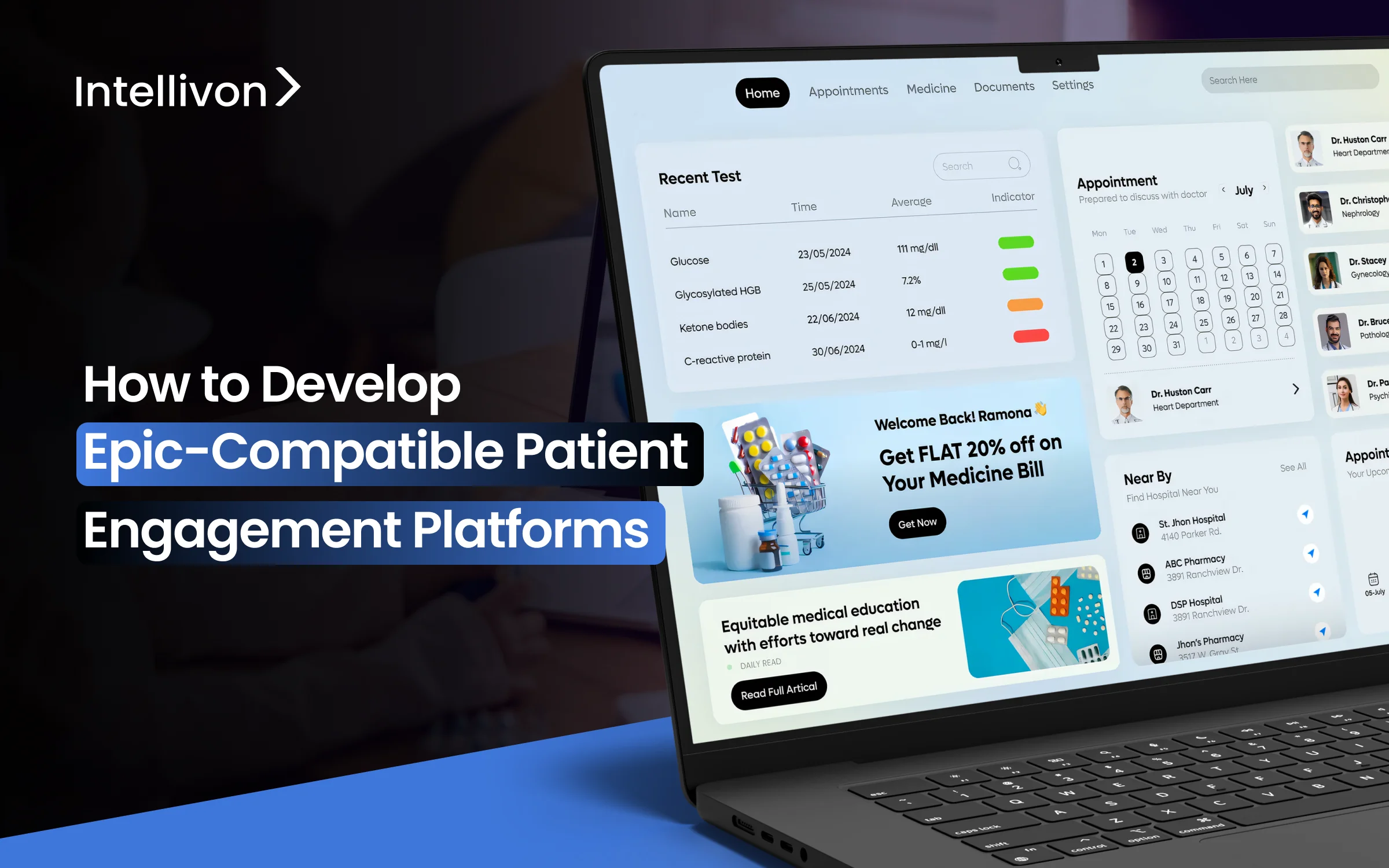
Patient engagement platforms are often grouped together, but only a small number can function reliably in Epic environments. Epic-compatible patient engagement platforms are a specific type of enterprise healthcare system. In large healthcare organizations, engagement typically breaks down into access, care coordination, and follow-ups.
Teams often rely on disconnected tools that do not fit within Epic workflows. Over time, this fragmentation leads to operational inefficiencies, compliance risks, and limits visibility throughout the patient journey.
Intellivon develops Epic-compatible patient engagement platforms as part of the enterprise healthcare infrastructure. These platforms connect engagement workflows with Epic-controlled data, identity, and clinical processes. This way, engagement becomes part of care delivery instead of an additional digital layer.
Many organizations think that Epic compatibility simply means having API access or App Orchard certification. While that improves connectivity, it does not guarantee enterprise reliability. Without careful platform design, engagement tools have a hard time scaling across hospitals and regions. This blog explains what these platforms contain, how they function within Epic environments, and how we can build them from the ground up.
Key Takeaways Of The Patient Engagement Platforms Market
Patient engagement platforms are gaining traction as healthcare organizations digitize care delivery. At the same time, chronic conditions and value-based care models are increasing the need for continuous patient interaction.
These platforms support portals, mobile experiences, and virtual care touchpoints. More importantly, they help enterprises improve communication, treatment adherence, and care outcomes across large patient populations.
The patient engagement platforms market continues to expand rapidly. In 2025, the market is estimated at USD 31.0 billion and is projected to reach USD 149.2 billion by 2035. This growth reflects a compound annual growth rate (CAGR) of 17.0% over the forecast period.
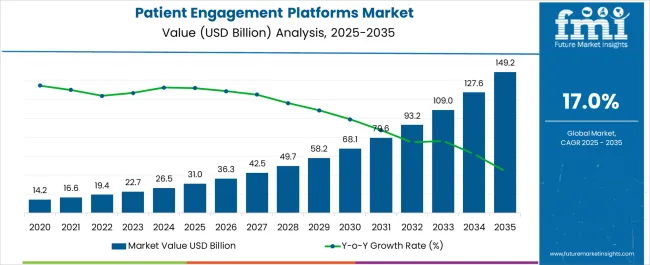
Key Drivers:
- Shift toward patient-centric and value-based care models increases demand for continuous, measurable patient engagement.
- Deeper EHR integration, cloud platforms, and analytics enable real-time engagement within governed clinical workflows.
- Rising chronic disease burden, combined with regulatory mandates such as HITECH, pushes enterprises toward standardized engagement platforms.
Adoption Trends in Enterprise Healthcare
- Providers hold the largest share as hospitals and clinics integrate engagement platforms for scheduling, communication, and care coordination.
- Technology-led platforms account for nearly 68% of market revenue, reflecting growing reliance on scalable, software-driven engagement models.
- Cloud and web-based deployments dominate as enterprises prioritize flexibility, faster rollout, and multi-site scalability over on-premise systems.
Epic-compatible patient engagement platforms help enterprises reduce appointment no-shows and avoidable readmissions. At the same time, portals and mobile apps improve treatment adherence by keeping engagement connected to clinical workflows.
These platforms also deliver measurable financial impact. In the U.S., healthcare systems estimate USD 24–48 billion in annual savings through productivity gains and operational efficiencies.
Meanwhile, multi-channel engagement across portals, messaging, and telehealth streamlines workflows for health systems. As a result, teams reduce manual effort while maintaining consistent patient communication at scale.
What Is an Epic-Compatible Patient Engagement Platform?
An Epic-compatible patient engagement platform is an enterprise system designed to work inside Epic-governed workflows, not alongside them. It enables patient communication, scheduling, care updates, and follow-ups while respecting Epic’s data models, identity controls, and compliance rules.
Unlike standalone apps, it stays connected to clinical workflows, ensuring engagement remains accurate, secure, and operationally reliable at scale.
Difference Between Generic and Epic-Compatible PEPs
Not all patient engagement platforms serve the same purpose. While many tools focus on communication or experience, only a specific class can operate reliably inside Epic environments. Understanding this difference is critical for enterprises planning long-term, scalable engagement strategies.
Generic platforms prioritize speed and surface-level engagement. Epic-compatible enterprise platforms, however, are designed to function within governed clinical workflows, identity systems, and compliance frameworks.
Generic vs Epic-Compatible Patient Engagement Platforms
| Aspect | Generic Engagement Platforms | Epic-Compatible Enterprise PEPs |
| Core purpose | Improve patient communication and experience | Enable engagement within Epic-governed clinical workflows |
| Relationship with Epic | Operates outside Epic with limited or no workflow alignment | Operates inside Epic workflows and governance boundaries |
| Integration depth | API-level or data-sync integration | Workflow, identity, consent, and audit-level integration |
| Identity & access | Separate login and access logic | Inherits Epic identity, proxy access, and role controls |
| Consent management | App-level or manual consent handling | Epic-aligned consent and authorization enforcement |
| Clinical reliability | Suitable for lightweight engagement | Designed for clinical-grade, enterprise reliability |
| Scalability | Struggles as usage and complexity grow | Scales across hospitals, regions, and care models |
| Enterprise compliance | Requires additional controls | Built to meet healthcare compliance requirements by design |
Choosing a generic engagement platform may work for pilots or limited use cases. However, these tools often create parallel workflows and governance gaps as adoption grows. Over time, this leads to operational risk and limited scalability.
Epic-compatible patient engagement platforms avoid these issues by design. They embed engagement directly into Epic environments, allowing enterprises to scale engagement without fragmenting workflows, identity, or compliance controls.
Where Epic-Compatible Patient Engagement Platforms Operate
Epic-compatible patient engagement platforms do not sit outside care delivery. Instead, they operate within the systems that already govern how care is delivered, managed, and regulated. This distinction defines why they scale reliably in enterprise environments.
1. Clinical Workflows
Epic-compatible PEPs work directly within clinical workflows such as scheduling, test results, care plans, and follow-ups. Engagement triggers align with real clinical events rather than manual updates. As a result, patients receive timely and relevant communication without disrupting care delivery.
Because these platforms follow Epic workflows, clinicians avoid duplicate work. Engagement supports care instead of creating parallel processes that must be managed separately.
2. Provider Operations
Beyond clinical care, Epic-compatible PEPs support day-to-day provider operations. They align with how staff manage access, communication, and coordination across departments. This keeps engagement consistent across hospitals, clinics, and care teams.
When engagement operates within provider workflows, teams gain better visibility. Operations remain predictable even as patient volume and complexity increase.
3. Compliance and Governance Frameworks
Epic governs identity, consent, access, and auditability across healthcare systems. Epic-compatible PEPs respect these controls instead of recreating them externally. This ensures engagement remains compliant as regulations evolve.
By operating within Epic’s governance framework, enterprises reduce risk. Engagement stays traceable, secure, and manageable at scale.
Epic-compatible patient engagement platforms succeed because they operate where care already happens. By aligning with clinical workflows, provider operations, and governance frameworks, they deliver engagement without compromising reliability or compliance.
65% Portal Adoption Shows Why Engagement Must Work Inside Epic
Patient engagement no longer sits at the edges of healthcare delivery. With 65% of individuals actively using patient portals and proxy access rising from 24% to 51%, engagement has become a shared, system-level expectation. This shift has direct implications for how enterprises design and deploy patient engagement platforms.
As usage expands across patients and caregivers, engagement must operate within governed clinical systems. Epic-compatible patient engagement platforms address this need by aligning access, identity, and workflows inside Epic environments rather than outside them.
1. Engagement Has Moved Into Enterprise Workflows
Portal usage at this scale signals a clear shift in behavior. Patients and caregivers now expect engagement to reflect real clinical activity, not disconnected updates. As a result, engagement workflows increasingly intersect with scheduling, results, care plans, and follow-ups.
When engagement operates outside Epic, enterprises struggle to maintain consistency. Duplicate workflows emerge, data drifts out of sync, and operational teams lose visibility. Epic-compatible platforms prevent this by embedding engagement directly into enterprise workflows.
2. Proxy Access Changes Identity and Consent Requirements
The rise in proxy access fundamentally alters engagement design. Caregivers, family members, and care coordinators now interact with patient data at scale. This requires precise identity management, role-based access, and consent enforcement.
Standalone engagement tools cannot support this complexity reliably. In contrast, Epic-compatible patient engagement platforms inherit Epic’s identity and governance models. Consequently, enterprises maintain control without introducing compliance risk.
3. Why Epic’s Access Model Cannot Be Bypassed
Epic governs how identity, consent, and access function across clinical systems. Therefore, engagement platforms must integrate with these controls rather than replicate them. Bypassing Epic creates parallel identity systems that are difficult to audit and manage.
Epic-compatible platforms align engagement logic with Epic’s access framework. This approach ensures engagement remains secure, traceable, and consistent as usage scales across departments and regions.
The increase to 65% portal usage and 51% proxy access reflects more than adoption growth. It signals a structural shift in how engagement must operate inside enterprise healthcare. Epic-compatible patient engagement platforms exist to meet this reality, not to work around it.
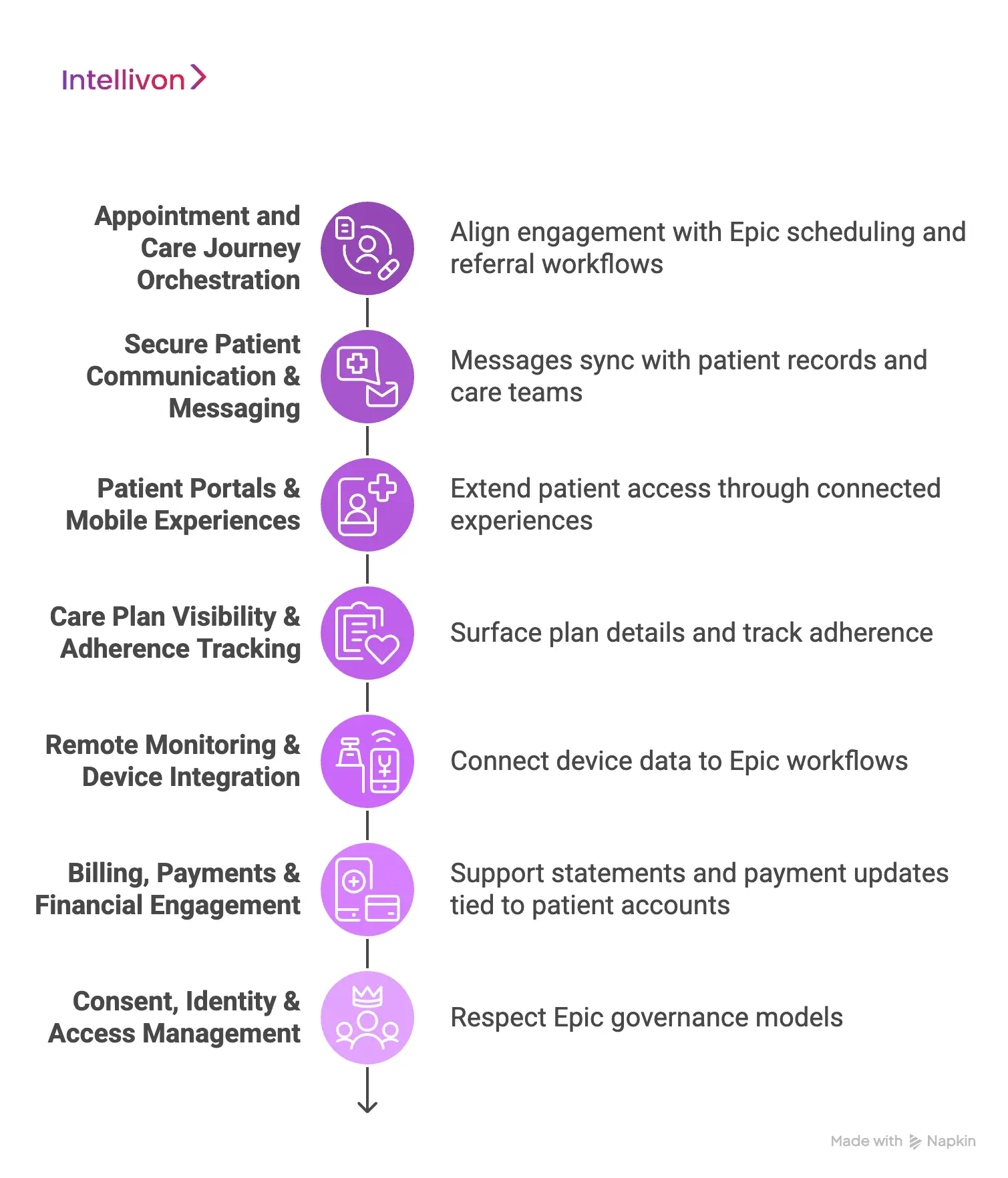
Core Capabilities of Epic-Compatible Patient Engagement Platforms
Epic-compatible patient engagement platforms support more than communication. They enable engagement to function as part of enterprise care delivery. Each capability connects directly to Epic workflows to ensure reliability, consistency, and scale.
1. Appointment and Care Journey Orchestration
Epic-compatible platforms align engagement with Epic scheduling and referral workflows. Appointment reminders, confirmations, and follow-ups are triggered from real scheduling events. As a result, patients receive timely updates without manual coordination.
These platforms also support end-to-end care journeys. Engagement continues across referrals, pre-visit preparation, and post-visit follow-ups. This reduces gaps that often appear when scheduling and engagement operate separately.
2. Secure Patient Communication & Messaging
Secure messaging operates within Epic-governed workflows rather than external inboxes. Messages sync with patient records, care teams, and encounter context. This keeps communication relevant and traceable.
Because messaging follows Epic workflows, providers avoid fragmented conversations. Engagement supports care delivery without creating additional operational burden.
3. Patient Portals & Mobile Experiences
Epic-compatible platforms extend patient access through portals and mobile apps without duplicating Epic systems. Patients view updates, results, and instructions through connected experiences. Meanwhile, data remains consistent across systems.
This approach avoids multiple portals or conflicting information. Enterprises maintain a single source of truth while improving patient access and usability.
4. Care Plan Visibility & Adherence Tracking
Care plans drive many engagement actions in enterprise healthcare. Epic-compatible platforms surface plan details, instructions, and milestones to patients at the right time. Engagement reflects clinical intent rather than generic reminders.
As patients interact with care plans, adherence signals flow back into Epic workflows. This allows care teams to track progress and intervene when needed.
5. Remote Monitoring & Device Integration
When enterprises use remote patient monitoring, engagement platforms connect device data to Epic workflows. Readings align with care plans, alerts, and follow-up protocols. This keeps monitoring clinically meaningful.
Instead of isolated dashboards, RPM data supports real care decisions. Engagement remains tied to provider oversight and governance.
6. Billing, Payments & Financial Engagement
Financial engagement works best when aligned with Epic billing workflows. Epic-compatible platforms support statements, reminders, and payment updates tied to patient accounts. This reduces confusion and delays.
By keeping financial engagement inside Epic workflows, enterprises improve transparency. Patients understand obligations without navigating disconnected systems.
7. Consent, Identity & Access Management
Epic governs identity, consent, and access across healthcare systems. Epic-compatible platforms respect these models instead of recreating them externally. This ensures consistent access for patients and caregivers.
As engagement scales, governance remains intact. Enterprises maintain control over who can see, act on, and manage patient information.
Epic-compatible patient engagement platforms succeed because their capabilities align with how Epic operates. By supporting scheduling, communication, care plans, monitoring, billing, and governance, they deliver engagement that works at enterprise scale.
Different Forms of Epic-Compatible PEPs
Epic-compatible patient engagement platforms do not follow a single model. Enterprises adopt different forms depending on scale, complexity, and long-term strategy.
Understanding these categories helps organizations choose platforms that fit both current needs and future growth.
1. Epic-Embedded Patient Engagement Tools
Epic provides native engagement capabilities that operate directly inside the EHR. These tools are tightly integrated with Epic workflows and require minimal external coordination.
Common examples include Epic MyChart and Epic’s built-in communication and scheduling modules.
Strengths
Epic-embedded tools work seamlessly with existing workflows. They offer reliable access to scheduling, results, and messaging without additional integration overhead.
Limitations
These tools are limited in customization and experience flexibility. They often struggle to support advanced engagement journeys or cross-system coordination.
When there are enough
Epic-native tools work well for basic patient access and communication. However, they become restrictive when enterprises need differentiated experiences or broader orchestration.
2. Epic-Integrated Third-Party Engagement Platforms
These platforms operate outside Epic but integrate deeply with Epic workflows. They extend engagement capabilities without replacing the EHR.
Examples include Luma Health, Well Health, Get Well Network, Relatient, and Phreesia.
How they coexist with Epic
These platforms sync scheduling, messaging, intake, and follow-ups with Epic data. Engagement actions reflect Epic events while offering more flexibility than native tools.
Where they add value
They improve access, communication, and experience design. Many enterprises use them to reduce no-shows, streamline intake, and modernize patient touchpoints.
3. Built for Multi-EHR Environments
Some enterprises require engagement platforms that operate across multiple EHR systems. These platforms support Epic while remaining vendor-neutral.
Examples include Salesforce Health Cloud, Validic, Twistle, and Xealth.
Why large enterprises choose these platforms
They support growth through mergers, acquisitions, and partnerships. Engagement remains consistent even as EHR environments change.
Their role in complex ecosystems
These platforms orchestrate engagement across providers, payers, and care settings. Epic becomes one system among many, not a limiting boundary.
Epic-compatible patient engagement platforms take different forms depending on enterprise needs. While Epic-native tools cover foundational use cases, integrated and multi-EHR platforms enable scale, flexibility, and long-term growth. Choosing the right form depends on how far an organization plans to extend engagement beyond Epic alone.
Architecture of Epic-Compatible Patient Engagement Platforms
Epic-compatible patient engagement platforms rely on a layered architecture to function reliably at enterprise scale. Each layer serves a distinct role and aligns with how Epic governs care delivery. This separation prevents tight coupling and reduces operational risk as usage grows.
By organizing the platform into layers, enterprises gain flexibility without sacrificing control. Engagement remains adaptable while Epic continues to anchor clinical workflows and data integrity.
1. Engagement Experience Layer
Patients and caregivers interact with the platform through portals, mobile apps, and notifications. This layer focuses on clarity and usability, not business logic or data ownership. It presents information in a way that is easy to understand and act on.
Despite being user-facing, this layer never works in isolation. Every interaction connects back to Epic workflows. That connection ensures patients see information that care teams can support and verify.
2. Workflow Orchestration Layer
Care activity determines how engagement flows through the system. The orchestration layer listens for Epic events such as appointments, results, or care plan updates. It decides what engagement action should happen and when.
By reacting to real clinical events, this layer removes guesswork. Engagement stays timely and relevant, while teams avoid manual coordination. As workflows evolve, orchestration adapts without redesign.
3. Interoperability and Integration Layer
All communication with Epic passes through this layer. It manages data exchange, event updates, and workflow signals using Epic-approved interfaces. Other parts of the platform never connect to Epic directly.
This separation limits the blast radius when changes occur. Epic upgrades or configuration updates remain contained. Integration stays predictable instead of fragile over time.
4. Identity, Consent, and Access Layer
Access control follows Epic’s identity and consent models. Patients, caregivers, and staff inherit permissions based on Epic definitions rather than separate platform rules. Proxy access and role-based visibility remain consistent.
As engagement expands, governance stays intact. Audit trails remain clear, and enterprises avoid fragmented identity systems that create compliance gaps.
5. Data and State Management Layer
Engagement generates its own state, such as message delivery or task completion. This layer stores the temporary information without duplicating clinical records. Epic always remains the system of record.
By separating engagement state from clinical data, conflicts are avoided. Care teams trust Epic data, while engagement workflows continue without interruption.
6. Security, Compliance, and Monitoring Layer
Security controls and compliance checks operate continuously across the platform. Logging, monitoring, and audit readiness are built into daily operations, and not added later. Issues surface early instead of after failures.
As engagement scales across sites and regions, oversight remains consistent. Enterprises maintain control even as volume and complexity increase.
Epic-compatible patient engagement platforms succeed because their architecture respects Epic’s role as the clinical backbone. A layered design separates experience, workflows, integration, identity, and governance. This structure allows engagement to scale without disrupting care delivery.
How We Build Epic-Compatible Patient Engagement Platforms
At Intellivon, we build Epic-compatible patient engagement platforms as enterprise healthcare systems. We do not treat them as front-end tools layered on top of Epic. Instead, we design them to work inside Epic-governed workflows from the start.
This approach reduces operational risk and prevents rework later. Each step in our process focuses on scale, compliance, and long-term reliability across enterprise environments.
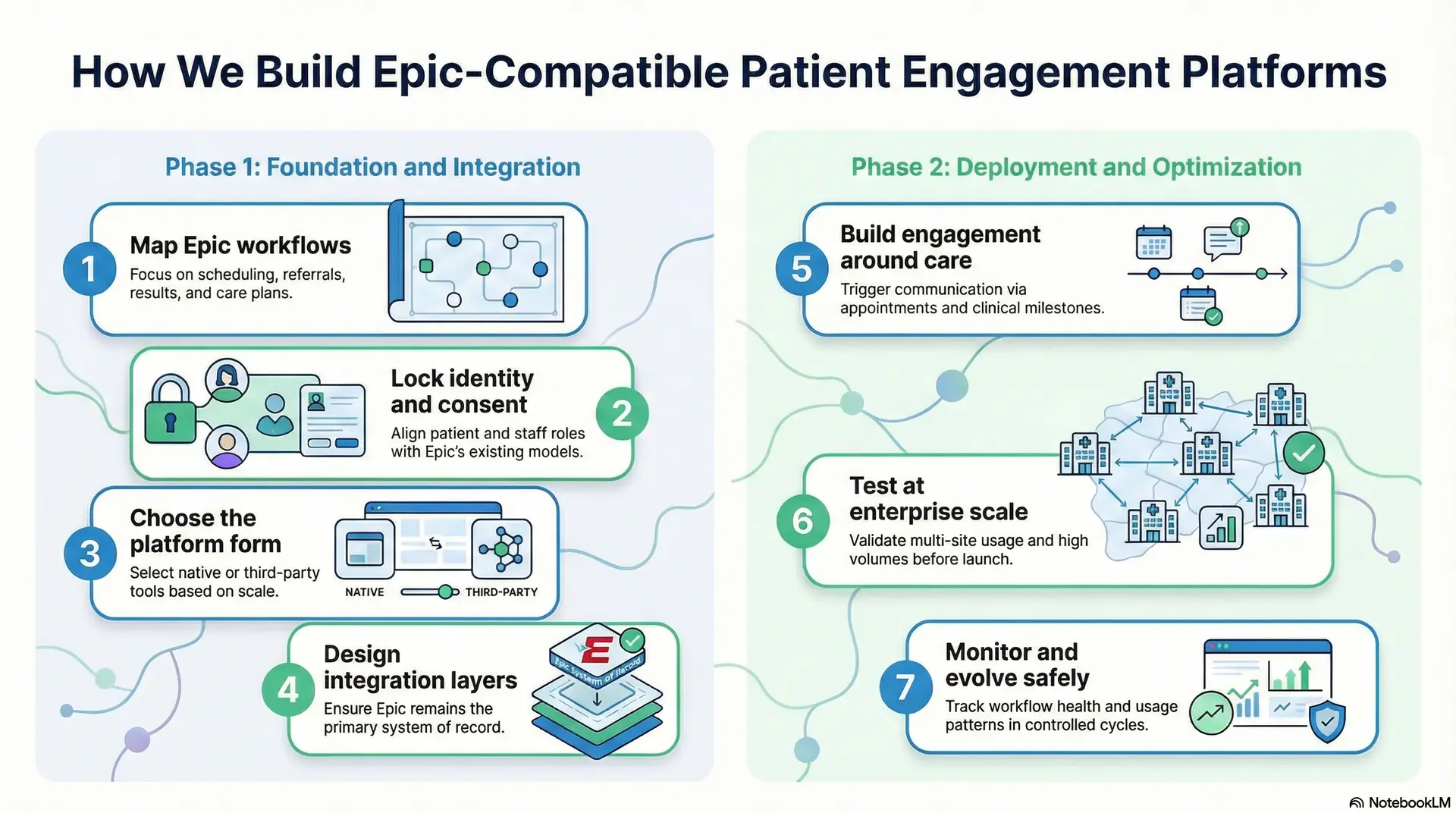
Step 1: Map Epic workflows
We begin by identifying the Epic workflows that should drive engagement. Scheduling, referrals, results, care plans, and follow-ups receive close attention. These workflows determine when engagement should happen.
At the same time, we document where engagement should not occur. This prevents noise and unnecessary communication. As a result, engagement stays tied to real care activity.
Step 2: Lock identity and consent
Next, we define identity, access, and consent rules. Patient access, caregiver proxy access, and staff roles align directly with Epic’s existing models. Nothing new is invented or duplicated.
Consent handling and audit needs are addressed early. Compliance teams stay involved from the start. This avoids delays and security gaps during rollout.
Step 3: Choose the platform form
Not every organization needs the same platform setup. Some rely on Epic-native tools, while others need third-party or enterprise platforms. Scale, customization, and future growth guide this decision.
Choosing the right form early prevents overengineering. It also ensures the platform can expand without structural changes later.
Step 4: Design integration layers
Integration is planned as layered connections, not one-off links. Workflow triggers, data access, and updates follow Epic-approved paths. Epic always remains the system of record.
By isolating integration logic, the platform stays stable during Epic upgrades. Maintenance becomes predictable instead of reactive.
Step 5: Build engagement around care
Engagement logic follows clinical events rather than static rules. Appointments, results, and care milestones trigger communication. At the same time, manual scheduling is avoided.
This keeps engagement timely and relevant. Care teams do not need to manage exceptions or parallel workflows.
Step 6: Test at enterprise scale
Testing goes beyond a single clinic or department. We validate multi-site usage, complex roles, and high volumes. At the same time, edge cases receive attention before launch.
This step prevents failures during expansion. Platforms go live ready for real-world use.
Step 7: Monitor and evolve safely
After launch, monitoring focuses on workflow health and usage patterns. Engagement performance is tracked without disrupting care delivery. Here, changes happen in controlled cycles.
As needs evolve, the platform adapts without breaking Epic alignment. At the same time, governance and reliability remain intact over time.
Intellivon builds Epic-compatible patient engagement platforms through a structured, workflow-first process. Each step supports scale, compliance, and operational stability. This ensures engagement works inside Epic today and remains reliable as enterprises grow.
Cost To Build Epic-Compatible Patient Engagement Platforms
At Intellivon, Epic-compatible patient engagement platforms are built as regulated enterprise healthcare systems, not as engagement tools added on top of Epic. The focus remains on platforms that operate reliably within Epic workflows while supporting scale across hospitals, regions, and care models. Every architectural decision accounts for workflow integrity, identity governance, compliance controls, and long-term interoperability risk.
When budget constraints exist, scope is adjusted with intent. However, core elements such as Epic workflow alignment, consent enforcement, identity and proxy access, auditability, and operational reliability are never compromised. As a result, enterprises avoid expensive remediation cycles after launch. Predictable delivery replaces rework, and long-term ROI stays protected.
Estimated Phase-Wise Cost Breakdown
| Phase | Description | Estimated Cost Range (USD) |
| Discovery & Epic Workflow Mapping | Engagement use cases, Epic workflow alignment, operational, and compliance assessment | $7,000 – $12,000 |
| Platform Architecture Design | Layered platform design, Epic integration approach, scalability planning | $9,000 – $16,000 |
| Identity, Consent & Governance | Proxy access, role-based access, consent logic, audit workflows | $9,000 – $15,000 |
| Core Engagement Platform Development | Scheduling flows, messaging, portals, and care plan engagement logic | $18,000 – $30,000 |
| Epic Integrations | Scheduling, encounters, messaging, results, and billing touchpoints | $16,000 – $28,000 |
| Role-Based Interfaces | Patient, caregiver, admin, operations, and support interfaces | $9,000 – $15,000 |
| Security & Compliance Controls | Encryption, access control, audit trails, and monitoring | $10,000 – $16,000 |
| Testing & Validation | Workflow testing, security validation, and enterprise readiness | $7,000 – $11,000 |
| Deployment & Scale Readiness | Cloud or hybrid setup, performance tuning, and monitoring | $8,000 – $14,000 |
Total initial investment: $93,000 – $187,000
Ongoing maintenance and optimization: 15–20% of the initial build per year
Hidden Costs Enterprises Should Plan For
Even well-planned Epic-compatible engagement programs face pressure when indirect costs are overlooked. Planning for these early protects budgets and timelines as adoption grows.
- Integration complexity increases as new Epic modules, sites, or workflows are added
- Compliance overhead grows with audits, privacy reviews, and policy updates
- Governance requires ongoing tuning of consent and proxy access models
- Infrastructure costs rise with analytics, real-time engagement, and AI usage
- Change management includes onboarding clinical, IT, and operations teams
- Continuous monitoring becomes critical as engagement volume increases
Best Practices to Avoid Budget Overruns
Based on Intellivon’s experience delivering enterprise healthcare platforms, the following practices consistently lead to controlled costs and predictable outcomes.
- Define Epic workflows and engagement triggers before expanding features
- Embed governance, identity, and auditability into the core platform design
- Use modular components that scale without redesigning the platform
- Plan Epic integrations early to avoid costly retrofitting later
- Maintain visibility across performance, security, and compliance metrics
- Design for ongoing Epic updates rather than one-time alignment
Request a tailored proposal from Intellivon’s healthcare platform experts to receive a delivery roadmap aligned with your budget constraints, Epic environment, and long-term patient engagement strategy.
Common Challenges in Developing Epic-Compatible PEPs
Epic-compatible patient engagement platforms fail for predictable reasons. Teams often build engagement like a consumer app, then try to connect it to Epic later. However, Epic environments demand workflow alignment, governance, and operational reliability from the start.
The challenges below show where projects typically break. Each one also explains how Intellivon solves it in real enterprise deployments.
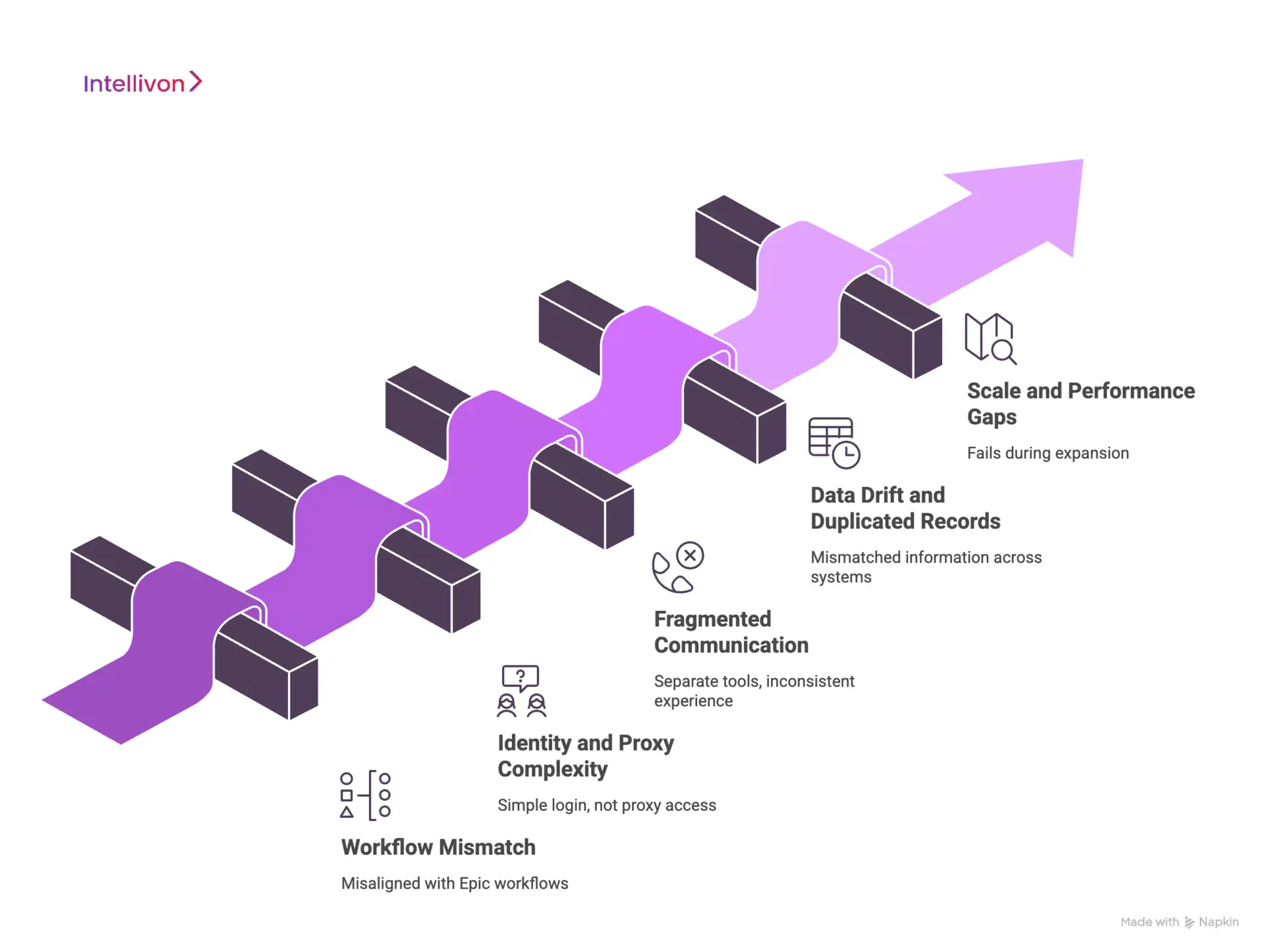
1. Workflow mismatch
Many platforms send reminders or messages without aligning to Epic workflows. As a result, staff see engagement activity that does not match scheduling, referrals, or follow-up plans. Over time, teams create manual workarounds to keep patients informed.
This mismatch also causes trust issues. Patients receive information that care teams cannot quickly provide. Therefore, engagement becomes noise instead of support.
How We Solve It
Intellivon maps Epic workflows before building engagement flows. We anchor triggers to real Epic events, not assumptions. As a result, engagement follows scheduling, results, and care plans consistently.
We also validate workflows with operations teams early. This reduces exceptions and keeps the platform usable at scale.
2. Identity and proxy complexity
Proxy access is common in enterprise care delivery. Caregivers, parents, and care coordinators need controlled access to patient information. However, many engagement platforms treat identity as a simple login problem.
This creates governance gaps. Separate identity rules lead to inconsistent access and audit risk. Consequently, enterprises struggle to scale engagement safely.
How We Solve It
Intellivon aligns identity, consent, and proxy access to Epic’s models. We define roles and permissions early, then enforce them across all channels. This keeps access consistent as user volume grows.
Audit trails remain clear because we avoid parallel identity systems. Enterprises maintain control without slowing down engagement.
3. Fragmented communication
Many organizations deploy separate tools for messaging, portals, and telehealth. While each tool may work alone, the overall experience becomes fragmented. Here, patients receive mixed instructions, and staff manage multiple queues.
Over time, fragmentation increases operational burden. It also reduces patient confidence because communication feels inconsistent.
How We Solve It
Our experts design engagement as a single coordinated experience. We connect messaging, updates, and follow-ups to Epic contexts. This reduces handoffs and keeps conversations traceable.
We also simplify routing and escalation paths. Teams manage engagement without juggling multiple systems.
4. Data drift and duplicated records
Some engagement platforms store their own copies of patient data. Others sync data on delays or with partial coverage. This leads to mismatched information across systems.
Data drift creates operational risk. Care teams lose confidence in what the engagement platform displays. As a result, they revert to manual communication.
How We Solve It
Intellivon keeps Epic as the system of record. We limit stored data to engagement state, such as message status or task completion. This prevents conflicting records.
We also design controlled update paths back to Epic. Enterprises maintain consistency while still enabling real-time engagement.
5. Scale and performance gaps
Engagement often works during pilots and fails during expansion. Multi-site deployments introduce more roles, more workflows, and higher message volume. Without preparation, platforms slow down or break.
Performance issues create immediate operational pain. Staff lose time, and patients receive delayed updates. As a result, adoption drops.
How We Solve It
Our experts test for enterprise scale early. We validate throughput, role complexity, and multi-site workflows before rollout. This prevents surprises during expansion.
Monitoring and alerting remain in place after launch. Teams detect issues early and maintain reliability.
Epic-compatible patient engagement platforms fail when teams treat Epic as a simple integration target. Success requires workflow alignment, governance, and scale-ready architecture.
Intellivon solves these challenges through structured design, controlled integration, and enterprise validation from day one.
Conclusion
Epic-compatible patient engagement platforms are no longer optional for enterprise healthcare. As engagement moves deeper into clinical workflows, platforms must operate inside Epic rather than alongside it. This shift requires more than integrations or feature additions.
Enterprises need platforms designed with workflow alignment, identity governance, compliance controls, and scale in mind. When these foundations are missing, engagement breaks down, trust erodes, and operational costs rise.
Building Epic-compatible PEPs correctly solves these challenges. Engagement becomes consistent, secure, and reliable across departments, sites, and care journeys. More importantly, platforms remain adaptable as Epic environments evolve.
Success depends on intent. When engagement is built as an enterprise healthcare infrastructure, organizations protect long-term ROI while improving patient and provider experiences at scale.
Build An Epic-Compatible Patient Engagement Platform With Intellivon
At Intellivon, Epic-compatible patient engagement platforms are built as regulated enterprise healthcare systems, not as engagement layers added on top of Epic. Every architectural and delivery decision prioritizes workflow integrity, identity governance, compliance controls, and long-term operational stability. This ensures engagement platforms function reliably within Epic environments, not just during initial rollout.
As engagement programs expand across hospitals, clinics, and care models, stability becomes critical. Governance, performance, and audit readiness remain consistent as patient volume, proxy access, and workflow complexity increase. Organizations retain control over engagement workflows, data access, and compliance without introducing fragmentation, operational risk, or rework.
Why Partner With Intellivon?
- Enterprise-grade patient engagement architecture designed for Epic-governed healthcare environments
- Proven delivery across Epic-connected health systems, multi-site networks, and enterprise care platforms
- Compliance-by-design approach covering identity, consent, proxy access, and auditability
- Secure, modular platform architecture supporting cloud, hybrid, and on-prem deployments
- AI-ready engagement foundations enabling analytics, automation, and intelligent workflows with governance and oversight
Book a strategy call to explore how Intellivon can help you build and scale an Epic-compatible patient engagement platform with confidence, control, and long-term enterprise value.
FAQs
Q1. What makes a patient engagement platform Epic-compatible?
A1. An Epic-compatible patient engagement platform works inside Epic workflows, not alongside them. It aligns with Epic scheduling, messaging, identity, and consent models. This ensures engagement remains accurate, secure, and operationally reliable at enterprise scale.
Q2. Can patient engagement platforms work with Epic without replacing Epic tools?
A2. Yes. Epic-compatible platforms extend Epic rather than replace it. They add flexibility and orchestration while Epic remains the system of record. This approach avoids duplication and preserves clinical and operational control.
Q3. Is the Epic App Orchard certification enough for enterprise deployment?
A3. No. App Orchard certification validates baseline security and integration standards. However, enterprise success depends on workflow alignment, identity governance, and performance at scale. Certification alone does not guarantee operational reliability.
Q4. How long does it take to build an Epic-compatible patient engagement platform?
A4. Timelines vary by scope and complexity. Most enterprise-grade platforms require several months for workflow mapping, integration, governance setup, and validation. Rushing development often leads to rework after launch.
Q5. Why should enterprises build Epic-compatible engagement platforms instead of generic tools?
A5. Generic tools struggle at scale because they operate outside Epic workflows. Epic-compatible platforms reduce fragmentation, improve compliance, and support multi-site operations. As a result, enterprises achieve long-term stability and better ROI.