billing integration, care coordination | Medium | $120,000 – $250,000 |
| Multi-Facility Hospital Platform | Patient engagement, operations across hospital groups | Medium–High | $250,000 – $400,000 |
| Enterprise-Grade Hospital Platform | Network-wide clinical, financial, and analytics systems | High | $400,000 – $500,000+ |
These ranges reflect typical production-ready healthcare deployments rather than small proofs of concept. They account for integration scope, governance effort, validation cycles, and readiness for real hospital environments.
Tier-Wise Cost to Develop Custom Hospital Software Platforms
The cost to develop custom hospital software platforms increases with scale. Department tools cost less, while multi-hospital and IDN platforms require higher investment and longer timelines.
As responsibility grows, engineering effort and governance requirements also expand. The tiers below reflect how most healthcare organizations structure their investments in 2026.
1. Department-Level Cost
Department-level solutions focus on a single function such as scheduling, reporting, or basic patient management. These systems usually serve a limited user group and require fewer integrations.
Because the scope stays contained, the development effort remains relatively predictable. However, even small systems must meet healthcare security and compliance standards.
Most organizations choose this tier when they need quick operational improvement without large infrastructure changes.
2. Hospital-Wide Cost
Hospital-wide platforms support multiple departments within one facility. They often connect clinical workflows, billing processes, and operational dashboards.
At this level, interoperability becomes more important. Teams must ensure consistent data flow across systems and user roles. As a result, testing effort and governance work increase.
Many mid-sized hospitals invest in this tier to improve coordination without committing to full network transformation.
3. Multi-Hospital Enterprise Cost
Multi-hospital platforms operate across facility groups or regional networks. These systems must handle higher transaction volumes and more complex identity and consent requirements.
In addition, cross-site reporting and standardized workflows become critical. Engineering teams must design for scalability from the beginning.
Consequently, both cost and delivery timelines increase compared to single-hospital deployments.
4. Academic and IDN Platform Cost
Academic medical centers and integrated delivery networks demand the highest level of platform maturity. These environments typically require advanced analytics, research workflows, and deep interoperability across diverse systems.
Because of this complexity, governance, validation, and performance engineering take significantly more effort. Organizations in this tier usually prioritize long-term platform stability over short-term savings.
Platform Cost Comparison Table
| Platform Scope | Typical Users | Complexity | Cost Range | Timeline |
| Department-Level Solution | Single department teams | Low | $70,000 – $120,000 | 3–5 months |
| Hospital-Wide Platform | Multi-department hospital staff | Medium | $120,000 – $250,000 | 5–8 months |
| Multi-Hospital Platform | Regional hospital networks | Medium–High | $250,000 – $400,000 | 8–12 months |
| Academic / IDN Platform | Large health systems and research centers | High | $400,000 – $500,000+ | 12–18 months |
The cost to develop custom hospital software platforms rises in direct proportion to platform responsibility. Therefore, accurate budgeting starts with defining scope, scale, and integration depth early.
Organizations that align investment with long-term platform goals typically avoid expensive rework later.
Custom Hospital Software ROI Typically Achieved in 3 to 18 Months
Custom hospital software often delivers measurable ROI within 3 to 18 months by improving workflow efficiency, strengthening revenue capture, and reducing operational waste.
The ROI depends on platform scope, deployment scale, and how deeply the software connects with clinical and financial workflows. Below are the key areas where enterprises typically see the fastest returns.
1. Operational Efficiency Gains
One of the earliest benefits appears in day-to-day operations. Custom platforms streamline manual processes that often slow down hospital teams.
For example, automated patient intake, smarter bed management, and digital care coordination reduce administrative workload. As a result, staff spend more time on patient care instead of paperwork. Many hospitals report measurable productivity gains within the first few months after deployment.
2. Revenue Cycle Improvement
Revenue leakage remains a major concern for large providers. Custom hospital software helps tighten billing workflows and improve charge capture accuracy.
Integrated eligibility checks, automated coding support, and cleaner claims submission reduce denials and rework. In addition, finance teams gain better visibility into payment cycles. Therefore, many organizations see revenue uplift shortly after stabilizing the platform.
3. Clinical Productivity Impact
Clinical teams benefit when workflows become more connected and less fragmented. Custom systems reduce the time clinicians spend searching for information across multiple tools.
Unified patient views, faster order management, and real-time alerts support quicker decision-making. Consequently, providers can handle higher patient volumes without increasing staffing at the same pace. This efficiency directly contributes to faster ROI realization.
4. Infrastructure and Cost Reduction
Legacy hospital environments often carry hidden infrastructure costs. Custom platforms built on modern architecture help reduce this burden over time.
Cloud optimization, better resource utilization, and retirement of redundant systems lower ongoing IT spend. In addition, centralized platforms simplify maintenance and support. These savings accumulate steadily and strengthen long-term financial performance.
5. Data Visibility and Strategic Value
Beyond immediate savings, custom hospital software creates long-term strategic value through better data access.
Real-time dashboards, predictive analytics, and cross-facility reporting give leadership clearer insight into performance trends. As a result, organizations can make faster operational and financial decisions. While harder to quantify upfront, this visibility often drives significant downstream value.
Custom hospital software should not be viewed only as a technology expense. When aligned with clinical workflows and financial operations, it becomes a measurable growth lever.
Many healthcare enterprises begin to see returns within 3 to 18 months, especially when platforms are built with interoperability, automation, and scalability in mind. The real advantage comes from sustained efficiency and revenue improvement that compounds over time.
Key Cost Drivers While Developing Custom Hospital Software Platforms
The biggest cost drivers in custom hospital software development include interoperability work, compliance engineering, AI enablement, and enterprise-scale infrastructure requirements.
Below are the areas that most strongly influence the cost to develop custom hospital software platforms in 2026.
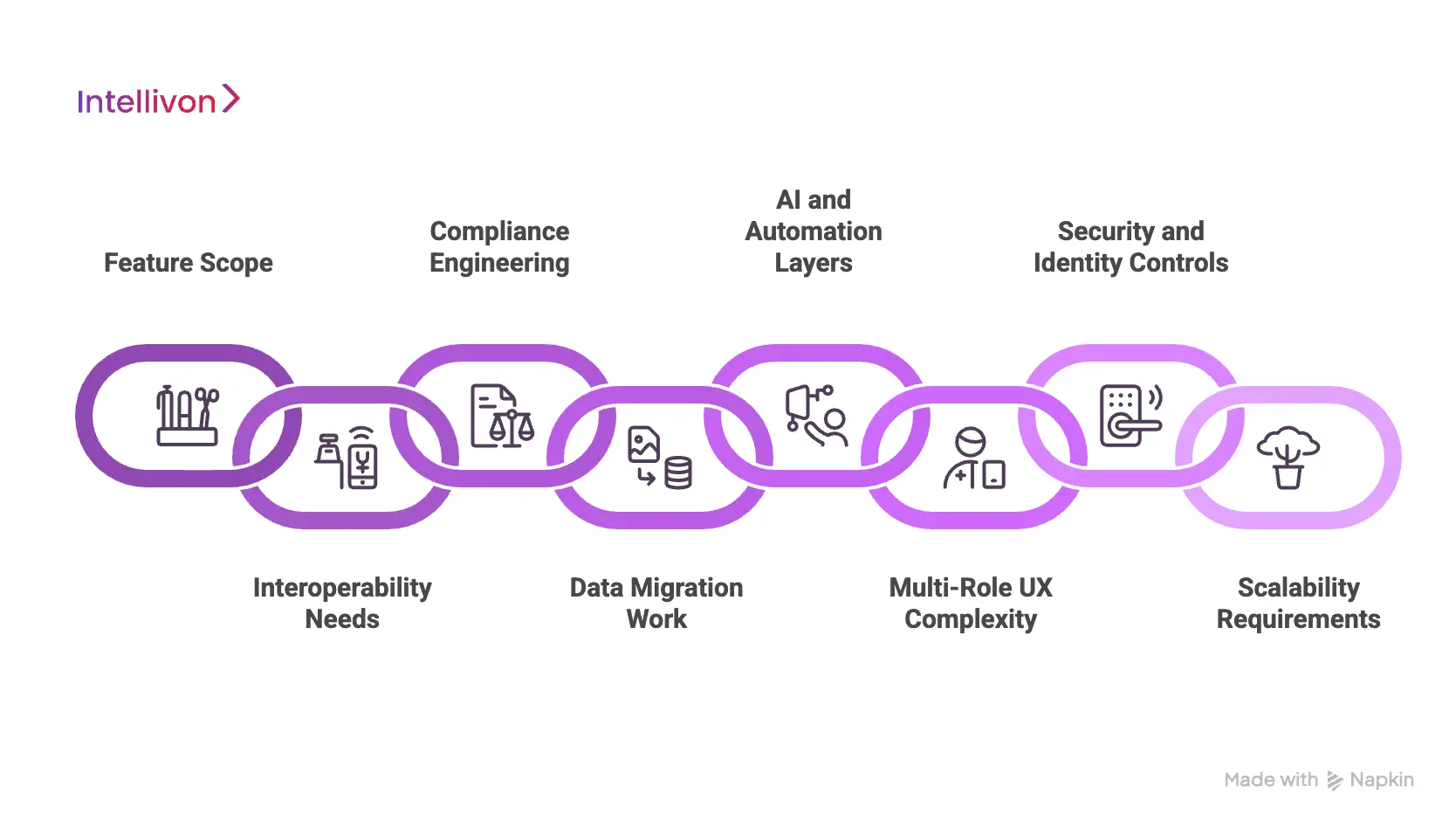
1. Feature Scope
The breadth of clinical and operational features directly affects development effort. Simple scheduling or reporting tools require limited workflows. In contrast, platforms that manage care coordination, billing, and analytics demand more engineering depth.
As feature scope expands, teams must design more workflows, validations, and user permissions. Consequently, both build time and testing effort increase.
2. Interoperability Needs
Interoperability is often the largest hidden cost driver. Most hospital platforms must exchange data with EHRs, labs, imaging systems, and payer networks.
Support for HL7 and FHIR standards adds additional validation and mapping work. In addition, each external connection requires ongoing maintenance. Therefore, platforms with deep ecosystem connectivity typically carry higher long-term costs.
3. Compliance Engineering
Healthcare software must meet strict regulatory expectations from the start. Security controls, audit logging, consent tracking, and data protection mechanisms all require careful implementation.
Unlike many other industries, compliance cannot be added later without risk. Because of this, regulated engineering work significantly increases upfront investment.
4. Data Migration Work
Many hospitals still operate on legacy systems that hold years of clinical and financial data. Moving this data safely into a new platform requires careful planning and validation.
Data cleansing, mapping, and reconciliation often take longer than expected. As a result, migration work can become a major contributor to total project cost.
5. AI and Automation Layers
Advanced analytics and automation features add another cost layer. Predictive models, clinical decision support, and intelligent workflow routing require specialized engineering and data preparation.
While these capabilities deliver strong long-term value, they increase both development complexity and infrastructure needs in the short term.
6. Multi-Role UX Complexity
Hospital platforms must support many different user types. Clinicians, nurses, administrators, and finance teams all interact with the system in different ways.
Designing role-specific dashboards and workflows takes more effort than building a single-user interface. Therefore, UX complexity often expands design and testing timelines.
7. Security and Identity Controls
Healthcare environments demand strong identity management and access controls. Role-based permissions, single sign-on, and consent enforcement must work reliably across systems.
In addition, security teams require detailed monitoring and audit visibility. These safeguards increase engineering and validation work but remain essential for enterprise readiness.
8. Scalability Requirements
Platforms that serve multiple facilities must handle high transaction volumes and peak usage periods. This requires careful infrastructure planning and performance testing.
High-availability architecture, failover planning, and load optimization all add to the total cost. However, these investments prevent stability issues as the organization grows.
The cost to develop custom hospital software platforms depends less on visible features and more on underlying enterprise requirements. Interoperability depth, compliance rigor, and scalability expectations typically drive the largest budget shifts.
Organizations that evaluate these factors early are far better positioned to control costs and build platforms that remain reliable over time.
Phase-Wise Cost to Develop Custom Hospital Software Platforms
Hospital software budgets spread across discovery, engineering, integration, and compliance. Core development takes the largest share, but other phases add high cost.
Many healthcare leaders focus only on the total budget. However, understanding where money actually goes is far more useful during planning. Development is important, yet architecture, interoperability, and validation often consume a large portion of the spend.
Therefore, a phase-wise view helps organizations forecast more accurately. It also prevents underfunding critical steps that protect long-term platform stability.
Phase-Wise Budget Distribution (Typical Enterprise Range)
Example based on a mid-to-large platform budget of $250,000–$400,000.
| Phase | % of Budget | Typical Cost Range | What Enterprises Actually Pay For |
| Discovery and Architecture | 10–15% | $25,000 – $60,000 | Requirements mapping, system design, compliance planning |
| UX and Workflow Design | 15–20% | $37,500 – $80,000 | Clinical UX research, role-based flows, usability validation |
| Core Platform Engineering | 35–45% | $87,500 – $180,000 | Backend services, APIs, data models, core functionality |
| Integration and Interoperability | 10–20% | $25,000 – $80,000 | EHR connections, HL7/FHIR mapping, ecosystem interfaces |
| Testing and Compliance | 10–15% | $25,000 – $60,000 | Security validation, performance testing, and audit readiness |
| Deployment and Rollout | 5–10% | $12,500 – $40,000 | Production setup, training support, and go-live stabilization |
1. Discovery and Architecture Cost
The discovery phase establishes the platform blueprint. Teams define requirements, map workflows, and design the technical foundation.
In healthcare environments, this stage also includes early compliance planning. Although the cost share is smaller, strong discovery work reduces expensive redesign later.
2. UX and Clinical Workflow Cost
Healthcare usability requires careful design across multiple roles. Clinicians, nurses, and administrators all interact differently with the system.
Design teams build role-specific journeys and validate workflows with real scenarios. Therefore, UX investment often grows as workflow complexity increases.
3. Core Engineering Cost
Core platform engineering typically consumes the largest portion of the budget. This phase covers backend services, data architecture, and business logic.
Because this layer supports long-term scalability, quality standards remain high. As a result, engineering effort drives a significant share of total spend.
4. Integration and Interoperability Cost
Most hospital platforms must exchange data across multiple systems. Connections to EHRs, labs, and financial platforms require careful mapping and validation.
Each interface also needs monitoring and maintenance. Consequently, interoperability work often becomes one of the most underestimated cost areas.
5. Testing and Compliance Cost
Healthcare software must pass rigorous validation before going live. Teams conduct functional testing, security checks, and performance validation.
In addition, compliance teams verify audit readiness and data protection controls. Although sometimes overlooked, this phase protects the organization from operational risk.
6. Deployment and Rollout Cost
The final phase prepares the platform for real-world use. Teams configure production environments and support early adoption.
Training and stabilization activities also occur here. While smaller in budget share, a structured rollout prevents disruption after launch.
The cost to develop custom hospital software platforms is distributed across several critical phases. Core engineering takes the largest share, yet interoperability and compliance work significantly influence the final budget.
Organizations that plan phase-wise investments early are far more likely to deliver stable, enterprise-ready systems without cost overruns.
Hidden Costs While Developing Custom Hospital Software Platforms
Hidden costs in custom hospital software projects often come from interoperability upkeep, compliance updates, data cleanup, and post-launch support rather than initial development.
Therefore, organizations that identify hidden cost areas early can protect both timelines and budgets. Below are the most common expense drivers that surface in real enterprise deployments.
1. Interoperability Maintenance
Initial integrations are only the starting point. Once the platform goes live, interfaces with EHRs, labs, and external systems require continuous monitoring.
Standards evolve, vendor APIs change, and data mappings need periodic updates. As a result, ongoing interoperability maintenance can quietly increase total ownership costs over time.
2. Compliance Updates
Healthcare regulations do not remain static. Security policies, audit requirements, and privacy controls often change as new guidance emerges.
Each update may require code adjustments, validation cycles, and documentation work. Therefore, compliance engineering should be treated as a recurring investment rather than a one-time task.
3. Data Migration Cleanup
Legacy data rarely moves cleanly into modern platforms. During migration, teams often discover duplicate records, missing fields, or inconsistent formats.
Fixing these issues requires manual review, mapping adjustments, and reconciliation checks. Consequently, data cleanup can extend timelines and increase project costs if not planned properly.
4. Infrastructure Scaling
Early environments are usually sized for pilot usage. However, once adoption grows, infrastructure demands increase quickly.
Higher transaction volumes, more concurrent users, and expanded analytics workloads all drive additional cloud or hosting costs. Planning for scale from the beginning helps avoid sudden budget pressure later.
5. Change Management and Training
Technology adoption depends heavily on user readiness. Clinicians and administrative teams often need structured training and workflow adjustments.
If change management is underfunded, productivity may drop during rollout. Therefore, successful programs allocate budget for onboarding, support, and user enablement activities.
6. Post-Launch Enhancements
No hospital platform remains static after go-live. Users quickly request refinements, new reports, and workflow improvements.
Without a structured enhancement roadmap, these updates can accumulate into unplanned spending. Smart organizations reserve capacity for continuous improvement from the start.
The cost to develop custom hospital software platforms extends well beyond initial development. Interoperability upkeep, regulatory changes, infrastructure growth, and user adoption all influence long-term spend.
Healthcare organizations that plan for these hidden costs early are far better positioned to protect ROI and maintain platform stability as operations expand.
Build vs Buy vs Modernize: Which Is Better
The right path for custom hospital software depends on workflow complexity, interoperability depth, and long-term control requirements, not just upfront cost.
Healthcare organizations rarely start from the same baseline. Some operate rigid legacy environments. Others rely on packaged HIS tools that limit flexibility. Therefore, the decision to build, buy, or modernize should reflect long-term operational strategy, not short-term budget pressure.
In practice, the cost to develop custom hospital software platforms must be evaluated against hidden licensing costs, integration limits, and future scalability needs. Leaders who assess total ownership early make far more stable technology investments.
Build vs Buy vs Modernize Comparison
| Approach | Upfront Cost | Long-Term Cost Profile | Risk Level | Best Fit Scenario |
| Buy (Off-the-Shelf HIS) | Low | Can rise with licensing, customization, and vendor dependency | Medium | Hospitals needing rapid deployment with standard workflows |
| Build (Custom Platform) | Medium to High | Often lower at scale with full architectural control | Medium* | Health systems requiring deep integration and long-term flexibility |
| Modernize (Legacy Extension) | Medium | Variable and can increase if technical debt persists | Medium to High | Organizations preserving legacy investments while improving capabilities |
Risk depends heavily on partner expertise and architectural discipline.
1. When Buying Works
Buying makes sense when speed and predictability matter most. Hospitals can deploy faster and avoid large upfront engineering programs.
This path typically fits smaller providers or clearly defined use cases. However, over time, licensing growth and customization limits may reduce flexibility. Therefore, buyers should evaluate vendor lock-in risk and integration depth early in the process.
2. When Custom Build Wins
Custom development becomes the stronger option when workflows are complex or highly differentiated. Multi-facility health systems often require tighter control over data flow and user experience.
A well-architected platform supports interoperability, automation, and phased expansion. Although the initial investment is higher, many enterprises achieve better long-term economics and strategic control. This is especially true when platforms become core operational infrastructure.
3. When Modernization Makes Sense
Modernization works best when legacy systems still provide operational value. Instead of full replacement, organizations upgrade selected components or introduce interoperability layers.
This approach reduces short-term disruption and protects prior investments. However, technical debt can remain if the underlying architecture stays constrained. Therefore, modernization should include a clear roadmap toward future platform flexibility.
Each path carries trade-offs across cost, risk, and long-term flexibility. In the next section, we explore practical strategies organizations use to control the cost to develop custom hospital software platforms while still building for enterprise scale.
How to Reduce the Cost to Develop Custom Hospital Software Platforms
Hospitals can reduce the cost to develop custom hospital software platforms by adopting modular architecture, prioritizing interoperability early, and aligning compliance from the start.
Controlling costs in healthcare software is less about cutting features and more about making smart architectural decisions early. Many overruns occur because teams underestimate integration work, compliance effort, or long-term scalability needs. Therefore, the most effective savings come from disciplined planning rather than late-stage budget cuts.
Healthcare organizations that treat platform engineering as a phased, governed program typically achieve better financial outcomes. The strategies below reflect what works in real enterprise environments.
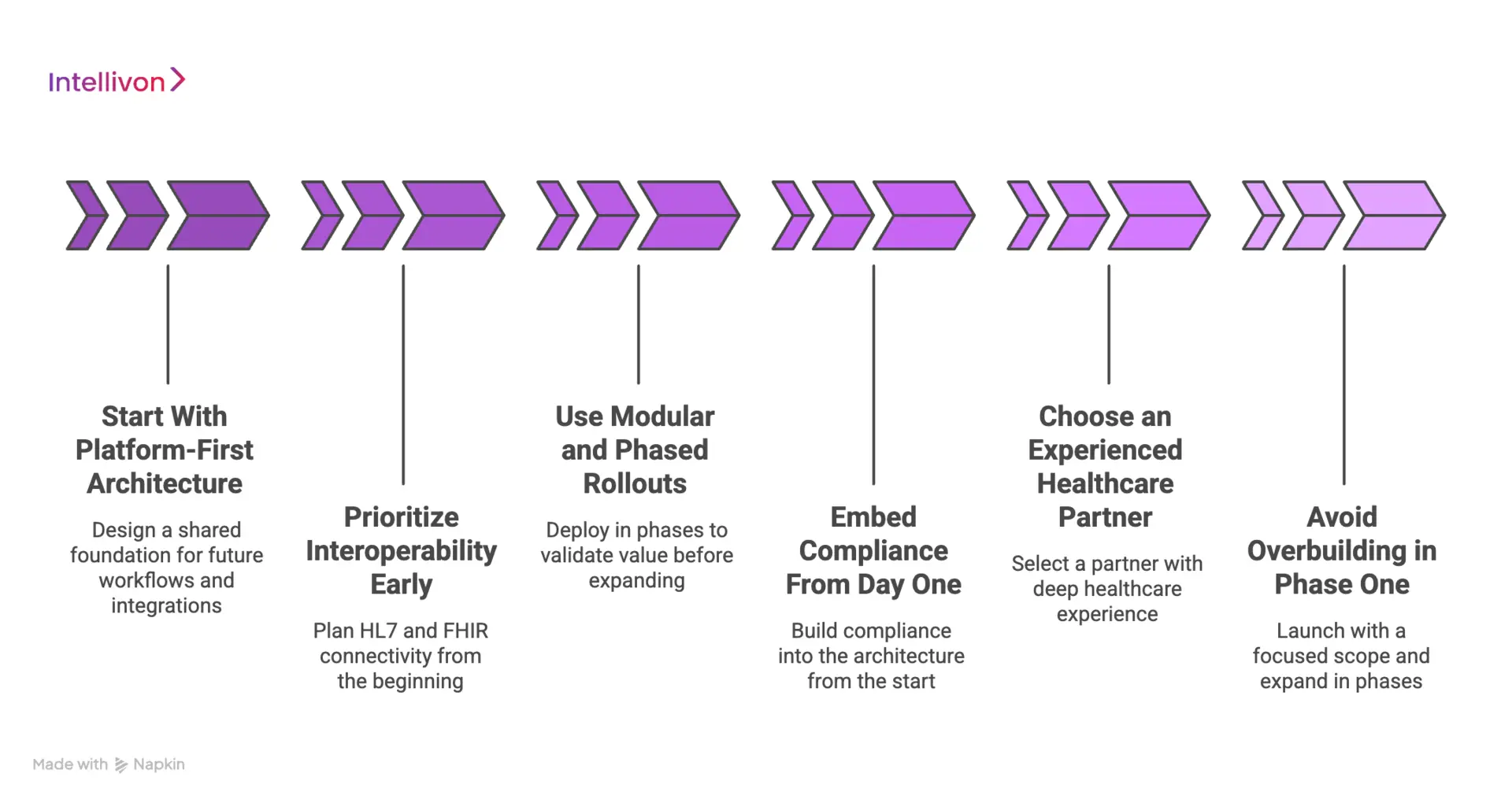
1. Start With Platform-First Architecture
A platform-first approach prevents expensive rework later. Instead of building isolated modules, teams design a shared foundation that supports future workflows and integrations.
This method improves reuse and reduces duplication across departments. As a result, new capabilities can be added without rebuilding core components. Over time, this significantly lowers total development and maintenance costs.
2. Prioritize Interoperability Early
Interoperability is one of the most underestimated cost drivers. When integrations are added late, teams often face complex redesign and data mapping issues.
By planning HL7 and FHIR connectivity from the beginning, organizations avoid expensive retrofits. In addition, early interface planning improves data quality and reduces long-term maintenance effort.
3. Use Modular and Phased Rollouts
Large, all-at-once deployments carry higher financial and operational risk. A phased rollout allows teams to validate value before expanding investment.
Modular delivery also helps organizations spread budget across milestones. Therefore, leadership gains better financial control while still moving toward enterprise scale.
4. Embed Compliance From Day One
Compliance work becomes costly when treated as an afterthought. Retrofitting security, audit controls, or consent management often requires significant redesign.
Instead, organizations should build compliance into the architecture from the start. This approach reduces validation cycles and prevents costly remediation later in the program.
5. Choose an Experienced Healthcare Partner
Execution quality has a direct impact on total cost. Teams with deep healthcare experience anticipate interoperability, governance, and workflow challenges earlier.
As a result, they avoid many of the delays and redesign cycles that inflate budgets. Partner selection, therefore, is one of the most important cost control decisions leaders make.
6. Avoid Overbuilding in Phase One
Many organizations attempt to deliver full enterprise capability in the first release. This often increases risk and delays time to value.
A more effective approach is to launch with a focused, high-impact scope and expand in phases. This strategy improves early ROI and keeps the initial investment more predictable.
Reducing the cost to develop custom hospital software platforms requires disciplined planning and not a feature compromise. Organizations that prioritize architecture, interoperability, and phased delivery consistently achieve stronger financial outcomes. With the right strategy in place, healthcare leaders can control costs while still building platforms that scale confidently over time.
Conclusion
Custom hospital software is no longer just an IT expense. It is a strategic investment that shapes efficiency, revenue performance, and long-term scalability. Organizations that plan architecture, interoperability, and compliance early typically control costs more effectively.
With the right approach, the cost to develop custom hospital software platforms becomes predictable and value-driven. Intellivon helps healthcare enterprises build secure, scalable platforms that deliver measurable impact and support sustainable digital growth.
Why Choose Intellivon for Custom Hospital Platforms
At Intellivon, custom hospital software platforms are engineered as regulated healthcare infrastructure, not disconnected applications layered onto legacy environments. Every architectural and delivery decision prioritizes interoperability depth, governance controls, and long-term operational resilience.
As hospital platforms expand across departments, facilities, and partner ecosystems, consistency becomes essential. Performance, compliance posture, and audit readiness remain stable even as user volume, transaction load, and workflow complexity increase. This disciplined approach helps healthcare organizations scale without introducing fragmentation or operational risk.
Why Partner With Intellivon?
- Enterprise-grade hospital platform architecture designed for regulated healthcare ecosystems
- Proven delivery across multi-hospital networks and complex clinical environments
- Compliance-by-design framework with embedded audit visibility and policy enforcement
- Secure, modular platform supporting cloud, hybrid, and on-prem deployments
- AI-ready foundation enabling advanced analytics, automation, and predictive intelligence
Book a strategy call to explore how Intellivon can help you design and scale custom hospital software platforms with confidence, control, and long-term enterprise value.
FAQs
Q1. How much does it cost to develop custom hospital software?
A1. The cost to develop custom hospital software typically ranges from $70,000 to $500,000 or more. The final budget depends on platform scope, interoperability depth, compliance requirements, and the number of facilities involved.
Q2. What factors increase hospital software development costs the most?
A2. The biggest cost drivers include EHR integration, HL7 and FHIR interoperability, regulatory compliance, multi-role workflows, and scalability requirements. In addition, data migration and AI features can significantly increase total investment.
Q3. How long does it take to build a custom hospital platform?
A3. Most hospital software platforms take between 3 and 18 months to build. Smaller departmental tools launch faster, while multi-hospital or enterprise platforms require longer timelines due to integration and validation work.
Q4. Is custom hospital software worth the investment for large providers?
A4. Yes, many healthcare organizations achieve strong ROI through improved efficiency, better revenue capture, and reduced manual work. However, value depends on proper architecture, interoperability planning, and a phased rollout strategy.
Q5. Can hospitals reduce the cost of developing custom software platforms?
A5. Yes. Hospitals can control costs by using modular architecture, prioritizing interoperability early, embedding compliance from the start, and rolling out features in phases. Choosing an experienced healthcare technology partner also reduces expensive rework.