The average healthcare breach costs more than $10 million per incident, and many of the most expensive cases trace back to unsecured data from clinical speech, logs, or third-party transcription tools. The rise of ambient AI scribes has made physician workflows faster, but it has also expanded the attack surface. To combat this, ambient AI scribes need to be HIPAA-aligned from the first line of code. The real challenge is building an AI scribe that treats compliance, auditability, and patient trust as core infrastructure.
At Intellivon, we build enterprise-grade ambient AI scribe platforms for hospital environments, including noisy rooms, telehealth sessions, specialty-specific terminology, and strict HIPAA compliance requirements. Our systems are engineered to process speech securely, maintain accuracy at scale, apply redaction automatically, and move structured notes into EHR workflows with complete auditability. In this blog, we will walk through how we design and deploy HIPAA-compliant scribe platforms from the ground up and what it takes to make them reliable for enterprise use.
Key Takeaways of the AI Scribe Platforms Market
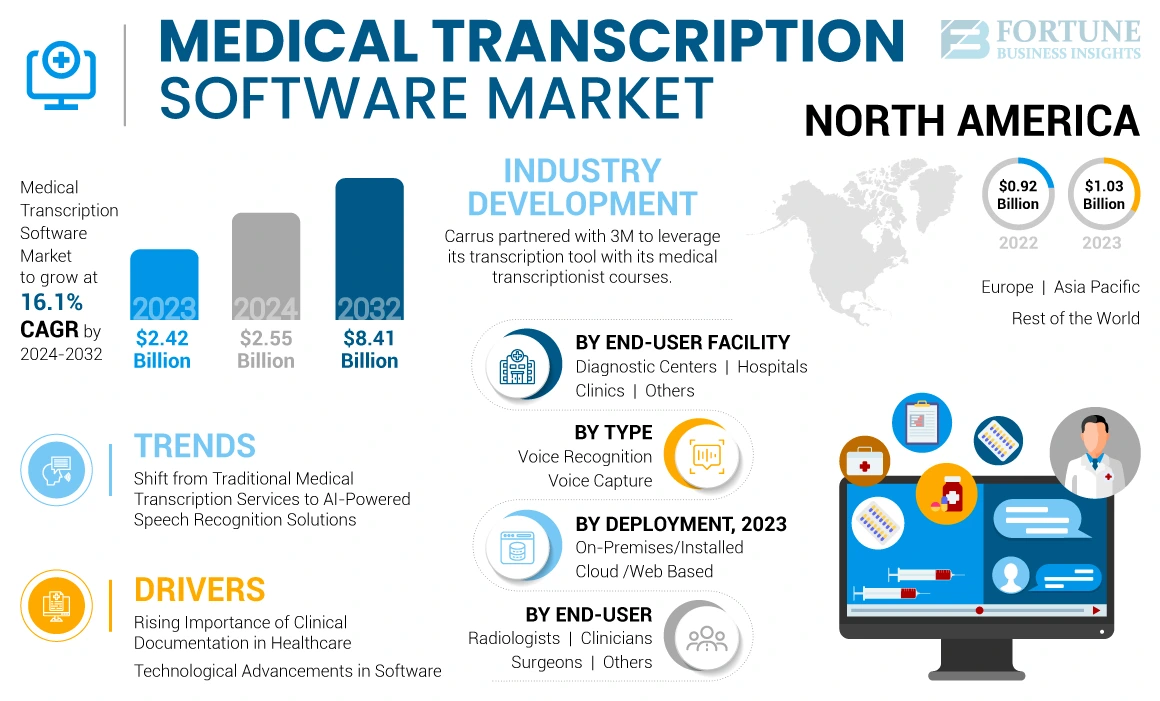
The global medical transcription software market was valued at USD 2.55 billion in 2024 and is projected to reach USD 8.41 billion by 2032, growing at a CAGR of 16.3%. This growth reflects higher demand for accurate clinical documentation, wider telemedicine adoption, and increasing reliance on AI-powered speech recognition and NLP to improve speed and accuracy. Hospitals are shifting from manual or outsourced transcription to automated scribing because the economics and operational outcomes are stronger.
Key Takeaways:
- The ambient AI scribe platform market was valued at approximately $600 million in 2025, with adoption expected to reach 40% of large hospital systems by 2028.
- Ambient AI scribes save physicians up to two hours per day and reduce documentation errors by 30%.
- Emergency medicine, psychiatry, and outpatient care show the highest adoption due to burnout reduction and workflow efficiency.
- ROI payback periods fall between 18 and 24 months, driven by faster chart closures, higher coding accuracy, and a 25% gain in patient throughput.
- More than 80% of clinicians report better patient interactions and improved satisfaction due to reduced “pajama time.”
- Cloud deployments now account for over 50% of implementations, enabling faster onboarding and smooth EHR integration with Epic and Cerner.
- Fewer than 10 vendors hold more than 75% market share, and many are expanding into real-time clinical decision support.
- Compliance remains a top adoption driver, with platforms adding audit trails and encryption to meet strict healthcare regulations.
Ambient AI scribing has shifted from early adoption to enterprise scaling. Hospitals now treat it as core infrastructure for efficiency, patient experience, and financial performance.
What Are HIPAA-Compliant AI Scribes?
A HIPAA-compliant AI scribe is a clinical documentation system that listens to patient encounters, converts spoken language into structured medical notes, and stores or transfers that information in a way that meets all federal privacy and security requirements.
Beyond transcribing speech, it protects every stage of the data journey, like audio capture, processing, storage, and EHR hand-off, using safeguards that match hospital compliance standards.
Compliance matters before rollout because ambient audio exposes more PHI than traditional documentation methods. A single capture can include names, dates, medication lists, financial details, and personal history. If even one stage of processing is unencrypted, the hospital carries the full legal and financial risk.
How HIPAA-Compliant AI Scribes Work
A compliant scribe turns real clinical conversation into structured notes while protecting PHI at every step. The workflow looks simple to clinicians, but underneath it is a secure, audited pipeline that keeps sensitive data safe.
1. Real-Time Audio Capture
The system records live encounters in exam rooms, telehealth sessions, or inpatient units. Audio is encrypted the moment it is captured, so no raw voice data sits unprotected on devices, networks, or temporary storage.
This prevents exposure long before transcription begins.
2. Medical Speech Recognition & Clinical NLP
Speech is converted into text using models trained on medical language. The engine understands drug names, procedures, diagnoses, symptoms, and clinical abbreviations.
It also detects different speakers, which helps avoid mixing up voices in conversations with nurses, residents, or family members. Generic speech tools rarely achieve this level of precision.
3. Structured Note Generation
After the text is processed, the scribe organizes the information into clean clinical documentation and filters out irrelevant chatter.
Sensitive identifiers that do not belong in the written record are removed. The output is a readable medical note that fits hospital charting formats.
4. Clinician Review & EHR Write-Back
The clinician edits or approves the note before it goes into the chart. Once confirmed, the scribe writes the structured note into the correct patient record with proper encounter mapping. Versioning prevents overwrites, and audit logs record every action for compliance.
A HIPAA-compliant scribe handles documentation end-to-end without exposing PHI or disrupting workflows. It gives clinicians automation they can trust and a security model hospitals can defend.
Regulatory Rules HIPAA-Compliant Scribes Must Follow
Once a scribe starts listening to clinical conversations, it becomes part of the hospital’s PHI ecosystem. That means every stage of the pipeline must follow the same regulations that apply to EHR systems and clinical databases.
Most transcription tools never meet this bar, which is why compliance needs to be engineered from the start.
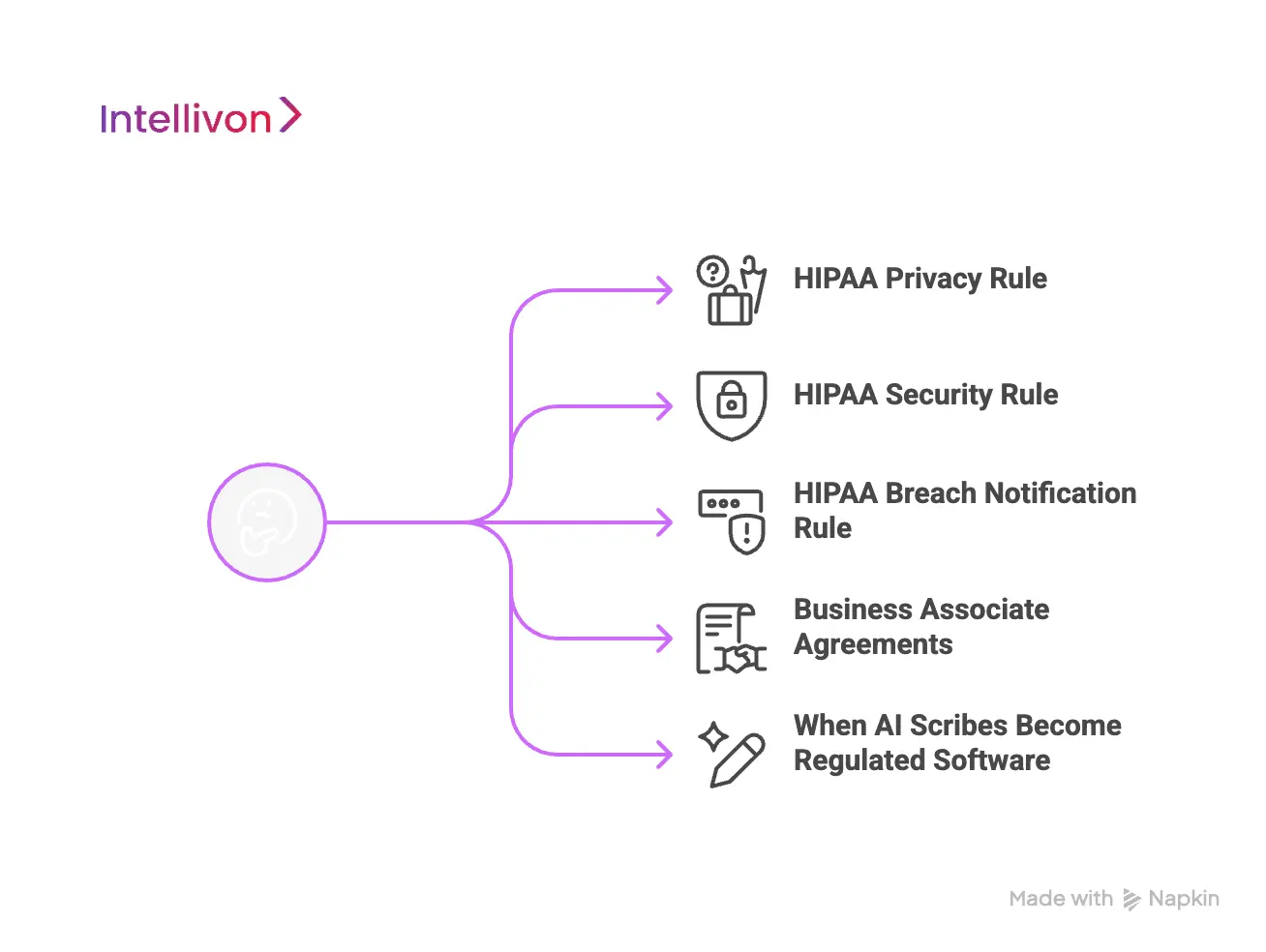
1. HIPAA Privacy Rule
The Privacy Rule determines who can access patient information and how that access is controlled.
A compliant scribe keeps PHI visible only to authorized clinical users and logs every time data is viewed, edited, or exported. This ensures full traceability if an audit or investigation ever occurs.
2. HIPAA Security Rule
The Security Rule focuses on how PHI is protected. A scribe must encrypt audio and text, restrict access through authentication controls, and store data in secure zones.
It also needs monitoring that detects suspicious behavior. If any part of the pipeline leaves PHI unencrypted or stored in unmanaged systems, the platform falls outside HIPAA boundaries.
3. HIPAA Breach Notification Rule
If a data exposure occurs, hospitals are legally required to report it. A compliant scribe makes this possible by keeping complete audit trails.
Administrators can see who accessed the note, what was changed, and whether data left the secure environment. Without these records, an organization cannot meet regulatory deadlines.
4. Business Associate Agreements
Any vendor touching PHI must sign a Business Associate Agreement. This includes cloud hosting, speech recognition engines, analytics tools, or storage services.
Without a BAA, liability shifts entirely to the hospital. Many consumer voice tools fail here because they process audio but refuse contractual responsibility for the data.
5. When AI Scribes Become Regulated Software
If a scribe goes beyond documentation and starts influencing diagnosis or treatment decisions, it may fall under FDA or EU AI Act oversight. Even when used only for note creation, many organizations still want processes that mirror regulated software to protect future innovation.
A system can only be considered “HIPAA-compliant” when every vendor, workflow, and data path meets these requirements. Anything less introduces operational, legal, and financial risk.
Can Compliant AI Scribes Prevent the $11 Million Cost of a Healthcare Breach?
Clinical documentation looks routine, but every recorded sentence becomes protected health information the moment it is captured.
When AI scribes are not designed with HIPAA safeguards, they create a new, fast-moving PHI pipeline that traditional security teams often cannot see.
1. Healthcare Breaches Are the Most Expensive in the World
According to the IBM Cost of a Data Breach Report, the average healthcare breach now costs $10.93 million per incident.
That number includes investigation, legal action, downtime, remediation, lost productivity, and patient churn. No other industry, which includes finance, government, retail, or energy, comes close.
A single unsecured audio buffer, cached transcript, or unencrypted prompt log can trigger that outcome.
2. Stolen Medical Records Have a Higher Black-Market Value
Cybercriminals target healthcare because PHI is more profitable than credit card data. Reports from Statista, Experian, and the HIMSS Cybersecurity Survey show stolen medical records selling for $250–$1,000 each, compared to $5–$30 for a stolen credit card.
A single physician encounter can contain dozens of identifiers, multiplying the risk instantly.
3. Breaches Take Almost a Year to Detect
The longer a breach remains undetected, the more it costs. The Ponemon Institute found that healthcare breaches take 269–323 days to identify and contain. Additionally, IBM reports that breaches discovered after 200 days cost 23% more.
This matters because non-compliant scribes generate data that sits outside the EHR: temporary audio storage, analytics outputs, text caches, and prompt histories. These locations rarely appear in routine security audits.
4. Shadow Data Stores Are the Real Threat
The HIPAA Journal reports that up to 89% of healthcare breaches originate in “shadow data stores”, which include unmanaged logs, unencrypted cloud buckets, cached transcription files, or developer test environments.
Most hospitals secure Epic or Cerner. Very few secure the systems that sit around them.
5. Multi-Vendor Workflows Increase Financial Exposure
AI scribe pipelines often rely on multiple vendors: speech models, cloud storage, LLM APIs, or analytics tools. IBM’s Cloud Security analysis shows that breaches involving multi-cloud or hybrid environments cost $5.29M+ on average, and take longer to resolve.
When vendors lack BAAs, the hospital carries full legal liability.
6. Downtime Makes the Problem Worse
The Ponemon Institute estimates that hospitals lose $7,500–$7,900 per minute of downtime during incident response or system shutdowns.
As a result, documentation halts, scheduling slows, notes get delayed, and care teams lose time.
7. Penalties Keep Rising
The U.S. Office for Civil Rights continues to issue heavy penalties for improper PHI handling, unencrypted media, or unauthorized third-party access. Settlements range from $10,000 to over $3 million, all publicly documented on the HHS site. Every case started with avoidable exposure.
For hospitals, a compliant scribe does more than automate notes. It eliminates the risk that traditional security tools can’t detect, prevents multimillion-dollar breach scenarios, and protects patient trust where it matters most.
Enterprise-Grade Architecture of a Compliant AI Scribe
An enterprise scribe platform is more than ASR plugged into an EHR. It is a layered system engineered to keep PHI protected from the moment audio is captured until the final note is stored.
Each layer has a specific responsibility: secure ingestion, redaction, clinical interpretation, human validation, safe write-back, and continuous auditability. If even one stage is built without compliance controls, the entire platform becomes a legal liability.
1. Secure Data Capture and Ingestion
Every recording starts with encrypted audio streaming. Data is encrypted at capture, not after it leaves the device. Hospitals often run this stage inside private networks, VPNs, or VPC-isolated environments, so voice traffic never touches consumer speech services or public endpoints.
This prevents PHI from leaking through microphones, local storage, cached browser sessions, or mobile apps.
2. Redaction and PHI-Safe Processing Pipelines
Before any model begins interpreting text, identifying elements are removed or masked. That includes names, dates, contact details, family relationships, and location details that do not belong in temporary storage.
Redaction happens inside a secure zone, and de-identified text is passed to NLP or LLM components. This prevents raw PHI from ending up in logs, analytics tools, or prompt histories that are difficult to monitor.
3. Clinical NLP With Safety Controls
Enterprise deployments require more than transcription accuracy. The system must understand medical terminology, speaker roles, medications, dosages, and abbreviations. Safety layers detect uncertainty and hold output instead of guessing.
This protects against invented clinical statements, which are the kind of errors that can damage trust and introduce malpractice risk. Many organizations require explainability records as well, showing where information came from and how the model interpreted it.
4. Human-in-the-Loop Review
Every note flows to a clinician before entering the chart. Providers correct mistakes, add missing context, or reject suggestions. This step is part of the risk model.
Human review ensures the system supports clinical judgment instead of replacing it. It also creates a clear chain of accountability if documentation is audited later.
5. EHR Integration With Versioning and Audit History
Once approved, the note is written into the correct encounter with proper timestamps and clinician attribution. Enterprise scribes use APIs or SMART-on-FHIR workflows to avoid manual copy-paste.
Version logs prevent silent overwrites, and rollback options allow administrators to revert documentation without data loss. This protects against corruption and preserves the legal integrity of medical records.
6. Monitoring, Audit Trails, and Access Controls
Every data event, including access, review, modification, and write-back, is logged. Administrators can see who touched PHI, when it happened, and where it moved. These logs support internal audits, incident response, and HIPAA investigations.
Role-based access, MFA, session controls, and least-privilege policies ensure that only authorized users can view or edit patient information.
A system designed this way does more than automate documentation. It treats audio as regulated data, enforces security boundaries across every processing step, and creates a traceable path from the first spoken word to the final signed chart entry. That is the difference between a consumer transcription tool and an enterprise-grade, HIPAA-aligned scribe platform.
Safeguards For Building HIPAA-Compliant AI Scribes
HIPAA compliance is not a checkbox. A scribe platform touches protected information at every stage of the workflow, which means privacy and security must be engineered into the system rather than added at the end. A compliant platform needs to have administrative, technical, and physical safeguards:
1. Administrative Safeguards
Administrative safeguards govern how people and processes handle PHI. They decide who can access data, how risk is monitored, and how incidents are documented.
A. Access Controls & Permissions
Only authorized clinical users should see patient information. Role-based access ensures physicians can view and edit notes, while non-clinical staff cannot. Session controls, MFA, and least-privilege permissions prevent unauthorized views or accidental exposure.
B. Workforce Training
Even the best technology fails if teams don’t handle data correctly. Hospitals require training on how AI scribes operate, how PHI is protected, and what actions trigger risk. Training reduces human error, which remains one of the top causes of HIPAA violations.
C. Risk Assessments & Audits
Regular assessments validate that PHI stays protected as the system scales. Audit reports show who accessed the data, what changed, and whether any event requires reporting. These records are critical during internal investigations and OCR reviews.
D. Vendor Management & BAAs
Every vendor involved in capturing, processing, or storing PHI must sign a Business Associate Agreement. That includes cloud hosting, speech recognition engines, analytics tools, and storage layers. Without BAAs, legal liability shifts to the hospital. Consumer transcription platforms often fail here.
2. Technical Safeguards
Technical safeguards protect PHI within the technology stack, like devices, networks, servers, and software. For AI scribes, this layer is where most breaches occur if not engineered correctly.
A. Encryption in Transit & at Rest
Audio and text must be encrypted the moment they are captured. PHI should never appear unprotected in temporary files, storage buckets, or network traffic. Encryption turns exposed data into useless data.
B. Identity & Authentication
Only verified users can access patient notes. Systems need MFA, strong credential rules, session timeouts, and revocation controls that remove access the moment a user leaves the organization.
C. PHI Minimization & Zoning
The platform should only store the minimum PHI needed for documentation. Redaction removes identifiers before text reaches NLP, analytics, or LLM components. PHI zoning ensures raw data never touches unsecured logs or prompts.
D. Audit Logs & Breach Detection
The system logs every access, view, edit, or export. If a note leaves the secure environment, administrators know who moved it and when. These logs make it possible to identify and contain incidents quickly, which is essential for compliance.
3. Physical Safeguards
Physical controls protect the hardware and data centers where PHI resides.
A. Secure Data Centers
Servers must run in controlled facilities with restricted access, monitoring, and compliance certifications. Most hospitals require SOC 2, ISO 27001, or similar security standards.
B. Device Security
Laptops, tablets, or local hardware used for recording must be protected. Lost or stolen devices are still one of the most common causes of HIPAA incidents. Encryption and remote wipe capabilities reduce that risk.
C. Backup & Disaster Recovery
If a system goes offline, PHI cannot be lost or corrupted. Regular backups, integrity checks, and recovery plans keep notes safe during outages, failures, or cyberattacks.
A HIPAA-compliant scribe doesn’t rely on one safeguard. It combines administrative policies, technical architecture, and physical security to create a closed system where sensitive data remains protected from start to finish.
How We Make HIPAA-Compliant AI Scribes
A compliant scribe is not a single model plugged into a microphone. It is an engineered workflow that treats clinical audio as regulated data from the moment a session begins. At Intellivon, each stage is designed to keep PHI protected, maintain clinical accuracy, and integrate smoothly into hospital systems.
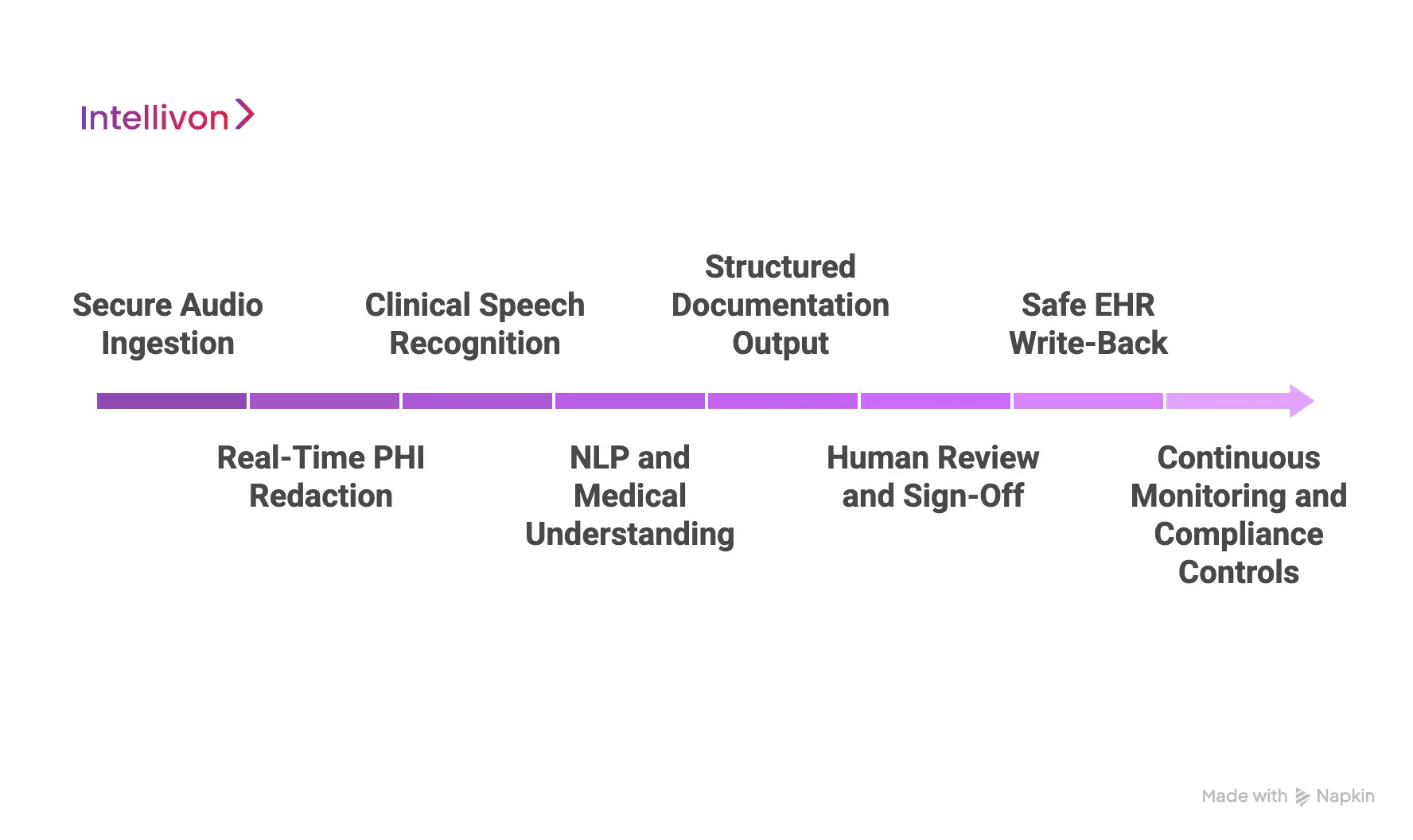
1. Secure Audio Ingestion
The process starts at the device level. Our applications stream audio through encrypted channels the moment a clinician begins recording. Nothing is stored locally, and there are no unprotected audio files sitting in device storage.
Hospitals often route traffic through private networks or VPC isolation, so PHI never touches public endpoints or consumer speech APIs. This prevents exposure before transcription even begins.
2. Real-Time PHI Redaction
Raw clinical speech contains sensitive identifiers. A compliant platform cannot allow those details to pass into logs, analytics tools, or LLM prompts.
Intellivon applies automated redaction inside a protected zone. Names, phone numbers, addresses, and other identifiers are scrubbed before the text moves downstream. This reduces PHI footprint and eliminates the biggest hidden risk in scribe deployments.
3. Clinical Speech Recognition
Transcription accuracy is critical, but hospitals need more than word matching. Our speech models are trained on clinical terminology, specialty vocabulary, drug names, and acronyms.
They work in noisy rooms, under masks, and with overlapping voices. Speaker separation ensures the system knows who said what, which prevents confusion when multiple people are talking in exam rooms or wards.
4. NLP and Medical Understanding
After transcription, the platform applies clinical NLP to extract meaning. It distinguishes relevant clinical information from casual conversation. It recognizes symptoms, diagnoses, plans, and instructions.
If the model is uncertain, it does not guess. It flags the text for review. This protects documentation quality and prevents fabricated medical statements from entering the record.
5. Structured Documentation Output
Rather than returning a raw transcript, Intellivon generates clear, structured notes that match hospital documentation formats. Histories, assessments, and plans are organized into the sections clinicians expect.
This reduces editing time and keeps documentation consistent across departments. Notes look like they were written by staff, not a machine.
6. Human Review and Sign-Off
Automation accelerates charting, but clinicians stay in control. Every note is reviewed and edited before it becomes part of the record. Providers can correct wording, add details, or reject suggestions.
This step protects clinical integrity and preserves legal accountability. It also helps teams adopt the system with confidence, because nothing changes without their approval.
7. Safe EHR Write-Back
Once a note is approved, Intellivon writes it into the correct encounter using controlled integrations. SMART on FHIR, secure APIs, and encounter mapping ensure documentation lands in the right chart with the right timestamp.
Versioning prevents silent overwrites, and administrators can track every change. If a provider edits a note later, the system keeps a full history for audit and compliance.
8. Continuous Monitoring and Compliance Controls
Compliance does not stop at deployment. The system monitors access, edits, exports, and write-backs in real time.
Administrators can see who touched PHI and where it traveled. If a policy violation occurs, alerts surface immediately. Audit logs support internal reviews, security teams, and OCR inquiries. This makes compliance measurable instead of assumed.
This is the difference between a speech-to-text tool and a deployment-ready, HIPAA-aligned scribe. Intellivon designs platforms that deliver automation without creating new exposure points, workflow disruptions, or clinical risk. The result is a system hospitals can trust technically, legally, and operationally.
Our Risk Assessment Process for HIPAA-Compliant AI Scribe Systems
Building a compliant scribe is not only about accuracy or integration. It is about identifying every place PHI could appear, every system it touches, and every failure mode that could create exposure. A structured risk assessment makes this predictable instead of reactive.
1. Data Flow Analysis
We start by mapping how data moves through the platform. That includes capture, processing, redaction, storage, user access, and EHR write-back. Each stage must operate inside protected environments, so there are no “dark corners” where audio or text can sit unseen.
2. PHI Exposure Checks
The team evaluates where PHI could land temporarily: browser caches, audio buffers, logs, analytics outputs, or LLM prompts. Any location that cannot be monitored or encrypted is eliminated or redesigned. This prevents silent leaks long before they become incidents.
3. Encryption & Access Controls
Every asset containing PHI is encrypted at rest and in transit. Only authorized users can access notes, and all accounts are tied to identity verification and session controls. If credentials are compromised, access can be revoked instantly.
4. Third-Party Compliance Review
Vendors touching PHI, like cloud platforms, speech engines, and storage tools, must meet the same compliance standards and sign Business Associate Agreements. If a provider cannot offer encryption, logging, and breach reporting, they are removed from the pipeline.
5. Redaction Accuracy Testing
Real clinical audio contains overlapping speech, noise, accents, and domain-specific language. The scribe is tested across these scenarios to verify that identifiers are removed before text reaches downstream components. This stops PHI from entering logs or prompts.
6. Audit Logs & Incident Response
Every action in the system is tracked. If someone views, edits, exports, or deletes a note, there is a record. Audit logs make it possible to respond quickly to security events and provide clear evidence during compliance investigations.
7. Clinical Safety Validation
A scribe must stay silent when uncertain. We test how the model handles ambiguity, misheard terms, similar drug names, and unfamiliar accents. If confidence drops, output is flagged for review instead of being guessed. This protects patient safety and documentation integrity.
A risk assessment ensures the platform remains secure even as usage grows. Instead of relying on trust, hospitals get verifiable proof that every part of the system protects PHI.
Overcoming Challenges In Making HIPAA-Compliant AI Scribes
Ambient AI scribes look simple in a demo. Real deployment inside hospitals is different. Clinical speech is messy, PHI appears everywhere, and compliance failures often hide in small technical gaps. These challenges determine whether a platform can operate at enterprise scale.
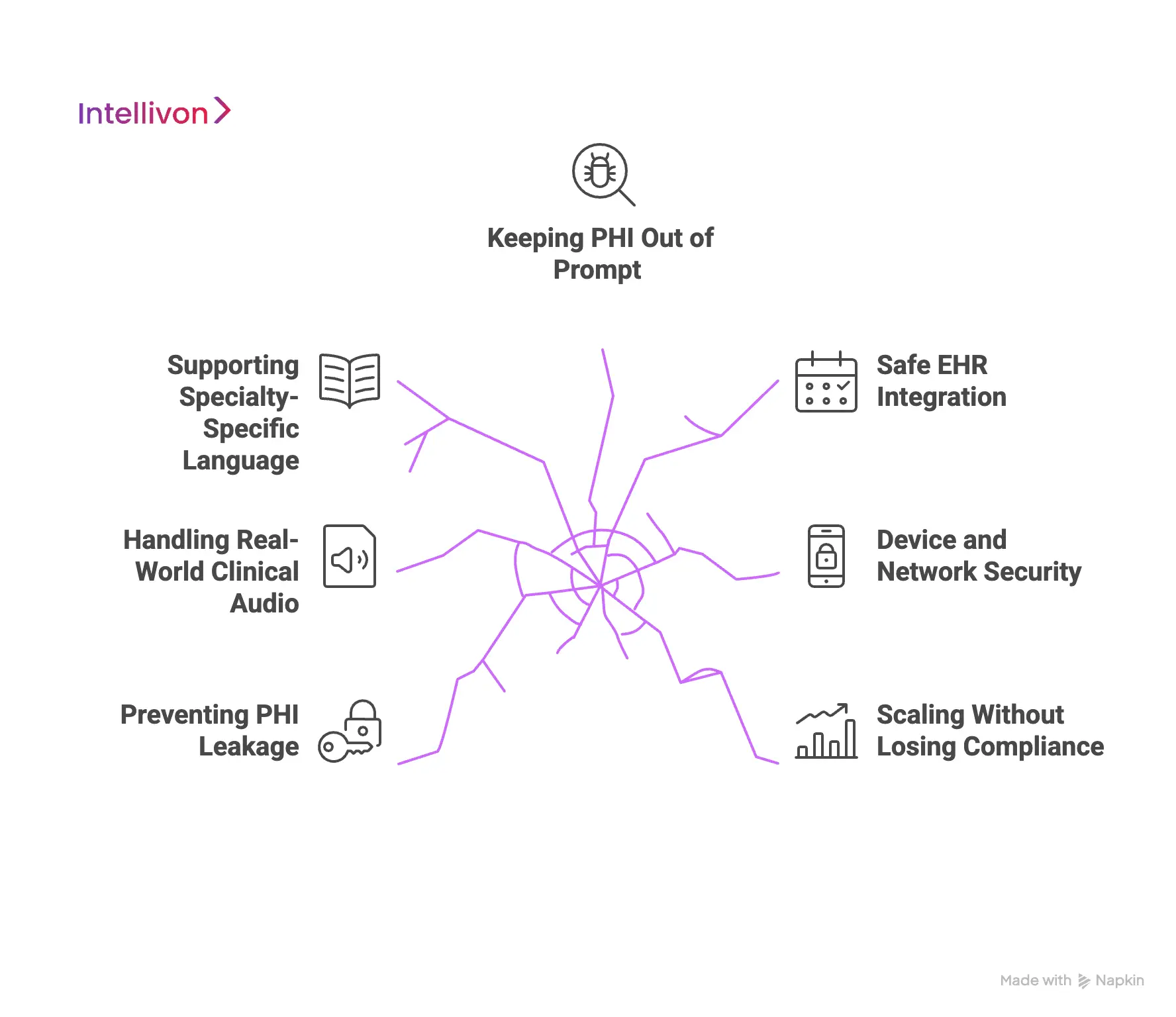
1. Preventing PHI Leakage
Clinical conversations contain identifiers that can land in transcripts, logs, analytics tools, or model prompts. One unsecured location is enough to create exposure.
How Intellivon solves it: Our experts build PHI zoning into the architecture. At the same time, Identifiers are redacted before text reaches NLP or LLM layers, and every downstream system runs in monitored, encrypted environments. Nothing touches third-party services without a BAA and full auditability.
2. Handling Real-World Clinical Audio
Hospitals are noisy. Alarms, overlapping speech, PPE, and hallway talk make transcription unreliable. Off-the-shelf ASR breaks down fast in these environments.
How Intellivon solves it: We train models on multi-speaker audio, accents, specialty vocabulary, and real hospital noise profiles. Confidence scoring catches uncertainty, so the system holds output instead of guessing.
3. Supporting Specialty-Specific Language
Clinical terminology changes by department. Cardiology, pediatrics, oncology, and behavioral health all speak differently. A single generic model introduces errors and slows clinician review.
How Intellivon solves it: We build specialty language packs with custom vocabularies and structured note templates. Output matches real documentation styles used by each service line.
4. Keeping PHI Out of Prompt
Many AI tools store text for optimization. In healthcare, that becomes a hidden risk because logs are rarely monitored with the same rigor as EHR systems.
How Intellivon solves it: Prompt and analytics layers stay PHI-clean. Redaction happens before the text reaches those components. Audit trails verify that raw PHI never lands in cached buffers, SDK logs, or developer environments.
5. Safe EHR Integration
If a scribe inserts notes into the wrong chart or overwrites existing data, clinical trust collapses. Hospitals need automation, not new failure points.
How Intellivon solves it: Notes are written into the correct encounter and timestamp using structured integrations such as SMART on FHIR and secure APIs. Versioning protects record integrity, and administrators can trace every change.
6. Device and Network Security
Tablets, workstations, and Wi-Fi networks create new attack surfaces. Lost hardware and unsecured connections remain common causes of HIPAA incidents.
How Intellivon solves it: Recording occurs inside secure applications with encrypted streams and no local storage. If a device is lost, access can be revoked instantly. Remote wipe and session limits close the loop.
7. Scaling Without Losing Compliance
A pilot with five physicians is easy. A rollout across hundreds of clinicians, sites, and telehealth channels increases data flow and risk.
How Intellivon solves it: Deployments run on cloud-native, VPC-isolated infrastructure with monitoring, redundancy, backup policies, and disaster recovery. Compliance controls scale automatically as usage grows.
These challenges appear in every hospital. Solving them requires more than speech recognition. It demands security engineering, clinical context, and infrastructure designed for regulated environments. That is the difference between a transcription tool and a HIPAA-aligned enterprise scribe platform.
Conclusion
Ambient AI scribes are becoming foundational to modern clinical workflows, but accuracy alone is not enough. Hospitals need platforms that protect PHI, integrate cleanly with the EHR, maintain auditability, and earn the trust of clinicians who rely on every word in the chart. When compliance is engineered into the architecture, a scribe reduces workload, strengthens documentation quality, and removes hidden risk.
If your organization is exploring compliant AI documentation, Intellivon can help you design and deploy a secure, scalable platform built for real clinical environments. We build systems hospitals can trust, technically, operationally, and legally.
Build a HIPAA-Compliant AI Scribe With Intellivon
At Intellivon, we design HIPAA-aligned scribe platforms that capture clinical conversations with accuracy, protect every piece of PHI, and integrate into real hospital workflows. Teams reduce documentation time, eliminate after-hours charting, and strengthen record quality without disrupting care.
Every deployment is engineered for enterprise reliability: secure infrastructure, audited data flows, and performance that scales across specialties, locations, and telehealth environments.
Why Partner With Intellivon?
- Compliance-Built Architecture: PHI encryption, access controls, audit trails, and documented data flows align with HIPAA, GDPR, and FDA expectations. Hospitals gain traceability, legal defensibility, and a predictable security posture.
- Healthcare-Tuned AI Models: Our ASR, NLP, and summarization models are trained on clinical speech, medical vocabulary, and noisy real-world environments. Notes arrive clean, structured, and ready for clinician approval.
- Seamless EHR Connectivity: Integration uses FHIR, HL7, or SMART on FHIR, so notes post directly into the correct chart and are timestamped. No copy-paste. No workflow interruptions.
- Enterprise-Ready Infrastructure: Deployments run on secure cloud or on-prem environments with load balancing, monitoring, and disaster recovery. The platform stays available even during peak demand.
- Continuous Improvement: Built-in MLOps watches for drift, retrains models, and tunes accuracy as usage grows. The system learns from real clinical behavior instead of freezing at launch.
- Zero-Trust Security: Encryption at every layer, identity verification, segmentation, and continuous threat detection protect sensitive data without slowing down clinical operations.
- Designed for Adoption: Clinician review screens, editing controls, and clear audit history build trust. Providers stay in charge of documentation, not the system.
- Healthcare Delivery Experience: Our team has years of experience designing regulated AI systems for hospitals, health tech platforms, and large healthcare networks.
Book a strategy call with our team to see how a custom HIPAA-compliant scribe could reduce workload, protect data, and scale across your enterprise.
FAQs
Q1. Are AI scribes actually HIPAA-compliant?
A1. Yes, but only when they follow the full set of HIPAA privacy, security, and breach notification requirements. A compliant platform encrypts audio at capture, stores data in protected zones, removes identifiers before NLP or LLM processing, and keeps audit logs for every access event.
Q2. Can a hospital be fined if an AI scribe mishandles PHI?
A2. Yes. If PHI passes through an unsecured service, lands in logs, or reaches a vendor without a BAA, the hospital is legally responsible for the breach. OCR penalties have ranged from small fines to multi-million-dollar settlements. Compliance must be proven through logs, access controls, and documented data flows, and not assumed.
Q3. Do HIPAA-compliant scribes store patient audio or transcripts?
A3. Only if storage is required and permitted by policy. Enterprise platforms encrypt data at rest, restrict access, and ensure notes can be deleted or retained according to governance rules. Many solutions minimize storage by processing audio in real time and only keeping approved clinical notes inside the EHR.
Q4. Can AI scribes work in noisy hospital environments?
A4. They can, but only if the speech engine is trained on real clinical audio. Enterprise-grade systems handle overlapping voices, hallway noise, accents, masks, and specialty terminology. Generic ASR tools struggle in these conditions and often reduce accuracy.
Q5. How long does it take to implement a compliant AI scribe?
A5. Timelines depend on EHR connectivity, infrastructure, and rollout plans. Many hospitals complete technical integration in weeks, then onboard departments in phases. Successful deployments focus on clinician adoption, workflow fit, and policy alignment, and not just the model.