Telehealth is now firmly embedded within enterprise hospital operations. But as scale increases, telehealth is judged on governance, accountability, and operational resilience, instead of capacity.
Scaling telehealth introduces an entirely different class of challenges than launching it, such as workflow bottlenecks and integration debt. At the same time, governance gaps appear as virtual care expands across specialties, facilities, and regulatory boundaries. At scale, telehealth systems fail through clinician overload and growing compliance risk.
This is where infrastructure design becomes decisive. With over a decade of experience building enterprise-grade healthcare platforms, Intellivon works with hospital systems to engineer telehealth as a governed operating layer rather than a collection of tools. This blog draws on this experience and breaks down how we scale telehealth infrastructure for enterprise hospital systems while keeping them intact and compliant throughout.
The Right Time To Get Your Telehealth Infrastructure Scaled
The global telehealth market was valued at USD 196.81 billion in 2025 and is expected to grow to USD 244.30 billion in 2026, reaching nearly USD 1,367.36 billion by 2035 at a CAGR of 23.19%. As a result, telehealth is no longer an experimental delivery channel. It is becoming a core operating layer for healthcare systems, payers, and employers.
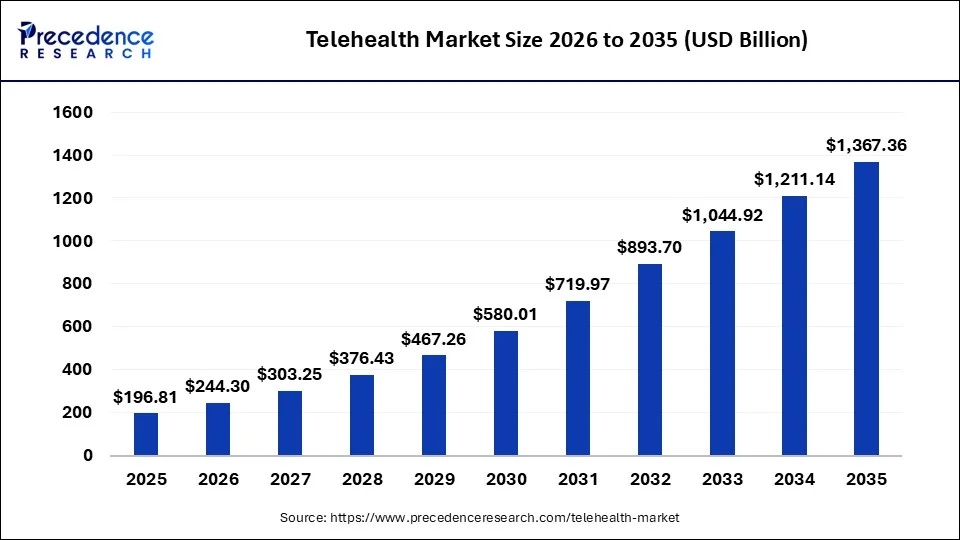
Key Growth Drivers:
- Chronic diseases and aging populations now require continuous remote oversight rather than episodic, in-person care.
- Widespread smartphone use, affordable broadband, and wearables enable always-on data capture and mobile-first care delivery.
- Patients increasingly demand convenient, flexible care that reduces time and cost burdens, especially among digital-native groups.
- Proven improvements in access, continuity, and outcomes have made telehealth a mainstream healthcare delivery model.
- Beyond market expansion, the strongest case for telehealth investment comes from measurable operational and clinical returns.
Telehealth delivers clear operational and clinical ROI when embedded into care workflows. Lower no-show rates improve revenue capture and clinician utilisation, especially in high-volume outpatient settings. A 2025 study of publicly insured type 2 diabetes patients reported a 71.4% reduction in missed appointments with comparable clinical outcomes. Virtual transition-of-care programs further reduce post-discharge gaps, with one large health system reporting 30-day readmissions of 14.9% versus a 20.1% benchmark and follow-up no-shows below 5%. Across telemedicine programs, readmissions typically decline by 1–5 percentage points, depending on care design and patient population.
Investing in telehealth apps right now makes commercial sense because adoption is accelerating while monetisation models are maturing. These improvements protect margins under value-based contracts, reduce penalties, and create repeatable, enterprise-scale profitability.
What Breaks When Telehealth Scales In Large Hospital Systems
When telehealth scales in large hospital systems, hidden weaknesses surface in workflows, infrastructure, governance, and accountability, long before systems visibly fail.
Below are the most common areas where large hospital systems experience friction.
1. Fragmented Clinical Workflows
As telehealth expands, clinical workflows often diverge across departments. Each specialty adapts virtual care to its own needs, using different intake methods, triage rules, and follow-up processes. Over time, these variations create inconsistency in care delivery and accountability.
Patients experience uneven journeys, while clinicians struggle with unclear handoffs. In addition, care teams spend more time coordinating work across systems. This increases cognitive load and contributes directly to burnout.
2. Infrastructure That Cannot Absorb Peak Demand
Pilot-ready infrastructure rarely anticipates sustained concurrency. As usage grows, video, messaging, documentation, and integrations compete for shared resources. Performance issues appear gradually rather than as full-outages.
Join times increase, calls drop intermittently, and documentation updates lag behind encounters. These issues compound during peak periods such as flu season or post-discharge surges. Over time, trust in the platform erodes among clinicians and staff.
3. EHR And System Integration Bottlenecks
Telehealth relies heavily on seamless integration with enterprise systems. Scheduling, documentation, orders, billing, and analytics must remain synchronized across workflows. At scale, tightly coupled integrations become a limiting factor.
Synchronous data writes slow down encounters and introduce latency. Manual workarounds emerge to keep care moving. As a result, clinicians switch between systems mid-visit, increasing error risk and operational friction.
4. Governance And Accountability Gaps
Scaling telehealth multiplies decision paths across the organization. Without formal governance, ownership becomes unclear when issues arise. Questions surface around triage rules, escalation thresholds, and access approvals. Inconsistent decision-making slows response times and increases risk exposure.
Over time, informal governance gives way to reactive fixes. These gaps often surface during audits or operational incidents rather than through proactive planning.
5. Security And Compliance Exposure
Each new telehealth endpoint expands the security perimeter. Patient devices, clinician tools, APIs, and third-party services increase complexity. When identity and access controls are fragmented, visibility suffers. Audit logs become incomplete or inconsistent across systems.
Privacy incidents take longer to investigate and remediate. This exposure grows quickly as telehealth spans regions with different regulatory requirements.
6. Operational Cost Creep
Telehealth costs tend to rise quietly as programs scale. Multiple vendors, overlapping licenses, and duplicated infrastructure accumulate over time. Without consolidated visibility, utilization remains unclear.
Some systems are overprovisioned, while others become bottlenecks. Finance teams see rising spend without a clear connection to outcomes. This weakens confidence in telehealth as a sustainable investment.
Telehealth falters when growth outpaces foundational design. Addressing these issues requires treating telehealth as shared infrastructure, and not isolated tools. The next phase of maturity begins with architectural and operational intent.
Core Infrastructure Layers Required For Scalable Telehealth
Scalable telehealth depends on a layered infrastructure that separates communication, clinical systems, data, identity, and devices, allowing hospitals to grow without operational or compliance breakdowns.
Each layer below plays a distinct role in supporting scale.
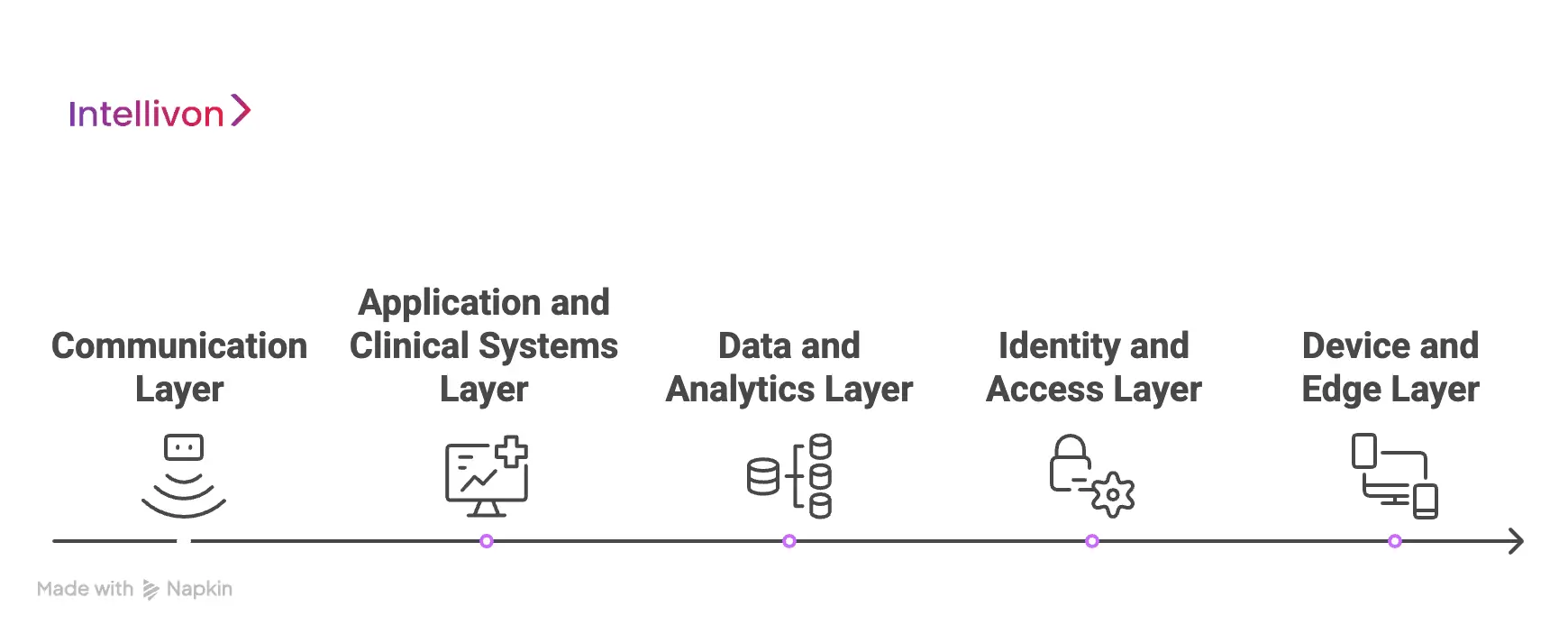
1. Communication Layer
The communication layer enables how patients and clinicians interact during virtual care. It includes video visits, voice calls, secure messaging, and asynchronous exchanges such as images or documents. At enterprise scale, this layer must support high concurrency without degrading quality during peak demand.
Reliability becomes more important than novelty, especially when care spans multiple specialties and facilities. Separating communication services from clinical systems allows hospitals to scale capacity without interrupting care delivery.
2. Application And Clinical Systems Layer
This layer governs how care is delivered, recorded, and reimbursed across the organization. It includes telehealth applications, EHR systems, care coordination tools, imaging platforms, and billing workflows. When these systems are tightly coupled, scaling introduces latency and operational friction.
Event-driven and asynchronous integration patterns reduce bottlenecks while preserving clinical continuity. This design allows care teams to work efficiently even as volumes increase.
3. Data And Analytics Layer
Telehealth produces large volumes of clinical, operational, and media data. Visit records, clinical notes, recordings, and device data must remain accessible without slowing live workflows.
A dedicated data and analytics layer supports reporting, quality monitoring, and financial analysis independently of care delivery systems. In addition, it enables advanced analytics and AI use cases as programs mature. Strong governance at this layer ensures consistency across departments and regions.
4. Identity And Access Layer
As telehealth expands, managing access becomes increasingly complex. Patients, clinicians, administrators, and partners all require different permissions based on role and context. A centralized identity and access layer enforces role-based controls consistently across systems.
It also ensures that access decisions are auditable and aligned with clinical accountability. Without this layer, security and compliance risks grow quietly as scale increases.
5. Device And Edge Layer
Telehealth interactions increasingly occur outside traditional hospital environments. Patient smartphones, clinician laptops, diagnostic peripherals, and remote monitoring devices all connect to the platform.
This layer must handle variability in networks, hardware, and user behavior without compromising security or experience. Edge processing helps reduce latency and manage bandwidth efficiently. Treating devices as a first-class infrastructure concern prevents fragility as adoption grows.
Scalable telehealth depends less on individual tools and more on how systems are structured. Designing telehealth as a layered infrastructure creates a foundation that can support long-term enterprise care delivery.
Architecture Required To Scale Telehealth Infrastructure
Enterprise telehealth scales reliably when architecture separates concerns across layers, allowing hospitals to expand volume, services, and regions without destabilizing care delivery.
The sections below outline the architectural layers required to support enterprise-scale telehealth.
1. Cloud And Compute Layer
This layer provides the elastic foundation that allows telehealth systems to scale with demand. It handles compute capacity for video processing, application services, integrations, and analytics workloads.
At scale, this layer must support rapid scaling during peak usage while maintaining predictable performance. A hybrid or multi-region setup also ensures resilience during localized failures.
Typical technologies at this layer include:
- Public cloud platforms (AWS, Azure, GCP)
- Virtual machines and autoscaling groups
- Container runtimes and managed Kubernetes services
- Multi-region deployment and failover configurations
2. Application And Service Layer
The application layer is where telehealth functionality is delivered to users.It includes services for scheduling, video sessions, messaging, clinical documentation, and care coordination.
At enterprise scale, these services must scale independently to avoid system-wide slowdowns. Breaking functionality into modular services also simplifies updates and feature expansion.
Typical technologies at this layer include:
- Microservices architectures
- Container orchestration platforms
- Backend frameworks for clinical and operational services
- Service meshes for traffic management and observability
3. Integration And API Layer
Telehealth does not operate in isolation within hospitals. This layer manages how telehealth services exchange data with EHRs, labs, imaging, billing, and external partners. At scale, synchronous integrations create latency and operational risk.
Event-driven and API-first designs reduce coupling and improve system resilience.
Typical technologies at this layer include:
- API gateways and management platforms
- HL7, FHIR, and DICOM interfaces
- Event streaming platforms
- Message queues and asynchronous processing services
4. Data And Storage Layer
Telehealth generates large volumes of clinical and operational data. This layer stores visit records, clinical notes, media files, audit logs, and analytics datasets.
It must support long-term retention, fast retrieval, and compliance with data residency requirements. Separating transactional and analytical storage prevents reporting workloads from impacting live care.
Typical technologies at this layer include:
- Relational and NoSQL databases
- Object storage for media and large files
- Data warehouses and lake architectures
- Backup, archival, and retention management systems
5. Identity, Security, And Governance Layer
As telehealth scales, controlling access becomes critical. This layer governs authentication, authorization, auditability, and policy enforcement across all systems.
Centralized identity ensures consistent access rules regardless of location or service. Governance mechanisms at this layer reduce compliance risk and support regulatory audits.
Typical technologies at this layer include:
- Identity and access management platforms
- Role-based and attribute-based access controls
- Encryption and key management services
- Centralized logging and audit trail systems
6. Device And Edge Layer
Telehealth interactions increasingly happen outside hospital walls. This layer manages patient devices, clinician endpoints, and connected diagnostic tools. It must handle network variability, device diversity, and intermittent connectivity without compromising security.
Edge processing helps reduce latency and improve reliability for distributed users.
Typical technologies at this layer include:
- Mobile and web client applications
- Device management and endpoint security tools
- Edge computing and caching services
- Secure connectivity protocols and SDKs
Enterprise telehealth succeeds when architecture anticipates growth rather than reacting to it. Layered designs allow hospitals to scale volume, add services, and expand regions without repeated rework. Each layer creates clear ownership and limits the blast radius of change.
Ensuring Security and Compliance While Scaling Telehealth
Telehealth can only scale safely when security and compliance are embedded into platform design, enforcing access, accountability, and auditability across every virtual care interaction.
The following areas demand focused attention as scale increases.
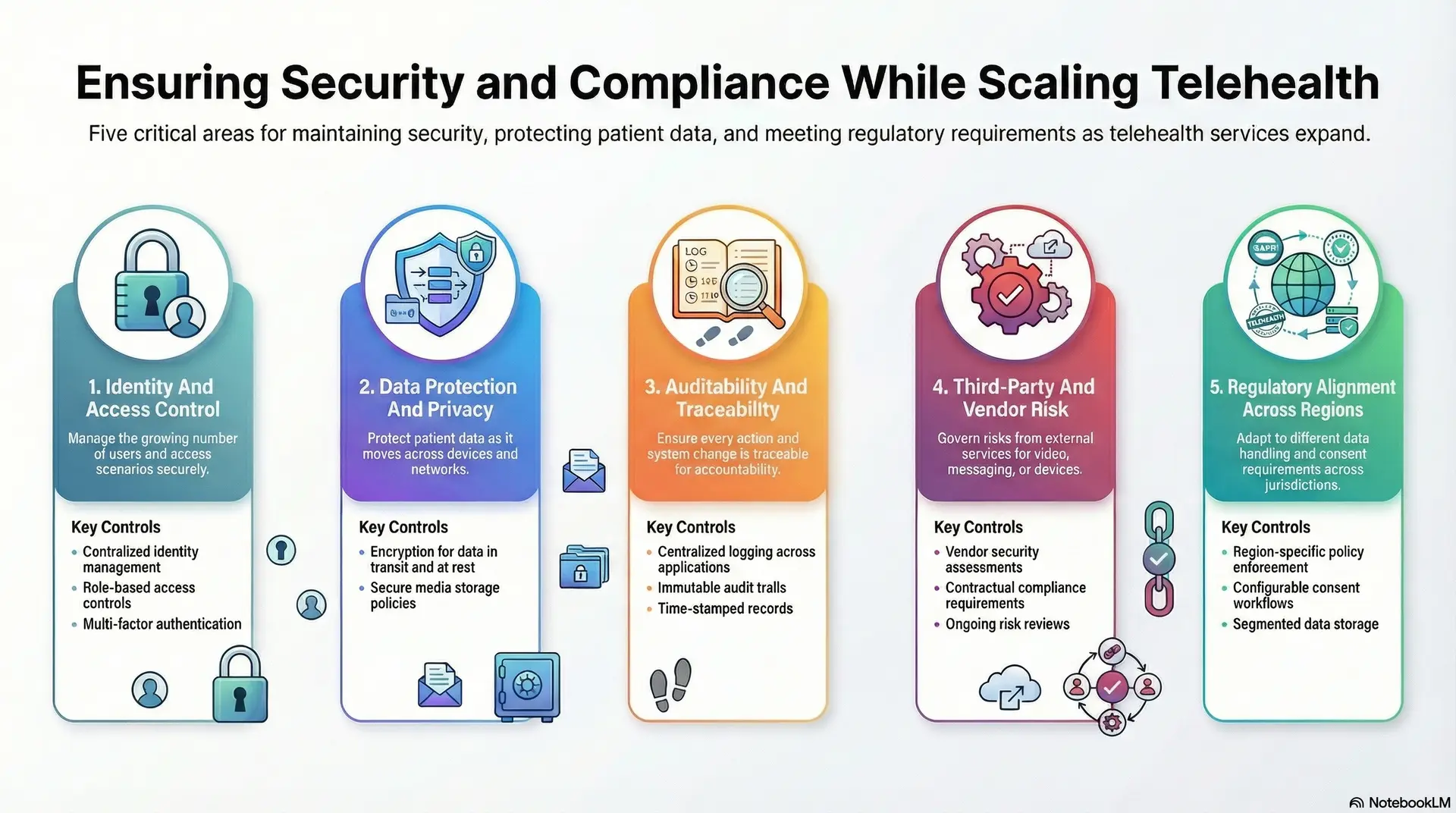
1. Identity And Access Control
Scaling telehealth multiplies the number of users and access scenarios. Patients, clinicians, administrators, and external partners all interact with systems differently and at different times. Without centralized identity controls, access decisions become inconsistent and difficult to audit.
Strong role-based and context-aware access models ensure that users only see what they are authorized to see. This clarity protects patient data while supporting clinical efficiency.
Key controls at this layer include:
- Centralized identity and access management platforms
- Role-based and attribute-based access controls
- Multi-factor authentication for privileged users
- Context-aware session management
2. Data Protection And Privacy
Telehealth data moves continuously across systems, devices, and networks. Clinical notes, video streams, messages, and device data must remain protected throughout their lifecycle. As scale increases, manual controls no longer suffice.
Encryption, data segmentation, and clear retention policies become essential. These safeguards ensure privacy requirements are met without slowing care delivery.
Key controls at this layer include:
- Encryption for data in transit and at rest
- Tokenization or masking for sensitive fields
- Data residency and retention enforcement
- Secure media storage and access policies
3. Auditability And Traceability
Enterprise telehealth environments must provide clear accountability. Every clinical action, access event, and system change should be traceable. Without consistent audit trails, investigations become slow and incomplete.
At scale, this creates regulatory and legal exposure. Centralized logging and immutable records provide the visibility required for audits and internal reviews.
Key controls at this layer include:
- Centralized logging across applications and services
- Immutable audit trails for clinical and administrative actions
- Time-stamped access and change records
- Integration with enterprise monitoring tools
4. Third-Party And Vendor Risk
Telehealth platforms often rely on external services for video, messaging, analytics, or devices. As usage grows, third-party dependencies increase exposure. Without governance, vendor risks accumulate quietly.
Clear standards for onboarding, monitoring, and reviewing partners help contain this risk. Regular assessments ensure external services meet hospital security and compliance expectations.
Key controls at this layer include:
- Vendor security assessments and onboarding standards
- Contractual compliance and data handling requirements
- Ongoing risk reviews and performance monitoring
- Controlled integration and access scopes
5. Regulatory Alignment Across Regions
Large hospital systems often operate across multiple jurisdictions. Each region may impose different requirements around data handling, consent, and reporting. Scaling telehealth without accounting for these differences creates compliance gaps.
Configurable policies and region-aware controls allow hospitals to adapt without duplicating platforms. This flexibility supports growth while maintaining regulatory alignment.
Key controls at this layer include:
- Region-specific policy enforcement
- Configurable consent and data handling workflows
- Segmented data storage by jurisdiction
- Centralized compliance reporting
Security and compliance create the trust required for virtual care to operate at enterprise scale. By embedding controls into identity, data, and governance layers, hospitals reduce risk without adding friction.
EHR and Workflow Integration Of Telehealth Infrastructure
Telehealth scales effectively only when it is deeply integrated into EHRs and clinical workflows, ensuring continuity of care, operational efficiency, and financial accuracy across the enterprise.
The following integration areas determine whether telehealth strengthens or fragments enterprise operations.
1. Scheduling And Access Workflows
Scheduling is often the first point of failure when telehealth scales. If virtual visits are booked outside the EHR, duplicate records and mismatched availability appear quickly. Integrated scheduling ensures patients, clinicians, and care teams operate from a single source of truth.
It also supports specialty-specific rules, eligibility checks, and capacity planning. As a result, access improves without increasing administrative burden.
Integration elements at this layer include:
- EHR-native scheduling and availability management
- Virtual visit types aligned to service lines
- Eligibility and referral checks
- Capacity and load balancing logic
2. Clinical Documentation And Orders
Documentation must remain continuous across virtual and in-person care when telehealth notes live outside the EHR, clinical context fragments. Integrated documentation ensures visit notes, orders, and clinical decisions are captured where clinicians already work.
This reduces re-entry, improves accuracy, and supports downstream care. Over time, it also strengthens longitudinal patient records.
Integration elements at this layer include:
- Real-time or asynchronous note write-back
- Order entry and result reconciliation
- Clinical templates for virtual care
- Structured data capture for analytics
3. Care Coordination And Follow-Ups
Telehealth often extends beyond a single encounter. Follow-ups, referrals, diagnostics, and medication changes must flow into existing care coordination workflows. Without integration, tasks are missed or delayed.
Embedded workflows ensure virtual visits trigger the same downstream actions as in-person care. This consistency improves outcomes and operational reliability.
Integration elements at this layer include:
- Task and referral generation
- Follow-up scheduling and reminders
- Care team notifications
- Integration with care management tools
4. Billing, Coding, And Revenue Workflows
Revenue leakage becomes visible when telehealth scales. Disconnected billing workflows lead to missed charges, incorrect codes, and delayed reimbursement. Integrated billing ensures virtual encounters follow the same revenue cycle processes as other care modalities.
It also supports payer-specific rules and reporting. This alignment protects financial performance as volume grows.
Integration elements at this layer include:
- Automated charge capture
- Telehealth-specific coding support
- Claims submission and reconciliation
- Financial reporting and audit trails
5. Workflow Orchestration Across Systems
Enterprise telehealth spans multiple systems and teams. Orchestration ensures these systems work together without manual coordination. Rules-based workflows route cases based on urgency, specialty, and availability.
Asynchronous processing prevents bottlenecks during peak demand. This orchestration layer keeps care moving smoothly as complexity increases.
Integration elements at this layer include:
- Workflow engines and rules management
- Event-driven triggers and notifications
- Escalation and exception handling
- Cross-system state management
Telehealth integration succeeds when it feels invisible to clinicians. Deep EHR and workflow integration preserves continuity, reduces friction, and supports scale. It also ensures virtual care strengthens enterprise operations instead of creating parallel processes.
AI, Analytics, And IoMT As Telehealth Scale Multipliers
As telehealth programs grow, manual coordination becomes a limiting factor. Volume increases faster than teams can triage, route, and follow up on care requests. AI, analytics, and IoMT do not replace clinical judgment, but they remove friction from decision-heavy workflows.
When applied thoughtfully, these capabilities allow hospitals to scale virtual care without proportionally scaling staff or cost. The value lies in how these tools are embedded into existing workflows.
1. AI-Driven Triage And Routing
AI supports early decision-making when demand exceeds immediate clinical capacity.
By analyzing intake data, symptoms, history, and risk signals, AI models help prioritize cases and route them appropriately.
This reduces unnecessary synchronous visits and ensures urgent cases reach clinicians faster. Over time, routing accuracy improves clinician utilization and patient outcomes. The result is a more balanced workload across service lines.
Common capabilities at this layer include:
- Symptom-based triage models
- Risk scoring and prioritization
- Rules-assisted visit routing
- Capacity-aware clinician assignment
2. Clinician Load Optimization
As telehealth scales, uneven workloads create burnout and inefficiency. AI can identify patterns in demand, visit duration, and follow-up requirements. These insights help distribute work more evenly across teams and shifts.
Optimization improves coverage during peak periods without extending hours. This creates a more sustainable operating model for virtual care.
Common capabilities at this layer include:
- Demand forecasting models
- Visit duration prediction
- Shift and capacity optimization
- Workload balancing across teams
3. Analytics For Utilization And Outcomes
Scaling telehealth without visibility leads to blind growth. Analytics provide insight into how virtual care is actually used across departments and populations. Leaders can track utilization trends, clinical outcomes, and access gaps.
These insights guide service line expansion and operational adjustments. Over time, analytics support evidence-based decisions instead of assumptions.
Common capabilities at this layer include:
- Telehealth utilization dashboards
- Outcome and quality metrics
- No-show and drop-off analysis
- Service line performance tracking
4. ROI And Financial Performance Tracking
Financial impact becomes harder to measure as programs grow. Analytics link telehealth activity to revenue, cost avoidance, and efficiency gains.
This includes tracking reduced no-shows, optimizing staffing, and avoiding readmissions. Clear ROI signals build confidence among stakeholders. They also inform investment decisions as programs expand.
Common capabilities at this layer include:
- Revenue and reimbursement tracking
- Cost utilization analysis
- Productivity and efficiency metrics
- Longitudinal ROI reporting
5. IoMT And RPM Integration
IoMT and remote monitoring extend telehealth beyond episodic visits. Connected devices generate continuous data that informs clinical decisions between encounters.
At scale, secure ingestion and processing become critical. Edge processing reduces bandwidth strain and supports timely alerts. When integrated well, IoMT strengthens chronic and post-acute care models.
Common capabilities at this layer include:
- Secure device integration frameworks
- Edge data processing and filtering
- Alerting and escalation workflows
- Integration with care management systems
AI, analytics, and IoMT amplify telehealth only when embedded into workflows. When aligned with enterprise operations, they become force multipliers for scale. This intelligence layer allows hospitals to grow telehealth programs responsibly and sustainably.
How We Scale Telehealth Infrastructure for Enterprise Hospitals
Scaling telehealth in enterprise hospitals needs more than technical upgrades. It requires a repeatable process that aligns clinical workflows, platform architecture, governance, and measurable business outcomes.
Our teams approach this as an infrastructure program, not a feature rollout. That structure helps hospital systems expand virtual care without creating fragmentation or hidden risk.
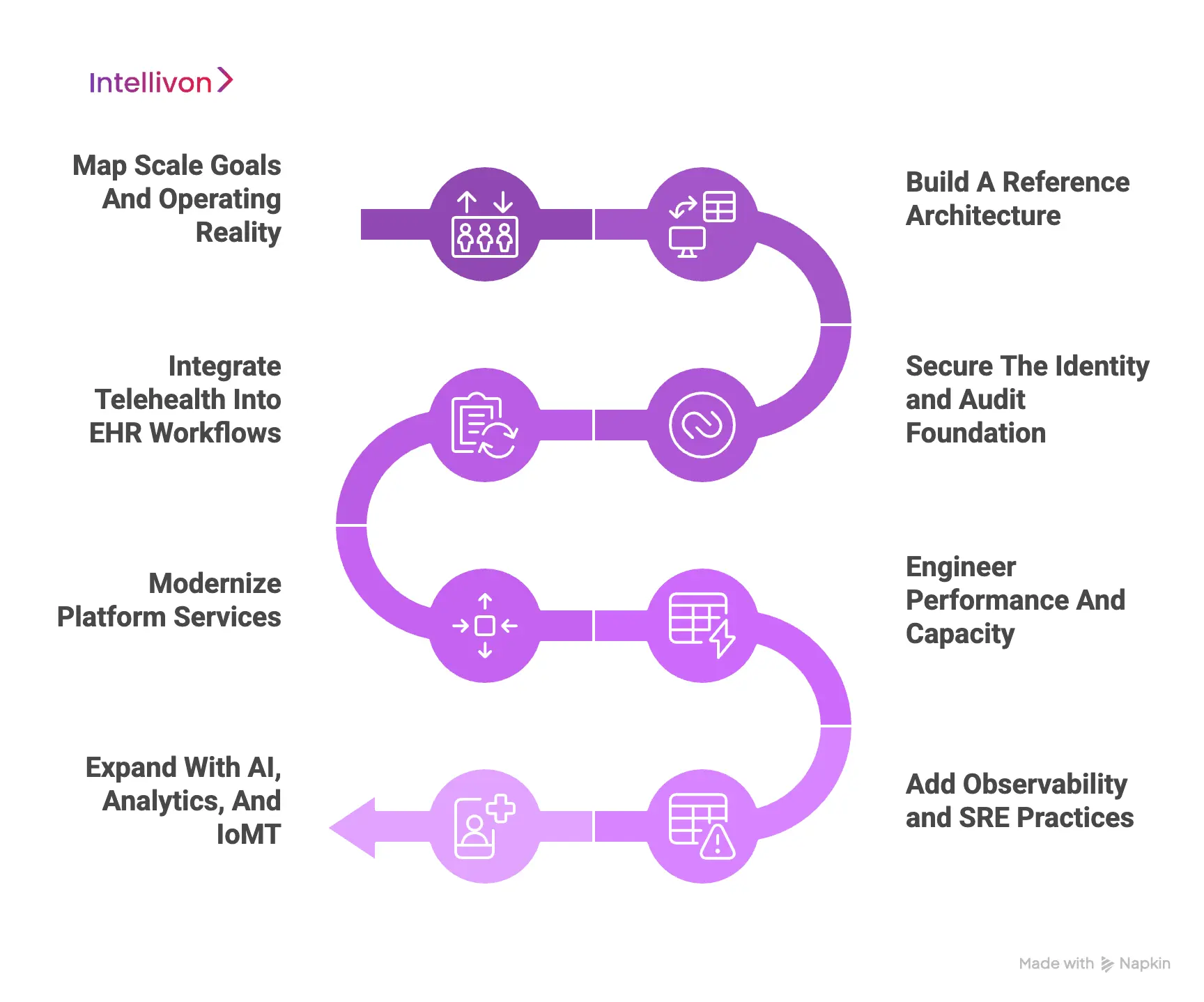
Step 1: Map Scale Goals And Operating Reality
We start by clarifying what “scale” means in your system. Volume growth, new specialties, multi-site rollout, and regional expansion create different constraints. We also identify where telehealth currently breaks, such as bottlenecks in scheduling, documentation, or triage.
This step creates a grounded scope that leadership can sponsor and teams can execute.
What we deliver:
- Scale targets by service line and facility
- Current-state workflow and systems map
- Risk and constraint register
- 90-day priority roadmap
Step 2: Build A Reference Architecture
Next, we define the target architecture that fits your environment. This includes how services are layered, how data flows, and where governance is enforced.
In addition, we align ownership across IT, clinical operations, security, and finance so decisions do not stall. This prevents architecture drift as more departments come online.
What we deliver:
- Layered telehealth reference architecture
- Service boundaries and integration patterns
- Ownership and decision framework
- Standards for future expansion
Step 3: Secure The Identity and Audit Foundation
Before scaling usage, we harden access and accountability. We standardize authentication, role-based access, and audit logging across every telehealth interaction.
This reduces compliance exposure as the user base expands. It also speeds investigations because logs remain consistent across systems.
What we deliver:
- Centralized IAM and role models
- MFA and privileged access controls
- Audit trail and log governance
- Compliance-ready access reporting
Step 4: Integrate Telehealth Into EHR Workflows
We then remove “telehealth as a parallel system” behaviors. Scheduling, documentation, orders, billing, and follow-ups must function within the same clinical workflow.
Therefore, we prioritize EHR integration points that reduce manual work and prevent data gaps. This step improves clinician adoption because the workflow feels familiar.
What we deliver:
- EHR scheduling and visit type alignment
- Documentation and order write-back
- Referral and follow-up workflows
- Billing and coding integration support
Step 5: Modernize Platform Services
With workflows connected, we address platform scalability. We separate critical services so video, scheduling, messaging, and integrations can scale independently.
This limits the blast radius of change and reduces performance drift. It also allows upgrades without disrupting care delivery.
What we deliver:
- Modular service design and scaling plan
- Container and orchestration strategy
- API and event-driven integration plan
- Deployment and release framework
Step 6: Engineer Performance And Capacity
Scaling fails when peak demand creates slowdowns that teams cannot explain. We baseline performance, run load tests, and model capacity for surge events.
In addition, we tune network, database, and media workflows to reduce latency and drop rates. This builds operational confidence before large rollouts.
What we deliver:
- Load testing and performance baselines
- Peak demand and surge capacity models
- Autoscaling and traffic management rules
- Latency and reliability optimization plan
Step 7: Add Observability and SRE Practices
Once the scale begins, visibility becomes as important as capability. We implement monitoring for system health and real user experience, such as join times and drop rates. We also establish incident response playbooks and escalation models across teams.
This reduces downtime impact and strengthens continuous improvement.
What we deliver:
- Telehealth observability dashboards
- Distributed tracing and log correlation
- Incident playbooks and escalation paths
- Post-incident review and improvement loop
Step 8: Expand With AI, Analytics, And IoMT In A Controlled Way
Finally, we add intelligent scale multipliers where they produce a measurable impact. AI supports triage, routing, and clinician load balancing without altering clinical accountability.
Analytics link utilization to outcomes and ROI signals that leadership can trust. IoMT and RPM integrations are introduced with secure ingestion and edge considerations to avoid bandwidth and alert fatigue.
What we deliver:
- AI-assisted triage and routing strategy
- Utilization, outcomes, and ROI analytics
- IoMT and RPM integration architecture
- Continuous optimization roadmap
Enterprise hospitals need telehealth infrastructure that grows without chaos. A structured scaling process keeps architecture, compliance, and workflows aligned as programs expand. It also helps leaders connect investment to measurable outcomes, not just platform activity. This is where Intellivon becomes valuable as a delivery partner, because execution requires both healthcare context and enterprise engineering depth.
How Intellivon Solves Common Telehealth Scaling Mistakes
Most telehealth scaling failures stem from architectural shortcuts, fragmented governance, and workflow misalignment, all of which can be corrected through enterprise-grade platform design and execution.
Intellivon’s role is to identify these patterns early and correct them through architecture, integration, and governance, not through surface-level fixes. Below are the most common scaling mistakes and how they are resolved.
1. Treating Telehealth As A Standalone Tool
Many hospitals expand telehealth as a separate application layered onto existing systems. This creates parallel workflows, duplicate data entry, and fragmented ownership. As usage grows, clinicians switch between systems mid-care, increasing friction and error risk.
How Intellivon solves it:
Intellivon designs telehealth as an operating layer integrated into core hospital systems. Virtual care workflows align directly with EHR scheduling, documentation, and billing. This removes parallel processes and restores continuity across care delivery.
2. Scaling Volume Before Fixing Workflows
Hospitals often increase visit capacity without standardizing workflows first. Each department adapts telehealth independently, leading to inconsistent triage, follow-ups, and escalation paths. At scale, this results in missed actions and uneven patient experiences.
How Intellivon solves it:
Our experts establish shared workflow orchestration across service lines. Rules-based routing, standardized follow-up logic, and clear escalation models are enforced at the platform level. This ensures growth does not dilute care quality or accountability.
2. Overloading Infrastructure Instead Of Redesigning It
When performance degrades, the default response is to add servers or licenses. This treats symptoms rather than causes. Tightly coupled services continue to compete for resources, and performance issues persist during peak demand.
How Intellivon solves it:
Intellivon restructures telehealth platforms using modular, service-based architectures. Video, scheduling, messaging, and integrations scale independently. This limits the impact of demand spikes and stabilizes performance under load.
3. Leaving Security And Compliance Until After Scale
Security controls that work for pilots often break at enterprise scale. Fragmented identity systems, inconsistent logging, and unclear access rules create audit gaps. These issues usually surface during incidents or regulatory reviews.
How Intellivon solves it:
Our healthcare platform architects embed security and compliance into the foundation of telehealth platforms. Centralized identity, role-based access, and unified audit trails are enforced across all interactions. This reduces risk while maintaining clinical efficiency.
4. Lacking Visibility Into Performance And ROI
As telehealth expands, leaders lose clear insight into what is working. Utilization rises, but outcomes, costs, and productivity remain opaque. Without visibility, investment decisions become reactive.
How Intellivon solves it:
Intellivon implements analytics and observability tied to real operational signals. Performance, utilization, outcomes, and financial metrics are tracked together. This gives leadership a clear view of impact and informs confident scaling decisions.
Telehealth scaling challenges emerge when growth outpaces structure, governance, and integration. Intellivon addresses these issues by redesigning how telehealth is built and operated, not by adding surface-level fixes. The result is a platform that scales with control, clarity, and measurable value.
Conclusion
Telehealth has reached a point where scale is no longer optional for large hospital systems. What determines success now is not adoption speed, but how well virtual care is designed, governed, and integrated into core operations. When telehealth is treated as shared infrastructure, hospitals gain control over performance, compliance, cost, and clinical continuity. When it is treated as a collection of tools, growth introduces friction and risk.
Enterprise leaders who approach telehealth scaling deliberately see impact faster. Workflows stabilize, clinicians regain confidence, and financial signals become clearer. More importantly, virtual care becomes a dependable extension of the hospital’s operating model, not a parallel system that needs constant intervention. This shift turns telehealth from a cost center into a growth and access enabler.
Why Choose Intellivon To Scale Your Telehealth Infrastructure?
At Intellivon, we build scalable telehealth platforms as enterprise operating systems, not virtual care tools extended beyond their limits. Our platforms are designed to govern how patients enter care, how clinicians deliver and document virtual services, and how security, performance, and accountability are maintained as telehealth expands across departments, facilities, and regions.
Each solution is engineered for healthcare organizations operating at enterprise scale. Platforms are architecture-first and compliance-led, with telehealth embedded into EHR workflows, identity controls, data governance, and operational monitoring layers. As virtual care programs grow in volume and complexity, clinical oversight, system reliability, and financial predictability remain stable rather than reactive.
Why Partner With Intellivon?
- Enterprise-grade telehealth architecture aligned with multi-hospital scale, service-line expansion, and long-term platform sustainability
- Deep interoperability expertise across EHRs, care management systems, diagnostics, identity platforms, analytics, and enterprise infrastructure
- Compliance-by-design delivery supporting HIPAA, regional data requirements, audit readiness, and clinical accountability at scale
- Performance and reliability engineering that prevents degradation during peak demand and sustained concurrency
- AI-assisted orchestration and analytics that improve triage, utilization, and operational efficiency without removing clinician control
- Proven enterprise delivery model with phased rollout, workflow validation, and predictable scaling across regions and care models
Talk to Intellivon’s healthcare platform architects to explore how a scalable telehealth infrastructure can integrate into your existing ecosystem, reduce operational friction, and support growth without compromising governance or care quality.
FAQs
Q1. How do enterprise hospitals scale telehealth without disrupting clinical workflows?
A1. Enterprise hospitals scale telehealth successfully by embedding virtual care directly into existing EHR and clinical workflows. Scheduling, documentation, orders, billing, and follow-ups must operate through the same systems clinicians already use.
This avoids parallel processes and reduces manual coordination as volume grows. Workflow orchestration, not additional tools, is what preserves continuity at scale.
Q2. What infrastructure is required to scale telehealth across multiple hospitals?
Scaling telehealth across hospital networks requires a layered architecture, not just more capacity. This includes cloud and compute elasticity, modular application services, asynchronous integrations, centralized identity, and governed data layers.
Each layer must scale independently to prevent performance issues from cascading. Without this separation, growth introduces fragility instead of resilience.
Q3. Why do telehealth platforms slow down as patient volume increases?
A3. Telehealth platforms slow down when tightly coupled systems compete for shared resources. Synchronous EHR integrations, monolithic services, and unmanaged video workloads create latency under concurrency.
These issues often appear as longer join times and delayed documentation rather than outages. Redesigning architecture, not adding servers, resolves the root cause.
Q4. How can hospitals maintain security and compliance while scaling telehealth?
Hospitals maintain security at scale by enforcing centralized identity, role-based access, and unified audit logging across all telehealth interactions. Security must be embedded into platform design rather than applied after deployment.
This approach ensures access decisions remain consistent and auditable as users, devices, and regions increase. Compliance becomes operational, not reactive.
Q5. What business outcomes should hospitals expect from scaled telehealth infrastructure?
A5. When telehealth is scaled correctly, hospitals see reduced no-shows, improved clinician utilization, and more predictable operational costs. Virtual transition-of-care programs often reduce readmissions and follow-up gaps.
Over time, leadership gains clearer ROI visibility tied to utilization, outcomes, and staffing efficiency. Telehealth shifts from a cost center to a growth enabler.