Doctors spend nearly two hours on documentation for every hour of patient care. This goes beyond being a productivity issue and trickles into retention issues as well, directly impacting your finances. Ambient scribes offer a solution to this problem by automatically capturing patient conversations and producing clinical notes using AI. However, the main challenge is not the technology, but how to integrate it.
Without smooth connectivity to Epic or Cerner, ambient scribes turn into just another separate tool that adds more friction. However, when integrated properly, ambient documentation goes straight into your EHR. This cuts down on note completion time while keeping compliance and clinical accuracy intact.
At Intellivon, we focus on creating strong integrations that link ambient AI scribe platforms directly to Epic and Cerner settings. This blog explains our integration paths, including HL7 and FHIR APIs and native EHR modules. It also covers the compliance and security needs you’ll need to consider and the implementation strategies that make sure your ambient scribing solution delivers results effectively.
Key Takeaways of the EHR (Electronic Health Records) Market
The global EHR market is valued at $30.1 billion for 2025, with cloud-based solutions accounting for $13.85 billion and on-premise solutions reaching $16.25 billion, and projected to accelerate to $37.26 billion by 2032.
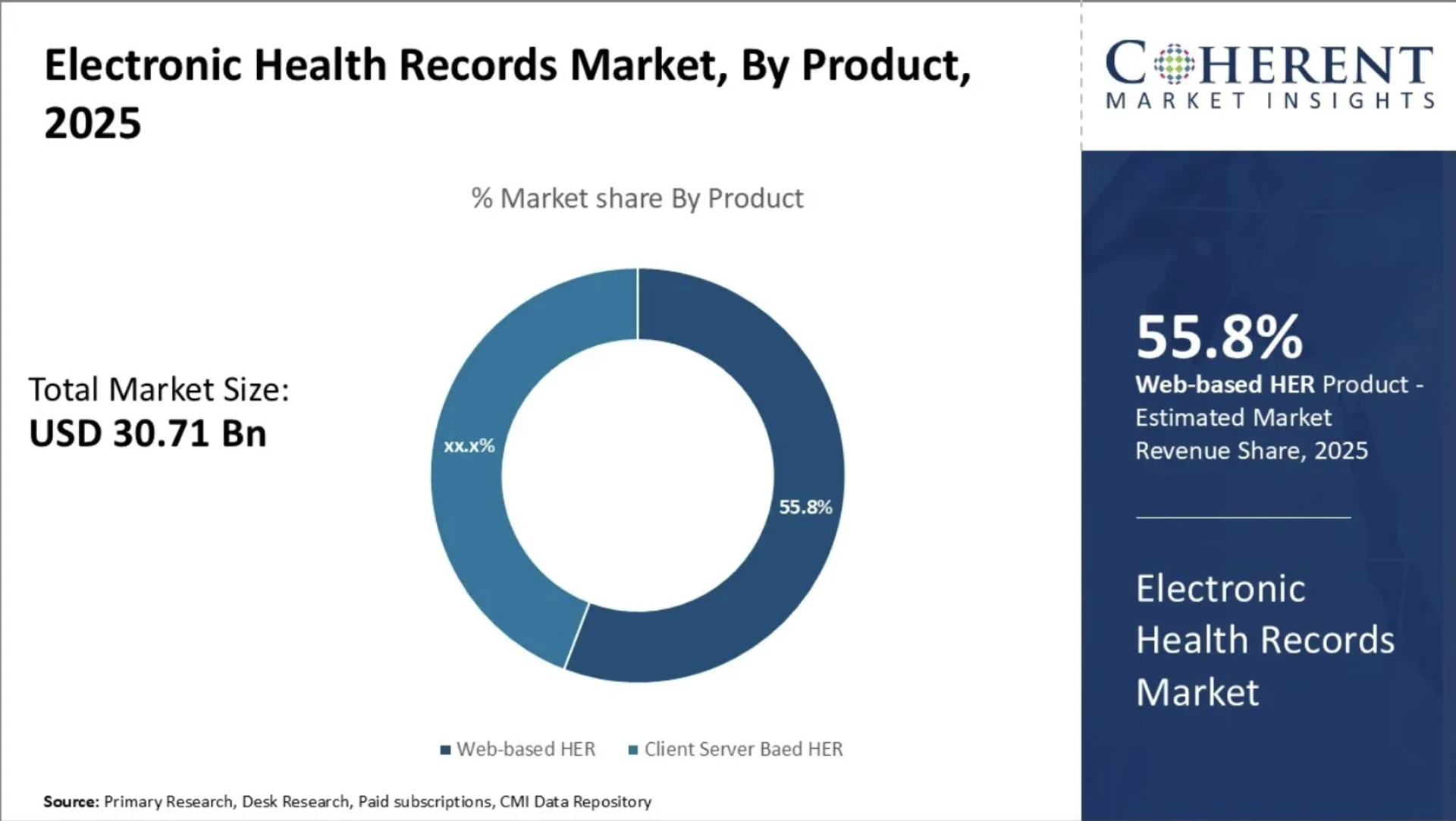
Key Market Indicators
- Hospitals account for 46.7% of market revenue, driven by high patient volumes and complex care delivery.
- Web-based EHRs now represent nearly 50% of all deployments due to scalability and reduced infrastructure burden.
- 96% of U.S. hospitals use an EHR, but user satisfaction remains mixed, averaging 60–70% among mid-market practices.
- Epic controls records for 30–94% of U.S. patients, while Cerner (Oracle Health) is investing in AI-first automation and cloud-native EHR modernization.
Ambient Scribe Adoption and Impact
- The ambient scribe market generated $600 million in 2025, with adoption reaching 35% among large health systems.
- Kaiser Permanente reports 65–70% physician usage, proving deep enterprise penetration.
- Market studies project 60% of providers will use ambient scribes by the end of 2025.
- Epic-integrated ambient deployments show a 9.3% increase in same-day appointment closure and a 30% reduction in after-hours documentation.
- Health systems report improved patient experience, more natural clinician-patient interaction, and a measurable reduction in burnout.
- Ambient scribes save clinicians up to 15,000 hours per year, restoring face-to-face communication and reducing clerical burden.
- Large enterprise hospitals report 60–75% cost savings compared to human scribes, translating into $150,000–$396,000 in annual documentation savings per site.
Hospitals adopting ambient AI scribes inside Epic and Cerner are gaining throughput, cutting documentation costs, and improving clinician retention.
These market outcomes should motivate hospital leaders to adopt ambient AI scribes now, while technology, interoperability, and EHR ecosystems are aligned for rapid deployment.
What Are Ambient AI Scribes in Hospitals?
Ambient AI scribes are software systems that listen to conversations between clinicians and patients, turning them into complete medical notes. Instead of typing during the visit or completing charts late at night, clinicians can speak naturally while the system creates a structured note that flows into Epic or Cerner.
It operates quietly in the background, easing the burden of manual documentation while allowing the clinician to control the final record. Hospitals use this method to cut down on clerical work, improve chart accuracy, and bring back direct patient engagement.
Unlike traditional transcription, ambient scribes recognize what is clinically important. They identify symptoms, medications, assessments, plans, and orders, then fill those details into the right fields in the electronic record. The physician reviews and signs the note as usual, which means existing legal and workflow requirements remain the same, and only manual typing is eliminated.
How Ambient Scribes Work in the Clinical Workflow
Ambient scribes fit into the daily routine without forcing clinicians to change how they work. Before the visit starts, the system connects to the scheduled appointment and links to the correct chart.
During the encounter, it listens through a microphone on a workstation, mobile device, or telehealth platform. There are no special commands or scripted phrases. The conversation remains natural.
As the appointment continues, the scribe builds the note in real time. It separates the history of present illness, review of systems, assessment, plan, and follow-up details.
When the visit ends, the clinician opens the draft inside Epic or Cerner, makes quick edits if needed, and signs it. Hospitals appreciate this because the approval process remains unchanged, and nothing new is added to the clinician’s workflow.
1. Connecting to the Patient Encounter
The system pulls patient details, appointment context, and encounter type directly from the EHR, ensuring every note is linked to the correct chart. This prevents documentation gaps and protects billing accuracy.
2. Listening During the Appointment
The scribe captures natural speech without requiring commands or rigid formats. Clinicians maintain eye contact and communicate freely, rather than splitting attention between the screen and the patient.
3. Building the Note in Real Time
Structured notes are generated section by section, using clinical logic that mirrors how physicians document their visits. Most of the note is finished by the time the encounter ends.
4. Review and Signature
Clinicians remain the final authority. They review, confirm accuracy, and sign inside the EHR. Nothing changes about compliance or responsibility.
How AI Works Inside Ambient Scribes
AI in ambient scribes brings together speech recognition, medical language models, and structured data logic. Speech recognition captures the conversation and converts spoken language into text. Natural language processing then identifies what matters clinically and filters out casual dialogue.
Medically relevant information is organized into the right documentation fields, such as history, assessment, or plan, so the final result looks like a note written by the clinician, not a transcript.
1. Speech Recognition
The model understands clinical terminology, abbreviations, symptoms, medications, and diagnostic language, even when spoken quickly or informally. This avoids the common errors found in consumer speech-to-text tools.
2. NLP for Clinical Structure
The system interprets medical meaning, and not just words. It recognizes relationships between complaints, findings, treatments, and outcomes, then formats the note accordingly.
3. Integration With Epic and Cerner
Once the note is ready, it is written into the EHR with the correct encounter attachment, timestamp, and authorship. The workflow stays compliant, traceable, and audit-ready.
With this setup, documentation becomes lighter and more accurate without interrupting the rhythm of clinical care. Hospitals gain measurable time back for their teams, while clinicians keep full ownership of the medical record.
Why Hospitals Need Ambient AI Scribes Integrated Into Epic & Cerner
Hospitals have already fixed the EHR problem. The real issue is the time clinicians spend feeding the EHR. Even in well-optimized Epic and Cerner environments, documentation has grown faster than clinical capacity. Ambient AI scribes close that gap only when they operate inside the EHR, not beside it.
1. Documentation Is Overtaking Patient Care
Multiple peer-reviewed studies confirm what every hospital already feels: that documentation has overtaken clinical time.
A large study published in the Journal of General Internal Medicine found that physicians spend 16 minutes and 14 seconds inside the EHR for every patient encounter.
A separate analysis in JAMA Internal Medicine reported that most clinicians add 1.5 to 2 hours of after-hours charting every night.
Digital workflows were supposed to reduce administrative burden. Instead, a study from Duke University showed the average primary care doctor performs 4,000 mouse clicks per day while charting in the EHR.
For hospitals, this means longer visit times, slower throughput, overworked clinicians, and shrinking patient capacity. AI scribes reduce the time spent documenting, but the full benefit only appears when the note lands directly in Epic or Cerner without extra steps.
2. Missed or Late Documentation
Incomplete notes are a billing problem. The U.S. Agency for Healthcare Research and Quality estimates that hospitals lose $3–4 billion every year due to incomplete or missing documentation that affects coding and reimbursement.
Peer-reviewed research published in Applied Clinical Informatics found that adding NLP-driven documentation increased correct E&M code capture by 12–17%. When ambient scribes integrate into Epic and Cerner, billing accuracy improves without adding another interface or extra steps for clinicians.
3. Hospitals Already Have the Infrastructure
Ambient scribing succeeds because hospitals do not need new systems or hardware. Epic and Cerner already provide the data pathways. According to KLAS Research and the American Hospital Association, Epic and Cerner power 60% of U.S. acute care hospitals.
FHIR-enabled API access expanded from 72% of hospitals in 2021 to 87% in 2023, according to the Office of the National Coordinator for Health IT.
HL7 International reports that 70% of U.S. clinical data moves through HL7 messages. Hospitals do not have to rebuild infrastructure or rip out legacy systems. The plumbing for ambient scribing already exists in Epic and Cerner, but it has not been fully used until now.
4. Real-Time Performance Matters
If results are delayed or inaccurate, clinicians abandon the tool. That means ambient scribing is a latency and scale problem.
Stanford’s Machine Learning Group benchmarked clinical speech recognition systems at 95% word-level accuracy. NVIDIA’s healthcare inference benchmark shows that providers trust real-time results only when end-to-end latency stays under 300 milliseconds.
A HIMSS Machine Learning panel found that a single clinic can generate 4–7 hours of voice data per clinician per day, and large systems reach petabyte-scale annually. Only solutions embedded directly into Epic and Cerner can handle this volume without overloading IT teams or violating PHI policies.
5. Solving the Workforce Capacity Problem
Hospitals are losing clinicians faster than they can replace them. Reducing documentation is a staffing necessity. Mayo Clinic research shows 71% of physicians identify documentation as the leading cause of burnout.
The Association of American Medical Colleges projects a shortage of up to 124,000 physicians by 2034. Hospitals that reduce administrative strain recover clinical hours, increase capacity, and protect their workforce.
Ambient AI scribes solve documentation problems only when they sit inside Epic and Cerner workflows. Hospitals already have the infrastructure, compliance pathways, and EHR adoption. The missing layer is automation that turns real conversation into structured notes, without adding a single click.
How Ambient Scribes Work With Epic and Cerner
Ambient scribes need to fit inside existing clinical workflows. Hospitals cannot afford more pop-ups, extra screens, or tools that operate outside the EHR. The value appears when the scribe feels invisible, where it joins the appointment, listens in the background, builds the note, and waits for the clinician to review it inside Epic or Cerner.
Every step matches the way hospitals already work, which makes adoption easier and keeps daily operations smooth:
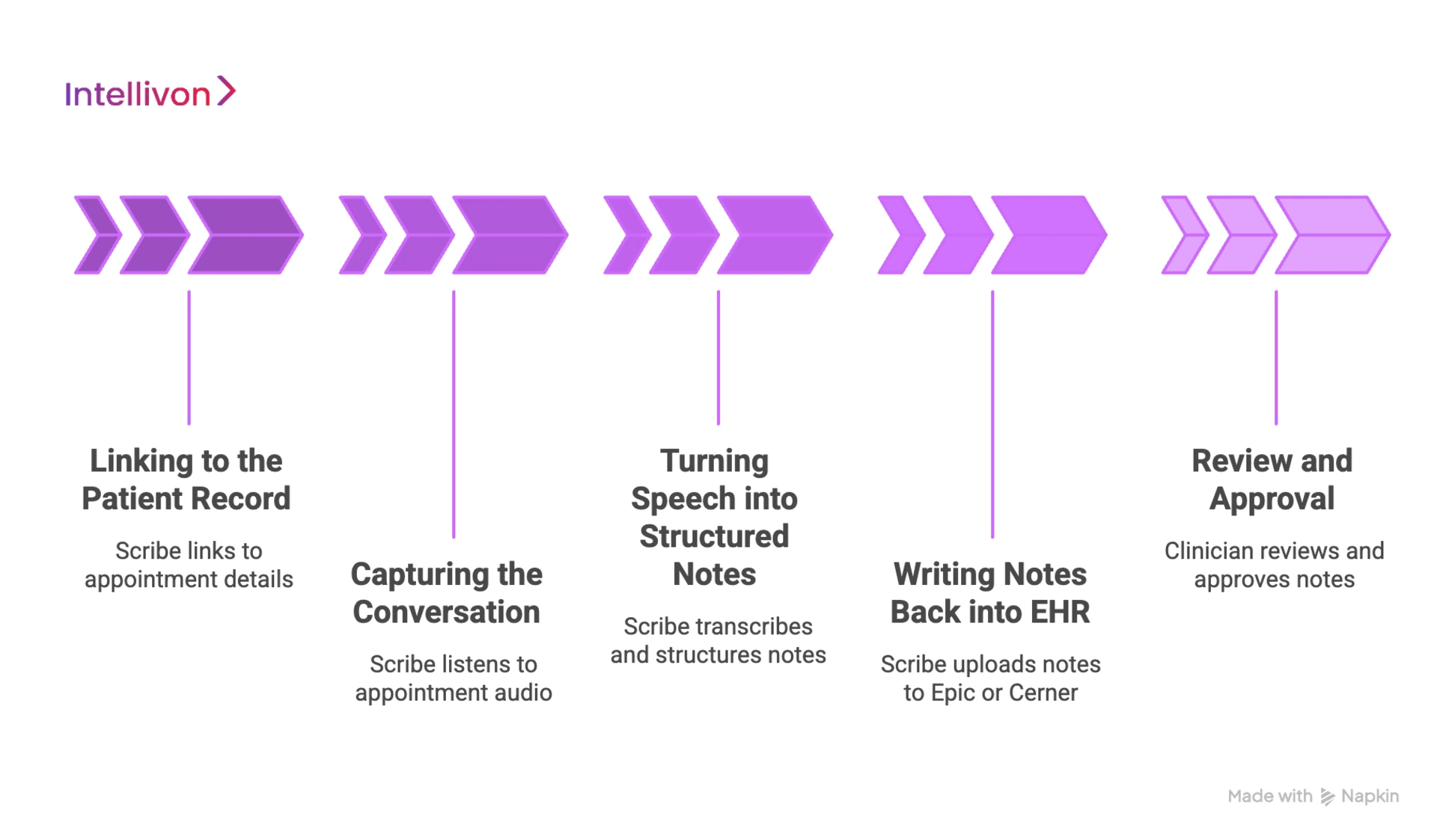
1. Linking to the Patient Record
Before a visit begins, the ambient scribe connects to the scheduled appointment. It pulls patient details, the encounter type, and the clinician assigned to the visit. This prevents notes from being stored in the wrong chart and protects billing accuracy.
For Epic users, this usually happens through Haiku or Rover on mobile or directly within Hyperspace. In Cerner environments, the connection is made through PowerChart or workstation audio access.
2. Capturing the Conversation
During the appointment, the scribe listens through a microphone on a mobile device, desktop, or telehealth platform. Nothing about the interaction changes. Clinicians speak naturally, patients respond, and the system captures what matters.
There are no commands or pauses to dictate. This is where hospitals see the most visible difference. Eye contact improves, clinicians stay engaged, and the computer stops interrupting the clinical relationship.
3. Turning Speech Into Structured Notes
While the discussion continues, the scribe starts building the note. It separates the visit into familiar sections such as the history of present illness, review of systems, and assessment and plan.
Medications, allergies, complaints, and risks are placed in the right fields. The draft is ready by the time the visit ends, so the clinician is not left with an empty template or half-written text box.
4. Writing Notes Back Into EHR
Once the draft is complete, the scribe pushes the note into the EHR. It attaches to the correct encounter, preserves timestamps, and shows the clinician as the author. Nothing about the hospital’s approval workflow changes.
The provider opens the note, makes small edits if required, and signs it for the record. Each action is stored in the audit trail, just like a manually typed note.
5. Review and Approval
Clinicians remain in control at every step. They decide what stays in the note and what needs adjustment.
When they sign, the documentation becomes part of the official medical record. Hospitals appreciate this because it keeps compliance, legal responsibility, and chart ownership exactly where they belong.
Ambient scribes remove repetitive typing, reduce charting time, and help clinicians finish notes inside the visit window rather than at the end of the day.
When the entire workflow lives inside Epic or Cerner, adoption becomes natural and hospitals see value quickly without forcing teams to change how they practice medicine.
Epic & Cerner Integration Standards for Ambient Scribes
Hospitals cannot add technology that sits on the edge of compliance. Ambient scribes must follow the same security rules, audit processes, and documentation standards already enforced inside Epic and Cerner.
The system may listen like a human scribe, but the data handling, authentication, and note delivery need to meet enterprise-grade expectations. Every integration is measured on privacy, traceability, and reliability.
1. FHIR, SMART on FHIR, and HL7
Most ambient scribes connect to Epic and Cerner through FHIR or SMART on FHIR. These standards allow the system to read patient context, link to the correct encounter, and return structured notes.
HL7 remains widely used in hospitals with mixed systems. It moves clinical data between departments, legacy tools, and the EHR. Using these standards keeps integrations predictable and makes scaling easier across multi-hospital networks.
2. Secure Authentication and Access Controls
Hospitals require strict access rules. OAuth2 is used to verify identity and protect clinical data while it moves between the scribe and the EHR.
Role-based controls restrict who can review, edit, or approve notes. These controls prevent unauthorized access and keep each action tied to the right provider. If a clinician signs the note, the EHR records it exactly like any other entry.
3. PHI Protection and Data Handling
Ambient scribes handle sensitive audio. That means hospitals expect encryption while data moves and while it is stored. No data should be left unprotected in transit, and audio is not allowed to live on devices long-term.
Hospitals prefer systems that extract only the clinical details needed to complete the note. Most deployments store the final text, not the audio.
4. Audit Trails and Legal Integrity
Epic and Cerner record every action linked to a clinical note. The integration must maintain timestamps, authorship, and version history.
If a provider edits the note, the EHR logs the change. If a note is signed, the platform records it as part of the official medical record. This protects hospitals in malpractice cases, third-party audits, and billing reviews.
5. HIPAA and HITECH Compliance
Ambient scribes fall under the same regulations as any clinical documentation tool. These platforms must meet HIPAA and HITECH requirements for data privacy and security. Hospitals often run vendor security reviews before deployment.
The system needs to show how data moves, how long it is stored, and who can access it. When a solution integrates correctly into Epic or Cerner, compliance becomes clear and verifiable.
These standards ensure ambient scribes do not disrupt clinical operations or introduce new risks. When each requirement is met, hospitals can deploy the technology confidently and let clinicians document without typing, dictation, or after-hours charting.
Tools, APIs & Frameworks for Integration into Epic
Successful Epic integrations depend on using the tools Epic already supports. Hospitals should not need custom development, manual workarounds, or new documentation portals. The best ambient scribes connect to Epic through standard APIs, established authentication models, and familiar clinical workflows. When these frameworks are used correctly, the scribe feels native inside Hyperspace, Haiku, or Rover.
1. FHIR APIs
Epic exposes a wide set of FHIR APIs that let ambient scribes pull patient context and write structured documentation back into the chart. This keeps the integration clean and scalable across multiple departments or locations.
It also avoids the need for screen scraping or manual data entry, which reduces IT maintenance. Because FHIR is a modern, standards-based approach, it works with current and future versions of Epic.
2. SMART on FHIR
SMART on FHIR allows the ambient scribe to run securely inside Epic. Clinicians do not open a separate window or use another tool. They stay in Hyperspace, complete the visit, and the note appears in the right location.
Authentication flows through Epic’s existing login, and user permissions stay intact. Hospitals prefer this method because everything remains inside a controlled environment with clear audit trails.
3. Epic App Orchard
Epic’s App Orchard provides approved access to APIs and testing sandboxes. Vendors listed in App Orchard have followed Epic’s security, privacy, and interoperability rules.
For hospitals, this creates confidence that the scribe meets enterprise requirements. It also gives IT teams the visibility they need to validate how the integration works.
4. Haiku & Rover Mobile Apps
Many Epic providers use Haiku and Rover for mobile documentation, bedside visits, and telehealth. Ambient scribes often capture audio through these apps, which makes deployment easier for outpatient clinics and hospital floors.
The drafted note returns to Hyperspace for review, so the approval process stays consistent. Clinics and hospitals see adoption rise quickly because clinicians are already comfortable with these apps.
5. Hyperspace Write-Back & Audit Trails
Once the note is complete, the scribe sends it back into Hyperspace. It lands in the correct chart, linked to the right encounter, with timestamps and authorship preserved.
Edits, approvals, and signatures follow the same workflow clinicians already use. Every step is recorded in Epic’s audit log, which keeps documentation legally defensible.
When ambient scribes rely on these tools and frameworks, hospitals gain automation without risking compliance or workflow disruption. The system blends into Epic, clinicians stay in control, and documentation becomes faster, cleaner, and more consistent across departments.
Tools, APIs & Frameworks for Integration into Cerner
Cerner environments vary more than Epic, especially across large health systems with mixed deployments. Ambient scribes need flexible integration paths that work for both modern, cloud-enabled sites and older on-premise systems. When the technology uses Cerner’s approved APIs and established workflows, hospitals can roll out automation quickly without restructuring their EHR.
1. Cerner Ignite APIs
Ignite APIs give ambient scribes access to patient records using FHIR. The system can read encounter data, identify the right chart, and write notes back into PowerChart.
Because Ignite follows widely accepted interoperability rules, hospitals avoid custom engineering work. IT teams can deploy faster, support more clinics, and keep everything inside Cerner’s security framework.
2. Millennium Web Services (REST and SOAP)
Some Cerner deployments do not have full FHIR coverage. Millennium Web Services provides REST or SOAP endpoints that let ambient scribes connect securely, even in older environments.
This matters for multi-hospital networks where Cerner runs on different versions. The scribe still pulls the encounter and sends the finished note back, without waiting for a full system upgrade.
3. PowerChart Integration
Most clinical work in Cerner happens inside PowerChart. The draft note needs to appear in the same documentation screen clinicians already use.
Ambient scribes push the structured note to PowerChart, making it easy for providers to read, edit, and sign. Nothing changes about signature rules, legal requirements, or billing workflows.
4. UI Automation for Legacy Installs
In hospitals where APIs are locked down or unavailable, ambient scribes use UI automation. This method mirrors the steps a clinician takes when typing a note into PowerChart. It captures and inputs the text automatically, without adding screens or requiring manual transfers. Hospitals like this option because it delivers automation quickly, especially in older or fragmented Cerner setups.
5. Identity, Attribution & Audit Logging
Cerner tracks every action in the chart. Ambient scribes must preserve timestamps, authorship, and version history. When a clinician signs the note, Cerner logs it as part of the official medical record.
If the note is edited later, the system records the change. This protects hospitals during billing reviews, compliance audits, and malpractice disputes.
When ambient scribes use Cerner’s approved tools and frameworks, the technology becomes predictable and safe to roll out at scale. Hospitals reduce documentation time, improve note quality, and support clinicians without adding new software for them to learn.
How We Integrate Ambient Scribes into Epic and Cerner
Hospitals do not want another pilot that drags on for months or disrupts clinical operations. They want a predictable path from evaluation to full rollout, with clear technical checkpoints and minimal workflow change. Intellivon follows a structured approach that works in Epic and Cerner environments of all sizes, whether cloud-based, hybrid, or legacy on-premise systems.
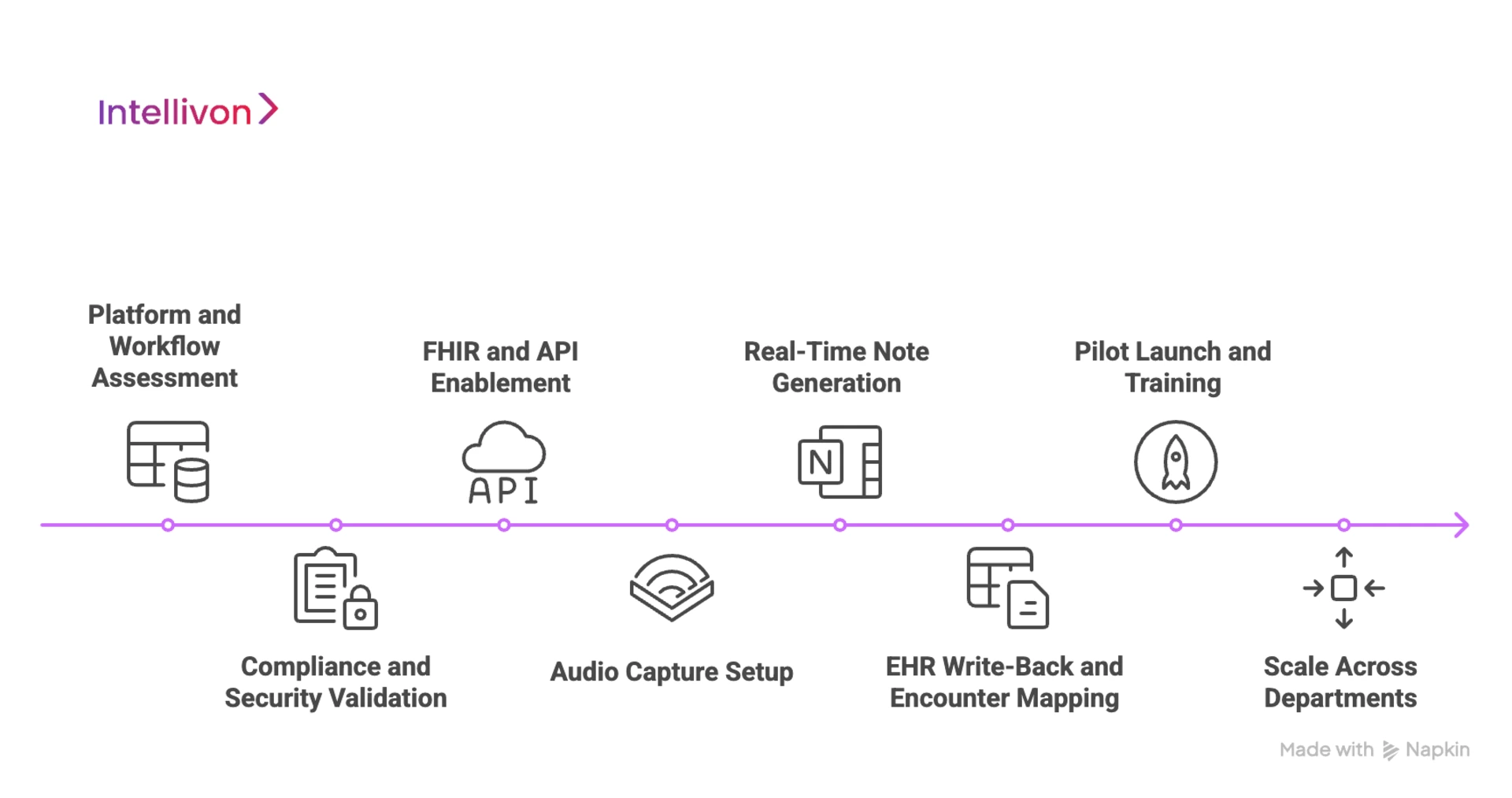
1. Platform and Workflow Assessment
Every Epic and Cerner environment has its own setup. Some hospitals manage a single inpatient facility, while others run multi-state networks with numerous specialties and outpatient centers. We start by mapping how clinicians currently document, the EHR configuration, and the sources of inefficiency.
This helps us identify which departments will benefit first and whether to use FHIR, SMART on FHIR, Ignite APIs, Millennium Web Services, or UI automation. Instead of deploying a generic integration, we tailor the strategy to actual clinical behavior.
2. Compliance and Security Validation
Ambient scribes handle PHI, so the security model must be completely secure before any clinician goes live. Our engineers collaborate with hospital IT and compliance teams to document encryption, access control, identity governance, audit trails, and retention rules. Nothing is hidden or left to be addressed later.
The outcome is a deployment where compliance officers, CISOs, and security teams clearly understand how data moves, how long it is stored, and how it is permanently removed. Hospitals can proceed knowing the system is ready for audits and meets regulatory standards.
3. FHIR and API Enablement
Modern Epic environments support FHIR and SMART on FHIR for straightforward read/write access. In these situations, we enable patient context retrieval, encounter ID linkage, and structured note placement. Cerner deployments can vary widely. Some provide full FHIR support, while others use older modules.
When FHIR coverage is limited, we revert to Millennium Web Services or secure UI automation. This allows documentation to continue without pushing the hospital into an expensive system upgrade or waiting for IT to update infrastructure.
4. Audio Capture Setup
Ambient systems should not alter how providers interact with patients. Audio capture is set up through Epic Haiku or Rover, Cerner PowerChart, secure workstation microphones, or telehealth platforms.
The system listens passively, without scripted commands or dictation rules. Clinicians speak normally, patients respond naturally, and the draft builds silently in the background. The only indication of the scribe’s presence is that the note is ready at the end of the visit.
5. Real-Time Note Generation
As the encounter proceeds, the system converts natural speech into structured documentation that includes HPI, ROS, exam findings, assessment, plan, orders, and follow-up details.
Our team adjusts the clinical language model for each specialty since an orthopedic note and a cardiology note differ. Improving specialty accuracy early reduces editing time and helps clinicians trust the system more quickly. Most providers are surprised to find that the draft needs only minor adjustments.
6. EHR Write-Back and Encounter Mapping
Once the draft is complete, the note is written back into Hyperspace or PowerChart and linked to the correct encounter. Timestamps, authorship, and legal signatures function exactly as they do in the hospital’s current process.
There are no side systems, no copy-pasting, and no separate document inboxes to check. Coders and compliance teams see notes as they always have, just tidier and finished sooner.
7. Pilot Launch and Training
We begin with a small group of clinicians across one or two specialties. Training is short because the system operates within the EHR, not in a new interface. Within a few shifts, most providers complete their notes during the workday instead of logging in after dinner or on weekends.
IT and clinical leadership receive real-time dashboards showing accuracy, latency, usage, and sign-off rates. Pilots are based on data, not guesswork.
8. Scale Across Departments
Once we prove accuracy and adoption, we expand the rollout by specialty. Some hospitals transition from outpatient clinics to inpatient units, while others start with primary care and then move into cardiology, orthopedics, emergency medicine, or telehealth.
Throughout the scaling process, our team monitors performance, note quality, and clinician feedback to ensure the system remains dependable as volume increases. Hospitals consistently see fewer late charts, faster visit wrap-ups, better revenue integrity, and improved staff morale.
This method allows hospitals to implement ambient scribes without waiting for major EHR upgrades or forcing clinicians into new workflows. Intellivon manages the technical workload while providers concentrate on patient care.
Real-World Examples of Ambient Scribes in Epic & Cerner
Ambient scribes are moving beyond pilots and into full enterprise deployment. Large health systems are using voice-based documentation inside Epic and Cerner to reduce charting time, improve note quality, and restore face-to-face patient interaction. These real-world examples show how the technology performs in production environments, and not just controlled demos.
1. Kaiser Permanente (Epic)
Kaiser Permanente is one of the largest Epic customers in the U.S., and thousands of their physicians now use Abridge’s ambient scribe directly inside Epic workflows.
The system listens during visits, generates a structured draft, and places the note into the correct chart for review and signature. Clinicians report faster documentation, fewer after-hours notes, and more natural patient conversations because typing is removed from the exam room.
2. UNC Health (Epic)
UNC Health is rolling out Nuance DAX Copilot inside Epic to automate note creation across inpatient and outpatient settings. The draft note appears directly in Epic, so clinicians never leave the EHR.
Early rollout shows reduced time-to-signature and improved note consistency across specialties. Because the tool works inside Hyperspace, IT teams did not have to introduce new interfaces or change approval workflows.
3. Lifespan Health System (Epic)
Lifespan selected DAX Copilot to serve a multi-hospital network, including primary care and high-acuity specialties. Notes are generated during the encounter and pushed straight into Epic for editing and sign-off.
The consistency of formatting across departments has been a major advantage, especially for billing teams and compliance officers who rely on standardized documentation.
4. Intermountain Health (Epic)
Intermountain is expanding its ambient documentation initiative across a multi-state network. Their deployment focuses on reducing clinician burnout and restoring time that would otherwise be spent charting after hours.
The solution generates structured notes inside Epic, matched to the correct encounter, which has led to higher throughput and shorter chart closure times. Clinical teams report fewer unfinished notes at the end of the day.
5. Adventist Health (Cerner / Oracle Health)
Adventist Health uses ambient documentation through Augmedix, which integrates directly with Cerner. The draft note appears in the appropriate Cerner workflow, making review and editing simple for clinicians who already live inside PowerChart.
Because Augmedix holds Oracle-validated integration, the rollout did not require major EHR changes. The system supports multiple specialties and maintains consistency across outpatient clinics and hospitals.
Conclusion
Ambient scribes have moved past pilots and proof-of-concept phases. Hospitals using them inside Epic and Cerner are seeing the practical benefits, like shorter documentation cycles, fewer unfinished notes, and more time for patients instead of keyboards. When the technology fits naturally into daily workflow, clinicians feel the difference at the end of every shift.
Choosing the right partner matters. Ambient documentation touches PHI, audit logs, billing quality, and clinical trust. A credible engineering team treats compliance as part of the architecture, not an afterthought. With strong security, accurate note generation, and a clean Epic or Cerner integration, the hospital gains a tool that feels dependable, not disruptive.
Integrate Ambient Scribes Into Epic and Cerner With Intellivon
At Intellivon, we engineer ambient scribe solutions that fit naturally inside Epic and Cerner. Every deployment focuses on accurate clinical documentation, seamless EHR integration, and enterprise-grade compliance. The result is a system that reduces manual charting, improves note quality, and gives clinicians time back without adding new software for them to learn.
Why Partner With Intellivon
- Compliance-First Engineering: Data governance is built into the architecture. Deployments align with HIPAA, HITECH, GDPR, and regional audit requirements, with secure PHI handling, identity control, encryption, and full traceability.
- Native Epic & Cerner Integration: FHIR, SMART on FHIR, Ignite APIs, Millennium Web Services, UI automation, Haiku/Rover support, and PowerChart write-back ensure notes appear in the right encounter for clinicians to review and sign inside the EHR they already use.
- Specialty-Trained Medical Language Models: Our NLP pipelines are tuned for orthopedics, pediatrics, cardiology, behavioral health, and more. The result is fewer edits, higher accuracy, and faster sign-off across departments.
- Scalable Cloud-Native Infrastructure: Deploy on AWS, Azure, or GCP with real-time latency targets and high-availability design. Hospitals gain performance and reliability even at enterprise volume.
- Proven Healthcare Expertise: With 11+ years in clinical AI and large-scale EHR integrations, our team works with hospitals, health systems, and multi-clinic networks that demand reliability and regulatory confidence.
Let’s build a future where clinicians focus on patients, not on clacking keyboards.
Request a strategy consultation to explore how Intellivon can integrate ambient documentation into your Epic or Cerner environment securely, compliantly, and at enterprise scale.
FAQs
Q1. How much does it cost to integrate ambient scribes into Epic or Cerner?
A1. Costs vary by EHR setup and scope. Most hospitals invest $50,000–$150,000 for full deployment, including security, API enablement, and specialty tuning. Annual optimization typically runs 15–20% of the initial build.
Q2. Do ambient scribes work inside Hyperspace or PowerChart?
A2. Yes. Modern systems write notes directly into Hyperspace (Epic) or PowerChart (Cerner), so clinicians review and sign in the same place they already document.
Q3. Is it safe to use ambient scribes with PHI conversations?
A3. Enterprise deployments operate under HIPAA, encryption, identity control, and audit logging. Audio is processed securely, and most hospitals do not store voice long-term, but only the final text remains in the EHR.
Q4. How accurate is ambient documentation in busy clinical settings?
A4. Accuracy depends on specialty models and noise handling. Systems trained for clinical speech can separate multiple speakers, filter background noise, and produce structured notes even in fast, high-volume environments.
Q5. Can ambient scribes reduce after-hours charting?
A5. Yes. Hospitals report faster note completion and fewer unfinished charts because the draft is ready at the end of the visit. Many clinicians finish documentation during clinic hours instead of at night.