A single patient episode spreads data in many places, such as the ER visit, the CT scan, three days in the hospital, a cardiology consult, and remote monitoring after discharge. Each step creates records that different care teams need, sometimes in just minutes. When data moves quickly, clinicians can make better decisions. At the same time, when it doesn’t, they are left guessing or waiting.
The system that supports this data movement must run continuously and not only when someone starts a batch job. As they connect more hospitals, regions, and apps, the complexity increases. Hospitals manage patient identity across organizations, enforcing consent preferences, creating audit logs, and ensuring everything performs well while data flows in real time.
We have learned at Intellivon that interoperability cannot be added after the fact. It must be built into the core system. Working across multiple EHR environments and hospital networks has taught us that the choices you make early on directly affect whether your system can scale, remain compliant, and withstand operational pressure.
This blog will break down the basic structures you need to build interoperability systems that are sustainable. We will cover the main platform layers, important design strategies, relevant standards, and the organized approach needed to support long-term growth across care ecosystems.
Key Takeaways Of The Health Interoperability Market
Healthcare interoperability solutions are accelerating due to TEFCA requirements, growing EHR ecosystems, and rising demand for real-time data exchange across providers, payers, and AI systems. Modern interoperability platforms enable standardized FHIR and HL7 data exchange, reduce data silos, and support more efficient value-based care delivery.
The global healthcare interoperability solutions market was valued at USD 3.94 billion in 2024. It is projected to grow from USD 4.50 billion in 2025 to approximately USD 14.47 billion by 2034, reflecting a CAGR of 13.89% between 2025 and 2034.
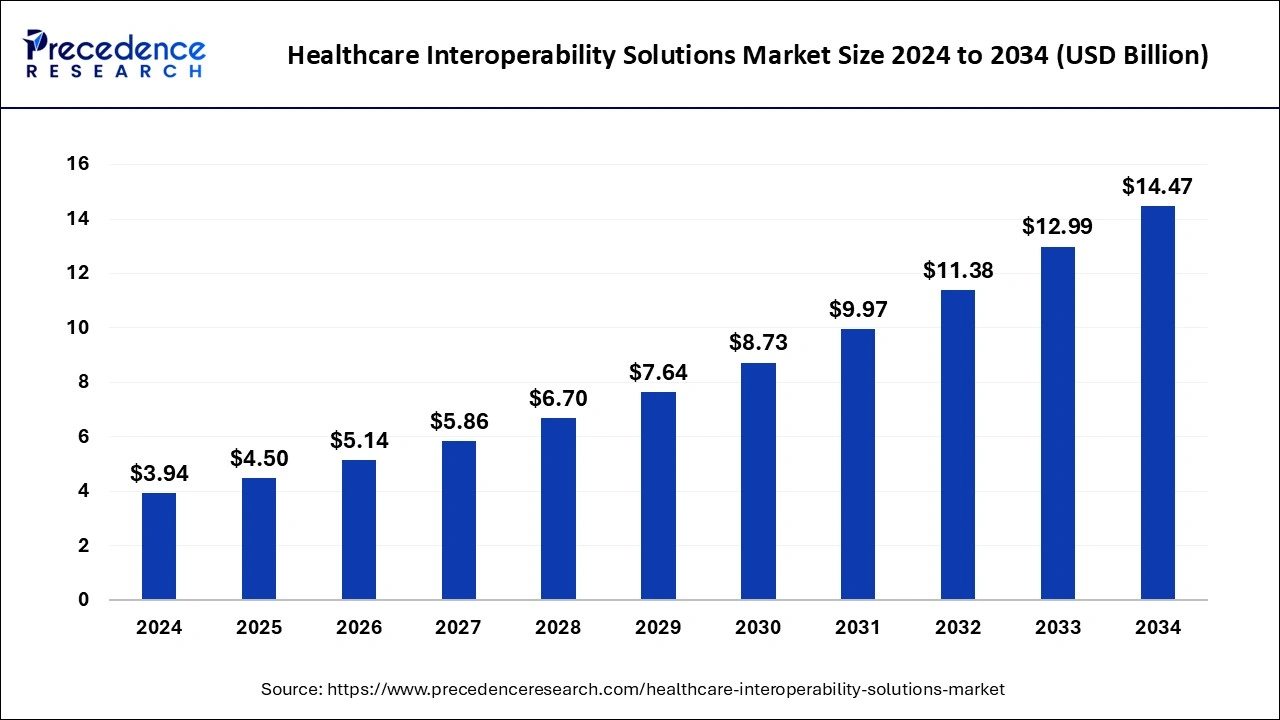
Key Growth Drivers:
- Regulatory Mandates: ONC and TEFCA are accelerating nationwide data exchange adoption. Hybrid interoperability models are expanding rapidly, especially in APAC, growing at nearly 23% CAGR.
- Digital Health Shift: Rising EHR adoption and population health management initiatives are driving sustained market growth of roughly 13–14% CAGR. At the same time, AI and ML applications are increasing the demand for real-time clinical data access.
- Value-Based Care: Interoperability helps reduce duplicate testing and operational inefficiencies while supporting long-term chronic care management. Growing chronic disease populations continue to increase hospital data exchange requirements.
Hybrid interoperability deployments currently lead the market with nearly 40.8% share, as organizations combine cloud scalability with on-premise security to support multi-site healthcare operations.
At the same time, healthcare providers represent the largest end-user segment at 66.8%, with strong investment in organizational interoperability growing at approximately 14.10% CAGR. These trends reinforce why scalable interoperability architecture must support hybrid infrastructure models, secure cross-site data exchange, and enterprise-grade performance to enable reliable, long-term ecosystem connectivity.
What Is a Scalable Healthcare Interoperability System
A scalable healthcare interoperability system is designed to support growing data exchange across hospitals, partners, applications, and regulatory networks without performance loss or compliance risk. It ensures data moves reliably across systems as transaction volume, users, and integrations increase.
These platforms are built using distributed architecture, standardized data models, and automated governance controls to maintain performance, security, and audit readiness as healthcare ecosystems expand over time.
What “Scalable” Actually Means in Healthcare Interoperability Architecture
Scalability in healthcare interoperability is not only about handling higher data volume. It means supporting expanding ecosystems, new data types, stricter compliance requirements, and continuous system availability.
As healthcare organizations connect more hospitals, applications, and networks, interoperability architecture must maintain performance, data integrity, and regulatory compliance under increasing complexity.
1. Multi-EHR, Multi-Partner, Multi-Region Scale
Modern interoperability platforms must support multiple EHR systems, external partners, and geographic regions simultaneously. Each new connection increases identity, security, and data routing complexity.
Architecture must enable onboarding without redesigning core systems. It should support regional data rules and partner-specific workflows without creating fragmentation.
2. Real-Time, Batch, and Bulk Data Movement
Healthcare data moves in multiple patterns. Clinical alerts require real-time exchange. Population health reporting often uses batch transfers. Research and analytics require bulk data exports.
Scalable architecture must support all three patterns without performance conflicts. Event-driven processing and workload isolation help maintain system stability.
3. Patient-Facing, Partner-Facing, and Regulatory Data Flows
Interoperability systems must serve patient apps, provider networks, payer integrations, and regulatory reporting simultaneously. Each flow has different latency, security, and audit requirements.
Architecture must enforce policy-based access and workload prioritization. This prevents lower-priority workloads from affecting critical clinical data exchange.
4. Compliance Scaling: Audit, Consent, and Traceability
As ecosystems grow, compliance complexity increases. More partners and applications create more audit trails, consent records, and access events.
Scalable platforms automate audit logging, consent enforcement, and traceability across all data flows. This reduces manual compliance workload and lowers regulatory risk.
5. Operational Scaling: Monitoring, Incident Response, and Upgrades
Large interoperability platforms must support continuous monitoring, fast incident response, and safe system upgrades. Downtime can directly affect care delivery and reporting obligations.
Scalable architecture includes observability pipelines, automated alerting, and controlled release strategies. This ensures stability during updates and expansion.
In healthcare interoperability, scalability means sustaining performance, compliance, and reliability as ecosystems expand. Organizations must design architecture that supports multiple systems, data flows, and regulatory environments simultaneously.
16 Minutes Per Visit on EHRs Highlights Workflow Inefficiencies
Clinical studies show that physicians spend roughly 16 minutes per patient visit interacting with the EHR. Observational research published on PubMed and broader health IT time-motion studies support this estimate. On the surface, this may appear to be a usability problem. However, at an enterprise level, it signals deeper data workflow inefficiencies.
Much of this time is spent searching for information, navigating fragmented records, and reconciling data from multiple systems.
1. Why Clinicians Spend So Much Time on EHRs
Most EHR platforms were designed to store clinical data, not move it efficiently across care environments. As a result, patient data often exists across multiple disconnected systems. Clinicians must manually piece together records during each encounter.
This forces providers to spend time locating and validating data instead of acting on it. The problem is not only interface design. It is how data is structured, accessed, and shared across the healthcare enterprise.
2. What This Means for Healthcare Enterprises
When clinicians spend 16 minutes per visit on EHR-related tasks, the impact extends beyond productivity. It directly affects care delivery speed, clinician experience, and operational efficiency.
This inefficiency influences appointment throughput, care responsiveness, and provider burnout risk. It also increases operational costs tied to manual data reconciliation. As patient volumes grow, the cost of fragmented data access grows with it.
3. How FHIR-Native Data Exchange Changes This Dynamic
FHIR-native healthcare data exchange platforms address this problem at the architectural level. They enable standardized, API-driven access to clinical data across systems and care environments.
This allows faster retrieval of complete patient records and reduces manual searching. Clinicians gain near real-time access to labs, medications, and patient history. Care teams also see consistent, synchronized data views across systems.
As a result, clinicians spend less time navigating systems and more time delivering patient care.
For enterprise leaders, the 16-minute statistic highlights how data architecture directly impacts workforce efficiency, cost structure, and care delivery outcomes.
Workflow redesign at the application layer alone cannot solve this challenge. The long-term solution requires rethinking how clinical data moves across systems and organizations.
This is why FHIR-native healthcare data exchange platforms are becoming strategic infrastructure investments rather than incremental technology upgrades.
Common Failure Patterns in Healthcare Interoperability Architecture
Many interoperability initiatives succeed during early deployment but struggle as ecosystem complexity increases. The failure rarely comes from standard selection or API availability. It usually comes from architectural decisions that cannot support expanding data volume, partners, and regulatory demands.
Understanding these failure patterns helps organizations avoid costly redesigns and operational disruptions later. The following issues appear consistently across large-scale interoperability programs.
1. Interface Sprawl and Dependency Chains
Many organizations scale interoperability by adding more point-to-point integrations. Over time, this creates fragile dependency chains across systems, interfaces, and workflows.
When one system changes, multiple downstream integrations break. This increases maintenance costs and slows partner onboarding.
2. Fragmented Identity Across Systems
Patient, provider, and organizational identities often exist in multiple disconnected systems. Without centralized identity orchestration, data matching becomes inconsistent and error-prone.
This creates clinical risk, duplicate records, and reporting inaccuracies. At scale, identity fragmentation becomes a major operational and compliance concern.
3. Consent Managed Outside Core Architecture
In many environments, consent is captured in workflows but not enforced at the data access layer. This creates gaps between policy intent and actual data usage.
As partner ecosystems grow, manual consent checks become impossible to maintain. Automated, architecture-level consent enforcement becomes mandatory for scale.
4. EHR Polling and Source System Overload
Polling-based integration models create unnecessary load on EHR systems. As application and partner demand increase, polling frequency also increases.
This degrades source system performance and increases data latency. Event-driven architecture reduces this load and improves data freshness.
5. Duplicated Data Transformation Logic
When each integration builds its own data transformation logic, mapping complexity increases rapidly. This creates inconsistent data interpretation across systems.
Over time, maintenance becomes difficult, and data quality issues increase. Centralized transformation and canonical models help control this complexity.
6. Limited Observability and Audit Traceability
Many interoperability systems lack end-to-end visibility across data flows. This makes troubleshooting slow and increases incident recovery time.
Incomplete audit trails also increase regulatory risk. Scalable platforms require unified observability and audit pipelines.
7. Governance Added After Deployment
Some interoperability programs prioritize connectivity speed over governance design. Compliance, audit, and policy controls are added later.
This often requires platform redesign and increases long-term cost. Governance must be built into architecture from the start.
Interoperability failures rarely happen because of missing technology. They happen because architecture cannot support ecosystem growth. Organizations that recognize these failure patterns early can design interoperability platforms that scale safely, maintain compliance, and support long-term operational stability.
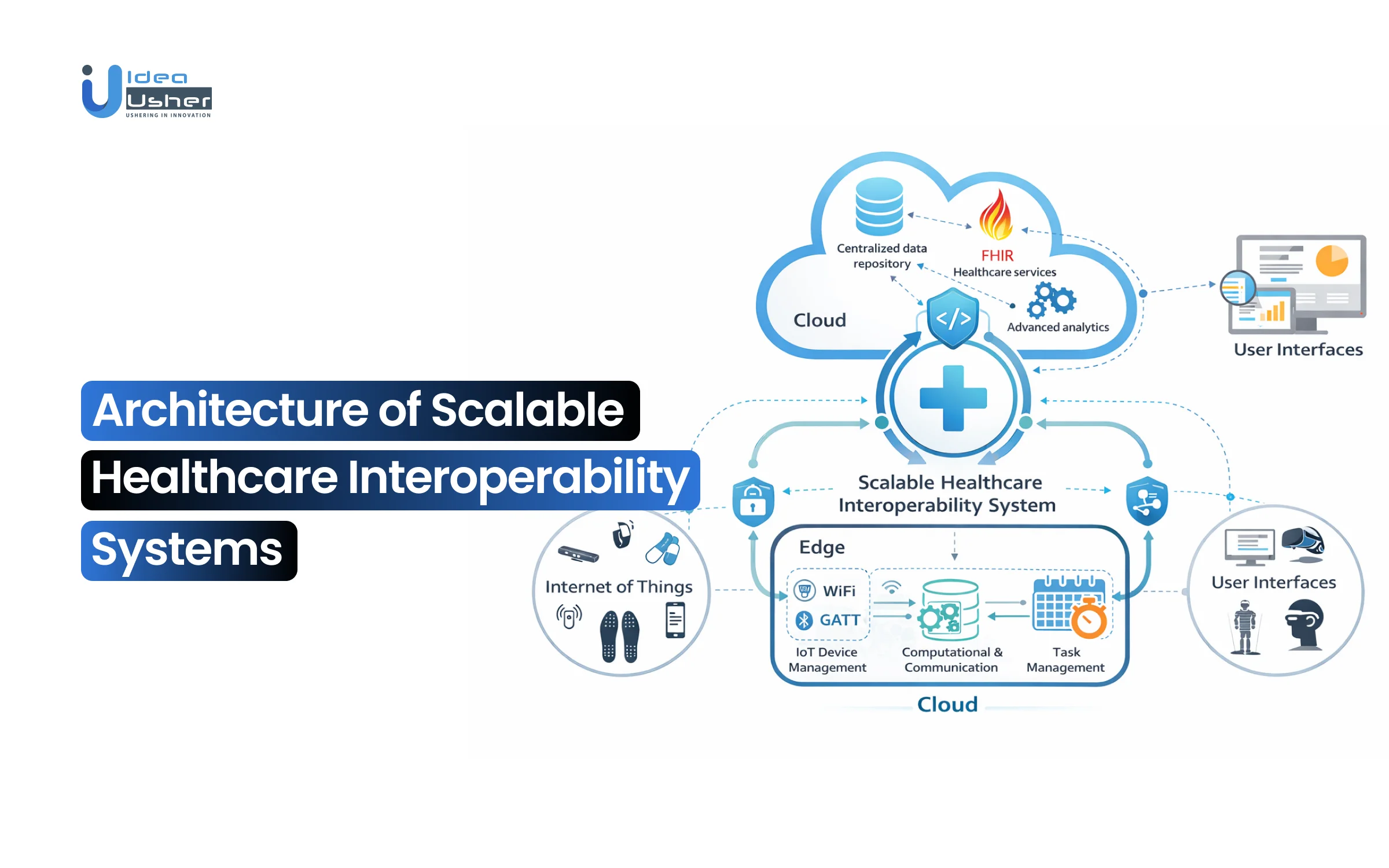
Architecture of a Scalable Healthcare Interoperability Platform
Scalable healthcare interoperability platforms must operate as a distributed data infrastructure, not as integration middleware. As healthcare ecosystems expand, platforms must support real-time clinical workflows, regulatory reporting, partner integrations, and patient-facing applications simultaneously.
A layered architecture helps isolate workloads, enforce governance controls, and maintain performance under growing data and transaction volumes. Each layer plays a distinct role in maintaining interoperability, reliability, security, and long-term scalability.
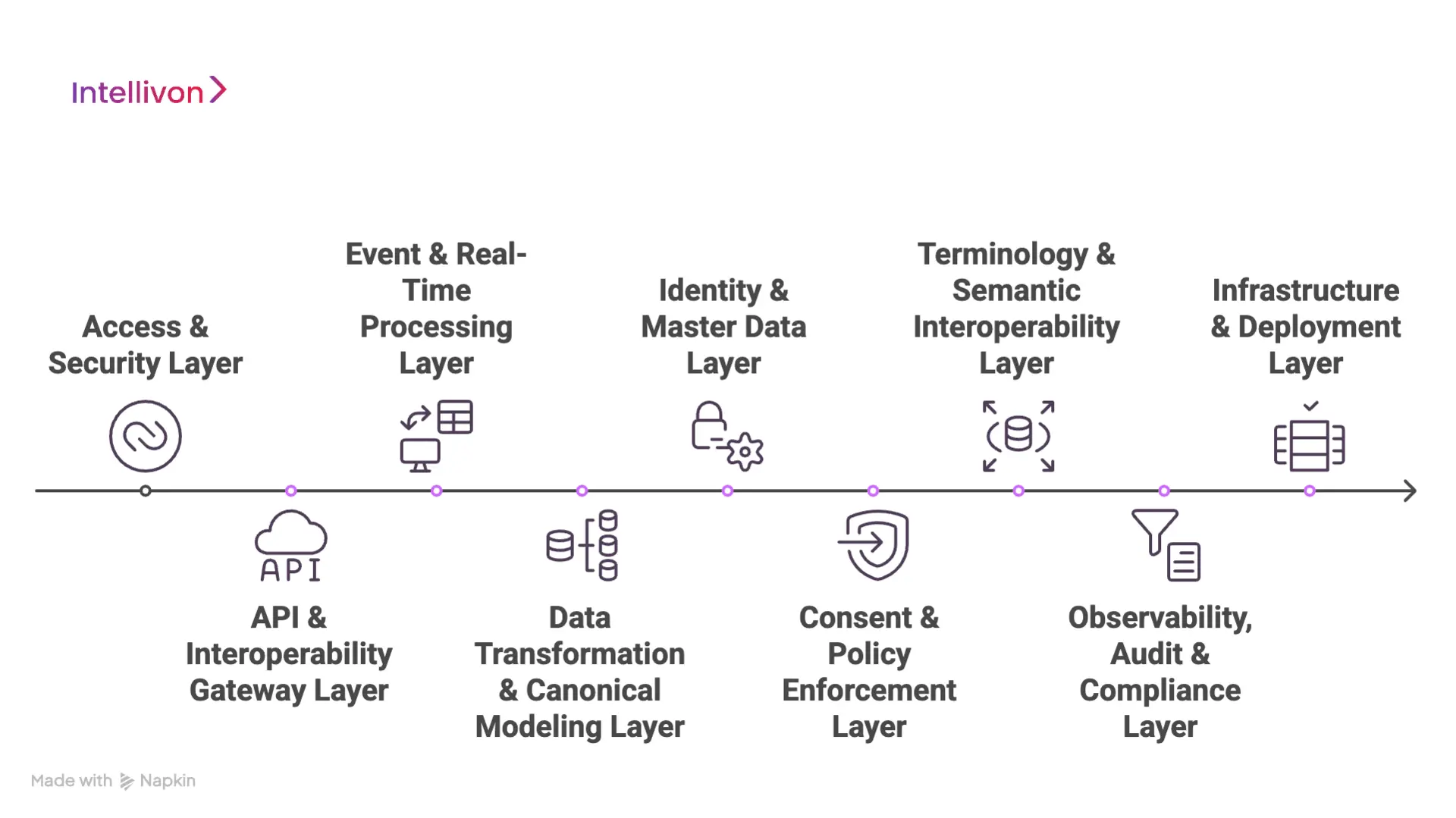
1. Access & Security Layer
This layer controls how users, applications, and partner systems access interoperability services. It enforces authentication, authorization, and trust boundaries across the ecosystem.
Modern platforms use OAuth-based authorization models, Zero Trust security principles, and strict application onboarding governance. This ensures only verified systems and users can access clinical data.
2. API & Interoperability Gateway Layer
The interoperability gateway manages all inbound and outbound data exchange. It exposes FHIR APIs, enforces rate limits, and manages tenant isolation across organizations.
Gateway controls also support API versioning and lifecycle management. This allows systems to evolve without breaking existing integrations or disrupting clinical workflows.
3. Event & Real-Time Processing Layer
Real-time interoperability depends on event-driven architecture rather than polling-based data exchange. This layer manages subscriptions, event routing, and publish-subscribe communication patterns.
Event processing allows systems to react instantly to clinical updates, such as lab results or admission events. It also reduces load on source systems and improves data freshness.
4. Data Transformation & Canonical Modeling Layer
Healthcare data originates from multiple formats and standards. This layer converts incoming data into a canonical model before distributing it across systems.
HL7 messages, proprietary feeds, and legacy data formats are normalized before being mapped to FHIR resources. Centralized transformation improves data consistency and reduces integration complexity.
5. Identity & Master Data Layer
This layer ensures consistent identification of patients, providers, and organizations across systems. It supports enterprise master patient index strategies and identity resolution workflows.
Centralized identity management reduces duplicate records and improves care coordination. It also strengthens reporting accuracy and compliance tracking.
6. Consent & Policy Enforcement Layer
Consent must be enforced automatically at the data access level. This layer manages dynamic consent rules, policy engines, and purpose-of-use enforcement.
Automated policy enforcement ensures regulatory compliance across all data flows. It also reduces manual compliance review and audit preparation effort.
7. Terminology & Semantic Interoperability Layer
This layer ensures clinical data maintains consistent meaning across systems. It manages terminology normalization, code translation, and version control.
Terminology services support SNOMED, LOINC, and other clinical coding standards. This improves analytics accuracy and clinical decision support reliability.
8. Observability, Audit & Compliance Layer
Large interoperability platforms must support full visibility across data pipelines. This layer captures audit logs, traceability data, and operational telemetry.
Advanced observability supports incident investigation, compliance reporting, and forensic analysis. Replay capabilities allow teams to recover or reprocess failed transactions safely.
9. Infrastructure & Deployment Layer
This layer supports system reliability, availability, and geographic distribution. It enables multi-region deployments, high availability configurations, and disaster recovery planning.
Modern interoperability platforms support zero-downtime upgrades and rolling deployments. This ensures continuous system availability during expansion and updates.
A scalable interoperability architecture depends on coordinated operation across multiple platform layers. Each layer contributes to performance, compliance, and ecosystem reliability. When designed together, these layers enable healthcare organizations to expand interoperability safely without introducing operational risk or compliance gaps.
Strategies That Help Healthcare Interoperability Systems Scale
Scalable interoperability platforms require more than a layered architecture. They require design strategies that allow systems to expand safely as data volume, partner networks, and regulatory complexity increase. Without these strategies, platforms often become difficult to maintain, expensive to scale, and risky to operate.
The following design approaches consistently appear in healthcare interoperability systems that support long-term ecosystem growth and operational stability.
1. Microservices-Based Platform Design
Microservices separate critical interoperability capabilities into independent services. These services typically include identity resolution, consent enforcement, FHIR data services, event processing, and transformation engines.
This separation prevents failures in one service from affecting the entire platform. It also allows teams to scale specific workloads without overprovisioning the entire system.
2. Containerization and Automated Orchestration
Containerized services ensure consistent runtime behavior across development, testing, and production environments. Orchestration platforms automatically scale services based on workload demand.
In healthcare interoperability, this supports sudden traffic increases from patient apps, reporting requirements, or partner integrations. Automated scaling helps maintain performance without manual intervention.
3. Event-Driven Data Exchange
Event-driven interoperability replaces constant polling with real-time notifications and event messaging. Systems publish clinical updates, and subscribed systems receive them instantly.
This reduces load on source systems and improves data freshness. It also supports real-time care workflows such as alerts, care coordination, and monitoring.
4. Polyglot Data Storage Strategy
Different interoperability workloads require different storage models. Transactional clinical data, high-volume telemetry, and audit logs have very different performance and storage requirements.
Polyglot persistence allows each workload to use the most efficient database technology. This improves performance and reduces infrastructure cost at scale.
5. Canonical Data Modeling and Centralized Transformation
Canonical data models standardize how data is represented across systems. Centralized transformation pipelines ensure consistent data mapping across integrations.
This reduces duplication of transformation logic. It also improves data quality and simplifies the onboarding of new systems and partners.
6. API-First and Standards-Driven Integration
API-first interoperability design ensures that data services are accessible through standardized interfaces. Standards-based APIs improve compatibility across systems and reduce custom integration effort.
This approach supports long-term ecosystem expansion and simplifies third-party application integration.
7. Built-In Governance and Compliance Automation
Governance controls must operate inside the architecture, not as external review processes. Automated audit logging, consent enforcement, and policy controls reduce compliance risk.
This also reduces manual operational workload. It allows organizations to scale interoperability without increasing compliance overhead.
Scalable healthcare interoperability requires combining strong architecture with proven design strategies. Microservices, event-driven processing, canonical modeling, and automated governance together enable reliable ecosystem growth.
Interoperability Standards That Power Enterprise-Scale Data Exchange
Technology architecture alone cannot guarantee interoperability. Scalable healthcare data exchange requires standards that define how data is structured, interpreted, and securely accessed across organizations. Without strong standards alignment, even advanced platforms struggle to maintain data consistency and compliance at scale.
Enterprise interoperability platforms rely on layered standards that support data transport, clinical meaning, and secure application integration. Together, these standards enable reliable and repeatable data exchange across healthcare ecosystems.
1. Syntactic Interoperability Standards
Syntactic standards define how healthcare data is formatted and transmitted between systems. They ensure structured data moves consistently across APIs, messaging workflows, and integration pipelines.
Common syntactic standards support:
- Structured message exchange across clinical systems
- API-driven data transport across applications
- Consistent payload formatting across partners and networks
- Automation of data ingestion and processing workflows
Modern interoperability environments primarily rely on JSON and XML-based formats to support large-scale healthcare data exchange.
2. Semantic Interoperability Standards
Semantic standards ensure clinical data keeps the same meaning across systems. They standardize how diagnoses, lab results, medications, and clinical observations are interpreted across care environments.
Enterprise semantic interoperability depends on:
- Standardized clinical coding across systems and partners
- Centralized terminology services and mapping governance
- Version-controlled code systems and update workflows
- Consistent data interpretation across analytics and clinical systems
Terminology systems such as SNOMED CT and LOINC help maintain clinical data consistency at scale.
3. Data Exchange and Resource Standards
Data exchange standards define how healthcare data is organized, accessed, and shared across systems. These standards enable modern API-driven interoperability ecosystems.
FHIR-based exchange supports:
- Standardized clinical resource structures across systems
- Real-time API-driven data access
- Event-based interoperability workflows
- Bulk data exchange for analytics and reporting
FHIR enables interoperability platforms to scale data exchange across applications, partners, and regulatory environments.
4. Secure Access and Application Integration Standards
Secure access standards enable third-party applications to safely connect to healthcare systems. They ensure patient data remains protected while supporting digital ecosystem expansion.
Secure interoperability frameworks support:
- Standardized application authentication and authorization
- Controlled third-party application onboarding
- Secure API-based data access
- Fine-grained data access permissions and audit tracking
SMART on FHIR enables secure, standardized integration of third-party applications into clinical workflows.
Interoperability standards form the foundation of scalable healthcare data exchange. When combined with strong platform architecture, they enable consistent data movement, reliable clinical interpretation, and secure ecosystem expansion. Organizations that align architecture and standards strategy early can scale interoperability programs while maintaining compliance, performance, and data quality.
Regulatory and Compliance Requirements That Directly Shape Architecture
In healthcare interoperability, regulation is not a downstream consideration. It directly influences how systems are designed, deployed, and operated.
As data exchange expands across hospitals, partners, and digital ecosystems, regulatory complexity increases. A scalable interoperability architecture must support automated compliance enforcement, continuous audit readiness, and secure data access across all workflows.
1. Data Access Transparency and Patient Data Rights
Modern healthcare regulations increasingly require organizations to provide transparent and controlled data access. Patients, providers, and authorized applications must be able to access data safely without compromising privacy or security.
Architecture must support:
- Controlled API-based data access
- Patient-authorized third-party application integration
- Data access logging and traceability
- Real-time access permission enforcement
Without architecture-level access controls, organizations risk compliance gaps and data exposure.
2. Auditability and End-to-End Traceability
Regulators require organizations to prove who accessed data, when it was accessed, and how it was used. Manual audit tracking cannot support large interoperability ecosystems.
Scalable platforms must include:
- Centralized audit logging across all data pipelines
- Immutable access records and activity tracking
- End-to-end data lineage visibility
- Automated compliance reporting capabilities
Audit readiness must be continuous, not event-based.
3. Consent Enforcement and Data Sharing Governance
Consent management is no longer limited to capturing patient permission. Systems must enforce consent rules dynamically across all data flows and partner integrations.
Architecture must support:
- Policy-based consent enforcement
- Purpose-of-use validation during data access
- Real-time consent verification across applications
- Consent lifecycle tracking and updates
Automated consent enforcement reduces compliance risk and operational workload.
4. Data Security, Privacy, and Zero Trust Requirements
Healthcare data security requirements continue to increase as digital ecosystems expand. Security must be embedded across infrastructure, application, and data layers.
Modern interoperability architecture must include:
- Zero Trust access models
- Encryption across data storage and transmission
- Continuous security monitoring and threat detection
- Secure identity federation across partner systems
Security architecture directly impacts regulatory compliance and breach risk.
5. Cross-Organization and Cross-Region Data Governance
As interoperability expands across regions and partner networks, data governance requirements become more complex. Different regions and organizations may enforce different data access and storage rules.
Architecture must support:
- Region-specific data residency controls
- Cross-network data governance policies
- Federated data access and identity trust models
- Policy-driven data routing and storage decisions
This ensures compliance while supporting multi-region interoperability.
Regulatory requirements are now primary architecture drivers in healthcare interoperability. Scalable platforms must embed compliance controls directly into data exchange, identity management, and access workflows.
Organizations that design interoperability architecture with compliance at the core can scale ecosystems while maintaining audit readiness, data security, and regulatory confidence.
How We Build the Architecture of a Scalable Healthcare Interoperability System
At Intellivon, interoperability architecture is designed as a regulated healthcare data infrastructure, not as integration tooling layered onto existing systems. The goal is to create platforms that support multi-EHR ecosystems, partner expansion, and regulatory compliance without introducing performance or operational risk.
The following step-by-step approach ensures interoperability architecture remains scalable, secure, and audit-ready as healthcare ecosystems grow.
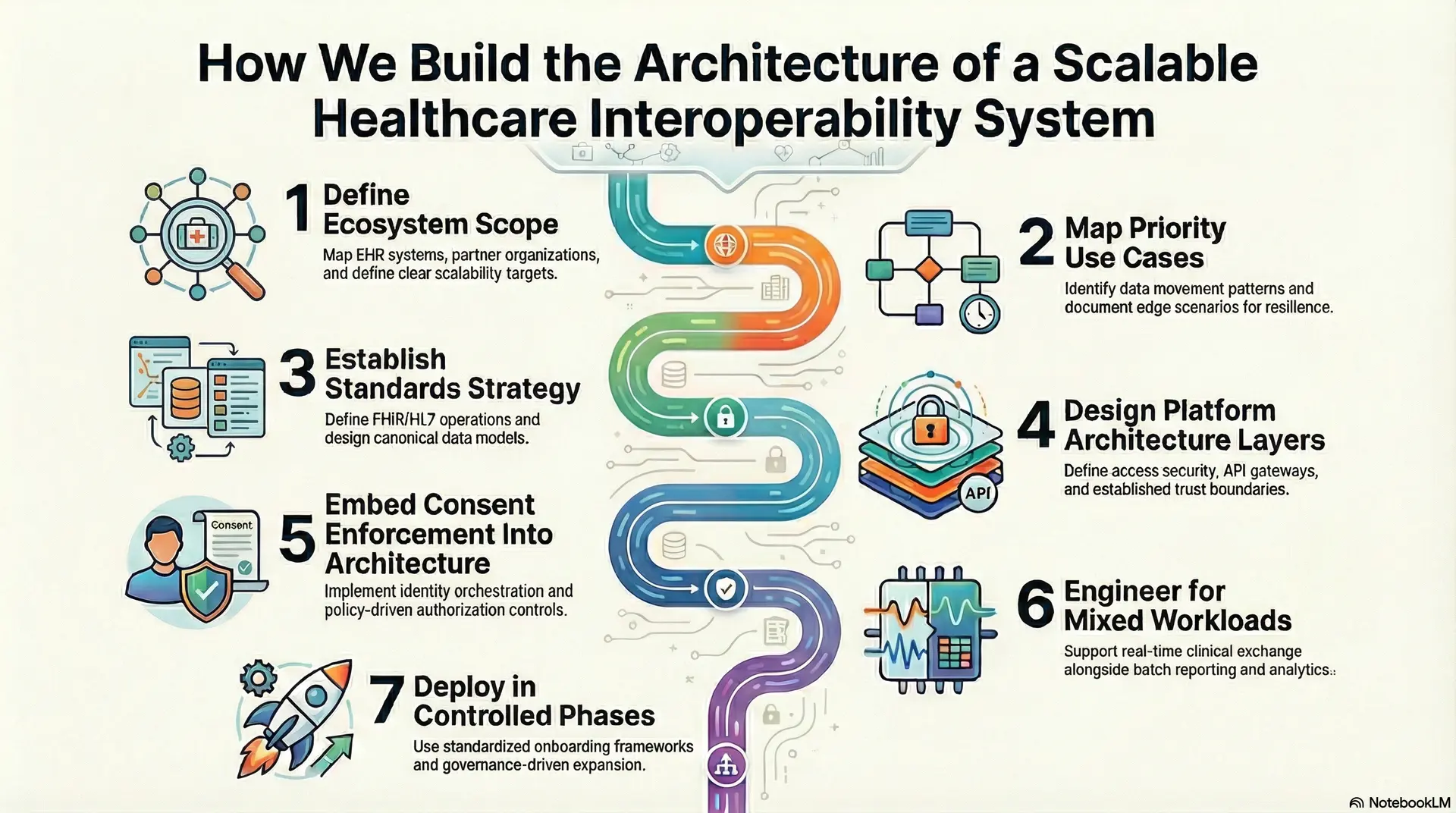
Step 1: Define Ecosystem Scope
Architectural design begins with mapping the full interoperability ecosystem. This includes EHR systems, partner organizations, patient applications, and regulatory data exchange requirements.
Clear scalability targets are defined for transaction volume, user growth, and integration expansion. This prevents future redesign caused by underestimated scale or ecosystem complexity.
Step 2: Map Priority Use Cases
Critical clinical, operational, and reporting workflows are mapped across systems and organizations. Real-time, batch, and bulk data movement patterns are identified early in the design process.
Edge scenarios such as downtime handling, duplicate event management, and partial data availability are also documented to improve platform resilience.
Step 3: Establish Standards Strategy
Standards strategy defines how FHIR, HL7, and legacy data formats will operate across the platform. Canonical data models are designed to normalize data across multiple systems and sources.
Centralized data transformation reduces mapping duplication and improves long-term interoperability consistency.
Step 4: Design Platform Architecture Layers
A layered interoperability architecture is defined across access security, API gateway, event processing, transformation pipelines, identity, consent, terminology, and audit services. Trust boundaries are also established across organizations, applications, and data domains.
This ensures secure cross-entity data exchange while maintaining platform isolation and governance control.
Step 5: Embed Consent Enforcement Into Architecture
Enterprise identity orchestration is implemented across patients, providers, and organizations. Authorization models enforce least-privilege data access across applications and partner systems.
Consent enforcement operates through policy-driven controls rather than manual workflows. This ensures consistent compliance across all data exchange scenarios.
Step 6: Engineer for Mixed Workloads
Architectural design supports real-time clinical exchange alongside batch reporting and bulk analytics workloads. Event-driven processing reduces source system load and improves data freshness.
Observability, audit automation, and compliance telemetry are built into platform operations. This enables continuous audit readiness and faster incident response.
Step 7: Deploy in Controlled Phases
Implementation follows phased rollout aligned to high-value workflows and interoperability priorities. Standardized onboarding frameworks are used for new partners, applications, and data sources.
Platform expansion follows governance-driven processes rather than custom integration work. This ensures predictable scaling and long-term operational stability.
Scalable healthcare interoperability requires disciplined architecture design, governance-driven delivery, and platform-level compliance enforcement.
Intellivon applies a platform-first approach that allows healthcare organizations to expand interoperability safely across systems, partners, and regions while maintaining performance, security, and regulatory confidence.
Future of Scalable Healthcare Interoperability Architecture
Healthcare interoperability architecture is moving beyond system connectivity toward ecosystem orchestration. Future platforms will not only move data between systems but also support real-time decision-making, automated compliance enforcement, and patient-controlled data access across networks.
As healthcare ecosystems become more distributed, interoperability architecture must support higher transaction volume, stricter regulatory controls, and continuous system availability. The next phase of interoperability will focus on intelligent, event-driven, and policy-aware data infrastructure.
1. Event-First Interoperability Architecture
Future interoperability platforms will prioritize event-driven data exchange over request-based models. Real-time clinical events will trigger downstream workflows across care teams, analytics platforms, and patient applications.
Event-first architecture will reduce source system load and improve care coordination speed. It will also support real-time population health and remote monitoring workflows.
2. AI-Assisted Interoperability and Data Governance
AI will increasingly support data routing, anomaly detection, and data quality monitoring across interoperability pipelines. Automated governance tools will identify policy violations and data inconsistencies before they impact operations.
Future platforms will combine AI with human oversight to maintain regulatory compliance and operational reliability. This will reduce manual data review and accelerate interoperability scaling.
3. Patient-Controlled and Consent-Driven Data Ecosystems
Future interoperability models will give patients greater control over how their data is shared across organizations. Consent enforcement will operate dynamically across applications, partners, and data exchange networks.
Architecture must support real-time consent updates and purpose-based data access. This will strengthen trust and regulatory alignment across digital health ecosystems.
4. Network-Native and Cross-Exchange Interoperability
Interoperability will increasingly operate across network-of-network exchange models. Platforms must support cross-network identity trust, data routing, and audit traceability across organizations and regions.
Future architectures will support standardized exchange frameworks and cross-network data governance. This will enable faster partner onboarding and broader data collaboration.
5. Cloud-Hybrid and Distributed Interoperability Infrastructure
Future interoperability platforms will continue using hybrid infrastructure models. Organizations will combine cloud scalability with on-premise control for sensitive clinical workloads.
Distributed infrastructure will support multi-region resilience, low-latency access, and regulatory data residency requirements. This will improve platform reliability during ecosystem expansion.
The future of healthcare interoperability architecture will be defined by intelligence, automation, and ecosystem-scale reliability. Organizations must design platforms that support real-time data exchange, automated governance, and distributed infrastructure from the start.
Conclusion
A scalable healthcare interoperability architecture determines how safely and efficiently healthcare ecosystems can grow. Platforms designed for real-time exchange, automated compliance, and multi-system coordination help organizations avoid operational and regulatory risk. As data exchange demands increase, architecture-first interoperability becomes essential.
Healthcare organizations that invest in scalable, standards-driven, and governance-led interoperability platforms will be better prepared to support evolving care models, digital innovation, and long-term ecosystem expansion.
Build a Scalable Healthcare Interoperability Architecture
At Intellivon, scalable interoperability architectures are built as regulated healthcare data infrastructure designed for secure, compliant data exchange across EHRs, hospitals, partners, and digital health ecosystems.
Every architecture and delivery decision prioritizes governance, identity orchestration, consent enforcement, and audit-ready data access. As interoperability expands across regions and partners, platforms maintain stability, performance, and compliance without introducing fragmentation or operational risk.
Why Partner With Intellivon?
- Enterprise-grade interoperability architecture for multi-EHR, multi-partner, and multi-region ecosystems
- Proven delivery across hospital networks, HIEs, and enterprise interoperability programs
- Compliance-by-design with automated audit trails, policy enforcement, and traceability
- Advanced identity orchestration and consent-driven data exchange across jurisdictions
- Secure modular platform supporting cloud, hybrid, and on-prem deployments
- Real-time interoperability across event, query, and API-based exchange models
- Scalable partner onboarding and governance-driven integration workflows
- AI-ready data infrastructure supporting analytics, automation, and predictive insights
- End-to-end observability across performance, security, and compliance operations
Book a strategy call to explore how Intellivon can help you design and scale interoperability architecture with confidence, compliance control, and long-term enterprise value.
FAQs
Q1. What makes healthcare interoperability architecture scalable?
A1. Scalable interoperability architecture supports growing data exchange across hospitals, partners, and applications without performance loss or compliance risk. It combines distributed system design, standardized data models, and automated governance to maintain reliability as ecosystems expand.
Q2. Is FHIR alone enough to build scalable healthcare interoperability systems?
A2. FHIR enables standardized data exchange, but scalability requires more than APIs. Organizations also need identity orchestration, consent enforcement, event-driven processing, observability, and compliance automation to support enterprise-scale interoperability.
Q3. Why do many healthcare interoperability platforms fail at scale?
A3. Most failures occur when systems are built as integration layers instead of data platforms. As partner networks and data volume grow, identity fragmentation, audit gaps, and performance bottlenecks create operational and compliance risks.
Q4. How does interoperability architecture support value-based care and real-time clinical workflows?
A4. Scalable interoperability enables real-time access to patient data across care environments. This improves care coordination, reduces duplicate testing, and supports population health and chronic care management.
Q5. How do healthcare organizations future-proof their interoperability architecture?
A5. Future-ready interoperability platforms use standards-driven APIs, event-based data exchange, automated compliance controls, and hybrid infrastructure models. This allows organizations to adapt to new regulations, technologies, and ecosystem expansion.