Healthcare enterprises are under growing pressure to do more with less. Patient volumes are rising, chronic conditions are expanding, and workforce shortages are tightening operational capacity. Despite heavy investments in digital infrastructure, many systems still respond after issues escalate into costly hospitalizations or emergencies.
Predictive health monitoring apps are reshaping this model by combining AI, wearable data, and clinical records. This helps healthcare organizations detect early warning signs, anticipate risk, and act before complications occur. The impact marks a strategic shift in how enterprises deliver care and sustain long-term efficiency.
We design AI-driven predictive health monitoring apps that scale seamlessly, ensure compliance, and strengthen clinical trust. In this blog, we will break down the complete cost of building a predictive health monitoring app, from design to deployment, and how we build these apps from the ground up.
Can AI Fix Healthcare’s $600 Billion Preventable Care Crisis?
Healthcare enterprises are approaching a breaking point. Despite years of digital transformation and record health-tech investment, preventable hospitalizations, chronic disease readmissions, and operational inefficiencies still cost the industry hundreds of billions each year.
According to the OECD, unsafe care drains nearly 13% of total health budgets, amounting to roughly $606 billion annually. A large portion of that loss stems from avoidable admissions, delayed interventions, and unmanaged chronic conditions.
The Economics of Reaction Are Broken
Traditional care models rely on reaction rather than foresight. Each missed signal results in higher treatment costs, avoidable readmissions, and mounting liability.
With critical-care systems now generating over 1,000 data points per second per patient, enterprises are drowning in information they can’t yet act on effectively.
Without predictive infrastructure, healthcare remains reactive, and reaction is expensive.
The Predictive Advantage
AI-driven predictive health monitoring platforms are changing that trajectory by rebalancing healthcare economics around prevention, precision, and efficiency. Here is how:
1. Prevention Over Treatment
Predictive analytics now enable anticipating patient deterioration, infection risk, and the likelihood of readmission before symptoms manifest. These systems have demonstrated 25% lower readmission rates and up to 50% higher treatment adherence.
For large networks, these savings directly impact operating margins and value-based care reimbursements.
2. Resource Optimization at Scale
Hospitals that deploy predictive models for capacity planning report notable efficiency gains. Mount Sinai Health System, for instance, achieved 20% better utilization and 15% lower operational overhead using AI-based forecasting.
These improvements compound across enterprise operations, from staffing to supply management.
3. Portfolio-Level ROI
Predictive systems also create transparent, audit-ready data pipelines that reduce compliance risk and legal exposure. Once scaled, they serve as enterprise intelligence engines, informing executive decisions across departments.
McKinsey estimates predictive health systems could save global healthcare providers over $300 billion annually, positioning them among the most financially transformative AI investments in healthcare.
The Executive Urgency
The industry has reached a tipping point. Preventable care costs continue to rise, staff shortages deepen, and regulators are tightening audit and outcome requirements.
For healthcare enterprises, investing in predictive health monitoring rests on economic resilience. AI-powered predictive monitoring is reshaping the financial logic of healthcare itself.
What Are Predictive Health Monitoring Apps?
Predictive health monitoring apps are advanced digital systems that analyze continuous streams of health data to anticipate potential medical risks before they become emergencies.
Unlike traditional monitoring tools that only record or display metrics, these platforms transform real-time data from wearables, electronic health records (EHRs), and connected medical devices into actionable predictions.
They serve as an early warning system for healthcare enterprises, enabling proactive interventions, improved care coordination, and reduced treatment costs. For large hospital networks and insurers, these apps are operational assets that will enhance patient outcomes while strengthening financial sustainability.
How It Works
Predictive health monitoring apps operate through a layered architecture designed for data ingestion, model inference, and actionable output.
- Data Collection: Continuous input from wearables, IoT sensors, EHR systems, and patient-reported outcomes forms the foundation.
- Integration & Normalization: The data is standardized through secure APIs and health data protocols (HL7, FHIR) to ensure interoperability across systems.
- Predictive Analysis: Machine learning models process historical and real-time data to calculate risk probabilities, for example, predicting a patient’s likelihood of infection or readmission.
- Alert & Action Layer: The app sends risk-based notifications to clinicians or patients, enabling early interventions and adaptive care planning.
For enterprises, the sophistication of this workflow determines ROI. Systems that integrate seamlessly with existing EHRs and enterprise data warehouses deliver measurable operational efficiency and faster adoption across departments.
How AI Powers These Apps
Artificial intelligence acts as the engine of predictive health monitoring. It enables the system to go beyond data tracking into forecasting, personalization, and automation.
- Pattern Recognition: AI models identify hidden correlations in patient data, such as early indicators of heart failure or respiratory decline, long before symptoms appear.
- Personalized Baselines: Through continuous learning, AI adjusts predictions for each individual, accounting for lifestyle, genetics, and environmental factors.
- Predictive Alerts: AI automates triage and prioritization, flagging high-risk cases in real time so clinicians can intervene immediately.
- Continuous Improvement: As more data flows in, models retrain themselves, increasing accuracy and minimizing false alarms over time.
These capabilities make AI-driven predictive apps essential infrastructure for future healthcare systems. They turn fragmented, reactive operations into intelligent, proactive ecosystems that anticipate patient needs, optimize resources, and elevate long-term enterprise value.
Key Takeaways Of The Healthcare Predictive Analytics Market
The global healthcare predictive analytics market is scaling rapidly, reflecting the industry’s shift toward proactive, data-driven care. Valued at USD 14.51 billion in 2023, it grew to USD 17.99 billion in 2024 and is projected to reach nearly USD 154.61 billion by 2034, expanding at a CAGR of 24% (2024–2034).
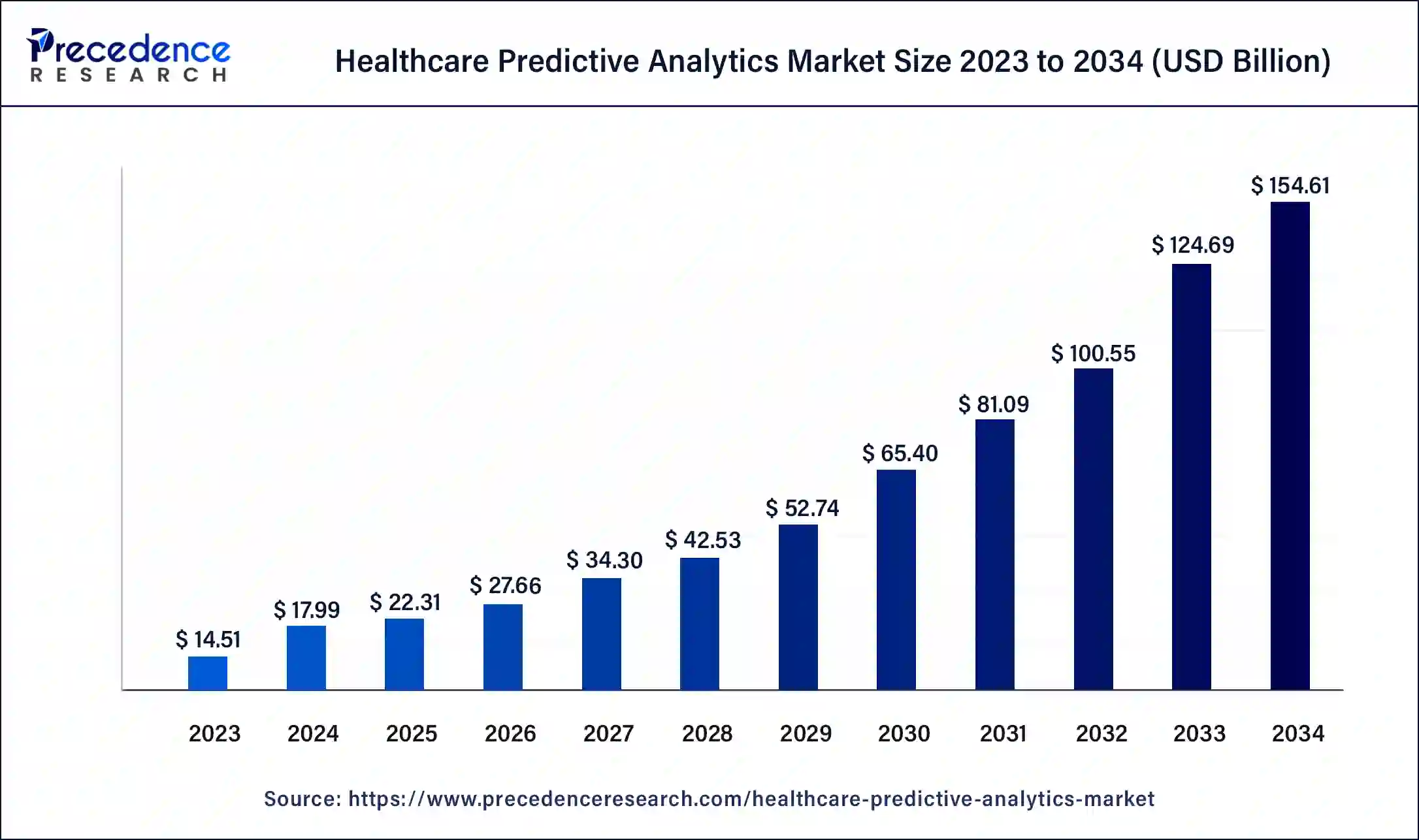
Key Market Drivers
- Rising Wearable Adoption: Growing integration of IoT-enabled wearables and smartphone-based monitoring for chronic disease management, mental health, and medication compliance.
- Preventive Care Mindset: Increasing health awareness and the shift toward preventive care, supported by insurers and providers promoting digital tools to reduce hospital costs.
- AI and Data Innovation: Rapid integration of AI-powered predictive analytics, blockchain-secured health data, and virtual health assistants enabling personalized care insights.
- Telemedicine Expansion: Broader use of telehealth and remote patient monitoring to enable continuous health tracking, early intervention, and improved outcomes.
- Regulatory Confidence: Strong data protection frameworks such as HIPAA (U.S.) and GDPR (Europe) are fostering enterprise confidence in digital health adoption.
Enterprise Investment Trends
- Rising AI Adoption: Around 29% of healthcare leaders are already investing in generative AI for digital health, with 56% planning to do so within three years.
- Strong Funding Momentum: AI-based digital health startups accounted for 40% of Q1 2024 investment, totaling $1.1 billion in venture funding.
- Strategic Enterprise Motivation: Organizations are investing to predict outcomes, optimize operations, enhance diagnostics, and improve patient engagement through predictive health platforms.
In summary, the predictive health monitoring apps market is entering a high-growth phase driven by chronic disease prevalence, rising consumer awareness, and enterprise adoption of AI-driven technologies.
For forward-looking healthcare organizations, investing in predictive health platforms is a strategic opportunity to lead in personalized, preventive, and data-secure healthcare delivery.
Core Features Of A Predictive Health Monitoring App
The purpose of predictive healthcare monitoring apps extends beyond data collection to empowering clinicians, insurers, and healthcare networks with actionable foresight. When designed well, these platforms redefine operational efficiency and financial sustainability for entire healthcare enterprises. Below are features that form the foundation of every enterprise-grade predictive healthcare monitoring solution.
1. Data Collection and Integration
Prediction starts with reliable, real-time data. A predictive healthcare monitoring app continuously aggregates information from wearables, IoT medical devices, EHRs, and connected hospital systems.
This steady data flow, which is standardized through FHIR or HL7 protocols, ensures nothing falls through the cracks. The result is a unified, continuously updating view of patient health that allows AI models to detect trends early.
2. AI Predictive Analytics Engine
This is the heart of the platform. Machine learning algorithms analyze millions of historical and live data points to identify emerging health risks, whether it’s early signs of cardiac distress, respiratory decline, or infection probability.
Over time, the engine refines its predictions through continuous learning, giving clinicians a window into what might happen next, not just what’s happening now.
3. Personalized Health Scoring
Every individual carries unique risk factors. A dynamic health scoring model translates complex analytics into a simple, intuitive metric that reflects a patient’s real-time wellness. It accounts for age, genetics, medication adherence, and activity levels to provide an evolving score that clinicians can monitor.
This personalized index helps healthcare enterprises prioritize patients who need attention most, improving care coordination and reducing costs.
4. Real-Time Alerts
Time is critical in healthcare. When the system detects a risk pattern, such as a sharp heart-rate deviation or a drop in oxygen saturation, it triggers instant alerts to clinicians and caregivers.
These notifications, displayed through intuitive early-warning dashboards, allow rapid triage and prevent potential emergencies. For enterprises managing high patient volumes, this automation minimizes escalation costs while enhancing responsiveness.
5. Interoperable EHR
Prediction thrives on connectivity. To work across departments, the app must integrate seamlessly with existing hospital systems, diagnostic devices, and insurer databases.
Using a secure API-driven architecture, it synchronizes health data in real time while maintaining consistency across platforms. This interoperability transforms fragmented information into a single predictive ecosystem that supports enterprise-wide decision-making.
6. Compliance Security Framework
Healthcare prediction is only as strong as its data governance. A predictive app must embed HIPAA, GDPR, and FDA-compliant frameworks to secure sensitive information throughout its lifecycle.
Encryption, multi-layered authentication, and role-based access protect patient trust while ensuring audit-readiness.
7. Patient Engagement Interfaces
Prediction without engagement has no impact. A predictive healthcare monitoring app should empower clinicians with visual dashboards to interpret risk trends, while offering patients intuitive mobile interfaces that promote accountability and adherence.
These engagement touchpoints close the feedback loop, transforming AI-driven predictions into collaborative, proactive care decisions.
8. Explainable AI and Model Governance
Transparency builds trust in AI-led medicine. Explainable AI (XAI) ensures clinicians understand how and why a particular risk score or prediction was made. This interpretability strengthens adoption, helps satisfy regulatory scrutiny, and promotes ethical governance.
For enterprises, it’s what turns advanced algorithms into accountable, real-world clinical tools.
Each of these capabilities supports a single goal, which is turning healthcare from reactive to predictive. Predictive healthcare monitoring apps are becoming the operational backbone of next-generation healthcare systems.
Cost Of Building a Predictive Health Monitoring App
Building a predictive healthcare monitoring app involves much more than coding an interface. It’s an exercise in integrating data science, compliance frameworks, and interoperability into a system that performs reliably under enterprise conditions. The total cost depends on factors like scope, infrastructure, regulatory alignment, and the level of AI sophistication required.
For most healthcare organizations, the average cost to build a predictive healthcare monitoring app ranges between $50,000 and $150,000, depending on how deeply AI, analytics, and compliance systems are integrated.
1. MVP (Minimum Viable Product): $50,000 – $75,000
A minimum viable version focuses on the essentials:
- Core patient monitoring features connected to wearable or device data.
- Simple AI models offering preliminary health insights or alerts.
- Basic dashboards for patients and clinicians.
- Standard data security and cloud hosting setup.
This version is ideal for pilot projects or early-stage hospital programs that want to validate predictive functionality before full-scale deployment.
2. Mid-Tier Predictive App: $80,000 – $110,000
This level includes expanded intelligence and enterprise integration.
- Machine learning models trained on clinical datasets for risk scoring, readmission prediction, or trend analysis.
- Seamless integration with EHR systems (FHIR/HL7) and connected IoT sensors.
- Custom dashboards for clinicians and administrators with role-based permissions.
- HIPAA and GDPR-compliant architecture, complete with encrypted APIs and secure authentication.
At this range, enterprises start achieving operational efficiency, where the app actively supports preventive care workflows and data-driven interventions at scale.
3. Enterprise-Grade Predictive Platform: $120,000 – $150,000
A full-scale predictive platform functions as a connected ecosystem.
- Advanced AI engines for continuous health forecasting and personalized treatment recommendations.
- Integration with multi-hospital networks, insurer systems, and telemedicine portals.
- Real-time alert systems using AI-driven triage and early-warning dashboards.
- Comprehensive compliance features, model governance, and explainable AI frameworks.
- Scalable cloud infrastructure capable of handling thousands of patient data streams simultaneously.
This investment is suited for large healthcare providers, insurers, and enterprise networks building long-term, data-driven care ecosystems.
Balancing Cost and Value
Predictive healthcare apps are long-term assets, not one-time builds. A well-designed system can reduce hospital readmissions by 20–30%, improve treatment adherence by 50%, and strengthen compliance readiness across departments. The returns from these efficiencies often exceed the initial investment within the first operational year.
Enterprises should view the $50,000–$150,000 investment range as the cost of building foundational intelligence into their healthcare operations, a cost that pays for itself through better decisions, improved patient outcomes, and sustainable growth.
Phase-Wise Cost Breakdown of Building a Predictive Healthcare Monitoring App
At Intellivon, we design predictive healthcare monitoring systems that balance innovation with cost sustainability. Our pricing framework adapts to each enterprise’s clinical workflows, compliance requirements, and infrastructure scale, rather than enforcing a one-size-fits-all model.
If early projections exceed budgets, we refine scope collaboratively while preserving the app’s core intelligence, which is accuracy, interoperability, compliance, and trust.
Phase-Wise Cost Estimates
| Phase | Description | Estimated Cost Range (USD) |
| 1. Discovery & Strategic Alignment | Requirement gathering, user journey mapping, compliance scoping (HIPAA, GDPR, FDA), ROI modeling, and KPI alignment workshops. | $8,000 – $15,000 |
| 2. Architecture & Design Blueprint | Designing the system’s architecture — data ingestion pipelines, AI model placement, dashboard flow, and integration mapping for EHR and IoT systems. | $10,000 – $20,000 |
| 3. Data Preparation & Integration Setup | Aggregating and cleaning patient data, establishing secure API connections, integrating wearable/IoT data streams, and setting up FHIR/HL7 interoperability. | $10,000 – $20,000 |
| 4. Core AI Model Development | Training and validating predictive algorithms for risk scoring, early anomaly detection, and readmission forecasting using real or synthetic datasets. | $15,000 – $30,000 |
| 5. Front-End & Dashboard Development | Creating clinician dashboards, patient engagement interfaces, and real-time alert systems with visual analytics and reporting capabilities. | $8,000 – $18,000 |
| 6. Security & Compliance Framework | Implementing HIPAA/GDPR data encryption, anonymization protocols, explainability modules, and audit trail systems aligned with healthcare regulations. | $7,000 – $15,000 |
| 7. Testing & Quality Assurance | Verifying AI accuracy, stress testing data pipelines, ensuring compliance readiness, and conducting pilot rollouts with hospital teams. | $5,000 – $10,000 |
| 8. Deployment & Cloud Integration | Cloud deployment, multi-region hosting, uptime monitoring, disaster recovery setup, and initial user onboarding for clinicians and administrators. | $5,000 – $12,000 |
- Total Initial Investment Range: $50,000 – $150,000
- Ongoing Maintenance & Optimization (Annual): 15–20% of Initial Build Cost
Hidden Costs Enterprises Should Anticipate
- Integration Complexity: Legacy hospital or EHR systems often require custom connectors or middleware for seamless data synchronization.
- Regulatory Overhead: Continuous validation, audits, and documentation for HIPAA, GDPR, and FDA compliance can add recurring expenses.
- Data Harmonization: Cleaning and normalizing unstructured patient data from multiple sources takes time and resource allocation.
- Cloud & API Usage: Costs scale with the number of patients monitored, data frequency, and real-time analytics load.
- Adoption & Training: Clinical teams need onboarding to interpret AI-driven insights and integrate predictions into their workflows.
- Model Retraining: Predictive algorithms must be recalibrated periodically as new data patterns emerge.
Best Practices to Prevent Budget Overruns
- Start with a Focused Scope: Build a predictive model around one chronic condition (e.g., cardiac or diabetic risk) before expanding coverage.
- Embed Compliance Early: Design data governance frameworks from day one to avoid retrofitting costs.
- Use Modular Architecture: Reuse data ingestion, analytics, and alert modules across multiple predictive programs.
- Prioritize Explainability: Ensure AI outputs are interpretable by clinicians to accelerate approval and trust.
- Maintain Human Oversight: Keep physicians and data scientists in the loop to validate predictions and minimize bias.
- Iterate Gradually: Roll out updates, retraining cycles, and feature expansions in controlled sprints to maintain stability.
When enterprises work with Intellivon, they gain a technology partner focused on sustainability, compliance, and measurable ROI. Our experts design predictive monitoring platforms that scale securely, deliver actionable intelligence, and align with your operational realities.
Request a tailored quote from Intellivon, and we’ll architect a predictive healthcare monitoring app that fits your budget, meets your compliance goals, and strengthens your enterprise’s data-driven healthcare strategy.
Key Factors Affecting the Development Cost of Predictive Health Monitoring Apps
The cost of building a predictive health monitoring app isn’t determined by development hours alone. It’s shaped by strategic, technical, and regulatory decisions that define how intelligent, scalable, and compliant the system will be. While most enterprise builds fall within $50,000 to $150,000, the final figure depends on the app’s architecture, AI sophistication, data infrastructure, and long-term maintenance strategy.
Below are the key elements that influence this cost, and how each one impacts the final investment and ROI for healthcare enterprises.
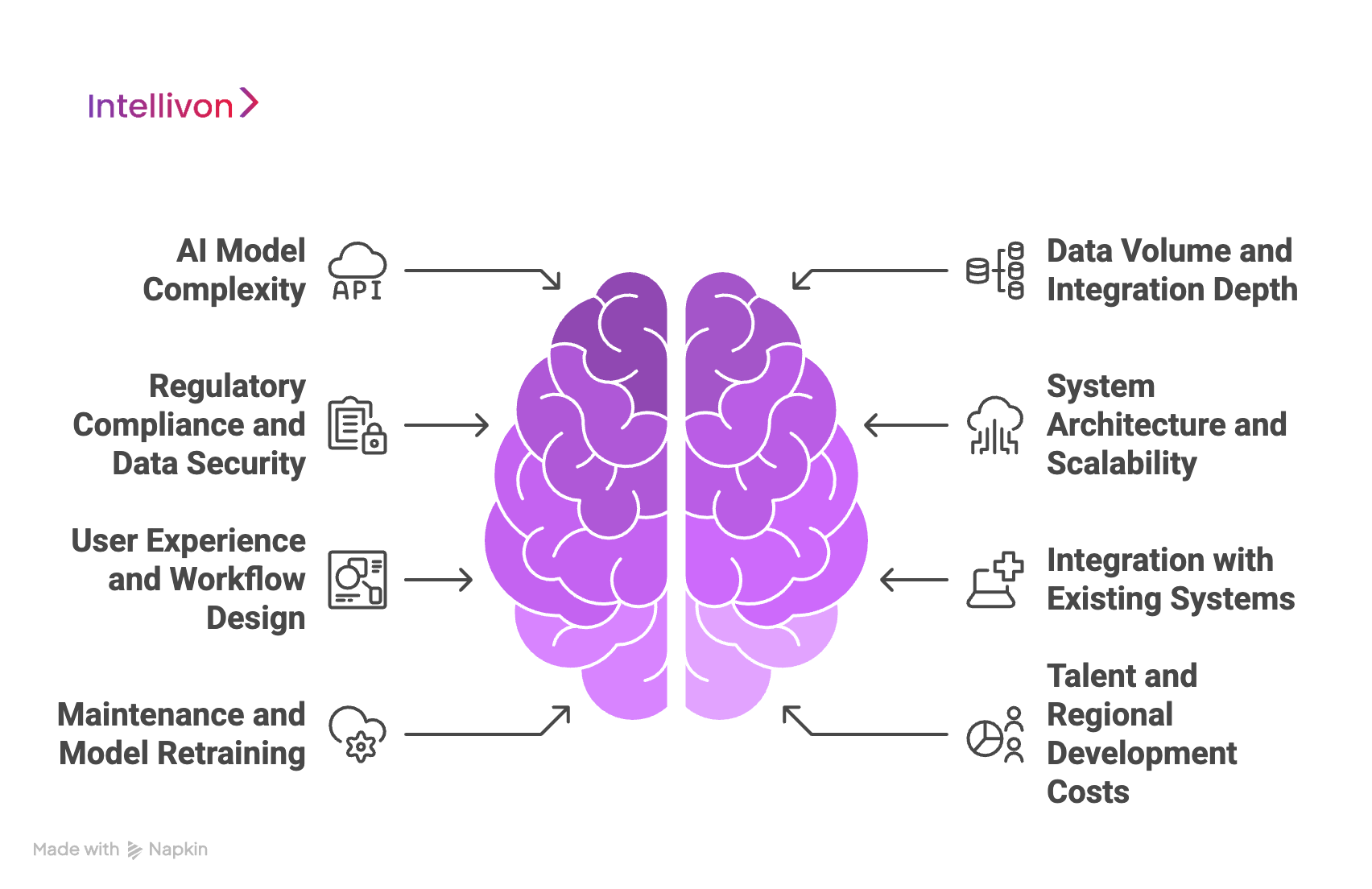
1. AI Model Complexity
The intelligence layer of the app is usually the biggest cost driver. A basic rules-based system that flags anomalies in vitals is relatively affordable, but advanced platforms use machine learning and deep learning models capable of predicting disease risks, readmissions, or sudden deterioration with high accuracy.
Training and validating these models with clinical data, domain experts, and real-world feedback loops adds significant cost but also defines the platform’s long-term value. For enterprises targeting clinical-grade accuracy and reliability, AI model development can account for up to 30–35% of total expenditure.
2. Data Volume and Integration Depth
Prediction relies on continuous and clean data. Integrating sources such as EHRs, wearables, IoT medical devices, and lab systems through interoperability frameworks like FHIR and HL7 increases both accuracy and development complexity.
Data harmonization, which includes cleaning, normalizing, and unifying different formats, adds time but ensures the system operates without blind spots. The more diverse and continuous the data streams, the more predictive the app becomes, which often justifies the additional investment.
3. Regulatory Compliance and Data Security
Healthcare operates under strict global standards like HIPAA, GDPR, and FDA digital health guidelines. Embedding compliance into the architecture, through encryption, anonymization, and audit-ready logging, is essential from day one.
While this may add up to 20–25% to the total build cost, it prevents far greater losses later from penalties, downtime, or reputational damage. Compliance is the foundation of enterprise scalability and patient trust.
4. System Architecture and Scalability
The app’s architecture determines its resilience and long-term sustainability. Cloud-native, API-first, and microservices architectures cost more initially but allow seamless scaling as user volume and data load grow.
Investing in high-availability servers, redundancy, and real-time analytics infrastructure ensures the system performs under enterprise conditions. Though this requires higher initial spend, it reduces operational costs and technical debt in the long run.
5. User Experience and Workflow Design
In predictive healthcare, usability defines adoption. Designing intuitive dashboards, visual alert systems, and mobile interfaces for both clinicians and patients demands specialized UX expertise.
This adds design and testing time but ensures engagement, which is a factor directly tied to ROI. Apps that integrate effortlessly into existing clinical workflows see faster adoption, higher satisfaction scores, and better compliance with preventive care goals.
6. Integration with Existing Systems
Hospitals, insurers, and digital health networks already operate multiple platforms, from HIS and LIS to CRM and telemedicine portals. Building custom APIs or middleware that connect predictive systems with these existing solutions adds development effort but is vital for real-world deployment.
Without seamless integration, even the best predictive model risks becoming an isolated tool rather than a unified intelligence layer across the organization.
7. Maintenance and Model Retraining
Once deployed, predictive systems require continuous optimization. AI models must be retrained regularly as new data, patient behaviors, and treatment patterns evolve.
Ongoing maintenance, including cloud monitoring, compliance audits, and performance tuning, typically costs 15–20% of the initial build annually. This ensures the platform remains accurate, secure, and adaptable to new medical insights and regulatory updates.
8. Talent and Regional Development Costs
Finally, the team behind the build plays a significant role in total expenditure. Projects involving AI engineers, clinical data scientists, and compliance architects from specialized markets cost more than generic development teams, but the difference shows in stability and outcomes.
Enterprises that prioritize expertise over low-cost outsourcing achieve higher reliability, better compliance readiness, and faster time-to-value.
Each of these factors carries its own weight, but together they shape both the cost and quality of your predictive health monitoring system. At Intellivon, we help healthcare organizations find that balance, building predictive health ecosystems that are accurate, scalable, and financially sustainable from the very first line of code.
How We Build Predictive Health Monitoring Apps
At Intellivon, we approach predictive healthcare app development as a structured collaboration between data science, clinical expertise, and enterprise engineering.
Every build is designed to deliver measurable ROI, from improving patient outcomes to optimizing operations and compliance. Here’s how we build predictive health monitoring platforms that scale with confidence.
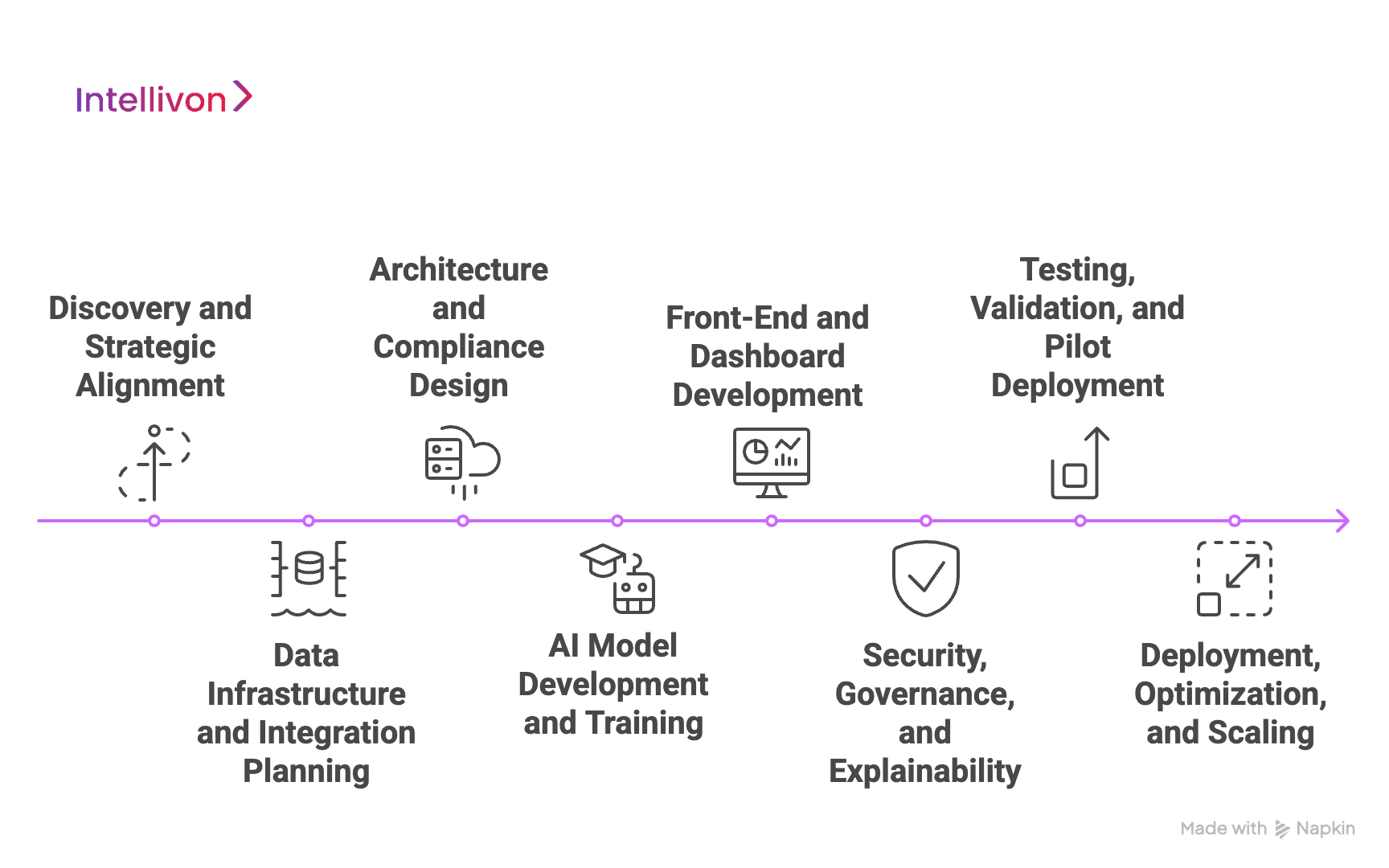
Step 1: Discovery and Strategic Alignment
We begin by understanding your enterprise objectives, which include the problems you want to solve, the outcomes you want to measure, and the compliance frameworks you must operate within.
This phase includes requirement gathering, stakeholder interviews, workflow mapping, and ROI modeling. The goal is to align predictive capabilities with real business and clinical priorities before development begins.
Step 2: Data Infrastructure and Integration Planning
Predictive accuracy depends on data consistency and accessibility. Our engineers design the data ingestion and integration blueprint, connecting wearables, IoT devices, EHRs, and hospital databases through secure APIs and healthcare data standards such as FHIR and HL7.
We ensure data is cleansed, normalized, and ready for predictive analytics, setting the stage for reliable, real-time insights.
Step 3: Architecture and Compliance Design
Next, we establish the system’s foundation, a cloud-native, API-first architecture that balances scalability, speed, and data protection.
Our architecture embeds HIPAA, GDPR, and FDA digital health compliance at every level, from data encryption to access control. This “compliance-by-design” approach prevents costly reworks later and accelerates regulatory approval.
Step 4: AI Model Development and Training
The intelligence layer defines the app’s predictive power. Our data scientists design and train machine learning and deep learning models that can detect anomalies, predict readmissions, and assess chronic condition risks.
Models are validated against historical datasets and real-world clinical feedback to ensure accuracy, fairness, and explainability, which are all critical for enterprise trust and compliance.
Step 5: Front-End and Dashboard Development
Data is only valuable when it’s understandable. We build intuitive clinician dashboards and patient engagement interfaces that transform AI predictions into actionable insights.
This includes real-time alert panels, visual health trends, and personalized health scores, all designed for ease of use across mobile, tablet, and enterprise dashboards.
Step 6: Security, Governance, and Explainability
Predictive healthcare requires more than AI accuracy it demands accountability. We integrate explainable AI (XAI) frameworks so every prediction can be traced and justified.
Governance modules monitor model performance, bias, and drift, while encryption and continuous monitoring keep all patient data secure and auditable under HIPAA and GDPR mandates.
Step 7: Testing, Validation, and Pilot Deployment
Before full rollout, we conduct extensive functional, security, and compliance testing. Our QA teams simulate real-world clinical workflows to validate prediction accuracy and alert timing.
A controlled pilot deployment allows your teams to test usability and refine feedback loops, ensuring a stable, adoption-ready system before enterprise scaling.
Step 8: Deployment, Optimization, and Scaling
Once validated, the platform moves into production. We deploy it on a secure, scalable cloud environment with regional hosting, uptime monitoring, and disaster recovery capabilities.
Post-launch, Intellivon provides ongoing support for model retraining, system optimization, and user training, ensuring the platform continues to learn and deliver value as your data grows.
Our process combines strategic foresight with technical precision, helping healthcare enterprises build predictive systems that not only forecast risk but also prevent crises before they occur.
From architecture to AI ethics, every decision balances innovation with compliance and intelligence with trust.
Overcoming Challenges To Building A Predictive Health Monitoring App
Building a predictive health monitoring app lies in engineering trust, accuracy, and compliance at scale. Enterprises face several hurdles along the way, but each can be overcome with the right strategy, architecture, and partner.
1. Fragmented Data Ecosystems
Healthcare data often lives in silos, across EHRs, wearables, and legacy hospital systems , making integration complex. Without unified data pipelines, predictive accuracy weakens.
We use FHIR and HL7-based integration frameworks to consolidate fragmented data streams securely, creating a single source of truth that powers accurate AI insights.
2. Limited Data Quality and Bias
Low-quality or biased datasets can lead to misleading predictions and compliance risks. Noise, duplication, and missing records are common barriers in healthcare data.
Our experts implement data cleansing, deduplication, and bias-detection pipelines that prepare datasets for reliable model training, ensuring fairness, clinical relevance, and trust in predictions.
3. Regulatory Complexity
Navigating compliance across HIPAA, GDPR, and FDA digital health regulations can slow development timelines and inflate costs if handled late in the process.
We embed compliance from day one. We build with security-first architectures, audit-ready encryption, and automated consent management, ensuring regulatory readiness while maintaining agility.
4. AI Model Interpretability
In healthcare, predictions without explanations erode clinician trust. AI “black boxes” can trigger resistance and regulatory pushback.
Intellivon integrates Explainable AI (XAI) frameworks that show exactly how and why predictions are made, thereby strengthening transparency, facilitating FDA and EU AI Act alignment, and boosting clinical adoption.
5. Integration with Legacy Systems
Many healthcare enterprises still rely on outdated infrastructure that doesn’t easily connect with new predictive systems.
Our engineers design API-first, modular architectures that enable interoperability with existing hospital information systems and cloud infrastructures, ensuring seamless modernization without disruption.
6. Ensuring Continuous Model Accuracy
Predictive models degrade over time if not retrained on fresh data. Outdated models can lead to missed alerts or false positives.
We deploy continuous learning pipelines that retrain models automatically using new clinical data, preserving performance, reliability, and long-term ROI for enterprise clients.
7. Scaling Securely
As predictive platforms expand, maintaining security across multiple endpoints becomes a major concern. Breaches can result in regulatory penalties and reputational loss.
Intellivon’s DevSecOps and zero-trust architecture ensure that every user, API, and dataset is continuously verified and protected, enabling enterprises to scale safely across geographies and networks.
8. Driving Adoption
Even the most advanced predictive platform fails if end users don’t adopt it. Resistance often stems from workflow disruption or lack of training.
We prioritize UX co-design and onboarding programs that fit seamlessly into clinician routines while educating patients on how to interpret predictive insights, turning technology into collaboration.
Each of these challenges represents an opportunity for innovation when addressed strategically. At Intellivon, we help healthcare enterprises move beyond obstacles to build predictive ecosystems that are secure, transparent, and clinically trusted, transforming risk into resilience and data into foresight.
Conclusion
Predictive health monitoring represents the next leap in preventive medicine, transforming care from reactive treatment to proactive intervention. As data grows more complex and regulations tighten, enterprises can no longer afford fragmented, manual systems.
They need a solution provider capable of aligning AI innovation with compliance, scalability, and clinical trust. With the right partner, predictive health platforms can go beyond monitoring to anticipate risks, personalize care, and optimize resources. The future of healthcare belongs to those who act early, invest wisely, and turn prediction into measurable, long-term value.
Build a Predictive Health Monitoring App With Intellivon
At Intellivon, we design predictive health monitoring platforms that combine AI intelligence, clinical compliance, and enterprise scalability.
Our systems empower healthcare organizations to detect early risks, improve patient outcomes, and optimize resource allocation, all while integrating seamlessly with existing EHR, IoT, and hospital infrastructures.
Every build is engineered to meet global regulatory, operational, and security standards, enabling enterprises to deliver measurable ROI from day one.
Why Partner With Intellivon?
- Compliance-First Architecture: Every solution is built in alignment with HIPAA, GDPR, FDA SaMD, and EU AI Act frameworks — ensuring data integrity, patient trust, and audit-readiness across regions.
- AI-Powered Prediction Engine: Our predictive models leverage continuous learning and explainable AI to anticipate deterioration risks, reduce readmissions, and enable real-time intervention with clinical-grade accuracy.
- Seamless Interoperability: Designed for enterprise ecosystems, our platforms integrate effortlessly with EHRs, wearables, and IoT sensors through FHIR and HL7, ensuring uninterrupted data flow without disrupting workflows.
- Scalable Cloud-Native Infrastructure: Elastic deployment models support multi-hospital scalability, real-time monitoring, and 24/7 uptime — all optimized for performance, compliance, and cost efficiency.
- Continuous Model Optimization: Integrated MLOps pipelines enable drift detection, retraining, and performance monitoring, keeping predictive accuracy consistent as health data evolves.
- Zero-Trust Security Framework: Advanced encryption, identity management, and continuous threat detection safeguard sensitive data while maintaining accessibility for authorized users.
- Human-Centered Design: Our clinician dashboards and patient engagement interfaces transform AI predictions into clear, actionable insights — improving adoption, satisfaction, and clinical outcomes.
- Proven Healthcare Expertise: With years of experience delivering large-scale healthcare AI systems, we bring validated frameworks, compliance maturity, and measurable success metrics to every project.
Book a strategy call with Intellivon today to explore how a predictive health monitoring platform tailored to your enterprise can transform care delivery, reduce costs, and prepare your organization for the next decade of AI-driven preventive healthcare.
FAQs
Q1. How much does it cost to build a predictive health monitoring app for hospitals or healthcare enterprises?
A1. The cost typically ranges from $50,000 to $150,000, depending on features, data integration depth, AI model complexity, and compliance requirements. Enterprise-grade builds that include explainable AI, real-time alerts, and HIPAA/GDPR alignment are on the higher end but deliver significantly better ROI and scalability.
Q2. What key technologies are used in predictive health monitoring app development?
A2. These apps combine AI, machine learning, IoT, cloud computing, and data analytics to collect and analyze real-time health data. Common integrations include FHIR/HL7 APIs, wearable device sensors, and cloud-native microservices for scalability and interoperability across hospital systems.
Q3. How do predictive health monitoring apps ensure patient data security and compliance?
A3. Security and compliance are achieved through end-to-end encryption, anonymization, multi-factor authentication, and audit-ready logging. Most enterprise builds follow HIPAA, GDPR, and FDA digital health frameworks to protect sensitive patient data and ensure regulatory approval during deployment.
Q4. How long does it take to build a predictive health monitoring platform from scratch?
A4. Development timelines vary between 4 to 10 months, depending on project scope and enterprise integration needs. A basic MVP can be built within 3–4 months, while a full-scale system with AI explainability, multi-hospital integration, and compliance automation takes longer but delivers lasting operational value.
Q5. What ROI can healthcare enterprises expect from predictive health monitoring systems?
A5. Predictive platforms help reduce hospital readmissions by up to 25–30%, improve treatment adherence by 50%, and lower operational overhead through smarter resource allocation. Enterprises typically recover their investment within the first year through improved outcomes, reduced penalties, and higher patient retention.





