Healthcare delivery faces constant pressure to do more without getting heavier. Expanding access, improving outcomes, and managing costs are all expected to happen at the same time. However, most organizations still treat virtual and physical care as separate programs. Virtual programs decrease access barriers but struggle when care needs to transition offline. In-person services offer value but remain expensive and hard to scale. Without a unified operating model, leaders focus on trade-offs instead of outcomes.
The DocGo and SteadyMD model shows a clearer path. Virtual care serves as the control layer, making in-person services more responsive, targeted, and easier to manage. Together, they create a care delivery system that meets patient needs while maintaining operational discipline.
At Intellivon, we have developed and integrated hybrid care platforms within complex healthcare settings, working directly with existing EHRs and enterprise systems. We recognize that healthcare data reflects the trust between organizations and the individuals they serve. Through this blog, we will explain how we build and steadily expand these systems from the ground up, all while maintaining trust and transparency.
Why Merge Virtual and In-Person Care Now?
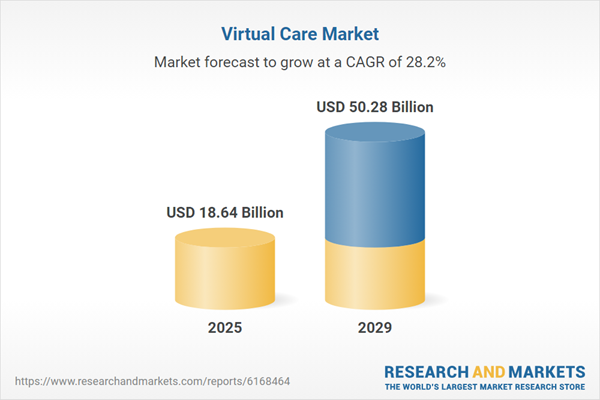
The virtual care market has expanded rapidly in recent years. Market value is projected to rise from $14.52 billion in 2024 to $18.64 billion in 2025, reflecting a compound annual growth rate of 28.4%, according to Research and Markets.
Virtual care platforms emphasize hybrid models, blending telehealth with in-person for seamless workflows, as seen in hospital “rooms of the future” initiatives with tele-rounding and AI analytics.
Key Growth Factors
- Workforce shortages and burnout: Hybrid frees bedside staff via virtual nursing/sitting, extending clinician careers and cutting labor costs fourfold.
- Regulatory easing and reimbursements: Post-COVID policies sustain 60-90% telehealth adoption, aligning hybrid with value-based care.
- Tech advancements: AI chatbots, FHIR interoperability, and wearables enable predictive analytics and 24/7 access.
- Patient demand: 40% of consumers plan ongoing telehealth use, up from 11% pre-COVID, prioritizing convenience.
Hospital Adoption Rates
- Telehealth doubled from 14% (2016) to 28% (2019), jumping to 60-90% during the pandemic
- Hybrid tracking tech rose from 36% (2012) to 55% (2015) clinically.
- Over 65% of providers/payers invest in digital platforms for hybrid patient journeys
- Rural networks like Powell achieved tenfold access gains via hybrid specialist pods.
Success Rates and ROI
- Hospitals report $2.4M+ annual ROI from diverted calls, 20-30% no-show reductions, and higher HCAHPS via virtual access.
- Hybrid boosts outcomes: Improved satisfaction, fewer transfers, and 75% Rx efficiency in similar deployments.
- Positions hospitals as innovators, with 1.9-3.1x uptake in centralized systems.
Growth Opportunities for Businesses
- White-label platforms for women’s health: Partner on EHR/staffing for hybrid clinics, targeting payers with 30% conversion uplift via AI personalization.
- Enterprise licensing: Offer RCM and compliance modules to hospitals for steady contracts and risk stratification ROI.
- AI-femtech expansion: Build preventive tools for fertility/menopause, integrating with insurers for high-throughput care.
What Is a Hybrid In-Person and Virtual Care Model Like DocGo + SteadyMD?
A hybrid platform like DocGo + SteadyMD is designed to deliver care wherever the patient is, without breaking clinical continuity. It brings virtual care, in-home services, scheduling, and documentation into a single operating model. Virtual care serves as the entry point and decision layer. In-person care is executed when physical intervention is required. Everything runs within one governed workflow.
The DocGo and SteadyMD combination reflects this structure in practice. SteadyMD contributes a nationwide virtual clinician network and longitudinal care capabilities. DocGo adds mobile, on-the-ground clinical services that can be dispatched quickly. Together, they enable care to move seamlessly from screen to doorstep, without forcing patients into facilities unless necessary.
Adoption has moved beyond experimentation. DocGo has reported high patient satisfaction and has scaled programs across large payer and provider partnerships. More importantly, the model supports real operational use cases like acute care at home, ED diversion, and care gap closure. This signals that hybrid platforms are becoming a viable delivery backbone, not a niche offering.
Features That Make It Stand Out
The DocGo and SteadyMD combination works because it integrates clinical ownership, logistics, and data continuity into one operating model. Each feature strengthens the handoff between virtual and in-person care. Together, they preserve safety, trust, and operational control.
1. Virtual Care as the Primary Control Layer
Virtual clinicians act as the first point of care and remain accountable throughout the episode. They assess symptoms, manage care plans, and decide when physical care is required. This keeps decisions centralized and reduces unnecessary in-person visits.
2. On-Demand In-Home Care Execution
Mobile clinical teams deliver care at home with full context. They arrive informed, prepared, and aligned with the virtual care plan. This reduces duplication and improves execution quality.
3. Unified Patient Data and Documentation
Virtual visits, in-home encounters, vitals, and outcomes feed into one longitudinal patient record. Clinicians access the same information across settings. This improves decision-making and simplifies audits.
4. Nationwide Coverage Without Fragmentation
Virtual care operates across all U.S. states through licensed clinicians. In-home services extend that reach locally. The platform scales geographically without creating disconnected workflows.
5. Built-In Compliance and Governance
Care delivery follows structured workflows with built-in consent tracking, role-based access, and auditable activity logs. Compliance is embedded into operations, not added later.
These features allow enterprises to scale access while maintaining control. They reduce operational drag and protect patient trust. Most importantly, they prove that virtual and in-person care can function as one system.
How Do DocGo and SteadyMD Merge Care Models?
DocGo and SteadyMD do not merge care models by layering tools. They merge them by redesigning how care decisions flow. Virtual and in-person services operate inside one coordinated delivery sequence, with clear ownership at every step.
This workflow replaces manual handoffs with structured escalation. It ensures that care moves smoothly from digital evaluation to physical execution without losing context, accountability, or data integrity. Below is how the model works in practice.
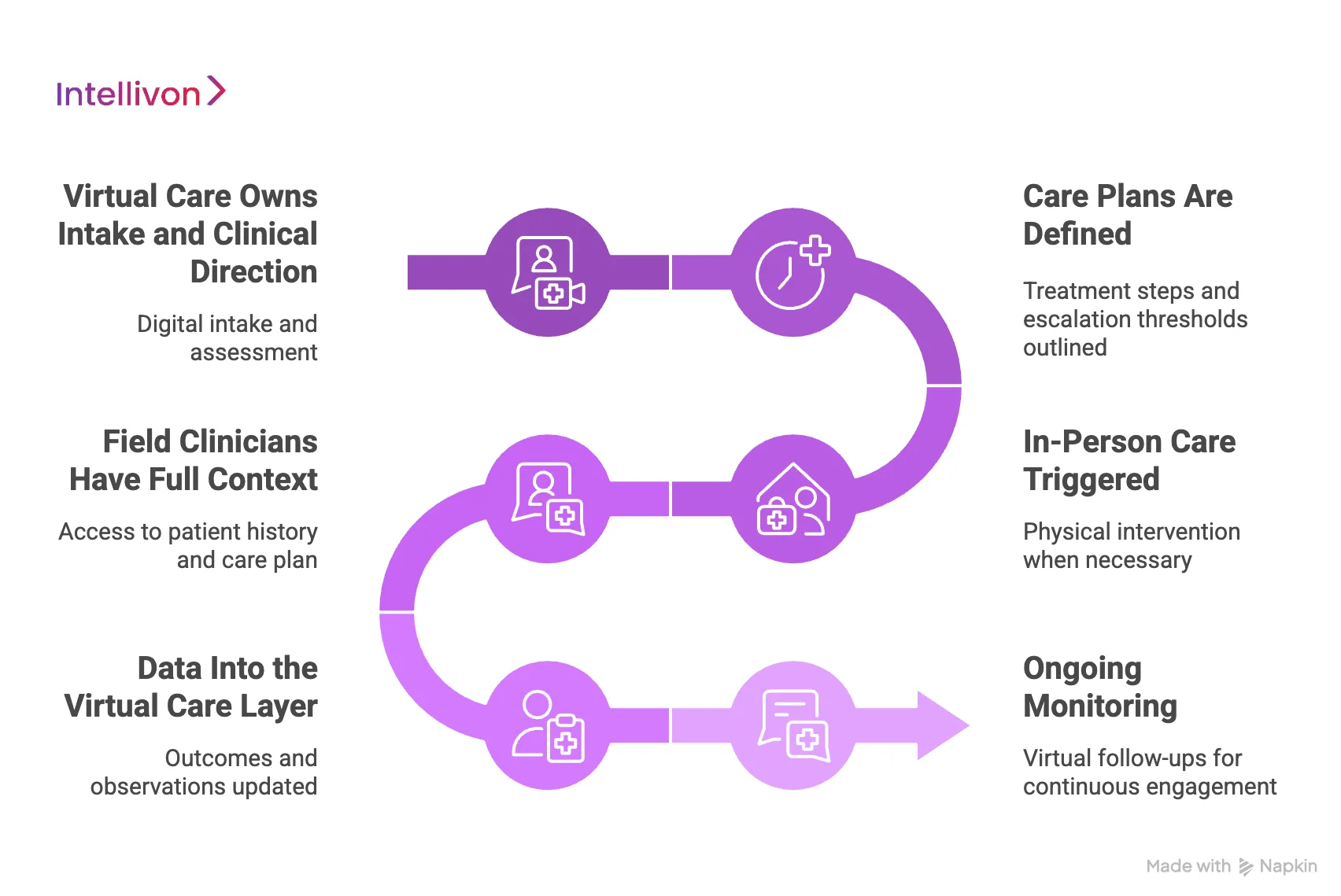
Step 1: Virtual Care Owns Intake and Clinical Direction
Care begins with a virtual clinical assessment. Patients enter through digital intake, symptom review, or scheduled follow-ups. Virtual clinicians evaluate risk, history, and current needs.
This step establishes clinical ownership early. Decisions do not wait for physical visits.
Step 2: Care Plans Are Defined
Based on the assessment, virtual clinicians create a care plan. This plan outlines treatment steps, monitoring requirements, and escalation thresholds.
Nothing is dispatched blindly. In-person care is intentional, not reactive.
Step 3: In-Person Care Triggered
When physical intervention is necessary, the platform triggers an in-home visit. The decision is clinical, not logistical.
This prevents overuse of field resources and keeps costs controlled.
Step 4: Field Clinicians Have Full Context
DocGo’s mobile clinicians receive the full care plan before arrival. They see patient history, recent vitals, and clinical notes.
This eliminates duplication. It also reduces on-site decision friction.
Step 5: Data Into the Virtual Care Layer
After the visit, outcomes, observations, and vitals flow back into the same patient record. Virtual clinicians review results and adjust the care plan if needed.
Care continuity remains intact.
Step 6: Ongoing Monitoring
Most follow-ups return to virtual care. Patients stay connected without repeated physical visits unless conditions change.
This keeps engagement high and utilization efficient.
Why a Workflow-Based Model Works
This step-by-step structure replaces ad hoc coordination with governed execution. Each phase has a clear owner, decision point, and data trail.
For enterprises, this means:
- Fewer handoff failures
- Better resource utilization
- Stronger compliance and audit readiness
- Consistent patient experience
DocGo and SteadyMD succeed because they integrate care models at the workflow level, not the interface level.
Hybrid Care Platforms Achieved 23,000 Acute Case Discharges
Hybrid care is no longer confined to low-acuity use cases. One of the clearest signals of maturity is the ability to safely manage acute episodes outside traditional hospital walls. Recent data shows that hybrid virtual and in-person care platforms have already supported over 23,000 acute care discharges through regulated hospital-at-home models.
This matters because acute care represents the highest bar for trust, governance, and operational discipline. Moving these cases out of physical hospitals requires far more than video visits or home health staffing.
1. Acute Care Moves Beyond Hospital Walls
Acute hospital care at home is not a workaround. It is a structured clinical model where patients who would traditionally be admitted receive hospital-level services at home.
Hybrid platforms make this possible by combining:
- Continuous virtual clinical oversight
- Scheduled in-home visits by trained medical staff
- Real-time escalation pathways back to inpatient settings
For enterprises, this proves that hybrid care can handle complexity, not just convenience.
2. Virtual Care Acts as the Control Layer
In these models, virtual care does not sit on the sidelines. It functions as the command center.
Clinical teams monitor patients remotely, review vitals, adjust treatment plans, and decide when in-person intervention is required. This reduces unnecessary physical visits while ensuring rapid response when conditions change.
The outcome is controlled escalation instead of blanket hospitalization.
3. In-Person Care Becomes Targeted and Intentional
Physical visits are no longer reactive or loosely coordinated. They are dispatched with context, timing, and purpose.
Field clinicians arrive with full visibility into patient history, care plans, and recent changes. This improves clinical execution and reduces duplication of effort.
From an operational perspective, this increases staff efficiency and lowers cost per episode.
4. Safety and Outcomes Hold Up at Scale
The ability to discharge acute cases safely signals operational maturity. These outcomes depend on tight coordination, reliable data flow, and clear accountability.
Hybrid platforms reduce risk by:
- Maintaining continuous clinical supervision
- Standardizing escalation thresholds
- Preserving full care documentation across modalities
For enterprise leaders, this demonstrates that hybrid care can meet quality expectations at scale.
Why This Matters for Enterprise Strategy
Acute care discharges are expensive, capacity-intensive, and difficult to scale. Hybrid platforms offer an alternative without compromising governance.
They help organizations:
- Free inpatient capacity without building new facilities
- Improve patient experience without lowering clinical standards
- Shift cost structures toward variable, controllable models
This is not a pilot-stage innovation. It is an operational lever.
Core Platform Components Required to Deliver Hybrid In-Person + Virtual Care
Hybrid in-person and virtual care only works when it is treated as a single operating system, not a collection of connected tools. At enterprise scale, every layer of care delivery must share context, follow the same rules, and write back to the same clinical truth. When platforms fail, it is rarely due to clinical gaps. It is because core components were designed in isolation.
Below are the foundational platform components required to deliver hybrid care that scales without fragmentation, protects data integrity, and maintains operational control.
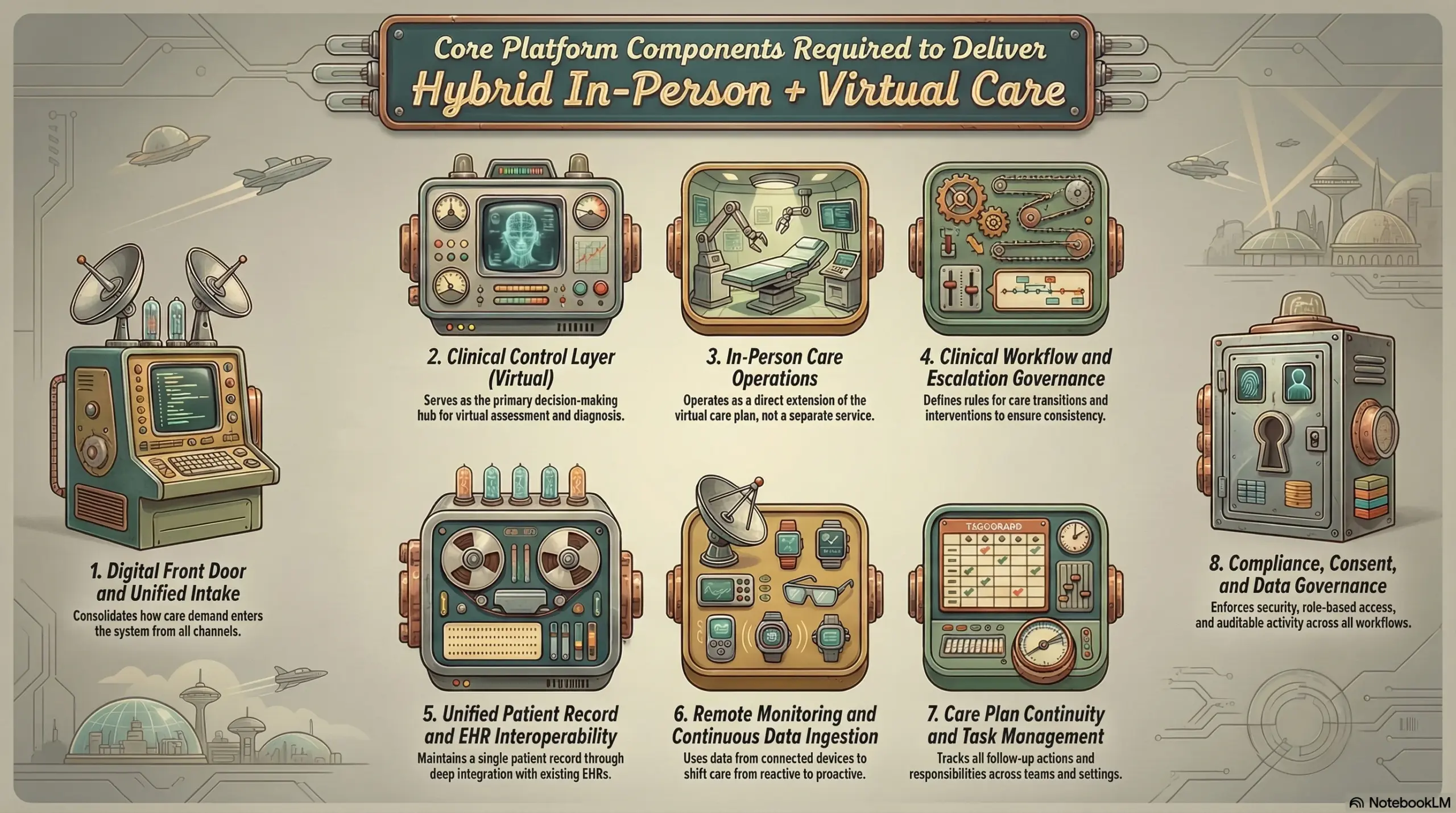
1. Digital Front Door and Unified Intake
The digital front door defines how care demand enters the system and how quickly it becomes actionable. It must consolidate intake across apps, portals, call centers, referrals, and employer channels without creating parallel workflows. Structured intake captures symptoms, risk indicators, prior history, and patient preferences early, which allows the platform to route care with intent rather than correction later.
2. Clinical Control Layer (Virtual)
The virtual care layer serves as the primary decision-making environment. It supports synchronous visits, asynchronous consults, secure messaging, and clinician workspaces that allow teams to assess, diagnose, and manage patients longitudinally. More importantly, it establishes clinical ownership early in the care journey.
In effective hybrid platforms, virtual care determines whether treatment remains digital or escalates to physical intervention. This control prevents unnecessary in-person utilization and keeps care aligned with clinical intent rather than logistical convenience.
3. In-Person Care Operations
In-person care must operate as an extension of the virtual care plan, not a parallel service line. This module manages clinician dispatch, visit workflows, on-site documentation, and task completion with full clinical context. Field teams arrive knowing exactly what to do, why they are there, and what outcomes are expected.
When in-person execution lacks this alignment, duplication increases, and trust erodes. Strong platforms eliminate that risk by embedding physical care directly into the same care logic that governs virtual delivery.
4. Clinical Workflow and Escalation Governance
Hybrid care introduces complexity that cannot be relied on judgment alone. Clinical workflow logic defines escalation thresholds, intervention triggers, and transition criteria between care settings. These rules ensure consistency while still allowing clinicians to exercise discretion within safe bounds.
For enterprise leaders, this layer is what transforms hybrid care into a repeatable operating model. It reduces variation, supports audit readiness, and enables scale without compromising quality.
5. Unified Patient Record and EHR Interoperability
Care continuity depends on a single longitudinal patient record. Virtual encounters, in-person documentation, vitals, orders, and outcomes must remain connected across the entire journey. This requires deep integration with existing EHR systems, not data duplication or shadow records.
The platform must write back cleanly without overwriting or fragmenting clinical history. When this layer is designed correctly, clinicians trust the data, and enterprises preserve the integrity of their most valuable asset.
6. Remote Monitoring and Continuous Data Ingestion
Hybrid platforms extend care beyond scheduled visits by ingesting data from monitoring devices and connected tools. Continuous signals allow clinicians to detect changes early and intervene before escalation becomes unavoidable. Alerts flow into the same care environment used for virtual and in-person management.
This layer shifts care from reactive to proactive. It also reduces unnecessary visits while improving clinical confidence.
7. Care Plan Continuity and Task Management
Hybrid care generates ongoing responsibility across weeks or months. This system tracks care plans, follow-up actions, and patient engagement steps across teams and settings. Responsibilities remain visible and assigned, regardless of where care occurs.
Without this layer, gaps appear quietly. With it, accountability stays clear and outcomes improve.
8. Compliance, Consent, and Data Governance
Healthcare platforms must earn trust continuously. This framework enforces role-based access, consent lifecycle management, and auditable activity across all workflows. Security controls operate without slowing clinicians or fragmenting care.
Compliance becomes part of execution, not an afterthought. That distinction matters at enterprise scale.
Hybrid in-person and virtual care cannot rely on stitched-together tools. It demands a cohesive platform where every component reinforces the next.
Enterprises that invest in this foundation move beyond pilots and into sustained scale. Those that do not remain trapped in coordination overhead.
Architecture for Hybrid In-Person and Virtual Care Platforms
Hybrid care architecture is not about connecting a telehealth tool to a field service app. It is about designing a system where clinical decisions, physical execution, and data governance operate through one coordinated backbone. When architecture is weak, hybrid care collapses into manual handoffs. On the other hand, when it is strong, care flows predictably across settings.
At an enterprise level, architecture determines whether hybrid care scales safely or stalls under complexity.
1. Virtual Care as the Clinical Control
In mature hybrid platforms, virtual care sits at the center of the architecture. It functions as the clinical control plane where intake, assessment, diagnosis, and care planning occur. Every care journey begins here, even when the end outcome requires physical intervention.
This design ensures that clinical ownership remains centralized. Decisions are made with full patient context, not fragmented inputs. In-person care is triggered intentionally, not reactively, which keeps utilization controlled and aligned with outcomes.
2. Event-Driven Delivery Care Modalities
Hybrid platforms rely on event-driven architecture rather than linear workflows. Clinical signals, monitoring thresholds, or care plan milestones generate events that trigger next actions. These events determine when an in-person visit is scheduled, modified, or canceled.
This approach replaces manual coordination with system logic. It also allows enterprises to adjust escalation rules without rebuilding workflows. As care models evolve, the platform adapts without disruption.
3. In-Person Care as an Execution Layer
Physical care delivery operates as an execution layer within the same architectural framework. Mobile clinicians, home visits, or facility-based services receive tasks generated by the virtual care layer. They do not create parallel records or independent workflows.
Field teams access the same care plans, documentation standards, and data structures. This keeps physical execution aligned with clinical intent and prevents divergence across settings.
4. Unified Data Layer Anchored to Existing EHRs
At the heart of the architecture sits a unified data layer that integrates with existing EHR systems. Virtual encounters, in-person documentation, vitals, orders, and outcomes flow through this layer without duplicating or overwriting records.
This approach preserves the integrity of enterprise healthcare data. It also maintains clinician trust, since the EHR remains the system of record while the hybrid platform orchestrates care around it.
5. Interoperability and Integration Services
Hybrid platforms depend on strong integration services. These services connect EHRs, scheduling systems, identity providers, monitoring devices, billing engines, and analytics tools. Standardized interfaces ensure data moves reliably across systems.
Well-designed integration layers reduce vendor lock-in. They also allow enterprises to evolve their ecosystem without breaking care delivery.
6. Security and Access Controls by Design
Security architecture must support care across locations, devices, and roles. Identity management ensures clinicians, field staff, and administrators have access only to what they need. Consent and authorization travel with the care journey.
This design protects sensitive data without slowing clinical workflows. Governance becomes continuous rather than episodic.
7. Integrated Operational Intelligence
Analytics are not an afterthought. They are built into the architecture from the start. Every action generates operational signals that inform utilization, outcomes, and cost.
Leadership gains real-time visibility into how hybrid care performs across regions and populations. Architecture becomes a source of insight, not just execution.
Why Architecture Determines Hybrid Care Success
Hybrid care fails when architecture treats virtual and physical delivery as separate systems. It succeeds when both operate within a shared control model. Architecture defines whether care scales with confidence or collapses under coordination overhead.
For enterprises, investing in the right architecture is not a technical choice. It is a strategic one that determines speed, safety, and trust.
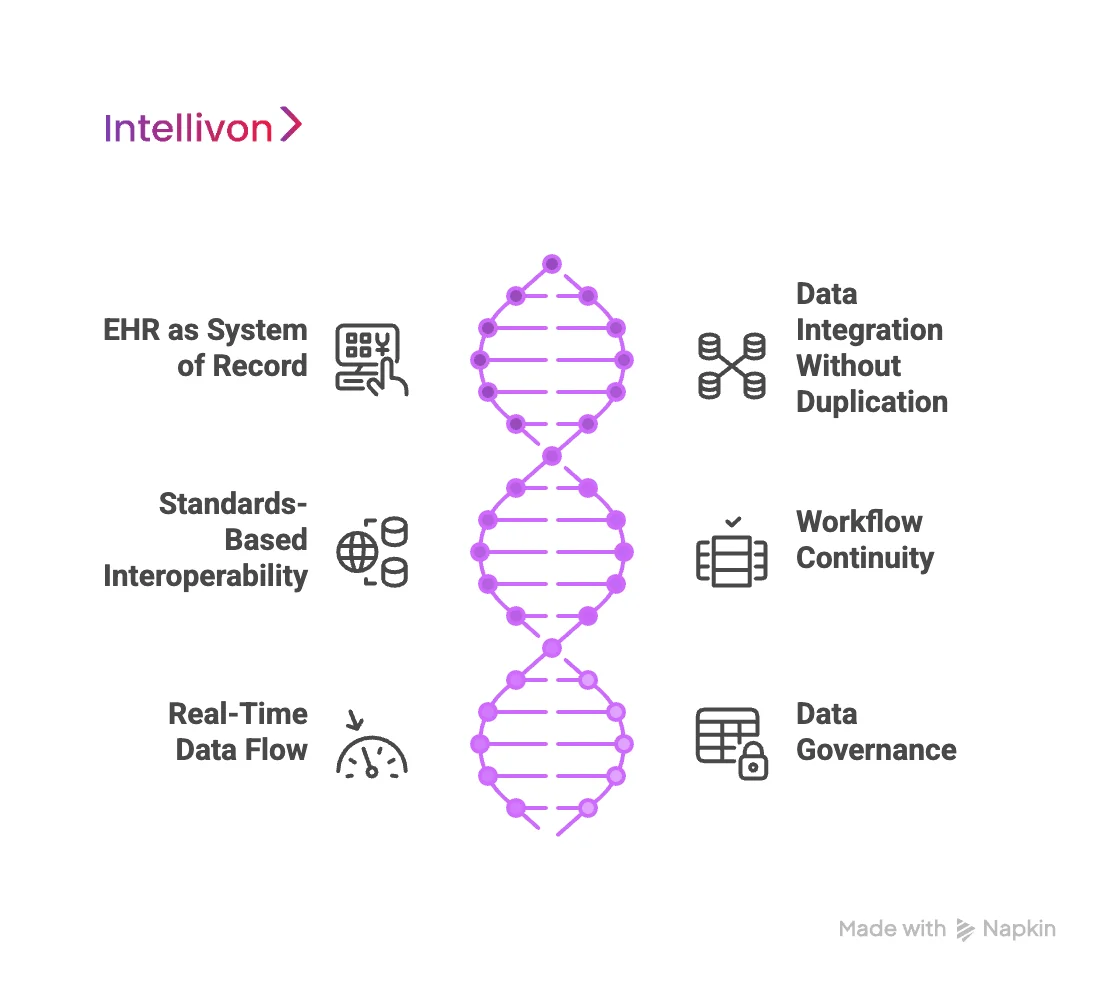
Data and EHR Integration in Hybrid Care Models
Data integration is where most hybrid care initiatives succeed or fail. Virtual and in-person care can only operate as one system if they share the same clinical truth.
For enterprises, that truth already lives inside existing EHRs, data warehouses, and operational systems. Any hybrid platform must integrate without disrupting them.
1. Treat the EHR as the System of Record
In mature hybrid models, the EHR remains the authoritative source of patient data. Diagnoses, orders, clinical notes, medications, and outcomes continue to live where clinicians already work. The hybrid platform sits around the EHR, coordinating care across settings without creating shadow records.
This approach preserves clinician trust and protects data integrity. It also avoids the risk of reconciliation errors that arise when multiple systems attempt to own the same clinical data.
2. Integrate Without Duplicating Data
Hybrid platforms must read from and write back to existing systems carefully. Virtual visits, in-home encounters, and monitoring data should flow into the patient record in a structured way. Each interaction adds context without overwriting prior history.
This requires disciplined data mapping and version control. When done correctly, clinicians see a complete care narrative rather than fragmented updates from multiple tools.
3. Use Standards to Maintain Flexibility
Enterprise healthcare environments are rarely uniform. Hybrid platforms must integrate across different EHR vendors, legacy systems, and regional configurations. Standards-based interoperability enables this without brittle custom builds.
FHIR, HL7, and secure APIs allow platforms to exchange data consistently while remaining adaptable. This flexibility matters as enterprises evolve their technology stacks over time.
4. Preserve Workflow Continuity
Integration should not force clinicians to change how they work. Hybrid platforms succeed when virtual and in-person data appear naturally within existing workflows. Orders, notes, and results should be accessible where decisions are made.
When platforms demand extra logins or manual reconciliation, adoption slows. Seamless integration keeps care moving without adding cognitive load.
5. Ensure Real-Time Data Flow
Hybrid care depends on timing. Virtual clinicians need immediate access to in-home visit outcomes. Field teams need current care plans and recent vitals before arrival. Delayed or batch-based data breaks continuity.
Real-time or near-real-time data exchange ensures decisions reflect the current patient status. This improves safety and reduces unnecessary escalation.
6. Build Governance Into the Data Layer
Hybrid care expands who accesses patient data and from where. Integration must enforce role-based access, consent rules, and audit trails across every interaction. These controls travel with the data, not just the application.
For enterprises, this protects regulatory compliance while supporting distributed care delivery.
Hybrid platforms do not fail because of care models. They fail because data integration was treated as a technical afterthought. Enterprises that invest early in clean, governed integration scale faster and with fewer disruptions.
Compliance and Liability Considerations in In-Person and Virtual Care Delivery
Compliance and liability shape whether hybrid care scales or stalls. When care moves across virtual and physical settings, risk does not disappear. It multiplies if governance is unclear. Enterprises must design compliance into the care model itself, not manage it after problems appear.
Hybrid care succeeds when responsibility, documentation, and accountability remain consistent across every interaction.
1. Define Clinical Accountability
Hybrid care often fails when accountability blurs. Virtual clinicians may assess and plan care, while in-person teams execute it. Without clear ownership, liability gaps emerge.
Enterprises must define who owns the episode at every stage. Clinical responsibility should follow the care plan, not the modality. Clear ownership reduces ambiguity during audits, escalations, and adverse events.
2. Manage Licensure and Scope
Virtual and in-person care introduce different licensure and scope rules. Clinicians must practice within state, regional, and specialty-specific boundaries. These constraints change as care crosses locations.
Hybrid platforms must enforce licensure checks automatically. Routing logic should prevent care delivery outside approved jurisdictions. Manual oversight does not scale and increases exposure.
3. Ensure Consistent Documentation
Documentation protects both patients and enterprises. In hybrid models, documentation must remain consistent regardless of where care occurs.
Virtual notes, in-home visit records, vitals, and follow-up actions should follow the same standards. Incomplete or mismatched records increase liability risk. Unified documentation also simplifies audits and legal review.
4. Embed Consent Management
Consent becomes more complex in hybrid care. Patients may consent to virtual care, in-home visits, remote monitoring, or data sharing separately.
Platforms must track consent dynamically and enforce it across workflows. Clinicians should see consent status in real time. This protects patient rights and reduces regulatory risk.
5. Secure Data Across Care Environments
Hybrid care expands the attack surface. Data flows across devices, locations, and networks. Security controls must travel with the data.
Role-based access, encryption, and audit trails should apply consistently. Field clinicians and virtual teams must access only what they need. Strong security reduces breach risk without slowing care delivery.
6. Prepare for Medical Liability and Risk Review
Hybrid care introduces new liability scenarios. Adverse events may involve multiple teams and settings. Enterprises must be able to reconstruct the full care journey.
Complete audit trails, time-stamped decisions, and documented handoffs support defensible care delivery. This preparation protects organizations during investigations and litigation.
Compliance failures arise from fragmented systems and unclear workflows. Hybrid care increases complexity, which amplifies these risks. Enterprises that design compliance into platforms reduce liability while improving care consistency.
How Intellivon Builds Enterprise-Grade Hybrid Care Platforms
Enterprises do not need another telehealth tool. They need a hybrid care platform that runs reliably inside clinical operations, protects data trust, and scales across regions without breaking workflows. That requires disciplined execution, not experimentation.
At Intellivon, we build hybrid in-person and virtual care platforms through an eight-step delivery model. Each step reduces risk and keeps clinical, operational, and data governance aligned from day one.
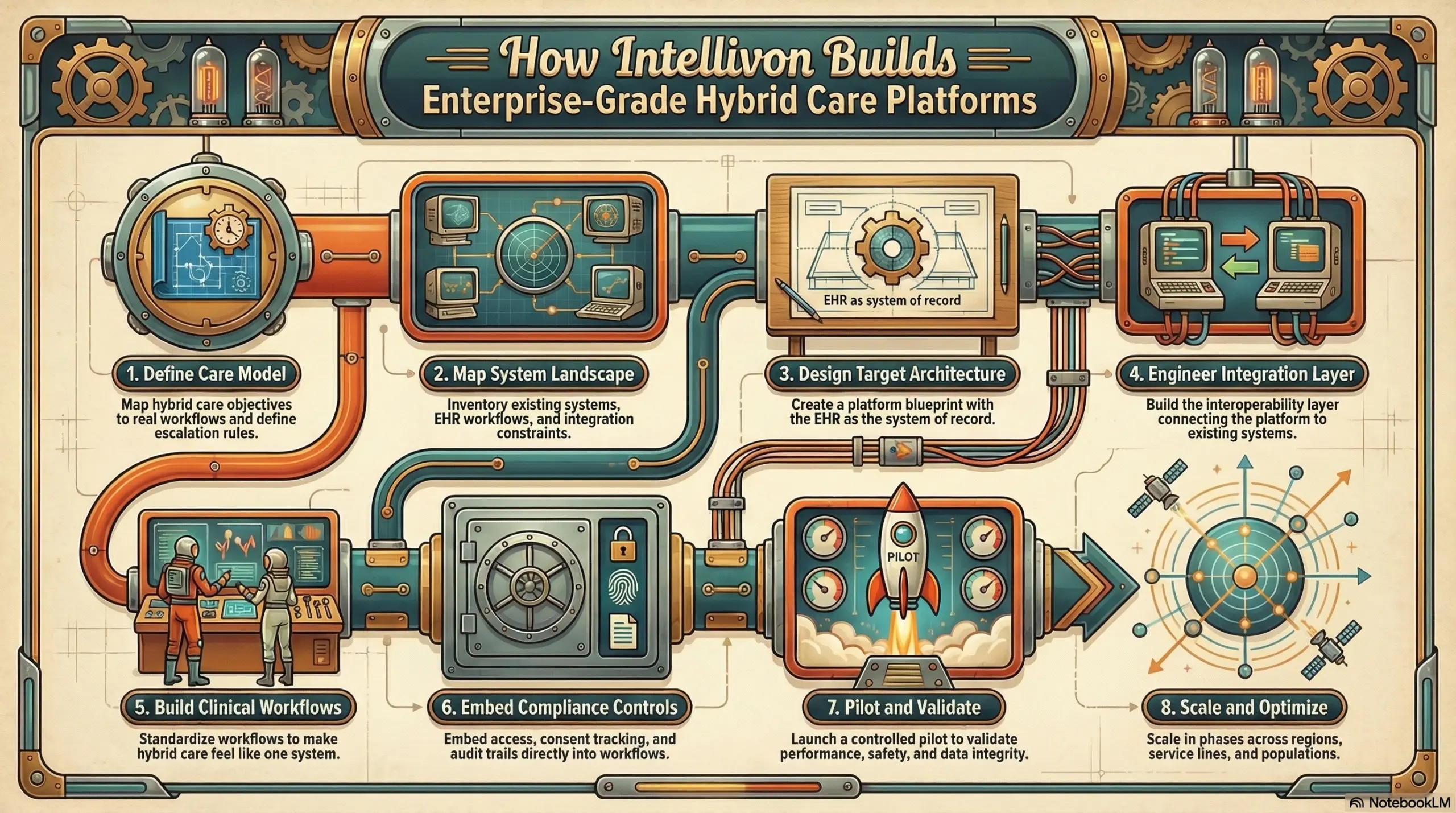
1. Define Care Model
We start by mapping your hybrid care objectives to real workflows. We identify where virtual care should own clinical direction and where in-person care must be executed. In addition, we define escalation rules, handoff points, and service boundaries so teams do not improvise under pressure.
This step clarifies ownership early. It also prevents scope creep later.
2. Map System Landscape
Next, we inventory your existing systems and integration constraints. This includes EHR workflows, scheduling tools, identity systems, billing engines, device ecosystems, and analytics stacks. We document where data lives, who owns it, and what cannot be disrupted.
Healthcare data is priceless because it underpins trust. We design around that reality.
3. Design Target Architecture
We create a platform blueprint that treats the EHR as the system of record. The hybrid platform becomes the orchestration layer that coordinates virtual care, in-person execution, and monitoring. We define data flows, event triggers, and service boundaries so the platform scales without brittle dependencies.
This architecture supports change. It also supports audits.
4. Engineer Integration Layer
We build the interoperability layer that connects your platform to existing systems without creating shadow records. At the same time, we also implement standards-based interfaces and secure APIs where possible. Additionally, we also design safe write-back patterns so new documentation and outcomes strengthen the longitudinal record.
Our goal is simple. Every care action should show up where clinicians already trust the data.
5. Build Clinical Workflows
We then build the workflows that make hybrid care feel like one system. This includes digital intake, virtual assessment, escalation triggers, dispatch tasks, visit documentation, and follow-ups. We standardize the sequence, so teams operate consistently across sites and regions.
Workflows reduce risk. They also improve throughput.
6. Embed Compliance Controls
Compliance cannot be bolted on later. We embed role-based access, consent tracking, audit trails, and policy controls directly into platform workflows. We also align documentation standards across virtual and in-person care so records remain defensible.
This step protects patients and reduces enterprise exposure.
7. Pilot and Validate
We launch a controlled pilot with clear success metrics. We validate operational performance, clinical safety, and data integrity under real conditions. In addition, we stress-test edge cases such as escalations, exceptions, and downtime scenarios.
Pilots are not demos. They are operational proof.
8. Scale and Optimize
Once the model performs, we scale in phases across regions, service lines, and populations. We add operational intelligence so leaders can track utilization, outcomes, and cost across modalities. We also iterate on workflow logic as the enterprise evolves and new programs come online.
Hybrid platforms should improve over time. They should not become technical debt. Enterprise-grade hybrid care requires more than good product design. It requires safe integration, governed workflows, and a delivery model that respects how healthcare systems operate today.
If you are building a hybrid care platform and need clarity on architecture, integration, or rollout strategy, Intellivon can help you move forward without disrupting what patients and clinicians already trust.
Build vs Buy A Hybrid Virtual Care + In-Person Platform
Most enterprises pause at this question for good reason. Hybrid care platforms touch clinical workflows, operations, data integrity, and regulatory exposure. Building in-house can feel like the safest way to retain control, especially when existing systems are complex and deeply trusted.
That instinct is valid. Control, customization, and internal ownership matter in healthcare. However, hybrid platforms introduce a level of operational and regulatory coupling that many teams only fully understand once development is underway.
What “Building In-House” Really Involves
Building a hybrid platform is not a single engineering effort. It requires designing clinical workflows that span virtual and physical care, enforcing multi-state licensure rules, and integrating deeply with live EHR systems without disrupting existing data. Each layer must remain compliant as regulations evolve.
Internal teams must also maintain the platform long term. That includes updating escalation logic, adapting to reimbursement changes, and supporting new care models as demand shifts. Over time, this work competes with other strategic priorities.
Where In-House Builds Commonly Feel the Strain
Most in-house efforts do not fail outright. They slow down. Clinical, IT, and operations teams move at different speeds. Regulatory review cycles extend timelines. Integration work becomes heavier than expected.
As the scope expands, teams often realize they are building infrastructure rather than delivering care innovation. The opportunity cost becomes clearer with time.
What Buying or Partnering Changes
Buying a packaged solution can reduce early development effort, but it often limits flexibility. Many off-the-shelf platforms struggle to adapt to enterprise workflows or integrate cleanly with existing systems.
A partnership model sits between these extremes. Enterprises retain strategic control while sharing execution risk. Platform design, compliance engineering, and EHR-safe integration benefit from prior experience without forcing rigid templates.
Why Some Enterprises Choose to Partner
Partnership decisions are rarely about speed alone. They are about certainty. Experienced partners understand how to merge hybrid platforms into existing environments without disrupting clinical data or trust.
They also bring tested patterns for compliance, escalation, and scale. This reduces the burden on internal teams and shortens the path to measurable impact.
A Practical Way to Compare the Options
Below is a neutral comparison to help frame the decision. It reflects tradeoffs, not winners.
| Decision Factor | Build In-House | Buy Off-the-Shelf | Partner to Build |
| Time to comply with the launch | Longer and variable | Faster, but constrained | Structured and predictable |
| Internal team load | High across IT, clinical, ops | Moderate | Shared and focused |
| EHR integration risk | High if untested | Moderate | Lower with prior experience |
| Flexibility over time | High | Limited | High |
| Regulatory adaptability | Internal responsibility | Vendor-dependent | Shared accountability |
| Long-term maintenance | Fully internal | Vendor-controlled | Collaborative |
How to Think About the Decision
The right choice depends on what the organization is optimizing for. If full internal ownership outweighs time, risk, and opportunity cost, building may make sense. If speed and standardization matter most, buying can work.
For many enterprises, partnering offers a balance. It preserves control while reducing execution risk. It allows teams to focus on care delivery while the platform evolves safely underneath.
Hybrid care platforms become foundational systems. Choosing how they are built determines not just speed to launch, but confidence at scale. Enterprises that approach this decision thoughtfully position themselves to move forward without disruption.
Conclusion
Hybrid in-person and virtual care is no longer an experiment or a side program. It is steadily becoming the operating model for modern healthcare delivery. Enterprises that treat it as a collection of tools struggle with fragmentation, rising costs, and growing risk. Those who treat it as a platform gain control, continuity, and scale.
The shift is not about replacing hospitals or eliminating in-person care. It is about using virtual care as the intelligence layer and physical care as targeted execution. When designed correctly, this model improves access, protects clinical quality, and creates more predictable economics across populations and regions.
Build A Hybrid In-Person And Virtual Care Platform With Intellivon
At Intellivon, we build hybrid in-person and virtual care platforms as enterprise operating systems, not telehealth tools layered onto existing workflows. Our platforms are designed to function as a unified care orchestration layer, connecting virtual clinical decision-making, in-person execution, EHR integration, and compliance governance into one controlled system.
Each solution is engineered for healthcare enterprises operating at scale. Platforms are infrastructure-first, compliance-led, and designed to support longitudinal care, acute escalation, and home-based services while preserving data integrity, clinical accountability, and predictable operating costs as care expands across regions and populations.
Why Partner With Intellivon?
- Hybrid care architecture aligned with virtual-first clinical control and targeted in-person execution
- Deep interoperability expertise across EHRs, scheduling systems, identity platforms, monitoring tools, and enterprise analytics stacks
- Compliance-by-design platforms supporting HIPAA, licensure controls, consent lifecycle management, and audit-ready operations
- Workflow-driven care orchestration enabling safe escalation, coordinated field delivery, and longitudinal follow-up
- Enterprise delivery model with phased rollout, KPI-led validation, and long-term platform scalability
Talk to Intellivon’s healthcare platform architects to explore how a DocGo + SteadyMD–style hybrid care platform can integrate into your existing systems, protect trusted clinical data, and support scalable in-person and virtual care delivery with confidence.
FAQs
Q1. What is a hybrid in-person and virtual care platform?
A1. A hybrid in-person and virtual care platform is an enterprise system that coordinates virtual clinical decision-making with physical care delivery. Virtual care owns intake, assessment, and care planning, while in-person teams execute targeted interventions. Both operate through a single workflow, data layer, and governance model to maintain continuity and control.
Q2. How does a hybrid care platform integrate with existing EHR systems?
A2. Hybrid platforms integrate with existing EHRs using standards-based APIs and controlled write-back workflows. The EHR remains the system of record, while the platform orchestrates care across virtual and in-person settings. This preserves data integrity, avoids duplication, and keeps clinician workflows intact.
Q3. What compliance requirements apply to hybrid virtual and in-person care platforms?
A3. Hybrid care platforms must support HIPAA safeguards, consent management, audit trails, licensure enforcement, and role-based access controls. Compliance must be embedded into workflows, so care teams can operate across settings without increasing regulatory or liability risk as scale increases.
Q4. How long does it take to build a hybrid in-person and virtual care platform?
A4. Most enterprises launch a Phase 1 hybrid platform within 12–16 weeks. This typically includes virtual care delivery, in-person orchestration, EHR integration, and compliance controls. Additional features and regions are added in phases once operational performance is validated.
Q5. Why do enterprises partner with Intellivon to build hybrid care platforms?
A5. Enterprises partner with Intellivon to reduce execution risk and protect existing clinical systems. Intellivon brings experience in compliance-first architecture, safe EHR integration, and scalable hybrid workflows. This allows organizations to launch faster while maintaining control, trust, and long-term flexibility.